Vemurafenib: Difference between revisions
fix header; add link |
KMaster888 (talk | contribs) MOS:BLUESEA |
||
| (47 intermediate revisions by 25 users not shown) | |||
| Line 1: | Line 1: | ||
{{Short description|Targeted cancer drug}} |
{{Short description|Targeted cancer drug}} |
||
{{Infobox drug |
|||
{{Drugbox |
|||
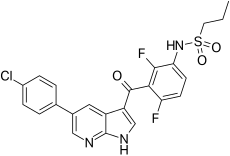
| IUPAC_name = ''N''-(3-{[5-(4-Chlorophenyl)-1''H''-pyrrolo[2,3-b]pyridin-3-yl]carbonyl}-2,4-difluorophenyl)propane-1-sulfonamide |
| IUPAC_name = ''N''-(3-{[5-(4-Chlorophenyl)-1''H''-pyrrolo[2,3-b]pyridin-3-yl]carbonyl}-2,4-difluorophenyl)propane-1-sulfonamide |
||
| verifiedrevid = 432742697 |
| verifiedrevid = 432742697 |
||
| Line 15: | Line 15: | ||
| licence_US = Vemurafenib |
| licence_US = Vemurafenib |
||
| pregnancy_AU = D |
| pregnancy_AU = D |
||
| pregnancy_AU_comment = <ref name="Zelboraf PI" /> |
|||
| pregnancy_US = D |
|||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| legal_AU = S4 |
| legal_AU = S4 |
||
| legal_AU_comment = <ref name="Zelboraf PI">{{cite web | title = Australian Product Information: Zelboraf® (vemurafenib) | url = https://www.guildlink.com.au/gc/ws/ro/pi.cfm?product=ropzelbo10615 | work = Roche Products Pty Limited | date = 25 March 2020 }}</ref> |
|||
| legal_CA = Rx-only |
| legal_CA = Rx-only |
||
| legal_UK = POM |
| legal_UK = POM |
||
| legal_US = Rx-only |
| legal_US = Rx-only |
||
| ⚫ | |||
<!--Identifiers--> |
<!--Identifiers--> |
||
| ⚫ | |||
| ⚫ | |||
| IUPHAR_ligand = 5893 |
| IUPHAR_ligand = 5893 |
||
| DrugBank = DB08881 |
| DrugBank = DB08881 |
||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} |
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} |
||
| ChemSpiderID = 24747352 |
| ChemSpiderID = 24747352 |
||
| ⚫ | |||
| KEGG_Ref = {{keggcite|correct|kegg}} |
| KEGG_Ref = {{keggcite|correct|kegg}} |
||
| KEGG = D09996 |
| KEGG = D09996 |
||
| ChEMBL = 1229517 |
| ChEMBL = 1229517 |
||
| ⚫ | |||
| ⚫ | |||
| PDB_ligand = 032 |
| PDB_ligand = 032 |
||
| ⚫ | |||
<!--Chemical data--> |
<!--Chemical data--> |
||
| C=23 | H=18 | Cl=1 | F=2 | N=3 | O=3 | S=1 |
| C=23 | H=18 | Cl=1 | F=2 | N=3 | O=3 | S=1 |
||
| molecular_weight = 489.92 g/mol |
|||
| smiles = CCCS(=O)(=O)Nc1ccc(F)c(c1F)C(=O)c2c[nH]c3c2cc(cn3)c4ccc(Cl)cc4 |
| smiles = CCCS(=O)(=O)Nc1ccc(F)c(c1F)C(=O)c2c[nH]c3c2cc(cn3)c4ccc(Cl)cc4 |
||
| StdInChI_Ref = {{stdinchicite|correct|chemspider}} |
| StdInChI_Ref = {{stdinchicite|correct|chemspider}} |
||
| Line 55: | Line 56: | ||
| Use = [[melanoma]] |
| Use = [[melanoma]] |
||
| Biological_target = [[BRAF (gene)|BRAF]] |
| Biological_target = [[BRAF (gene)|BRAF]] |
||
| ATC_prefix = L01 |
|||
| ATC_suffix = XE15 |
|||
| MOA_text = [[protein kinase inhibitor]] |
| MOA_text = [[protein kinase inhibitor]] |
||
| PDB_ligand = 032 |
| PDB_ligand = 032 |
||
| Line 62: | Line 61: | ||
}} |
}} |
||
'''Vemurafenib''' ([[International Nonproprietary Name|INN]], |
'''Vemurafenib''' ([[International Nonproprietary Name|INN]]), sold under the brand name '''Zelboraf''', is a [[medication]] used for the treatment of late-stage [[melanoma]].<ref name="pmid20823850">{{PDB|3OG7}}; {{cite journal | vauthors = Bollag G, Hirth P, Tsai J, Zhang J, Ibrahim PN, Cho H, Spevak W, Zhang C, Zhang Y, Habets G, Burton EA, Wong B, Tsang G, West BL, Powell B, Shellooe R, Marimuthu A, Nguyen H, Zhang KY, Artis DR, Schlessinger J, Su F, Higgins B, Iyer R, D'Andrea K, Koehler A, Stumm M, Lin PS, Lee RJ, Grippo J, Puzanov I, Kim KB, Ribas A, McArthur GA, Sosman JA, Chapman PB, Flaherty KT, Xu X, Nathanson KL, Nolop K | display-authors = 6 | title = Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma | journal = Nature | volume = 467 | issue = 7315 | pages = 596–599 | date = September 2010 | pmid = 20823850 | pmc = 2948082 | doi = 10.1038/nature09454 | bibcode = 2010Natur.467..596B }}</ref> It is an inhibitor of the [[BRAF (gene)|B-Raf enzyme]] and was developed by [[Plexxikon]].<ref name="pmid20823850" /> |
||
==Approvals== |
|||
| ⚫ | Vemurafenib |
||
| ⚫ | Vemurafenib |
||
| ⚫ | |||
| ⚫ | |||
== Mechanism of action == |
== Mechanism of action == |
||
Vemurafenib causes [[apoptosis|programmed cell death]] in [[melanoma]] cell lines.<ref name="pmid18458053">{{cite journal |vauthors=Sala E, Mologni L, Truffa S, Gaetano C, Bollag GE, Gambacorti-Passerini C | title = BRAF silencing by short hairpin RNA or chemical blockade by PLX4032 leads to different responses in melanoma and thyroid carcinoma cells | journal = |
Vemurafenib causes [[apoptosis|programmed cell death]] in [[melanoma]] cell lines.<ref name="pmid18458053">{{cite journal | vauthors = Sala E, Mologni L, Truffa S, Gaetano C, Bollag GE, Gambacorti-Passerini C | title = BRAF silencing by short hairpin RNA or chemical blockade by PLX4032 leads to different responses in melanoma and thyroid carcinoma cells | journal = Molecular Cancer Research | volume = 6 | issue = 5 | pages = 751–759 | date = May 2008 | pmid = 18458053 | doi = 10.1158/1541-7786.MCR-07-2001 | s2cid = 16031942 | doi-access = }}</ref> Vemurafenib interrupts the [[BRAF (gene)|B-Raf/MEK step]] on the [[MAPK/ERK pathway|B-Raf/MEK/ERK pathway]] − if the B-Raf has the common V600E mutation. |
