Myalgic encephalomyelitis/chronic fatigue syndrome: Difference between revisions
MEspringal (talk | contribs) |
mNo edit summary |
||
| Line 1: | Line 1: | ||
{{Short description|Chronic medical condition}} |
|||
<span class="plainlinks"></span>{{verylong|date=December 2007}} |
|||
{{Distinguish|text=[[Fatigue#Chronic|chronic fatigue]], a symptom experienced in many chronic illnesses, including [[idiopathic chronic fatigue]]}} |
|||
{{Infobox_Disease | |
|||
{{Featured article}} |
|||
Name = Chronic fatigue syndrome/ myalgic encephalomyelitis | |
|||
{{Use British English|date=March 2024}} |
|||
Image = | |
|||
{{Use dmy dates|date=July 2024}} |
|||
Caption = | |
|||
{{Cs1 config|name-list-style=vanc|display-authors=6}} |
|||
DiseasesDB = 1645 | |
|||
{{Infobox medical condition |
|||
ICD10 = {{ICD10|G|93|3|g|90}} | |
|||
| name = Myalgic encephalomyelitis/chronic fatigue syndrome |
|||
ICD9 = {{ICD9|780.71}} | |
|||
| synonyms = Post-viral fatigue syndrome (PVFS), systemic exertion intolerance disease (SEID)<ref name=IOM2015 />{{rp|20}} |
|||
ICDO = | |
|||
| speciality = [[Rheumatology]], [[rehabilitation medicine]], [[endocrinology]], [[infectious disease (medical specialty)|infectious disease]], [[neurology]], [[immunology]], [[general practice]], [[paediatrics]], other specialists in ME/CFS<ref name="NICE2021">{{cite web |title=Myalgic Encephalomyelitis (Or Encephalopathy)/Chronic Fatigue Syndrome: Diagnosis and Management: NICE Guideline|url=https://www.nice.org.uk/guidance/ng206/resources/myalgic-encephalomyelitis-or-encephalopathychronic-fatigue-syndrome-diagnosis-and-management-pdf-66143718094021 |url-status=live |publisher=[[National Institute for Health and Care Excellence]] (NICE) |date=29 October 2021 |access-date=9 March 2024 |archive-url=https://web.archive.org/web/20240208083814/https://www.nice.org.uk/guidance/ng206/resources/myalgic-encephalomyelitis-or-encephalopathychronic-fatigue-syndrome-diagnosis-and-management-pdf-66143718094021 |archive-date=8 February 2024}}</ref>{{Rp|pages=58}} |
|||
OMIM = | |
|||
| image = File:Icons symptoms ME CFS.svg |
|||
MedlinePlus = 001244 | |
|||
| caption = The four primary symptoms of ME/CFS according to the [[National Institute for Health and Care Excellence]] |
|||
eMedicineSubj = med | |
|||
| alt = Icons of the four key ME/CFS symptoms: low battery for profound fatigue, weak muscle for post-exertional malaise, bed for sleep problems and crossed wires in brain for cognitive difficulties. |
|||
eMedicineTopic = 3392 | |
|||
| symptoms = [[Post-exertional malaise|Worsening of symptoms with activity]], [[Fatigue#Chronic|long-term fatigue]], sleep problems, others<ref name="CDCsym2024" /> |
|||
eMedicine_mult = {{eMedicine2|ped|2795}} | |
|||
| onset = Peaks at 10–19 and 30–39 years old<ref name="pmid31379194" /> |
|||
MeshID = D015673 | |
|||
| duration = Long-term<ref>{{Cite web |date=29 October 2021 |title=Myalgic Encephalomyelitis (Or Encephalopathy)/Chronic Fatigue Syndrome: Diagnosis and Management: Information for the Public |url=https://www.nice.org.uk/guidance/ng206/informationforpublic |access-date=24 March 2024 |publisher=[[National Institute for Health and Care Excellence]] (NICE) |archive-date=4 April 2024 |archive-url=https://web.archive.org/web/20240404205135/https://www.nice.org.uk/guidance/ng206/informationforpublic |url-status=live }}</ref> |
|||
| causes = Unknown<ref name="pmid37793728" /> |
|||
| risks = Being female, [[genetics|family history]], viral infections<ref name="pmid37793728" /> |
|||
| diagnosis = Based on symptoms<ref name="pmid37226227" /> |
|||
| treatment = [[Symptomatic treatment|Symptomatic]]<ref name=CDC2024manage>{{cite web |date=10 May 2024 |title=Manage Myalgic Encephalomyelitis/Chronic Fatigue Syndrome |url-status=live |url=https://www.cdc.gov/me-cfs/management/ |archive-url=https://web.archive.org/web/20240518073532/https://www.cdc.gov/me-cfs/management/ |archive-date=18 May 2024 |access-date=18 May 2024|publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC)}}</ref> |
|||
| prevalence = About 0.17% to 0.89% (pre-[[COVID-19 pandemic]])<ref name=Lim2020/> |
|||
}} |
}} |
||
'''Chronic fatigue syndrome''' ('''CFS''') is one of several names given to a poorly understood, variably debilitating disorder of uncertain [[etiology|cause/causes]]. Based on a 1999 study of adults in the [[United States]], CFS is thought to affect approximately 4 per 1,000 adults.<ref name=pmid10527290>{{cite journal |author=Jason LA, Richman JA, Rademaker AW, Jordan KM, Plioplys AV, Taylor RR, McCready W, Huang CF, Plioplys S |title=A community-based study of chronic fatigue syndrome |journal=Arch. Intern. Med. |volume=159 |issue=18 |pages=2129-37 |year=1999 | url = http://archinte.ama-assn.org/cgi/content/full/159/18/2129?ck=nck |pmid=10527290}}</ref> |
|||
For unknown reasons, CFS occurs more often in women, and adults in their 40s and 50s.<ref>Gallagher AM, Thomas JM, Hamilton WT, White PD. Incidence of fatigue symptoms and diagnoses presenting in UK primary care from 1990 to 2001. ''J R Soc Med 2004;97:571-5. PMID 15574853.</ref><ref name="CDCRisk"/> The illness is estimated to be less prevalent in children and adolescents, but study results vary as to the degree.<ref name="DOI : 10.1300/J092v13n02_01">{{cite journal |author=Jason LA, Jordan K, Miike T, Bell DS, Lapp C, Torres-Harding S, Rowe K, Gurwitt A, De Meirleir K, Van Hoof ELS |title=A Pediatric Case Definition for Myalgic Encephalomyelitis and Chronic Fatigue Syndrome |journal=Journal of Chronic Fatigue Syndrome |volume=13 |issue=2-3 | pages = 1-44 |year=2006| url = <!--http://www.cfids-cab.org/rc/Jason-1.pdf--> | doi = 10.1300/J092v13n02_01}}</ref> |
|||
<!-- Definition and symptoms, wording vague and unspecific, more than just core symptoms --> |
|||
CFS often manifests with cognitive difficulties, chronic mental and physical exhaustion, often severe, and other characteristic symptoms in a previously healthy and active person. Despite promising avenues of [[medical research|research]], there remains no [[medical test|assay]] or [[pathology|pathological]] finding which is widely accepted to be diagnostic of CFS. It remains a [[diagnosis of exclusion]] based largely on patient history and [[symptom]]atic criteria, although a number of tests can aid diagnosis.<ref name="carr">{{cite journal | author = Carruthers BM, Jain AK, De Meirleir KL, Peterson DL, Klimas MD, Lerner AM, Bested AC, Flor-Henry P, Joshi P, Powles ACP, Sherkey JA, van de Sande MI | title = Myalgic encephalomyalitis/chronic fatigue syndrome: Clinical working definition, diagnostic and treatment protocols | journal = Journal of Chronic Fatigue Syndrome | volume = 11 | issue = 1 | pages = 7-36 | year = 2003 | url = http://www.cfids-cab.org/MESA/me_overview.pdf | doi = 10.1300/J092v11n01_02}}</ref> Whereas there is agreement on the genuine threat to health, happiness, and productivity posed by CFS, various [[physician|physicians']] groups, researchers, and patient activists champion very different nomenclature, diagnostic criteria, etiologic hypotheses, and treatments, resulting in controversy about nearly all aspects of the disorder. Even the term ''chronic fatigue syndrome'' is controversial because a large part of the patient community believes the name trivializes the illness.<ref name="Jason"/> |
|||
'''Myalgic encephalomyelitis/chronic fatigue syndrome''' ('''ME/CFS''') is a disabling [[Chronic condition|chronic illness]]. People with ME/CFS experience profound [[fatigue]] that does not go away with rest, as well as sleep issues and problems with memory or concentration. The [[Pathognomonic|hallmark]] symptom is [[post-exertional malaise]], a worsening of the illness which can start immediately or hours to days after even minor physical or mental activity. This "crash" can last from hours or days to several months. Further common symptoms include [[orthostatic intolerance|dizziness or faintness when upright]] and pain.<ref name="CDCsym2024">{{cite web|title=Symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome |url=https://www.cdc.gov/me-cfs/signs-symptoms/|date=10 May 2024|publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC)|access-date=17 May 2024|archive-date=17 May 2024|archive-url=https://web.archive.org/web/20240517191603/https://www.cdc.gov/me-cfs/signs-symptoms/|url-status=live}}</ref><ref name="IQWiG-2023" /> |
|||
<!-- Pathophysiology --> |
|||
''Chronic fatigue syndrome'' is not the same as "chronic fatigue”.<ref name="carr"/> Fatigue is a common symptom in many illnesses, but CFS is a multi-systemic disease and is relatively rare by comparison.<ref name="PMID_15699086">{{cite journal | author = Ranjith G | title = Epidemiology of chronic fatigue syndrome. | journal = Occup Med (Lond) | volume = 55 | issue = 1 | pages = 13-9 | year = 2005 | id = PMID 15699086}}</ref> [[#Diagnosis|Definitions]] (other than the 1991 [[United Kingdom|UK]] Oxford criteria)<ref name="oxford">{{cite journal | author = Sharpe M, Archard L, Banatvala J, Borysiewicz L, Clare A, David A, Edwards R, Hawton K, Lambert H, Lane R | title = A report--chronic fatigue syndrome: guidelines for research. | journal = J R Soc Med | volume = 84 | issue = 2 | pages = 118-21 | year = 1991 | id = PMID 1999813}} Synopsis by {{GPnotebook|-476446699}})</ref> require a number of features, the most common being severe mental and physical exhaustion which is "unrelieved by rest" (1994 Fukuda definition),<ref name="CDC1994">{{cite journal | author = Fukuda K, Straus S, Hickie I, Sharpe M, Dobbins J, Komaroff A | title = The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. | journal = Ann Intern Med | volume = 121 | issue = 12 | pages = 953-9 | year = 1994 | id = PMID 7978722}} [http://www.annals.org/cgi/content/full/121/12/953#F2 case definition]</ref> and may be worsened by even trivial exertion (a mandatory diagnostic criterion according to some systems). Most diagnostic criteria require that symptoms must be present for at least six months, and all state the symptoms must not be caused by other medical conditions. CFS patients may report many symptoms which are not included in all diagnostic criteria, including [[muscle weakness]], [[cognitive]] dysfunction, [[hypersensitivity]], [[orthostatic intolerance]], digestive disturbances, [[clinical depression|depression]], poor [[immune response]], and [[cardiac]] and [[Respiratory system|respiratory]] problems. It is unclear if these symptoms represent co-morbid conditions or are produced by an underlying etiology of CFS.<ref name="pmid:12562565">{{cite journal |author=Afari N, Buchwald D |title=Chronic fatigue syndrome: a review |journal=Am J Psychiatr |volume=160 |issue=2 |pages=221-36 |year=2003 |pmid=12562565 |url=http://ajp.psychiatryonline.org/cgi/content/full/160/2/221}}</ref> Some cases improve over time, and treatments (though none are universally accepted) bring a degree of improvement to many others, though full resolution may be only 5-10% according to the United States [[Centers for Disease Control and Prevention]] (CDC).<ref name="CDCBasic"/> |
|||
The cause of the disease is unknown.<ref name="CDC_Clinical2024" /> ME/CFS often starts after an infection, such as [[infectious mononucleosis|mononucleosis]].<ref name="Bateman-2021" /> It can run in families, but no [[genes]] that contribute to ME/CFS have been confirmed.<ref name="Dibble McGrath Ponting 2020 p.">{{cite journal |vauthors=Dibble JJ, McGrath SJ, Ponting CP |date=September 2020 |title=Genetic Risk Factors of ME/CFS: A Critical Review |journal=Human Molecular Genetics |volume=29 |issue=R1 |pages=R117–R124 |doi=10.1093/hmg/ddaa169 |pmc=7530519 |pmid=32744306}}</ref> ME/CFS is associated with changes in the nervous and immune systems, as well as in energy production.<ref name="pmid38443223">{{cite journal |vauthors=Annesley SJ, Missailidis D, Heng B, Josev EK, Armstrong CW |date=March 2024 |title=Unravelling Shared Mechanisms: Insights from Recent ME/CFS Research to Illuminate Long COVID Pathologies |url=|journal=Trends in Molecular Medicine |volume=30 |issue=5 |pages=443–458 |doi=10.1016/j.molmed.2024.02.003 |pmid=38443223 |doi-access=free}}</ref> Diagnosis is based on symptoms and a [[differential diagnosis]] because no diagnostic test is available.<ref name="pmid37226227" /><ref>{{Cite web |title=Myalgic encephalomyelitis (Chronic fatigue syndrome) - Symptoms, diagnosis and treatment {{!}} BMJ Best Practice US |url=https://bestpractice.bmj.com/topics/en-us/277 |access-date=2024-10-21 |website=bestpractice.bmj.com |language=en-us}}</ref><ref>{{Cite web |title=Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (CFS) {{!}} Diseases & Conditions {{!}} 5MinuteConsult |url=https://5minuteconsult.com/collectioncontent/1-151513/diseases-and-conditions/myalgic-encephalomyelitis-chronic-fatigue-syndrome-cfs |access-date=2024-11-25 |website=5minuteconsult.com}}</ref><ref name="pmid28033311" /> |
|||
<!-- Management and epidemiology --> |
|||
==Nomenclature== |
|||
The illness can improve or worsen over time, but full recovery is uncommon.<ref name="Bateman-2021">{{cite journal |vauthors=Bateman L, Bested AC, Bonilla HF, Chheda BV, Chu L, Curtin JM, Dempsey TT, Dimmock ME, Dowell TG, Felsenstein D, Kaufman DL, Klimas NG, Komaroff AL, Lapp CW, Levine SM, Montoya JG, Natelson BH, Peterson DL, Podell RN, Rey IR, Ruhoy IS, Vera-Nunez MA, Yellman BP |date=November 2021 |title=Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of Diagnosis and Management |journal=Mayo Clinic Proceedings |volume=96 |issue=11 |pages=2861–2878 |doi=10.1016/j.mayocp.2021.07.004 |pmid=34454716 |s2cid=237419583 |doi-access=free |title-link=doi}}</ref> No therapies or medications are approved to treat the condition, and management is aimed at relieving symptoms.<ref name="NICE2021" />{{Rp|pages=29}} [[Pacing (activity management)|Pacing of activities]] can help avoid worsening symptoms, and counselling may help in coping with the illness.<ref name=CDC2024manage /> Before the [[COVID-19 pandemic]], ME/CFS affected two to nine out of every 1,000 people, depending on the definition.<ref name="Lim2020">{{cite journal |vauthors=Lim EJ, Ahn YC, Jang ES, Lee SW, Lee SH, Son CG |date=February 2020 |title=Systematic Review and Meta-Analysis Of the Prevalence of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME) |journal=Journal of Translational Medicine |volume=18 |issue=1 |pages=100 |doi=10.1186/s12967-020-02269-0 |pmc=7038594 |pmid=32093722 |doi-access=free |title-link=doi}}</ref> However, many people fit ME/CFS diagnostic criteria after contracting [[long COVID]].<ref name="Davis-2023">{{cite journal |vauthors=Davis HE, McCorkell L, Vogel JM, Topol EJ |date=March 2023 |title=Long COVID: Major Findings, Mechanisms and Recommendations |journal=Nature Reviews. Microbiology |volume=21 |issue=3 |pages=133–146 |doi=10.1038/s41579-022-00846-2 |pmc=9839201 |pmid=36639608}}</ref> ME/CFS occurs more often in women than in men. It is more common in [[middle age]], but can occur at all ages, including childhood.<ref name="CDC_Basics" /> |
|||
The naming of chronic fatigue syndrome has been challenging, since consensus is lacking within the medical, research, and patient communities regarding the defining features of the syndrome. It may be considered by different authorities to be a central nervous system, metabolic, (post-)infectious, immune system or neuropsychiatric disorder. |
|||
<!-- Society and culture --> |
|||
There are a number of different terms which have been identified at various times with this disorder. |
|||
ME/CFS has a large social and economic impact, and the disease can be socially isolating.<ref name="Boulazreg_2024">{{Cite journal | vauthors = Boulazreg, S, Rokach A |date=17 July 2020 |title=The Lonely, Isolating, and Alienating Implications of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome |journal=Healthcare |language=en |volume=8 |issue=4 |pages=413–433 |doi=10.3390/healthcare8040413 |issn=2164-1846 |doi-access=free|pmid=33092097 |pmc=7711762 }}</ref> About a quarter of those affected are unable to leave their bed or home.<ref name="IQWiG-2023">{{Cite book |last=Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) |url=https://www.iqwig.de/download/n21-01_me-cfs-aktueller-kenntnisstand_abschlussbericht_v1-0.pdf |title=Myalgische Enzephalomyelitis / Chronic Fatigue Syndrome (ME/CFS): Aktueller Kenntnisstand |date=17 April 2023 |publisher=[[Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen]] |language=de |trans-title=Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): current state of knowledge |issn=1864-2500 |access-date=8 November 2023 |archive-url=https://web.archive.org/web/20231102160213/https://www.iqwig.de/download/n21-01_me-cfs-aktueller-kenntnisstand_abschlussbericht_v1-0.pdf |archive-date=2 November 2023 |url-status=live}}</ref>{{Rp|3}} People with ME/CFS often face stigma in healthcare settings, and care is complicated by [[Controversies related to ME/CFS|controversies around the cause and treatments]] of the illness.<ref name="Hussein-2024">{{Cite journal |last1=Hussein |first1=Said |last2=Eiriksson |first2=Lauren |last3=MacQuarrie |first3=Maureen |last4=Merriam |first4=Scot |last5=Dalton |first5=Maria |last6=Stein |first6=Eleanor |last7=Twomey |first7=Rosie |date=2024 |title=Healthcare System Barriers Impacting the Care of Canadians with Myalgic Encephalomyelitis: A Scoping Review |journal=Journal of Evaluation in Clinical Practice |volume=30 |issue=7 |pages=1337–1360 |language=en |doi=10.1111/jep.14047 |issn=1356-1294|doi-access=free |pmid=39031904 }}</ref> Doctors may be unfamiliar with ME/CFS, as it is often not fully covered in medical school.<ref name="Davis-2023"/> Historically, research funding for ME/CFS has been far below that of diseases with comparable impact.<ref name="Tyson_2022">{{Cite journal |vauthors=Tyson S, Stanley K, Gronlund TA, Leary S, Emmans Dean M, Dransfield C, Baxter H, Elliot R, Ephgrave R, Bolton M, Barclay A, Hoyes G, Marsh B, Fleming R, Crawford J |date=2022 |title=Research Priorities for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): The Results of a James Lind Alliance Priority Setting Exercise |journal=Fatigue: Biomedicine, Health & Behavior |language=en |volume=10 |issue=4 |pages=200–211 |doi=10.1080/21641846.2022.2124775 |issn=2164-1846 |s2cid=252652429 |doi-access=free}}</ref> |
|||
* ''Myalgic encephalomyelitis'' or ME translates to "inflammation of the brain and spinal cord with muscle pain" and first appeared as "benign myalgic encephalomyelitis" in a ''[[The Lancet|Lancet]]'' editorial by Sir [[Donald Acheson]] in 1956.<ref name=Acheson1956>{{cite journal |author=[Anonymous] |title=A new clinical entity? |journal=Lancet |volume=270 |issue=6926 |pages=789–90 |year=1956 |pmid=13320887 |doi=}}</ref> In a 1959 review he referred to several older reports that appeared to describe a similar syndrome.<ref name="ach">{{cite journal | author = Acheson E | title = The clinical syndrome variously called benign myalgic encephalomyelitis, Iceland disease and epidemic neuromyasthenia. | journal = Am J Med | volume = 26 | issue = 4 | pages = 569-95 | year = 1959 | id = PMID 13637100}}</ref> The neurologist [[Russell Brain, 1st Baron Brain|Lord Brain]] included ME in the 1962 sixth edition of his textbook of neurology,<ref>{{cite book |editor=Brain R |authorlink= |title=Diseases of the Nervous System |edition=6 |year=1962}}</ref> A 1978 [[British Medical Journal]] article stated the [[Royal Society of Medicine]] conference to discuss the illness during that year clearly agreed Myalgic Encephalomyelitis was a distinct name for the disease. The article also stated the previous word (benign) used with ME was rejected as unsatisfactory and misleading because the condition may be devastating to the patient.<ref name="pmid647324">{{cite journal | author = No authors listed | title = Epidemic myalgic encephalomyelitis | url = http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=647324 | journal = Br Med J.| volume = 1 | issue = 6125 | pages = 1436-7 | Date = 1978 06 03 | id = PMID 647324}}</ref> In 1988 both the [[British Department of Health|UK Department of Health and Social Services]] and the [[British Medical Association]] officially recognized it as a legitimate and potentially distressing disorder.{{Fact|date=October 2007}} Opponents of the term ME state that there is no objective evidence of inflammation. In some patients diagnosed with CFS (e.g. the case of [[Sophia Mirza]]), central nervous system inflammation has been documented. Many patients, and some research and medical professionals in the United Kingdom and Canada, use this term in preference to or in conjunction with CFS (ME/CFS or CFS/ME). The international association of researchers and clinicians is named IACFS/ME. |
|||
* ''Myalgic encephalopathy'', similar to the above, with "pathy" referring to unspecified pathology rather than inflammation; this term has some support in the UK and US. |
|||
* ''Chronic Epstein-Barr virus'' (CEBV) or ''Chronic Mononucleosis''; the term CEBV was introduced in 1985 by virologists Dr. Stephen Straus<ref name="pmid2578268">{{cite journal | author = Straus S, Tosato G, Armstrong G, Lawley T, Preble O, Henle W, Davey R, Pearson G, Epstein J, Brus I | title = Persisting illness and fatigue in adults with evidence of Epstein-Barr virus infection. | journal = Ann Intern Med | volume = 102 | issue = 1 | pages = 7-16 | year = 1985 | id = PMID 2578268}}</ref> and Dr. Jim Jones<ref name="pmid2578266">{{cite journal | author = Jones J, Ray C, Minnich L, Hicks M, Kibler R, Lucas D | title = Evidence for active Epstein-Barr virus infection in patients with persistent, unexplained illnesses: elevated anti-early antigen antibodies. | journal = Ann Intern Med | volume = 102 | issue = 1 | pages = 1-7 | year = 1985 | id = PMID 2578266}}</ref> in the United States. The [[Epstein-Barr virus]], a neurotropic virus that more commonly causes [[infectious mononucleosis]], was thought by Straus and Jones to be the cause of CFS. Subsequent discovery of the closely related ''[[HHV-6|human herpesvirus 6]]'' shifted the direction of biomedical studies, although a vastly expanded and substantial body of published research continues to show active viral infection or reinfection of CFS patients by these two viruses. These viruses are also found in healthy controls, lying dormant. |
|||
* ''Chronic fatigue syndrome'' (CFS) was proposed in 1988 by researchers from the [[United States|U.S.]] [[Centers for Disease Control and Prevention]] (CDC) to replace the name chronic Epstein-Barr virus syndrome when they published an initial case definition for research of the illness after investigating the 1984 Lake Tahoe ME epidemic.<ref name=Holmes1988/> CFS is used increasingly over other designations, particularly in the United States. Many patients and clinicians perceive the term as trivializing,<ref name="Jason">Jason LA, Taylor RR. (2001). Measuring Attributions About Chronic Fatigue Syndrome. ''J Chronic Fatigue Syndr'' '''8''' (3/4); 31-40 [http://www.cfids-cab.org/cfs-inform/Welcome/jason.taylor01.txt TXT formal]</ref> and as the 1994 Fukuda paper itself cedes, stigmatizing, which led to a movement in the United States to change the name and definition.<ref name="name">{{cite web | title = Advocacy Archives: Name Change | publisher = The CFIDS Association of America | url = http://www.cfids.org/advocacy/name-change.asp | accessdate = 2008-01-16 }}</ref> Eighty-five percent of respondents to a 1997 survey conducted by the [[Chronic Fatigue Immune Dysfunction Syndrome Association of America]] wanted the name changed.<ref name="Jason"/> The CFS Coordinating Committee (CFSCC) of the U.S. [[Department of Health and Human Services]] formed a name change workgroup in 2000.<ref>{{Citation | last = Lavrich | first = Carol | title = Name Change Workgroup, CFSCC | publisher = US Department of Health and Human Services, Chronic Fatigue Syndrome Advisory Committee |date=September 29 2003 | location = National Institutes of Health Building 31C, Conference Room 10, Bethesda, Maryland | url = http://www.hhs.gov/advcomcfs/sept_meeting_min.html#carollavrich | accessdate = 2007-12-29}}</ref> Terms were recommended which implied specific underlying etiologies or pathologic processes, but work was shelved in December 2003 when the successor CFS Advisory Committee (CFSAC) decided a name change would be too disruptive at that time.<ref>{{Citation | last = Bell D.S. et al | title = Name Change | publisher = US Department of Health and Human Services Chronic Fatigue Syndrome Advisory Committee (CFSAC) |
