Wilson's disease: Difference between revisions
Citation bot (talk | contribs) Removed parameters. | Use this bot. Report bugs. | #UCB_CommandLine |
|||
| (45 intermediate revisions by 24 users not shown) | |||
| Line 1: | Line 1: | ||
{{short description|Genetic multisystem copper-transport disease}} |
{{short description|Genetic multisystem copper-transport disease}} |
||
{{distinguish|text=[[Wilson's temperature syndrome]], an alternative medicine concept}} |
{{distinguish|text=[[Wilson's temperature syndrome]], an alternative medicine concept}} |
||
{{cs1 config|name-list-style=vanc}} |
|||
{{Infobox medical condition (new) |
{{Infobox medical condition (new) |
||
| name = Wilson's disease |
| name = Wilson's disease |
||
| image = |
| image = Wilson's Disease 4.jpg |
||
| image_size = |
| image_size = |
||
| caption = |
| caption = Boy with Wilson's disease |
||
| synonyms = Wilson disease, hepatolenticular degeneration |
| synonyms = Wilson disease, hepatolenticular degeneration |
||
| field = [[Gastroenterology]] |
| field = [[Gastroenterology]] |
||
| Line 22: | Line 23: | ||
}} |
}} |
||
<!-- Definition and symptoms --> |
<!-- Definition and symptoms --> |
||
'''Wilson's disease''' is a [[genetic disorder]] |
'''Wilson's disease''' (also called '''hepatolenticular degeneration''') is a [[genetic disorder]] characterized by the excess build-up of [[copper]] in the body. Symptoms are typically related to the [[brain]] and [[liver]]. Liver-related symptoms include [[vomiting]], weakness, [[ascites|fluid build-up in the abdomen]], [[edema|swelling of the legs]], [[jaundice|yellowish skin]], and [[pruritus|itchiness]]. Brain-related symptoms include [[tremor]]s, muscle stiffness, trouble in speaking, personality changes, anxiety, and [[psychosis]].<ref name=NIH2014>{{cite web|access-date=2016-11-06|title=Wilson Disease|url=https://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/wilson-disease/Pages/facts.aspx|website=NIDDK|date=July 2014|url-status=dead|archive-url=https://web.archive.org/web/20161004223012/https://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/wilson-disease/Pages/facts.aspx|archive-date=2016-10-04}}</ref> |
||
<!-- Cause and diagnosis --> |
<!-- Cause and diagnosis --> |
||
Wilson's disease is caused by a [[mutation]] in the [[Wilson disease protein]] (''ATP7B'') [[gene]]. This protein [[Transport protein|transports]] excess copper into [[bile]], where it is excreted in waste products. The condition is [[autosomal recessive]]; for |
Wilson's disease is caused by a [[mutation]] in the [[Wilson disease protein]] (''ATP7B'') [[gene]]. This protein [[Transport protein|transports]] excess copper into [[bile]], where it is excreted in waste products. The condition is [[autosomal recessive]]; for people to be affected, they must inherit a mutated copy of the gene from both parents. Diagnosis may be difficult and often involves a combination of blood tests, urine tests, and a [[liver biopsy]]. [[Genetic testing]] may be used to screen family members of those affected.<ref name=NIH2014/> |
||
<!-- Treatment --> |
<!-- Treatment --> |
||
Wilson's disease is typically treated with dietary changes and medication. Dietary changes involve eating a low-copper diet and not using copper cookware. Medications used include [[chelating agents]] such as [[trientine]] and [[d-penicillamine]] and [[zinc supplements]]. Complications of Wilson's disease can include [[liver failure |
Wilson's disease is typically treated with dietary changes and medication. Dietary changes involve eating a low-copper diet and not using copper cookware. Medications used include [[chelating agents]], such as [[trientine]] and [[d-penicillamine|<small>D</small>-penicillamine]], and [[zinc supplements]]. Complications of Wilson's disease can include [[liver failure]] and [[Renal tubular acidosis|kidney problems]]. A [[liver transplantation|liver transplant]] may be helpful to those for whom other treatments are not effective or if liver failure occurs.<ref name=NIH2014/> |
||
<!-- History and epidemiology --> |
<!-- History and epidemiology --> |
||
Wilson's disease occurs in about |
Wilson's disease occurs in about one in 30,000 people.<ref name=NIH2014/> Symptoms usually begin between the ages of 5 and 35 years.<ref name=NIH2014/> It was first described in 1854 by German pathologist [[Friedrich Theodor von Frerichs]] and is named after British neurologist [[Samuel Alexander Kinnier Wilson|Samuel Wilson]].<ref>{{cite web|access-date=2016-11-06|title=Whonamedit – dictionary of medical eponyms|url=http://www.whonamedit.com/synd.cfm/1818.html|website=www.whonamedit.com|url-status=dead|archive-url=https://web.archive.org/web/20161107014106/http://www.whonamedit.com/synd.cfm/1818.html|archive-date=2016-11-07}}</ref> |
||
==Signs and symptoms== |
==Signs and symptoms== |
||
The main sites of copper accumulation are the [[liver]] and |
The main sites of copper accumulation are the [[liver]] and [[Human brain|brain]]. Consequently, liver disease and neuropsychiatric symptoms are the main features that lead to diagnosis.<ref name=Ala>{{cite journal |vauthors=Ala A, Walker AP, Ashkan K, Dooley JS, Schilsky ML |title=Wilson's disease |journal=Lancet |volume=369 |issue=9559 |pages=397–408 |year=2007 |pmid=17276780 |doi=10.1016/S0140-6736(07)60196-2|s2cid=24663871 }}</ref> People with liver problems tend to come for medical attention earlier (generally as children or teenagers) than those with neurological and psychiatric symptoms, who tend to be in their 20s or older. Some are identified only because relatives have been diagnosed with Wilson's disease; many of these, when tested, turn out to have been experiencing symptoms of the condition but have not received a diagnosis.<ref name=Merle2007>{{cite journal |vauthors=Merle U, Schaefer M, Ferenci P, Stremmel W |title=Clinical presentation, diagnosis and long-term outcome of Wilson's disease: a cohort study |journal=Gut |volume=56 |issue=1 |pages=115–20 |year=2007 |pmid=16709660 |doi=10.1136/gut.2005.087262 |pmc=1856673 }}</ref> |
||
===Liver disease=== |
===Liver disease=== |
||
Liver disease may present itself as [[tiredness]], increased bleeding tendency or confusion (due to [[hepatic encephalopathy]]) and [[portal hypertension]]. The |
Liver disease may present itself as [[tiredness]], [[jaundice]], increased bleeding tendency or confusion (due to [[hepatic encephalopathy]]), and [[portal hypertension]].<ref>{{Cite web |title=Wilson's disease - Symptoms and causes |url=https://www.mayoclinic.org/diseases-conditions/wilsons-disease/symptoms-causes/syc-20353251 |access-date=2022-10-05 |website=Mayo Clinic |language=en}}</ref> The last, a condition in which the pressure in the [[portal vein]] is markedly increased, leads to [[esophageal varices]] (distended veins in the [[esophagus]] that may bleed in a life-threatening fashion) as well as enlargement of the spleen ([[splenomegaly]]) and accumulation of fluid in the abdominal cavity ([[ascites]]). On examination, signs of chronic liver disease such as [[spider angioma]]ta (small distended blood vessels, usually on the chest) may be observed. [[Chronic active hepatitis]] has already caused [[cirrhosis]] of the liver in most patients by the time they develop symptoms. While most people with cirrhosis have an increased risk of [[hepatocellular carcinoma]] (liver cancer), this risk is relatively low in Wilson's disease.<ref name=Ala/> |
||
About 5% of all people are diagnosed only when they develop fulminant [[acute liver failure]], often in the context of |
About 5% of all people are diagnosed only when they develop [[fulminant]] [[acute liver failure]], often in the context of [[hemolytic anemia]] (anemia due to the destruction of red blood cells). This leads to abnormalities in protein production (identified by [[Coagulopathy|deranged coagulation]]) and metabolism by the liver. The deranged protein metabolism leads to the accumulation of waste products, such as [[ammonia]], in the bloodstream. When these irritate the brain, patients develop [[hepatic encephalopathy]] – a serious condition that causes confusion, coma, seizures and, finally, life-threatening [[Cerebral edema|swelling of the brain]]).<ref name=Ala/> |
||
===Neuropsychiatric symptoms=== |
===Neuropsychiatric symptoms=== |
||
[[File:Wilson's Disease 5.jpg|thumb|Girl with Wilson's disease showing neurological symptoms]] |
|||
About half of the people with Wilson's disease have neurological or psychiatric symptoms. Most initially have mild cognitive deterioration and clumsiness, as well as changes in behavior. Specific neurological symptoms usually then follow, often in the form of [[parkinsonism]] (cogwheel rigidity, [[bradykinesia]] or slowed movements and a lack of balance are the most common parkinsonian features<ref name=Lorincz2010 />) with or without a typical hand [[tremor]], masked facial expressions, slurred speech, [[ataxia]] (lack of coordination) or [[dystonia]] (twisting and repetitive movements of part of the body). [[Seizure]]s and [[migraine]] appear to be more common in Wilson's disease.<ref name=Ala/> A characteristic tremor described as "wing-beating tremor" is encountered in many people with Wilson's; this is absent at rest but can be provoked by abducting the arms and flexing the elbows toward the midline.<ref>{{cite book|last=Pagonabarraga|first=J|title=Practical Neurology|date=2012|publisher=Wolters Kluwer/Lippincott Williams & Wilkins Heath|location=Philadelphia|isbn=978-1451142631|page=282|edition=4th|author2=Goetz, C |editor=Biller, J}}</ref> |
About half of the people with Wilson's disease have neurological or psychiatric symptoms. Most initially have mild cognitive deterioration and clumsiness, as well as changes in behavior. Specific neurological symptoms usually then follow, often in the form of [[parkinsonism]] (cogwheel rigidity, [[bradykinesia]], or slowed movements and a lack of balance are the most common parkinsonian features<ref name=Lorincz2010 />) with or without a typical hand [[tremor]], masked facial expressions, slurred speech, [[ataxia]] (lack of coordination), or [[dystonia]] (twisting and repetitive movements of part of the body). [[Seizure]]s and [[migraine]] appear to be more common in Wilson's disease.<ref name=Ala/> A characteristic tremor described as "wing-beating tremor" is encountered in many people with Wilson's; this is absent at rest but can be provoked by abducting the arms and flexing the elbows toward the midline.<ref>{{cite book|last=Pagonabarraga|first=J|title=Practical Neurology|date=2012|publisher=Wolters Kluwer/Lippincott Williams & Wilkins Heath|location=Philadelphia|isbn=978-1451142631|page=282|edition=4th|author2=Goetz, C |editor=Biller, J}}</ref> |
||
Cognition can also be affected in Wilson's disease |