||
Vemurafenib only works in melanoma patients whose cancer has a V600E BRAF mutation (that is, at [[amino acid]] position number 600 on the B-Raf protein, the normal [[valine]] is replaced by [[glutamic acid]]).<ref>{{cite journal |vauthors=Maverakis E, Cornelius LA, Bowen GM, Phan T, Patel FB, Fitzmaurice S, He Y, Burrall B, Duong C, Kloxin AM, Sultani H, Wilken R, Martinez SR, Patel F | title = Metastatic melanoma - a review of current and future treatment options | journal = Acta |
Vemurafenib only works in melanoma patients whose cancer has a V600E BRAF mutation (that is, at [[amino acid]] position number 600 on the B-Raf protein, the normal [[valine]] is replaced by [[glutamic acid]]).<ref>{{cite journal | vauthors = Maverakis E, Cornelius LA, Bowen GM, Phan T, Patel FB, Fitzmaurice S, He Y, Burrall B, Duong C, Kloxin AM, Sultani H, Wilken R, Martinez SR, Patel F | display-authors = 6 | title = Metastatic melanoma - a review of current and future treatment options | journal = Acta Dermato-Venereologica | volume = 95 | issue = 5 | pages = 516–524 | date = May 2015 | pmid = 25520039 | doi = 10.2340/00015555-2035 | doi-access = free }}</ref> About 60% of melanomas have this mutation. It also has efficacy against the rarer V600K BRAF (the normal valine is replaced by [[lysine]]) mutation. Melanoma cells without these mutations are not inhibited by vemurafenib; the drug paradoxically stimulates normal BRAF and may promote tumor growth in such cases.<ref name="pmid20130576">{{cite journal | vauthors = Hatzivassiliou G, Song K, Yen I, Brandhuber BJ, Anderson DJ, Alvarado R, Ludlam MJ, Stokoe D, Gloor SL, Vigers G, Morales T, Aliagas I, Liu B, Sideris S, Hoeflich KP, Jaiswal BS, Seshagiri S, Koeppen H, Belvin M, Friedman LS, Malek S | display-authors = 6 | title = RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth | journal = Nature | volume = 464 | issue = 7287 | pages = 431–435 | date = March 2010 | pmid = 20130576 | doi = 10.1038/nature08833 | doi-access = free | bibcode = 2010Natur.464..431H }}</ref><ref name="pmid20149136">{{cite journal | vauthors = Halaban R, Zhang W, Bacchiocchi A, Cheng E, Parisi F, Ariyan S, Krauthammer M, McCusker JP, Kluger Y, Sznol M | display-authors = 6 | title = PLX4032, a selective BRAF(V600E) kinase inhibitor, activates the ERK pathway and enhances cell migration and proliferation of BRAF melanoma cells | journal = Pigment Cell & Melanoma Research | volume = 23 | issue = 2 | pages = 190–200 | date = April 2010 | pmid = 20149136 | pmc = 2848976 | doi = 10.1111/j.1755-148X.2010.00685.x }}</ref> |
||
===Resistance=== |
===Resistance=== |
||
Three mechanisms of resistance to vemurafenib (covering 40% of cases) have been discovered: |
Three mechanisms of resistance to vemurafenib (covering 40% of cases) have been discovered: |
||
* Cancer cells begin to overexpress cell surface protein [[PDGFRB]], creating an alternative survival pathway. |
* Cancer cells begin to overexpress cell surface protein [[PDGFRB]], creating an alternative survival pathway. |
||
* A second [[oncogene]] called [[Neuroblastoma RAS viral oncogene homolog|NRAS]] mutates, reactivating the normal BRAF survival pathway.<ref name="pmid21107323">{{cite journal |vauthors=Nazarian R, Shi H, Wang Q, Kong X, Koya RC, Lee H, Chen Z, Lee MK, Attar N, Sazegar H, Chodon T, Nelson SF, McArthur G, Sosman JA, Ribas A, Lo RS | title = Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation | journal = Nature | volume = 468| issue = 7326| pages = 973–977|date= |
* A second [[oncogene]] called [[Neuroblastoma RAS viral oncogene homolog|NRAS]] mutates, reactivating the normal BRAF survival pathway.<ref name="pmid21107323">{{cite journal | vauthors = Nazarian R, Shi H, Wang Q, Kong X, Koya RC, Lee H, Chen Z, Lee MK, Attar N, Sazegar H, Chodon T, Nelson SF, McArthur G, Sosman JA, Ribas A, Lo RS | display-authors = 6 | title = Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation | journal = Nature | volume = 468 | issue = 7326 | pages = 973–977 | date = December 2010 | pmid = 21107323 | pmc = 3143360 | doi = 10.1038/nature09626 | bibcode = 2010Natur.468..973N }} |
||
* {{cite news |date=November 25, 2010 |title=Researchers Uncover Drug-Resistance Mechanisms in BRAF Melanoma |work=Genetic Engineering & Biotechnology News |url=http://www.genengnews.com/gen-news-highlights/researchers-uncover-drug-resistance-mechanisms-in-braf-melanoma/81244289/}}</ref> |
|||
* [[Stromal cell]] secretion of [[hepatocyte growth factor]] (HGF).<ref name="pmid22763439">{{cite journal |vauthors=Straussman R, Morikawa T, Shee K, Barzily-Rokni M, Qian ZR, Du J, Davis A, Mongare MM, Gould J, Frederick DT, Cooper ZA, Chapman PB, Solit DB, Ribas A, Lo RS, Flaherty KT, Ogino S, Wargo JA, Golub TR | title = Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion | journal = Nature | volume = 487 | issue = 7408 | pages = |
