Antiarrhythmic agent: Difference between revisions
CrafterNova (talk | contribs) →Vaughan Williams classification: ref fix, wording, removed redundancy |
Grbdeveaux (talk | contribs) m Typo arrhytmia > arrhythmia |
||
| (7 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
{{short description|Heart rhythm medication}} |
{{short description|Heart rhythm medication}} |
||
{{Infobox drug class |
|||
| Name = Antiarrhythmic agents |
|||
| Synonyms = antiarrhythmics, cardiac dysrhythmia medications |
|||
| Image = Amiodarone_structure.svg |
|||
| ImageClass = skin-invert-image |
|||
| Alt = Amiodarone |
|||
| Use = [[Arrhythmia]], [[Atrial fibrillation]], [[Ventricular tachycardia]], etc. |
|||
| Caption = [[Skeletal formula]] of [[amiodarone]], a common antiarrhythmic. |
|||
| Biological_target = Cardiac ion channels |
|||
| ATC_prefix = C01B |
|||
| MeshID = D000889 |
|||
| Drugs.com = {{Drugs.com|drug-class|antiarrhythmic-agents}} |
|||
| Consumer_Reports = |
|||
| medicinenet = |
|||
| rxlist = |
|||
}} |
|||
'''Antiarrhythmic agents''', also known as '''cardiac dysrhythmia medications''', are a class of [[drug]]s that are used to suppress abnormally fast rhythms ([[tachycardia]]s), such as [[atrial fibrillation]], [[supraventricular tachycardia]] and [[ventricular tachycardia]]. |
'''Antiarrhythmic agents''', also known as '''cardiac dysrhythmia medications''', are a class of [[drug]]s that are used to suppress abnormally fast rhythms ([[tachycardia]]s), such as [[atrial fibrillation]], [[supraventricular tachycardia]] and [[ventricular tachycardia]]. |
||
| Line 7: | Line 22: | ||
==Action potential== |
==Action potential== |
||
[[File:Cardiac action potential.svg|thumb|440px|Drugs affecting the [[cardiac action potential]]|alt=Plot of membrane potential versus time]] |
[[File:Cardiac action potential.svg|thumb|440px|class=skin-invert-image|Drugs affecting the [[cardiac action potential]]|alt=Plot of membrane potential versus time]] |
||
{{main|Cardiac action potential}} |
{{main|Cardiac action potential}} |
||
| Line 128: | Line 143: | ||
* [[Digoxin]] |
* [[Digoxin]] |
||
* [[Magnesium sulfate (medical use)|Magnesium sulfate]] |
* [[Magnesium sulfate (medical use)|Magnesium sulfate]] |
||
|Work by other or unknown mechanisms |
|Work by other or unknown mechanisms |
||
| |
| |
||
* Contraindicated in ventricular arrhythmias |
* Contraindicated in ventricular arrhythmias |
||
* Adenosine is used to treat [[supraventricular tachycardia]]s, especially in heart failure and atrial fibrillation<ref>{{Citation |last=Singh |first=Shashank |title=Adenosine |date=2023 |url=http://www.ncbi.nlm.nih.gov/books/NBK519049/ |work=StatPearls |access-date=2023-12-12 |place=Treasure Island (FL) |publisher=StatPearls Publishing |pmid=30085591 |last2=McKintosh |first2=Rebecca}}</ref> |
* Adenosine is used to treat [[supraventricular tachycardia]]s, especially in heart failure and atrial fibrillation<ref>{{Citation |last=Singh |first=Shashank |title=Adenosine |date=2023 |url=http://www.ncbi.nlm.nih.gov/books/NBK519049/ |work=StatPearls |access-date=2023-12-12 |place=Treasure Island (FL) |publisher=StatPearls Publishing |pmid=30085591 |last2=McKintosh |first2=Rebecca}}</ref> |
||
* Magnesium sulfate is used to treat ''[[torsades de pointes]]'', a type of |
* Magnesium sulfate is used to treat ''[[torsades de pointes]]'', a type of arrhythmia |
||
|- <!-- THIS IS TRUE |
|- <!-- THIS IS TRUE |
||
--> |
--> |
||
| Line 148: | Line 163: | ||
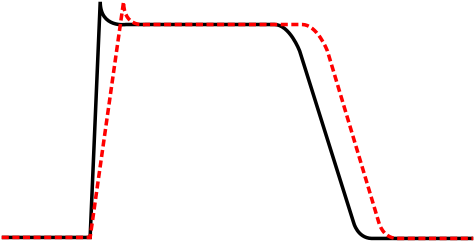
* Class Ic drugs do not significantly affect the action potential (no shift) |
* Class Ic drugs do not significantly affect the action potential (no shift) |