Cognition can also be affected in Wilson's disease, in two non-mutually exclusive categories: [[frontal lobe disorder]] (may present as [[impulsivity]], impaired judgement, [[promiscuity]], [[apathy]], and [[executive dysfunction]] with poor planning and decision-making) and [[subcortical dementia]] (may present as slow thinking, memory loss, and [[executive dysfunction]], without signs of [[aphasia]], [[apraxia]], or [[agnosia]]). These cognitive involvements are thought to be related and closely linked to psychiatric manifestations of the disease.<ref name=Lorincz2010>{{cite journal | author=Lorincz MT | year=2010 | title=Neurologic Wilson's disease | journal=Annals of the New York Academy of Sciences | volume=1184 | issue=1 | pages=173–87 | doi=10.1111/j.1749-6632.2009.05109.x | pmid=20146697 | bibcode=2010NYASA1184..173L | hdl=2027.42/78731 | s2cid=2989668 | url=https://deepblue.lib.umich.edu/bitstream/2027.42/78731/1/j.1749-6632.2009.05109.x.pdf | hdl-access=free }}</ref> |
||
Psychiatric problems due to Wilson's disease may include behavioral changes, [[clinical depression|depression]], [[anxiety disorders]], and [[psychosis]].<ref name=Ala/> Psychiatric symptoms are commonly seen in conjunction with neurological symptoms and are rarely manifested on their own. These symptoms are often poorly defined and can sometimes be attributed to other causes. Because of this, diagnosis of Wilson's disease is rarely made when only psychiatric symptoms are present.<ref name=Lorincz2010 /> |
Psychiatric problems due to Wilson's disease may include behavioral changes, [[clinical depression|depression]], [[anxiety disorders]], and [[psychosis]].<ref name=Ala/> Psychiatric symptoms are commonly seen in conjunction with neurological symptoms and are rarely manifested on their own. These symptoms are often poorly defined and can sometimes be attributed to other causes. Because of this, diagnosis of Wilson's disease is rarely made when only psychiatric symptoms are present.<ref name=Lorincz2010 /> |
||
=== Other organ systems === |
=== Other organ systems === |
||
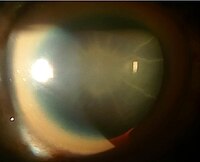
[[File:Kayser-Fleischer ringArrow.jpg|thumb|A brown ring on the edge of the iris ([[Kayser–Fleischer ring]]) is common in Wilson's disease, especially when neurological symptoms are present.]] |
|||
Medical conditions have been linked with copper accumulation in Wilson's disease: |
Medical conditions have been linked with copper accumulation in Wilson's disease: |
||
* '''Eyes:''' [[Kayser–Fleischer ring]]s (KF rings) |
* '''Eyes:''' [[Kayser–Fleischer ring]]s (KF rings) may be visible in the [[cornea]] of the eyes, either directly or on [[slit lamp]] examination, as deposits of copper form a ring around the cornea. This is due to copper deposition in [[Descemet's membrane]]. These rings can be either dark brown, golden, or reddish-green, are 1 to 3mm wide, and appear at the corneal limbus. They do not occur in all people with Wilson's disease, and may be seen in people with chronic [[cholestasis]].<ref name="Pandey">{{cite journal|url=https://www.ncbi.nlm.nih.gov/books/NBK459187/|title=Kayser-Fleischer Ring|date=21 June 2022|last1=Pandey|first1=Nivedita|last2=John|first2=Savio|access-date=30 November 2022|publisher=StatPearls Publishing|location=Treasure Island, Florida|journal=StatPearls|pmid=29083643}}</ref><ref name="Roberts2008">{{cite journal|last1=Roberts|first1=Eve A.|last2=Schilsky|first2=Michael L. |title=Diagnosis and treatment of Wilson disease: An update|journal=Hepatology|volume=47|issue=6|year=2008|pages=2089–2111|doi=10.1002/hep.22261|doi-access=free|pmid=18506894}}</ref> Wilson's disease is also associated with sunflower [[cataract]]s exhibited by brown or green pigmentation of the anterior and posterior lens capsule.<ref>{{cite book |last=Yanoff |first=Myron|author2=Jay S. Duker |title=Ophthalmology|year=2008|publisher=Mosby|location=Edinburgh|isbn=978-0323057516 |pages=411|edition=3rd}}</ref> Neither causes significant visual loss.<ref name=Ala/> KF rings occur in approximately 66% of diagnosed cases (more often in those with neurological symptoms rather than with liver problems).<ref name=Merle2007/> |
||
* '''Kidneys:''' [[renal tubular acidosis#Type 2-Proximal RTA|renal tubular acidosis]] (Type 2), a disorder of [[bicarbonate]] handling by the [[proximal tubule]]s leads to [[nephrocalcinosis]] (calcium accumulation in the kidneys), a weakening of bones (due to calcium and phosphate loss), and occasionally [[aminoaciduria]] (loss of essential [[amino acid]]s needed for protein synthesis).<ref name=Ala/> |
* '''Kidneys:''' [[renal tubular acidosis#Type 2-Proximal RTA|renal tubular acidosis]] (Type 2), a disorder of [[bicarbonate]] handling by the [[proximal tubule]]s leads to [[nephrocalcinosis]] (calcium accumulation in the kidneys), a weakening of bones (due to calcium and phosphate loss), and occasionally [[aminoaciduria]] (loss of essential [[amino acid]]s needed for protein synthesis).<ref name=Ala/> |
||
* '''Heart:''' [[cardiomyopathy]] (weakness of the heart muscle) is a rare but recognized problem in Wilson's disease; it may lead to [[heart failure]] (fluid accumulation due to decreased pump function) and [[cardiac arrhythmia]]s (episodes of irregular and/or abnormally fast or slow heart beat).<ref name=Ala/> |
* '''Heart:''' [[cardiomyopathy]] (weakness of the heart muscle) is a rare but recognized problem in Wilson's disease; it may lead to [[heart failure]] (fluid accumulation due to decreased pump function) and [[cardiac arrhythmia]]s (episodes of irregular and/or abnormally fast or slow heart beat).<ref name=Ala/> |
||
* '''Hormones:''' [[hypoparathyroidism]] (failure of the [[parathyroid gland]]s leading to low calcium levels), [[infertility]], and [[recurrent miscarriage]].<ref name=Ala/> |
* '''Hormones:''' [[hypoparathyroidism]] (failure of the [[parathyroid gland]]s leading to low calcium levels), [[panhypopituitarism]] (leading to decreased production of hormones from the pituitary gland), [[infertility]], and [[recurrent miscarriage]].<ref name=Ala/><ref name="Roberts 2023">{{cite journal |last1=Roberts |first1=Eve A. |last2=Schilsky |first2=Michael L. |title=Current and Emerging Issues in Wilson's Disease |journal=New England Journal of Medicine |date=7 September 2023 |volume=389 |issue=10 |pages=922–938 |doi=10.1056/NEJMra1903585|pmid=37672695 |s2cid=261581755 }}</ref> |
||
*'''Musculoskeletal:''' Arthritis and thinning of the bones ([[osteopenia]] or [[osteoporosis]]).<ref name="Roberts2003" /> |
|||
<gallery widths="200" heights="200"> |
<gallery widths="200" heights="200"> |
||
File:Sunflower cataract.jpg|Sunflower cataract and thick KF ring of a 40-year-old male with Wilson's disease and decompensated |
File:Sunflower cataract.jpg|Sunflower cataract and thick KF ring of a 40-year-old male with Wilson's disease and decompensated [[chronic liver disease]] |
||
File:KF ring 1.jpg|Diffuse illumination of cornea |
File:KF ring 1.jpg|Diffuse illumination of cornea |
||
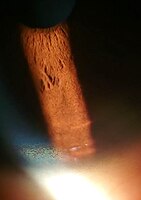
File:KF ring 2.jpg|Copper deposition on corneal Descemet's membrane |
File:KF ring 2.jpg|Copper deposition on corneal Descemet's membrane |
||
| Line 65: | Line 69: | ||
{{main|ATP7B}} |
{{main|ATP7B}} |
||
The Wilson's disease gene (''ATP7B'') is on [[chromosome 13]] (13q14.3) and is expressed primarily in the liver, [[kidney]], and [[placenta]]. The gene codes for a [[P-ATPase|P-type]] (cation transport enzyme) [[ATPase]] that transports copper into [[bile]] and incorporates it into [[ceruloplasmin]].<ref name=Ala/> |
The Wilson's disease gene (''ATP7B'') is on [[chromosome 13]] (13q14.3) and is expressed primarily in the liver, [[kidney]], and [[placenta]]. The gene codes for a [[P-ATPase|P-type]] (cation transport enzyme) [[ATPase]] that transports copper into [[bile]] and incorporates it into [[ceruloplasmin]].<ref name=Ala/> Most people who have Wilson's disease – 60% – are [[homozygous]] for ''ATP7B'' mutations (two abnormal copies), and 30% of them have only one abnormal copy. In about 10% of cases, people with Wilson's disease have no detectable mutations.<ref name=Merle2007/> |
||
Although 300 mutations of ''ATP7B'' have been described, |
Although 300 possible mutations of ''ATP7B'' have been described, a very small number of those cause most cases of Wilson's disease; which mutation an individual will have tends to be specific to the population they are part of. For instance, in Western populations, the H1069Q mutation (replacement of a [[histidine]] by a [[glutamine]] at position 1069 in the protein) is present in 37%–63% of cases, while in China this mutation is very uncommon; R778L ([[arginine]] to [[leucine]] at 778) is found more often there. Relatively little is known about the relative impact of the various mutations, although the H1069Q mutation seems to predict later onset and predominantly neurological problems, according to some studies.<ref name=Ala/><ref name=deBie2007>{{cite journal |vauthors=de Bie P, Muller P, Wijmenga C, Klomp LW |title=Molecular pathogenesis of Wilson and Menkes disease: correlation of mutations with molecular defects and disease phenotypes |journal=J. Med. Genet. |volume=44 |issue=11 |pages=673–88 |date=November 2007 |pmid=17717039 |pmc=2752173 |doi=10.1136/jmg.2007.052746 }}</ref> A comprehensive clinically annotated resource, WilsonGen, provides a clinical classification for the variants as per the recent ACMG & AMP guidelines.<ref>{{Cite journal|last1=Kumar|first1=Mukesh|last2=Gaharwar|first2=Utkarsh|last3=Paul|first3=Sangita|last4=Poojary|first4=Mukta|last5=Pandhare|first5=Kavita|last6=Scaria|first6=Vinod|last7=Bk|first7=Binukumar|date=2020-06-03|title=WilsonGen a comprehensive clinically annotated genomic variant resource for Wilson's Disease|journal=Scientific Reports|language=en|volume=10|issue=1|page=9037|doi=10.1038/s41598-020-66099-2|pmid=32493955|pmc=7270127|bibcode=2020NatSR..10.9037K|issn=2045-2322}}</ref> |
||
A normal variation in the ''[[PRNP]]'' gene can modify the course of the disease by delaying the age of onset and affecting the type of symptoms that develop. This gene produces [[prion protein]], which is active in the brain and other tissues and also appears to be involved in transporting copper.<ref>{{cite journal |vauthors=Grubenbecher S, Stüve O, Hefter H, Korth C |title=Prion protein gene codon 129 modulates clinical course of neurological Wilson disease |journal=NeuroReport |volume=17 |issue=5 |pages=549–52 |year=2006 |pmid=16543824 |doi=10.1097/01.wnr.0000209006.48105.90|s2cid=37186426 }}</ref> A role for the ''[[Apolipoprotein E|ApoE]]'' gene was initially suspected but could not be confirmed.<ref name=deBie2007/> |
A normal variation in the ''[[PRNP]]'' gene can modify the course of the disease by delaying the age of onset and affecting the type of symptoms that develop. This gene produces [[prion protein]], which is active in the brain and other tissues and also appears to be involved in transporting copper.<ref>{{cite journal |vauthors=Grubenbecher S, Stüve O, Hefter H, Korth C |title=Prion protein gene codon 129 modulates clinical course of neurological Wilson disease |journal=NeuroReport |volume=17 |issue=5 |pages=549–52 |year=2006 |pmid=16543824 |doi=10.1097/01.wnr.0000209006.48105.90|s2cid=37186426 }}</ref> A role for the ''[[Apolipoprotein E|ApoE]]'' gene was initially suspected, but could not be confirmed.<ref name=deBie2007/> |
||
The condition is inherited in an autosomal recessive pattern. |
The condition is inherited in an autosomal recessive pattern. To inherit it, both of the parents of an individual must carry an affected gene. Most people with Wilson's disease have no family history of the condition.<ref name=deBie2007/> People with only one abnormal gene are called carriers (heterozygotes) and may have mild, but medically insignificant, abnormalities of copper metabolism.<ref name=Roberts2003/> |