* [[Stromal cell]] secretion of [[hepatocyte growth factor]] (HGF).<ref name="pmid22763439">{{cite journal | vauthors = Straussman R, Morikawa T, Shee K, Barzily-Rokni M, Qian ZR, Du J, Davis A, Mongare MM, Gould J, Frederick DT, Cooper ZA, Chapman PB, Solit DB, Ribas A, Lo RS, Flaherty KT, Ogino S, Wargo JA, Golub TR | display-authors = 6 | title = Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion | journal = Nature | volume = 487 | issue = 7408 | pages = 500–504 | date = July 2012 | pmid = 22763439 | pmc = 3711467 | doi = 10.1038/nature11183 | bibcode = 2012Natur.487..500S }}</ref><ref name="pmid22763448">{{cite journal | vauthors = Wilson TR, Fridlyand J, Yan Y, Penuel E, Burton L, Chan E, Peng J, Lin E, Wang Y, Sosman J, Ribas A, Li J, Moffat J, Sutherlin DP, Koeppen H, Merchant M, Neve R, Settleman J | display-authors = 6 | title = Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors | journal = Nature | volume = 487 | issue = 7408 | pages = 505–509 | date = July 2012 | pmid = 22763448 | pmc = 3724525 | doi = 10.1038/nature11249 | bibcode = 2012Natur.487..505W }}</ref> |
||
| ⚫ | |||
== Clinical trials == |
|||
| ⚫ | At the maximum tolerated dose (MTD) of 960 mg twice a day 31% of patients get skin lesions that may need surgical removal.<ref name="pmid20823850"/> The BRIM-2 trial investigated 132 patients; the most common adverse events were [[arthralgia]] in 58% of patients, skin rash in 52%, and photosensitivity in 52%. In order to better manage side effects some form of dose modification was necessary in 45% of patients. The median daily dose was 1750 mg, 91% of the MTD.<ref>{{cite journal | title=BRIM-2 Upholds Benefits Emerging with Vemurafenib in Melanoma |journal=Oncology & Biotech News |volume=5 |issue=7 |date=July 2011 |url=http://www.onclive.com/publications/obtn/2011/july-2011/BRIM-2-Upholds-Benefits-Emerging-with-Vemurafenib-in-Melanoma }}</ref> |
||
| ⚫ | In a [[Phases of clinical research|phase I clinical study]], vemurafenib (then known as PLX4032) was able to reduce numbers of cancer cells in over half of a group of 16 patients with advanced melanoma. The treated group had a median increased survival time of 6 months over the control group.<ref>{{cite news | url = http://news.bbc.co.uk/2/hi/health/8076743.stm | title=Drug hope for advanced melanoma | publisher=BBC News | |
||
== History == |
|||
| ⚫ | A second phase I study, in patients with a V600E mutation in B-Raf, ~80% showed partial to complete regression. The regression lasted from 2 to 18 months.<ref name="pmid20818844">{{cite journal |vauthors=Flaherty KT, Puzanov I, Kim KB, Ribas A, McArthur GA, Sosman JA, O'Dwyer PJ, Lee RJ, Grippo JF, Nolop K, Chapman PB | title = Inhibition of mutated, activated BRAF in metastatic melanoma | journal = |
||
| ⚫ | In a [[Phases of clinical research|phase I clinical study]], vemurafenib (then known as PLX4032) was able to reduce numbers of cancer cells in over half of a group of 16 patients with advanced melanoma. The treated group had a median increased survival time of 6 months over the control group.<ref>{{cite news | url = http://news.bbc.co.uk/2/hi/health/8076743.stm | title=Drug hope for advanced melanoma | publisher=BBC News | access-date=2009-06-07 | date=2009-06-02}}</ref><ref name="urlTarget Cancer - A Roller Coaster Chase for a Cure - Series ">{{cite news | url = https://www.nytimes.com/2010/02/22/health/research/22trial.html | title = A Roller Coaster Chase for a Cure | vauthors = Harmon A | date = 2010-02-21 | work = [[The New York Times]] }}</ref><ref name="pmid20019269">{{cite journal | vauthors = Garber K | title = Cancer research. Melanoma drug vindicates targeted approach | journal = Science | volume = 326 | issue = 5960 | pages = 1619 | date = December 2009 | pmid = 20019269 | doi = 10.1126/science.326.5960.1619 | bibcode = 2009Sci...326.1619G }}</ref><ref name="urlPhase I study of PLX4032: Proof of concept for V600E BRAF mutation as a therapeutic target in human cancer. - ASCO">{{cite web | url = http://www.asco.org/ASCOv2/Meetings/Abstracts?&vmview=abst_detail_view&confID=65&abstractID=34909 | title = Phase I study of PLX4032: Proof of concept for V600E BRAF mutation as a therapeutic target in human cancer | vauthors = Flaherty K | work = 2009 ASCO Annual Meeting Abstract, J Clin Oncol 27:15s, 2009 (suppl; abstr 9000) | access-date = 2010-09-10 | archive-date = 2013-01-27 | archive-url = https://web.archive.org/web/20130127201543/http://www.asco.org/ASCOv2/Meetings/Abstracts?&vmview=abst_detail_view&confID=65&abstractID=34909 | url-status = dead }}</ref> |
||
| ⚫ | A second phase I study, in patients with a V600E mutation in B-Raf, ~80% showed partial to complete regression. The regression lasted from 2 to 18 months.<ref name="pmid20818844">{{cite journal | vauthors = Flaherty KT, Puzanov I, Kim KB, Ribas A, McArthur GA, Sosman JA, O'Dwyer PJ, Lee RJ, Grippo JF, Nolop K, Chapman PB | display-authors = 6 | title = Inhibition of mutated, activated BRAF in metastatic melanoma | journal = The New England Journal of Medicine | volume = 363 | issue = 9 | pages = 809–819 | date = August 2010 | pmid = 20818844 | pmc = 3724529 | doi = 10.1056/NEJMoa1002011 }} |
||
| ⚫ | In early 2010 a [[Clinical trial#Phase I|Phase I]] trial<ref name=" |