||
<div class="skin-invert-image"> |
|||
<gallery mode="packed" widths="360px" heights="160"> |
<gallery mode="packed" widths="360px" heights="160"> |
||
File:Action potential class Ia.svg|Class Ia |
File:Action potential class Ia.svg|Class Ia |
||
| Line 153: | Line 169: | ||
File:Action potential class Ic.svg|Class Ic |
File:Action potential class Ic.svg|Class Ic |
||
</gallery> |
</gallery> |
||
</div> |
|||
{{clear}} |
|||
===Class II agents=== |
===Class II agents=== |
||
| Line 160: | Line 178: | ||
===Class III agents=== |
===Class III agents=== |
||
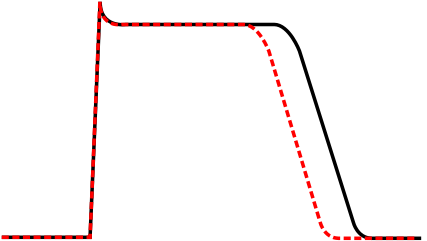
[[Image:Action potential Class III.svg|thumb|Effect of class III drugs on length of action potential]] |
[[Image:Action potential Class III.svg|thumb|class=skin-invert-image|Effect of class III drugs on length of action potential]] |
||
Class III agents predominantly [[Potassium channel blocker|block the potassium channels]], thereby prolonging repolarization.<ref>{{cite journal | last1 = Lenz | first1 = TL | last2 = Hilleman | first2 = DE | year = 2000 | title = Dofetilide, a New Class III Antiarrhythmic Agent | pmid = 10907968 | journal = Pharmacotherapy | volume = 20 | issue = 7| pages = 776–786 | doi=10.1592/phco.20.9.776.35208| s2cid = 19897963 }}</ref> Since these agents do not affect the sodium channel, conduction velocity is not decreased. The prolongation of the action potential duration and refractory period, combined with the maintenance of normal conduction velocity, prevent re-entrant arrhythmias. (The re-entrant rhythm is less likely to interact with tissue that has become refractory). The class III agents exhibit reverse-use dependence (their potency increases with slower heart rates, and therefore improves maintenance of sinus rhythm). Inhibiting potassium channels results in slowed atrial-ventricular myocyte repolarization. Class III agents have the potential to prolong the QT interval of the EKG, and may be proarrhythmic (more associated with development of polymorphic VT). |
Class III agents predominantly [[Potassium channel blocker|block the potassium channels]], thereby prolonging repolarization.<ref>{{cite journal | last1 = Lenz | first1 = TL | last2 = Hilleman | first2 = DE | year = 2000 | title = Dofetilide, a New Class III Antiarrhythmic Agent | pmid = 10907968 | journal = Pharmacotherapy | volume = 20 | issue = 7| pages = 776–786 | doi=10.1592/phco.20.9.776.35208| s2cid = 19897963 }}</ref> Since these agents do not affect the sodium channel, conduction velocity is not decreased. The prolongation of the action potential duration and refractory period, combined with the maintenance of normal conduction velocity, prevent re-entrant arrhythmias. (The re-entrant rhythm is less likely to interact with tissue that has become refractory). The class III agents exhibit reverse-use dependence (their potency increases with slower heart rates, and therefore improves maintenance of sinus rhythm). Inhibiting potassium channels results in slowed atrial-ventricular myocyte repolarization. Class III agents have the potential to prolong the QT interval of the EKG, and may be proarrhythmic (more associated with development of polymorphic VT). |
||
| Line 181: | Line 199: | ||
# Sympatholytic drugs (drugs blocking the effects of the [[sympathetic nervous system]]): examples included [[bretylium]] and [[Beta blocker|adrenergic beta-receptors blocking drugs]]. This is similar to the modern classification, which focuses on the latter category. |
# Sympatholytic drugs (drugs blocking the effects of the [[sympathetic nervous system]]): examples included [[bretylium]] and [[Beta blocker|adrenergic beta-receptors blocking drugs]]. This is similar to the modern classification, which focuses on the latter category. |
||