|||
Second Meeting |date = December 03 2003 | location = Hubert H. Humphrey Building, 200 Independence Avenue, SW, Room 800, Washington, DC 20201 | url = http://www.hhs.gov/advcomcfs/dec_meeting_min.html#name_change | accessdate = 2008-01-16}}</ref> |
|||
* Chronic fatigue immune dysfunction syndrome (CFIDS); many patients and advocacy groups in the USA use the term CFIDS, in an attempt to reduce the psychiatric stigma attached to "chronic fatigue," as well as the public perception of CFS as a psychiatric syndrome. The term also calls attention to the immune dysfunction in patients which research suggests is an integral part of the illness.<ref name="Buchwald">{{cite journal | author = Buchwald D, Cheney P, Peterson D, Henry B, Wormsley S, Geiger A, Ablashi D, Salahuddin S, Saxinger C, Biddle R | title = A chronic illness characterized by fatigue, neurologic and immunologic disorders, and active human herpesvirus type 6 infection. | journal = Ann Intern Med | volume = 116 | issue = 2 | pages = 103-13 | year = 1992 | id = PMID 1309285}}</ref><ref name="PMID_16612182"/> |
|||
* ''[[Post-viral fatigue syndrome]]'' (PVFS); this is a related disorder. According to ME researcher, Dr. Melvin Ramsay, "The crucial differentiation between ME and other forms of post-viral fatigue syndrome lies in the striking variability of the symptoms not only in the course of a day but often within the hour<ref name="Ramsay86">Ramsay MA (1986), "Postviral Fatigue Syndrome. The saga of Royal Free disease", Londen, ISBN 0-906923-96-4</ref>. |
|||
* ''Low Natural Killer Syndrome'' (LNKS); this term reflected research on patients showing diminished in-vitro [[natural killer cell]] activity in a small 1987 study in Japan.<ref name="CFS Straus">{{cite book | last = edited by Straus |
|||
| first = Stephen E. | title = Chronic Fatigue Syndrome | publisher = Marcel Dekker Inc. | date = 1994 | location = New York, Basel, Hong Kong | page = 227 | id = | isbn = 0824791878 }}</ref><ref name="LNKS">{{cite journal |author= Aoki T, Usuda Y, Miyakoshi H, Tamura K, Herberman RB. |title = Low natural killer syndrome: clinical and immunologic features |journal=Nat Immun Cell Growth Regul. |volume=6 |issue=3 |pages=116-28 |year=1987 |pmid=2442602}}</ref> A case definition for CFS in Japan<ref name="Japan 1991Case">{{cite journal |author= Kitani T, Kuratsune H, Yamaguchi K. |title = Diagnostic criteria for chronic fatigue syndrome by the CFS Study Group in Japan |journal=Nippon Rinsho. |volume=50 |issue=11 |pages=2600-5 |year= Nov 1992 |pmid=1287236 }}</ref> was adopted in 1991 based on the CDC 1988 criteria, an updated diagnostic guideline is planned.<ref name="HistoryJapan">{{cite journal |author= Hashimoto N. et al |title = History of chronic fatigue syndrome |journal=Nippon Rinsho. |volume=65 |issue=6 |pages=975-82 |year= Jun 2007 |pmid=17561685}}</ref> |
|||
* ''Yuppie Flu''; this was a factually inaccurate term first published in a November 1990 ''[[Newsweek]]'' cover story and never official medical terminology. It reflects a stereotypical assumption that CFS mainly affects the affluent ("[[yuppie]]s"), and implies that it is a form of [[Burnout (psychology)|burnout]].<ref name="flu">{{Citation | author =Cowley, Geoffrey, with Mary Hager and Nadine Joseph | title = Chronic Fatigue Syndrome | journal = Newsweek | pages = Cover Story |date=1990-11-12}}</ref> CFS, however, affects people of all races, genders, and social standings<ref name=pmid10527290/>, and is not a form of [[influenza|flu]]. The phrase is considered [[List of disability-related terms with negative connotations|offensive]] by patients and clinicians.<ref>Compact Oxford English Dictionary, Oxford University Press[http://www.askoxford.com/concise_oed/yuppieflu?view=uk]</ref><ref>Packhard, Randall M. (2004). Emerging Illnesses and Society: Negotiating the Public Health Agenda. Johns Hopkins University Press, p. 156. ISBN 0-801-879-426</ref><ref>Anon. "New Therapy For Chronic Fatigue Syndrome To Be Tested At Stanford" Medical News Today[http://www.medicalnewstoday.com/medicalnews.php?newsid=60423]</ref> |
|||
* Uncommonly used terms include ''Akureyri Disease'', ''Iceland disease'' (in [[Iceland]]),<ref>{{cite journal |author=Blattner R |title=Benign myalgic encephalomyelitis (Akureyri disease, Iceland disease) |journal=J. Pediatr. |volume=49 |issue=4 |pages=504-6 |year=1956 |pmid=13358047}}</ref> ''[[Royal Free Hospital|Royal Free]] disease'' (after the location of an outbreak),<ref name="Ramsay-RF"/> ''atypical [[poliomyelitis]]''<ref name="Gilliam38"/>, ''epidemic neuromyasthenia'', ''epidemic vasculitis'', ''[[raphe nucleus]] encephalopathy'', and ''Tapanui flu'' (after the [[New Zealand]] town [[Tapanui]] where the first doctor in the country to investigate the disease, Dr [[Peter Snow (doctor)|Peter Snow]], lived). |
|||
== |
== Classification and terminology == |
||
ME/CFS has been classified as a [[Neurological disorder|neurological disease]] by the [[World Health Organization]] (WHO) since 1969, initially under the name [[History of ME/CFS#Case definitions (1986 onwards)|''benign myalgic encephalomyelitis'']].<ref>{{Cite book |vauthors = Bateman L |title=Neurobiology of Brain Disorders : Biological Basis of Neurological and Psychiatric Disorders |publisher=[[Elsevier]] |year=2022 |isbn=978-0-323-85654-6 | veditors = Zigmond M, Wiley C, Chesselet MF |edition=2nd |chapter=Fibromyalgia and myalgic encephalomyelitis/chronic fatigue syndrome }}</ref>{{rp|564}} The classification of ME/CFS as a neurological disease is based on symptoms which indicate a central role of the nervous system.<ref name="pmid328732972">{{cite journal |vauthors=Shan ZY, Barnden LR, Kwiatek RA, Bhuta S, Hermens DF, Lagopoulos J |date=September 2020 |title=Neuroimaging Characteristics of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Systematic Review |url=|journal=Journal of Translational Medicine |volume=18 |issue=1 |pages=335 |doi=10.1186/s12967-020-02506-6 |pmc=7466519 |pmid=32873297 |doi-access=free}}</ref> Alternatively, on the basis of abnormalities in [[White blood cell|immune cells]], ME/CFS is sometimes labelled a [[Neuroimmunology|neuroimmune]] condition.<ref name="Marshall-Gradisnik_2022" /> The disease can further be regarded as a [[post-acute infection syndrome]] (PAIS) or an infection-associated chronic illness.<ref name="CDC_Clinical2024" /><ref name="pmid35585196" /> PAISes such as [[long COVID]] and [[Lyme disease|post-treatment Lyme disease syndrome]] share many symptoms with ME/CFS and are suspected to have a similar cause.<ref name="pmid35585196">{{cite journal |vauthors=Choutka J, Jansari V, Hornig M, Iwasaki A |date=May 2022 |title=Unexplained Post-Acute Infection Syndromes |url= |journal=Nature Medicine |volume=28 |issue=5 |pages=911–923 |doi=10.1038/s41591-022-01810-6 |pmid=35585196 |s2cid=248889597 |doi-access=free}}</ref> |
|||
===Onset=== |
|||
Many names have been proposed for the illness. The most commonly used are ''chronic fatigue syndrome'', ''myalgic encephalomyelitis'', and the umbrella term ''myalgic encephalomyelitis/chronic fatigue syndrome'' (''ME/CFS''). Reaching consensus on a name has been challenging because the cause and pathology remain unknown.<ref name="IOM2015">{{cite book |last1=Committee on the Diagnostic Criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome |url=https://www.ncbi.nlm.nih.gov/books/NBK274235/pdf/Bookshelf_NBK274235.pdf |title=Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness |last2=Board on the Health of Select Populations |author3=Institute of Medicine |date=10 February 2015 |publisher=[[National Academies Press]] |isbn=978-0-309-31689-7 |pmid=25695122 |access-date=28 July 2020 |archive-url=https://web.archive.org/web/20170120175658/https://www.ncbi.nlm.nih.gov/books/NBK274235/pdf/Bookshelf_NBK274235.pdf |archive-date=20 January 2017 |url-status=live}}</ref>{{rp|29–30}} In the WHO's most recent classification, the [[ICD-11]], chronic fatigue syndrome and myalgic encephalomyelitis are named under post-viral fatigue syndrome.<ref name="ICD11">{{cite web |title=8E49 Postviral Fatigue Syndrome |url=https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f569175314 |url-status=live |archive-url=https://archive.today/20180801205234/https://icd.who.int/browse11/l-m/en%23/http://id.who.int/icd/entity/294762853#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f569175314 |archive-date=1 August 2018 |access-date=20 May 2020 |website=ICD-11 – Mortality and Morbidity Statistics |publisher=[[World Health Organization]]}}</ref> The term ''post-infectious fatigue syndrome'' was initially proposed as a subset of "chronic fatigue syndrome" with a documented triggering infection, but might also be used as a synonym of ME/CFS or as a broader set of fatigue conditions after infection.<ref name="pmid35585196" /> |
|||
====Sudden onset cases==== |
|||
The majority of CFS cases start suddenly,<ref name="PMID_9201648"/> usually accompanied by a "flu-like illness"<ref name="pmid:12562565"/><ref>{{cite journal | author = Sairenji T, Nagata K | title = Viral infections in chronic fatigue syndrome. | journal = Nippon Rinsho | volume = 65 | issue = 6 | pages = 991-6 | year = 2007 | id = PMID 17561687}}</ref><ref>{{cite journal | author = Evengård B, Jonzon E, Sandberg A, Theorell T, Lindh G | title = Differences between patients with chronic fatigue syndrome and with chronic fatigue at an infectious disease clinic in Stockholm, Sweden. | journal = Psychiatry Clin Neurosci | volume = 57 | issue = 4 | pages = 361-8 | year = 2003 | id = PMID 12839515}}</ref><ref>{{cite journal | author = Evengård B, Schacterle RS, Komaroff AL | title = Chronic fatigue syndrome: new insights and old ignorance. | journal = J Intern Med | volume = 246 | issue = 5 | pages = 455-69 | year = 1999 | id = PMID 10583715}}</ref> which is more likely to occur in winter<ref>{{cite journal | author = Jason LA, Taylor RR, Carrico AW | title = A community-based study of seasonal variation in the onset of chronic fatigue syndrome and idiopathic chronic fatigue. | journal = Chronobiol Int | volume = 18 | issue = 2 | pages = 315-9 | year = 2001 | id = PMID 11379670}}</ref><ref>{{cite journal | author = Zhang QW, Natelson BH, Ottenweller JE, Servatius RJ, Nelson JJ, De Luca J, Tiersky L, Lange G | title = Chronic fatigue syndrome beginning suddenly occurs seasonally over the year. | journal = Chronobiol Int | volume = 17 | issue = 1 | pages = 95-9 | year = 2000 | id = PMID 10672437}}</ref>, while a significant proportion of cases begin within several months of severe adverse stress.<ref>{{cite journal | author = Hatcher S, House A | title = Life events, difficulties and dilemmas in the onset of chronic fatigue syndrome: a case-control study. | journal = Psychol Med | volume = 33 | issue = 7 | pages = 1185-92 | year = 2003 | id = PMID 14580073 | url: http://eprints.whiterose.ac.uk/1226/1/house3.pdf}}</ref><ref name="PMID_10367610">{{cite journal | author = Theorell T, Blomkvist V, Lindh G, Evengard B | title = Critical life events, infections, and symptoms during the year preceding chronic fatigue syndrome (CFS): an examination of CFS patients and subjects with a nonspecific life crisis. | journal = Psychosom Med. | volume = 61 | issue = 3 | pages = 304-10 | id = PMID 10367610}}</ref><ref name="PMID_9201648">{{cite journal | author = Salit IE | title = Precipitating factors for the chronic fatigue syndrome. | journal = J Psychiatr Res | volume = 31 | issue = 1 | pages = 59-65 | year = 1997 | id = PMID 9201648}}</ref> Many people report getting a case of a [[influenza|flu]]-like or other [[respiratory infection]] such as [[bronchitis]], from which they seem never to fully recover and which evolves into CFS. The diagnosis of [[Post Viral Fatigue Syndrome]] is sometimes given in the early stage of the illness.<ref name="PMID:16950834"/> One study reported CFS occurred in some patients following a [[vaccination]] or a [[blood transfusion]].<ref name="Becker02">{{cite journal | author = De Becker P, McGregor N, De Meirleir K | title = Possible Triggers and Mode of Onset of Chronic Fatigue Syndrome | journal = Journal of Chronic Fatigue Syndrome | volume = 10 | issue = 2 | pages = 2-18 | year = 2002 | doi = 10.1300/J092v10n02_02}}</ref> The accurate prevalence and exact roles of infection and stress in the development of CFS however are currently unknown. |
|||
Many individuals with ME/CFS object to the term ''chronic fatigue syndrome''. They consider the term simplistic and trivialising, which in turn prevents the illness from being taken seriously.<ref name="IOM2015" />{{rp|234}}<ref name="Bhatia-2023">{{Cite journal |vauthors=Bhatia S, Jason LA |date=24 February 2023 |title=Using Data Mining and Time Series to Investigate ME and CFS Naming Preferences |url=http://journals.sagepub.com/doi/10.1177/10442073231154027 |url-status=live |journal=Journal of Disability Policy Studies |volume=35 |pages=65–72 |doi=10.1177/10442073231154027 |issn=1044-2073 |s2cid=257198201 |archive-url=https://web.archive.org/web/20231106033933/https://journals.sagepub.com/doi/10.1177/10442073231154027 |archive-date=6 November 2023 |access-date=15 October 2023}}</ref> At the same time, there are also issues with the use of ''myalgic encephalomyelitis'' (myalgia means muscle pain and [[encephalitis|encephalomyelitis]] means brain and spinal cord inflammation), as there is only limited evidence of brain inflammation implied by the name.<ref name="BMJbest_practice3" />{{rp|3}} The umbrella term ''ME/CFS'' would retain the better-known phrase ''CFS'' without trivialising the disease, but some people object to this name too, as they see CFS and ME as distinct illnesses.<ref name="Bhatia-2023" /> |
|||
====Gradual onset cases==== |
|||
Other cases have a gradual onset, sometimes spread over years<ref name="Becker02"/>. Patients with [[Lyme disease]] may, despite a standard course of treatment, "evolve" clinically from the symptoms of acute Lyme to those similar to CFS<ref>{{cite journal | author = Donta S | title = Late and chronic Lyme disease. | journal = Med Clin North Am | volume = 86|issue = 2|pages = 341-9, vii|year = 2002|id = PMID 11982305}}</ref>. This has become [[Lyme disease controversy|an area of great controversy]]. |
|||
A 2015 report from the US Institute of Medicine recommended the illness be renamed ''systemic exertion intolerance disease'' (''SEID'') and suggested new diagnostic criteria.<ref name="IOM2015" /> While the new name was not widely adopted, the diagnostic criteria were taken over by the CDC. Like ''CFS'', the name ''SEID'' only focuses on a single symptom, and opinion from those affected was generally negative.<ref>{{Cite journal |vauthors=Jason LA, Johnson M |date=2 April 2020 |title=Solving the ME/CFS Criteria and Name Conundrum: The Aftermath of IOM |journal=Fatigue: Biomedicine, Health & Behavior |volume=8 |issue=2 |pages=97–107 |doi=10.1080/21641846.2020.1757809 |issn=2164-1846 |s2cid=219011696}}</ref> |
|||
===Course=== |
|||
It can be inferred from the 2003 "Canadian" clinical working definition of ME/CFS<ref name="carr"/> that there are 8 categories of symptoms: |
|||
* [[Fatigue (physical)|Fatigue]]: Unexplained, persistent, or recurrent physical and mental fatigue/[[exhaustion]] that substantially reduces activity levels and is not relieved (or not completely relieved) by rest. |
|||
== Signs and symptoms == |
|||
* Post-exertional [[malaise]]: An inappropriate loss of physical and mental stamina, rapid muscular and cognitive fatigability, post exertional malaise and/or fatigue and/or pain and a tendency for other associated symptoms to worsen with a pathologically slow recovery period of usually 24 hours or longer. According to the authors of the Canadian clinical working definition of ME/CFS<ref name="carr"/>, the malaise that follows exertion is often reported to be similar to the generalized pain, discomfort and fatigue associated with the acute phase of influenza. Although common in CFS, this may not be the most severe symptom in the individual case, where other symptoms (such as headaches, neurocognitive difficulties, pain and sleep disturbances) can dominate. |
|||
ME/CFS causes debilitating fatigue, sleep problems, and [[post-exertional malaise]] (PEM, overall symptoms getting worse after mild activity). In addition, cognitive issues, [[orthostatic intolerance]] (dizziness or nausea when upright) or other physical symptoms may be present (see also {{Section link|2=Diagnostic criteria|nopage=yes}}). Symptoms significantly reduce the ability to function and typically last for three to six months before a diagnosis can be confirmed.<ref name="IQWiG-2023" />{{Rp|page=13}}<ref name="NICE2021" />{{Rp|page=11}} ME/CFS usually starts after an infection. Onset can be sudden or more gradual over weeks to months.<ref name="Bateman-2021" /> |
|||
=== Core symptoms === |
|||
* [[Dyssomnia|Sleep dysfunction]]: "Unrefreshing" sleep/rest, poor sleep quantity, [[insomnia]] or rhythm disturbances. A study found that most CFS patients have clinically significant sleep abnormalities that are potentially treatable.<ref>{{cite journal | author = Krupp LB, Jandorf L, Coyle PK, Mendelson WB | title = Sleep disturbance in chronic fatigue syndrome. | journal = J Psychosom Res | volume = 37 | issue = 4 | pages = 325-31 | year = 1993 | id = PMID 8510058}}</ref> Several studies suggest that while CFS patients may experience altered sleep architecture (such as reduced sleep efficiency, a reduction of deep sleep, prolonged sleep initiation, and alpha-wave intrusion during deep sleep) and mildly disordered breathing, overall sleep dysfunction does not seem to be a critical or causative factor in CFS.<ref>{{cite journal | author = Reeves WC, Heim C, Maloney EM, Youngblood LS, Unger ER, Decker MJ, Jones JF, Rye DB | title = Sleep characteristics of persons with chronic fatigue syndrome and non-fatigued controls: results from a population-based study. | journal = BMC Neurol | volume = 6 | pages = 41 | year = 2006 | id = PMID 17109739}}</ref><ref>{{cite journal | author = Watson NF, Kapur V, Arguelles LM, Goldberg J, Schmidt DF, Armitage R, Buchwald D | title = Comparison of subjective and objective measures of insomnia in monozygotic twins discordant for chronic fatigue syndrome. | journal = Sleep | volume = 26 | issue = 3 | pages = 324-8 | year = 2003 | id = PMID 12749553}}</ref><ref>{{cite journal | author = Van Hoof E, De Becker P, Lapp C, Cluydts R, De Meirleir K | title = Defining the occurrence and influence of alpha-delta sleep in chronic fatigue syndrome. | journal = Am J Med Sci | volume = 333 | issue = 2 | pages = 78-84 | year = 2007 | id = PMID 17301585}}</ref><ref>{{cite journal | author = Ball N, Buchwald DS, Schmidt D, Goldberg J, Ashton S, Armitage R | title = Monozygotic twins discordant for chronic fatigue syndrome: objective measures of sleep. | journal = J Psychosom Res | volume = 56 | issue = 2 | pages = 207-12 | year = 2004 | id = PMID 15016580}}</ref> Sleep may present with vivid disturbing dreams, and exhaustion can worsen sleep dysfunction.<ref name="carr2">"Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Clinical Case Definition and Guidelines for Medical Practitioners - An Overview of the Canadian Consensus Document"; authored by Carruthers and van de Sande; published in 2005, ISBN 0-9739335-0-X, [http://www.mefmaction.net/documents/me_overview.pdf]</ref> |
|||
People with ME/CFS experience persistent debilitating [[fatigue]]. It is made worse by normal physical, mental, emotional, and social activity, and is not a result of ongoing overexertion.<ref name="CDCsym2024" /><ref name="NICE2021" />{{Rp|pages=12}} Rest provides limited relief from fatigue. Particularly in the initial period of illness, this fatigue is described as "flu-like". Individuals may feel "physically drained" and unable to start or finish activities. They may also feel restless while fatigued, describing their experience as "wired but tired". When starting an activity, muscle strength may drop rapidly, which can lead to difficulty with coordination, clumsiness or sudden [[weakness]]. Mental fatigue may also make cognitive efforts difficult.<ref name="NICE2021" />{{Rp|pages=12,57, 95}}<ref>{{Cite journal |last=Jason |first=Leonard |last2=Jessen |first2=Tricia |last3=Porter |first3=Nicole |last4=Boulton |first4=Aaron |last5=Gloria-Njoku |first5=Mary |date=2009-07-16 |title=Examining Types of Fatigue Among Individuals with ME/CFS |url=https://dsq-sds.org/index.php/dsq/article/view/938 |journal=Disability Studies Quarterly |language=en |volume=29 |issue=3 |doi=10.18061/dsq.v29i3.938 |issn=2159-8371|doi-access=free }}</ref><ref>{{Cite journal |last=Jason |first=Leonard A. |last2=Boulton |first2=Aaron |last3=Porter |first3=Nicole S. |last4=Jessen |first4=Tricia |last5=Njoku |first5=Mary Gloria |last6=Friedberg |first6=Fred |date=2010-02-24 |title=Classification of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome by Types of Fatigue |url=http://www.tandfonline.com/doi/abs/10.1080/08964280903521370 |journal=Behavioral Medicine |language=en |volume=36 |issue=1 |pages=24–31 |doi=10.1080/08964280903521370 |issn=0896-4289 |pmc=4852700 |pmid=20185398}}</ref> The fatigue experienced in ME/CFS is of a longer duration and greater severity than in other conditions characterized by fatigue.<ref name="IQWiG-2023" />{{Rp|page=|pages=5–6}} |
|||
The hallmark feature of ME/CFS is a worsening of symptoms after exertion, known as [[post-exertional malaise]] or ''post-exertional symptom exacerbation''.<ref name="pmid37793728" /> PEM involves increased fatigue and is disabling. It can also include flu-like symptoms, pain, cognitive difficulties, gastrointestinal issues, [[nausea]], and sleep problems.<ref name="IQWiG-2023" />{{Rp|page=6}} [[File:Timeframe of PEM from daily activities.jpg|alt=The onset of PEM is usually within two days. Peak PEM occurs within seven, while recovery can take months. |thumb|upright=1.5|Typical time frames of post-exertional malaise after normal daily activities]] All types of activities that require energy, whether physical, cognitive, social, or emotional, can trigger PEM.<ref name="NICE-2021-D" />{{Rp|page=49}} Examples include attending a school event, food shopping, or even taking a shower.<ref name="CDCsym2024" /> For some, being in a stimulating environment can be sufficient to trigger PEM.<ref name="NICE-2021-D" />{{Rp|page=49}} PEM usually starts 12 to 48 hours after the activity,<ref name="CDC_strategies2024">{{cite web |date=10 May 2024 |title=Strategies to Prevent Worsening of Symptoms |url=https://www.cdc.gov/me-cfs/hcp/clinical-care/treating-the-most-disruptive-symptoms-first-and-preventing-worsening-of-symptoms.html |url-status=live |archive-url=https://web.archive.org/web/20240518105522/https://www.cdc.gov/me-cfs/hcp/clinical-care/treating-the-most-disruptive-symptoms-first-and-preventing-worsening-of-symptoms.html |archive-date=18 May 2024 |access-date=18 May 2024 |publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC)}}</ref> but can also follow immediately after. PEM can last hours, days, weeks, or months.<ref name="IQWiG-2023" />{{Rp|page=6}} Extended periods of PEM, commonly referred to as "crashes" or "flare-ups" by people with the illness, can lead to a prolonged relapse.<ref name="NICE-2021-D" />{{Rp|page=50}} |