||
* {{cite web | vauthors = Lowe D |date=September 9, 2010 |title=PLX4032: The Good News and the Bad News |website=Corante |department=In the Pipeline |url=http://pipeline.corante.com/archives/2010/09/09/plx4032_the_good_news_and_the_bad_news.php |archive-url=https://web.archive.org/web/20100911204820/http://pipeline.corante.com/archives/2010/09/09/plx4032_the_good_news_and_the_bad_news.php |archive-date=2010-09-11}}</ref> |
|||
| ⚫ | In early 2010 a [[Clinical trial#Phase I|Phase I]] trial<ref name="NCT00405587">{{ClinicalTrialsGov|NCT00405587|Safety Study of PLX4032 in Patients With Solid Tumors}}</ref> for solid tumors (including [[colorectal cancer]]), and a [[Clinical trial#Phase II|phase II]] study (for metastatic melanoma) were ongoing.<ref name="NCT00949702">{{ClinicalTrialsGov|NCT00949702|A Study of RO5185426 in Previously Treated Patients With Metastatic Melanoma}}</ref> |
||
| ⚫ | A phase III trial (vs [[dacarbazine]]) in patients with previously untreated metastatic melanoma showed an improved rates of overall and progression-free survival.<ref name="PLX4032_phase_3_trial">{{cite press release | url = http://www.plexxikon.com/view.cfm/74/Press-Releases | title = Plexxikon Announces First Patient Dosed in Phase 3 Trial of PLX4032 (RG7204) for Metastatic Melanoma | date = 2010-01-08 | publisher = Plexxikon }}</ref> |
||
| ⚫ | A phase III trial (vs [[dacarbazine]]) in patients with previously untreated metastatic melanoma showed an improved rates of overall and progression-free survival.<ref name="PLX4032_phase_3_trial">{{cite press release | url = http://www.plexxikon.com/view.cfm/74/Press-Releases | title = Plexxikon Announces First Patient Dosed in Phase 3 Trial of PLX4032 (RG7204) for Metastatic Melanoma | date = 2010-01-08 | publisher = Plexxikon | access-date = 2011-02-03 | archive-date = 2020-12-01 | archive-url = https://web.archive.org/web/20201201091352/https://www.plexxikon.com/view.cfm/74/Press-Releases | url-status = dead }}</ref> |
||
| ⚫ | In June 2011, positive results were reported from the phase III BRIM3 BRAF-mutation melanoma study.<ref name=BRIM3-1>{{cite news |url=http://www.genengnews.com/gen-news-highlights/plexxikon-and-roche-report-positive-data-from-phase-iii-braf-mutation-melanoma-study/81245246/ |title=Plexxikon and Roche Report Positive Data from Phase III BRAF Mutation Melanoma Study |date=6 June 2011 }}</ref> The BRIM3 trial reported good updated results in 2012.<ref name=ASCO2012>{{cite web |url=http://www.chemotherapyadvisor.com/vemurafenib-improves-overall-survival-in-patients-with-metastatic-melanoma/article/244197/ |
||
| ⚫ | In June 2011, positive results were reported from the phase III BRIM3 BRAF-mutation melanoma study.<ref name=BRIM3-1>{{cite news |url=http://www.genengnews.com/gen-news-highlights/plexxikon-and-roche-report-positive-data-from-phase-iii-braf-mutation-melanoma-study/81245246/ |title=Plexxikon and Roche Report Positive Data from Phase III BRAF Mutation Melanoma Study | work = Genetic Engineering & Biotechnology News | publisher = Mary Ann Liebert Publishers |date=6 June 2011 }}</ref> The BRIM3 trial reported good updated results in 2012.<ref name=ASCO2012>{{cite web |url=http://www.chemotherapyadvisor.com/vemurafenib-improves-overall-survival-in-patients-with-metastatic-melanoma/article/244197/ |title=Vemurafenib Improves Overall Survival in Patients with Metastatic Melanoma |access-date=2012-12-17 |archive-date=2022-01-11 |archive-url=https://web.archive.org/web/20220111060630/https://www.optimizely.com/idio/ |url-status=dead }}</ref> |
||
| ⚫ | Further trials are planned including a trial of vemurafenib co-administered with GDC-0973 ([[cobimetinib]]), a [[MEK inhibitor|MEK-inhibitor]].<ref name=BRIM3-1/> After good results in 2014 the combination was submitted to the |
||
| ⚫ | Further trials are planned including a trial of vemurafenib co-administered with GDC-0973 ([[cobimetinib]]), a [[MEK inhibitor|MEK-inhibitor]].<ref name=BRIM3-1/> After good results in 2014, the combination was submitted to the European Medical Agency and the US [[Food and Drug Administration]] for marketing approval.<ref>{{Cite web |url=http://www.exelixis.com/pipeline/GDC_0973_xl518 |title=Cobimetinib at exelixis.com |access-date=2015-02-04 |archive-url=https://web.archive.org/web/20150204043254/http://www.exelixis.com/pipeline/GDC_0973_xl518 |archive-date=2015-02-04 |url-status=dead }}</ref> |
||
| ⚫ | In January 2015 trial results compared vemurafenib with the combination of [[dabrafenib]] and [[trametinib]] for metastatic melanoma.<ref>{{cite web |url= |
||
| ⚫ | In January 2015, trial results compared vemurafenib with the combination of [[dabrafenib]] and [[trametinib]] for metastatic melanoma.<ref>{{cite web |url=https://www.cancernetwork.com/view/mekbraf-inhibitor-combo-reduces-death-one-third-melanoma |title=MEK/BRAF Inhibitor Combo Reduces Death by One-Third in Melanoma |year=2015 }}</ref> |
||
| ⚫ | |||