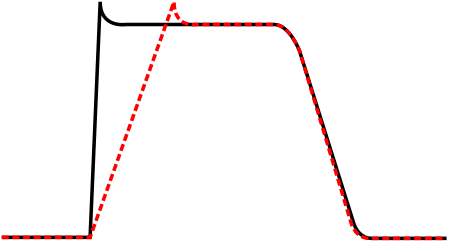
# Compounds that prolong the action potential: matching the modern classification, with the key drug example being [[amiodarone]], and a surgical example being [[thyroidectomy]]. This was not a defining characteristic in an earlier review by Charlier et al. (1968),<ref>{{cite journal|last1=Charlier|first1=R|last2=Deltour|first2=G|last3=Baudine|first3=A|last4=Chaillet|first4=F|title=Pharmacology of amiodarone, and anti-anginal drug with a new biological profile.|journal=Arzneimittel-Forschung|date=November 1968|volume=18|issue=11|pages=1408–1417|pmid=5755904}}</ref> but was supported by experimental data presented by Vaughan Williams (1970).{{r|VW70|p=461}} The figure illustrating these findings was also published in the same year by Singh and Vaughan Williams.<ref>{{cite journal|last1=Singh|first1=BN|last2=Vaughan Williams|first2=EM|title=The effect of amiodarone, a new anti-anginal drug, on cardiac muscle.|journal=British Journal of Pharmacology|date=August 1970|volume=39|issue=4|pages=657–667|pmid=5485142|doi=10.1111/j.1476-5381.1970.tb09891.x|pmc=1702721}}</ref> |
# Compounds that prolong the action potential: matching the modern classification, with the key drug example being [[amiodarone]], and a surgical example being [[thyroidectomy]]. This was not a defining characteristic in an earlier review by Charlier et al. (1968),<ref>{{cite journal|last1=Charlier|first1=R|last2=Deltour|first2=G|last3=Baudine|first3=A|last4=Chaillet|first4=F|title=Pharmacology of amiodarone, and anti-anginal drug with a new biological profile.|journal=Arzneimittel-Forschung|date=November 1968|volume=18|issue=11|pages=1408–1417|pmid=5755904}}</ref> but was supported by experimental data presented by Vaughan Williams (1970).{{r|VW70|p=461}} The figure illustrating these findings was also published in the same year by Singh and Vaughan Williams.<ref>{{cite journal|last1=Singh|first1=BN|last2=Vaughan Williams|first2=EM|title=The effect of amiodarone, a new anti-anginal drug, on cardiac muscle.|journal=British Journal of Pharmacology|date=August 1970|volume=39|issue=4|pages=657–667|pmid=5485142|doi=10.1111/j.1476-5381.1970.tb09891.x|pmc=1702721}}</ref> |
||
# Drugs acting like [[ |
# Drugs acting like [[diphenylhydantoin]] (DPH): mechanism of action unknown, but others had attributed its cardiac action to an indirect action on the brain;<ref>{{cite journal|last1=Damato|first1=Anthony N.|title=Diphenylhydantoin: Pharmacological and clinical use|journal=Progress in Cardiovascular Diseases|date=1 July 1969|volume=12|issue=1|pages=1–15|doi=10.1016/0033-0620(69)90032-2|pmid=5807584}}</ref> this drug is better known as antiepileptic drug [[phenytoin]]. |
||
==Sicilian gambit classification== |
==Sicilian gambit classification== |
||
| Line 189: | Line 207: | ||
==Modernized Oxford classification by Lei, Huang, Wu, and Terrar== |
==Modernized Oxford classification by Lei, Huang, Wu, and Terrar== |
||
[[File: Wikipedia_table_11_copy.jpg|thumb|Common anti-arrhythmic drugs under the modernized classification according to Lei et al. 2018]] |
[[File: Wikipedia_table_11_copy.jpg|thumb|class=skin-invert-image|Common anti-arrhythmic drugs under the modernized classification according to Lei et al. 2018]] |
||