|||
Unrefreshing sleep is a further core symptom. People wake up exhausted and stiff rather than restored after a night's sleep. This can be caused by a pattern of [[Sleep inversion|sleeping during the day and being awake at night]], shallow sleep, or broken sleep. However, even a full night's sleep is typically non-restorative. Some individuals experience insomnia, [[hypersomnia]] (excessive sleepiness), or vivid nightmares.<ref name="NICE-2021-D"/>{{Rp|page=50}} |
|||
* [[Pain and nociception|Pain]]: Pain is often widespread and migratory in nature, including a significant degree of [[myalgia|muscle pain]] and/or [[arthralgia|joint pain]] (without joint swelling or redness, and may be transitory). Other symptoms include [[headache]]s (particularly of a new type, severity, or duration), [[lymph node]] pain, [[sore throat]]s, and [[abdominal pain]] (often as a symptom of [[irritable bowel syndrome]]). Patients also report bone, eye and [[Orchalgia|testicular pain]], [[neuralgia|nerve pain]] and painful skin sensitivity. [[Chest pain]] has been attributed variously to [[microvascular disease]] or [[cardiomyopathy]] by researchers, and many patients also report painful [[tachycardia]]. A systematic review assessing the studies of chronic pain in CFS found that although the exact prevalence is unknown, it is strongly disabling in patients, but unrelated to depression.<ref name="PMID_16843021">{{cite journal | author = Meeus M, Nijs J, Meirleir KD | title = Chronic musculoskeletal pain in patients with the chronic fatigue syndrome: A systematic review. | journal = Eur J Pain | volume = 11 | issue = 4 | pages = 377-386 | year = 2007 | id = PMID 16843021}}</ref> |
|||
[[Cognitive disorder|Cognitive dysfunction]] in ME/CFS can be as disabling as physical symptoms, leading to difficulties at work or school, as well as in social interactions.<ref name="IQWiG-2023" />{{Rp|page=7}} People with ME/CFS sometimes describe it as "brain fog",<ref name="CDCsym2024" /> and report a slowdown in information processing.<ref name="IQWiG-2023" />{{Rp|page=7}} Individuals may have difficulty speaking, struggling to find words and names. They may have trouble concentrating or [[Human multitasking|multitasking]], or may have difficulties with short-term memory.<ref name="NICE2021" /> Tests often show problems with short-term visual memory, [[Mental chronometry|reaction time]] and [[Reading|reading speed]]. There may also be problems with [[attention]] and [[verbal memory]].<ref name="pmid35140252">{{cite journal |vauthors=Aoun Sebaiti M, Hainselin M, Gounden Y, Sirbu CA, Sekulic S, Lorusso L, Nacul L, Authier FJ |date=February 2022 |title=Systematic Review and Meta-Analysis Of Cognitive Impairment in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) |url=|journal=Scientific Reports |volume=12 |issue=1 |pages=2157 |doi=10.1038/s41598-021-04764-w |pmc=8828740 |pmid=35140252|bibcode=2022NatSR..12.2157A }}</ref> |
|||
* [[Neurological]]/[[cognitive]] manifestations: Common occurrences include [[confusion]], [[forgetfulness]], mental fatigue/[[brain fog]], impairment of concentration and short-term memory consolidation, disorientation, difficulty with information processing, categorizing and word retrieval, and perceptual and sensory disturbances (e.g. spatial instability and disorientation and inability to focus vision), [[ataxia]] (unsteady and clumsy motion of the limbs or torso), muscle weakness and "twitches". There may also be cognitive or sensory overload (e.g. photophobia and hypersensitivity to noise and/or emotional overload, which may lead to "crash" periods and/or anxiety). A review of research relating to the neuropsychological functioning in CFS was published in 2001 and found that slowed processing speed, impaired working memory and poor learning of information are the most prominent features of cognitive dysfunctioning in patients with CFS, which couldn't be accounted solely by the severity of the depression and anxiety.<ref>{{cite journal | author = Michiels V, Cluydts R | title = Neuropsychological functioning in chronic fatigue syndrome: a review. | journal = Acta Psychiatr Scand | volume = 103 | issue = 2 | pages = 84-93 | year = 2001 | id = PMID 11167310}}</ref> |
|||
People with ME/CFS often experience [[orthostatic intolerance]], symptoms that start or worsen with standing or sitting. Symptoms, which include nausea, lightheadedness, and cognitive impairment, often improve again after lying down.<ref name="Bateman-2021" /> Weakness and vision changes may also be triggered by the upright posture.<ref name="CDCsym2024" /> Some have [[postural orthostatic tachycardia syndrome]] (POTS), an excessive increase in [[heart rate]] after standing up, which can result in [[Syncope (medicine)|fainting]].<ref name="IQWiG-2023" />{{Rp|page=7}} Additionally, individuals may experience [[orthostatic hypotension]], a drop in blood pressure after standing.<ref name="BMJbest_practice3" />{{Rp|page=17}} |
|||
* [[Autonomic nervous system|Autonomic]] manifestations: Common occurrences include [[orthostatic intolerance]], neurally mediated [[hypotension]] (NMH), [[postural orthostatic tachycardia syndrome]] (POTS), delayed postural [[hypotension]], [[lightheadedness]], extreme [[pallor]], [[nausea]] and [[irritable bowel syndrome]], urinary frequency and bladder dysfunction, [[palpitation]]s with or without [[cardiac arrhythmia]]s, and exertional [[dyspnea]] (perceived difficulty breathing or pain on breathing). |
|||
=== Other common symptoms === |
|||
* [[Neuroendocrine]] manifestations: Common occurrences include poor [[thermoregulation|temperature control]] or loss of thermostatic stability, subnormal body temperature and marked daily fluctuation, sweating episodes, recurrent feelings of feverishness and cold extremities, intolerance of extremes of heat and cold, digestive disturbances<ref>{{cite journal | author = Burnet RB, Chatterton BE | title = Gastric emptying is slow in chronic fatigue syndrome. | journal = BMC Gastroenterol | volume = 4 | pages = 32 | year = 2004 | id = PMID 15619332 | doi: 10.1186/1471-230X-4-32}}</ref> and/or marked weight change - anorexia or abnormal appetite, loss of adaptability and worsening of symptoms with stress. |
|||
Pain and [[hyperalgesia]] (an abnormally increased sensitivity to pain) are common in ME/CFS. The pain is not accompanied by swelling or redness.<ref name="BMJbest_practice3" />{{Rp|page=16}} The pain can be present in muscles ([[myalgia]]) and [[arthralgia|joints]]. Individuals with ME/CFS may have chronic pain behind the eyes and in the neck, as well as [[neuropathic pain]] (related to disorders of the nervous system).<ref name="IQWiG-2023" />{{Rp|page=8}} Headaches and [[migraine]]s that were not present before the illness can occur as well. However, chronic daily headaches may indicate an alternative diagnosis.<ref name="BMJbest_practice3" />{{Rp|page=16}} |
|||
Additional common symptoms include [[irritable bowel syndrome]] or other problems with digestion, chills and [[night sweats]], [[shortness of breath]] or an [[Arrhythmia|irregular heartbeat]]. Some experience sore [[lymph node]]s and a sore throat. People may also develop allergies or become sensitive to foods, lights, noise, smells or chemicals.<ref name="CDCsym2024" /> |
|||
* [[Immune]] manifestations: Common occurrences include tender lymph nodes, recurrent sore throat, recurrent flu-like symptoms, general malaise, new sensitivities to food and/or medications and/or chemicals (which may complicate treatment). At least one study has confirmed that most CFS patients reduce or cease alcohol intake, mostly due to personal experience of worsening symptoms<ref>{{cite journal | author = Woolley J, Allen R, Wessely S | title = Alcohol use in chronic fatigue syndrome. | journal = J Psychosom Res | volume = 56 | issue = 2 | pages = 203-6 | year = 2004 | id = PMID 15016579}}</ref> (although the cause of this is unknown and may not be strictly "immunological" as implied by the symptom list). |
|||
== Illness severity == |
|||
===Activity levels=== |
|||
ME/CFS often leads to serious disability, but the degree varies considerably.<ref name="CDC_Clinical2024">{{cite web |date=10 May 2024 |title=Clinical Overview of ME/CFS |url=https://www.cdc.gov/me-cfs/hcp/clinical-overview/ |url-status=live |archive-url=https://web.archive.org/web/20240517192407/https://www.cdc.gov/me-cfs/hcp/clinical-overview/ |archive-date=17 May 2024 |access-date=17 May 2024 |publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC)}}</ref> ME/CFS is generally classified into four categories of illness severity:<ref name="NICE2021"/>{{Rp|page=8}}<ref name="BMJbest_practice3">{{Cite book |url=https://bestpractice.bmj.com/topics/en-gb/277 |title=BMJ Best Practice: Myalgic Encephalomyelitis (Chronic Fatigue Syndrome) |vauthors=Baraniuk JN, Marshall-Gradisnik S, Eaton-Fitch N |date=January 2024 |publisher=[[BMJ (company)|BMJ Publishing Group]] |access-date=19 January 2024 |url-access=subscription |archive-url=https://web.archive.org/web/20240219120522/https://auth.bmj.com/as/authorization.oauth2?response_type=code&client_id=bmj-bp-client-id&scope=openid%20profile%20bmj_access%20bmj_id&state=ENbX8qK-k7MG_rSrufgtPvjK66pOSygEI5Vm7b_AQQY%3D&redirect_uri=https://bestpractice.bmj.com/login/oauth2/code/bp-client&code_challenge_method=S256&nonce=drW8TQUhsuIuiLIEvrg4WXsMERFsV9emHb-7Yg-SYrQ&code_challenge=Hldf9BnRpXVwaG1wsQNJwmn_zWe8bfqpbf0uUZK8emA&template_name=UNKNOWN_USER&ip=207.241.225.241&acr_values=USER_LOGIN |archive-date=19 February 2024 |url-status=live}}</ref>{{Rp|page=10}} |
|||
Patients report critical reductions in levels of physical activity<ref name="PMID_8771284">{{cite journal | author = McCully KK, Sisto SA, Natelson BH | title = Use of exercise for treatment of chronic fatigue syndrome. | journal = Sports Med | volume = 21 | issue = 1 | pages = 35-48 | year = 1996 | id = PMID 8771284}}</ref> and are as impaired as persons whose fatigue can be explained by another medical or a psychiatric condition.<ref name="PMID_14577835">{{cite journal | author = Solomon L, Nisenbaum R, Reyes M, Papanicolaou DA, Reeves WC | title = Functional status of persons with chronic fatigue syndrome in the Wichita, Kansas, population. | journal = Health Qual Life Outcomes | volume = 1 | issue = 1 | pages = 48 | year = 2003 | id = PMID 14577835 | url = http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=14577835}}</ref> According to the CDC, studies show that the disability in CFS patients is comparable to some well-known, very severe medical conditions, such as; [[multiple sclerosis]], [[AIDS]], [[lupus]], [[rheumatoid arthritis]], [[heart disease]], end-stage [[renal disease]], [[chronic obstructive pulmonary disease]] (COPD) and similar chronic conditions.<ref>[http://www.cdc.gov/od/oc/media/transcripts/t061103.htm?id=36410] Press Conference: The Chronic Fatigue and Immune Dysfunction Syndrome Association of America and The Centers For Disease Control and Prevention Press Conference at The National Press Club to Launch a Chronic Fatigue Syndrome Awareness Campaign - [[November 3]] [[2006]], 10 a.m. ET</ref><ref>[http://www.cdc.gov/cfs/cfssymptomsHCP.htm] The Centers For Disease Control and Prevention (website): Chronic Fatigue Syndrome > For Healthcare Professionals > Symptoms > Clinical Course</ref> The severity of symptoms and disability is the same in both genders<ref>{{cite journal | author = Ho-Yen DO, McNamara I | title = General practitioners' experience of the chronic fatigue syndrome | journal = Br J Gen Pract | volume = 41 | issue = 349 | pages = 324-6 | year = 1991 | id = PMID 1777276}}</ref>, and chronic pain is strongly disabling in CFS patients<ref name="PMID_16843021"> </ref>, but despite a common diagnosis the functional capacity of CFS patients varies greatly.<ref name="PMID_12783037">{{cite journal | author = Vanness JM, Snell CR, Strayer DR, Dempsey L 4th, Stevens SR | title = Subclassifying chronic fatigue syndrome through exercise testing. | journal = Med Sci Sports Exerc | volume = 35 | issue = 6 | pages = 908-13 | year = 2003 | id = PMID 12783037}}</ref> While some patients are able to lead a relatively normal life, others are totally bed-bound and unable to care for themselves. A systematic review found that in a synthesis of studies, 42% of patients were employed, 54% were unemployed, 64% reported CFS-related work limitations, 55% were on disability benefits or temporary sick leave, and 19% worked full-time.<ref>{{cite journal | author = Ross SD, Estok RP, Frame D, Stone LR, Ludensky V, Levine CB | title = Disability and chronic fatigue syndrome: a focus on function. | journal = Arch Intern Med | volume = 164 | issue = 10 | pages = 1098-107 | year = 2004 | id = PMID 15159267 | url = http://archinte.ama-assn.org/cgi/content/full/164/10/1098}}</ref> |
|||
* People with mild ME/CFS can usually still work and care for themselves, but they will need their free time to recover from these activities rather than engage in social and leisure activities. |
|||
* Moderate severity impedes [[activities of daily living]] (self-care activities, such as making a meal). People are usually unable to work and require frequent rest. |
|||
* Those with severe ME/CFS are homebound and can do only limited activities of daily living, for instance brushing their teeth. They may be wheelchair-dependent and spend the majority of their time in bed. |
|||
* With very severe ME/CFS, people are mostly bed-bound and cannot care for themselves. |
|||
[[File:QoL comparison ME-CFS.svg|thumb|upright=1.4|Results of a study on the [[quality of life]] of individuals with ME/CFS, showing it to be lower than in 20 other chronic conditions|alt=A bar graph showing the average quality of life score of those with ME/CFS.]] |
|||
==Proposed causes and pathophysiology== |
|||
Roughly a quarter of those living with ME/CFS fall into the mild category, and half fall into the moderate or moderate-to-severe categories.<ref name="pmid37793728">{{cite journal |vauthors=Grach SL, Seltzer J, Chon TY, Ganesh R |date=October 2023 |title=Diagnosis and Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome |journal=Mayo Clinic Proceedings |volume=98 |issue=10 |pages=1544–1551 |doi=10.1016/j.mayocp.2023.07.032 |pmid=37793728 |s2cid=263665180 |doi-access=free}}</ref> The final quarter falls into the severe or very severe category.<ref name="IQWiG-2023" />{{Rp|3}} Severity may change over time. Symptoms might get worse, improve, or the illness may go into remission for a period of time.<ref name="CDC_Clinical2024"/> People who feel better for a period of time may overextend their activities, triggering PEM and a worsening of symptoms.<ref name="CDC_strategies2024"/> |
|||
The cause of CFS is unknown, although a large number of causes have been proposed. In a basic overview of CFS for health professionals, the CDC states that "''After more than 3,000 research studies, there is now abundant scientific evidence that CFS is a real physiological illness.''"<ref>[http://www.cdc.gov/cfs/pdf/Basic_Overview.pdf CDC - CFS Basic Overview] (PDF file, 31 KB)</ref> The cause of CFS may be different for different patients, but if so, the various causes may result in a common clinical outcome. |
|||
Those with severe and very severe ME/CFS experience more extreme and diverse symptoms. They may face severe weakness and greatly limited ability to move. They can lose the ability to speak, swallow, or communicate completely due to cognitive issues. They can further experience severe pain and hypersensitivities to touch, light, sound, and smells.<ref name="NICE2021"/>{{Rp|pages=50}} Minor day-to-day activities can be sufficient to trigger PEM.<ref name="Bateman-2021" /> |
|||
===Neurological abnormalities=== |
|||
Researchers have found evidence that CFS may involve distinct neurological abnormalities. [[MRI]] and [[SPECT]] scans show abnormalities within the brain.<ref name="pmid8141020">{{cite journal |author=Schwartz RB, Garada BM, Komaroff AL, ''et al'' |title=Detection of intracranial abnormalities in patients with chronic fatigue syndrome: comparison of MR imaging and SPECT |journal=AJR. American journal of roentgenology |volume=162 |issue=4 |pages=935–41 |year=1994 |pmid=8141020 |doi=}}</ref> Studies have shown that CFS patients have abnormalities in blood flow to the brain<ref name="pmid9861623">{{cite journal |author=Abu-Judeh HH, Levine S, Kumar M, ''et al'' |title=Comparison of SPET brain perfusion and 18F-FDG brain metabolism in patients with chronic fatigue syndrome |journal=Nuclear medicine communications |volume=19 |issue=11 |pages=1065–71 |year=1998 |pmid=9861623 |doi=}}</ref> possibly indicative of viral cause<ref name="pmid8141022">{{cite journal |author=Schwartz RB, Komaroff AL, Garada BM, ''et al'' |title=SPECT imaging of the brain: comparison of findings in patients with chronic fatigue syndrome, AIDS dementia complex, and major unipolar depression |journal=AJR. American journal of roentgenology |volume=162 |issue=4 |pages=943–51 |year=1994 |pmid=8141022 |doi=}}</ref> and similar but not identical compared to patients with clinical depression.<ref name="pmid10974961">{{cite journal |author=MacHale SM, Lawŕie SM, Cavanagh JT, ''et al'' |title=Cerebral perfusion in chronic fatigue syndrome and depression |journal=The British journal of psychiatry : the journal of mental science |volume=176 |issue= |pages=550–6 |year=2000 |pmid=10974961 |doi=}}</ref><ref name="pmid9121617">{{cite journal |author=Fischler B, D'Haenen H, Cluydts R, ''et al'' |title=Comparison of 99m Tc HMPAO SPECT scan between chronic fatigue syndrome, major depression and healthy controls: an exploratory study of clinical correlates of regional cerebral blood flow |journal=Neuropsychobiology |volume=34 |issue=4 |pages=175–83 |year=1996 |pmid=9121617 |doi=}}</ref> |
|||
A number of studies have shown that CFS patients have abnormal levels of neurotransmitters including increased [[serotonin]]<ref name="pmid1282370">{{cite journal |author=Demitrack MA, Gold PW, Dale JK, Krahn DD, Kling MA, Straus SE |title=Plasma and cerebrospinal fluid monoamine metabolism in patients with chronic fatigue syndrome: preliminary findings |journal=Biol. Psychiatry |volume=32 |issue=12 |pages=1065–77 |year=1992 |pmid=1282370 |doi=}}</ref><ref name="pmid15982993">{{cite journal |author=Badawy AA, Morgan CJ, Llewelyn MB, Albuquerque SR, Farmer A |title=Heterogeneity of serum tryptophan concentration and availability to the brain in patients with the chronic fatigue syndrome |journal=J. Psychopharmacol. (Oxford) |volume=19 |issue=4 |pages=385–91 |year=2005 |pmid=15982993 |doi=10.1177/0269881105053293}}</ref> (the opposite of what is found in primary depression).<ref name="pmid8550954">{{cite journal |author=Cleare AJ, Bearn J, Allain T, ''et al'' |title=Contrasting neuroendocrine responses in depression and chronic fatigue syndrome |journal=Journal of affective disorders |volume=34 |issue=4 |pages=283–9 |year=1995 |pmid=8550954 |doi=}}</ref> Reduced brain serotonin receptor sensitivity or number,<ref name="pmid15691524">{{cite journal |author=Cleare AJ, Messa C, Rabiner EA, Grasby PM |title=Brain 5-HT1A receptor binding in chronic fatigue syndrome measured using positron emission tomography and [11C]WAY-100635 |journal=Biol. Psychiatry |volume=57 |issue=3 |pages=239–46 |year=2005 |pmid=15691524 |doi=10.1016/j.biopsych.2004.10.031}}</ref> and high auto antibodies to serotonin have also been found.<ref name="pmid9392689">{{cite journal |author=Klein R, Berg PA |title=High incidence of antibodies to 5-hydroxytryptamine, gangliosides and phospholipids in patients with chronic fatigue and fibromyalgia syndrome and their relatives: evidence for a clinical entity of both disorders |journal=Eur. J. Med. Res. |volume=1 |issue=1 |pages=21–6 |year=1995 |pmid=9392689 |doi=}}</ref> Recent studies found altered gene expression in the brain’s serotonin and sympathetic nervous system pathways,<ref name="pmid16610957">{{cite journal |author=Goertzel BN, Pennachin C, de Souza Coelho L, Gurbaxani B, Maloney EM, Jones JF |title=Combinations of single nucleotide polymorphisms in neuroendocrine effector and receptor genes predict chronic fatigue syndrome |journal=Pharmacogenomics |volume=7 |issue=3 |pages=475–83 |year=2006 |pmid=16610957 |doi=10.2217/14622416.7.3.475}}</ref> with altered responses of the HPA axis to serotonin.<ref name="pmid9226729">{{cite journal |author=Dinan TG, Majeed T, Lavelle E, Scott LV, Berti C, Behan P |title=Blunted serotonin-mediated activation of the hypothalamic-pituitary-adrenal axis in chronic fatigue syndrome |journal=Psychoneuroendocrinology |volume=22 |issue=4 |pages=261–7 |year=1997 |pmid=9226729 |doi=}}</ref> Other reported neurotransmitter irregularities include [[glutamate]],<ref name="pmid12414265">{{cite journal |author=Kuratsune H, Yamaguti K, Lindh G, ''et al'' |title=Brain regions involved in fatigue sensation: reduced acetylcarnitine uptake into the brain |journal=Neuroimage |volume=17 |issue=3 |pages=1256–65 |year=2002 |pmid=12414265 |doi=}}</ref> [[acetylcholine]] sensitivity associated increased cutaneous microcirculation,<ref name="pmid15041034">{{cite journal |author=Spence VA, Khan F, Kennedy G, Abbot NC, Belch JJ |title=Acetylcholine mediated vasodilatation in the microcirculation of patients with chronic fatigue syndrome |journal=Prostaglandins Leukot. Essent. Fatty Acids |volume=70 |issue=4 |pages=403–7 |year=2004 |pmid=15041034 |doi=10.1016/j.plefa.2003.12.016}}</ref> and autoantibodies to cholinergic receptors associated with central pain.<ref name="pmid12851722">{{cite journal |author=Tanaka S, Kuratsune H, Hidaka Y, ''et al'' |title=Autoantibodies against muscarinic cholinergic receptor in chronic fatigue syndrome |journal=Int. J. Mol. Med. |volume=12 |issue=2 |pages=225–30 |year=2003 |pmid=12851722 |doi=}}</ref> [[Beta-endorphin]], a natural pain killer, has been found to be low in CFS patients, the opposite of what is found in primary depression.<ref name="pmid9844768">{{cite journal |author=Conti F, Pittoni V, Sacerdote P, Priori R, Meroni PL, Valesini G |title=Decreased immunoreactive beta-endorphin in mononuclear leucocytes from patients with chronic fatigue syndrome |journal=Clin. Exp. Rheumatol. |volume=16 |issue=6 |pages=729–32 |year=1998 |pmid=9844768 |doi=}}</ref><ref name="pmid12131069">{{cite journal |author=Panerai AE, Vecchiet J, Panzeri P, ''et al'' |title=Peripheral blood mononuclear cell beta-endorphin concentration is decreased in chronic fatigue syndrome and fibromyalgia but not in depression: preliminary report |journal=The Clinical journal of pain |volume=18 |issue=4 |pages=270–3 |year=2002 |pmid=12131069 |doi=}}</ref> |
|||
Individuals with ME/CFS have decreased quality of life when evaluated by the [[SF-36]] questionnaire, especially in the domains of physical and social functioning, general health, and vitality. However, their emotional functioning and mental health are not much lower than those of healthy individuals.<ref name="pmid28033311">{{cite journal |vauthors=Unger ER, Lin JS, Brimmer DJ, Lapp CW, Komaroff AL, Nath A, Laird S, Iskander J |date=December 2016 |title=CDC Grand Rounds: Chronic Fatigue Syndrome – Advancing Research and Clinical Education |url=https://www.cdc.gov/mmwr/volumes/65/wr/pdfs/mm655051a4.pdf |url-status=live |journal=MMWR. Morbidity and Mortality Weekly Report |volume=65 |issue=50–51 |pages=1434–1438 |doi=10.15585/mmwr.mm655051a4 |pmid=28033311 |archive-url=https://web.archive.org/web/20170106010408/https://www.cdc.gov/mmwr/volumes/65/wr/pdfs/mm655051a4.pdf |archive-date=6 January 2017 |access-date=5 January 2017 |quote= |doi-access=free |title-link=doi}}</ref> Functional impairment in ME/CFS can be greater than [[multiple sclerosis]], [[Cardiovascular disease|heart disease]], or [[lung cancer]].<ref name="Bateman-2021" /> Fewer than half of people with ME/CFS are employed, and roughly one in five have a full-time job.<ref name="Lim2020" /> |