| ⚫ | At the maximum tolerated dose (MTD) of 960 mg twice a day 31% of patients get skin lesions that may need surgical removal.<ref name="pmid20823850"/> The BRIM-2 trial investigated 132 patients; the most common adverse events were [[arthralgia]] in 58% of patients, skin rash in 52%, and photosensitivity in 52%. In order to better manage side effects some form of dose modification was necessary in 45% of patients. The median daily dose was 1750 mg, 91% of the MTD.<ref>{{cite journal | title=BRIM-2 Upholds Benefits Emerging with Vemurafenib in Melanoma |journal=Oncology & Biotech News |volume=5 |issue=7 |date=July 2011 |url=http://www.onclive.com/publications/obtn/2011/july-2011/BRIM-2-Upholds-Benefits-Emerging-with-Vemurafenib-in-Melanoma }}</ref> |
||
== Society and culture == |
|||
=== Legal status === |
|||
| ⚫ | Vemurafenib was approved in the United States for the treatment of late-stage melanoma in August 2011,<ref>{{cite press release |url=http://www.gene.com/gene/news/press-releases/display.do?method=detail&id=13567 |title=FDA Approves Zelboraf (Vemurafenib) and Companion Diagnostic for BRAF Mutation-Positive Metastatic Melanoma, a Deadly Form of Skin Cancer |publisher=Genentech |access-date=2011-08-17}}</ref> making it the first drug designed using [[fragment-based lead discovery]] to gain regulatory approval.<ref name="pmid23060265">{{cite journal | vauthors = Bollag G, Tsai J, Zhang J, Zhang C, Ibrahim P, Nolop K, Hirth P | title = Vemurafenib: the first drug approved for BRAF-mutant cancer | journal = Nature Reviews. Drug Discovery | volume = 11 | issue = 11 | pages = 873–886 | date = November 2012 | pmid = 23060265 | doi = 10.1038/nrd3847 | s2cid = 9337155 }}</ref> |
||
| ⚫ | Vemurafenib was approved for use in Canada in February 2012.<ref>{{Cite web |url=http://www.hc-sc.gc.ca/dhp-mps/prodpharma/sbd-smd/drug-med/nd_ad_2012_zelboraf_148693-eng.php |title=Notice of Decision for ZELBORAF | date = 11 March 2012 |access-date = 21 April 2012 |archive-url=https://web.archive.org/web/20120502011736/http://www.hc-sc.gc.ca/dhp-mps/prodpharma/sbd-smd/drug-med/nd_ad_2012_zelboraf_148693-eng.php |archive-date=2 May 2012 |url-status=dead | work = Health Canada }}</ref> |
||
| ⚫ | In February 2012, the [[European Commission]] approved vemurafenib as a monotherapy for the treatment of adults with BRAF [[V600E]] [[mutation]] positive unresectable or [[metastatic melanoma]], the most aggressive form of skin cancer.<ref>{{cite web | title = First Personalized Cancer Medicine Allows Patients with Deadly Form of Metastatic Melanoma to Live Significantly Longer | url = http://oncozine.com/profiles/blogs/first-personalized-cancer-medicine-allows-patients-deadly-form-of | vauthors = Hofland P | work = Onco'Zine | publisher = The International Cancer Network | date = February 20, 2012 | access-date = February 18, 2013 | archive-url = https://web.archive.org/web/20120411134824/http://oncozine.com/profiles/blogs/first-personalized-cancer-medicine-allows-patients-deadly-form-of | archive-date = April 11, 2012 | url-status = dead | df = mdy-all }}</ref> |
||
| ⚫ | In November 2017, the US [[Food and Drug Administration]] (FDA) approved vemurafenib for the treatment of people with [[Erdheim–Chester disease]] (ECD), a rare type of histiocytic neoplasm.<ref>{{Cite press release|url=https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm583931.htm|title=FDA approves first treatment for certain patients with Erdheim–Chester disease, a rare blood cancer|website=U.S. [[Food and Drug Administration]] (FDA)|access-date=2018-05-20}}</ref><ref>{{cite journal | vauthors = Diamond EL, Subbiah V, Lockhart AC, Blay JY, Puzanov I, Chau I, Raje NS, Wolf J, Erinjeri JP, Torrisi J, Lacouture M, Elez E, Martínez-Valle F, Durham B, Arcila ME, Ulaner G, Abdel-Wahab O, Pitcher B, Makrutzki M, Riehl T, Baselga J, Hyman DM | display-authors = 6 | title = Vemurafenib for BRAF V600-Mutant Erdheim-Chester Disease and Langerhans Cell Histiocytosis: Analysis of Data From the Histology-Independent, Phase 2, Open-label VE-BASKET Study | journal = JAMA Oncology | volume = 4 | issue = 3 | pages = 384–388 | date = March 2018 | pmid = 29188284 | pmc = 5844839 | doi = 10.1001/jamaoncol.2017.5029 }}</ref> |
||
== Research == |
|||
A trial combining vemurafenib and ipilimumab was stopped in April 2013 because of signs of [[Hepatotoxicity|liver toxicity]].<ref>{{Cite news|url=https://www.economist.com/news/science-and-technology/21592599-researchers-and-drug-companies-are-ganging-up-new-push-against|title=Getting close and personal|date=January 4, 2014|newspaper=The Economist|issn=0013-0613|access-date=2016-04-15}}</ref> |
A trial combining vemurafenib and ipilimumab was stopped in April 2013 because of signs of [[Hepatotoxicity|liver toxicity]].<ref>{{Cite news|url=https://www.economist.com/news/science-and-technology/21592599-researchers-and-drug-companies-are-ganging-up-new-push-against|title=Getting close and personal|date=January 4, 2014|newspaper=The Economist|issn=0013-0613|access-date=2016-04-15}}</ref> |
||
== Treating Hairy Cell Leukemia == |
|||