A recent publication (2018) has now emerged with a fully modernised drug classification.<ref>{{cite journal |last1=Lei |first1=Ming |last2=Wu |first2=Lin |last3=Terrar |first3=Derek A. |last4=Huang |first4=Christopher L.-H. |title=Modernized Classification of Cardiac Antiarrhythmic Drugs |journal=Circulation |date=23 October 2018 |volume=138 |issue=17 |pages=1879–1896 |doi=10.1161/CIRCULATIONAHA.118.035455|pmid=30354657 |doi-access=free }}</ref> This preserves the simplicity of the original Vaughan Williams framework while capturing subsequent discoveries of sarcolemmal, sarcoplasmic reticular and cytosolic biomolecules. The result is an expanded but pragmatic classification that encompasses approved and potential anti-arrhythmic drugs. This will aid our understanding and clinical management of cardiac arrhythmias and facilitate future therapeutic developments. It starts by considering the range of pharmacological targets, and tracks these to their particular cellular electrophysiological effects. It retains but expands the original Vaughan Williams classes I to IV, respectively covering actions on Na+ current components, autonomic signalling, K<sup>+</sup> channel subspecies, and molecular targets related to Ca<sup>2+</sup> homeostasis. It now introduces new classes incorporating additional targets, including: |
A recent publication (2018) has now emerged with a fully modernised drug classification.<ref>{{cite journal |last1=Lei |first1=Ming |last2=Wu |first2=Lin |last3=Terrar |first3=Derek A. |last4=Huang |first4=Christopher L.-H. |title=Modernized Classification of Cardiac Antiarrhythmic Drugs |journal=Circulation |date=23 October 2018 |volume=138 |issue=17 |pages=1879–1896 |doi=10.1161/CIRCULATIONAHA.118.035455|pmid=30354657 |doi-access=free }}</ref> This preserves the simplicity of the original Vaughan Williams framework while capturing subsequent discoveries of sarcolemmal, sarcoplasmic reticular and cytosolic biomolecules. The result is an expanded but pragmatic classification that encompasses approved and potential anti-arrhythmic drugs. This will aid our understanding and clinical management of cardiac arrhythmias and facilitate future therapeutic developments. It starts by considering the range of pharmacological targets, and tracks these to their particular cellular electrophysiological effects. It retains but expands the original Vaughan Williams classes I to IV, respectively covering actions on Na+ current components, autonomic signalling, K<sup>+</sup> channel subspecies, and molecular targets related to Ca<sup>2+</sup> homeostasis. It now introduces new classes incorporating additional targets, including: |
||
*Class 0: ion channels involved in automaticity |
*Class 0: ion channels involved in automaticity |
||
| Line 201: | Line 219: | ||
* [[Cardiac Arrhythmia Suppression Trial]] (CAST) |
* [[Cardiac Arrhythmia Suppression Trial]] (CAST) |
||
* [[Electrocardiogram]] |
* [[Electrocardiogram]] |
||
* [[Management of atrial fibrillation]] |
|||
* [[Proarrhythmic agent]] |
* [[Proarrhythmic agent]] |
||
Latest revision as of 22:41, 21 December 2024
| Antiarrhythmic agents | |
|---|---|
| Drug class | |
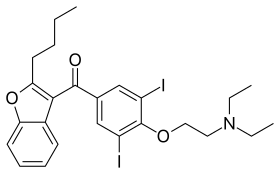 Skeletal formula of amiodarone, a common antiarrhythmic. | |
| Class identifiers | |
| Synonyms | antiarrhythmics, cardiac dysrhythmia medications |
| Use | Arrhythmia, Atrial fibrillation, Ventricular tachycardia, etc. |
| ATC code | C01B |
| Biological target | Cardiac ion channels |
| Clinical data | |
| Drugs.com | Drug Classes |
| External links | |
| MeSH | D000889 |
| Legal status | |
| In Wikidata | |
Antiarrhythmic agents, also known as cardiac dysrhythmia medications, are a class of drugs that are used to suppress abnormally fast rhythms (tachycardias), such as atrial fibrillation, supraventricular tachycardia and ventricular tachycardia.