|||
;Dysautonomia |
|||
[[Dysautonomia]] is the disruption of the function of the [[autonomic nervous system]] (ANS). The ANS controls many aspects of [[homeostasis]]. The dysautonomia that evidences itself in CFS shows up mostly in problems of [[orthostatic intolerance]] - the inability to stand up without feeling dizzy, faint, nauseated, etc{{Fact|date=January 2008}}. Research into the orthostatic intolerance found in CFS indicates it is very similar to that found in [[postural orthostatic tachycardia syndrome]] (POTS){{Fact|date=January 2008}}. POTS and CFS patients exhibit reduced blood flows to the heart upon standing that result in reduced blood flow to the brain. The reduced blood flows to the heart are believed to originate in blood pooling in the lower body upon standing. Many CFS patients report symptoms of orthostatic intolerance and low or lowered blood pressure.<ref>{{cite journal |author=Newton JL, Okonkwo O, Sutcliffe K, Seth A, Shin J, Jones DE |title=Symptoms of autonomic dysfunction in chronic fatigue syndrome |journal=QJM |volume=100 |issue=8 |pages=519-26 |year=2007 |pmid=17617647 |doi=10.1093/qjmed/hcm057}}</ref> |
|||
== Causes == |
|||
;Inner-ear disorders |
|||
The cause of ME/CFS is not yet known.<ref name="Bateman-2021" /> Between 60% and 80% of cases start after an infection, usually a viral infection.<ref name="BMJbest_practice3" />{{rp|5}}<ref name="pmid37793728" /> A genetic factor is believed to contribute, but there is no single gene known to be responsible for increased risk. Instead, many gene variants probably have a small individual effect, but their combined effect can be strong.<ref name="Dibble McGrath Ponting 2020 p." /> Other factors may include problems with the nervous and immune systems, as well as energy metabolism.<ref name="Bateman-2021" /> ME/CFS is a biological disease, not a psychological condition,<ref name="pmid28033311" /><ref name="CDC_Clinical2024" /> and is not due to [[deconditioning]].<ref name="pmid28033311" /><ref name="Bateman-2021" /> |
|||
{{main|balance disorder}} |
|||
Besides viruses, other reported triggers include stress, traumatic events, and environmental exposures such as to [[Mold|mould]].<ref name="IQWiG-2023" />{{Rp|page=21}} Bacterial infections such as [[Q fever|Q-fever]] are other potential triggers.<ref name="BMJbest_practice3" />{{rp|5}} ME/CFS may further occur after physical trauma, such as an accident or surgery.<ref name="CDC_Clinical2024" /> Pregnancy has been reported in around 3% to 10% of cases as a trigger.<ref name="pmid37234076">{{cite journal |vauthors=Pollack B, von Saltza E, McCorkell L, Santos L, Hultman A, Cohen AK, Soares L |date=2023 |title=Female Reproductive Health Impacts of Long COVID and Associated Illnesses Including ME/CFS, POTS, And Connective Tissue Disorders: A Literature Review |url=|journal=Frontiers in Rehabilitation Sciences |volume=4 |issue= |pages=1122673 |doi=10.3389/fresc.2023.1122673 |doi-access=free |pmc=10208411 |pmid=37234076}}</ref> ME/CFS can also begin with multiple minor triggering events, followed by a final trigger that leads to a clear onset of symptoms.<ref name="pmid37793728" /> |
|||
Problems such as [[Meniere's]], [[tumor]] in the inner ear, {{Fact|date=May 2007}} or [[Benign Paroxysmal Positional Vertigo]] (BPPV) can cause dizziness, [[vertigo (medical)|vertigo]], and fatigue. Recurrent [[ear infection]]s are common in some CFS sufferers{{Fact|date=January 2008}}. [[Tinnitus]] is also quite common.<ref name="isbn0-9695662-0-4">{{cite book |author=Byron M. Hyde |title=The Clinical and scientific basis of myalgic encephalomyelitis/chronic fatigue syndrome |publisher=Nightingale Research Foundation |location=Ogdensburg, N.Y |year=1992 |pages= |isbn=0-9695662-0-4 |oclc= |doi=}}</ref> Antibodies associated with hearing loss have been found in CFS and FMS patients with inner ear disorders <ref name="pmid9677490">{{cite journal |author=Heller U, Becker EW, Zenner HP, Berg PA |title=[Incidence and clinical relevance of antibodies to phospholipids, serotonin and ganglioside in patients with sudden deafness and progressive inner ear hearing loss] |language=German |journal=HNO |volume=46 |issue=6 |pages=583-6 |year=1998 |pmid=9677490 |doi=}}</ref> |
|||
=== Risk factors === |
|||
;Orthostatic hypotension |
|||
ME/CFS can affect people of all ages, ethnicities, and income levels, but it is more common in women than men.<ref name="Lim2020" /> People with a history of frequent infections are more likely to develop it.<ref name="pmid38443223" /> Those with family members who have ME/CFS are also at higher risk, suggesting a genetic factor.<ref name="Dibble McGrath Ponting 2020 p." /> In the United States, [[white Americans]] are diagnosed more frequently than other groups,<ref name="CDC_Basics">{{Cite web |date=10 May 2024 |title=ME/CFS Basics |url=https://www.cdc.gov/me-cfs/about/index.html |archive-url=https://web.archive.org/web/20240523214910/https://www.cdc.gov/me-cfs/about/index.html |archive-date=23 May 2024 |access-date=25 May 2024 |publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC) |language=en-us}}</ref> but the illness is probably at least as prevalent among African Americans and Hispanics.<ref name="CDCEpide2023">{{cite web |date=21 March 2023 |title=Epidemiology |url=https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/epidemiology.html |url-status=dead |archive-url=https://web.archive.org/web/20240306031847/https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/epidemiology.html |archive-date=6 March 2024 |access-date=13 April 2024 |publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC)}}</ref> It used to be thought that ME/CFS was more common among those with higher incomes. Instead, people in minority groups or lower income groups may have increased risks due to poorer nutrition, lower healthcare access, and increased work stress.<ref name="Lim2020" /> |
|||
Syndromes of [[orthostatic intolerance]], in particular [[neurally mediated hypotension]] (NMH) and [[postural orthostatic tachycardia syndrome]] (POTS), have been shown to be associated with chronic fatigue syndrome.<ref>Tolan R, Stewart J. [http://www.emedicine.com/ped/topic2795.htm "Chronic Fatigue Syndrome"], ''eMedicine'', [[August 17]] [[2006]], retrieved [[November 9]] [[2006]].</ref><ref> Rowe, PC. [http://www.pediatricnetwork.org/medical/OI/johnshopkins.htm "General Information Brochure on Orthostatic Intolerance and its Treatment"], ''Chronic Fatigue Clinic, Johns Hopkins Children's Center'', February 2003, retrieved [[November 9]] [[2006]].</ref> These conditions, which reduce blood flow to the brain after periods of standing, can be diagnosed with a [[tilt table test]]. A clinical trial of [[fludrocortisone]], a drug sometimes used to treat low blood pressure, showed little or no benefit for people with CFS.<ref>{{cite journal |author=Rowe P, Calkins H, DeBusk K, McKenzie R, Anand R, Sharma G, Cuccherini B, Soto N, Hohman P, Snader S, Lucas K, Wolff M, Straus S |title=Fludrocortisone acetate to treat neurally mediated hypotension in chronic fatigue syndrome: a randomized controlled trial |journal=JAMA |volume=285 |issue=1 |pages=52-9 |year=2001 |pmid=11150109}}</ref> |
|||
=== Viral infections === |
|||
===Psychiatric abnormalities=== |
|||
{{main|Post-acute infection syndrome}} |
|||
;Depression |
|||
There is some overlap in symptoms between depression and CFS, and sometimes cases of CFS are mistakenly attributed to [[clinical depression]]. There are, however, many clinical differences between the two<ref name="Stein">Stein E (2001), "How to differentiate CFS from Psychiatric Disorder", Presented at The Alison Hunter Memorial Foundation Third International Clinical and Scientific Conference, Sydney, Australia</ref>. |
|||
Viral infections have long been suspected to cause ME/CFS, based on the observation that ME/CFS sometimes occurs in outbreaks and is possibly connected to [[autoimmune disease]]s.<ref name="pmid37898798">{{cite journal |vauthors=Hwang JH, Lee JS, Oh HM, Lee EJ, Lim EJ, Son CG |date=October 2023 |title=Evaluation of Viral Infection as an Etiology of ME/CFS: A Systematic Review and Meta-Analysis |url=|journal=Journal of Translational Medicine |volume=21 |issue=1 |pages=763 |doi=10.1186/s12967-023-04635-0 |doi-access=free |pmc=10612276 |pmid=37898798}}</ref> How viral infections cause ME/CFS is unclear; it could be via [[Virus latency|viral persistence]] or via a "hit and run" mechanism, in which infections dysregulate the immune system or cause autoimmunity.<ref name="pmid30285773">{{cite journal |vauthors=Rasa S, Nora-Krukle Z, Henning N, Eliassen E, Shikova E, Harrer T, Scheibenbogen C, Murovska M, Prusty BK |date=October 2018 |title=Chronic Viral Infections in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) |url=|journal=Journal of Translational Medicine |volume=16 |issue=1 |pages=268 |doi=10.1186/s12967-018-1644-y |doi-access=free |pmc=6167797 |pmid=30285773}}</ref> |
|||
Clinical depression often responds well to physical exercise, whereas CFS is characterised by exercise intolerance but with a willingness to be active. (See section on [[#Post-exertion symptom exacerbation|post-exertion symptom exacerbation]].) |
|||
Comorbid depression occurs in 10-15% of CFS patients and should be treated as usual, except that the patient’s energy level, cognitive dysfunction and drug sensitivity must be taken into account<ref name="Stein" />. Comorbid depression may be a pre-existing condition, or the result of living with CFS. |
|||
Different types of viral infection have been implicated in ME/CFS, including airway infections, [[bronchitis]], [[gastroenteritis]], or an acute "flu-like illness".<ref name="IQWiG-2023" />{{Rp|page=226}} Between 15% and 50% of people with [[long COVID]] also meet the diagnostic criteria for ME/CFS.<ref name="IQWiG-2023" />{{Rp|page=228}} Of people who get [[infectious mononucleosis]], which is caused by the [[Epstein–Barr virus]] (EBV), around 8% to 15% develop ME/CFS, depending on criteria.<ref name="IQWiG-2023" />{{Rp|page=226}} Other viral infections that can trigger ME/CFS are the [[Influenza A virus subtype H1N1|H1N1 influenza virus]], [[Varicella zoster virus|varicella zoster]] (the virus that causes [[chickenpox]] and [[shingles]]), and [[SARS-CoV-1]].<ref name="pmid37433988">{{cite journal |vauthors=Altmann DM, Whettlock EM, Liu S, Arachchillage DJ, Boyton RJ |date=October 2023 |title=The Immunology of Long COVID |journal=Nature Reviews. Immunology |volume=23 |issue=10 |pages=618–634 |doi=10.1038/s41577-023-00904-7 |pmid=37433988 |s2cid=259831825 |doi-access=free}}</ref> |
|||
===Stress and trauma=== |
|||
The majority of people who experience stress/trauma do not develop CFS, but these factors (including infection) increase the likelihood of acquiring CFS within one year<ref name="PMID_9201648">{{cite journal | author = Salit IE | title = Precipitating factors for the chronic fatigue syndrome. | journal = J Psychiatr Res | volume = 31 | issue = 1 | pages = 59-65 | year = 1997 | id = PMID 9201648}}</ref><ref name="PMID_10367610">{{cite journal | author = Theorell T, Blomkvist V, Lindh G, Evengard B | title = Critical life events, infections, and symptoms during the year preceding chronic fatigue syndrome (CFS): an examination of CFS patients and subjects with a nonspecific life crisis. | journal = Psychosom Med. | volume = 61 | issue = 3 | pages = 304-10 | id = PMID 10367610}}</ref> and a genetic disposition to CFS has been demonstrated. Two studies suggest that self-reported childhood stress/trauma significantly increases the likelihood of acquiring CFS as an adult: A preliminary study found a 3 to 8 fold increase (depending on the trauma type).<ref>{{cite journal | author = Heim C, Wagner D, Maloney E, Papanicolaou DA, Solomon L, Jones JF, Unger ER, Reeves WC | title = Early adverse experience and risk for chronic fatigue syndrome: results from a population-based study. | journal = Arch Gen Psychiatry | volume = 63 | issue = 11 | pages = 1258-66 | year = 2006 | id = PMID 17088506}}</ref> A study involving participants from the Swedish Twin Registry found that in matched case-control analyses, higher emotional instability and self-reported stress were significant risk factors (odds ratios, 1.72 and 1.64, respectively), while in co-twin control analyses the risk of emotional instability decreased to 1.02 whereas that of stress increased to 5.81 (suggesting genetic influences); there was also no association between [[Extraversion and introversion|extraversion]] and fatigue.<ref>{{cite journal | author = Kato K, Sullivan PF, Evengard B, Pedersen NL | title = Premorbid predictors of chronic fatigue. | journal = Arch Gen Psychiatry | volume = 63 | issue = 11 | pages = 1267-72 | year = 2006 | id = PMID 17088507 | url = http://archpsyc.ama-assn.org/cgi/content/full/63/11/1267}}</ref> Anxiety disorders have been associated with CFS in 5-15 year olds.<ref name="DOI_10.1136/bmj.327.7416.654">{{cite journal | author = T Chalder, R Goodman, S Wessely, M Hotopf, H Meltzer | title = Epidemiology of chronic fatigue syndrome and self reported myalgic encephalomyelitis in 5-15 year olds: cross sectional study. | journal = BMJ | volume = 327 | pages = 654-655 | year = 2003 | id = DOI 10.1136/bmj.327.7416.654 | url = http://www.bmj.com/cgi/content/full/327/7416/654}}</ref> |
|||
Reactivation of latent viruses, in particular EBV and [[human herpesvirus 6]], has also been hypothesised to drive symptoms. EBV is present in about 90% of people, usually in a latent state.<ref name="pmid37718435">{{cite journal |vauthors=Ruiz-Pablos M, Paiva B, Zabaleta A |date=September 2023 |title=Epstein-Barr Virus-Acquired Immunodeficiency in Myalgic encephalomyelitis-Is It Present in Long COVID? |url=|journal=Journal of Translational Medicine |volume=21 |issue=1 |pages=633 |doi=10.1186/s12967-023-04515-7 |doi-access=free |pmc=10506247 |pmid=37718435}}</ref><ref>{{Cite report |url=https://www.ninds.nih.gov/sites/default/files/2024-05/Report%20of%20the%20MECFS%20Research%20Roadmap%20Working%20Group%20of%20Council_508C.pdf |title=Report of the ME/CFS Research Roadmap Working Group of Council | vauthors = Bateman L, Hanson M |date=15 May 2024 |publisher=[[National Institutes of Health]] (NIH) |access-date=25 May 2024 |archive-url=https://web.archive.org/web/20240522195146/https://www.ninds.nih.gov/sites/default/files/2024-05/Report%20of%20the%20MECFS%20Research%20Roadmap%20Working%20Group%20of%20Council_508C.pdf |archive-date=22 May 2024 |url-status=live}}</ref>{{Rp|page=13}} The levels of [[Antibody|antibodies]] to EBV are commonly higher in people with ME/CFS, indicating possible viral reactivation.<ref name="Eriksen">{{cite journal |vauthors=Eriksen W |date=16 August 2018 |title=ME/CFS, Case Definition, And Serological Response to Epstein–Barr Virus. A Systematic Literature Review |journal=Fatigue: Biomedicine, Health & Behavior |volume=6 |issue=4 |pages=220–34 |doi=10.1080/21641846.2018.1503125 |s2cid=80898744 |quote=}}</ref> |
|||
The CDC stated in 2006, their studies found gene mutation and abnormal gene activity levels in CFS patients that relate to the function of the hypothalamus-pituitary-adrenal (HPA) axis, which helps regulate the body's stress response.<ref name="CDC April 20 2006">{{cite web | last = Reeves W | coauthors = Vernon S | title = Press Briefing on Chronic Fatigue Syndrome | publisher = Centers for Disease Control and Prevention | date = April 20, 2006 | url = http://www.cdc.gov/od/oc/media/transcripts/t060420.htm | format = HTM | accessdate = 2008-01-27}}</ref> Earlier CFS research also found evidence that suggested abnormal stress response was associated with subtle dysfunction of the HPA axis. Questions remain about the pathophysiology of these findings.<ref>{{cite journal | author = Roberts AD, Wessely S, Chalder T, Papadopoulos A, Cleare AJ | title = Salivary cortisol response to awakening in chronic fatigue syndrome. | journal = Br J Psychiatry | volume = 184 | pages = 136-41 | year = 2004 | id = PMID 14754825}}</ref><ref>{{cite journal | author = Gaab J, Huster D, Peisen R, Engert V, Heitz V, Schad T, Schurmeyer TH, Ehlert U | title = Hypothalamic-pituitary-adrenal axis reactivity in chronic fatigue syndrome and health under psychological, physiological, and pharmacological stimulation. | journal = Psychosom Med | volume = 64 | issue = 6 | pages = 951-62 | year = 2002 | id = PMID 12461200}}</ref><ref>{{cite journal | author = Gaab J, Engert V, Heitz V, Schad T, Schurmeyer TH, Ehlert U | title = Associations between neuroendocrine responses to the Insulin Tolerance Test and patient characteristics in chronic fatigue syndrome. | journal = J Psychosom Res | volume = 56 | issue = 4 | pages = 419-24 | year = 2004 | id = PMID 15094026}}</ref> The controversy surrounding CFS has caused some social issues for patients and may contribute to their stress (see the [[Chronic fatigue syndrome#Social issues|Social issues]] section). |
|||
== Pathophysiology == |
|||
===Oxidative stress=== |
|||
ME/CFS is associated with changes in several areas, including the nervous and immune systems, as well as disturbances in energy metabolism.<ref name="CDC_Clinical2024" /><ref name="pmid38443223" /> Neurological differences include [[autonomic nervous system]] dysfunction and a change in brain structure and [[metabolism]].<ref name="Maksoud2020">{{cite journal |vauthors=Maksoud R, du Preez S, Eaton-Fitch N, Thapaliya K, Barnden L, Cabanas H, Staines D, Marshall-Gradisnik S |date=2020 |title=A Systematic Review of Neurological Impairments in Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome Using Neuroimaging Techniques |journal=PLOS ONE |volume=15 |issue=4 |pages=e0232475 |bibcode=2020PLoSO..1532475M |doi=10.1371/journal.pone.0232475 |pmc=7192498 |pmid=32353033 |doi-access=free |title-link=doi}}</ref> Observed changes in the [[immune system]] include decreased [[natural killer cell]] function and, in some cases, [[autoimmunity]].<ref name="pmid38443223" /> |
|||
[[Oxidative stress]] is an imbalance between the production of reactive oxygen and a biological system's ability to readily detoxify the reactive intermediates or easily repair the resulting damage. Several studies<ref>{{cite journal | author = Kennedy G, Spence VA, McLaren M, Hill A, Underwood C, Belch JJ | title = Oxidative stress levels are raised in CFS and are associated with clinical symptoms. | journal = Free Radic Biol Med | volume = 39 | issue = 5 | pages = 584-9 | year = 2005 | id = PMID 16085177}}</ref><ref>{{cite journal | author = Jammes Y, Steinberg JG, Mambrini O, Bregeon F, Delliaux S | title = Chronic fatigue syndrome: assessment of increased oxidative stress and altered muscle excitability in response to incremental exercise. | journal = J Intern Med | volume = 257 | issue = 3 | pages = 299-310 | year = 2005 | id = PMID 15715687}}</ref><ref>{{cite journal | author = Richards RS, Wang L, Jelinek H | title = Erythrocyte oxidative damage in chronic fatigue syndrome. | journal = Arch Med Res | volume = 38 | issue = 1 | pages = 94-8 | year = 2007 | id = PMID 17174731}}</ref><ref>{{cite journal | author = Vecchiet J, Cipollone F, Falasca K, Mezzetti A, Pizzigallo E, Bucciarelli T, De Laurentis S, Affaitati G, De Cesare D, Giamberardino MA | title = Relationship between musculoskeletal symptoms and blood markers of oxidative stress in patients with chronic fatigue syndrome. | journal = Neurosci Lett | volume = 335 | issue = 3 | pages = 151-4 | year = 2003 | id = PMID 12531455}}</ref><ref>{{cite journal | author = Fulle S, Mecocci P, Fano G, Vecchiet I, Vecchini A, Racciotti D, Cherubini A, Pizzigallo E, Vecchiet L, Senin U, Beal MF | title = Specific oxidative alterations in vastus lateralis muscle of patients with the diagnosis of chronic fatigue syndrome. | journal = Free Radic Biol Med | volume = 29 | issue = 12 | pages = 1252-9 | year = 2000 | id = PMID 11118815}}</ref><ref>{{cite journal | author = Richards RS, Roberts TK, McGregor NR, Dunstan RH, Butt HL | title = Blood parameters indicative of oxidative stress are associated with symptom expression in chronic fatigue syndrome. | journal = Redox Rep | volume = 5 | issue = 1 | pages = 35-41 | year = 2000 | id = PMID 10905542}}</ref> and a review<ref>{{cite journal | author = Nijs J, Meeus M, De Meirleir K | title = Chronic musculoskeletal pain in chronic fatigue syndrome: recent developments and therapeutic implications. | journal = Man Ther | volume = 11 | issue = 3 | pages = 187-91 | year = 2006 | id = PMID 16781183}}</ref> have implicated oxidative stress in CFS symptoms; especially relating to fatigue, pain and postexertional malaise/exercise intolerance. According to research, the findings on oxidative stress and nitrosative stress ([[nitric oxide]]-related toxicity); are associated with an inflammatory response, seem consistent with abnormal 2-5A synthetase/[[RNase L]] enzyme (antiviral) activity and involves an immune response, against disrupted [[lipid membrane]] components, (by-products of [[lipid peroxidation]] ) and to nitric-oxide modified [[amino acids]]; related to symptoms and severity in CFS.<ref name="pmid17693979">{{cite journal |author=Maes M, Mihaylova I, Bosmans E |title=Not in the mind of neurasthenic lazybones but in the cell nucleus: patients with chronic fatigue syndrome have increased production of nuclear factor kappa beta |journal=Neuro Endocrinol. Lett. |volume=28 |issue=4 |pages=456–62 |year=2007 |pmid=17693979 |doi=}}</ref> <ref name="PMID_15796202">{{cite journal | author = Snell CR, Vanness JM, Strayer DR, Stevens SR | title = Exercise capacity and immune function in male and female patients with chronic fatigue syndrome (CFS). | journal = In Vivo | volume = 19 | issue = 2 | pages = 387-90 | year = 2005 | id = PMID 15796202}}</ref> <ref name="pmid17159817">{{cite journal |author=Maes M, Mihaylova I, Leunis JC |title=Chronic fatigue syndrome is accompanied by an IgM-related immune response directed against neopitopes formed by oxidative or nitrosative damage to lipids and proteins |journal=Neuro Endocrinol. Lett. |volume=27 |issue=5 |pages=615–21 |year=2006 |pmid=17159817 |doi=}}</ref> |
|||
Gene expression studies suggest a common link between oxidative stress, immune system dysfunction and potassium imbalance in CFS patients leading to impaired nerve balance strongly reflected in abnormal [[heart rate]] variability.<ref name="pmid16610951">{{cite journal |author=Broderick G, Craddock RC, Whistler T, Taylor R, Klimas N, Unger ER |title=Identifying illness parameters in fatiguing syndromes using classical projection methods |journal=Pharmacogenomics |volume=7 |issue=3 |pages=407–19 |year=2006 |pmid=16610951 |doi=10.2217/14622416.7.3.407}}</ref> |
|||
=== |
=== Neurological === |
||
A range of structural, biochemical, and functional abnormalities are found in brain imaging studies of people with ME/CFS.<ref name="Marshall-Gradisnik_2022" /><ref name="Maksoud2020" /> Common findings are changes in the [[brainstem]] and the use of additional brain areas for cognitive tasks. Other consistent findings, based on a smaller number of studies, are low metabolism in some areas, reduced [[serotonin transporter]]s, and problems with [[Neurovascular unit|neurovascular coupling]].<ref name="pmid328732972" /> |
|||