||
There are several hereditary diseases that cause copper overload in the liver; Wilson's disease is the most common of them. All can cause [[cirrhosis]] at a young age. The other copper overload diseases are [[Indian childhood cirrhosis]] (ICC), endemic Tyrolean infantile cirrhosis, and idiopathic copper toxicosis. These three, unlike Wilson's disease, are not related to ''ATP7B'' mutations; for example, ICC has been linked to mutations in the ''[[Keratin 8|KRT8]]'' and the ''[[Keratin 18|KRT18]]'' genes.<ref name=deBie2007/> |
|||
==Pathophysiology== |
==Pathophysiology== |
||
[[Image:Copper metabolism.png|thumb|Normal absorption and distribution of copper |
[[Image:Copper metabolism.png|thumb|Normal absorption and distribution of copper: Cu = copper, CP = [[ceruloplasmin]], green = ATP7B carrying copper]] |
||
Copper is needed by the body for a [[Copper#Biological role|number of functions]], predominantly as a [[Cofactor (biochemistry)|cofactor]] for a number of enzymes such as ceruloplasmin, [[cytochrome c oxidase]], [[dopamine beta hydroxylase|dopamine β-hydroxylase]], [[superoxide dismutase]] and [[tyrosinase]].<ref name=deBie2007/> |
Copper is needed by the body for a [[Copper#Biological role|number of functions]], predominantly as a [[Cofactor (biochemistry)|cofactor]] for a number of enzymes such as ceruloplasmin, [[cytochrome c oxidase]], [[dopamine beta hydroxylase|dopamine β-hydroxylase]], [[superoxide dismutase]], and [[tyrosinase]].<ref name=deBie2007/> |
||
Copper enters the body through the [[Human gastrointestinal tract|digestive tract]]. A transporter protein on the [[enterocyte|cells of the small bowel]], [[SLC31A1|copper membrane transporter 1]] (Ctr1; SLC31A1), carries copper inside the cells, where some is bound to [[metallothionein]] and part is carried by [[ATOX1]] to an organelle known as the [[Golgi apparatus|trans-Golgi network]]. Here, in response to rising concentrations of copper, an enzyme called [[ATP7A]] (Menkes' protein) releases copper into the [[portal vein]] to the liver. Liver cells also carry the CMT1 protein, and metallothionein and ATOX1 bind it inside the cell, but here |
Copper enters the body through the [[Human gastrointestinal tract|digestive tract]]. A transporter protein on the [[enterocyte|cells of the small bowel]], [[SLC31A1|copper membrane transporter 1]] (Ctr1; SLC31A1), carries copper inside the cells, where some is bound to [[metallothionein]] and part is carried by [[ATOX1]] to an organelle known as the [[Golgi apparatus|trans-Golgi network]]. Here, in response to rising concentrations of copper, an enzyme called [[ATP7A]] (Menkes' protein) releases copper into the [[portal vein]] to the liver. Liver cells also carry the CMT1 protein, and metallothionein and ATOX1 bind it inside the cell, but here, ATP7B links copper to ceruloplasmin and releases it into the bloodstream, as well as removing excess copper by secreting it into bile. Both functions of ATP7B are impaired in Wilson's disease. Copper accumulates in the liver tissue; ceruloplasmin is still secreted, but in a form that lacks copper (termed apo-ceruloplasmin) and is rapidly degraded in the bloodstream.<ref name=deBie2007/> |
||
When the amount of copper in the liver overwhelms the proteins that normally bind it, it causes oxidative damage through a process known as [[Fenton's reagent|Fenton chemistry]]; this damage eventually leads to [[hepatitis|chronic active hepatitis]], [[fibrosis]] (deposition of connective tissue) and [[cirrhosis]]. The liver also releases copper into the bloodstream that is not bound to ceruloplasmin. This free copper precipitates throughout the body but particularly in the kidneys, eyes and brain. In the brain, most copper is deposited in the [[basal ganglia]], particularly in the [[putamen]] and [[globus pallidus]] (together called the |
When the amount of copper in the liver overwhelms the proteins that normally bind it, it causes oxidative damage to the liver through a process known as [[Fenton's reagent|Fenton chemistry]]; this damage eventually leads to [[hepatitis|chronic active hepatitis]], [[fibrosis]] (deposition of connective tissue), and [[cirrhosis]]. The liver also releases copper into the bloodstream that is not bound to ceruloplasmin. This free copper precipitates throughout the body, but particularly in the kidneys, eyes, and brain. In the brain, most copper is deposited in the [[basal ganglia]], particularly in the [[putamen]] and [[globus pallidus]] (together called the [[lenticular nucleus]]); these areas normally participate in the coordination of movement and play a significant role in neurocognitive processes such as the processing of stimuli and mood regulation. Damage to these areas, again by Fenton chemistry, produces the neuropsychiatric symptoms seen in Wilson's disease.<ref name=deBie2007/> |
||
Why Wilson's disease causes hemolysis is unclear, but various lines of evidence suggest that a high level of free (nonceruloplasmin-bound) copper may be directly affecting the oxidation of [[hemoglobin]], or inhibiting the energy-supplying enzymes in [[red blood cell]]s, or causing direct damage to [[cell membrane]]s.<ref>{{cite book |last=Lee |first=GR |veditors=Lee GR, Foerster J, Lukens J |title=Wintrobe's clinical hematology |edition=10th |volume=1 |year=1999 |publisher=Williams & Wilkins |isbn=978-0-683-18242-2 |pages=[https://archive.org/details/wintrobesclinica0000unse/page/1298 1298] |chapter=Chapter 48: acquired hemolytic anaemias resulting from direct effects of infectious, chemical or physical agents |display-editors=etal |chapter-url=https://archive.org/details/wintrobesclinica0000unse/page/1298 }}</ref> |
|||
==Diagnosis== |
==Diagnosis== |
||
[[Image:Basal ganglia and related structures (2).svg|thumb|Location of the basal ganglia, the part of the brain affected by Wilson's disease]] |
[[Image:Basal ganglia and related structures (2).svg|thumb|Location of the basal ganglia, the part of the brain affected by Wilson's disease]] |
||
Wilson's disease may be suspected on the basis of any of the symptoms mentioned above, or when a close relative has been found to have Wilson's. Most have slightly abnormal [[liver function tests]] such as |
Wilson's disease may be suspected on the basis of any of the symptoms mentioned above, or when a close relative has been found to have Wilson's. Most have slightly abnormal [[liver function tests]] such as raised [[aspartate transaminase]], [[alanine transaminase]], and [[bilirubin]] levels. If the liver damage is significant, [[albumin]] may be decreased due to an inability of damaged liver cells to produce this protein; likewise, the [[prothrombin time]] (a test of [[coagulation]]) may be prolonged as the liver is unable to produce proteins known as clotting factors.<ref name=Ala/> [[Alkaline phosphatase]] levels are relatively low in those with Wilson's-related acute liver failure.<ref name="pmid3758940">{{cite journal |vauthors = Shaver WA, Bhatt H, Combes B |title=Low serum alkaline phosphatase activity in Wilson's disease |journal=Hepatology |volume=6 |issue=5 |pages=859–63 |year=1986 |pmid=3758940 |doi=10.1002/hep.1840060509|s2cid=24055787 |doi-access=free }}</ref> If neurological symptoms are seen, [[magnetic resonance imaging]] <!-- (MRI) --> of the brain is usually performed; this shows [[hyperintensity|hyperintensities]] in the part of the brain called the [[basal ganglia]] in the [[spin-spin relaxation time|T2]] setting.<ref name="Roberts2003">{{cite journal |last1=Roberts |first1=Eve A. |last2=Schilsky |first2=Michael L. |title=A practice guideline on Wilson disease |journal=Hepatology |year=2003 |volume=37 |issue=6 |pages=1475–92 |pmid=12774027 |doi=10.1053/jhep.2003.50252 |s2cid=263620 |doi-access=free }}</ref> MRI may also demonstrate the characteristic [[Face of the Giant Panda Sign|"face of the giant panda"]] pattern.<ref name=Panda>{{cite journal |vauthors=Das SK, Ray K |title=Wilson's disease: an update |journal=Nat Clin Pract Neurol |volume=2 |issue=9 |pages=482–93 |date=September 2006 |pmid=16932613 |doi=10.1038/ncpneuro0291 |s2cid=205340375 }}</ref> |
||
No totally reliable test for Wilson's disease is known, but levels of ceruloplasmin and copper in the blood, as well of the amount of copper excreted in urine during a 24-hour period, are together used to form an impression of the amount of copper in the body. The most accurate test is a [[liver biopsy]].<ref name=Ala/> |
|||
===Ceruloplasmin=== |
===Ceruloplasmin=== |
||
[[Image:PBB Protein CP image.jpg|thumb|Ceruloplasmin]] |
[[Image:PBB Protein CP image.jpg|thumb|Ceruloplasmin]] |
||
Levels of |
Levels of ceruloplasmin are abnormally low (<0.2 g/L) in 80–95% of cases.<ref name=Ala/> It can be present at normal levels, though, in people with ongoing [[inflammation]], as it is an [[acute phase protein]]. Low ceruloplasmin is also found in [[Menkes disease]] and [[aceruloplasminemia]], which are related to, but much rarer than Wilson's disease.<ref name=Ala/><ref name=Roberts2003/> The combination of neurological symptoms, eye signs, and a low ceruloplasmin level is considered sufficient for the diagnosis of Wilson's disease. In many cases, however, further tests are needed.<ref name=Roberts2003/> |
||
The combination of neurological symptoms, Kayser–Fleischer rings and a low ceruloplasmin level is considered sufficient for the diagnosis of Wilson's disease. In many cases, however, further tests are needed.<ref name=Roberts/> |
|||
===Serum and urine copper=== |
===Serum and urine copper=== |
||
Serum copper is low, which may seem paradoxical given that Wilson's disease is a disease of copper excess. However, 95% of plasma copper is carried by ceruloplasmin which is often low in Wilson's disease. Urine copper is elevated in Wilson's disease and is collected for 24 hours in a bottle with a copper-free liner. Levels above 100 μg/24h (1.6 μmol/24h) confirm Wilson's disease, and levels above 40 μg/24h (0.6 μmol/24h) are strongly indicative.<ref name=Ala/> High urine copper levels are not unique to Wilson's disease; they are sometimes observed in [[autoimmune hepatitis]] and in [[cholestasis]] (any disease obstructing the flow of bile from the liver to the small bowel).<ref name= |
Serum copper is low, which may seem paradoxical given that Wilson's disease is a disease of copper excess. However, 95% of plasma copper is carried by ceruloplasmin, which is often low in Wilson's disease. Urine copper is elevated in Wilson's disease and is collected for 24 hours in a bottle with a copper-free liner. Levels above 100 μg/24h (1.6 μmol/24h) confirm Wilson's disease, and levels above 40 μg/24h (0.6 μmol/24h) are strongly indicative.<ref name=Ala/> High urine copper levels are not unique to Wilson's disease; they are sometimes observed in [[autoimmune hepatitis]] and in [[cholestasis]] (any disease obstructing the flow of bile from the liver to the small bowel).<ref name=Roberts2003/> |
||
| ⚫ | In children, the following [[penicillamine]] test may be used: a 500 mg oral dose of penicillamine is administered, and all urine collected for 24 hours. If the entire day's urine contains more than 1600 μg (25 μmol) of copper, it is a reliable indicator of Wilson's disease. This test has not been validated in adults.<ref name=Roberts2003/> |