Many attempts have been made to classify antiarrhythmic agents. Many of the antiarrhythmic agents have multiple modes of action, which makes any classification imprecise.
Action potential
[edit]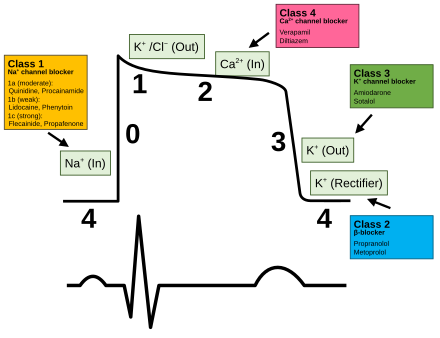
The cardiac myocyte has two general types of action potentials: conduction system and working myocardium. The action potential is divided into 5 phases and shown in the diagram. The sharp rise in voltage ("0") corresponds to the influx of sodium ions, whereas the two decays ("1" and "3", respectively) correspond to the sodium-channel inactivation and the repolarizing efflux of potassium ions. The characteristic plateau ("2") results from the opening of voltage-sensitive calcium channels. Each phase utilizes different channels and it is useful to compare these phases to the most common classification system — Vaughan Williams — described below.
Vaughan Williams classification
[edit]The Vaughan Williams classification[1] was introduced in 1970 by Miles Vaughan Williams.[2]
Vaughan Williams was a pharmacology tutor at Hertford College, Oxford. One of his students, Bramah N. Singh,[3] contributed to the development of the classification system. The system is therefore sometimes known as the Singh-Vaughan Williams classification.
The five main classes in the Vaughan Williams classification of antiarrhythmic agents are:
- Class I agents interfere with the sodium (Na+) channel.
- Class II agents are anti-sympathetic nervous system agents. Most agents in this class are beta blockers.
- Class III agents affect potassium (K+) efflux.
- Class IV agents affect calcium channels and the AV node.
- Class V agents work by other or unknown mechanisms.
With regard to management of atrial fibrillation, classes I and III are used in rhythm control as medical cardioversion agents, while classes II and IV are used as rate-control agents.
| Class | Known as | Examples | Mechanism | Medical uses[4] |
|---|---|---|---|---|
| Ia | Fast sodium channel blockers | Na+ channel block (intermediate association/dissociation) and K+ channel blocking effect.
Class Ia drugs prolong the action potential and has an intermediate effect on the 0 phase of depolarization. |
| |
| Ib | Na+ channel block (fast association/dissociation).
Class Ib drugs shorten the action potential of myocardial cell and has a weak effect on the initiation of phase 0 of depolarization |
| ||
| Ic | Na+ channel block (slow association/dissociation).
Class Ic drugs do not affect action potential duration and have the strongest effect on the initiation phase 0 of depolarization |
| ||
| II | Beta-blockers | Beta blocker Propranolol also has some sodium channel-blocking effect. |
| |
| III | Potassium channel blockers | K+ channel blocker
Sotalol is also a beta blocker[5] |
| |
| IV | Calcium channel blockers | Ca2+ channel blocker |
| |
| V | Work by other or unknown mechanisms |
|
Class I agents
[edit]The class I antiarrhythmic agents interfere with the sodium channel. Class I agents are grouped by what effect they have on the Na+ channel, and what effect they have on cardiac action potentials.