In 2012, a grant from the [[Hairy cell leukemia]] Foundation supported the discovery of the BRAF mutation in classic HCL. This discovery charted a new path forward for many patients. It improved diagnosis and opened the door for additional therapies to be used in managing HCL.<ref>{{cite web|url=https://www.hairycellleukemia.org/blog/campaignlaunch |title=Hairy Cell Leukemia: Celebrating Progress? |website=HCLF Blog |date=July 29, 2022 |access-date=July 25, 2022}}</ref> In a phase II clinical trial, Memorial Sloan Kettering is testing Vemurafenib, plus Obinutuzumab, in patients with previously untreated classical hairy cell leukemia.<ref name = "NCT03410875">{{ClinicalTrialsGov|NCT03410875|Hairy Cell Leukemia with Vemurafebib}}</ref> A separate clinical study treatment with only Vemurafenib (or monotherarpy) demonstrated high response rates in relapsed/refractory (R/R) hairy cell leukemia (HCL), achieving an overall response rate of 86%, including 33% complete response (CR) and 53% partial response. However, after a median follow-up of 40 months, 21 of 31 responders (68%) experienced relapse with a median relapse-free survival (RFS) of 19 months (range, 12.5-53.9 months).<ref>{{cite journal | vauthors = Handa S, Lee JO, Derkach A, Stone RM, Saven A, Altman JK, Grever MR, Rai KR, Shukla M, Vemuri S, Montoya S, Taylor J, Abdel-Wahab O, Tallman MS, Park JH | display-authors = 6 | title = Long-term outcomes in patients with relapsed or refractory hairy cell leukemia treated with vemurafenib monotherapy | journal = Blood | volume = 140 | issue = 25 | pages = 2663–2671 | date = December 2022 | doi = 10.1182/blood.2022016183 | pmid = 35930750 | pmc = 9935554 }}</ref> |
|||
{{Clear}} |
{{Clear}} |
||
== References == |
== References == |
||
{{Reflist}} |
{{Reflist}} |
||
==Further reading== |
== Further reading == |
||
* {{cite book | title=Medical Genetics Summaries | chapter=Vemurafenib Therapy and BRAF and NRAS Genotype | chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK447416/ | veditors=Pratt VM, McLeod HL, Rubinstein WS, Scott SA, Dean LC, Kattman BL, Malheiro AJ | display-editors=3 | publisher=[[National Center for Biotechnology Information]] (NCBI) | year=2017 | pmid=28809522 | id=Bookshelf ID: NBK447416 | vauthors=Dean L | url=https://www.ncbi.nlm.nih.gov/books/NBK61999/ }} |
* {{cite book | title=Medical Genetics Summaries | chapter=Vemurafenib Therapy and BRAF and NRAS Genotype | chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK447416/ | veditors=Pratt VM, McLeod HL, Rubinstein WS, Scott SA, Dean LC, Kattman BL, Malheiro AJ | display-editors=3 | publisher=[[National Center for Biotechnology Information]] (NCBI) | year=2017 | pmid=28809522 | id=Bookshelf ID: NBK447416 | vauthors=Dean L | url=https://www.ncbi.nlm.nih.gov/books/NBK61999/ }} |
||
{{Targeted cancer therapeutic agents}} |
|||
==External links== |
|||
{{Growth factor receptor modulators}} |
|||
* {{cite web | url = https://druginfo.nlm.nih.gov/drugportal/name/vemurafenib | publisher = U.S. National Library of Medicine | work = Drug Information Portal | title = Vemurafenib }} |
|||
| ⚫ | |||
{{Extracellular chemotherapeutic agents}} |
|||
| ⚫ | |||
[[Category:Antineoplastic and immunomodulating drugs]] |
[[Category:Antineoplastic and immunomodulating drugs]] |
||
[[Category:B-Raf inhibitors]] |
[[Category:B-Raf inhibitors]] |
||
[[Category: |
[[Category:4-Chlorophenyl compounds]] |
||
| ⚫ | |||
[[Category:CYP2D6 inhibitors]] |
|||
[[Category:CYP3A4 inducers]] |
|||
[[Category:Fluoroarenes]] |
[[Category:Fluoroarenes]] |
||
[[Category:Sulfonamides]] |
[[Category:Sulfonamides]] |
||
| ⚫ | |||
[[Category:Chemotherapy]] |
[[Category:Chemotherapy]] |
||
[[Category:Hoffmann-La Roche |
[[Category:Drugs developed by Hoffmann-La Roche]] |
||
[[Category: |
[[Category:Drugs developed by Genentech]] |
||
[[Category:Daiichi Sankyo]] |
[[Category:Daiichi Sankyo]] |
||
[[Category:Diarylketones]] |
|||
Latest revision as of 16:50, 24 November 2024
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌvɛməˈræfənɪb/ VEM-ə-RAF-ə-nib |
| Trade names | Zelboraf |
| Other names | PLX4032, RG7204, PLX4720, RO5185426 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a612009 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.287.801 |
| Chemical and physical data | |
| Formula | C23H18ClF2N3O3S |
| Molar mass | 489.92 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
| vemurafenib | |
|---|---|
| Drug mechanism | |
 Crystallographic structure of B-Raf (rainbow colored, N-terminus = blue, C-terminus = red) complexed with vemurafenib (spheres, carbon = white, oxygen = red, nitrogen = blue, chlorine = green, fluorine = cyan, sulfur = yellow).[2] | |
| Therapeutic use | melanoma |
| Biological target | BRAF |
| Mechanism of action | protein kinase inhibitor |
| External links | |
| PDB ligand id | 032: PDBe, RCSB PDB |
| LIGPLOT | 3og7 |
Vemurafenib (INN), sold under the brand name Zelboraf, is a medication used for the treatment of late-stage melanoma.[2] It is an inhibitor of the B-Raf enzyme and was developed by Plexxikon.[2]
Mechanism of action
[edit]Vemurafenib causes programmed cell death in melanoma cell lines.[3] Vemurafenib interrupts the B-Raf/MEK step on the B-Raf/MEK/ERK pathway − if the B-Raf has the common V600E mutation.