||
=== Slit-lamp examination === |
|||
| ⚫ | In children, the [[penicillamine]] test may be used |
||
The eyes of the patient are examined using a [[slit lamp]] to look for [[Kayser–Fleischer ring]]s, which are strongly associated with Wilson's disease and are caused by copper deposition on the inner [[cornea]] in [[Descemet's membrane]].<ref name="Pandey"/> |
|||
===Liver biopsy=== |
===Liver biopsy=== |
||
Once other investigations have indicated Wilson's disease, the ideal test is the removal of a small amount of liver tissue through a |
Once other investigations have indicated Wilson's disease, the ideal test is the removal of a small amount of liver tissue through a liver biopsy. This is assessed microscopically for the degree of [[steatosis]] and cirrhosis, and [[histochemistry]] and quantification of copper are used to measure the severity of the copper accumulation. A level of 250 [[microgram|μg]] of copper per gram of dried liver tissue confirms Wilson's disease. Occasionally, lower levels of copper are found; in that case, the combination of the biopsy findings with all other tests could still lead to a formal diagnosis of Wilson's.<ref name=Ala/> |
||
In the earlier stages of the disease, the biopsy typically shows |
In the earlier stages of the disease, the biopsy typically shows steatosis (deposition of fatty material), increased [[glycogen]] in the [[Cell nucleus|nucleus]], and areas of [[necrosis]] (cell death). In more advanced disease, the changes observed are quite similar to those seen in autoimmune hepatitis, such as infiltration by [[inflammation|inflammatory]] cells, piecemeal necrosis, and fibrosis (scar tissue). In advanced disease, finally, cirrhosis is the main finding. In acute liver failure, degeneration of the liver cells and collapse of the liver tissue architecture is seen, typically on a background of cirrhotic changes. Histochemical methods for detecting copper are inconsistent and unreliable, and taken alone are regarded as insufficient to establish a diagnosis.<ref name=Roberts2003/> |
||
===Genetic testing=== |
===Genetic testing=== |
||
Mutation analysis of the ''ATP7B'' gene, as well as other genes linked to copper accumulation in the liver, may be performed. Once a mutation is confirmed, |
Mutation analysis of the ''ATP7B'' gene, as well as other genes linked to copper accumulation in the liver, may be performed. Once a mutation is confirmed, family members can be screened for the disease as part of [[clinical genetics]] family counseling.<ref name=Ala/> Regional distributions of genes associated with Wilson's disease are important to follow, as this can help clinicians design appropriate screening strategies. Since mutations of the ''ATP7B'' gene vary between populations, research and genetic testing done in countries such as the USA or United Kingdom can pose problems, as they tend to have more mixed populations.<ref>{{Cite journal|title = Regional distribution of mutations of the ATP7B gene in patients with Wilson disease: impact on genetic testing|journal = Human Genetics|date = 2006-06-22|issn = 0340-6717|pages = 151–159|volume = 120|issue = 2|doi = 10.1007/s00439-006-0202-5|language = en|first = Peter|last = Ferenci|pmid=16791614|s2cid = 10124665}}</ref> |
||
==Treatment== |
==Treatment== |
||
===Diet=== |
===Diet=== |
||
In general, a diet low in copper-containing foods is recommended |
In general, a diet low in copper-containing foods is recommended. High-copper foods avoided in Wilson's disease include [[mushroom]]s, [[nut (fruit)|nuts]], [[chocolate]], dried [[fruit]], liver, sesame seeds, sesame oil, and [[shellfish]].<ref name=Ala/> |
||
===Medication=== |
===Medication=== |
||
Medical treatments are available for Wilson's disease. Some increase the removal of copper from the body, while others prevent the absorption of copper from the diet. |
Medical treatments are available for Wilson's disease. Some increase the removal of copper from the body, while others prevent the absorption of copper from the diet. |
||
Generally, |
Generally, penicillamine is the first treatment used. This binds to copper (by [[chelation]]) and leads to excretion of copper in the urine. Hence, monitoring of the amount of copper in the urine can be done to ensure a sufficiently high dose is taken. Penicillamine is not without problems; about 20% experience a side effect or complication of penicillamine treatment, such as drug-induced [[systemic lupus erythematosus|lupus]] (causing joint pains and a skin rash) or [[myasthenia gravis|myasthenia]] (a nerve condition leading to muscle weakness). In those who presented with neurological symptoms, almost half experience a paradoxical worsening in their symptoms. While this phenomenon is observed in other treatments for Wilson's, it is usually taken as an indication for discontinuing penicillamine and commencing second-line treatment.<ref name=Ala/><ref name=Roberts2003/> Those intolerant to penicillamine may instead be commenced on [[trientine hydrochloride]], which also has chelating properties. Some recommend trientine as first-line treatment, but experience with penicillamine is more extensive.<ref name=Roberts2003/> A further agent with known activity in Wilson's disease, under clinical investigation by [[Wilson Therapeutics]], is [[bis-choline tetrathiomolybdate|tetrathiomolybdate]]. It is regarded as experimental,<ref name=Roberts2003/> though some studies have shown a beneficial effect.<ref name=Ala/> |
||
Once all results have returned to normal, [[zinc]] (usually in the form of a [[zinc acetate]] prescription called Galzin) may be used instead of chelators to maintain stable copper levels in the body. Zinc stimulates [[metallothionein]], a protein in gut cells that binds copper and prevents |
Once all results have returned to normal, [[zinc]] (usually in the form of a [[zinc acetate]] prescription called Galzin) may be used instead of chelators to maintain stable copper levels in the body. Zinc stimulates [[metallothionein]], a protein in gut cells that binds copper and prevents its absorption and transport to the liver. Zinc therapy is continued unless symptoms recur or if the urinary excretion of copper increases.<ref name=Roberts2003/> |
||
In rare cases where none of the oral treatments |
In rare cases where none of the oral treatments is effective, especially with severe neurological disease, [[dimercaprol]] (British anti-Lewisite) is occasionally necessary. This treatment is injected [[Intramuscular injection|intramuscularly]] (into a muscle) every few weeks and has unpleasant side effects such as pain.<ref name=Walshe1996>{{cite journal |author=Walshe JM |title=Treatment of Wilson's disease: the historical background |journal=QJM |volume=89 |issue=7 |pages=553–55 |date=July 1996 |pmid=8759497 |doi=10.1093/qjmed/89.7.553|doi-access=free }}</ref> |
||
People who are [[asymptomatic]] (for instance, those diagnosed through family screening or only as a result of abnormal test results) are generally treated, as the copper accumulation may cause long-term damage in the future. |
People who are [[asymptomatic]] (for instance, those diagnosed through family screening or only as a result of abnormal test results) are generally treated, as the copper accumulation may cause long-term damage in the future. Whether these people are best treated with penicillamine or zinc acetate is unclear.<ref name=Roberts2003/> |
||
===Physical and occupational therapies=== |
===Physical and occupational therapies=== |
||
[[Physiotherapy]] and occupational therapy are beneficial for patients with the |
[[Physiotherapy]] and occupational therapy are beneficial for patients with the neurological form of the disease. The copper-chelating treatment may take up to six months to start working, and these therapies can assist in coping with [[ataxia]], [[dystonia]], and tremors, as well as preventing the development of [[contracture]]s that can result from dystonia.<ref name=Brewer2005>{{cite journal |vauthors=Brewer GJ, Askari FK | title=Wilson's disease: clinical management and therapy | journal=Journal of Hepatology | year=2005 | volume=42 | issue=Suppl 1 | pages=13–21 | pmid=15777568 | doi=10.1016/j.jhep.2004.11.013| doi-access=free }}</ref> |
||
===Transplantation=== |
===Transplantation=== |
||
[[Liver transplantation]] is an effective cure for Wilson's disease but is used only in particular scenarios because of the risks and complications associated with the procedure. It is used mainly in people with [[fulminant]] liver failure who fail to respond to medical treatment or in those with advanced chronic liver disease. Liver transplantation is avoided in severe neuropsychiatric |
[[Liver transplantation]] is an effective cure for Wilson's disease, but is used only in particular scenarios because of the risks and complications associated with the procedure. It is used mainly in people with [[fulminant]] liver failure who fail to respond to medical treatment or in those with advanced chronic liver disease. Liver transplantation is avoided in severe neuropsychiatric illnesses, in which its benefit has not been demonstrated.<ref name=Ala/><ref name=Roberts2003/> |
||
==Prognosis== |
==Prognosis== |
||
Left untreated, Wilson's disease tends to become progressively worse and is eventually fatal. With early detection and treatment, most of those affected can live relatively normal lives. Liver and |
Left untreated, Wilson's disease tends to become progressively worse and is eventually fatal. Serious complications include liver cirrhosis, acute kidney failure, and psychosis. [[Liver cancer]] and [[cholangiocarcinoma]] may occur, but at a lower incidence than other chronic liver diseases, and the risk is greatly reduced with treatment.<ref name="Roberts 2023" /> With early detection and treatment, most of those affected can live relatively normal lives and have a life expectancy close to that of the general population.<ref name="Roberts 2023" /> Liver and neurological damage that occurs prior to treatment may improve, but it is often permanent.<ref>{{Cite web|url=https://www.niddk.nih.gov/health-information/liver-disease/wilson-disease/definition-facts|title=Definition and Facts {{!}} NIDDK|website=National Institute of Diabetes and Digestive and Kidney Diseases|language=en-US|access-date=2019-02-01}}</ref> Fertility is usually normal and pregnancy complications are not increased in those with Wilson's disease that is treated.<ref name="Roberts 2023" /> |
||
==History== |
==History== |
||
The disease bears the name of |
The disease bears the name of [[United Kingdom|British]] physician [[Samuel Alexander Kinnier Wilson]] (1878–1937), a [[Neurology|neurologist]] who described the condition, including the pathological changes in the brain and liver, in 1912.<ref name=Wilson1912>{{cite journal | author=Kinnier Wilson SA | title=Progressive lenticular degeneration: a familial nervous disease associated with cirrhosis of the liver | journal=Brain | year=1912 | volume=34 | issue=1 | pages=295–507 | doi=10.1093/brain/34.4.295 | url=https://zenodo.org/record/1431640 }}</ref> Wilson's work had been predated by, and drew on, reports from German neurologist [[Karl Friedrich Otto Westphal|Karl Westphal]] (in 1883), who termed it "pseudo-sclerosis"; by the British neurologist [[William Richard Gowers|William Gowers]] (in 1888);<ref name=Robertson/> by the Finnish neuropathologist Ernst Alexander Homén (in 1889–1892), who noted the hereditary nature of the disease;<ref name=Homén1892>{{cite journal | author=Homén EA |title=Eine eigenthümliche bei drei Geschwistern auftretende typische Krankheit unter der Form einer progressiven Dementia in Verbindung mit ausgedehnten Gefässveränderungen (wohl Lues hereditaria tarda) |journal=Archiv für Psychiatrie und Nervenkrankheiten |volume=24|pages=1–38 |date=1892 }}</ref> and by [[Adolph Strümpell]] (in 1898), who noted hepatic cirrhosis.<ref name=Robertson>{{cite journal |author=Robertson WM |title=Wilson's disease |journal=Arch. Neurol. |volume=57 |issue=2 |pages=276–77 |date=February 2000 |pmid=10681092 |doi=10.1001/archneur.57.2.276 }}</ref> Neuropathologist John Nathaniel Cumings made the link with copper accumulation in both the liver and the brain in 1948.<ref name="pmid18124738">{{cite journal |author=Cumings JN |title=The copper and iron content of brain and liver in the normal and in hepato-lenticular degeneration |journal=Brain |volume=71 |issue=Dec |pages=410–15 |year=1948 |pmid=18124738 |doi=10.1093/brain/71.4.410 }}</ref> The occurrence of hemolysis was noted in 1967.<ref>{{cite journal |doi=10.1056/NEJM196702232760804 |vauthors=McIntyre N, Clink HM, Levi AJ, Cumings JN, Sherlock S |title=Hemolytic anemia in Wilson's disease |journal=N. Engl. J. Med. |volume=276 |issue=8 |pages=439–44 |date=February 1967 |pmid=6018274}}</ref> |
||
In 1951, Cumings, and |
In 1951, Cumings (in England), and New Zealand neurologist [[Derek Denny-Brown (doctor)|Derek Denny-Brown]] (working in the United States), simultaneously reported the first effective treatment, using the metal chelator [[dimercaprol|British anti-Lewisite]].<ref>{{cite journal |author=Cumings JN |title=The effects of B.A.L. in hepatolenticular degeneration |journal=Brain |volume=74 |issue=1 |pages=10–22 |date=March 1951 |pmid=14830662 |doi=10.1093/brain/74.1.10}}</ref><ref>{{cite journal |doi=10.1056/NEJM195112132452401 |vauthors=Denny-Brown D, Porter H |title=The effect of BAL (2,3-dimercaptopropanol) on hepatolenticular degeneration (Wilson's disease) |journal=N. Engl. J. Med. |volume=245 |issue=24 |pages=917–25 |date=December 1951 |pmid=14882450}}</ref> This treatment had to be injected, but was one of the first therapies available in the field of neurology, a field that classically was able to observe and diagnose, but had few treatments to offer.<ref name=Robertson/><ref>{{cite journal |vauthors=Vilensky JA, Robertson WM, Gilman S |title=Denny-Brown, Wilson's disease, and BAL (British antilewisite [2,3-dimercaptopropanol]) |journal=Neurology |volume=59 |issue=6 |pages=914–16 |date=September 2002 |pmid=12297577 |doi=10.1212/wnl.59.6.914}}</ref> The first oral chelation agent effective in Wilson's disease, [[penicillamine]], was discovered in 1956 by British neurologist John Walshe.<ref name=Walshe1956>{{cite journal |author=Walshe JM |title=Wilson's disease; new oral therapy |journal=Lancet |volume= 270|issue=6906 |pages=25–26 |date=January 1956 |pmid=13279157 |doi=10.1016/S0140-6736(56)91859-1}}</ref> In 1982, Walshe also introduced trientine,<ref>{{cite journal |author=Walshe JM |title=Treatment of Wilson's disease with trientine (triethylene tetramine) dihydrochloride |journal=Lancet |volume=1 |issue=8273 |pages=643–47 |date=March 1982 |pmid=6121964 |doi=10.1016/S0140-6736(82)92201-2|s2cid=205999334 }}</ref> and was the first to develop tetra-thiomolybdate for clinical use.<ref>{{cite journal |vauthors=Harper PL, Walshe JM |title=Reversible pancytopenia secondary to treatment with tetrathiomolybdate |journal=Br. J. Haematol. |volume=64 |issue=4 |pages=851–53 |date=December 1986 |pmid=3801328 |doi=10.1111/j.1365-2141.1986.tb02250.x|s2cid=11546705 |doi-access=free }}</ref> Zinc acetate therapy initially made its appearance in the Netherlands, where physicians Schouwink and Hoogenraad used it in 1961 and in the 1970s, respectively, and was further developed later by Brewer and colleagues at the [[University of Michigan]].<ref name=Walshe1996/><ref>{{cite journal |author=Brewer GJ |title=Recognition, diagnosis, and management of Wilson's disease |journal=Proc. Soc. Exp. Biol. Med. |volume=223 |issue=1 |pages=39–46 |date=January 2000 |pmid=10632959 |url=http://www.ebmonline.org/cgi/content/full/223/1/39 |doi=10.1046/j.1525-1373.2000.22305.x |url-status=dead |archive-url=https://web.archive.org/web/20080409223216/http://www.ebmonline.org/cgi/content/full/223/1/39 |archive-date=2008-04-09 |access-date=2008-05-20 }}</ref> |
||
The genetic basis of Wilson's disease, and its link to ''ATP7B'' mutations, was elucidated by several research groups in the 1980s and 1990s.<ref name="pmid8298639">{{cite journal |vauthors=Bull PC, Thomas GR, Rommens JM, Forbes JR, Cox DW |title=The Wilson disease gene is a putative copper transporting P-type ATPase similar to the Menkes gene |journal=Nat. Genet. |volume=5 |issue=4 |pages=327–37 |year=1993 |pmid=8298639 |doi=10.1038/ng1293-327|s2cid=1236890 }}</ref><ref name="pmid8298641">{{cite journal |vauthors=Tanzi RE, Petrukhin K, Chernov I, etal |title=The Wilson disease gene is a copper transporting ATPase with homology to the Menkes disease gene |journal=Nat. Genet. |volume=5 |issue=4 |pages=344–50 |year=1993 |pmid=8298641 |doi=10.1038/ng1293-344|s2cid=610188 }}</ref> |
The genetic basis of Wilson's disease, and its link to ''ATP7B'' mutations, was elucidated by several research groups in the 1980s and 1990s.<ref name="pmid8298639">{{cite journal |vauthors=Bull PC, Thomas GR, Rommens JM, Forbes JR, Cox DW |title=The Wilson disease gene is a putative copper transporting P-type ATPase similar to the Menkes gene |journal=Nat. Genet. |volume=5 |issue=4 |pages=327–37 |year=1993 |pmid=8298639 |doi=10.1038/ng1293-327|s2cid=1236890 }}</ref><ref name="pmid8298641">{{cite journal |vauthors=Tanzi RE, Petrukhin K, Chernov I, etal |title=The Wilson disease gene is a copper transporting ATPase with homology to the Menkes disease gene |journal=Nat. Genet. |volume=5 |issue=4 |pages=344–50 |year=1993 |pmid=8298641 |doi=10.1038/ng1293-344|s2cid=610188 }}</ref> |
||
==In other animals== |
==In other animals== |
||
Hereditary copper accumulation has been described in [[Bedlington Terrier]]s,<ref>{{cite journal |vauthors=Sternlieb I, Twedt DC, Johnson GF, etal |title=Inherited copper toxicity of the liver in Bedlington terriers |journal=Proc. R. Soc. Med. |volume=70 |
Hereditary copper accumulation has been described in [[Bedlington Terrier]]s,<ref>{{cite journal |vauthors=Sternlieb I, Twedt DC, Johnson GF, etal |title=Inherited copper toxicity of the liver in Bedlington terriers |journal=Proc. R. Soc. Med. |volume=70 |issue= Suppl 3|pages=8–9 |year=1977 |pmid=122681 |pmc=1543595}}</ref> where it generally only affects the liver. In Bedlington Terriers it is due to mutations in the ''[[COMMD1]]'' (or ''MURR1'') gene.<ref>{{cite journal |vauthors=van De Sluis B, Rothuizen J, Pearson PL, van Oost BA, Wijmenga C |title=Identification of a new copper metabolism gene by positional cloning in a purebred dog population |journal=Hum. Mol. Genet. |volume=11 |issue=2 |pages=165–73 |year=2002 |pmid=11809725 |doi=10.1093/hmg/11.2.165 |doi-access=free }}</ref> The discovery of these mutations in the dogs led researchers to examine the corresponding human genes, but ''COMMD1'' mutations could not be detected in humans with non-Wilsonian copper accumulation states (such as [[Indian childhood cirrhosis]]).<ref>{{cite journal |vauthors=Müller T, van de Sluis B, Zhernakova A, etal |title=The canine copper toxicosis gene MURR1 does not cause non-Wilsonian hepatic copper toxicosis |journal=J. Hepatol. |volume=38 |issue=2 |pages=164–68 |year=2003 |pmid=12547404 |doi=10.1016/S0168-8278(02)00356-2}}</ref> |
||
==See also== |
==See also== |
||
* [[Copper in health]] |
* [[Copper in health]] |
||
* [[Menkes syndrome]] |
|||
==References== |
==References== |
||
| Line 156: | Line 160: | ||
==External links== |
==External links== |
||
{{Commons category|Wilson's disease}} |
{{Commons category|Wilson's disease}} |
||
*{{Curlie|Health/Conditions_and_Diseases/Nutritional_and_Metabolic_Disorders/Vitamins_and_Minerals/Wilson's_Disease/}} |
|||
* {{NLM|wilsondisease|Wilson disease}} |
* {{NLM|wilsondisease|Wilson disease}} |
||
{{Medical condition classification and resources |
{{Medical condition classification and resources |
||
Latest revision as of 18:09, 2 December 2024
| Wilson's disease | |
|---|---|
| Other names | Wilson disease, hepatolenticular degeneration |
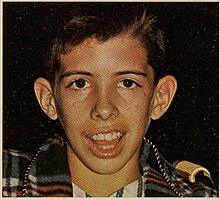 | |
| Boy with Wilson's disease | |
| Specialty | Gastroenterology |
| Symptoms | Swelling of the legs, yellowish skin, personality changes[1] |
| Usual onset | Age 5 to 35[1] |
| Causes | Genetic |
| Differential diagnosis | Chronic liver disease, Parkinson's disease, multiple sclerosis, others[2][3] |
| Treatment | Dietary changes, chelating agents, zinc supplements, liver transplant[1] |
| Frequency | ~1 per 30,000[1] |
Wilson's disease (also called hepatolenticular degeneration) is a genetic disorder characterized by the excess build-up of copper in the body. Symptoms are typically related to the brain and liver. Liver-related symptoms include vomiting, weakness, fluid build-up in the abdomen, swelling of the legs, yellowish skin, and itchiness. Brain-related symptoms include tremors, muscle stiffness, trouble in speaking, personality changes, anxiety, and psychosis.[1]
Wilson's disease is caused by a mutation in the Wilson disease protein (ATP7B) gene. This protein transports excess copper into bile, where it is excreted in waste products. The condition is autosomal recessive; for people to be affected, they must inherit a mutated copy of the gene from both parents. Diagnosis may be difficult and often involves a combination of blood tests, urine tests, and a liver biopsy. Genetic testing may be used to screen family members of those affected.[1]
Wilson's disease is typically treated with dietary changes and medication. Dietary changes involve eating a low-copper diet and not using copper cookware. Medications used include chelating agents, such as trientine and D-penicillamine, and zinc supplements. Complications of Wilson's disease can include liver failure and kidney problems. A liver transplant may be helpful to those for whom other treatments are not effective or if liver failure occurs.[1]
Wilson's disease occurs in about one in 30,000 people.[1] Symptoms usually begin between the ages of 5 and 35 years.[1] It was first described in 1854 by German pathologist Friedrich Theodor von Frerichs and is named after British neurologist Samuel Wilson.[4]
Signs and symptoms
[edit]The main sites of copper accumulation are the liver and brain. Consequently, liver disease and neuropsychiatric symptoms are the main features that lead to diagnosis.[5] People with liver problems tend to come for medical attention earlier (generally as children or teenagers) than those with neurological and psychiatric symptoms, who tend to be in their 20s or older. Some are identified only because relatives have been diagnosed with Wilson's disease; many of these, when tested, turn out to have been experiencing symptoms of the condition but have not received a diagnosis.[6]
Liver disease
[edit]Liver disease may present itself as tiredness, jaundice, increased bleeding tendency or confusion (due to hepatic encephalopathy), and portal hypertension.[7] The last, a condition in which the pressure in the portal vein is markedly increased, leads to esophageal varices (distended veins in the esophagus that may bleed in a life-threatening fashion) as well as enlargement of the spleen (splenomegaly) and accumulation of fluid in the abdominal cavity (ascites). On examination, signs of chronic liver disease such as spider angiomata (small distended blood vessels, usually on the chest) may be observed. Chronic active hepatitis has already caused cirrhosis of the liver in most patients by the time they develop symptoms. While most people with cirrhosis have an increased risk of hepatocellular carcinoma (liver cancer), this risk is relatively low in Wilson's disease.[5]
About 5% of all people are diagnosed only when they develop fulminant acute liver failure, often in the context of hemolytic anemia (anemia due to the destruction of red blood cells). This leads to abnormalities in protein production (identified by deranged coagulation) and metabolism by the liver. The deranged protein metabolism leads to the accumulation of waste products, such as ammonia, in the bloodstream. When these irritate the brain, patients develop hepatic encephalopathy – a serious condition that causes confusion, coma, seizures and, finally, life-threatening swelling of the brain).[5]
Neuropsychiatric symptoms
[edit]
About half of the people with Wilson's disease have neurological or psychiatric symptoms. Most initially have mild cognitive deterioration and clumsiness, as well as changes in behavior. Specific neurological symptoms usually then follow, often in the form of parkinsonism (cogwheel rigidity, bradykinesia, or slowed movements and a lack of balance are the most common parkinsonian features[8]) with or without a typical hand tremor, masked facial expressions, slurred speech, ataxia (lack of coordination), or dystonia (twisting and repetitive movements of part of the body). Seizures and migraine appear to be more common in Wilson's disease.[5] A characteristic tremor described as "wing-beating tremor" is encountered in many people with Wilson's; this is absent at rest but can be provoked by abducting the arms and flexing the elbows toward the midline.[9]
Cognition can also be affected in Wilson's disease, in two non-mutually exclusive categories: frontal lobe disorder (may present as impulsivity, impaired judgement, promiscuity, apathy, and executive dysfunction with poor planning and decision-making) and subcortical dementia (may present as slow thinking, memory loss, and executive dysfunction, without signs of aphasia, apraxia, or agnosia). These cognitive involvements are thought to be related and closely linked to psychiatric manifestations of the disease.[8]
Psychiatric problems due to Wilson's disease may include behavioral changes, depression, anxiety disorders, and psychosis.[5] Psychiatric symptoms are commonly seen in conjunction with neurological symptoms and are rarely manifested on their own. These symptoms are often poorly defined and can sometimes be attributed to other causes. Because of this, diagnosis of Wilson's disease is rarely made when only psychiatric symptoms are present.[8]
Other organ systems
[edit]
Medical conditions have been linked with copper accumulation in Wilson's disease:
- Eyes: Kayser–Fleischer rings (KF rings) may be visible in the cornea of the eyes, either directly or on slit lamp examination, as deposits of copper form a ring around the cornea. This is due to copper deposition in Descemet's membrane. These rings can be either dark brown, golden, or reddish-green, are 1 to 3mm wide, and appear at the corneal limbus. They do not occur in all people with Wilson's disease, and may be seen in people with chronic cholestasis.[10][11] Wilson's disease is also associated with sunflower cataracts exhibited by brown or green pigmentation of the anterior and posterior lens capsule.[12] Neither causes significant visual loss.[5] KF rings occur in approximately 66% of diagnosed cases (more often in those with neurological symptoms rather than with liver problems).[6]
- Kidneys: renal tubular acidosis (Type 2), a disorder of bicarbonate handling by the proximal tubules leads to nephrocalcinosis (calcium accumulation in the kidneys), a weakening of bones (due to calcium and phosphate loss), and occasionally aminoaciduria (loss of essential amino acids needed for protein synthesis).[5]
- Heart: cardiomyopathy (weakness of the heart muscle) is a rare but recognized problem in Wilson's disease; it may lead to heart failure (fluid accumulation due to decreased pump function) and cardiac arrhythmias (episodes of irregular and/or abnormally fast or slow heart beat).[5]
- Hormones: hypoparathyroidism (failure of the parathyroid glands leading to low calcium levels), panhypopituitarism (leading to decreased production of hormones from the pituitary gland), infertility, and recurrent miscarriage.[5][13]
- Musculoskeletal: Arthritis and thinning of the bones (osteopenia or osteoporosis).[14]
-
Sunflower cataract and thick KF ring of a 40-year-old male with Wilson's disease and decompensated chronic liver disease
-
Diffuse illumination of cornea
-
Copper deposition on corneal Descemet's membrane
Genetics
[edit]
The Wilson's disease gene (ATP7B) is on chromosome 13 (13q14.3) and is expressed primarily in the liver, kidney, and placenta. The gene codes for a P-type (cation transport enzyme) ATPase that transports copper into bile and incorporates it into ceruloplasmin.[5] Most people who have Wilson's disease – 60% – are homozygous for ATP7B mutations (two abnormal copies), and 30% of them have only one abnormal copy. In about 10% of cases, people with Wilson's disease have no detectable mutations.[6]
Although 300 possible mutations of ATP7B have been described, a very small number of those cause most cases of Wilson's disease; which mutation an individual will have tends to be specific to the population they are part of. For instance, in Western populations, the H1069Q mutation (replacement of a histidine by a glutamine at position 1069 in the protein) is present in 37%–63% of cases, while in China this mutation is very uncommon; R778L (arginine to leucine at 778) is found more often there. Relatively little is known about the relative impact of the various mutations, although the H1069Q mutation seems to predict later onset and predominantly neurological problems, according to some studies.[5][15] A comprehensive clinically annotated resource, WilsonGen, provides a clinical classification for the variants as per the recent ACMG & AMP guidelines.[16]
A normal variation in the PRNP gene can modify the course of the disease by delaying the age of onset and affecting the type of symptoms that develop. This gene produces prion protein, which is active in the brain and other tissues and also appears to be involved in transporting copper.[17] A role for the ApoE gene was initially suspected, but could not be confirmed.[15]
The condition is inherited in an autosomal recessive pattern. To inherit it, both of the parents of an individual must carry an affected gene. Most people with Wilson's disease have no family history of the condition.[15] People with only one abnormal gene are called carriers (heterozygotes) and may have mild, but medically insignificant, abnormalities of copper metabolism.[14]
There are several hereditary diseases that cause copper overload in the liver; Wilson's disease is the most common of them. All can cause cirrhosis at a young age. The other copper overload diseases are Indian childhood cirrhosis (ICC), endemic Tyrolean infantile cirrhosis, and idiopathic copper toxicosis. These three, unlike Wilson's disease, are not related to ATP7B mutations; for example, ICC has been linked to mutations in the KRT8 and the KRT18 genes.[15]
Pathophysiology
[edit]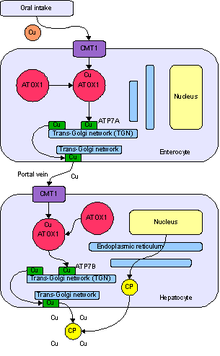
Copper is needed by the body for a number of functions, predominantly as a cofactor for a number of enzymes such as ceruloplasmin, cytochrome c oxidase, dopamine β-hydroxylase, superoxide dismutase, and tyrosinase.[15]
Copper enters the body through the digestive tract. A transporter protein on the cells of the small bowel, copper membrane transporter 1 (Ctr1; SLC31A1), carries copper inside the cells, where some is bound to metallothionein and part is carried by ATOX1 to an organelle known as the trans-Golgi network. Here, in response to rising concentrations of copper, an enzyme called ATP7A (Menkes' protein) releases copper into the portal vein to the liver. Liver cells also carry the CMT1 protein, and metallothionein and ATOX1 bind it inside the cell, but here, ATP7B links copper to ceruloplasmin and releases it into the bloodstream, as well as removing excess copper by secreting it into bile. Both functions of ATP7B are impaired in Wilson's disease. Copper accumulates in the liver tissue; ceruloplasmin is still secreted, but in a form that lacks copper (termed apo-ceruloplasmin) and is rapidly degraded in the bloodstream.[15]
When the amount of copper in the liver overwhelms the proteins that normally bind it, it causes oxidative damage to the liver through a process known as Fenton chemistry; this damage eventually leads to chronic active hepatitis, fibrosis (deposition of connective tissue), and cirrhosis. The liver also releases copper into the bloodstream that is not bound to ceruloplasmin. This free copper precipitates throughout the body, but particularly in the kidneys, eyes, and brain. In the brain, most copper is deposited in the basal ganglia, particularly in the putamen and globus pallidus (together called the lenticular nucleus); these areas normally participate in the coordination of movement and play a significant role in neurocognitive processes such as the processing of stimuli and mood regulation. Damage to these areas, again by Fenton chemistry, produces the neuropsychiatric symptoms seen in Wilson's disease.[15]
Why Wilson's disease causes hemolysis is unclear, but various lines of evidence suggest that a high level of free (nonceruloplasmin-bound) copper may be directly affecting the oxidation of hemoglobin, or inhibiting the energy-supplying enzymes in red blood cells, or causing direct damage to cell membranes.[18]
Diagnosis
[edit]
Wilson's disease may be suspected on the basis of any of the symptoms mentioned above, or when a close relative has been found to have Wilson's. Most have slightly abnormal liver function tests such as raised aspartate transaminase, alanine transaminase, and bilirubin levels. If the liver damage is significant, albumin may be decreased due to an inability of damaged liver cells to produce this protein; likewise, the prothrombin time (a test of coagulation) may be prolonged as the liver is unable to produce proteins known as clotting factors.[5] Alkaline phosphatase levels are relatively low in those with Wilson's-related acute liver failure.[19] If neurological symptoms are seen, magnetic resonance imaging of the brain is usually performed; this shows hyperintensities in the part of the brain called the basal ganglia in the T2 setting.[14] MRI may also demonstrate the characteristic "face of the giant panda" pattern.[20]
No totally reliable test for Wilson's disease is known, but levels of ceruloplasmin and copper in the blood, as well of the amount of copper excreted in urine during a 24-hour period, are together used to form an impression of the amount of copper in the body. The most accurate test is a liver biopsy.[5]
Ceruloplasmin
[edit]
Levels of ceruloplasmin are abnormally low (<0.2 g/L) in 80–95% of cases.[5] It can be present at normal levels, though, in people with ongoing inflammation, as it is an acute phase protein. Low ceruloplasmin is also found in Menkes disease and aceruloplasminemia, which are related to, but much rarer than Wilson's disease.[5][14] The combination of neurological symptoms, eye signs, and a low ceruloplasmin level is considered sufficient for the diagnosis of Wilson's disease. In many cases, however, further tests are needed.[14]
Serum and urine copper
[edit]Serum copper is low, which may seem paradoxical given that Wilson's disease is a disease of copper excess. However, 95% of plasma copper is carried by ceruloplasmin, which is often low in Wilson's disease. Urine copper is elevated in Wilson's disease and is collected for 24 hours in a bottle with a copper-free liner. Levels above 100 μg/24h (1.6 μmol/24h) confirm Wilson's disease, and levels above 40 μg/24h (0.6 μmol/24h) are strongly indicative.[5] High urine copper levels are not unique to Wilson's disease; they are sometimes observed in autoimmune hepatitis and in cholestasis (any disease obstructing the flow of bile from the liver to the small bowel).[14]
In children, the following penicillamine test may be used: a 500 mg oral dose of penicillamine is administered, and all urine collected for 24 hours. If the entire day's urine contains more than 1600 μg (25 μmol) of copper, it is a reliable indicator of Wilson's disease. This test has not been validated in adults.[14]
Slit-lamp examination
[edit]The eyes of the patient are examined using a slit lamp to look for Kayser–Fleischer rings, which are strongly associated with Wilson's disease and are caused by copper deposition on the inner cornea in Descemet's membrane.[10]
Liver biopsy
[edit]Once other investigations have indicated Wilson's disease, the ideal test is the removal of a small amount of liver tissue through a liver biopsy. This is assessed microscopically for the degree of steatosis and cirrhosis, and histochemistry and quantification of copper are used to measure the severity of the copper accumulation. A level of 250 μg of copper per gram of dried liver tissue confirms Wilson's disease. Occasionally, lower levels of copper are found; in that case, the combination of the biopsy findings with all other tests could still lead to a formal diagnosis of Wilson's.[5]
In the earlier stages of the disease, the biopsy typically shows steatosis (deposition of fatty material), increased glycogen in the nucleus, and areas of necrosis (cell death). In more advanced disease, the changes observed are quite similar to those seen in autoimmune hepatitis, such as infiltration by inflammatory cells, piecemeal necrosis, and fibrosis (scar tissue). In advanced disease, finally, cirrhosis is the main finding. In acute liver failure, degeneration of the liver cells and collapse of the liver tissue architecture is seen, typically on a background of cirrhotic changes. Histochemical methods for detecting copper are inconsistent and unreliable, and taken alone are regarded as insufficient to establish a diagnosis.[14]
Genetic testing
[edit]Mutation analysis of the ATP7B gene, as well as other genes linked to copper accumulation in the liver, may be performed. Once a mutation is confirmed, family members can be screened for the disease as part of clinical genetics family counseling.[5] Regional distributions of genes associated with Wilson's disease are important to follow, as this can help clinicians design appropriate screening strategies. Since mutations of the ATP7B gene vary between populations, research and genetic testing done in countries such as the USA or United Kingdom can pose problems, as they tend to have more mixed populations.[21]
Treatment
[edit]Diet
[edit]In general, a diet low in copper-containing foods is recommended. High-copper foods avoided in Wilson's disease include mushrooms, nuts, chocolate, dried fruit, liver, sesame seeds, sesame oil, and shellfish.[5]
Medication
[edit]Medical treatments are available for Wilson's disease. Some increase the removal of copper from the body, while others prevent the absorption of copper from the diet.
Generally, penicillamine is the first treatment used. This binds to copper (by chelation) and leads to excretion of copper in the urine. Hence, monitoring of the amount of copper in the urine can be done to ensure a sufficiently high dose is taken. Penicillamine is not without problems; about 20% experience a side effect or complication of penicillamine treatment, such as drug-induced lupus (causing joint pains and a skin rash) or myasthenia (a nerve condition leading to muscle weakness). In those who presented with neurological symptoms, almost half experience a paradoxical worsening in their symptoms. While this phenomenon is observed in other treatments for Wilson's, it is usually taken as an indication for discontinuing penicillamine and commencing second-line treatment.[5][14] Those intolerant to penicillamine may instead be commenced on trientine hydrochloride, which also has chelating properties. Some recommend trientine as first-line treatment, but experience with penicillamine is more extensive.[14] A further agent with known activity in Wilson's disease, under clinical investigation by Wilson Therapeutics, is tetrathiomolybdate. It is regarded as experimental,[14] though some studies have shown a beneficial effect.[5]
Once all results have returned to normal, zinc (usually in the form of a zinc acetate prescription called Galzin) may be used instead of chelators to maintain stable copper levels in the body. Zinc stimulates metallothionein, a protein in gut cells that binds copper and prevents its absorption and transport to the liver. Zinc therapy is continued unless symptoms recur or if the urinary excretion of copper increases.[14]
In rare cases where none of the oral treatments is effective, especially with severe neurological disease, dimercaprol (British anti-Lewisite) is occasionally necessary. This treatment is injected intramuscularly (into a muscle) every few weeks and has unpleasant side effects such as pain.[22]
People who are asymptomatic (for instance, those diagnosed through family screening or only as a result of abnormal test results) are generally treated, as the copper accumulation may cause long-term damage in the future. Whether these people are best treated with penicillamine or zinc acetate is unclear.[14]
Physical and occupational therapies
[edit]Physiotherapy and occupational therapy are beneficial for patients with the neurological form of the disease. The copper-chelating treatment may take up to six months to start working, and these therapies can assist in coping with ataxia, dystonia, and tremors, as well as preventing the development of contractures that can result from dystonia.[23]
Transplantation
[edit]Liver transplantation is an effective cure for Wilson's disease, but is used only in particular scenarios because of the risks and complications associated with the procedure. It is used mainly in people with fulminant liver failure who fail to respond to medical treatment or in those with advanced chronic liver disease. Liver transplantation is avoided in severe neuropsychiatric illnesses, in which its benefit has not been demonstrated.[5][14]
Prognosis
[edit]Left untreated, Wilson's disease tends to become progressively worse and is eventually fatal. Serious complications include liver cirrhosis, acute kidney failure, and psychosis. Liver cancer and cholangiocarcinoma may occur, but at a lower incidence than other chronic liver diseases, and the risk is greatly reduced with treatment.[13] With early detection and treatment, most of those affected can live relatively normal lives and have a life expectancy close to that of the general population.[13] Liver and neurological damage that occurs prior to treatment may improve, but it is often permanent.[24] Fertility is usually normal and pregnancy complications are not increased in those with Wilson's disease that is treated.[13]
History
[edit]The disease bears the name of British physician Samuel Alexander Kinnier Wilson (1878–1937), a neurologist who described the condition, including the pathological changes in the brain and liver, in 1912.[25] Wilson's work had been predated by, and drew on, reports from German neurologist Karl Westphal (in 1883), who termed it "pseudo-sclerosis"; by the British neurologist William Gowers (in 1888);[26] by the Finnish neuropathologist Ernst Alexander Homén (in 1889–1892), who noted the hereditary nature of the disease;[27] and by Adolph Strümpell (in 1898), who noted hepatic cirrhosis.[26] Neuropathologist John Nathaniel Cumings made the link with copper accumulation in both the liver and the brain in 1948.[28] The occurrence of hemolysis was noted in 1967.[29]
In 1951, Cumings (in England), and New Zealand neurologist Derek Denny-Brown (working in the United States), simultaneously reported the first effective treatment, using the metal chelator British anti-Lewisite.[30][31] This treatment had to be injected, but was one of the first therapies available in the field of neurology, a field that classically was able to observe and diagnose, but had few treatments to offer.[26][32] The first oral chelation agent effective in Wilson's disease, penicillamine, was discovered in 1956 by British neurologist John Walshe.[33] In 1982, Walshe also introduced trientine,[34] and was the first to develop tetra-thiomolybdate for clinical use.[35] Zinc acetate therapy initially made its appearance in the Netherlands, where physicians Schouwink and Hoogenraad used it in 1961 and in the 1970s, respectively, and was further developed later by Brewer and colleagues at the University of Michigan.[22][36]
The genetic basis of Wilson's disease, and its link to ATP7B mutations, was elucidated by several research groups in the 1980s and 1990s.[37][38]
In other animals
[edit]Hereditary copper accumulation has been described in Bedlington Terriers,[39] where it generally only affects the liver. In Bedlington Terriers it is due to mutations in the COMMD1 (or MURR1) gene.[40] The discovery of these mutations in the dogs led researchers to examine the corresponding human genes, but COMMD1 mutations could not be detected in humans with non-Wilsonian copper accumulation states (such as Indian childhood cirrhosis).[41]
See also
[edit]References
[edit]- ^ a b c d e f g h i "Wilson Disease". NIDDK. July 2014. Archived from the original on 2016-10-04. Retrieved 2016-11-06.
- ^ Lynn DJ, Newton HB, Rae-Grant A (2004). The 5-minute Neurology Consult. Lippincott Williams & Wilkins. p. 442. ISBN 9780683307238. Archived from the original on 2016-11-07.
- ^ Sahani DV, Samir AE (2016). Abdominal Imaging: Expert Radiology Series (2 ed.). Elsevier Health Sciences. p. 400. ISBN 9780323431613. Archived from the original on 2016-11-07.
- ^ "Whonamedit – dictionary of medical eponyms". www.whonamedit.com. Archived from the original on 2016-11-07. Retrieved 2016-11-06.
- ^ a b c d e f g h i j k l m n o p q r s t u v Ala A, Walker AP, Ashkan K, Dooley JS, Schilsky ML (2007). "Wilson's disease". Lancet. 369 (9559): 397–408. doi:10.1016/S0140-6736(07)60196-2. PMID 17276780. S2CID 24663871.
- ^ a b c Merle U, Schaefer M, Ferenci P, Stremmel W (2007). "Clinical presentation, diagnosis and long-term outcome of Wilson's disease: a cohort study". Gut. 56 (1): 115–20. doi:10.1136/gut.2005.087262. PMC 1856673. PMID 16709660.
- ^ "Wilson's disease - Symptoms and causes". Mayo Clinic. Retrieved 2022-10-05.
- ^ a b c Lorincz MT (2010). "Neurologic Wilson's disease" (PDF). Annals of the New York Academy of Sciences. 1184 (1): 173–87. Bibcode:2010NYASA1184..173L. doi:10.1111/j.1749-6632.2009.05109.x. hdl:2027.42/78731. PMID 20146697. S2CID 2989668.
- ^ Pagonabarraga J, Goetz, C (2012). Biller, J (ed.). Practical Neurology (4th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Heath. p. 282. ISBN 978-1451142631.
- ^ a b Pandey N, John S (21 June 2022). "Kayser-Fleischer Ring". StatPearls. Treasure Island, Florida: StatPearls Publishing. PMID 29083643. Retrieved 30 November 2022.
- ^ Roberts EA, Schilsky ML (2008). "Diagnosis and treatment of Wilson disease: An update". Hepatology. 47 (6): 2089–2111. doi:10.1002/hep.22261. PMID 18506894.
- ^ Yanoff M, Jay S. Duker (2008). Ophthalmology (3rd ed.). Edinburgh: Mosby. p. 411. ISBN 978-0323057516.
- ^ a b c d Roberts EA, Schilsky ML (7 September 2023). "Current and Emerging Issues in Wilson's Disease". New England Journal of Medicine. 389 (10): 922–938. doi:10.1056/NEJMra1903585. PMID 37672695. S2CID 261581755.
- ^ a b c d e f g h i j k l m n Roberts EA, Schilsky ML (2003). "A practice guideline on Wilson disease". Hepatology. 37 (6): 1475–92. doi:10.1053/jhep.2003.50252. PMID 12774027. S2CID 263620.
- ^ a b c d e f g de Bie P, Muller P, Wijmenga C, Klomp LW (November 2007). "Molecular pathogenesis of Wilson and Menkes disease: correlation of mutations with molecular defects and disease phenotypes". J. Med. Genet. 44 (11): 673–88. doi:10.1136/jmg.2007.052746. PMC 2752173. PMID 17717039.
- ^ Kumar M, Gaharwar U, Paul S, Poojary M, Pandhare K, Scaria V, Bk B (2020-06-03). "WilsonGen a comprehensive clinically annotated genomic variant resource for Wilson's Disease". Scientific Reports. 10 (1): 9037. Bibcode:2020NatSR..10.9037K. doi:10.1038/s41598-020-66099-2. ISSN 2045-2322. PMC 7270127. PMID 32493955.
- ^ Grubenbecher S, Stüve O, Hefter H, Korth C (2006). "Prion protein gene codon 129 modulates clinical course of neurological Wilson disease". NeuroReport. 17 (5): 549–52. doi:10.1097/01.wnr.0000209006.48105.90. PMID 16543824. S2CID 37186426.
- ^ Lee GR (1999). "Chapter 48: acquired hemolytic anaemias resulting from direct effects of infectious, chemical or physical agents". In Lee GR, Foerster J, Lukens J, et al. (eds.). Wintrobe's clinical hematology. Vol. 1 (10th ed.). Williams & Wilkins. pp. 1298. ISBN 978-0-683-18242-2.
- ^ Shaver WA, Bhatt H, Combes B (1986). "Low serum alkaline phosphatase activity in Wilson's disease". Hepatology. 6 (5): 859–63. doi:10.1002/hep.1840060509. PMID 3758940. S2CID 24055787.
- ^ Das SK, Ray K (September 2006). "Wilson's disease: an update". Nat Clin Pract Neurol. 2 (9): 482–93. doi:10.1038/ncpneuro0291. PMID 16932613. S2CID 205340375.
- ^ Ferenci P (2006-06-22). "Regional distribution of mutations of the ATP7B gene in patients with Wilson disease: impact on genetic testing". Human Genetics. 120 (2): 151–159. doi:10.1007/s00439-006-0202-5. ISSN 0340-6717. PMID 16791614. S2CID 10124665.
- ^ a b Walshe JM (July 1996). "Treatment of Wilson's disease: the historical background". QJM. 89 (7): 553–55. doi:10.1093/qjmed/89.7.553. PMID 8759497.
- ^ Brewer GJ, Askari FK (2005). "Wilson's disease: clinical management and therapy". Journal of Hepatology. 42 (Suppl 1): 13–21. doi:10.1016/j.jhep.2004.11.013. PMID 15777568.
- ^ "Definition and Facts | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved 2019-02-01.
- ^ Kinnier Wilson SA (1912). "Progressive lenticular degeneration: a familial nervous disease associated with cirrhosis of the liver". Brain. 34 (1): 295–507. doi:10.1093/brain/34.4.295.
- ^ a b c Robertson WM (February 2000). "Wilson's disease". Arch. Neurol. 57 (2): 276–77. doi:10.1001/archneur.57.2.276. PMID 10681092.
- ^ Homén EA (1892). "Eine eigenthümliche bei drei Geschwistern auftretende typische Krankheit unter der Form einer progressiven Dementia in Verbindung mit ausgedehnten Gefässveränderungen (wohl Lues hereditaria tarda)". Archiv für Psychiatrie und Nervenkrankheiten. 24: 1–38.
- ^ Cumings JN (1948). "The copper and iron content of brain and liver in the normal and in hepato-lenticular degeneration". Brain. 71 (Dec): 410–15. doi:10.1093/brain/71.4.410. PMID 18124738.
- ^ McIntyre N, Clink HM, Levi AJ, Cumings JN, Sherlock S (February 1967). "Hemolytic anemia in Wilson's disease". N. Engl. J. Med. 276 (8): 439–44. doi:10.1056/NEJM196702232760804. PMID 6018274.
- ^ Cumings JN (March 1951). "The effects of B.A.L. in hepatolenticular degeneration". Brain. 74 (1): 10–22. doi:10.1093/brain/74.1.10. PMID 14830662.
- ^ Denny-Brown D, Porter H (December 1951). "The effect of BAL (2,3-dimercaptopropanol) on hepatolenticular degeneration (Wilson's disease)". N. Engl. J. Med. 245 (24): 917–25. doi:10.1056/NEJM195112132452401. PMID 14882450.
- ^ Vilensky JA, Robertson WM, Gilman S (September 2002). "Denny-Brown, Wilson's disease, and BAL (British antilewisite [2,3-dimercaptopropanol])". Neurology. 59 (6): 914–16. doi:10.1212/wnl.59.6.914. PMID 12297577.
- ^ Walshe JM (January 1956). "Wilson's disease; new oral therapy". Lancet. 270 (6906): 25–26. doi:10.1016/S0140-6736(56)91859-1. PMID 13279157.
- ^ Walshe JM (March 1982). "Treatment of Wilson's disease with trientine (triethylene tetramine) dihydrochloride". Lancet. 1 (8273): 643–47. doi:10.1016/S0140-6736(82)92201-2. PMID 6121964. S2CID 205999334.
- ^ Harper PL, Walshe JM (December 1986). "Reversible pancytopenia secondary to treatment with tetrathiomolybdate". Br. J. Haematol. 64 (4): 851–53. doi:10.1111/j.1365-2141.1986.tb02250.x. PMID 3801328. S2CID 11546705.
- ^ Brewer GJ (January 2000). "Recognition, diagnosis, and management of Wilson's disease". Proc. Soc. Exp. Biol. Med. 223 (1): 39–46. doi:10.1046/j.1525-1373.2000.22305.x. PMID 10632959. Archived from the original on 2008-04-09. Retrieved 2008-05-20.
- ^ Bull PC, Thomas GR, Rommens JM, Forbes JR, Cox DW (1993). "The Wilson disease gene is a putative copper transporting P-type ATPase similar to the Menkes gene". Nat. Genet. 5 (4): 327–37. doi:10.1038/ng1293-327. PMID 8298639. S2CID 1236890.
- ^ Tanzi RE, Petrukhin K, Chernov I, et al. (1993). "The Wilson disease gene is a copper transporting ATPase with homology to the Menkes disease gene". Nat. Genet. 5 (4): 344–50. doi:10.1038/ng1293-344. PMID 8298641. S2CID 610188.
- ^ Sternlieb I, Twedt DC, Johnson GF, et al. (1977). "Inherited copper toxicity of the liver in Bedlington terriers". Proc. R. Soc. Med. 70 (Suppl 3): 8–9. PMC 1543595. PMID 122681.
- ^ van De Sluis B, Rothuizen J, Pearson PL, van Oost BA, Wijmenga C (2002). "Identification of a new copper metabolism gene by positional cloning in a purebred dog population". Hum. Mol. Genet. 11 (2): 165–73. doi:10.1093/hmg/11.2.165. PMID 11809725.
- ^ Müller T, van de Sluis B, Zhernakova A, et al. (2003). "The canine copper toxicosis gene MURR1 does not cause non-Wilsonian hepatic copper toxicosis". J. Hepatol. 38 (2): 164–68. doi:10.1016/S0168-8278(02)00356-2. PMID 12547404.
External links
[edit]- Wilson disease at NLM Genetics Home Reference