Class I agents are called membrane-stabilizing agents, "stabilizing" referring to the decrease of excitogenicity of the plasma membrane which is brought about by these agents. (Also noteworthy is that a few class II agents like propranolol also have a membrane stabilizing effect.)
Class I agents are divided into three groups (Ia, Ib, and Ic) based upon their effect on the length of the action potential.[10][11]
- Class Ia drugs lengthen the action potential (right shift)
- Class Ib drugs shorten the action potential (left shift)
- Class Ic drugs do not significantly affect the action potential (no shift)
Class II agents
[edit]Class II agents are conventional beta blockers. They act by blocking the effects of catecholamines at the β1-adrenergic receptors, thereby decreasing sympathetic activity on the heart, which reduces intracellular cAMP levels and hence reduces Ca2+ influx. These agents are particularly useful in the treatment of supraventricular tachycardias. They decrease conduction through the AV node.
Class II agents include atenolol, esmolol, propranolol, and metoprolol.
Class III agents
[edit]
Class III agents predominantly block the potassium channels, thereby prolonging repolarization.[12] Since these agents do not affect the sodium channel, conduction velocity is not decreased. The prolongation of the action potential duration and refractory period, combined with the maintenance of normal conduction velocity, prevent re-entrant arrhythmias. (The re-entrant rhythm is less likely to interact with tissue that has become refractory). The class III agents exhibit reverse-use dependence (their potency increases with slower heart rates, and therefore improves maintenance of sinus rhythm). Inhibiting potassium channels results in slowed atrial-ventricular myocyte repolarization. Class III agents have the potential to prolong the QT interval of the EKG, and may be proarrhythmic (more associated with development of polymorphic VT).
Class III agents include: bretylium, amiodarone, ibutilide, sotalol, dofetilide, vernakalant, and dronedarone.
Class IV agents
[edit]Class IV agents are slow non-dihydropyridine calcium channel blockers. They decrease conduction through the AV node, and shorten phase two (the plateau) of the cardiac action potential. They thus reduce the contractility of the heart, so may be inappropriate in heart failure. However, in contrast to beta blockers, they allow the body to retain adrenergic control of heart rate and contractility.[citation needed]
Class IV agents include verapamil and diltiazem.
Class V and others
[edit]Since the development of the original Vaughan Williams classification system, additional agents have been used that do not fit cleanly into categories I through IV. Such agents include:
- Adenosine is used intravenously for terminating supraventricular tachycardias.[13]
- Digoxin decreases conduction of electrical impulses through the AV node and increases vagal activity via its action on the central nervous system. Via indirect action, it leads to an increase in acetylcholine production, stimulating M2 receptors on AV node leading to an overall decrease in speed of conduction.
- Magnesium sulfate is an antiarrhythmic drug, but only used against very specific arrhythmias[14] such as torsades de pointes.[15][16]
History
[edit]The initial classification system had 4 classes, although their definitions different from the modern classification. Those proposed in 1970 were:[2]
- Drugs with a direct membrane action: the prototype was quinidine, and lignocaine was a key example. Differing from other authors, Vaughan-Williams describe the main action as a slowing of the rising phase of the action potential.
- Sympatholytic drugs (drugs blocking the effects of the sympathetic nervous system): examples included bretylium and adrenergic beta-receptors blocking drugs. This is similar to the modern classification, which focuses on the latter category.
- Compounds that prolong the action potential: matching the modern classification, with the key drug example being amiodarone, and a surgical example being thyroidectomy. This was not a defining characteristic in an earlier review by Charlier et al. (1968),[17] but was supported by experimental data presented by Vaughan Williams (1970).[2]: 461 The figure illustrating these findings was also published in the same year by Singh and Vaughan Williams.[18]
- Drugs acting like diphenylhydantoin (DPH): mechanism of action unknown, but others had attributed its cardiac action to an indirect action on the brain;[19] this drug is better known as antiepileptic drug phenytoin.