When compared with CFS patients with normal natural killer cell activity, a 2006 study found those with lower levels reported less vigor, more daytime dysfunction, and more cognitive impairment; with the researchers suggesting this to be useful at subtyping.<ref>{{cite journal | author = Siegel SD, Antoni MH, Fletcher MA, Maher K, Segota MC, Klimas N | title = Impaired natural immunity, cognitive dysfunction, and physical symptoms in patients with chronic fatigue syndrome: preliminary evidence for a subgroup? | journal = J Psychosom Res | volume = 60 | issue = 6 | pages = 559-66 | year = 2006 | id = PMID 16731230}}</ref> A systematic review on the immunology of CFS (published in 2003) found an inverse association between study quality and findings of low levels of natural killer cells (suggesting that the association may be related to study methodology), although no such association was found with studies finding abnormalities in T cells and cytokine levels.<ref>{{cite journal | author = Lyall M, Peakman M, Wessely S | title = A systematic review and critical evaluation of the immunology of chronic fatigue syndrome. | journal = J Psychosom Res | volume = 55 | issue = 2 | pages = 79-90 | year = 2003 | id = PMID 12932505}}</ref> In 2006 an updated review on the phenomenology and pathophysiology of CFS found that, "immune system involvement in the pathogenesis of CFS seems certain but the findings on the specific mechanisms are still inconsistent."<ref name="PMID_16612182">{{cite journal | author = Cho HJ, Skowera A, Cleare A, Wessely S | title = Chronic fatigue syndrome: an update focusing on phenomenology and pathophysiology. | journal = Curr Opin Psychiatry | volume = 19 | issue = 1 | pages = 67-73 | year = 2006 | id = PMID 16612182}}</ref> There is also evidence that people with CFS have improper gene expression including both over expression and under expression of genes involved in the immune system (see the [[Chronic fatigue syndrome#Gene expression|gene expression]] section). |
|||
[[Neuroinflammation]] has been proposed as an underlying mechanism of ME/CFS that could explain a large set of symptoms. Several studies suggest neuroinflammation in the [[brain cortex|cortical]] and [[limbic system|limbic]] regions of the brain. Individuals with ME/CFS, for instance, have higher brain [[lactic acid|lactate]] and [[choline]] levels, which are signs of neuroinflammation. More direct evidence from two small [[positron emission tomography]] studies of [[microglia]], a type of immune cell in the brain, were contradictory, however.<ref name="pmid38016575">{{cite journal |vauthors=Lee JS, Sato W, Son CG |title=Brain-Regional Characteristics and Neuroinflammation in ME/CFS Patients from Neuroimaging: A Systematic Review and Meta-Analysis |journal=Autoimmunity Reviews |volume=23 |issue=2 |pages=103484 |date=November 2023 |pmid=38016575 |doi=10.1016/j.autrev.2023.103484 |url=|doi-access=free }}</ref><ref>{{cite journal | vauthors = VanElzakker MB, Brumfield SA, Lara Mejia PS | title = Neuroinflammation and Cytokines in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Critical Review of Research Methods | journal = Frontiers in Neurology | volume = 9 | pages = 1033 | date = 2019 | pmid = 30687207 | pmc = 6335565 | doi = 10.3389/fneur.2018.01033 | doi-access = free }}</ref> |
|||
====RNase L deregulation==== |
|||
Several studies have detected an abnormal form and activity level of 2-5A synthetase/[[RNase L]] enzyme (antiviral immune response) in some CFS patients<ref>{{cite journal | author = Tiev KP, Demettre E, Ercolano P, Bastide L, Lebleu B, Cabane J | title = RNase L levels in peripheral blood mononuclear cells: 37-kilodalton/83-kilodalton isoform ratio is a potential test for chronic fatigue syndrome. | journal = Clin Diagn Lab Immunol | volume = 10 | issue = 2 | pages = 315-6 | year = 2003 | id = PMID 12626460}}</ref><ref>{{cite journal | author = Demettre E, Bastide L, D'Haese A, De Smet K, De Meirleir K, Tiev KP, Englebienne P, Lebleu B | title = Ribonuclease L proteolysis in peripheral blood mononuclear cells of chronic fatigue syndrome patients. | journal = J Biol Chem | volume = 277 | issue = 38 | pages = 35746-51 | year = 2002 | id = PMID 12118002}}</ref><ref>{{cite journal | author = Shetzline SE, Martinand-Mari C, Reichenbach NL, Buletic Z, Lebleu B, Pfleiderer W, Charubala R, De Meirleir K, De Becker P, Peterson DL, Herst CV, Englebienne P, Suhadolnik RJ | title = Structural and functional features of the 37-kDa 2-5A-dependent RNase L in chronic fatigue syndrome. | journal = J Interferon Cytokine Res | volume = 22 | issue = 4 | pages = 443-56 | year = 2002 | id = PMID 12034027}}</ref><ref name="Suhadolnik97">{{cite journal | author = Suhadolnik RJ, Peterson DL, O'Brien K, Cheney PR, Herst CV, Reichenbach NL, Kon N, Horvath SE, Iacono KT, Adelson ME, De Meirleir K, De Becker P, Charubala R, Pfleiderer W | title = Biochemical evidence for a novel low molecular weight 2-5A-dependent RNase L in chronic fatigue syndrome. | journal = J Interferon Cytokine Res | volume = 17 | issue = 7 | pages = 377-85 | year = 1997 | id = PMID 9243369}}</ref><ref>{{cite journal | author = Fremont M, El Bakkouri K, Vaeyens F, Herst CV, De Meirleir K, Englebienne P | title = 2',5'-Oligoadenylate size is critical to protect RNase L against proteolytic cleavage in chronic fatigue syndrome. | journal = Exp Mol Pathol | volume = 78 | issue = 3 | pages = 239-46 | year = 2005 | id = PMID 15924878}}</ref><ref>{{cite journal | author = Suhadolnik RJ, Reichenbach NL, Hitzges P, Sobol RW, Peterson DL, Henry B, Ablashi DV, Muller WE, Schroder HC, Carter WA, et al | title = Upregulation of the 2-5A synthetase/RNase L antiviral pathway associated with chronic fatigue syndrome. | journal = Clin Infect Dis | volume = 18 | issue = Suppl 1 | pages = S96-104 | year = 1994 | id = PMID 8148461}}</ref> that appears to correlate with a reduction in exercise capacity.<ref name="PMID_15082102">{{cite journal | author = Nijs J, De Meirleir K, Meeus M, McGregor NR, Englebienne P | title = Chronic fatigue syndrome: intracellular immune deregulations as a possible etiology for abnormal exercise response. | journal = Med Hypotheses | volume = 62 | issue = 5 | pages = 759-65 | year = 2004 | id = PMID 15082102}}</ref><ref>{{cite journal | author = Snell CR, Vanness JM, Strayer DR, Stevens SR | title = Physical performance and prediction of 2-5A synthetase/RNase L antiviral pathway activity in patients with chronic fatigue syndrome. | journal = In Vivo | volume = 16 | issue = 2 | pages = 107-9 | year = 2002 | id = PMID 12073768}}</ref><ref>{{cite journal | author = Nijs J, Meeus M, McGregor NR, Meeusen R, de Schutter G, van Hoof E, de Meirleir K | title = Chronic fatigue syndrome: exercise performance related to immune dysfunction. | journal = Med Sci Sports Exerc | volume = 37 | issue = 10 | pages = 1647-54 | year = 2005 | id = PMID 16260962}}</ref><ref name="PMID_15796202">{{cite journal | author = Snell CR, Vanness JM, Strayer DR, Stevens SR | title = Exercise capacity and immune function in male and female patients with chronic fatigue syndrome (CFS). | journal = In Vivo | volume = 19 | issue = 2 | pages = 387-90 | year = 2005 | id = PMID 15796202}}</ref> A review published in 2005 suggested that this impaired pathway is of clinical importance and that further studies addressing treatment of this deregulation are warranted.<ref>{{cite journal | author = Nijs J, De Meirleir K | title = Impairments of the 2-5A synthetase/RNase L pathway in chronic fatigue syndrome. | journal = In Vivo | volume = 19 | issue = 6 | pages = 1013-21 | year = 2005 | id = PMID 16277015}}</ref> A study found that elevated RNase L did not correlate with alpha-delta sleep.<ref>{{cite journal | author = Van Hoof E, De Becker P, Lapp C, Cluydts R, De Meirleir K | title = Defining the occurrence and influence of alpha-delta sleep in chronic fatigue syndrome. | journal = Am J Med Sci | volume = 333 | issue = 2 | pages = 78-84 | year = 2007 | id = PMID 17301585}}</ref> |
|||
ME/CFS affects sleep. Individuals experience decreased [[sleep efficiency]], [[Sleep onset latency|take longer to fall asleep]], and take longer to achieve [[Rapid eye movement sleep|REM sleep]], a phase of sleep characterised by rapid eye movement. Changes to [[Non-rapid eye movement sleep|non-REM sleep]] have also been found, together suggesting a role of the autonomic nervous system.<ref name="pmid36948138">{{cite journal |vauthors=Mohamed AZ, Andersen T, Radovic S, Del Fante P, Kwiatek R, Calhoun V, Bhuta S, Hermens DF, Lagopoulos J, Shan ZY |title=Objective Sleep Measures in Chronic Fatigue Syndrome Patients: A Systematic Review and Meta-Analysis |journal=Sleep Medicine Reviews |volume=69 |issue= |pages=101771 |date=June 2023 |pmid=36948138 |doi=10.1016/j.smrv.2023.101771 |pmc=10281648 |url=}}</ref> Individuals often have a [[chronotropic incompetence|blunted heart rate response to exercise]], but a higher heart rate during a [[tilt table test]] when the body is rotated from lying flat to an upright position. This again suggests dysfunction in the autonomic nervous system.<ref name="pmid31651868">{{cite journal |vauthors=Nelson MJ, Bahl JS, Buckley JD, Thomson RL, Davison K |date=October 2019 |title=Evidence of Altered Cardiac Autonomic Regulation in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Systematic Review and Meta-Analysis |url=|journal=Medicine |volume=98 |issue=43 |pages=e17600 |doi=10.1097/MD.0000000000017600 |pmc=6824690 |pmid=31651868}}</ref> |
|||
====Hyperactive immunity==== |
|||
[[Autoimmune]] disorders, [[Hypersensitivity|representing a hyperactive immune system]], most likely through a [[Cell-mediated immunity|cell-mediated]] process, have been suggested.<ref>Kennedy G, Spence V, Underwood C, Belch JJ. Increased neutrophil apoptosis in chronic fatigue syndrome. |
|||
J Clin Pathol. 2004 Aug;57(8):891-3.</ref><ref>Patarca R, Klimas NG, Lugtendorf S, Antoni M, Fletcher MA. Dysregulated expression of tumor necrosis factor in chronic fatigue syndrome: interrelations with cellular sources and patterns of soluble immune mediator expression. |
|||
Clin Infect Dis. 1994 Jan;18 Suppl 1:S147-53.</ref> In July 2005, researchers in the UK reported significant gene changes in the [[white blood cells]] in CFS patients consistent with the theory of immune system activation, possibly by an [[antigen]] triggering a constant immune fatigue state. The study, led by Dr Jonathan Kerr, discovered that 35 white blood cell genes, out of a total of 9,522 genes scanned were demonstrating differential function. There was also suggestion of neuronal and mitochondrial dysfunction as a result.<ref>Original Research Paper, from the Journal of Clinical Pathology http://www.cfids.org/cfidslink/2005/cfs-gene.pdf</ref> |
|||
=== |
=== Immunological === |
||
People with ME/CFS often have immune system abnormalities. A consistent finding in studies is a decreased function of natural killer cells, a type of immune cell that targets virus-infected and tumour cells.<ref name="pmid31727160">{{cite journal |vauthors=Eaton-Fitch N, du Preez S, Cabanas H, Staines D, Marshall-Gradisnik S |date=November 2019 |title=A Systematic Review of Natural Killer Cells Profile and Cytotoxic Function in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome |url=|journal=Systematic Reviews |volume=8 |issue=1 |pages=279 |doi=10.1186/s13643-019-1202-6 |doi-access=free |pmc=6857215 |pmid=31727160}}</ref> They are also more likely to have active viral infections, correlating with cognitive issues and fatigue. [[T cell]]s show less metabolic activity. This may reflect they have reached an exhausted state and cannot respond effectively against [[pathogen]]s.<ref name="pmid38443223" /> |
|||
Patients with CFS commonly develop additional problems with [[allergy|allergies]] or [[food intolerance]]. <ref>{{cite conference |first=Emms TM |last= |authorlink= |coauthors= Roberts TK, Butt HL, et al|title=Food Intolerance in Chronic Fatigue Syndrome |booktitle= |pages=Conference Paper 15 |publisher=American Association for Chronic Fatigue Syndrome |date=Jan. 2001 |location=Seattle WA |url= |accessdate= |id= }}</ref> |
|||
<ref name="pmid11703165">{{cite journal |author=Logan AC, Wong C |title=Chronic fatigue syndrome: oxidative stress and dietary modifications |journal=Alternative medicine review : a journal of clinical therapeutic |volume=6 |issue=5 |pages=450-9 |year=2001 |pmid=11703165 |doi=}}</ref> |
|||
<ref name="isbn0-9695662-0-4">{{cite book |author=Nightingale Research Foundation; Goldstein, Jay E.; Byron M. Hyde |title=The Clinical and scientific basis of myalgic encephalomyelitis/chronic fatigue syndrome |publisher=Nightingale Research Foundation |location=Ogdensburg, N.Y |year=1992 |pages=521-538, chapter57, The Role of Food Intolerance in Chronic Fatigue Syndrome |isbn=0-9695662-0-4 |oclc= |doi=}}</ref> |
|||
Autoimmunity has been proposed to be a factor in ME/CFS. There is a subset of people with ME/CFS with increased levels of [[Autoantibody|autoantibodies]], possibly as a result of [[Molecular mimicry|viral mimicry]].<ref name="Autoimmunity Reviews pp. 601–609" /> Some may have higher levels of autoantibodies to [[muscarinic acetylcholine receptor]]s as well as to [[Beta-2 adrenergic receptor|β2 adrenergic receptors]].<ref name="Autoimmunity Reviews pp. 601–609">{{cite journal |vauthors=Sotzny F, Blanco J, Capelli E, Castro-Marrero J, Steiner S, Murovska M |date=June 2018 |title=Myalgic Encephalomyelitis/Chronic Fatigue Syndrome – Evidence for an Autoimmune Disease |journal=Autoimmunity Reviews |volume=17 |issue=6 |pages=601–609 |doi=10.1016/j.autrev.2018.01.009 |pmid=29635081 |doi-access=free |collaboration=European Network on ME/CFS (EUROMENE) |title-link=doi}}</ref><ref name="pmid38443223" /> Problems with these receptors can lead to impaired blood flow.<ref name="Autoimmunity Reviews 2020 p.">{{cite journal |vauthors=Wirth K, Scheibenbogen C |date=June 2020 |title=A Unifying Hypothesis of the Pathophysiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Recognitions from the Finding of Autoantibodies Against Β2-Adrenergic Receptors |journal=Autoimmunity Reviews |volume=19 |issue=6 |pages=102527 |doi=10.1016/j.autrev.2020.102527 |pmid=32247028 |doi-access=free |title-link=doi}}</ref> |
|||
====Immunodeficiency==== |
|||
[[Immunodeficiency]] disorders (representing an underactive immune system) have been reported. As early as 1989, a study was published in Australia that documented a loss of immunological integrity in one hundred CFS sufferers.<ref>{{cite journal | author = Lloyd A, Wakefield D, Boughton C, Dwyer J | title = Immunological abnormalities in the chronic fatigue syndrome. | journal = Med J Aust | volume = 151 | issue = 3 | pages = 122-4 | year = 1989 | id = PMID 2787888}}</ref> The authors reported finding disordered ratios of T-cell subsets and reduced levels of [[immunoglobulin]]s specifically IgG 1 and IgG 3; these findings corresponded with similar findings in the U.S. among leading researchers. Most strikingly, using the French Multitest to measure the body's response to a variety of antigens, the Australian group found that 33% of the subjects were [[hypoallergic]], meaning they had a reduced immune response to the tested antigens, while an additional 55% were completely anergic (no immune response to the antigens). |
|||
=== |
=== Energy === |
||
[[File:Work rate at ventilatory threshold.jpg|thumb|upright=1.35|When people with ME/CFS exercise on consecutive days, their performance declines on the second day, unlike those with [[idiopathic chronic fatigue|unexplained chronic fatigue]] (ICF).|alt=A scatterplot with fifty datapoints. They show that people with ME/CFS score worse in work rate at ventilatory threshold than those with unexplained chronic fatigue on the second day of a 2-day exercise test.]] |
|||
* Several studies have implicated a higher level of bioactive transforming growth factor-beta (TGF-beta) in CFS patients.<ref>{{cite journal | author = Bennett AL, Chao CC, Hu S, Buchwald D, Fagioli LR, Schur PH, Peterson PK, Komaroff AL | title = Elevation of bioactive transforming growth factor-beta in serum from patients with chronic fatigue syndrome. | journal = J Clin Immunol | volume = 17 | issue = 2 | pages = 160-6 | year = 1997 | id = PMID 9083892}}</ref> |
|||
Objective signs of PEM have been found with the [[2-day CPET|2-day cardiopulmonary exercise test]].<ref name="pmid33327624">{{cite journal |vauthors=Lim EJ, Kang EB, Jang ES, Son CG |date=December 2020 |title=The Prospects of the Two-Day Cardiopulmonary Exercise Test (CPET) in ME/CFS Patients: A Meta-Analysis |url=|journal=Journal of Clinical Medicine |volume=9 |issue=12 |page=4040 |doi=10.3390/jcm9124040 |pmc=7765094 |pmid=33327624 |doi-access=free}}</ref> People with ME/CFS have lower performance compared to healthy controls on the first test. On the second test, healthy people's scores stay roughly the same or increase slightly, while those with ME/CFS have a clinically significant decrease in work rate at the [[Lactate threshold|anaerobic threshold]]. Potential causes include mitochondrial dysfunction, and issues with the transport and use of oxygen.<ref name="Franklin-2022">{{Cite journal | vauthors = Franklin JD, Graham M |date=3 July 2022 |title=Repeated Maximal Exercise Tests of Peak Oxygen Consumption in People with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Systematic Review and Meta-Analysis |journal=Fatigue: Biomedicine, Health & Behavior |volume=10 |issue=3 |pages=119–135 |doi=10.1080/21641846.2022.2108628 |s2cid=251636593 |issn=2164-1846|doi-access = free | title-link = doi }}</ref> Some of the usual recovery processes following exercise may be lacking, providing an alternative explanation for PEM.<ref name="pmid38443223" /> |
|||
* A study published in 1995 found that 3 immunological tests (protein A binding, Raji cell, or C3/C4) best discriminated CFS patients from fatigued controls.<ref>{{cite journal | author = Natelson BH, Ellis SP, Braonain PJ, DeLuca J, Tapp WN | title = Frequency of deviant immunological test values in chronic fatigue syndrome patients. | journal = Clin Diagn Lab Immunol | volume = 2 | issue = 2 | pages = 238-40 | year = 1995 | id = PMID 7697537}}</ref> |
|||
* A recent study suggested that CFS may be characterized by an IgM-related immune response directed against disrupted lipid membrane components, by-products of lipid peroxidation, S-farnesyl-L-cysteine, and NO-modified amino-acids, which are normally not detected by the immune system but due to oxidative and nitrosative damage have become immunogenic.<ref>{{cite journal | author = Maes M, Mihaylova I, Leunis JC | title = Chronic fatigue syndrome is accompanied by an IgM-related immune response directed against neopitopes formed by oxidative or nitrosative damage to lipids and proteins. | journal = Neuro Endocrinol Lett | volume = 27 | issue = 5 | pages = 615-21 | year = 2006 | id = PMID 17159817}}</ref> |
|||
* Cytokine pattern; several studies <ref name="pmid14738459">{{cite journal |author=Skowera A, Cleare A, Blair D, Bevis L, Wessely SC, Peakman M |title=High levels of type 2 cytokine-producing cells in chronic fatigue syndrome |journal=Clin. Exp. Immunol. |volume=135 |issue=2 |pages=294–302 |year=2004 |pmid=14738459 |doi=}}</ref> <ref name="pmid11329477">{{cite journal |author=Hanson SJ, Gause W, Natelson B |title=Detection of immunologically significant factors for chronic fatigue syndrome using neural-network classifiers |journal=Clin. Diagn. Lab. Immunol. |volume=8 |issue=3 |pages=658–62 |year=2001 |pmid=11329477 |doi=10.1128/CDLI.8.3.658-662.2001}}</ref> <ref name="pmid11585638">{{cite journal |author=Visser J, Graffelman W, Blauw B, ''et al'' |title=LPS-induced IL-10 production in whole blood cultures from chronic fatigue syndrome patients is increased but supersensitive to inhibition by dexamethasone |journal=J. Neuroimmunol. |volume=119 |issue=2 |pages=343–9 |year=2001 |pmid=11585638 |doi=}}</ref> and a number of reviews <ref name="pmid12000020">{{cite journal |author=Patarca R |title=Cytokines and chronic fatigue syndrome |journal=Ann. N. Y. Acad. Sci. |volume=933 |issue= |pages=185–200 |year=2001 |pmid=12000020 |doi=}}</ref> <ref name="pmid11268418">{{cite journal |author=Visser JT, De Kloet ER, Nagelkerken L |title=Altered glucocorticoid regulation of the immune response in the chronic fatigue syndrome |journal=Ann. N. Y. Acad. Sci. |volume=917 |issue= |pages=868–75 |year=2000 |pmid=11268418 |doi=}}</ref> <ref name="pmid17364497">{{cite journal |author=Appel S, Chapman J, Shoenfeld Y |title=Infection and vaccination in chronic fatigue syndrome: myth or reality? |journal=Autoimmunity |volume=40 |issue=1 |pages=48–53 |year=2007 |pmid=17364497 |doi=10.1080/08916930701197273}}</ref> indicate there is a [[cytokine]] pattern of type 2 response including Th2 [[T helper cell]], bias in CFS. This promotes the [[humoral immune system]] which stimulates [[B cells]] and increases [[antibody]] production. It is suggested that this explains some immune dysfunctions in CFS. A reduction in Th1 response has also been found in some CFS studies. <ref name="pmid15471616">{{cite journal |author=Gaab J, Rohleder N, Heitz V, ''et al'' |title=Stress-induced changes in LPS-induced pro-inflammatory cytokine production in chronic fatigue syndrome |journal=Psychoneuroendocrinology |volume=30 |issue=2 |pages=188–98 |year=2005 |pmid=15471616 |doi=10.1016/j.psyneuen.2004.06.008}}</ref> <ref name="pmid9466535">{{cite journal |author=Visser J, Blauw B, Hinloopen B, ''et al'' |title=CD4 T lymphocytes from patients with chronic fatigue syndrome have decreased interferon-gamma production and increased sensitivity to dexamethasone |journal=J. Infect. Dis. |volume=177 |issue=2 |pages=451–4 |year=1998 |pmid=9466535 |doi=}}</ref> <ref name="pmid2166084">{{cite journal |author=Klimas NG, Salvato FR, Morgan R, Fletcher MA |title=Immunologic abnormalities in chronic fatigue syndrome |journal=J. Clin. Microbiol. |volume=28 |issue=6 |pages=1403–10 |year=1990 |pmid=2166084 |doi=}}</ref> with implications for altered Th1/Th2 balance. |
|||
* A study found that while exercise worsened symptoms in CFS patients, it also increased allergen challenge response only in the CFS group, regardless of allergy status.<ref name="PMID_12897748">{{cite journal | author = Sorensen B, Streib JE, Strand M, Make B, Giclas PC, Fleshner M, Jones JF | title = Complement activation in a model of chronic fatigue syndrome. | journal = J Allergy Clin Immunol | volume = 112 | issue = 2 | pages = 397-403 | year = 2003 | id = PMID 12897748}}</ref> |
|||
Studies have observed [[Mitochondrial disease|mitochondrial abnormalities]] in cellular energy production, but differences between studies make it hard to draw clear conclusions.<ref name="holden2020">{{cite journal |vauthors=Holden S, Maksoud R, Eaton-Fitch N, Cabanas H, Staines D, Marshall-Gradisnik S |date=July 2020 |title=A Systematic Review of Mitochondrial Abnormalities in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome/Systemic Exertion Intolerance Disease |journal=Journal of Translational Medicine |volume=18 |issue=1 |pages=290 |doi=10.1186/s12967-020-02452-3 |pmc=7392668 |pmid=32727475 |doi-access=free |title-link=doi}}</ref> [[Adenosine triphosphate|ATP]], the primary energy carrier in cells, is likely more frequently produced from [[lipid]]s and [[amino acid]]s than from [[carbohydrate]]s.<ref name="pmid38443223" /> |
|||
===Psychoneuroimmunological interactions=== |
|||
{{see|psychoneuroimmunology}} |
|||
A 2006 review published in ''Current neurovascular research'' states that there is growing evidence of autoantibodies to neuronal or endothelial (interior surface of blood vessels) targets in psychiatric disorders and hypothesizes how autoantibodies can play a role in the psychiatric disorders present in CFS.<ref>{{cite journal | author = Margutti P, Delunardo F, Ortona E | title = Autoantibodies associated with psychiatric disorders. | journal = Curr Neurovasc Res | volume = 3 | issue = 2 | pages =149-57 | year = 2006 | id = PMID 16719797}}</ref> Researchers involved in a review examining an immunological basis for CFS concluded that neuropsychiatric symptoms in CFS patients may be more closely related to disordered cytokine production by [[glial cells]] within the central nervous system rather than to circulating cytokines.<ref>{{cite journal | author = Vollmer-Conna U, Lloyd A, Hickie I, Wakefield D | title = Chronic fatigue syndrome: an immunological perspective. | journal = Aust N Z J Psychiatry | volume = 32 | issue = 4 | pages = 523-7 | year = 1998 | id = PMID 9711366}}</ref> In one study, [[autoantibodies]] for muscarinic cholinergic receptor had been found in over half of the CFS patients and seemed to correlate with the severity of the "feeling of muscle weakness".<ref>{{cite journal | author = Tanaka S, Kuratsune H, Hidaka Y, Hakariya Y, Tatsumi KI, Takano T, Kanakura Y, Amino N | title = Autoantibodies against muscarinic cholinergic receptor in chronic fatigue syndrome. | journal = Int J Mol Med | volume = 12 | issue = 2 | pages = 225-30 | year = 2003 | id = PMID 12851722}}</ref> Elevated levels of nitric oxide (not to be confused with nitrous oxide) has been found in some CFS patients<ref name="PMID_15082102">{{cite journal | author = Nijs J, De Meirleir K, Meeus M, McGregor NR, Englebienne P | title = Chronic fatigue syndrome: intracellular immune deregulations as a possible etiology for abnormal exercise response. | journal = Med Hypotheses | volume = 62 | issue = 5 | pages = 759-65 | year = 2004 | id = PMID 15082102}}</ref>. One hypothesis is that elevated levels of nitric oxide may contribute to a "sensitization" of the nervous system that results in behavioral changes.<ref name="PMID_15617866">{{cite journal | author = Nijs J, Van de Velde B, De Meirleir K | title = Pain in patients with chronic fatigue syndrome: does nitric oxide trigger central sensitisation? | journal = Med Hypotheses | volume = 64 | issue = 3 | pages = 558-62 | year = 2005 | id = PMID 15617866}}</ref> |
|||
=== |
=== Other === |
||
Some people with ME/CFS have abnormalities in their [[hypothalamic–pituitary–adrenal axis]] hormones. This can include [[adrenal insufficiency|lower cortisol levels]], less change in cortisol levels throughout the day, and a weaker reaction to stress and stimuli.<ref name="Morris2016rev">{{cite journal |vauthors=Morris G, Anderson G, Maes M |date=November 2017 |title=Hypothalamic-Pituitary-Adrenal Hypofunction in Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS) as a Consequence of Activated Immune-Inflammatory And Oxidative and Nitrosative Pathways |journal=Molecular Neurobiology |volume=54 |issue=9 |pages=6806–6819 |doi=10.1007/s12035-016-0170-2 |pmid=27766535 |s2cid=3524276}}</ref> Other proposed abnormalities are reduced [[Cerebral circulation|blood flow to the brain]] under orthostatic stress (as found in a tilt table test), [[Small fiber peripheral neuropathy|small-fibre neuropathy]], and an increase in the amount of [[Gut microbiota|gut microbes]] entering the blood.<ref name="BMJbest_practice3" />{{Rp|page=9}} The diversity of [[Gut microbiota|gut microbes]] is reduced compared to healthy controls.<ref name="pmid38443223" /> Women with ME/CFS are more likely to experience [[endometriosis]], [[Primary ovarian insufficiency|early menopause]], and other menstrual irregularities compared to women without the condition.<ref name="CDC_Clinical2024" /> |
|||
;Enteroviruses |
|||
Often, there is evidence of [[enterovirus]]es, e.g. the [[Coxsackie virus]]<ref name="Ramsay86"/>. The type of enterovirus varies, which can affect symptoms. In the times of [[polio]] outbreaks, [[paresis]] was often found in ME patients; this is no longer the case<ref name="isbn0-9695662-0-4"/>. Stomach biopsies of 80% of CFS patients showed the presence of enteroviruses in one study, as opposed to only 20% among controls, and nearly all biopsy specimens had microscopic evidence of mild chronic inflammation.<ref>{{cite journal |author=Chia JK, Chia AY |title=Chronic fatigue syndrome is associated with chronic enterovirus infection of the stomach |journal=J Clin Pathol |volume=Online preprint |issue= |pages= |year=2007 |pmid=17872383 |doi=10.1136/jcp.2007.050054}}</ref> Hyde and others suggest that these enteroviruses had been latent to be awakened by another, triggering infection, after which the immune system stays chronically active to combat the enterovirus.<ref name="isbn0-9695662-0-4"/> |
|||
== Diagnosis == |
|||
;Epstein-Barr virus |
|||
Diagnosis of ME/CFS is based on symptoms<ref name="pmid37226227" /> and involves taking a [[medical history]] and a mental and physical examination.<ref name="CDC2020diag" /> No specific lab tests are approved for diagnosis; while physical abnormalities can be found, no single finding is considered sufficient for diagnosis.<ref name="Bateman-2021" /><ref name="pmid37226227">{{cite journal | vauthors = Maksoud R, Magawa C, Eaton-Fitch N, Thapaliya K, Marshall-Gradisnik S | title = Biomarkers for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): a systematic review | journal = BMC Medicine | volume = 21 | issue = 1 | pages = 189 | date = May 2023 | pmid = 37226227 | pmc = 10206551 | doi = 10.1186/s12916-023-02893-9 | doi-access = free }}</ref> Blood and urine tests are used to rule out other conditions that could be responsible for the symptoms.<ref name="CDC2020diag">{{cite web |date=13 May 2024 |title=Diagnosing ME/CFS |url=https://www.cdc.gov/me-cfs/diagnosis/ |url-status=live |archive-url=https://web.archive.org/web/20240517195301/https://www.cdc.gov/me-cfs/diagnosis/ |archive-date=17 May 2024 |access-date=17 May 2024 |publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC)}}</ref> People with ME/CFS often face significant delays in obtaining a diagnosis, and diagnoses may be missed altogether.<ref name="NICE2021" />{{Rp|pages=66}} Specialists in ME/CFS may be asked to confirm the diagnosis, as primary care physicians often lack a good understanding of the illness.<ref name="NICE2021" />{{Rp|page=68}} |
|||
For many years the ubiquitous [[Epstein-Barr virus]], present in 90% of the population, was the principal suspect based on abnormal immunologic responses observed in uncontrolled studies.<ref name="pmid2578266"/><ref name="pmid2578268"/> Subsequent studies using various types of controls have had mixed conclusions.<ref name="pmid3033337">{{cite journal |author=Holmes GP, Kaplan JE, Stewart JA, Hunt B, Pinsky PF, Schonberger LB |title=A cluster of patients with a chronic mononucleosis-like syndrome. Is Epstein-Barr virus the cause? |journal=JAMA |volume=257 |issue=17 |pages=2297-302 |year=1987 |pmid=3033337 |doi=}}</ref><ref name="pmid1319246">{{cite journal | author = Kawai K, Kawai A | title = Studies on the relationship between chronic fatigue syndrome and Epstein-Barr virus in Japan. | journal = Intern Med | volume = 31 | issue = 3 | pages = 313-8 | year = 1992 | id = PMID 1319246}}</ref><ref name="pmid5113035">{{cite journal | author = Lerner A, Beqaj S, Deeter R, Fitzgerald J | title = IgM serum antibodies to Epstein-Barr virus are uniquely present in a subset of patients with the chronic fatigue syndrome. | journal = In Vivo | volume = 18 | issue = 2 | pages = 101-6 | year =2004 | id = PMID 15113035}}</ref> |
|||
=== Diagnostic criteria === |
|||
;Other viruses |
|||
{{Main|Clinical descriptions of ME/CFS}} |
|||
Other implicated viruses include [[cytomegalovirus]], and [[HHV-6|human herpesvirus type-6]] (HHV-6).<ref>{{cite journal | author = Ablashi D, Eastman H, Owen C, Roman M, Friedman J, Zabriskie J, Peterson D, Pearson G, Whitman J | title = Frequent HHV-6 reactivation in multiple sclerosis (MS) and chronic fatigue syndrome (CFS) patients. | journal = J Clin Virol | volume = 16 | issue = 3 | pages = 179-91 | year = 2000 | id = PMID 10738137}}</ref><ref>{{cite journal | author = De Bolle L, Naesens L, De Clercq E | title = Update on human herpesvirus 6 biology, clinical features, and therapy. | journal = Clin Microbiol Rev | volume = 18 | issue = 1 | pages = 217-45 | year = 2005 | id = PMID 15653828}}</ref><ref>{{cite journal | author = Krueger G, Koch B, Hoffmann A, Rojo J, Brandt M, Wang G, Buja L | title = Dynamics of chronic active herpesvirus-6 infection in patients with chronic fatigue syndrome: data acquisition for computer modeling. | journal = In Vivo | volume = 15 | issue = 6 | pages = 461-5 | year = | id = PMID 11887330}}</ref><ref>{{cite journal | author = Caserta M, Mock D, Dewhurst S | title = Human herpesvirus 6. | journal = Clin Infect Dis | volume = 33 | issue = 6 | pages = 829-33 | year = 2001 | id = PMID 11512088}}</ref><ref>{{cite journal | author = Yalcin S, Kuratsune H, Yamaguchi K, Kitani T, Yamanishi K | title = Prevalence of human herpesvirus 6 variants A and B in patients with chronic fatigue syndrome. | journal = Microbiol Immunol | volume = 38 | issue = 7 | pages = 587-90 | year = 1994 | id = PMID 7968694}}</ref><ref>{{cite journal | author = Sairenji T, Yamanishi K, Tachibana Y, Bertoni G, Kurata T | title = Antibody responses to Epstein-Barr virus, human herpesvirus 6 and human herpesvirus 7 in patients with chronic fatigue syndrome. | journal = Intervirology | volume = 38 | issue = 5 | pages = 269-73 | year = 1995 | id = PMID 8724857}}</ref><ref name="Buchwald"/><ref name= "PMID: 7594679">{{cite journal | author = Patnaik M, Komaroff A, Conley E, Ojo-Amaize E, Peter J | title = Prevalence of IgM antibodies to human herpesvirus 6 early antigen (p41/38) in patients with chronic fatigue syndrome. | journal = J Infect Dis | volume = 172 | issue = 5 | pages = 1364-7 | year = 1995 | id = PMID 7594679}}</ref><ref name="PMID: 17276367">{{cite journal |author=Komaroff AL. |title=Is human herpesvirus-6 a trigger for chronic fatigue syndrome |
|||
{| class="wikitable floatright" |
|||
|journal=J Clin Virol. |volume=37 |issue=Suppl 1 |pages=S39-46 |date=2006 Dec |pmid=17276367 }}</ref> A review by Soto and Straus in 2000 states the evidence argues against an ongoing active herpes virus infection.<ref>{{cite journal | author = | title = Chronic Fatigue Syndrome and Herpesviruses: the Fading Evidence. | journal = Herpes | volume = 7 | issue = 2 | pages = 46-50 | year = 2000 | id = PMID 11867001}} |
|||
|+ ME/CFS symptoms according to five diagnostic criteria<ref name="IQWiG-2023" />{{rp|13}}<ref name="BMJbest_practice3" />{{rp|15}} |
|||
</ref> |
|||
! style="text-align: left; font-weight: normal;" |'''Symptom''' {{small|<br> M: Mandatory <br> O: Optional}} |
|||
!{{vert header|{{abbr|CDC|Centers for Disease Control and Prevention}}/Fukuda}} |
|||
!{{vert header|{{abbr|CCC|Canadian Consensus Criteria}}}} |
|||
!{{vert header|{{abbr|ICC|International Consensus Criteria}}}} |
|||
!{{vert header|{{abbr|IOM|Institute of Medicine}}}} |
|||
!{{vert header|{{abbr|NICE|National Institute for Health and Care Excellence}}}} |
|||
|- |
|||
|Fatigue |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
|- |
|||
|Functional impairment |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
|- |
|||
|PEM |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
|- |
|||
|Sleep problems |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
|- |
|||
|Cognitive issues |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
|- |
|||
|Pain or headaches |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #3B7D23; text-align: center;" |<span style="color:white">'''M'''</span> |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| |
|||
| |
|||
|- |
|||
|Orthostatic intolerance |
|||
| |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| |
|||
|- |
|||
|Flu or cold symptoms |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| |
|||
| |
|||
|- |
|||
|Nausea |
|||
| |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| |
|||
| |
|||
|- |
|||
|Cardiovascular problems |
|||
| |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| |
|||
| |
|||
|- |
|||
|Hypersensitivities |
|||
| |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| |
|||
| |
|||
|- |
|||
|Susceptibility to infection |
|||
| |
|||
| |
|||
| style="background: #8ED973; text-align: center;" |'''O''' |
|||
| |
|||
| |
|||
|} |
|||
Multiple research and clinical criteria exist to diagnose ME/CFS. These include the [[National Institute for Health and Care Excellence|NICE]] guidelines, [[National Academy of Medicine|Institute of Medicine]] (IOM) criteria, the International Consensus Criteria (ICC), the Canadian Consensus Criteria (CCC), and [[Centers for Disease Control and Prevention|CDC]] criteria. The criteria sets were all developed based on expert consensus and differ in the required symptoms and which conditions preclude a diagnosis of ME/CFS.<ref name="BMJbest_practice3" />{{Rp|page=14}} The definitions differ in their conceptualisation of the cause and mechanisms of ME/CFS.<ref name="Lim_2020">{{cite journal |vauthors=Lim EJ, Son CG |date=July 2020 |title=Review of Case Definitions for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) |journal=Journal of Translational Medicine |volume=18 |issue=1 |pages=289 |doi=10.1186/s12967-020-02455-0 |pmc=7391812 |pmid=32727489 |doi-access=free |title-link=doi}}</ref> |
|||
===Endocrine dysfunction=== |
|||
[[Thyroid]] and [[adrenal]] disorders can cause CFS-like symptoms, as can several other known [[endocrine]] disorders. |
|||
As there is no single known [[biomarker]] for ME/CFS, it is not possible to determine which set of criteria is the most accurate. A trade-off must be made between overdiagnosis and missing more diagnoses. The broad Fukuda criteria have a higher risk of overdiagnosis, whereas the strict ICC criteria have a higher risk of missing people. The IOM and NICE criteria fall in the middle.<ref name="NICE-2021-D" />{{Rp|page=|pages=47–48}} |
|||
;HPA Axis |
|||
The 1994 CDC criteria, sometimes called the Fukuda criteria, require six months of persistent or relapsing fatigue for diagnosis, as well as the persistent presence of four out of eight other symptoms.<ref name="BMJbest_practice3" />{{Rp|page=35}} While used frequently, the Fukuda criteria have limitations: PEM and cognitive issues are not mandatory. The large variety of optional symptoms can lead to diagnosis of individuals who differ significantly from each other.<ref name="IQWiG-2023" />{{Rp|page=15|pages=}} |
|||
The [[HPA axis]] controls levels of [[hormones]] such as [[cortisol]] in the body. It is activated in a [[circadian]] (daily) cycle and modulated by [[Stress (medicine)|stress]], [[digestion]], [[illness]] and other factors, and is important in regulating energy metabolism, the immune system, stress responses and inflammation in the body. |
|||
The Canadian Consensus Criteria, another commonly used criteria set, was developed in 2003.<ref name="BMJbest_practice3" />{{Rp|page=14}} In addition to PEM, fatigue and sleep problems, pain and neurological or cognitive issues are required for diagnosis. Furthermore, three categories of symptoms are defined (orthostatic, thermal instability, and immunological). At least one symptom in two of these categories needs to be present.<ref name="IQWiG-2023" />{{Rp|page=15}}<ref name="BMJbest_practice3" />{{Rp|page=34}} People diagnosed under the CCC have more severe symptoms compared to those diagnosed under the Fukuda criteria. The 2011 International Consensus Criteria defines ME using symptom clusters and has no minimum duration of symptoms. Similarly to the CCC criteria, ICC is stricter than the Fukuda criteria and selects more severely ill people.<ref name="BMJbest_practice3" />{{Rp|page=14}} |
|||
The HPA axis has been much studied in CFS which has shown underactivation with low cortisol not caused by adrenal insufficiency. <ref name="pmid1659582">{{cite journal |author=Demitrack MA, Dale JK, Straus SE, ''et al'' |title=Evidence for impaired activation of the hypothalamic-pituitary-adrenal axis in patients with chronic fatigue syndrome |journal=J. Clin. Endocrinol. Metab. |volume=73 |issue=6 |pages=1224–34 |year=1991 |pmid=1659582 |doi=}}</ref> <ref name="pmid12700181">{{cite journal |author=Cleare AJ |title=The neuroendocrinology of chronic fatigue syndrome |journal=Endocr. Rev. |volume=24 |issue=2 |pages=236–52 |year=2003 |pmid=12700181 |doi=}}</ref> <ref name="pmid17596739">{{cite journal |author=Van Den Eede F, Moorkens G, Van Houdenhove B, Cosyns P, Claes SJ |title=Hypothalamic-pituitary-adrenal axis function in chronic fatigue syndrome |journal=Neuropsychobiology |volume=55 |issue=2 |pages=112–20 |year=2007 |pmid=17596739 |doi=10.1159/000104468}}</ref> These results have not been replicated in all CFS patients, so it is not clear whether this is just a subset of patients. It is also not clear if the HPA axis abnormalities are a cause or a result of the illness. However, a review has concluded, that even if the HPA axis dysfunctions are secondary to other factors; they are a likely factor in symptom propagation in CFS. <ref name="pmid17596739">{{cite journal |author=Van Den Eede F, Moorkens G, Van Houdenhove B, Cosyns P, Claes SJ |title=Hypothalamic-pituitary-adrenal axis function in chronic fatigue syndrome |journal=Neuropsychobiology |volume=55 |issue=2 |pages=112–20 |year=2007 |pmid=17596739 |doi=10.1159/000104468}}</ref> |
|||
The 2015 IOM criteria share significant similarities with the CCC but were developed to be easy to use for clinicians. Diagnosis requires fatigue, PEM, non-restorative sleep, and either cognitive issues (such as memory impairment) or orthostatic intolerance. Additionally, fatigue must persist for at least six months, substantially impair activities in all areas of life, and have a clearly defined onset.<ref name="IQWiG-2023" />{{Rp|page=|pages=16–17}} Symptoms must be present at least half of the time, and be of moderate severity or worse; previous criteria just required symptoms to be present.<ref name="BMJbest_practice3" />{{Rp|page=14}} In 2021, NICE revised its criteria based on the IOM criteria. The updated criteria require fatigue, PEM, non-restorative sleep, and cognitive difficulties persisting for at least three months.<ref name="IQWiG-2023" />{{Rp|page=|pages=16–17}} |
|||
===Gene expression=== |
|||
[[Gene expression]] is the process by which the inheritable information in a gene, such as the DNA sequence, is made into a functional gene product, such as protein or RNA. Research into CFS has found abnormalities in gene expression, and the CDC has conducted over twenty related studies itself.<ref>[http://www.cdc.gov/ncidod/diseases/cfs/publications/molecular_epi.htm] The Centers For Disease Control and Prevention (website): CFS Home > Publications > Molecular Epidemiology Program - Date: [[July 25]] [[2005]] - Content source: National Center for Infectious Diseases</ref> <ref name="CDC April 20 2006"/> It has been found that patients with CFS have specific abnormalities in expression of multiple genes which are involved in the biological process of transport (both vesicle-mediated and protein transport) and this became accentuated when CFS patients exercise.<ref>{{cite journal | author = Whistler T, Jones JF, Unger ER, Vernon SD | title = Exercise responsive genes measured in peripheral blood of women with chronic fatigue syndrome and matched control subjects. | journal = BMC Physiol | volume = 5 | issue = 1 | pages = 5 | year = 2005 | id = PMID 15790422 | url = http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=15790422}}</ref> Another study found that "the differentially expressed genes imply fundamental metabolic perturbations", such as those involved in purine and pyrimidine metabolism, glycolysis, oxidative phosphorylation, and glucose metabolism.<ref>{{cite journal | author = Whistler T, Unger ER, Nisenbaum R, Vernon SD | title = Integration of gene expression, clinical, and epidemiologic data to characterize Chronic Fatigue Syndrome. | journal = J Transl Med | volume = 1 | issue = 1 | pages = 10 | year = 2003 | id = PMID 14641939}}</ref> Several other studies have also suggested a genetic component to CFS involving immune dysfunction<ref>{{cite journal | author = Vernon SD, Unger ER, Dimulescu IM, Rajeevan M, Reeves WC | title = Utility of the blood for gene expression profiling and biomarker discovery in chronic fatigue syndrome. | journal = Dis Markers | volume = 18 | issue = 4 | pages = 193-9 | year = 2002 | id = PMID 12590173}}</ref>; T cell activation, perturbation of neuronal and mitochondrial function, possible links to organophosphate exposure and virus infection<ref>{{cite journal | author = Kaushik N, Fear D, Richards SC, McDermott CR, Nuwaysir EF, Kellam P, Harrison TJ, Wilkinson RJ, Tyrrell DA, Holgate ST, Kerr JR | title = Gene expression in peripheral blood mononuclear cells from patients with chronic fatigue syndrome. | journal = J Clin Pathol | volume = 58 | issue = 8 | pages = 826-32 | year = 2005 | id = PMID 16049284}}</ref>; immune response, apoptosis, ion channel activity, signal transduction, cell-cell signaling, regulation of cell growth and neuronal activity<ref>{{cite journal | author = Fang H, Xie Q, Boneva R, Fostel J, Perkins R, Tong W | title = Gene expression profile exploration of a large dataset on chronic fatigue syndrome. | journal = Pharmacogenomics | volume = 7 | issue = 3 | pages = 429-40 | year = 2006 | id = PMID 16610953}}</ref>; some of which may be treatable with drugs that are already available.<ref> BBC News ([[28 May]] [[2005]]) - [http://news.bbc.co.uk/2/hi/health/4580051.stm Scientists 'unlock ME genetics'] (study still in its early stages)</ref> Gene expression abnormalities have been found relating to the central nervous system, metabolism and immune system; and has been associated by the CDC with impaired response to physical and psychological stresses in people with CFS. <ref name="CDC April 20 2006"/> Linking genes to specific symptoms has been difficult, although is likely to be an important means to elucidate the pathogenesis of CFS.<ref>{{cite journal | author = Fostel J, Boneva R, Lloyd A | title = Exploration of the gene expression correlates of chronic unexplained fatigue using factor analysis. | journal = Pharmacogenomics | volume = 7 | issue = 3 | pages = 441-54 | year = 2006 | id = PMID 16610954}}</ref>Seven subtypes of CFS/ME patients with distinct clinical differences have been identied in one gene expression study.<ref name="pmid18057078">{{cite journal |author=Kerr J, Burke B, Petty R, ''et al'' |title=Seven genomic subtypes of Chronic Fatigue Syndrome / Myalgic Encephalomyelitis (CFS/ME): a detailed analysis of gene networks and clinical phenotypes |journal=J Clin Pathol |volume= |issue= |pages= |year=2007 |pmid=18057078 |doi=10.1136/jcp.2007.053553}}</ref> |
|||
Separate diagnostic criteria have been developed for children and young people. A diagnosis for children often requires a shorter symptom duration. For example, the CCC definition only requires three months of persistent symptoms in children compared to six months for adults.<ref name="IQWiG-2023" />{{Rp|page=|pages=17–18}} NICE requires only four weeks of symptoms to suspect ME/CFS in children, compared to six weeks in adults.<ref name="BMJbest_practice3" />{{Rp|page=15}} Exclusionary diagnoses also differ; for instance, children and teenagers may have [[School refusal|anxiety related to school attendance]], which could explain symptoms.<ref name="IQWiG-2023" />{{Rp|page=|pages=17–18}} |
|||
===Genetic polymorphisms=== |
|||
[[Polymorphism (biology)|Polymorphism]] in biology occurs when two or more clearly different types exist in the same population of the same species. Preliminary studies have suggested that the risk of developing CFS may be influenced by polymorphisms in genes affecting the central nervous, |
|||
<ref name="pmid18079067">{{cite journal |author=Smith AK, Dimulescu I, Falkenberg VR, ''et al'' |title=Genetic evaluation of the serotonergic system in chronic fatigue syndrome |journal=Psychoneuroendocrinology |volume=33 |issue=2 |pages=188–97 |year=2008 |pmid=18079067 |doi=10.1016/j.psyneuen.2007.11.001}}</ref><ref>{{cite journal | author=Narita M, Nishigami N, Narita N, Yamaguti K, Okado N, Watanabe Y, Kuratsune H | title=Association between serotonin transporter gene polymorphism and chronic fatigue syndrome | journal=Biochem. Biophys. Res. Commun. | volume=311 | issue=2 | pages=264-6 | year=2003 | pmid=14592408}}</ref> endocrine,<ref>{{cite journal | author=Goertzel BN, Pennachin C, de Souza Coelho L, Gurbaxani B, Maloney EM, Jones JF | title=Combinations of single nucleotide polymorphisms in neuroendocrine effector and receptor genes predict chronic fatigue syndrome | journal=Pharmacogenomics | volume=7 | issue=3 | pages=475-83 | year=2006 | pmid=16610957}}</ref><ref>{{cite journal | author=Smith AK, White PD, Aslakson E, Vollmer-Conna U, Rajeevan MS | title=Polymorphisms in genes regulating the HPA axis associated with empirically delineated classes of unexplained chronic fatigue | journal=Pharmacogenomics | volume=7 | issue=3 | pages=387-94 | year=2006 | pmid=16610949}}</ref><ref>{{cite journal | author=Torpy DJ, Bachmann AW, Gartside M, Grice JE, Harris JM, Clifton P, Easteal S, Jackson RV, Whitworth JA | title=Association between chronic fatigue syndrome and the corticosteroid-binding globulin gene ALA SER224 polymorphism | journal=Endocr. Res. | volume=30 | issue=3 | pages=417-29 | year=2004 | pmid=15554358}}</ref> immune,<ref>{{cite journal | author=Kerr JR | title=Pathogenesis of parvovirus B19 infection: host gene variability, and possible means and effects of virus persistence | journal=J. Vet. Med. B Infect. Dis. Vet. Public Health | volume=52 | issue=7-8 | pages=335-9 | year=2005 | pmid=16316396}}</ref><ref>{{cite journal | author=Carlo-Stella N, Badulli C, De Silvestri A, Bazzichi L, Martinetti M, Lorusso L, Bombardieri S, Salvaneschi L, Cuccia M | title=A first study of cytokine genomic polymorphisms in CFS: Positive association of TNF-857 and IFNgamma 874 rare alleles | journal=Clin. Exp. Rheumatol. | volume=24 | issue=2 | pages=179-82 | year=2006 | pmid=16762155}}</ref> and/or cardiovascular systems.<ref>{{cite journal | author=Vladutiu GD, Natelson BH | title=Association of medically unexplained fatigue with ACE insertion/deletion polymorphism in Gulf War veterans | journal=Muscle Nerve | volume=30 | issue=1 | pages=38-43 | year=2004 | pmid=15221876}}</ref> A review published in 2007 stated that certain genetic polymorphisms might be regarded as predisposing factors.<ref name="PMID_17419822">{{cite journal | author = Wyller VB | title = The chronic fatigue syndrome - an update | journal = Acta Neurol Scand Suppl | volume = 187 | pages = 7-14 | year = 2007 | id = PMID 17419822}}</ref> |
|||
=== Clinical assessment === |
|||
===Metabolic disorders=== |
|||
[[File:Could You Have MECFS.webp|thumb|upright=1.35|''Could You Have ME/CFS?'' handout from the US Centers for Disease Control and Prevention|alt=A leaflet from the CDC describing the Institute of Medicine criteria for ME/CFS.]] |
|||
[[Metabolic disorder]]s and [[mitochondrial disorder]]s can cause symptoms that strongly resemble CFS <ref name="pmid17293137">{{cite journal |author=van de Glind G, de Vries M, Rodenburg R, Hol F, Smeitink J, Morava E |title=Resting muscle pain as the first clinical symptom in children carrying the MTTK A8344G mutation |journal=Eur. J. Paediatr. Neurol. |volume=11 |issue=4 |pages=243–6 |year=2007 |pmid=17293137 |doi=10.1016/j.ejpn.2007.01.004}}</ref>. Mitochondrial disturbances have been discovered in patients diagnosed with [[postviral fatigue syndrome]]. |
|||
Screening can be done using the [[DePaul Symptom Questionnaire]], which assesses the frequency and severity of ME/CFS symptoms.<ref name="BMJbest_practice3" />{{Rp|24}} Individuals may struggle to answer questions related to PEM, if they are unfamiliar with the symptom. To find patterns in symptoms, they may be asked to keep a diary.<ref name="Bateman-2021" /> |
|||
<ref name="pmid1792865">{{cite journal |author=Behan WM, More IA, Behan PO |title=Mitochondrial abnormalities in the postviral fatigue syndrome |journal=Acta Neuropathol. |volume=83 |issue=1 |pages=61–5 |year=1991 |pmid=1792865 |doi=}}</ref> and mitochondrial dysfunction is considered a factor in PVFS and CDC defined CFS patients. <ref name="pmid16448567">{{cite journal |author=Vernon SD, Whistler T, Cameron B, Hickie IB, Reeves WC, Lloyd A |title=Preliminary evidence of mitochondrial dysfunction associated with post-infective fatigue after acute infection with Epstein Barr virus |journal=BMC Infect. Dis. |volume=6 |issue= |pages=15 |year=2006 |pmid=16448567 |doi=10.1186/1471-2334-6-15}}</ref> <ref name="pmid18177602">{{cite journal |author=Klimas NG, Koneru AO |title=Chronic fatigue syndrome: inflammation, immune function, and neuroendocrine interactions |journal=Curr Rheumatol Rep |volume=9 |issue=6 |pages=482–7 |year=2007 |pmid=18177602 |doi=}}</ref> <ref name="pmid16049284">{{cite journal |author=Kaushik N, Fear D, Richards SC, ''et al'' |title=Gene expression in peripheral blood mononuclear cells from patients with chronic fatigue syndrome |journal=J. Clin. Pathol. |volume=58 |issue=8 |pages=826–32 |year=2005 |pmid=16049284 |doi=10.1136/jcp.2005.025718}}</ref> <ref name="pmid17239370">{{cite journal |author=Pieczenik SR, Neustadt J |title=Mitochondrial dysfunction and molecular pathways of disease |journal=Exp. Mol. Pathol. |volume=83 |issue=1 |pages=84–92 |year=2007 |pmid=17239370 |doi=10.1016/j.yexmp.2006.09.008}}</ref> |
|||
A [[physical exam]] may appear completely normal, particularly if the individual has rested substantially before a doctor's visit.<ref name="Bateman-2021" /> There may be tenderness in the lymph nodes and abdomen or signs of hypermobility.<ref name="BMJbest_practice3" />{{Rp|17}} Answers to questions may show a temporary difficulty with finding words or other cognitive problems.<ref name="pmid37793728" /> [[Neuropsychological test|Cognitive tests]] and a two-day cardiopulmonary exercise test (CPET) can be helpful to document aspects of the illness, but they may be risky as they can cause severe PEM. They may be warranted to support a disability claim.<ref name="Bateman-2021" /> Orthostatic intolerance can be measured with a tilt table test. If that is unavailable, it can also be assessed with the simpler [[NASA lean test|NASA 10-minute lean test]], which tests the response to prolonged standing.<ref name="pmid37793728" /> |
|||
Folate deficiency (suspicion by elevated homocysteine and low serum folate) may mimick CFS symptoms.<ref>Lundell K, Qazi S, Eddy L, Uckun FM. Clinical activity of folinic acid in patients with chronic fatigue syndrome. Arzneimittelforschung. 2006;56(6):399-404.</ref><ref>Jacobson W, Saich T, Borysiewicz LK, Behan WM, Behan PO, Wreghitt TG. Serum folate and chronic fatigue syndrome. ''Neurology'' 1993 Dec;43(12):2645-7.</ref> |
|||
Standard laboratory findings are usually normal. Standard tests when suspecting ME/CFS include an HIV test, and blood tests to determine [[Complete blood count|full blood count]], [[Erythrocyte sedimentation rate|red blood cell sedimentation rate]] (ESR), [[C-reactive protein]], blood glucose and [[thyroid-stimulating hormone]]. Tests for [[Antinuclear antibody|antinuclear antibodies]] may come back positive, but below the levels that suggest the individual may have [[lupus]]. C-reactive protein levels are often at the high end of normal. [[Ferritin|Serum ferritin]] levels may be useful to test, as borderline [[Anemia|anaemia]] can make some ME/CFS symptoms worse.<ref name="BMJbest_practice3" />{{Rp|18}} |
|||
===Toxic agents=== |
|||
[[Insecticides]] have a possible effect on the cause and/or course of CFS. <ref name="pmid15826581">{{cite journal |author=Fernández-Solà J, Lluís Padierna M, Nogué Xarau S, Munné Mas P |title=[Chronic fatigue syndrome and multiple chemical hypersensitivity after insecticide exposure] |language=Spanish; Castilian |journal=Med Clin (Barc) |volume=124 |issue=12 |pages=451–3 |year=2005 |pmid=15826581 |doi=}}</ref><ref name="pmid7565234">{{cite journal |author=Dunstan RH, Donohoe M, Taylor W, ''et al'' |title=A preliminary investigation of chlorinated hydrocarbons and chronic fatigue syndrome |journal=Med. J. Aust. |volume=163 |issue=6 |pages=294–7 |year=1995 |pmid=7565234 |doi=}}</ref> |
|||
=== Differential diagnosis === |
|||
===Other findings=== |
|||
Some medical conditions have symptoms similar to ME/CFS. Diagnosis often involves clinical evaluation, testing, and specialist referrals to identify the correct condition. During the time other possible diagnoses are explored, advice can be given on symptom management to help prevent the condition from getting worse.<ref name="NICE2021" />{{Rp|pages=66–67}} Before a diagnosis of ME/CFS is confirmed, a waiting period is used to exclude acute medical conditions or symptoms which may resolve within that time frame.<ref name="Bateman-2021" /><ref>{{Cite journal |last1=Kingdon |first1=Caroline |last2=Lowe |first2=Adam |last3=Shepherd |first3=Charles |last4=Nacul |first4=Luis |date=2022 |title=What Primary Care Practitioners Need to Know about the New NICE Guideline for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in Adults |journal=Healthcare |language=en |volume=10 |issue=12 |pages=2438 |doi=10.3390/healthcare10122438 |doi-access=free |pmid=36553962 |pmc=9778354 |issn=2227-9032}}</ref> |
|||
Other findings regarding CFS in general include: |
|||
Possible differential diagnoses span a large set of specialties and depend on the medical history.<ref name="Bateman-2021" /> Examples are [[Infection|infectious diseases]], such as Epstein–Barr virus and [[Lyme disease]], and neuroendocrine disorders, including [[diabetes]] and [[hypothyroidism]]. [[Hematologic disease|Blood disorders]], such as [[Anemia|anaemia]], and some cancers may also present similar symptoms.<ref name="Bateman-2021" /><ref name="NICE-2021-D" />{{Rp|page=57}} Various rheumatological and autoimmune diseases, such as [[Sjögren syndrome|Sjögren's syndrome]], lupus, and [[arthritis]], may have overlapping symptoms with ME/CFS. Furthermore, it may be necessary to evaluate [[mental disorder|psychiatric diseases]], such as depression or [[substance use disorder]], as well as neurological disorders, such as [[narcolepsy]], [[multiple sclerosis]], and [[craniocervical instability]].<ref name="Bateman-2021" /><ref name="NICE-2021-D">{{Cite book |last=National Guideline Centre (UK) |url=https://www.ncbi.nlm.nih.gov/books/NBK579530/pdf/Bookshelf_NBK579530.pdf |title=Identifying and Diagnosing ME/CFS: Myalgic Encephalomyelitis (Or Encephalopathy) / Chronic Fatigue Syndrome: Diagnosis and Management: Evidence Review D |date=2021 |publisher=National Institute for Health and Care Excellence (NICE) |isbn=978-1-4731-4221-3 |series=NICE Evidence Reviews Collection |location=London |pmid=35438857 |access-date=23 September 2023 |archive-url=https://web.archive.org/web/20240219120717/https://www.ncbi.nlm.nih.gov/books/NBK579530/ |archive-date=19 February 2024 |url-status=live}}</ref>{{Rp|page=57}} Finally, sleep disorders, [[coeliac disease]], and side effects of medications may also explain symptoms.<ref name="Bateman-2021" /> |
|||
* A large study found that higher levels of exercise in childhood is associated with a lower risk of developing CFS later on. It also found that the development of CFS was not associated with other childhood or maternal factors such as psychological problems, academic ability, allergic tendencies, birth weight, birth order or obesity.<ref>{{cite journal | author = Viner R, Hotopf M | title = Childhood predictors of self reported chronic fatigue syndrome/myalgic encephalomyelitis in adults: national birth cohort study. | journal = BMJ | volume = 329 | issue = 7472 | pages = 941 | year = 2003 | id = PMID 15469945}}</ref> |
|||
Joint and muscle pain without swelling or inflammation is a common feature of ME/CFS, but is more closely associated with [[fibromyalgia]]. Modern definitions of fibromyalgia not only include widespread pain but also fatigue, sleep disturbances, and cognitive issues. This makes it difficult to distinguish ME/CFS from fibromyalgia<ref name="BMJbest_practice">{{Cite book |vauthors=Baraniuk JN |date=January 2022 |title=Myalgic Encephalomyelitis (Chronic Fatigue Syndrome) |url=https://bestpractice.bmj.com/topics/en-us/277/pdf/277/Myalgic%20encephalomyelitis%20(Chronic%20fatigue%20syndrome).pdf |access-date=30 September 2023 |publisher=BMJ Best Practice |url-access=subscription |archive-date=9 October 2023 |archive-url=https://web.archive.org/web/20231009170253/https://bestpractice.bmj.com/topics/en-us/277/pdf/277/Myalgic%20encephalomyelitis%20(Chronic%20fatigue%20syndrome).pdf |url-status=live }}</ref>{{rp|13, 26}} and the two are often co-diagnosed.<ref name="BMJbest_practice3" />{{rp||page=28}} |
|||
* Researchers compared 48 CFS patients with 29 controls and found that 10 of the CFS patients tested positive for enterovirus RNA (most closely to that of the coxsackie B virus) in their muscles while all of the 29 controls tested negative. 28 of the 48 CFS patients had an abnormal lactate response to exercise, including 9 of the 10 who tested positive for enterovirus RNA.<ref>{{cite journal | author = Lane RJ, Soteriou BA, Zhang H, Archard LC | title = Enterovirus related metabolic myopathy: a postviral fatigue syndrome. | journal = J Neurol Neurosurg Psychiatry | volume = 74 | issue = 10 | pages = 1382-6 | year = 2003 | id = PMID 14570830}}</ref> |
|||
Another common condition that often co-occurs with ME/CFS is hypermobile [[Ehlers–Danlos syndrome]] (EDS).<ref name="NICE-2021-D" />{{Rp|page=57}} Unlike ME/CFS, EDS is present from birth. People with ME/CFS are more often [[Hypermobility (joints)|hypermobile]] compared to the general population.<ref name="BMJbest_practice3" />{{rp||page=|pages=28–29}} [[Sleep apnea|Sleep apnoea]] may also co-occur with ME/CFS.<ref name="BMJbest_practice3" />{{Rp|page=16}} However, many diagnostic criteria require ruling out sleep disorders before confirming a diagnosis of ME/CFS.<ref name="IQWiG-2023" />{{Rp|page=7}} |
|||
*A study found that fatigue persists in a significant minority of patients for six months or more after infections, suggesting post-infective fatigue syndrome is a valid illness model for investigating CFS.<ref name="PMID:16950834">{{cite journal | author = Hickie I, Davenport T, Wakefield D, Vollmer-Conna U, Cameron B, Vernon SD, Reeves WC, Lloyd A; Dubbo Infection Outcomes Study Group | title = Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study. | journal = BMJ | volume = 333 | issue = 7568 | pages = 575 | year = 2006 | id = PMID 16950834}}</ref> |
|||
Like with other [[Chronic condition|chronic illnesses]], depression and anxiety co-occur frequently with ME/CFS. Depression may be [[Differential diagnosis|differentially diagnosed]] by the presence of feelings of worthlessness, the [[Anhedonia|inability to feel pleasure]], loss of interest, and/or guilt, and the absence of ME/CFS bodily symptoms such as [[autonomic dysfunction]], pain, migraines, and PEM.<ref name="BMJbest_practice3" />{{rp|27}} People with chronic fatigue, which is not due to ME/CFS or other chronic illnesses, may be diagnosed with [[Idiopathic chronic fatigue|idiopathic (unexplained) chronic fatigue]].<ref name="BMJbest_practice3" />{{rp|32}} |
|||
* In a study on people who had glandular fever (which is caused by the Epstein-Barr virus), no difference was found between the levels of virus in the blood from patients who recovered quickly when compared with those whose fatigue lasted more than six months, although the latter had an altered immune response. The scientists involved believed this suggests CFS can be caused by neurological damage done (during the acute infection phase) to parts of the brain which control perception of fatigue and pain.<ref>{{cite journal | author = Cameron B, Bharadwaj M, Burrows J, Fazou C, Wakefield D, Hickie I, Ffrench R, Khanna R, Lloyd A | title = Prolonged illness after infectious mononucleosis is associated with altered immunity but not with increased viral load. | journal = J Infect Dis | volume = 193 | issue = 5 | pages = 664-71 | year = 2006 | id = PMID 16453261}}</ref> |
|||
== Management == |
|||
* Abnormal lactic acid responses to exercise in some CFS patients,<ref name="pmid9631403">{{cite journal |author=Lane RJ, Barrett MC, Taylor DJ, Kemp GJ, Lodi R |title=Heterogeneity in chronic fatigue syndrome: evidence from magnetic resonance spectroscopy of muscle |journal=Neuromuscul. Disord. |volume=8 |issue=3-4 |pages=204–9 |year=1998 |pmid=9631403 |doi=}}</ref><ref name="pmid9527150">{{cite journal |author=Lane RJ, Barrett MC, Woodrow D, Moss J, Fletcher R, Archard LC |title=Muscle fibre characteristics and lactate responses to exercise in chronic fatigue syndrome |journal=J. Neurol. Neurosurg. Psychiatr. |volume=64 |issue=3 |pages=362–7 |year=1998 |pmid=9527150 |doi=}}</ref><ref name="pmid14570830">{{cite journal |author=Lane RJ, Soteriou BA, Zhang H, Archard LC |title=Enterovirus related metabolic myopathy: a postviral fatigue syndrome |journal=J. Neurol. Neurosurg. Psychiatr. |volume=74 |issue=10 |pages=1382–6 |year=2003 |pmid=14570830 |doi=}}</ref> has been suggested to be a factor in CFS because it is commonly believed to be responsible for muscle fatigue.<ref name="pmid16540714">{{cite journal |author=Lamb GD, Stephenson DG |title=Point: lactic acid accumulation is an advantage during muscle activity |journal=J. Appl. Physiol. |volume=100 |issue=4 |pages=1410–2; discussion 1414 |year=2006 |pmid=16540714 |doi=10.1152/japplphysiol.00023.2006}}</ref> However, some scientists have found that lactic acid may actually help prevent muscle fatigue rather than cause it, by keeping muscles properly responding to nerve signals.<ref>{{cite journal | author = Pedersen TH, Nielsen OB, Lamb GD, Stephenson DG | title = Intracellular acidosis enhances the excitability of working muscle. | journal = Science | volume = 305 | issue = 5687 | pages = 1144-7 | year = 2004 | id = PMID 15326352}}</ref> |
|||
{{Main|Management of ME/CFS}} |
|||
There is no approved drug treatment or cure for ME/CFS, although some symptoms can be treated or managed. Care for ME/CFS involves multidisciplinary healthcare professionals. Usually, the primary care clinician plays an important role in coordinating health care, social care and educational support for those still in school. This coordinator can help provide access to community resources such as [[occupational therapy]] and [[District nurse|district nursing]]. Management may start with treating the most disabling symptom first, and tackle symptoms one by one in further health care visits.<ref name="BMJbest_practice3" />{{Rp|page=46}} |
|||
* Essential fatty acid levels: Several studies published between 1990 a 2005 reported finding reduced levels of Omega-6 or Omega-3 [[essential fatty acids]] in [[cell membranes]] or [[serum]] in patients diagnosed with postviral fatigue syndrome or CDC defined CFS.<ref name="isbn0-471-56693-4">{{cite book |author=Horrobin, David F. |title=Omega-6 essential fatty acids: pathophysiology and roles in clinical medicine |publisher=Wiley-Liss |location= New York |year=1990 |pages=275-282 |isbn=0-471-56693-4 |oclc= |doi=}}</ref><ref name="pmid2270749">{{cite journal |author=Behan PO, Behan WM, Horrobin D |title=Effect of high doses of essential fatty acids on the postviral fatigue syndrome |journal=Acta Neurol. Scand. |volume=82 |issue=3 |pages=209-16 |year=1990 |pmid=2270749 |doi=}}</ref> <ref name="pmid1337561">{{cite journal |author=Ogawa R, Toyama S, Matsumoto H. |title=Chronic fatigue syndrome--cases in the Kanebo Memorial Hospital |journal=Nippon Rinsho. |volume=50 |issue=11 |pages=2648-52|year=1992 |pmid=1337561 |doi=}}</ref><ref name="pmid14744043">{{cite journal |author=Liu Z, Wang D, Xue Q, ''et al'' |title=Determination of fatty acid levels in erythrocyte membranes of patients with chronic fatigue syndrome |journal=Nutritional neuroscience |volume=6 |issue=6 |pages=389-92 |year=2003 |pmid=14744043 |doi=}}</ref><ref name="pmid16380690">{{cite journal |author=Maes M, Mihaylova I, Leunis JC |title=In chronic fatigue syndrome, the decreased levels of omega-3 poly-unsaturated fatty acids are related to lowered serum zinc and defects in T cell activation |journal=Neuro Endocrinol. Lett. |volume=26 |issue=6 |pages=745–51 |year=2005 |pmid=16380690 |doi=}}</ref>One study conducted in 1999 on Oxford criteria defined CFS patients (Warren et al.) found no significant differences in fatty acid levels between treatment and placebo groups.<ref name="pmid10071170">{{cite journal |author=Warren G, McKendrick M, Peet M |title=The role of essential fatty acids in chronic fatigue syndrome. A case-controlled study of red-cell membrane essential fatty acids (EFA) and a placebo-controlled treatment study with high dose of EFA |journal=Acta Neurol. Scand. |volume=99 |issue=2 |pages=112-6 |year=1999 |pmid=10071170 |doi=}}</ref> There have also been two controlled systematic proton neurospectroscopy studies of CFS patients that found raised levels of choline in brain areas consistent with an abnormality of essential fatty acid and phospholipid metabolism in the brain in CFS patients.<ref name="pmid16935966">{{cite journal |author=Puri BK |title=Long-chain polyunsaturated fatty acids and the pathophysiology of myalgic encephalomyelitis (chronic fatigue syndrome) |journal=J. Clin. Pathol. |volume=60 |issue=2 |pages=122–4 |year=2007 |pmid=16935966 |doi=10.1136/jcp.2006.042424}}</ref><ref name="pmid15041033">{{cite journal |author=Puri BK |title=The use of eicosapentaenoic acid in the treatment of chronic fatigue syndrome |journal=Prostaglandins Leukot. Essent. Fatty Acids |volume=70 |issue=4 |pages=399–401 |year=2004 |pmid=15041033 |doi=10.1016/j.plefa.2003.12.015}}</ref> These changes have been considered due to essential fatty acid deficiencies resulting from delta 6 [[desaturase]] (D6D) enzyme inhibition in CFS. Some researchers have suggested D6D inhibition is linked to a possible viral cause.<ref name="isbn0-9695662-0-4">{{cite book | author = Nightingale Research Foundation; Goldstein, Jay E.; Byron M. Hyde | title = The Clinical and scientific basis of myalgic encephalomyelitis/chronic fatigue syndrome | publisher = Nightingale Research Foundation | location = Ogdensburg, N.Y | year = 1992 | pages =628-633 | isbn = 0-9695662-0-4 | oclc = | doi = }}</ref> <ref name="pmid16935966">{{cite journal |author=Puri BK |title=Long-chain polyunsaturated fatty acids and the pathophysiology of myalgic encephalomyelitis (chronic fatigue syndrome) |journal=J. Clin. Pathol. |volume=60 |issue=2 |pages=122–4 |year=2007 |pmid=16935966 |doi=10.1136/jcp.2006.042424}}</ref><ref name="pmid15041033">{{cite journal |author=Puri BK |title=The use of eicosapentaenoic acid in the treatment of chronic fatigue syndrome |journal=Prostaglandins Leukot. Essent. Fatty Acids |volume=70 |issue=4 |pages=399–401 |year=2004 |pmid=15041033 |doi=10.1016/j.plefa.2003.12.015}}</ref><ref>{{cite journal |last=Carruthers |first=BM |authorlink= |coauthors=Jain AK et. al. |year=2003 |month= |title=Myalgic Encephomyelitis / Chronic fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols (a Consensus Document) |journal=Journal of Chronic Fatigue Syndrome |volume=11 |issue=1 |pages=66 |id= |url= |accessdate= |quote= }}</ref> However, researchers at an Australian University of Newcastle who reported finding, in CDC criteria defined CFS patients; a dysregulation in D6D enzyme activity and fatty acid changes consistent with an inflammatory mediated event. Found that both gradual and sudden onset had the same fatty acid anomaly differentiaiting them from controls, the primary lipid changes were potentially non-viral induced. Whilst sudden onset CFS patients could be differentiated by a key post-viral modification to fatty acids. <ref> McGregor N.R. Dunstan H.R. et al. 1998 “Alterations in Plasma Lipid Composition in Patients with CFS” presented at Conference; The Clinical and Scientific Basis of CFS, Sydney 1998, P38 </ref> <ref> McGregor N.R. Dunstan H.R. et al. 1998 “Assessment of Lipid Homeostasis in Sudden and Gradual Onset CFS Patients” presented at Conference; The Clinical and Scientific Basis of CFS, Sydney 1998, P39 </ref> |
|||
[[Pacing (activity management)|Pacing]], or managing one's activities to stay within energy limits, can reduce episodes of [[Post-exertional malaise|PEM]]. Addressing sleep problems with good [[sleep hygiene]], or medication if required, may be beneficial. Chronic pain is common in ME/CFS, and the CDC recommends consulting with a pain management specialist if [[over-the-counter]] painkillers are insufficient. For cognitive impairment, adaptations like organisers and calendars may be helpful.<ref name=CDC2024manage /> |
|||
* Carnitine deficiency; is said to produce symptoms of fatigue and myalgia similar to PVFS, ME and CFS. <ref name="isbn0-9695662-0-4">{{cite book | author = Nightingale Research Foundation; Goldstein, Jay E.; Byron M. Hyde | title = The Clinical and scientific basis of myalgic encephalomyelitis/chronic fatigue syndrome | publisher = Nightingale Research Foundation | location = Ogdensburg, N.Y | year = 1992 | pages =628-633 | isbn = 0-9695662-0-4 | oclc = | doi = }}</ref> <ref name="isbn0-471-92846-1">{{cite book |author=Jenkins, Rachel; Mowbray, James F. |title=Post-viral fatigue syndrome (Myalgic encephalomyelitis) |publisher=Wiley |location=New York |year=1991 |Chapter= Essential fatty acids and post viral fatigue syndrome, Author; Horribin DF, pp 393-404 |isbn=0-471-92846-1 |oclc= |doi=}}</ref> <ref name="pmid8148455">{{cite journal |author=Kuratsune H, Yamaguti K, Takahashi M, Misaki H, Tagawa S, Kitani T |title=Acylcarnitine deficiency in chronic fatigue syndrome |journal=Clin. Infect. Dis. |volume=18 Suppl 1 |issue= |pages=S62–7 |year=1994 |pmid=8148455 |doi=}}</ref> Several studies have reported finding [[carnitine]] abnormalities in CFS patients. including lower serum total carnitine, free carnitine and acylcarnitine levels.<ref name="pmid8544970">{{cite journal |author=Plioplys AV, Plioplys S |title=Serum levels of carnitine in chronic fatigue syndrome: clinical correlates |journal=Neuropsychobiology |volume=32 |issue=3 |pages=132–8 |year=1995 |pmid=8544970 |doi=}}</ref><ref name="pmid9854142">{{cite journal |author=Kuratsune H, Yamaguti K, Lindh G, ''et al'' |title=Low levels of serum acylcarnitine in chronic fatigue syndrome and chronic hepatitis type C, but not seen in other diseases |journal=Int. J. Mol. Med. |volume=2 |issue=1 |pages=51–6 |year=1998 |pmid=9854142 |doi=}}</ref><ref name="pmid8148455">{{cite journal |author=Kuratsune H, Yamaguti K, Takahashi M, Misaki H, Tagawa S, Kitani T |title=Acylcarnitine deficiency in chronic fatigue syndrome |journal=Clin. Infect. Dis. |volume=18 Suppl 1 |issue= |pages=S62–7 |year=1994 |pmid=8148455 |doi=}}</ref> The findings of reduced brain uptake of [[acetylcarnitine]] suggest that the levels of biosynthesis of [[neurotransmitters]] through acetylcarnitine might be reduced in some brain regions of CFS patients.<ref name="pmid12414265">{{cite journal |author=Kuratsune H, Yamaguti K, Lindh G, ''et al'' |title=Brain regions involved in fatigue sensation: reduced acetylcarnitine uptake into the brain |journal=Neuroimage |volume=17 |issue=3 |pages=1256–65 |year=2002 |pmid=12414265 |doi=}}</ref><ref name="pmid17561689">{{cite journal |author=Miwa S, Takikawa O |title=[Chronic fatigue syndrome and neurotransmitters] |language=Japanese |journal=Nippon Rinsho |volume=65 |issue=6 |pages=1005–10 |year=2007 |pmid=17561689 |doi=}}</ref> There has been a contradictory study that included Oxford criteria defined patients. Others report of finding reduced levels of carnitine together with reduced essential fatty acids in patients with CDC defined CFS.<ref name="pmid15967423">{{cite journal |author=Jones MG, Goodwin CS, Amjad S, Chalmers RA |title=Plasma and urinary carnitine and acylcarnitines in chronic fatigue syndrome |journal=Clin. Chim. Acta |volume=360 |issue=1-2 |pages=173–7 |year=2005 |pmid=15967423 |doi=10.1016/j.cccn.2005.04.029}}</ref><ref name="pmid15932738">{{cite journal |author=Li YJ, Wang DX, Bai XL, ''et al'' |title=[Clinical characteristics of patients with chronic fatigue syndrome: analysis of 82 cases] |language=Chinese |journal=Zhonghua Yi Xue Za Zhi |volume=85 |issue=10 |pages=701–4 |year=2005 |pmid=15932738 |doi=}}</ref> Carnitine and its esters are considered to regulate the immune networks and inflammation, through carnitine-dependent; transfer of fatty acids into cells, and mitochondrial energy production from beta-oxidation of long-chain fatty acids. A gene expression study indicates altered; carnitine function, mitochondrial function, and fatty acid metabolism in PVFS. Also that profiles of plasma lipids in subgroups of CDC defined CFS patients suggest anomalies including beta-oxidation of fatty acids. <ref name="pmid16448567">{{cite journal |author=Vernon SD, Whistler T, Cameron B, Hickie IB, Reeves WC, Lloyd A |title=Preliminary evidence of mitochondrial dysfunction associated with post-infective fatigue after acute infection with Epstein Barr virus |journal=BMC Infect. Dis. |volume=6 |issue= |pages=15 |year=2006 |pmid=16448567 |doi=10.1186/1471-2334-6-15}}</ref> <ref> McGregor N.R. Dunstan H.R. et al. 1998 “Classification of CFS Patients by Assessing Plasma lipid Homeostasis” presented at Conference; The Clinical and Scientific Basis of CFS, Sydney 1998, P40 </ref> <ref name="pmid15591010">{{cite journal |author=Famularo G, De Simone C, Trinchieri V, Mosca L |title=Carnitines and its congeners: a metabolic pathway to the regulation of immune response and inflammation |journal=Ann. N. Y. Acad. Sci. |volume=1033 |issue= |pages=132–8 |year=2004 |pmid=15591010 |doi=10.1196/annals.1320.012}}</ref> <ref name="pmid10540873">{{cite journal |author=Saheki T |title=[Carnitine as a vitamin-like biofactor] |language=Japanese |journal=Nippon Rinsho |volume=57 |issue=10 |pages=2270–5 |year=1999 |pmid=10540873 |doi=}}</ref> |
|||
[[Comorbid|Co-occurring conditions]] that may interact with and worsen ME/CFS symptoms are common, and treating these may help manage ME/CFS.<ref name="Bateman-2021" /> Commonly diagnosed ones include [[fibromyalgia]], irritable bowel syndrome, migraines and [[mast cell activation syndrome]].<ref name="BMJbest_practice3" />{{Rp|page=19}} The debilitating nature of ME/CFS can cause depression, [[anxiety]], or other psychological problems, which can be treated.<ref name="CDC2024manage" /> People with ME/CFS may be unusually sensitive to medications, especially ones that affect the central nervous system.<ref>{{Cite web |date=10 May 2024 |title=Monitoring the Use of Medicines and Supplements |url=https://www.cdc.gov/me-cfs/hcp/clinical-care/monitoring-the-use-of-medicines-and-supplements.html |access-date=25 May 2024 |archive-url=https://web.archive.org/web/20240525121239/https://www.cdc.gov/me-cfs/hcp/clinical-care/monitoring-the-use-of-medicines-and-supplements.html|archive-date=25 May 2024|publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC) }}</ref> |
|||
* Researchers have found that children and teenagers with CFS are several times more likely to have some hyperflexible joints<ref>{{cite journal | author = Barron DF, Cohen BA, Geraghty MT, Violand R, Rowe PC | title = Joint hypermobility is more common in children with chronic fatigue syndrome than in healthy controls. | journal = J Pediatr | volume = 141 | issue = 3 | pages = 421-5 | year = 2002 | id = PMID 12219066}}</ref> in an association with [[Ehlers-Danlos syndrome]]. |
|||
=== Pacing and energy management === |
|||
==Diagnosis== |
|||
[[File:FitbitIonicMomentDisplay.jpg|upright=1.35|thumb|A heart rate monitor can be helpful for energy management.|alt=A smart watch displaying heart rate on a person's wrist]] |
|||
At this time, there is no accepted conclusive test or series of tests of chronic fatigue syndrome. CFS is therefore largely an ''[[Diagnosis of exclusion|exclusionary diagnosis]]''. If a doctor suspects a patient may have CFS they should begin the diagnostic process by eliminating other potential causes of the patient's symptoms, as "chronic fatigue" and related symptoms can be caused by a wide variety of conditions which should be investigated and managed.<ref name=NICECG53>National Institute for Health and Clinical Excellence. ''Guideline 53: Chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy)''. London, 2007. ISBN 1846294533. [http://guidance.nice.org.uk/CG53 NICE CG53 page].</ref> |
|||
[[Pacing (activity management)|Pacing]], or activity management, involves balancing periods of rest with periods of activity.<ref name="CDC_strategies2024" /> The goal of pacing is to stabilize the illness and avoid triggering PEM.<ref name="Hoffmann_2024" /> This involves staying within an individual's available ''energy envelope'' to reduce the PEM "payback" caused by overexertion.<ref name="Jason2017">{{cite journal |vauthors=O'Connor K, Sunnquist M, Nicholson L, Jason LA, Newton JL, Strand EB |date=March 2019 |title=Energy Envelope Maintenance Among Patients with Myalgic Encephalomyelitis and Chronic Fatigue Syndrome: Implications of Limited Energy Reserves |journal=Chronic Illness |volume=15 |issue=1 |pages=51–60 |doi=10.1177/1742395317746470 |pmc=5750135 |pmid=29231037}}</ref> The technique was developed for ME/CFS in the 1980s.<ref name="Goudsmit2011">{{cite journal | vauthors = Goudsmit EM, Nijs J, Jason LA, Wallman KE | title = Pacing as a strategy to improve energy management in myalgic encephalomyelitis/chronic fatigue syndrome: a consensus document | journal = Disability and Rehabilitation | volume = 34 | issue = 13 | pages = 1140–1147 | date = 19 December 2011 | pmid = 22181560 | doi = 10.3109/09638288.2011.635746 |url=https://repository.uel.ac.uk/item/85yxz | access-date = 23 May 2020 | url-status = live | s2cid = 22457926 | archive-url=https://web.archive.org/web/20200728130945/https://repository.uel.ac.uk/item/85yxz | archive-date = 28 July 2020 }}</ref> |
|||
Pacing can involve breaking up large tasks into smaller ones and taking extra breaks, or creating easier ways to do activities. For example, this might include sitting down while doing the laundry. The decision to stop an activity (and rest or change an activity) is determined by self-awareness of a worsening of symptoms. Use of a [[heart rate monitor]] may help some individuals with pacing.<ref name="CDC2024manage" /> |
|||
===CDC 1994 criteria=== |
|||
The criteria most used in scientific research are those of the [[Centers for Disease Control and Prevention]] of 1994 by Fukuda e.a.<ref name="CDC1994"/> The following conditions must be met. |
|||
Research on pacing and energy envelope theory typically shows positive effects.<ref name="Jason2017" /><ref name="Sanal-Hayes_2023">{{cite journal |vauthors=Sanal-Hayes NE, Mclaughlin M, Hayes LD, Mair JL, Ormerod J, Carless D, Hilliard N, Meach R, Ingram J, Sculthorpe NF |date=October 2023 |title=A Scoping Review of 'Pacing' for Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Lessons Learned for the Long COVID Pandemic |journal=Journal of Translational Medicine |volume=21 |issue=1 |pages=720 |doi=10.1186/s12967-023-04587-5 |pmc=10576275 |pmid=37838675 |doi-access=free}}</ref> However, these studies have often had a low number of participants and have rarely included methods to check if study participants implemented pacing well.<ref name="Sanal-Hayes_2023" /> Pacing is difficult to apply for people with very severe ME/CFS, as the activities that trigger PEM in this group, such as eating, cannot be avoided completely.<ref name="Hoffmann_2024" /> |
|||
;Primary symptom |
|||
Clinically evaluated, unexplained, persistent or relapsing chronic fatigue that is: |
|||
* of new or definite onset (has not been lifelong); |
|||
* is not the result of ongoing exertion; |
|||
* is not substantially alleviated by rest; |
|||
* and results in substantial reduction in previous levels of occupational, educational, social, or personal activities. |
|||
Those with a stable illness who understand how to "listen to their body" may be able to carefully and flexibly increase their activity levels.<ref name="CDC_strategies2024" /> The goal of an exercise programme would be to increase stamina, while not interfering with everyday tasks or making the illness more severe.<ref name="BMJbest_practice3" />{{Rp|page=56}} In many chronic illnesses, intense exercise is beneficial, but in ME/CFS it is not recommended. The CDC states:<ref name="CDC2024manage" /> |
|||
;Additional requirement |
|||
The concurrent occurrence of four or more of the following symptoms, all of which must have persisted or recurred during 6 or more consecutive months of illness and must not have predated the fatigue: |
|||
#self-reported impairment in [[short-term memory]] or [[concentration]] severe enough to cause substantial reduction in previous levels of occupational, educational, social, or personal activities; |
|||
#[[sore throat]]; |
|||
#tender cervical or axillary [[lymph nodes]]; |
|||
#[[muscle pain]]; |
|||
#multi-[[joint pain]] without joint swelling or redness; |
|||
#[[headaches]] of a new type, pattern, or severity; |
|||
#unrefreshing [[sleep]]; |
|||
#post-exertional [[malaise]] lasting more than 24 hours. |
|||
{{blockquote|Vigorous aerobic exercise can benefit people with many chronic illnesses. But people with ME/CFS do not tolerate such exercise routines. Standard exercise recommendations for healthy people can be harmful for patients with ME/CFS. However, it is important that patients with ME/CFS undertake activities that they can tolerate.}} |
|||
;Final requirement |
|||
All other known causes of chronic fatigue must have been ruled out, specifically clinical depression, side effects of medication, eating disorders and substance abuse. |
|||
[[Graded exercise therapy]] (GET), a proposed treatment for ME/CFS that assumes deconditioning and a fear of activity play important roles in maintaining the illness, is no longer recommended for people with ME/CFS.<ref name="pmid37793728" /><ref name="BMJbest_practice3" />{{Rp|page=38}} Reviews of GET either see weak evidence of a small to moderate effect<ref name="Chou_2022">{{Cite book |url=https://www.cdc.gov/me-cfs/pdfs/systematic-review/file1-final-report-MECFS-Systematic-Review-508.pdf |title=Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): An Updated Systematic Evidence Review |vauthors=Chou R, McDonagh M, Griffins J, Grusing S |publisher= U.S. [[Centers for Disease Control and Prevention]] |year=2022 |access-date=30 March 2023 |archive-url=https://web.archive.org/web/20240214175237/https://www.cdc.gov/me-cfs/pdfs/systematic-review/file1-final-report-MECFS-Systematic-Review-508.pdf |archive-date=14 February 2024 |url-status=dead}}</ref><ref name="Lar20192">{{cite journal |vauthors=Larun L, Brurberg KG, Odgaard-Jensen J, Price JR |date=October 2019 |title=Exercise Therapy for Chronic Fatigue Syndrome |journal=The Cochrane Database of Systematic Reviews |volume=10 |issue=10 |pages=CD003200 |doi=10.1002/14651858.CD003200.pub8 |pmc=6953363 |pmid=31577366}}</ref> or no evidence of effectiveness.<ref name="Geraghty_2019">{{cite journal |vauthors=Geraghty K, Jason L, Sunnquist M, Tuller D, Blease C, Adeniji C |date=23 April 2019 |title=The 'Cognitive Behavioural Model' of Chronic Fatigue Syndrome: Critique of a Flawed Model |journal=Health Psychology Open |volume=6 |issue=1 |pages=2055102919838907 |doi=10.1177/2055102919838907 |pmc=6482658 |pmid=31041108}}</ref><ref name="Ahmed_2020">{{cite journal |vauthors=Ahmed SA, Mewes JC, Vrijhoef H |date=February 2020 |title=Assessment of the Scientific Rigour of Randomized Controlled Trials on the Effectiveness of Cognitive Behavioural Therapy and Graded Exercise Therapy for Patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Systematic Review |journal=Journal of Health Psychology |volume=25 |issue=2 |pages=240–255 |doi=10.1177/1359105319847261 |pmid=31072121 |s2cid=149443976}}</ref> GET can have serious adverse effects.<ref name="Hoffmann_2024" /> Similarly, a form of [[Cognitive behavioral therapy|cognitive behavioural therapy]] (CBT) that assumed the illness is maintained by unhelpful beliefs about the illness and avoidance of activity is no longer recommended.<ref name="Bateman-2021" /> |
|||
The clinical evaluation should include: |
|||
# A thorough history that covers medical and psychosocial circumstances at the onset of fatigue; depression or other psychiatric disorders; episodes of medically unexplained symptoms; alcohol or other substance abuse; and current use of prescription and over-the-counter medications and food supplements. |
|||
# A mental status examination to identify abnormalities in mood, intellectual function, memory, and personality. Particular attention should be directed toward current symptoms of depression or anxiety, self-destructive thoughts, and observable signs such as psychomotor retardation. Evidence of a psychiatric or neurologic disorder requires that an appropriate psychiatric, psychological, or neurologic evaluation be done. |
|||
# A thorough physical examination. |
|||
# A minimum battery of laboratory screening tests including complete blood count with leukocyte differential; erythrocyte sedimentation rate; serum levels of alanine aminotransferase, total protein, albumin, globulin, alkaline phosphatase, calcium, phosphorus, glucose, blood urea nitrogen, electrolytes, and creatinine; determination of thyroid-stimulating hormone; and urinalysis. |
|||
=== Symptom relief === |
|||
According to Fukuda e.a., other tests have no known value, unless indicated on an individual basis to confirm or exclude a differential diagnosis, such as [[multiple sclerosis]]. |
|||
The first management step for sleep problems in ME/CFS is improving sleep habits. If sleep problems remain after implementing sleep hygiene routines, [[Cognitive behavioral therapy for insomnia|cognitive behavioural therapy for insomnia]] can be offered. Avoiding naps during the day can further improve sleep,<ref name="BMJbest_practice3" />{{Rp|page=41}} but there may be a trade-off with needed rest during the day.<ref name="NICE2021" />{{rp|36}} Drugs that help with insomnia in fibromyalgia, such as [[trazodone]] or [[suvorexant]], may help in ME/CFS too.<ref name="pmid37793728" /> |
|||
Pain is initially managed with over-the-counter pain medication, such as [[ibuprofen]] or [[paracetamol]] ([[Paracetamol|acetaminophen]]). If this is insufficient, referral to a pain specialist or counselling on pain management can be the next step. Heat treatment, [[hydrotherapy]] and gentle massage can sometimes help. In addition, stretching and exercise may help with pain, but a balance must be struck, as they can trigger PEM.<ref name="CDC_strategies2024" /> While there is lack of evidence on pharmaceutical options for pain management in ME/CFS, medication that works for fibromyalgia may be tried, such as [[pregabalin]].<ref name="BMJbest_practice3" />{{Rp|page=42}}<ref name="pmid37793728" /> |
|||
===NICE (UK) 2007 criteria=== |
|||
The UK [[National Institute for Health and Clinical Excellence]] (NICE), published a multidisciplinary [[clinical practice guideline]] in 2007 in which the following criteria are employed:<ref name=NICECG53/> |
|||
* fatigue that is new, persistent and/or recurrent, not explained by other conditions and has resulted in a substantial reduction in activity level characterised by post-exertional malaise and/or fatigue (typically delayed, for example by at least 24 hours, with slow recovery over several days) ''and'' |
|||
* one or more of the following list of symptoms: difficulty with sleeping, muscle and/or joint pain at multiple sites without evidence of inflammation, headaches, painful lymph nodes that are not pathologically enlarged, sore throat, cognitive dysfunction, worsening of symptoms by physical or mental exertion, general malaise, dizziness and/or nausea and palpitations with no identifiable heart problem. |
|||
Like in other chronic illnesses, those with ME/CFS often experience mental health issues like anxiety and depression.<ref name="Bateman-2021" /> [[Psychotherapy]], such as CBT may help manage the stress of being ill and teach self-management strategies.<ref name="NICE2021" />{{Rp|page=42}} Family sessions may be useful to educate people close to those with ME/CFS about the severity of the illness.<ref name="BMJbest_practice3" />{{Rp|page=41}} [[Antidepressant]]s can be useful, but there may be more side effects than in the general population. For instance, it may be difficult to stop weight gain due to exercise intolerance.<ref name="BMJbest_practice3" />{{Rp|page=52}} |
|||
The diagnosis should be reconsidered if none of the following symptoms remain: post-exertional fatigue or malaise, cognitive difficulties, sleep disturbance, chronic pain.<ref name=NICECG53/> |
|||
Bowel issues are a common symptom of ME/CFS. For some, eliminating specific foods, such as [[caffeine]], [[Alcohol and health|alcohol]], [[gluten]], or dairy, can alleviate symptoms.<ref name="Bateman-2021" /> Those with orthostatic intolerance can benefit from increased salt and fluid intake.<ref name="Bateman-2021" /> [[Compression stockings]] can help with orthostatic intolerance.<ref name="Bateman-2021" /> |
|||
The guideline requires fatigue to have been present for 4 months in an adult or 3 months in a child. It expects a diagnosis in a child to be made by a pediatrician. There are no recommendations on who is to make the diagnosis in an adult. The guideline states that a referral to a ME/CFS specialist should be offered immediately to the severely ill.<ref name=NICECG53/> |
|||
=== Severe ME/CFS === |
|||
The NICE criteria have been criticized by patients' associations for being far too relaxed, recommending controversial CBT/GET and ignoring the WHO classification of CFS/ME as a neurological condition.<ref>{{cite web |url=http://www.meassociation.org.uk/content/view/335/ |title=The ME Association - NICE guideline on ME/CFS - MEA statement |accessdate = 2007-10-09 |format= |work=}}</ref> |
|||
People with moderate to severe ME/CFS may benefit from home adaptations and mobility aids, such as [[wheelchair]]s, disability parking, [[Transfer bench|shower chairs]], or [[stair lift]]s. To manage sensitivities to environmental stimuli, these stimuli can be limited. For instance, the surroundings can be made perfume-free, or an [[Blindfold|eye mask]] or [[earplug]]s can be used.<ref name="BMJbest_practice3" />{{Rp|pages=39–40}} Those with severe ME/CFS may have significant trouble getting nutrition. [[Parenteral nutrition|Intravenous feeding]] (via blood) or [[Feeding tube|tube feeding]] may be necessary to address this or to address [[electrolyte imbalance]]s.<ref name="pmid37793728" /> |
|||
Patients who cannot move easily in bed may need help to prevent [[Pressure ulcer|pressure sores]]. Regular repositioning is important to keep their joints flexible and prevent [[contracture]]s and stiffness. [[Osteoporosis]] may pose a risk over the long term.<ref>{{Cite web |date=13 May 2024 |title=ME/CFS Clinical Care for Severely Affected Patients |url=https://www.cdc.gov/me-cfs/hcp/clinical-care/me-cfs-clinical-care-for-severely-affected-patients.html |archive-url=https://web.archive.org/web/20240528171310/https://www.cdc.gov/me-cfs/hcp/clinical-care/me-cfs-clinical-care-for-severely-affected-patients.html |archive-date=28 May 2024 |access-date=15 June 2024 |publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC) |url-status=live}}</ref> Symptoms of severe ME/CFS may be misunderstood as neglect or abuse during well-being evaluations, and NICE recommends that professionals with experience in ME/CFS should be involved in any type of assessment for [[safeguarding]].<ref name="NICE2021" />{{rp|22}} |
|||
===Other systems=== |
|||
Other scoring systems have also been proposed to quantify CFS symptoms for research purposes. These include: |
|||
* Holmes ''et al'' (1988) scoring system.<ref name=Holmes1988>{{cite journal | author = Holmes G, Kaplan J, Gantz N, Komaroff A, Schonberger L, Straus S, