Acid–base disorder: Difference between revisions
m →Classification: Spelling changed to match 'alkalemia' |
Ozzie10aaaa (talk | contribs) Reference edited with ProveIt #proveit |
||
| (23 intermediate revisions by 15 users not shown) | |||
| Line 1: | Line 1: | ||
{{Short description|Abnormality of the human body's normal balance of acids and bases}} |
|||
{{ |
{{More citations needed|date=December 2010}} |
||
{{Infobox disease | |
|||
{{Infobox medical condition (new) |
|||
Name = Acid–base imbalance | |
|||
| name = Acid–base imbalance |
|||
| image = Davenport fig 10.jpg |
|||
| ⚫ | |||
| ⚫ | |||
| pronounce = |
|||
| ⚫ | |||
| specialty = [[Internal medicine]] |
|||
| ⚫ | |||
| symptoms = |
|||
| complications = |
|||
| onset = |
|||
| duration = |
|||
| ⚫ | |||
| types = |
|||
| ⚫ | |||
| causes = |
|||
| risks = |
|||
| diagnosis = |
|||
| differential = |
|||
| prevention = |
|||
| treatment = |
|||
| medication = |
|||
| prognosis = |
|||
| frequency = |
|||
| deaths = |
|||
}} |
}} |
||
| ⚫ | |||
'''Acid–base imbalance''' is an abnormality of the human body's normal [[acid–base homeostasis|balance of acids and bases]] that causes the [[blood plasma|plasma]] [[pH]] to deviate out of the normal range (7.35 to 7.45). In the [[fetus]], the normal range differs based on which umbilical vessel is sampled ([[umbilical vein]] pH is normally 7.25 to 7.45; [[umbilical artery]] pH is normally 7.18 to 7.38).<ref name="Yeomans">{{ |
'''Acid–base imbalance''' is an abnormality of the human body's normal [[acid–base homeostasis|balance of acids and bases]] that causes the [[blood plasma|plasma]] [[pH]] to deviate out of the normal range (7.35 to 7.45). In the [[fetus]], the normal range differs based on which umbilical vessel is sampled ([[umbilical vein]] pH is normally 7.25 to 7.45; [[umbilical artery]] pH is normally 7.18 to 7.38).<ref name="Yeomans">{{Cite journal |last=Yeomans |first=ER |last2=Hauth, JC |last3=Gilstrap, LC III |last4=Strickland DM |year=1985 |title=Umbilical cord pH, PCO2, and bicarbonate following uncomplicated term vaginal deliveries (146 infants) |journal=Am J Obstet Gynecol |volume=151 |issue=6 |pages=798–800 |doi=10.1016/0002-9378(85)90523-x |pmid=3919587}}</ref> It can exist in varying levels of severity, some life-threatening. |
||
==Classification== |
==Classification== |
||
| ⚫ | |||
| ⚫ | |||
An excess of acid is called [[acidosis]] or acidemia |
An excess of acid is called [[acidosis]] or acidemia, while an excess in bases is called [[alkalosis]] or alkalemia. The process that causes the imbalance is classified based on the cause of the disturbance (respiratory or metabolic) and the direction of change in pH (acidosis or alkalosis). This yields the following four basic processes: |
||
{| class="wikitable" |
{| class="wikitable" |
||
! process || [[pH]] || {{CO2|link=yes}} || compensation |
|||
|- |
|- |
||
| [[metabolic acidosis]] || down || down || respiratory |
| style="text-align:right;" | [[metabolic acidosis]] || style="text-align:center;" |{{down}} || style="text-align:center;" | {{down}} || respiratory |
||
|- |
|- |
||
| [[respiratory acidosis]] || down || up || renal |
| style="text-align:right;" | [[respiratory acidosis]] || style="text-align:center;" |{{down}} || style="text-align:center;" |{{up}} || renal |
||
|- |
|- |
||
| [[metabolic alkalosis]] || up || up || respiratory |
| style="text-align:right;" | [[metabolic alkalosis]] || style="text-align:center;" |{{up}} || style="text-align:center;" |{{up}} || respiratory |
||
|- |
|- |
||
| [[respiratory alkalosis]] || up |
| style="text-align:right;" | [[respiratory alkalosis]] || style="text-align:center;" |{{up}} || style="text-align:center;" |{{down}} || renal |
||
|} |
|} |
||
===Mixed disorders=== |
===Mixed disorders=== |
||
The presence of only one of the above derangements is called a ''simple'' acid–base disorder. In a ''mixed'' disorder more than one is occurring at the same time.<ref name="urlMixed Acid Base Disorders: Acid Base Tutorial, University of Connecticut Health Center">{{ |
The presence of only one of the above derangements is called a ''simple'' acid–base disorder. In a ''mixed'' disorder, more than one is occurring at the same time.<ref name="urlMixed Acid Base Disorders: Acid Base Tutorial, University of Connecticut Health Center">{{Cite web |title=Mixed Acid Base Disorders: Acid Base Tutorial, University of Connecticut Health Center |url=http://fitsweb.uchc.edu/student/selectives/TimurGraham/Mixed_Acid_Base_Disorders.html |url-status=dead |archive-url=https://web.archive.org/web/20090426054258/http://fitsweb.uchc.edu/student/selectives/TimurGraham/Mixed_Acid_Base_Disorders.html |archive-date=2009-04-26 |access-date=2009-05-09}}</ref> Mixed disorders may feature an acidosis and alkosis at the same time that partially counteract each other, or there can be two different conditions affecting the pH in the same direction. The phrase "mixed acidosis", for example, refers to [[metabolic acidosis]] in conjunction with [[respiratory acidosis]]. Any combination is possible, as metabolic acidosis and alkalosis can co exist together. |
||
===Calculation of imbalance=== |
===Calculation of imbalance=== |
||
The traditional approach to the study of acid–base physiology has been the [[empirical]] approach. The main variants are the [[base excess]] approach and the [[bicarbonate]] approach. The [[Quantitative analysis (chemistry)|quantitative]] approach introduced by [[Peter A Stewart]] in 1978<ref>{{ |
The traditional approach to the study of acid–base physiology has been the [[empirical]] approach. The main variants are the [[base excess]] approach and the [[bicarbonate]] approach. The [[Quantitative analysis (chemistry)|quantitative]] approach introduced by [[Peter A Stewart]] in 1978<ref>{{Cite journal |last=Stewart P |year=1978 |title=Independent and dependent variables of acid-base control |journal=Respir Physiol |volume=33 |issue=1 |pages=9–26 |doi=10.1016/0034-5687(78)90079-8 |pmid=27857}}</ref> is newer. |
||
==Causes== |
==Causes== |
||
| Line 54: | Line 63: | ||
==Compensation== |
==Compensation== |
||
{{Acids and bases}} |
{{Acids and bases}} |
||
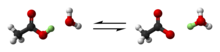
The body's acid–base balance is tightly regulated. Several [[buffering agent]]s exist which reversibly bind hydrogen ions and impede any change in pH. [[Extracellular]] buffers include [[bicarbonate]] and [[ammonia]], while [[protein]]s and [[phosphate]] act as [[intracellular]] buffers. The [[bicarbonate buffering system]] is especially key, as [[carbon dioxide]] (CO<sub>2</sub>) can be shifted through [[carbonic acid]] (H<sub>2</sub>CO<sub>3</sub>) to hydrogen ions and [[bicarbonate]] (HCO<sub>3</sub><sup>−</sup>) as shown below. |
The body's [[acid–base balance]] is tightly regulated. Several [[buffering agent]]s exist which reversibly bind hydrogen ions and impede any change in pH. [[Extracellular]] buffers include [[bicarbonate]] and [[ammonia]], while [[protein]]s and [[phosphate]] act as [[intracellular]] buffers. The [[bicarbonate buffering system]] is especially key, as [[carbon dioxide]] (CO<sub>2</sub>) can be shifted through [[carbonic acid]] (H<sub>2</sub>CO<sub>3</sub>) to hydrogen ions and [[bicarbonate]] (HCO<sub>3</sub><sup>−</sup>) as shown below. |
||
:< |
:<chem>HCO_3^- + H+ <=> H2CO3 <=> CO2 + H2O</chem> |
||
Acid–base imbalances that overcome the buffer system can be compensated in the short term by changing the rate of [[Ventilation (physiology)|ventilation]]. This alters the concentration of [[carbon dioxide]] in the blood, shifting the above reaction according to [[Le Chatelier's principle]], which in turn alters the pH. For instance, if the blood pH drops too low (''acidemia''), the body will compensate by increasing breathing, expelling CO<sub>2</sub>, and shifting the reaction above to the right such that fewer hydrogen ions are |
Acid–base imbalances that overcome the buffer system can be compensated in the short term by changing the rate of [[Ventilation (physiology)|ventilation]]. This alters the concentration of [[carbon dioxide]] in the blood, shifting the above reaction according to [[Le Chatelier's principle]], which in turn alters the pH. For instance, if the blood pH drops too low (''acidemia''), the body will compensate by increasing breathing, expelling CO<sub>2</sub>, and shifting the reaction above to the right such that fewer hydrogen ions are free–thus the pH will rise back to normal. For ''alkalemia'', the opposite occurs. |
||
The [[kidneys]] are slower to compensate, but [[renal physiology]] has several powerful mechanisms to control pH by the excretion of excess acid or base. In responses to acidosis, [[renal tubule|tubular]] cells reabsorb more bicarbonate from the tubular fluid, [[collecting duct]] cells secrete more hydrogen and generate more bicarbonate, and [[ammoniagenesis]] leads to increased formation of the NH<sub>3</sub> buffer. In responses to alkalosis, the kidney may excrete more bicarbonate by decreasing hydrogen ion secretion from the tubular epithelial cells, and lowering rates of [[glutamine]] metabolism and ammonia excretion. |
The [[kidneys]] are slower to compensate, but [[renal physiology]] has several powerful mechanisms to control pH by the excretion of excess acid or base. In responses to acidosis, [[renal tubule|tubular]] cells reabsorb more bicarbonate from the tubular fluid, [[collecting duct]] cells secrete more hydrogen and generate more bicarbonate, and [[ammoniagenesis]] leads to increased formation of the NH<sub>3</sub> buffer. In responses to alkalosis, the kidney may excrete more bicarbonate by decreasing hydrogen ion secretion from the tubular epithelial cells, and lowering rates of [[glutamine]] metabolism and ammonia excretion. |
||
==References== |
==References== |
||
{{ |
{{Reflist}} |
||
==External links== |
==External links== |
||
{{Medical resources| |
|||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
ICDO = | |
|||
OMIM = | |
|||
MedlinePlus = | |
|||
| ⚫ | |||
| ⚫ | |||
MeshID = D000137 | |
|||
}} |
|||
* [http://www.anaesthesiamcq.com/AcidBaseBook/ABindex.php On-line text at AnaesthesiaMCQ.com] |
* [http://www.anaesthesiamcq.com/AcidBaseBook/ABindex.php On-line text at AnaesthesiaMCQ.com] |
||
* {{Cite book |last=Nosek |first=Thomas M. |title=Essentials of Human Physiology |chapter=Section 7/7ch12/7ch12lin |chapter-url=http://humanphysiology.tuars.com/program/section7/7ch12/7ch12lin.htm |archive-url=https://web.archive.org/web/20160324124828/http://humanphysiology.tuars.com/program/section7/7ch12/7ch12lin.htm |archive-date=2016-03-24}} |
|||
* {{GeorgiaPhysiology|7/7ch12/7ch12lin}} |
|||
* [http://www2.kumc.edu/ki/physiology/course/nine/9_1.htm Overview at kumc.edu] |
* [https://web.archive.org/web/20061217055347/http://www2.kumc.edu/ki/physiology/course/nine/9_1.htm Overview at kumc.edu] |
||
* [http://sprojects.mmi.mcgill.ca/nephrology/presentation/presentation4.htm Overview at mcgill.ca] |
* [https://web.archive.org/web/20071024002625/http://sprojects.mmi.mcgill.ca/nephrology/presentation/presentation4.htm Overview at mcgill.ca] |
||
* [http://www.acidbase.org Stewart's original text at acidbase.org] |
* [http://www.acidbase.org Stewart's original text at acidbase.org] |
||
* [http://umed.med.utah.edu/ms2/renal/Word%20files/h)%20Acid_Base%20Physiology.htm Overview at med.utah.edu] |
* [http://umed.med.utah.edu/ms2/renal/Word%20files/h)%20Acid_Base%20Physiology.htm Overview at med.utah.edu] |
||
* [http://www.anaesthetist.com/icu/elec/ionz/Findex.htm#acid.htm Overview at anaesthetist.com] |
* [http://www.anaesthetist.com/icu/elec/ionz/Findex.htm#acid.htm Overview at anaesthetist.com] |
||
* [http://www.anst.uu.se/magnroos/Some%20notes%20on%20human%20acid.htm Overview at anst.uu.se] |
* [https://web.archive.org/web/20091114092125/http://www.anst.uu.se/magnroos/Some%20notes%20on%20human%20acid.htm Overview at anst.uu.se] |
||
* [http://www.acid-base.com/physiology.php Tutorial at acid-base.com] |
* [http://www.acid-base.com/physiology.php Tutorial at acid-base.com] |
||
* [http://www.anaesthesiamcq.com/AcidBaseBook/ABindex.php Online acid–base physiology text] |
* [http://www.anaesthesiamcq.com/AcidBaseBook/ABindex.php Online acid–base physiology text] |
||
* [http://www.lakesidepress.com/pulmonary/ABG/MixedAB.htm Diagnoses at lakesidepress.com] |
* [http://www.lakesidepress.com/pulmonary/ABG/MixedAB.htm Diagnoses at lakesidepress.com] |
||
* [http://www.nda.ox.ac.uk/wfsa/html/u16/u1602_01.htm Interpretation at nda.ox.ac.uk] |
* [https://web.archive.org/web/20040618202049/http://www.nda.ox.ac.uk/wfsa/html/u16/u1602_01.htm Interpretation at nda.ox.ac.uk] |
||
* [http://www.anaesthesiamcq.com/AcidBaseBook/ABindex.php Acid Base Tutorial] |
* [http://www.anaesthesiamcq.com/AcidBaseBook/ABindex.php Acid Base Tutorial] |
||
{{Cardiopulmonary therapy}} |
|||
{{Fluid, electrolyte, acid base metabolic pathology}} |
{{Fluid, electrolyte, acid base metabolic pathology}} |
||
{{Renal physiology}} |
{{Renal physiology}} |
||
Latest revision as of 14:36, 20 November 2024
This article needs additional citations for verification. (December 2010) |
| Acid–base imbalance | |
|---|---|
 | |
| A Davenport diagram illustrates acid–base imbalance graphically. | |
| Specialty | Internal medicine |
Acid–base imbalance is an abnormality of the human body's normal balance of acids and bases that causes the plasma pH to deviate out of the normal range (7.35 to 7.45). In the fetus, the normal range differs based on which umbilical vessel is sampled (umbilical vein pH is normally 7.25 to 7.45; umbilical artery pH is normally 7.18 to 7.38).[1] It can exist in varying levels of severity, some life-threatening.
Classification
[edit]| PaO2 | Arterial oxygen tension, or partial pressure |
|---|---|
| PAO2 | Alveolar oxygen tension, or partial pressure |
| PaCO2 | Arterial carbon dioxide tension, or partial pressure |
| PACO2 | Alveolar carbon dioxide tension, or partial pressure |
| PvO2 | Oxygen tension of mixed venous blood |
| P(A-a)O2 | Alveolar-arterial oxygen tension difference. The term formerly used (A-a DO2) is discouraged. |
| P(a/A)O2 | Alveolar-arterial tension ratio; PaO2:PAO2 The term oxygen exchange index describes this ratio. |
| C(a-v)O2 | Arteriovenous oxygen content difference |
| SaO2 | Oxygen saturation of the hemoglobin of arterial blood |
| SpO2 | Oxygen saturation as measured by pulse oximetry |
| CaO2 | Oxygen content of arterial blood |
| pH | Symbol relating the hydrogen ion concentration or activity of a solution to that of a standard solution; approximately equal to the negative logarithm of the hydrogen ion concentration. pH is an indicator of the relative acidity or alkalinity of a solution |
An excess of acid is called acidosis or acidemia, while an excess in bases is called alkalosis or alkalemia. The process that causes the imbalance is classified based on the cause of the disturbance (respiratory or metabolic) and the direction of change in pH (acidosis or alkalosis). This yields the following four basic processes:
| process | pH | CO2 | compensation |
|---|---|---|---|
| metabolic acidosis | respiratory | ||
| respiratory acidosis | renal | ||
| metabolic alkalosis | respiratory | ||
| respiratory alkalosis | renal |
Mixed disorders
[edit]The presence of only one of the above derangements is called a simple acid–base disorder. In a mixed disorder, more than one is occurring at the same time.[2] Mixed disorders may feature an acidosis and alkosis at the same time that partially counteract each other, or there can be two different conditions affecting the pH in the same direction. The phrase "mixed acidosis", for example, refers to metabolic acidosis in conjunction with respiratory acidosis. Any combination is possible, as metabolic acidosis and alkalosis can co exist together.
Calculation of imbalance
[edit]The traditional approach to the study of acid–base physiology has been the empirical approach. The main variants are the base excess approach and the bicarbonate approach. The quantitative approach introduced by Peter A Stewart in 1978[3] is newer.
Causes
[edit]There are numerous reasons that each of the four processes can occur (detailed in each article). Generally speaking, sources of acid gain include:
- Retention of carbon dioxide
- Production of nonvolatile acids from the metabolism of proteins and other organic molecules
- Loss of bicarbonate in feces or urine
- Intake of acids or acid precursors
Sources of acid loss include:
- Use of hydrogen ions in the metabolism of various organic anions
- Loss of acid in the vomitus or urine
- Gastric aspiration in hospital
- Severe diarrhea
- Carbon dioxide loss through hyperventilation
Compensation
[edit]The body's acid–base balance is tightly regulated. Several buffering agents exist which reversibly bind hydrogen ions and impede any change in pH. Extracellular buffers include bicarbonate and ammonia, while proteins and phosphate act as intracellular buffers. The bicarbonate buffering system is especially key, as carbon dioxide (CO2) can be shifted through carbonic acid (H2CO3) to hydrogen ions and bicarbonate (HCO3−) as shown below.
Acid–base imbalances that overcome the buffer system can be compensated in the short term by changing the rate of ventilation. This alters the concentration of carbon dioxide in the blood, shifting the above reaction according to Le Chatelier's principle, which in turn alters the pH. For instance, if the blood pH drops too low (acidemia), the body will compensate by increasing breathing, expelling CO2, and shifting the reaction above to the right such that fewer hydrogen ions are free–thus the pH will rise back to normal. For alkalemia, the opposite occurs.
The kidneys are slower to compensate, but renal physiology has several powerful mechanisms to control pH by the excretion of excess acid or base. In responses to acidosis, tubular cells reabsorb more bicarbonate from the tubular fluid, collecting duct cells secrete more hydrogen and generate more bicarbonate, and ammoniagenesis leads to increased formation of the NH3 buffer. In responses to alkalosis, the kidney may excrete more bicarbonate by decreasing hydrogen ion secretion from the tubular epithelial cells, and lowering rates of glutamine metabolism and ammonia excretion.
References
[edit]- ^ Yeomans, ER; Hauth, JC; Gilstrap, LC III; Strickland DM (1985). "Umbilical cord pH, PCO2, and bicarbonate following uncomplicated term vaginal deliveries (146 infants)". Am J Obstet Gynecol. 151 (6): 798–800. doi:10.1016/0002-9378(85)90523-x. PMID 3919587.
- ^ "Mixed Acid Base Disorders: Acid Base Tutorial, University of Connecticut Health Center". Archived from the original on 2009-04-26. Retrieved 2009-05-09.
- ^ Stewart P (1978). "Independent and dependent variables of acid-base control". Respir Physiol. 33 (1): 9–26. doi:10.1016/0034-5687(78)90079-8. PMID 27857.
External links
[edit]- On-line text at AnaesthesiaMCQ.com
- Nosek, Thomas M. "Section 7/7ch12/7ch12lin". Essentials of Human Physiology. Archived from the original on 2016-03-24.
- Overview at kumc.edu
- Overview at mcgill.ca
- Stewart's original text at acidbase.org
- Overview at med.utah.edu
- Overview at anaesthetist.com
- Overview at anst.uu.se
- Tutorial at acid-base.com
- Online acid–base physiology text
- Diagnoses at lakesidepress.com
- Interpretation at nda.ox.ac.uk
- Acid Base Tutorial