Sicilian gambit classification
[edit]Another approach, known as the "Sicilian gambit", placed a greater approach on the underlying mechanism.[20][21][22]
It presents the drugs on two axes, instead of one, and is presented in tabular form. On the Y axis, each drug is listed, in roughly the Singh-Vaughan Williams order. On the X axis, the channels, receptors, pumps, and clinical effects are listed for each drug, with the results listed in a grid. It is, therefore, not a true classification in that it does not aggregate drugs into categories.[23]
Modernized Oxford classification by Lei, Huang, Wu, and Terrar
[edit]
A recent publication (2018) has now emerged with a fully modernised drug classification.[24] This preserves the simplicity of the original Vaughan Williams framework while capturing subsequent discoveries of sarcolemmal, sarcoplasmic reticular and cytosolic biomolecules. The result is an expanded but pragmatic classification that encompasses approved and potential anti-arrhythmic drugs. This will aid our understanding and clinical management of cardiac arrhythmias and facilitate future therapeutic developments. It starts by considering the range of pharmacological targets, and tracks these to their particular cellular electrophysiological effects. It retains but expands the original Vaughan Williams classes I to IV, respectively covering actions on Na+ current components, autonomic signalling, K+ channel subspecies, and molecular targets related to Ca2+ homeostasis. It now introduces new classes incorporating additional targets, including:
- Class 0: ion channels involved in automaticity
- Class V: mechanically sensitive ion channels
- Class VI: connexins controlling electrotonic cell coupling
- Class VII: molecules underlying longer term signalling processes affecting structural remodeling.
It also allows for multiple drug targets/actions and adverse pro-arrhythmic effects. The new scheme will additionally aid development of novel drugs under development and is illustrated here.
See also
[edit]- Antiarrhythmic agents (category)
- Cardiac Arrhythmia Suppression Trial (CAST)
- Electrocardiogram
- Management of atrial fibrillation
- Proarrhythmic agent
References
[edit]- ^ Rang, Humphrey P.; Ritter, James M.; Flower, Rod J.; Henderson, Graeme (2012). Rang and Dale's pharmacology (7th ed.). Elsevier. p. 255. ISBN 9780702034718.
- ^ a b c Vaughan Williams, EM (1970) "Classification of antiarrhythmic drugs". In Symposium on Cardiac Arrhythmias (Eds. Sandoe E; Flensted-Jensen E; Olsen KH). Astra, Elsinore. Denmark (1970)[ISBN missing]
- ^ Kloner RA (2009). "A Salute to Our Founding Editor-in-Chief Bramah N. Singh, MD, DPhil, DSc, FRCP". Journal of Cardiovascular Pharmacology and Therapeutics. 14 (3): 154–156. doi:10.1177/1074248409343182. PMID 19721129. S2CID 44733401.
- ^ Unless else specified in boxes, then ref is: Rang, H. P. (2003). Pharmacology. Edinburgh: Churchill Livingstone. ISBN 978-0-443-07145-4.[page needed]
- ^ Kulmatycki KM, Abouchehade K, Sattari S, Jamali F (May 2001). "Drug-disease interactions: reduced beta-adrenergic and potassium channel antagonist activities of sotalol in the presence of acute and chronic inflammatory conditions in the rat". Br. J. Pharmacol. 133 (2): 286–294. doi:10.1038/sj.bjp.0704067. PMC 1572777. PMID 11350865.
- ^ Waller, Derek G.; Sampson, Tony (2013). Medical Pharmacology and Therapeutics E-Book. Elsevier Health Sciences. p. 144. ISBN 9780702055034.
- ^ "treatment of paroxysmal atrial fibrillation – General Practice Notebook". www.gpnotebook.co.uk.
- ^ "protocol for management of haemodynamically stable ventricular tachycardia – General Practice Notebook". www.gpnotebook.co.uk. Retrieved 2016-02-09.
- ^ Singh, Shashank; McKintosh, Rebecca (2023), "Adenosine", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30085591, retrieved 2023-12-12
- ^ Milne JR, Hellestrand KJ, Bexton RS, Burnett PJ, Debbas NM, Camm AJ (February 1984). "Class 1 antiarrhythmic drugs – characteristic electrocardiographic differences when assessed by atrial and ventricular pacing". Eur. Heart J. 5 (2): 99–107. doi:10.1093/oxfordjournals.eurheartj.a061633. PMID 6723689.
- ^ Trevor, Anthony J.; Katzung, Bertram G. (2003). Pharmacology. New York: Lange Medical Books/McGraw-Hill, Medical Publishing Division. p. 43. ISBN 978-0-07-139930-2.
- ^ Lenz, TL; Hilleman, DE (2000). "Dofetilide, a New Class III Antiarrhythmic Agent". Pharmacotherapy. 20 (7): 776–786. doi:10.1592/phco.20.9.776.35208. PMID 10907968. S2CID 19897963.
- ^ Conti JB, Belardinelli L, Utterback DB, Curtis AB (March 1995). "Endogenous adenosine is an antiarrhythmic agent". Circulation. 91 (6): 1761–1767. doi:10.1161/01.cir.91.6.1761. PMID 7882485.
- ^ Brugada P (July 2000). "Magnesium: an antiarrhythmic drug, but only against very specific arrhythmias". Eur. Heart J. 21 (14): 1116. doi:10.1053/euhj.2000.2142. PMID 10924290.
- ^ Hoshino K, Ogawa K, Hishitani T, Isobe T, Eto Y (October 2004). "Optimal administration dosage of magnesium sulfate for torsades de pointes in children with long QT syndrome". J Am Coll Nutr. 23 (5): 497S – 500S. doi:10.1080/07315724.2004.10719388. PMID 15466950. S2CID 30146333.
- ^ Hoshino K, Ogawa K, Hishitani T, Isobe T, Etoh Y (April 2006). "Successful uses of magnesium sulfate for torsades de pointes in children with long QT syndrome". Pediatr Int. 48 (2): 112–117. doi:10.1111/j.1442-200X.2006.02177.x. PMID 16635167. S2CID 24904388.
- ^ Charlier, R; Deltour, G; Baudine, A; Chaillet, F (November 1968). "Pharmacology of amiodarone, and anti-anginal drug with a new biological profile". Arzneimittel-Forschung. 18 (11): 1408–1417. PMID 5755904.
- ^ Singh, BN; Vaughan Williams, EM (August 1970). "The effect of amiodarone, a new anti-anginal drug, on cardiac muscle". British Journal of Pharmacology. 39 (4): 657–667. doi:10.1111/j.1476-5381.1970.tb09891.x. PMC 1702721. PMID 5485142.
- ^ Damato, Anthony N. (1 July 1969). "Diphenylhydantoin: Pharmacological and clinical use". Progress in Cardiovascular Diseases. 12 (1): 1–15. doi:10.1016/0033-0620(69)90032-2. PMID 5807584.
- ^ "The 'Sicilian Gambit'. A new approach to the classification of antiarrhythmic drugs based on their actions on arrhythmogenic mechanisms. The Task Force of the Working Group on Arrhythmias of the European Society of Cardiology". Eur. Heart J. 12 (10): 1112–1131. October 1991. PMID 1723682.
- ^ Vaughan Williams EM (November 1992). "Classifying antiarrhythmic actions: by facts or speculation". J Clin Pharmacol. 32 (11): 964–977. doi:10.1002/j.1552-4604.1992.tb03797.x. PMID 1474169. S2CID 70464824.
- ^ "Milestones in the Evolution of the Study of Arrhythmias". Retrieved 2008-07-31. [dead link]
- ^ Fogoros, Richard N. (1997). Antiarrhythmic drugs: a practical guide. Oxford: Blackwell Science. p. 49. ISBN 978-0-86542-532-3.
- ^ Lei, Ming; Wu, Lin; Terrar, Derek A.; Huang, Christopher L.-H. (23 October 2018). "Modernized Classification of Cardiac Antiarrhythmic Drugs". Circulation. 138 (17): 1879–1896. doi:10.1161/CIRCULATIONAHA.118.035455. PMID 30354657.