Sulfonylurea: Difference between revisions
CrafterNova (talk | contribs) removed some editorializing words, relocated medical uses Tags: Mobile edit Mobile web edit Advanced mobile edit |
No edit summary |
||
| (32 intermediate revisions by 13 users not shown) | |||
| Line 1: | Line 1: | ||
{{Short description|Class of organic compounds used in medicine and agriculture}} |
{{Short description|Class of organic compounds used in medicine and agriculture}} |
||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
'''Sulfonylureas''' or '''sulphonylureas''' are a class of [[organic compounds]] used in [[medicine]] and [[agriculture]]. The functional group consists of a [[sulfonyl]] group (-S(=O)<sub>2</sub>) with its sulphur atom bonded to a nitrogen atom of a [[ureylene]] group (N,N-dehydrourea, a dehydrogenated derivative of [[urea]]). The side chains R<sub>1</sub> and R<sub>2</sub> distinguish various sulfonylureas. Sulfonylureas are the most widely used herbicide.<ref>{{Citation |last1=Costello |first1=Ryan A. |title=Sulfonylureas |date=2024 |work=StatPearls |url=http://www.ncbi.nlm.nih.gov/books/NBK513225/ |access-date=2024-08-01 |place=Treasure Island (FL) |publisher=StatPearls Publishing |pmid=30020597 |last2=Nicolas |first2=Samar |last3=Shivkumar |first3=Abhijit}}</ref> |
|||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
They include [[glibenclamide]] (glyburide), [[glibornuride]], [[gliclazide]],<ref name="J.R. Karmokeretal.2017">{{cite journal | vauthors = Karmoker J, Priya R, Sarkar S, Islam S |year=2017 |title=Comparative in vitro equivalence evaluation of some local Gliclazide brands of Bangladesh |journal=The Pharma Innovation Journal |volume=6|pages=152–157|url= http://www.thepharmajournal.com/archives/2017/vol6issue3/PartC/6-2-15-510.pdf |access-date=2017-05-15}}</ref> [[glipizide]], [[gliquidone]], [[glisoxepide]] and [[glyclopyramide]]. |
|||
| ⚫ | |||
| ⚫ | They include [[glimepiride]], although it is sometimes considered a second-generation drug.<ref>{{cite book |vauthors=Triplitt CL, Reasner CA | chapter=Chapter 83: diabetes mellitus |veditors=DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM | title=Pharmacotherapy: a pathophysiologic approach | edition=8th | location=New York, NY | publisher=McGraw-Hill | year=2011 | pages=1274 | isbn=978-0-07-170354-3 }}</ref><ref name="isbn0-86577-840-X">{{cite book |author=Davidson J |title=Clinical diabetes mellitus: a problem-oriented approach |publisher=Thieme |location=Stuttgart |year=2000 |pages=422 |isbn=978-0-86577-840-5 | url=https://books.google.com/books?id=CRA5N-felmMC&pg=PA422 }}</ref> |
||
==Uses== |
|||
| ⚫ | |||
| ⚫ | They are widely used as [[antidiabetic drug]]s in the management of [[diabetes mellitus type 2]]. They act by increasing [[secretion]] of [[insulin]] from the [[beta cell]]s in the [[pancreas]].<ref>{{cite journal | vauthors = Seino S | title = Cell signalling in insulin secretion: the molecular targets of ATP, cAMP and sulfonylurea | journal = Diabetologia | volume = 55 | issue = 8 | pages = 2096–2108 | date = August 2012 | pmid = 22555472 | doi = 10.1007/s00125-012-2562-9 | s2cid = 7146975 }}</ref> |
||
==Agricultural uses== |
|||
| ⚫ | Sulfonylureas are also used experimentally to inhibit [[interleukin 1 beta]] |
||
| ⚫ | Many sulfonylureas are also used as [[herbicide]]s, because they can interfere with plant [[biosynthesis]] of certain [[amino acids]].<ref name="pmid18234503">{{cite journal | vauthors = Duggleby RG, McCourt JA, Guddat LW | title = Structure and mechanism of inhibition of plant acetohydroxyacid synthase | journal = Plant Physiology and Biochemistry | volume = 46 | issue = 3 | pages = 309–324 | date = March 2008 | pmid = 18234503 | doi = 10.1016/j.plaphy.2007.12.004 | bibcode = 2008PlPB...46..309D }}</ref> |
||
| ⚫ | As [[herbicide]]s sulfonylureas function by interfering with biosynthesis of the amino acids valine, isoleucine, and leucine, specifically via [[acetolactate synthase]] inhibition. Compounds in this class include amidosulfuron, azimsulfuron, bensulfuron-methyl, chlorimuron-ethyl, [[chlorsulfuron]], ethametsulfuron-methyl, cinosulfuron, ethoxysulfuron, [[flazasulfuron]], flupyrsulfuron-methyl-sodium, imazosulfuron, [[metsulfuron-methyl]], nicosulfuron,<ref name="EXTOXNET">{{cite web |title=Nicosulfuron |url=http://extoxnet.orst.edu/pips/nicosulf.htm |access-date=9 May 2013 |publisher=EXTOXNET}}</ref> oxasulfuron, primisulfuron-methyl, prosulfuron, pyrazosulfuron-ethyl, rimsulfuron, [[sulfometuron-methyl]], sulfosulfuron, thifensulfuron-methyl, triasulfuron, [[tribenuron-methyl]], and triflusulfuron-methyl.<ref>Arnold P. Appleby, Franz Müller, Serge Carpy "Weed Control" in Ullmann's Encyclopedia of Industrial Chemistry 2002, Wiley-VCH, Weinheim. {{doi|10.1002/14356007.a28_165}}</ref> These are broad-spectrum herbicides that kill plants weeds or pests by inhibiting the enzyme [[acetolactate synthase]]. In the 1960s, more than {{convert|1|kg/ha|abbr=on}} crop protection chemical was typically applied, while sulfonylureates allow as little as 1% as much material to achieve the same effect.<ref>{{Cite web |title=Pesticides in agriculture and environment: Impacts on human health |url=https://aesacademy.org/books/cae-vol-1/07.pdf |website=aesacademy.org}}</ref><ref name="s1308">{{cite journal |vauthors=Lamberth C, Jeanmart S, Luksch T, Plant A |date=August 2013 |title=Current challenges and trends in the discovery of agrochemicals |journal=Science |volume=341 |issue=6147 |pages=742–6 |bibcode=2013Sci...341..742L |doi=10.1126/science.1237227 |pmid=23950530 |s2cid=206548681}}</ref> |
||
Sulfonylureas are ineffective where there is absolute deficiency of insulin production such as in type 1 diabetes or post-pancreatectomy.{{cn|date=February 2023}} |
|||
| ⚫ | |||
===Treatment of type 2 diabetes=== |
|||
| ⚫ | They are widely used as [[antidiabetic drug]]s in the management of [[diabetes mellitus type 2]]. They act by increasing [[secretion]] of [[insulin]] from the [[beta cell]]s in the [[pancreas]].<ref>{{cite journal | vauthors = Seino S | title = Cell signalling in insulin secretion: the molecular targets of ATP, cAMP and sulfonylurea | journal = Diabetologia | volume = 55 | issue = 8 | pages = 2096–2108 | date = August 2012 | pmid = 22555472 | doi = 10.1007/s00125-012-2562-9 | s2cid = 7146975 }}</ref> |
||
Sulfonylureas are ineffective where there is absolute deficiency of insulin production such as in type 1 diabetes or post-pancreatectomy.<ref>{{Citation |title=Sulfonylureas |date=2012 |work=LiverTox: Clinical and Research Information on Drug-Induced Liver Injury |url=http://www.ncbi.nlm.nih.gov/books/NBK548361/ |access-date=2024-08-01 |place=Bethesda (MD) |publisher=National Institute of Diabetes and Digestive and Kidney Diseases |pmid=31643682}}</ref> |
|||
Sulfonylureas can be used to treat some types of [[neonatal diabetes]]. Historically, people with hyperglycemia and low blood insulin levels were diagnosed with type 1 diabetes by default, but it has been found that patients who receive this diagnosis before 6 months of age are often candidates for receiving sulfonylureas rather than insulin throughout life.<ref>{{cite journal | vauthors = Greeley SA, Tucker SE, Naylor RN, Bell GI, Philipson LH | title = Neonatal diabetes mellitus: a model for personalized medicine | journal = Trends in Endocrinology and Metabolism | volume = 21 | issue = 8 | pages = 464–472 | date = August 2010 | pmid = 20434356 | pmc = 2914172 | doi = 10.1016/j.tem.2010.03.004 }}</ref> |
Sulfonylureas can be used to treat some types of [[neonatal diabetes]]. Historically, people with hyperglycemia and low blood insulin levels were diagnosed with type 1 diabetes by default, but it has been found that patients who receive this diagnosis before 6 months of age are often candidates for receiving sulfonylureas rather than insulin throughout life.<ref>{{cite journal | vauthors = Greeley SA, Tucker SE, Naylor RN, Bell GI, Philipson LH | title = Neonatal diabetes mellitus: a model for personalized medicine | journal = Trends in Endocrinology and Metabolism | volume = 21 | issue = 8 | pages = 464–472 | date = August 2010 | pmid = 20434356 | pmc = 2914172 | doi = 10.1016/j.tem.2010.03.004 }}</ref> |
||
A 2011 [[Cochrane (organisation)|Cochrane]] [[systematic review]] evaluated the effects on treatment of [[Latent autoimmune diabetes in adults|Latent Autoimmune Diabetes in Adults]] (LADA) and found that Sulfonylureas did improve metabolic control of [[glucose]] at 3 and 12 months, even worsening [[Glycated hemoglobin|HbA1c]] levels in some cases, when compared to insulin.<ref name="Brophy_2011">{{cite journal | vauthors = Brophy S, Davies H, Mannan S, Brunt H, Williams R | title = Interventions for latent autoimmune diabetes (LADA) in adults | journal = The Cochrane Database of Systematic Reviews | issue = 9 | pages = CD006165 | date = September 2011 | pmid = 21901702 | pmc = 6486159 | doi = 10.1002/14651858.cd006165.pub3 }}</ref> The same review did not find improvement of fasting C-peptide following treatment with sulfonylurea.<ref name="Brophy_2011" /> Still, it is important to highlight that the studies available to be included in this review presented considerable flaws in quality and design.<ref name="Brophy_2011" /> |
A 2011 [[Cochrane (organisation)|Cochrane]] [[systematic review]] evaluated the effects on treatment of [[Latent autoimmune diabetes in adults|Latent Autoimmune Diabetes in Adults]] (LADA) and found that Sulfonylureas did not improve metabolic control of [[glucose]] at 3 and 12 months, even worsening [[Glycated hemoglobin|HbA1c]] levels in some cases, when compared to insulin.<ref name="Brophy_2011">{{cite journal | vauthors = Brophy S, Davies H, Mannan S, Brunt H, Williams R | title = Interventions for latent autoimmune diabetes (LADA) in adults | journal = The Cochrane Database of Systematic Reviews | issue = 9 | pages = CD006165 | date = September 2011 | volume = 2011 | pmid = 21901702 | pmc = 6486159 | doi = 10.1002/14651858.cd006165.pub3 }}</ref> The same review did not find improvement of fasting C-peptide following treatment with sulfonylurea.<ref name="Brophy_2011" /> Still, it is important to highlight that the studies available to be included in this review presented considerable flaws in quality and design.<ref name="Brophy_2011" /> |
||
While prior sulfonylureas were associated with worse outcomes, newer agents do not appear to increase the risk of death, heart attacks, or strokes.<ref>{{cite journal | vauthors = Rados DV, Pinto LC, Remonti LR, Leitão CB, Gross JL | title = Correction: The Association between Sulfonylurea Use and All-Cause and Cardiovascular Mortality: A Meta-Analysis with Trial Sequential Analysis of Randomized Clinical Trials | journal = PLOS Medicine | volume = 13 | issue = 6 | pages = e1002091 | date = June 2016 | pmid = 27340828 | pmc = 4920361 | doi = 10.1371/journal.pmed.1002091 }}</ref> This is further reinforced by a 2020 |
While prior sulfonylureas were associated with worse outcomes, newer agents do not appear to increase the risk of death, heart attacks, or strokes.<ref>{{cite journal | vauthors = Rados DV, Pinto LC, Remonti LR, Leitão CB, Gross JL | title = Correction: The Association between Sulfonylurea Use and All-Cause and Cardiovascular Mortality: A Meta-Analysis with Trial Sequential Analysis of Randomized Clinical Trials | journal = PLOS Medicine | volume = 13 | issue = 6 | pages = e1002091 | date = June 2016 | pmid = 27340828 | pmc = 4920361 | doi = 10.1371/journal.pmed.1002091 | doi-access = free }}</ref> This is further reinforced by a 2020 Cochrane [[systematic review]] which did not find enough evidence of reduction of all-cause mortality, serious adverse events, cardiovascular mortality, non-fatal [[myocardial infarction]], non-fatal [[stroke]] or end-stage renal disease when comparing [[metformin]] monotherapy to sulfonylureas.<ref name="Gnesin_2020">{{cite journal | vauthors = Gnesin F, Thuesen AC, Kähler LK, Madsbad S, Hemmingsen B | title = Metformin monotherapy for adults with type 2 diabetes mellitus | journal = The Cochrane Database of Systematic Reviews | volume = 2020 | issue = 6 | pages = CD012906 | date = June 2020 | pmid = 32501595 | pmc = 7386876 | doi = 10.1002/14651858.CD012906.pub2 | collaboration = Cochrane Metabolic and Endocrine Disorders Group }}</ref> This same review also did not find improvement in health-related quality of life.<ref name="Gnesin_2020" /> |
||
In individuals with [[Prediabetes|impaired-glucose tolerance]], a 2019 systematic review only found one suitable trial comparing the effects of Sulphonylurea with [[ |
In individuals with [[Prediabetes|impaired-glucose tolerance]], a 2019 systematic review only found one suitable trial comparing the effects of Sulphonylurea with [[metformin]] in reduction or delay of risk of developing type 2 diabetes, however this trial did not report patient-relevant outcomes.<ref>{{cite journal | vauthors = Madsen KS, Chi Y, Metzendorf MI, Richter B, Hemmingsen B | title = Metformin for prevention or delay of type 2 diabetes mellitus and its associated complications in persons at increased risk for the development of type 2 diabetes mellitus | journal = The Cochrane Database of Systematic Reviews | volume = 2019 | issue = 12 | pages = CD008558 | date = December 2019 | pmid = 31794067 | pmc = 6889926 | doi = 10.1002/14651858.CD008558.pub2 | collaboration = Cochrane Metabolic and Endocrine Disorders Group }}</ref> Another [[systematic review]] completed in the same year suggested that there is limited evidence if the combined used of Metformin with Sulphonylurea compared to the combination of Metformin plus another glucose-lowering intervention, provides benefit or harm in mortality, severe adverse events, [[Macrovascular disease|macrovascular]] and [[Microvascular disease|microvascular complications]].<ref name="Madsen_2019">{{cite journal | vauthors = Madsen KS, Kähler P, Kähler LK, Madsbad S, Gnesin F, Metzendorf MI, Richter B, Hemmingsen B | display-authors = 6 | title = Metformin and second- or third-generation sulphonylurea combination therapy for adults with type 2 diabetes mellitus | journal = The Cochrane Database of Systematic Reviews | volume = 4 | issue = 4 | pages = CD012368 | date = April 2019 | pmid = 30998259 | pmc = 6472662 | doi = 10.1002/14651858.CD012368.pub2 | editor-last = Cochrane Metabolic and Endocrine Disorders Group }}</ref> Combined Metformin and Sulphonylurea therapy did appear to lead to higher risk of [[Hypoglycemia]].<ref name="Madsen_2019" /> |
||
===Interleukin-1 β inhibitors=== |
|||
| ⚫ | |||
| ⚫ | Sulfonylureas are also used experimentally to inhibit release of [[interleukin 1 beta]] from the [[NALP3]] (or NLRP3) [[inflammasome]].<ref>{{Cite journal |last=Kulkarni |first=Amol A. |last2=Sajith |first2=Ayyiliath M. |last3=Duarte |first3=Trevor T. |last4=Tena |first4=Anahis |last5=Spencer |first5=Charles T. |last6=Bowen |first6=J. Phillip |date=2020 |title=Design, synthesis, and screening of sulfonylurea-derived NLRP3 inflammasome inhibitors |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7223447/ |journal=Medicinal Chemistry Research |volume=29 |issue=1 |pages=126–135 |doi=10.1007/s00044-019-02466-7 |issn=1054-2523 |pmc=7223447 |pmid=32435125}}</ref><ref>{{cite journal | vauthors = Coll RC, Robertson AA, Chae JJ, Higgins SC, Muñoz-Planillo R, Inserra MC, Vetter I, Dungan LS, Monks BG, Stutz A, Croker DE, Butler MS, Haneklaus M, Sutton CE, Núñez G, Latz E, Kastner DL, Mills KH, Masters SL, Schroder K, Cooper MA, O'Neill LA | display-authors = 6 | title = A small-molecule inhibitor of the NLRP3 inflammasome for the treatment of inflammatory diseases | journal = Nature Medicine | volume = 21 | issue = 3 | pages = 248–255 | date = March 2015 | pmid = 25686105 | pmc = 4392179 | doi = 10.1038/nm.3806 }}</ref> |
||
| ⚫ | Sulfonylureas – as opposed to [[metformin]], the [[thiazolidinedione]]s, [[pramlintide]] and other newer treatments – may induce [[hypoglycemia]] as a result of excesses in insulin production and release. Hypoglycemia appears to happen more often with sulfonylureas than compared to other treatments.<ref>{{cite journal | vauthors = Shyangdan DS, Royle P, Clar C, Sharma P, Waugh N, Snaith A | title = Glucagon-like peptide analogues for type 2 diabetes mellitus | journal = The Cochrane Database of Systematic Reviews | issue = 10 | pages = CD006423 | date = October 2011 | pmid = 21975753 | pmc = 6486297 | doi = 10.1002/14651858.cd006423.pub2 }}</ref> This typically occurs if the dose is too high, and the patient is fasting. Some people attempt to change eating habits to prevent this, however it can be counterproductive. |
||
| ⚫ | |||
| ⚫ | Sulfonylureas – as opposed to [[metformin]], the [[thiazolidinedione]]s, [[pramlintide]] and other newer treatments – may induce [[hypoglycemia]] as a result of excesses in insulin production and release. Hypoglycemia appears to happen more often with sulfonylureas than compared to other treatments.<ref>{{cite journal | vauthors = Shyangdan DS, Royle P, Clar C, Sharma P, Waugh N, Snaith A | title = Glucagon-like peptide analogues for type 2 diabetes mellitus | journal = The Cochrane Database of Systematic Reviews | issue = 10 | pages = CD006423 | date = October 2011 | volume = 2011 | pmid = 21975753 | pmc = 6486297 | doi = 10.1002/14651858.cd006423.pub2 }}</ref> This typically occurs if the dose is too high, and the patient is fasting. Some people attempt to change eating habits to prevent this, however it can be counterproductive. |
||
Like [[insulin]], sulfonylureas can induce weight gain, mainly as a result of their effect to increase insulin levels and thus use of glucose and other metabolic fuels. Other side-effects are: gastrointestinal upset, [[headache]] and [[hypersensitivity]] reactions. |
Like [[insulin]], sulfonylureas can induce weight gain, mainly as a result of their effect to increase insulin levels and thus use of glucose and other metabolic fuels. Other side-effects are: gastrointestinal upset, [[headache]] and [[hypersensitivity]] reactions. |
||
The safety of sulfonylurea therapy in pregnancy is unestablished. Prolonged hypoglycemia (4 to 10 days) has been reported in children borne to mothers taking sulfonylureas at the time of delivery.<ref name="www.accessdata.fda.gov">{{cite web |url=http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/017532s030lbl.pdf |title= Diaßeta (glyburide) Tablets USP | work = Sanofi-Aventis U.S. LLC | publisher = U.S. Food and Drug Administration | date = 2009 }}</ref> Impairment of liver or kidney function increase the risk of hypoglycemia, and are contraindications. Since other antidiabetic drugs cannot be used either under these circumstances, insulin therapy is typically recommended during pregnancy and in liver and [[kidney failure]], although some of the newer agents offer potentially better options. |
The safety of sulfonylurea therapy in pregnancy is unestablished. Prolonged hypoglycemia (4 to 10 days) has been reported in children borne to mothers taking sulfonylureas at the time of delivery.<ref name="www.accessdata.fda.gov">{{cite web |url=http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/017532s030lbl.pdf |title= Diaßeta (glyburide) Tablets USP | work = Sanofi-Aventis U.S. LLC | publisher = U.S. Food and Drug Administration | date = 2009 }}</ref> Impairment of liver or kidney function increase the risk of hypoglycemia, and are contraindications. Since other [[Diabetes medication|antidiabetic]] drugs cannot be used either under these circumstances, insulin therapy is typically recommended during pregnancy and in liver and [[kidney failure]], although some of the newer agents offer potentially better options. |
||
A 2011 Cochrane review found evidence that treatment of [[Latent autoimmune diabetes in adults|LADA]] using sulfonylureas lead to earlier insulin dependence in approximately 30% of cases.<ref name="Brophy_2011" /> |
A 2011 Cochrane review found evidence that treatment of [[Latent autoimmune diabetes in adults|LADA]] using sulfonylureas lead to earlier insulin dependence in approximately 30% of cases.<ref name="Brophy_2011" /> |
||
A 2014 Cochrane review found tentative evidence that people treated with sulfonylureas have fewer non-fatal cardiovascular events than those treated with metformin (RR 0.7) but a higher risk of severe hypoglycemia (RR 5.6). There was not enough data available to determine the risk of mortality or of cardiovascular mortality.<ref>{{cite journal | vauthors = Hemmingsen B, Schroll JB, Wetterslev J, Gluud C, Vaag A, Sonne DP, Lundstrøm LH, Almdal T | display-authors = 6 | title = Sulfonylurea versus metformin monotherapy in patients with type 2 diabetes: a Cochrane systematic review and meta-analysis of randomized clinical trials and trial sequential analysis | journal = CMAJ Open | volume = 2 | issue = 3 | pages = E162–E175 | date = July 2014 | pmid = 25295236 | pmc = 4185978 | doi = 10.9778/cmajo.20130073 }}</ref> An earlier review by the same group found a statistically significant increase in the risk of cardiovascular death for first generation sulfonylureas relative to placebo (RR 2.6) but there was not enough data to determine the relative risk of first generation sulfonylureas relative to insulin (RR 1.4). Likewise it was not possible to determine the relative mortality risk of second generation sulfonylureas relative to metformin (RR 1.0), insulin (RR 1.0), or placebo.<ref>{{cite journal | vauthors = Hemmingsen B, Schroll JB, Lund SS, Wetterslev J, Gluud C, Vaag A, Sonne DP, Lundstrøm LH, Almdal T | display-authors = 6 | title = Sulphonylurea monotherapy for patients with type 2 diabetes mellitus | journal = The Cochrane Database of Systematic Reviews | volume = 4 | issue = 4 | pages = CD009008 | date = April 2013 | pmid = 23633364 | doi = 10.1002/14651858.CD009008.pub2 | veditors = Hemmingsen B }} {{Retracted |
A 2014 Cochrane review found tentative evidence that people treated with sulfonylureas have fewer non-fatal cardiovascular events than those treated with metformin (RR 0.7) but a higher risk of severe hypoglycemia (RR 5.6). There was not enough data available to determine the risk of mortality or of cardiovascular mortality.<ref>{{cite journal | vauthors = Hemmingsen B, Schroll JB, Wetterslev J, Gluud C, Vaag A, Sonne DP, Lundstrøm LH, Almdal T | display-authors = 6 | title = Sulfonylurea versus metformin monotherapy in patients with type 2 diabetes: a Cochrane systematic review and meta-analysis of randomized clinical trials and trial sequential analysis | journal = CMAJ Open | volume = 2 | issue = 3 | pages = E162–E175 | date = July 2014 | pmid = 25295236 | pmc = 4185978 | doi = 10.9778/cmajo.20130073 }}</ref> An earlier review by the same group found a statistically significant increase in the risk of cardiovascular death for first generation sulfonylureas relative to placebo (RR 2.6) but there was not enough data to determine the relative risk of first generation sulfonylureas relative to insulin (RR 1.4). Likewise it was not possible to determine the relative mortality risk of second generation sulfonylureas relative to metformin (RR 1.0), insulin (RR 1.0), or placebo.<ref>{{cite journal | vauthors = Hemmingsen B, Schroll JB, Lund SS, Wetterslev J, Gluud C, Vaag A, Sonne DP, Lundstrøm LH, Almdal T | display-authors = 6 | title = Sulphonylurea monotherapy for patients with type 2 diabetes mellitus | journal = The Cochrane Database of Systematic Reviews | volume = 4 | issue = 4 | pages = CD009008 | date = April 2013 | pmid = 23633364 | doi = 10.1002/14651858.CD009008.pub2 | veditors = Hemmingsen B }} {{Retracted|doi=10.1002/14651858.CD009008.pub3|pmid=26222249|http://retractionwatch.com/2015/09/01/authors-pharma-ties-cause-cochrane-to-withdraw-two-diabetes-reviews/ ''Retraction Watch''}}</ref> The FDA requires sulfonylureas to carry a label warning regarding increased risk of cardiovascular death.<ref name="www.accessdata.fda.gov" /> |
||
A 2020 [[Cochrane (organisation)|Cochrane]] [[systematic review]] comparing [[metformin]] monotherapy to sulfonylureas did not find enough evidence of reduction of all-cause mortality, serious adverse events, cardiovascular mortality, non-fatal [[myocardial infarction]], non-fatal [[stroke]] or [[Chronic kidney disease|end-stage renal disease]].<ref name="Gnesin_2020" /> |
A 2020 [[Cochrane (organisation)|Cochrane]] [[systematic review]] comparing [[metformin]] monotherapy to sulfonylureas did not find enough evidence of reduction of all-cause mortality, serious adverse events, cardiovascular mortality, non-fatal [[myocardial infarction]], non-fatal [[stroke]] or [[Chronic kidney disease|end-stage renal disease]].<ref name="Gnesin_2020" /> |
||
Second-generation sulfonylureas have increased potency by weight, compared to first-generation sulfonylureas. Similarly, ACCORD (Action to Control Cardiovascular Risk in Diabetes)<ref name="pmid18539917">{{cite journal | vauthors = Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH, Probstfield JL, Simons-Morton DG, Friedewald WT | display-authors = 6 | title = Effects of intensive glucose lowering in type 2 diabetes | journal = The New England Journal of Medicine | volume = 358 | issue = 24 | pages = 2545–2559 | date = June 2008 | pmid = 18539917 | pmc = 4551392 | doi = 10.1056/NEJMoa0802743 }}</ref> and the VADT (Veterans Affairs Diabetes Trial)<ref name="pmid19092145">{{cite journal | vauthors = Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD | display-authors = 6 | title = Glucose control and vascular complications in veterans with type 2 diabetes | journal = The New England Journal of Medicine | volume = 360 | issue = 2 | pages = 129–139 | date = January 2009 | pmid = 19092145 | doi = 10.1056/NEJMoa0808431 | s2cid = 16608858 | doi-access = free }}</ref> studies showed no reduction in heart attack or death in patients assigned to tight glucose control with various drugs. |
Second-generation sulfonylureas have increased potency by weight, compared to first-generation sulfonylureas.<ref>{{Citation |title=Sulfonylureas, Second Generation |date=2012 |work=LiverTox: Clinical and Research Information on Drug-Induced Liver Injury |url=https://www.ncbi.nlm.nih.gov/books/NBK548133/ |access-date=2024-08-16 |place=Bethesda (MD) |publisher=National Institute of Diabetes and Digestive and Kidney Diseases |pmid=31643463}}</ref> Similarly, ACCORD (Action to Control Cardiovascular Risk in Diabetes)<ref name="pmid18539917">{{cite journal | vauthors = Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH, Probstfield JL, Simons-Morton DG, Friedewald WT | display-authors = 6 | title = Effects of intensive glucose lowering in type 2 diabetes | journal = The New England Journal of Medicine | volume = 358 | issue = 24 | pages = 2545–2559 | date = June 2008 | pmid = 18539917 | pmc = 4551392 | doi = 10.1056/NEJMoa0802743 }}</ref> and the VADT (Veterans Affairs Diabetes Trial)<ref name="pmid19092145">{{cite journal | vauthors = Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD | display-authors = 6 | title = Glucose control and vascular complications in veterans with type 2 diabetes | journal = The New England Journal of Medicine | volume = 360 | issue = 2 | pages = 129–139 | date = January 2009 | pmid = 19092145 | doi = 10.1056/NEJMoa0808431 | s2cid = 16608858 | doi-access = free }}</ref> studies showed no reduction in heart attack or death in patients assigned to tight glucose control with various drugs. |
||
== Interactions == |
=== Interactions === |
||
Drugs that potentiate or prolong the effects of sulfonylureas and therefore increase the risk of hypoglycemia include [[acetylsalicylic acid]] and derivatives, [[allopurinol]], [[sulfonamide (medicine)|sulfonamide]]s, and [[fibrate]]s. Drugs that worsen [[glucose tolerance]], contravening the effects of antidiabetics, include [[corticosteroid]]s, [[isoniazid]], [[oral contraceptive]]s and other [[estrogen]]s, [[sympathomimetic]]s, and [[thyroid hormone]]s. Sulfonylureas tend to interact with a wide variety of other drugs, but these interactions, as well as their clinical significance, vary from substance to substance.<ref name="AustriaCodex">{{cite book|title=Austria-Codex| veditors = Haberfeld H |publisher=Österreichischer Apothekerverlag| location=Vienna| year=2009| edition=2009/2010| isbn=978-3-85200-196-8|language=de }}</ref><ref name="Arzneistoff-Profile">{{cite book | title = Arzneistoff-Profile | veditors = Dinnendahl V, Fricke U | publisher = Govi Pharmazeutischer Verlag | location = Eschborn, Germany | year = 2010 | edition = 23 | volume = 4 | isbn = 978-3-7741-9846-3 | language = de | name-list-style = vanc }}</ref> |
Drugs that potentiate or prolong the effects of sulfonylureas and therefore increase the risk of hypoglycemia include [[acetylsalicylic acid]] and derivatives, [[allopurinol]], [[sulfonamide (medicine)|sulfonamide]]s, and [[fibrate]]s. Drugs that worsen [[glucose tolerance]], contravening the effects of antidiabetics, include [[corticosteroid]]s, [[isoniazid]], [[oral contraceptive]]s and other [[estrogen]]s, [[sympathomimetic]]s, and [[thyroid hormone]]s. Sulfonylureas tend to interact with a wide variety of other drugs, but these interactions, as well as their clinical significance, vary from substance to substance.<ref name="AustriaCodex">{{cite book|title=Austria-Codex| veditors = Haberfeld H |publisher=Österreichischer Apothekerverlag| location=Vienna| year=2009| edition=2009/2010| isbn=978-3-85200-196-8|language=de }}</ref><ref name="Arzneistoff-Profile">{{cite book | title = Arzneistoff-Profile | veditors = Dinnendahl V, Fricke U | publisher = Govi Pharmazeutischer Verlag | location = Eschborn, Germany | year = 2010 | edition = 23 | volume = 4 | isbn = 978-3-7741-9846-3 | language = de | name-list-style = vanc }}</ref> |
||
== Structure == |
== Structure == |
||
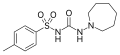
Sulfonylureas contain a central ''S''-arylsulfonylurea structure with a ''p''-substituent on the phenyl ring ('''R<sup>1</sup>''') and various groups terminating the urea ''N''{{prime}} end group ('''R<sup>2</sup>'''). Chemically, this functionality can be easily installed by reacting [[aryl]] [[sulfonamides]] (R<sup>1</sup>—C<sub>6</sub>H<sub>4</sub>—SO<sub>2</sub>NH<sub>2</sub>) with [[isocyanates]] (R<sup>2</sup>—NCO). |
|||
<gallery> |
<gallery> |
||
| Line 57: | Line 56: | ||
</gallery> |
</gallery> |
||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
They include [[glibenclamide]] (glyburide), [[glibornuride]], [[gliclazide]], [[glipizide]], [[gliquidone]], [[glisoxepide]] and [[glyclopyramide]]. |
|||
| ⚫ | |||
| ⚫ | They include [[glimepiride]], although it is sometimes considered a second-generation drug.<ref>{{cite book |vauthors=Triplitt CL, Reasner CA | chapter=Chapter 83: diabetes mellitus |veditors=DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM | title=Pharmacotherapy: a pathophysiologic approach | edition=8th | location=New York, NY | publisher=McGraw-Hill | year=2011 | pages=1274 | isbn=978-0-07-170354-3 }}</ref><ref name="isbn0-86577-840-X">{{cite book |author=Davidson J |title=Clinical diabetes mellitus: a problem-oriented approach |publisher=Thieme |location=Stuttgart |year=2000 |pages=422 |isbn=978-0-86577-840-5 | url=https://books.google.com/books?id=CRA5N-felmMC&pg=PA422 }}</ref> |
||
| ⚫ | |||
[[File:Glucose Insulin Release Pancreas.svg|thumb|Diagram of glucose reduction and insulin release in the pancreas]] |
[[File:Glucose Insulin Release Pancreas.svg|thumb|Diagram of glucose reduction and insulin release in the pancreas]] |
||
Sulfonylureas bind to and close [[ATP-sensitive potassium channel|ATP-sensitive K<sup>+</sup>]] (K<sub>ATP</sub>) channels on the cell membrane of pancreatic [[beta cell]]s, which depolarizes the cell by preventing potassium from exiting. This [[depolarization]] opens voltage-gated [[calcium|Ca]]<sup>2+</sup> channels. The rise in intracellular calcium leads to increased fusion of [[insulin]] granules with the cell membrane, and therefore increased [[Insulin#Synthesis|secretion]] of mature insulin.<ref name="pmid12475777">{{cite journal | vauthors = Proks P, Reimann F, Green N, Gribble F, Ashcroft F | title = Sulfonylurea stimulation of insulin secretion | journal = Diabetes | volume = 51 | issue = Suppl 3 | pages = S368–S376 | date = December 2002 | pmid = 12475777 | doi = 10.2337/diabetes.51.2007.S368 | doi-access = free }}</ref> |
Sulfonylureas bind to and close [[ATP-sensitive potassium channel|ATP-sensitive K<sup>+</sup>]] (K<sub>ATP</sub>) channels on the cell membrane of pancreatic [[beta cell]]s, which depolarizes the cell by preventing potassium from exiting. This [[depolarization]] opens voltage-gated [[calcium|Ca]]<sup>2+</sup> channels. The rise in intracellular calcium leads to increased fusion of [[insulin]] granules with the cell membrane, and therefore increased [[Insulin#Synthesis|secretion]] of mature insulin.<ref name="pmid12475777">{{cite journal | vauthors = Proks P, Reimann F, Green N, Gribble F, Ashcroft F | title = Sulfonylurea stimulation of insulin secretion | journal = Diabetes | volume = 51 | issue = Suppl 3 | pages = S368–S376 | date = December 2002 | pmid = 12475777 | doi = 10.2337/diabetes.51.2007.S368 | doi-access = free }}</ref> |
||
There is some evidence that sulfonylureas also sensitize β-cells to glucose, that they limit glucose production in the [[liver]], that they decrease lipolysis (breakdown and release of [[fatty acid]]s by [[adipose tissue]]) and decrease clearance of insulin by the liver.{{ |
There is some evidence that sulfonylureas also sensitize β-cells to glucose, that they limit glucose production in the [[liver]], that they decrease lipolysis (breakdown and release of [[fatty acid]]s by [[adipose tissue]]) and decrease clearance of insulin by the liver.<ref>{{Cite journal |last1=Yu |first1=Ming |last2=Feng |first2=Xiao-Yu |last3=Yao |first3=Shuai |last4=Wang |first4=Chang |last5=Yang |first5=Ping |date=2022-09-16 |title=Certain sulfonylurea drugs increase serum free fatty acid in diabetic patients: A systematic review and meta-analysis |journal=World Journal of Clinical Cases |volume=10 |issue=26 |pages=9524–9535 |doi=10.12998/wjcc.v10.i26.9524 |doi-access=free |issn=2307-8960 |pmc=9477688 |pmid=36159441}}</ref> |
||
The K<sub>ATP</sub> channel is an octameric complex of the [[inward-rectifier potassium ion channel]] K<sub>ir</sub>6.x and [[sulfonylurea receptor]] SUR which associate with a [[stoichiometry]] of 4:4.<ref name="pmid12475777"/> |
The K<sub>ATP</sub> channel is an octameric complex of the [[inward-rectifier potassium ion channel]] K<sub>ir</sub>6.x and [[sulfonylurea receptor]] SUR which associate with a [[stoichiometry]] of 4:4.<ref name="pmid12475777"/> |
||
Furthermore, it has been shown that sulfonylureas interact with the nucleotide exchange factor [[RAPGEF4|Epac2]].<ref>{{cite journal | vauthors = Zhang CL, Katoh M, Shibasaki T, Minami K, Sunaga Y, Takahashi H, Yokoi N, Iwasaki M, Miki T, Seino S | display-authors = 6 | title = The cAMP sensor Epac2 is a direct target of antidiabetic sulfonylurea drugs | journal = Science | volume = 325 | issue = 5940 | pages = 607–610 | date = July 2009 | pmid = 19644119 | doi = 10.1126/science.1172256 | s2cid = 8923842 | bibcode = 2009Sci...325..607Z }}</ref><ref>{{cite journal | vauthors = Takahashi T, Shibasaki T, Takahashi H, Sugawara K, Ono A, Inoue N, Furuya T, Seino S | display-authors = 6 | title = Antidiabetic sulfonylureas and cAMP cooperatively activate Epac2A | journal = Science Signaling | volume = 6 | issue = 298 | pages = ra94 | date = October 2013 | pmid = 24150255 | doi = 10.1126/scisignal.2004581 | s2cid = 27711862 }}</ref> Mice lacking this factor exhibited a decreased glucose-lowering effect upon sulfonylurea treatment. |
Furthermore, it has been shown that sulfonylureas interact with the nucleotide exchange factor [[RAPGEF4|Epac2]].<ref>{{cite journal | vauthors = Zhang CL, Katoh M, Shibasaki T, Minami K, Sunaga Y, Takahashi H, Yokoi N, Iwasaki M, Miki T, Seino S | display-authors = 6 | title = The cAMP sensor Epac2 is a direct target of antidiabetic sulfonylurea drugs | journal = Science | volume = 325 | issue = 5940 | pages = 607–610 | date = July 2009 | pmid = 19644119 | doi = 10.1126/science.1172256 | s2cid = 8923842 | bibcode = 2009Sci...325..607Z }}</ref><ref>{{cite journal | vauthors = Takahashi T, Shibasaki T, Takahashi H, Sugawara K, Ono A, Inoue N, Furuya T, Seino S | display-authors = 6 | title = Antidiabetic sulfonylureas and cAMP cooperatively activate Epac2A | journal = Science Signaling | volume = 6 | issue = 298 | pages = ra94 | date = October 2013 | pmid = 24150255 | doi = 10.1126/scisignal.2004581 | s2cid = 27711862 | hdl = 20.500.14094/D1005987 | hdl-access = free }}</ref> Mice lacking this factor exhibited a decreased glucose-lowering effect upon sulfonylurea treatment. |
||
==History== |
===History=== |
||
Sulfonylureas were discovered |
Sulfonylureas were discovered in 1942, by the chemist [[:fr:Marcel_Janbon#:~:text=Marcel%20Janbon%2C%20né%20le%2024,professeur%20de%20clinique%20médicale%20français.|Marcel Janbon]] and co-workers in France,<ref name="Janbon_1942">{{cite journal | vauthors = Janbon M, Chaptal J, Vedel A, Schaap J | title = Accidents hypoglycémiques graves par un sulfamidothiodiazol (le VK 57 ou 2254 RP) | journal = Montpellier Med. | volume = 441 | pages = 21–22 | year = 1942 }}</ref> who were studying [[Sulfonamide (medicine)|sulfonamide]] [[antibiotic]]s and discovered that the compound sulfonylurea induced [[hypoglycemia]] in animals.<ref name="pmid12468446">{{cite journal | vauthors = Patlak M | title = New weapons to combat an ancient disease: treating diabetes | journal = FASEB Journal | volume = 16 | issue = 14 | pages = 1853 | date = December 2002 | pmid = 12468446 | doi = 10.1096/fj.02-0974bkt | s2cid = 35412249 | doi-access = free }}</ref> |
||
[[Research and development]] ([[translational research]] and commercial application development) for sulfonylureas as pharmaceuticals (as diagnostic and therapeutic agents in prediabetes and diabetes) happened in the 1950s and 1960s, as explored at ''[[Tolbutamide#History|Tolbutamide § History]]''. |
[[Research and development]] ([[translational research]] and commercial application development) for sulfonylureas as pharmaceuticals (as diagnostic and therapeutic agents in prediabetes and diabetes) happened in the 1950s and 1960s, as explored at ''[[Tolbutamide#History|Tolbutamide § History]]''. |
||
Research and development (translational research and commercial application development) for sulfonylureas as herbicides happened in the 1970s and 1980s, as explored for example in a volume of the Sloan Technology Series focusing on the sociotechnological aspects of agriculture (Canine 1995);<ref name="Canine-1995">{{cite book | vauthors = Canine C |year=1995 |chapter=War on weeds |title=Dream Reaper: The Story of an Old-Fashioned Inventor in the High-Tech, High-Stakes World of Modern Agriculture |series=Sloan Technology Series |pages=189–213 |isbn=9780517472378 }}</ref> the [[DuPont Experimental Station]] led this development.<ref name="Canine-1995"/> |
Research and development (translational research and commercial application development) for sulfonylureas as herbicides happened in the 1970s and 1980s, as explored for example in a volume of the Sloan Technology Series focusing on the sociotechnological aspects of agriculture (Canine 1995);<ref name="Canine-1995">{{cite book | vauthors = Canine C |year=1995 |chapter=War on weeds |title=Dream Reaper: The Story of an Old-Fashioned Inventor in the High-Tech, High-Stakes World of Modern Agriculture |series=Sloan Technology Series |pages=189–213 |isbn=9780517472378 }}</ref> the [[DuPont Experimental Station]] led this development.<ref name="Canine-1995"/> |
||
==Herbicides== |
|||
| ⚫ | |||
== References == |
== References == |
||
Latest revision as of 14:08, 9 October 2024

Sulfonylureas or sulphonylureas are a class of organic compounds used in medicine and agriculture. The functional group consists of a sulfonyl group (-S(=O)2) with its sulphur atom bonded to a nitrogen atom of a ureylene group (N,N-dehydrourea, a dehydrogenated derivative of urea). The side chains R1 and R2 distinguish various sulfonylureas. Sulfonylureas are the most widely used herbicide.[1]
Agricultural uses
[edit]Many sulfonylureas are also used as herbicides, because they can interfere with plant biosynthesis of certain amino acids.[2]
As herbicides sulfonylureas function by interfering with biosynthesis of the amino acids valine, isoleucine, and leucine, specifically via acetolactate synthase inhibition. Compounds in this class include amidosulfuron, azimsulfuron, bensulfuron-methyl, chlorimuron-ethyl, chlorsulfuron, ethametsulfuron-methyl, cinosulfuron, ethoxysulfuron, flazasulfuron, flupyrsulfuron-methyl-sodium, imazosulfuron, metsulfuron-methyl, nicosulfuron,[3] oxasulfuron, primisulfuron-methyl, prosulfuron, pyrazosulfuron-ethyl, rimsulfuron, sulfometuron-methyl, sulfosulfuron, thifensulfuron-methyl, triasulfuron, tribenuron-methyl, and triflusulfuron-methyl.[4] These are broad-spectrum herbicides that kill plants weeds or pests by inhibiting the enzyme acetolactate synthase. In the 1960s, more than 1 kg/ha (0.89 lb/acre) crop protection chemical was typically applied, while sulfonylureates allow as little as 1% as much material to achieve the same effect.[5][6]
Medical uses
[edit]Treatment of type 2 diabetes
[edit]They are widely used as antidiabetic drugs in the management of diabetes mellitus type 2. They act by increasing secretion of insulin from the beta cells in the pancreas.[7]
Sulfonylureas are ineffective where there is absolute deficiency of insulin production such as in type 1 diabetes or post-pancreatectomy.[8]
Sulfonylureas can be used to treat some types of neonatal diabetes. Historically, people with hyperglycemia and low blood insulin levels were diagnosed with type 1 diabetes by default, but it has been found that patients who receive this diagnosis before 6 months of age are often candidates for receiving sulfonylureas rather than insulin throughout life.[9]
A 2011 Cochrane systematic review evaluated the effects on treatment of Latent Autoimmune Diabetes in Adults (LADA) and found that Sulfonylureas did not improve metabolic control of glucose at 3 and 12 months, even worsening HbA1c levels in some cases, when compared to insulin.[10] The same review did not find improvement of fasting C-peptide following treatment with sulfonylurea.[10] Still, it is important to highlight that the studies available to be included in this review presented considerable flaws in quality and design.[10]
While prior sulfonylureas were associated with worse outcomes, newer agents do not appear to increase the risk of death, heart attacks, or strokes.[11] This is further reinforced by a 2020 Cochrane systematic review which did not find enough evidence of reduction of all-cause mortality, serious adverse events, cardiovascular mortality, non-fatal myocardial infarction, non-fatal stroke or end-stage renal disease when comparing metformin monotherapy to sulfonylureas.[12] This same review also did not find improvement in health-related quality of life.[12]
In individuals with impaired-glucose tolerance, a 2019 systematic review only found one suitable trial comparing the effects of Sulphonylurea with metformin in reduction or delay of risk of developing type 2 diabetes, however this trial did not report patient-relevant outcomes.[13] Another systematic review completed in the same year suggested that there is limited evidence if the combined used of Metformin with Sulphonylurea compared to the combination of Metformin plus another glucose-lowering intervention, provides benefit or harm in mortality, severe adverse events, macrovascular and microvascular complications.[14] Combined Metformin and Sulphonylurea therapy did appear to lead to higher risk of Hypoglycemia.[14]
Interleukin-1 β inhibitors
[edit]Sulfonylureas are also used experimentally to inhibit release of interleukin 1 beta from the NALP3 (or NLRP3) inflammasome.[15][16]
Side effects
[edit]Sulfonylureas – as opposed to metformin, the thiazolidinediones, pramlintide and other newer treatments – may induce hypoglycemia as a result of excesses in insulin production and release. Hypoglycemia appears to happen more often with sulfonylureas than compared to other treatments.[17] This typically occurs if the dose is too high, and the patient is fasting. Some people attempt to change eating habits to prevent this, however it can be counterproductive.
Like insulin, sulfonylureas can induce weight gain, mainly as a result of their effect to increase insulin levels and thus use of glucose and other metabolic fuels. Other side-effects are: gastrointestinal upset, headache and hypersensitivity reactions.
The safety of sulfonylurea therapy in pregnancy is unestablished. Prolonged hypoglycemia (4 to 10 days) has been reported in children borne to mothers taking sulfonylureas at the time of delivery.[18] Impairment of liver or kidney function increase the risk of hypoglycemia, and are contraindications. Since other antidiabetic drugs cannot be used either under these circumstances, insulin therapy is typically recommended during pregnancy and in liver and kidney failure, although some of the newer agents offer potentially better options.
A 2011 Cochrane review found evidence that treatment of LADA using sulfonylureas lead to earlier insulin dependence in approximately 30% of cases.[10]
A 2014 Cochrane review found tentative evidence that people treated with sulfonylureas have fewer non-fatal cardiovascular events than those treated with metformin (RR 0.7) but a higher risk of severe hypoglycemia (RR 5.6). There was not enough data available to determine the risk of mortality or of cardiovascular mortality.[19] An earlier review by the same group found a statistically significant increase in the risk of cardiovascular death for first generation sulfonylureas relative to placebo (RR 2.6) but there was not enough data to determine the relative risk of first generation sulfonylureas relative to insulin (RR 1.4). Likewise it was not possible to determine the relative mortality risk of second generation sulfonylureas relative to metformin (RR 1.0), insulin (RR 1.0), or placebo.[20] The FDA requires sulfonylureas to carry a label warning regarding increased risk of cardiovascular death.[18]
A 2020 Cochrane systematic review comparing metformin monotherapy to sulfonylureas did not find enough evidence of reduction of all-cause mortality, serious adverse events, cardiovascular mortality, non-fatal myocardial infarction, non-fatal stroke or end-stage renal disease.[12]
Second-generation sulfonylureas have increased potency by weight, compared to first-generation sulfonylureas.[21] Similarly, ACCORD (Action to Control Cardiovascular Risk in Diabetes)[22] and the VADT (Veterans Affairs Diabetes Trial)[23] studies showed no reduction in heart attack or death in patients assigned to tight glucose control with various drugs.
Interactions
[edit]Drugs that potentiate or prolong the effects of sulfonylureas and therefore increase the risk of hypoglycemia include acetylsalicylic acid and derivatives, allopurinol, sulfonamides, and fibrates. Drugs that worsen glucose tolerance, contravening the effects of antidiabetics, include corticosteroids, isoniazid, oral contraceptives and other estrogens, sympathomimetics, and thyroid hormones. Sulfonylureas tend to interact with a wide variety of other drugs, but these interactions, as well as their clinical significance, vary from substance to substance.[24][25]
Structure
[edit]Sulfonylureas contain a central S-arylsulfonylurea structure with a p-substituent on the phenyl ring (R1) and various groups terminating the urea N′ end group (R2). Chemically, this functionality can be easily installed by reacting aryl sulfonamides (R1—C6H4—SO2NH2) with isocyanates (R2—NCO).
-
Chlorpropamide (1st generation)
-
Tolazamide (1st generation)
-
Gliclazide (2nd generation)
-
Glimepiride (2nd generation)
Classification
[edit]Sulfonylureas are divided into 3 classes on basis of therapeutic efficiency of their antidiabetic action:
- First-generation drugs:
They include acetohexamide, carbutamide, chlorpropamide, glycyclamide (tolcyclamide), metahexamide, tolazamide and tolbutamide.
- Second-generation drugs:
They include glibenclamide (glyburide), glibornuride, gliclazide, glipizide, gliquidone, glisoxepide and glyclopyramide.
- Third-generation drugs:
They include glimepiride, although it is sometimes considered a second-generation drug.[26][27]
Mechanism of action
[edit]
Sulfonylureas bind to and close ATP-sensitive K+ (KATP) channels on the cell membrane of pancreatic beta cells, which depolarizes the cell by preventing potassium from exiting. This depolarization opens voltage-gated Ca2+ channels. The rise in intracellular calcium leads to increased fusion of insulin granules with the cell membrane, and therefore increased secretion of mature insulin.[28]
There is some evidence that sulfonylureas also sensitize β-cells to glucose, that they limit glucose production in the liver, that they decrease lipolysis (breakdown and release of fatty acids by adipose tissue) and decrease clearance of insulin by the liver.[29]
The KATP channel is an octameric complex of the inward-rectifier potassium ion channel Kir6.x and sulfonylurea receptor SUR which associate with a stoichiometry of 4:4.[28]
Furthermore, it has been shown that sulfonylureas interact with the nucleotide exchange factor Epac2.[30][31] Mice lacking this factor exhibited a decreased glucose-lowering effect upon sulfonylurea treatment.
History
[edit]Sulfonylureas were discovered in 1942, by the chemist Marcel Janbon and co-workers in France,[32] who were studying sulfonamide antibiotics and discovered that the compound sulfonylurea induced hypoglycemia in animals.[33]
Research and development (translational research and commercial application development) for sulfonylureas as pharmaceuticals (as diagnostic and therapeutic agents in prediabetes and diabetes) happened in the 1950s and 1960s, as explored at Tolbutamide § History.
Research and development (translational research and commercial application development) for sulfonylureas as herbicides happened in the 1970s and 1980s, as explored for example in a volume of the Sloan Technology Series focusing on the sociotechnological aspects of agriculture (Canine 1995);[34] the DuPont Experimental Station led this development.[34]
References
[edit]- ^ Costello, Ryan A.; Nicolas, Samar; Shivkumar, Abhijit (2024), "Sulfonylureas", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30020597, retrieved 2024-08-01
- ^ Duggleby RG, McCourt JA, Guddat LW (March 2008). "Structure and mechanism of inhibition of plant acetohydroxyacid synthase". Plant Physiology and Biochemistry. 46 (3): 309–324. Bibcode:2008PlPB...46..309D. doi:10.1016/j.plaphy.2007.12.004. PMID 18234503.
- ^ "Nicosulfuron". EXTOXNET. Retrieved 9 May 2013.
- ^ Arnold P. Appleby, Franz Müller, Serge Carpy "Weed Control" in Ullmann's Encyclopedia of Industrial Chemistry 2002, Wiley-VCH, Weinheim. doi:10.1002/14356007.a28_165
- ^ "Pesticides in agriculture and environment: Impacts on human health" (PDF). aesacademy.org.
- ^ Lamberth C, Jeanmart S, Luksch T, Plant A (August 2013). "Current challenges and trends in the discovery of agrochemicals". Science. 341 (6147): 742–6. Bibcode:2013Sci...341..742L. doi:10.1126/science.1237227. PMID 23950530. S2CID 206548681.
- ^ Seino S (August 2012). "Cell signalling in insulin secretion: the molecular targets of ATP, cAMP and sulfonylurea". Diabetologia. 55 (8): 2096–2108. doi:10.1007/s00125-012-2562-9. PMID 22555472. S2CID 7146975.
- ^ "Sulfonylureas", LiverTox: Clinical and Research Information on Drug-Induced Liver Injury, Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases, 2012, PMID 31643682, retrieved 2024-08-01
- ^ Greeley SA, Tucker SE, Naylor RN, Bell GI, Philipson LH (August 2010). "Neonatal diabetes mellitus: a model for personalized medicine". Trends in Endocrinology and Metabolism. 21 (8): 464–472. doi:10.1016/j.tem.2010.03.004. PMC 2914172. PMID 20434356.
- ^ a b c d Brophy S, Davies H, Mannan S, Brunt H, Williams R (September 2011). "Interventions for latent autoimmune diabetes (LADA) in adults". The Cochrane Database of Systematic Reviews. 2011 (9): CD006165. doi:10.1002/14651858.cd006165.pub3. PMC 6486159. PMID 21901702.
- ^ Rados DV, Pinto LC, Remonti LR, Leitão CB, Gross JL (June 2016). "Correction: The Association between Sulfonylurea Use and All-Cause and Cardiovascular Mortality: A Meta-Analysis with Trial Sequential Analysis of Randomized Clinical Trials". PLOS Medicine. 13 (6): e1002091. doi:10.1371/journal.pmed.1002091. PMC 4920361. PMID 27340828.
- ^ a b c Gnesin F, Thuesen AC, Kähler LK, Madsbad S, Hemmingsen B, et al. (Cochrane Metabolic and Endocrine Disorders Group) (June 2020). "Metformin monotherapy for adults with type 2 diabetes mellitus". The Cochrane Database of Systematic Reviews. 2020 (6): CD012906. doi:10.1002/14651858.CD012906.pub2. PMC 7386876. PMID 32501595.
- ^ Madsen KS, Chi Y, Metzendorf MI, Richter B, Hemmingsen B, et al. (Cochrane Metabolic and Endocrine Disorders Group) (December 2019). "Metformin for prevention or delay of type 2 diabetes mellitus and its associated complications in persons at increased risk for the development of type 2 diabetes mellitus". The Cochrane Database of Systematic Reviews. 2019 (12): CD008558. doi:10.1002/14651858.CD008558.pub2. PMC 6889926. PMID 31794067.
- ^ a b Madsen KS, Kähler P, Kähler LK, Madsbad S, Gnesin F, Metzendorf MI, et al. (April 2019). Cochrane Metabolic and Endocrine Disorders Group (ed.). "Metformin and second- or third-generation sulphonylurea combination therapy for adults with type 2 diabetes mellitus". The Cochrane Database of Systematic Reviews. 4 (4): CD012368. doi:10.1002/14651858.CD012368.pub2. PMC 6472662. PMID 30998259.
- ^ Kulkarni, Amol A.; Sajith, Ayyiliath M.; Duarte, Trevor T.; Tena, Anahis; Spencer, Charles T.; Bowen, J. Phillip (2020). "Design, synthesis, and screening of sulfonylurea-derived NLRP3 inflammasome inhibitors". Medicinal Chemistry Research. 29 (1): 126–135. doi:10.1007/s00044-019-02466-7. ISSN 1054-2523. PMC 7223447. PMID 32435125.
- ^ Coll RC, Robertson AA, Chae JJ, Higgins SC, Muñoz-Planillo R, Inserra MC, et al. (March 2015). "A small-molecule inhibitor of the NLRP3 inflammasome for the treatment of inflammatory diseases". Nature Medicine. 21 (3): 248–255. doi:10.1038/nm.3806. PMC 4392179. PMID 25686105.
- ^ Shyangdan DS, Royle P, Clar C, Sharma P, Waugh N, Snaith A (October 2011). "Glucagon-like peptide analogues for type 2 diabetes mellitus". The Cochrane Database of Systematic Reviews. 2011 (10): CD006423. doi:10.1002/14651858.cd006423.pub2. PMC 6486297. PMID 21975753.
- ^ a b "Diaßeta (glyburide) Tablets USP" (PDF). Sanofi-Aventis U.S. LLC. U.S. Food and Drug Administration. 2009.
- ^ Hemmingsen B, Schroll JB, Wetterslev J, Gluud C, Vaag A, Sonne DP, et al. (July 2014). "Sulfonylurea versus metformin monotherapy in patients with type 2 diabetes: a Cochrane systematic review and meta-analysis of randomized clinical trials and trial sequential analysis". CMAJ Open. 2 (3): E162–E175. doi:10.9778/cmajo.20130073. PMC 4185978. PMID 25295236.
- ^ Hemmingsen B, Schroll JB, Lund SS, Wetterslev J, Gluud C, Vaag A, et al. (April 2013). Hemmingsen B (ed.). "Sulphonylurea monotherapy for patients with type 2 diabetes mellitus". The Cochrane Database of Systematic Reviews. 4 (4): CD009008. doi:10.1002/14651858.CD009008.pub2. PMID 23633364. (Retracted, see doi:10.1002/14651858.CD009008.pub3, PMID 26222249, Retraction Watch)
- ^ "Sulfonylureas, Second Generation", LiverTox: Clinical and Research Information on Drug-Induced Liver Injury, Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases, 2012, PMID 31643463, retrieved 2024-08-16
- ^ Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, Buse JB, et al. (June 2008). "Effects of intensive glucose lowering in type 2 diabetes". The New England Journal of Medicine. 358 (24): 2545–2559. doi:10.1056/NEJMoa0802743. PMC 4551392. PMID 18539917.
- ^ Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. (January 2009). "Glucose control and vascular complications in veterans with type 2 diabetes". The New England Journal of Medicine. 360 (2): 129–139. doi:10.1056/NEJMoa0808431. PMID 19092145. S2CID 16608858.
- ^ Haberfeld H, ed. (2009). Austria-Codex (in German) (2009/2010 ed.). Vienna: Österreichischer Apothekerverlag. ISBN 978-3-85200-196-8.
- ^ Dinnendahl V, Fricke U, eds. (2010). Arzneistoff-Profile (in German). Vol. 4 (23 ed.). Eschborn, Germany: Govi Pharmazeutischer Verlag. ISBN 978-3-7741-9846-3.
- ^ Triplitt CL, Reasner CA (2011). "Chapter 83: diabetes mellitus". In DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM (eds.). Pharmacotherapy: a pathophysiologic approach (8th ed.). New York, NY: McGraw-Hill. p. 1274. ISBN 978-0-07-170354-3.
- ^ Davidson J (2000). Clinical diabetes mellitus: a problem-oriented approach. Stuttgart: Thieme. p. 422. ISBN 978-0-86577-840-5.
- ^ a b Proks P, Reimann F, Green N, Gribble F, Ashcroft F (December 2002). "Sulfonylurea stimulation of insulin secretion". Diabetes. 51 (Suppl 3): S368–S376. doi:10.2337/diabetes.51.2007.S368. PMID 12475777.
- ^ Yu, Ming; Feng, Xiao-Yu; Yao, Shuai; Wang, Chang; Yang, Ping (2022-09-16). "Certain sulfonylurea drugs increase serum free fatty acid in diabetic patients: A systematic review and meta-analysis". World Journal of Clinical Cases. 10 (26): 9524–9535. doi:10.12998/wjcc.v10.i26.9524. ISSN 2307-8960. PMC 9477688. PMID 36159441.
- ^ Zhang CL, Katoh M, Shibasaki T, Minami K, Sunaga Y, Takahashi H, et al. (July 2009). "The cAMP sensor Epac2 is a direct target of antidiabetic sulfonylurea drugs". Science. 325 (5940): 607–610. Bibcode:2009Sci...325..607Z. doi:10.1126/science.1172256. PMID 19644119. S2CID 8923842.
- ^ Takahashi T, Shibasaki T, Takahashi H, Sugawara K, Ono A, Inoue N, et al. (October 2013). "Antidiabetic sulfonylureas and cAMP cooperatively activate Epac2A". Science Signaling. 6 (298): ra94. doi:10.1126/scisignal.2004581. hdl:20.500.14094/D1005987. PMID 24150255. S2CID 27711862.
- ^ Janbon M, Chaptal J, Vedel A, Schaap J (1942). "Accidents hypoglycémiques graves par un sulfamidothiodiazol (le VK 57 ou 2254 RP)". Montpellier Med. 441: 21–22.
- ^ Patlak M (December 2002). "New weapons to combat an ancient disease: treating diabetes". FASEB Journal. 16 (14): 1853. doi:10.1096/fj.02-0974bkt. PMID 12468446. S2CID 35412249.
- ^ a b Canine C (1995). "War on weeds". Dream Reaper: The Story of an Old-Fashioned Inventor in the High-Tech, High-Stakes World of Modern Agriculture. Sloan Technology Series. pp. 189–213. ISBN 9780517472378.