Vemurafenib only works in melanoma patients whose cancer has a V600E BRAF mutation (that is, at amino acid position number 600 on the B-Raf protein, the normal valine is replaced by glutamic acid).[4] About 60% of melanomas have this mutation. It also has efficacy against the rarer V600K BRAF (the normal valine is replaced by lysine) mutation. Melanoma cells without these mutations are not inhibited by vemurafenib; the drug paradoxically stimulates normal BRAF and may promote tumor growth in such cases.[5][6]
Resistance
[edit]Three mechanisms of resistance to vemurafenib (covering 40% of cases) have been discovered:
- Cancer cells begin to overexpress cell surface protein PDGFRB, creating an alternative survival pathway.
- A second oncogene called NRAS mutates, reactivating the normal BRAF survival pathway.[7]
- Stromal cell secretion of hepatocyte growth factor (HGF).[8][9]
Side effects
[edit]At the maximum tolerated dose (MTD) of 960 mg twice a day 31% of patients get skin lesions that may need surgical removal.[2] The BRIM-2 trial investigated 132 patients; the most common adverse events were arthralgia in 58% of patients, skin rash in 52%, and photosensitivity in 52%. In order to better manage side effects some form of dose modification was necessary in 45% of patients. The median daily dose was 1750 mg, 91% of the MTD.[10]
History
[edit]In a phase I clinical study, vemurafenib (then known as PLX4032) was able to reduce numbers of cancer cells in over half of a group of 16 patients with advanced melanoma. The treated group had a median increased survival time of 6 months over the control group.[11][12][13][14]
A second phase I study, in patients with a V600E mutation in B-Raf, ~80% showed partial to complete regression. The regression lasted from 2 to 18 months.[15]
In early 2010 a Phase I trial[16] for solid tumors (including colorectal cancer), and a phase II study (for metastatic melanoma) were ongoing.[17]
A phase III trial (vs dacarbazine) in patients with previously untreated metastatic melanoma showed an improved rates of overall and progression-free survival.[18]
In June 2011, positive results were reported from the phase III BRIM3 BRAF-mutation melanoma study.[19] The BRIM3 trial reported good updated results in 2012.[20]
Further trials are planned including a trial of vemurafenib co-administered with GDC-0973 (cobimetinib), a MEK-inhibitor.[19] After good results in 2014, the combination was submitted to the European Medical Agency and the US Food and Drug Administration for marketing approval.[21]
In January 2015, trial results compared vemurafenib with the combination of dabrafenib and trametinib for metastatic melanoma.[22]
Society and culture
[edit]Legal status
[edit]Vemurafenib was approved in the United States for the treatment of late-stage melanoma in August 2011,[23] making it the first drug designed using fragment-based lead discovery to gain regulatory approval.[24]
Vemurafenib was approved for use in Canada in February 2012.[25]
In February 2012, the European Commission approved vemurafenib as a monotherapy for the treatment of adults with BRAF V600E mutation positive unresectable or metastatic melanoma, the most aggressive form of skin cancer.[26]
In November 2017, the US Food and Drug Administration (FDA) approved vemurafenib for the treatment of people with Erdheim–Chester disease (ECD), a rare type of histiocytic neoplasm.[27][28]
Research
[edit]A trial combining vemurafenib and ipilimumab was stopped in April 2013 because of signs of liver toxicity.[29]
Treating Hairy Cell Leukemia
[edit]In 2012, a grant from the Hairy cell leukemia Foundation supported the discovery of the BRAF mutation in classic HCL. This discovery charted a new path forward for many patients. It improved diagnosis and opened the door for additional therapies to be used in managing HCL.[30] In a phase II clinical trial, Memorial Sloan Kettering is testing Vemurafenib, plus Obinutuzumab, in patients with previously untreated classical hairy cell leukemia.[31] A separate clinical study treatment with only Vemurafenib (or monotherarpy) demonstrated high response rates in relapsed/refractory (R/R) hairy cell leukemia (HCL), achieving an overall response rate of 86%, including 33% complete response (CR) and 53% partial response. However, after a median follow-up of 40 months, 21 of 31 responders (68%) experienced relapse with a median relapse-free survival (RFS) of 19 months (range, 12.5-53.9 months).[32]
References
[edit]- ^ a b "Australian Product Information: Zelboraf® (vemurafenib)". Roche Products Pty Limited. 25 March 2020.
- ^ a b c d PDB: 3OG7; Bollag G, Hirth P, Tsai J, Zhang J, Ibrahim PN, Cho H, et al. (September 2010). "Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma". Nature. 467 (7315): 596–599. Bibcode:2010Natur.467..596B. doi:10.1038/nature09454. PMC 2948082. PMID 20823850.
- ^ Sala E, Mologni L, Truffa S, Gaetano C, Bollag GE, Gambacorti-Passerini C (May 2008). "BRAF silencing by short hairpin RNA or chemical blockade by PLX4032 leads to different responses in melanoma and thyroid carcinoma cells". Molecular Cancer Research. 6 (5): 751–759. doi:10.1158/1541-7786.MCR-07-2001. PMID 18458053. S2CID 16031942.
- ^ Maverakis E, Cornelius LA, Bowen GM, Phan T, Patel FB, Fitzmaurice S, et al. (May 2015). "Metastatic melanoma - a review of current and future treatment options". Acta Dermato-Venereologica. 95 (5): 516–524. doi:10.2340/00015555-2035. PMID 25520039.
- ^ Hatzivassiliou G, Song K, Yen I, Brandhuber BJ, Anderson DJ, Alvarado R, et al. (March 2010). "RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth". Nature. 464 (7287): 431–435. Bibcode:2010Natur.464..431H. doi:10.1038/nature08833. PMID 20130576.
- ^ Halaban R, Zhang W, Bacchiocchi A, Cheng E, Parisi F, Ariyan S, et al. (April 2010). "PLX4032, a selective BRAF(V600E) kinase inhibitor, activates the ERK pathway and enhances cell migration and proliferation of BRAF melanoma cells". Pigment Cell & Melanoma Research. 23 (2): 190–200. doi:10.1111/j.1755-148X.2010.00685.x. PMC 2848976. PMID 20149136.
- ^ Nazarian R, Shi H, Wang Q, Kong X, Koya RC, Lee H, et al. (December 2010). "Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation". Nature. 468 (7326): 973–977. Bibcode:2010Natur.468..973N. doi:10.1038/nature09626. PMC 3143360. PMID 21107323.
- "Researchers Uncover Drug-Resistance Mechanisms in BRAF Melanoma". Genetic Engineering & Biotechnology News. November 25, 2010.
- ^ Straussman R, Morikawa T, Shee K, Barzily-Rokni M, Qian ZR, Du J, et al. (July 2012). "Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion". Nature. 487 (7408): 500–504. Bibcode:2012Natur.487..500S. doi:10.1038/nature11183. PMC 3711467. PMID 22763439.
- ^ Wilson TR, Fridlyand J, Yan Y, Penuel E, Burton L, Chan E, et al. (July 2012). "Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors". Nature. 487 (7408): 505–509. Bibcode:2012Natur.487..505W. doi:10.1038/nature11249. PMC 3724525. PMID 22763448.
- ^ "BRIM-2 Upholds Benefits Emerging with Vemurafenib in Melanoma". Oncology & Biotech News. 5 (7). July 2011.
- ^ "Drug hope for advanced melanoma". BBC News. 2009-06-02. Retrieved 2009-06-07.
- ^ Harmon A (2010-02-21). "A Roller Coaster Chase for a Cure". The New York Times.
- ^ Garber K (December 2009). "Cancer research. Melanoma drug vindicates targeted approach". Science. 326 (5960): 1619. Bibcode:2009Sci...326.1619G. doi:10.1126/science.326.5960.1619. PMID 20019269.
- ^ Flaherty K. "Phase I study of PLX4032: Proof of concept for V600E BRAF mutation as a therapeutic target in human cancer". 2009 ASCO Annual Meeting Abstract, J Clin Oncol 27:15s, 2009 (suppl; abstr 9000). Archived from the original on 2013-01-27. Retrieved 2010-09-10.
- ^ Flaherty KT, Puzanov I, Kim KB, Ribas A, McArthur GA, Sosman JA, et al. (August 2010). "Inhibition of mutated, activated BRAF in metastatic melanoma". The New England Journal of Medicine. 363 (9): 809–819. doi:10.1056/NEJMoa1002011. PMC 3724529. PMID 20818844.
- Lowe D (September 9, 2010). "PLX4032: The Good News and the Bad News". In the Pipeline. Corante. Archived from the original on 2010-09-11.
- ^ Clinical trial number NCT00405587 for "Safety Study of PLX4032 in Patients With Solid Tumors" at ClinicalTrials.gov
- ^ Clinical trial number NCT00949702 for "A Study of RO5185426 in Previously Treated Patients With Metastatic Melanoma" at ClinicalTrials.gov
- ^ "Plexxikon Announces First Patient Dosed in Phase 3 Trial of PLX4032 (RG7204) for Metastatic Melanoma" (Press release). Plexxikon. 2010-01-08. Archived from the original on 2020-12-01. Retrieved 2011-02-03.
- ^ a b "Plexxikon and Roche Report Positive Data from Phase III BRAF Mutation Melanoma Study". Genetic Engineering & Biotechnology News. Mary Ann Liebert Publishers. 6 June 2011.
- ^ "Vemurafenib Improves Overall Survival in Patients with Metastatic Melanoma". Archived from the original on 2022-01-11. Retrieved 2012-12-17.
- ^ "Cobimetinib at exelixis.com". Archived from the original on 2015-02-04. Retrieved 2015-02-04.
- ^ "MEK/BRAF Inhibitor Combo Reduces Death by One-Third in Melanoma". 2015.
- ^ "FDA Approves Zelboraf (Vemurafenib) and Companion Diagnostic for BRAF Mutation-Positive Metastatic Melanoma, a Deadly Form of Skin Cancer" (Press release). Genentech. Retrieved 2011-08-17.
- ^ Bollag G, Tsai J, Zhang J, Zhang C, Ibrahim P, Nolop K, Hirth P (November 2012). "Vemurafenib: the first drug approved for BRAF-mutant cancer". Nature Reviews. Drug Discovery. 11 (11): 873–886. doi:10.1038/nrd3847. PMID 23060265. S2CID 9337155.
- ^ "Notice of Decision for ZELBORAF". Health Canada. 11 March 2012. Archived from the original on 2 May 2012. Retrieved 21 April 2012.
- ^ Hofland P (February 20, 2012). "First Personalized Cancer Medicine Allows Patients with Deadly Form of Metastatic Melanoma to Live Significantly Longer". Onco'Zine. The International Cancer Network. Archived from the original on April 11, 2012. Retrieved February 18, 2013.
- ^ "FDA approves first treatment for certain patients with Erdheim–Chester disease, a rare blood cancer". U.S. Food and Drug Administration (FDA) (Press release). Retrieved 2018-05-20.
- ^ Diamond EL, Subbiah V, Lockhart AC, Blay JY, Puzanov I, Chau I, et al. (March 2018). "Vemurafenib for BRAF V600-Mutant Erdheim-Chester Disease and Langerhans Cell Histiocytosis: Analysis of Data From the Histology-Independent, Phase 2, Open-label VE-BASKET Study". JAMA Oncology. 4 (3): 384–388. doi:10.1001/jamaoncol.2017.5029. PMC 5844839. PMID 29188284.
- ^ "Getting close and personal". The Economist. January 4, 2014. ISSN 0013-0613. Retrieved 2016-04-15.
- ^ "Hairy Cell Leukemia: Celebrating Progress?". HCLF Blog. July 29, 2022. Retrieved July 25, 2022.
- ^ Clinical trial number NCT03410875 for "Hairy Cell Leukemia with Vemurafebib" at ClinicalTrials.gov
- ^ Handa S, Lee JO, Derkach A, Stone RM, Saven A, Altman JK, et al. (December 2022). "Long-term outcomes in patients with relapsed or refractory hairy cell leukemia treated with vemurafenib monotherapy". Blood. 140 (25): 2663–2671. doi:10.1182/blood.2022016183. PMC 9935554. PMID 35930750.
Further reading
[edit]- Dean L (2017). "Vemurafenib Therapy and BRAF and NRAS Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28809522. Bookshelf ID: NBK447416.
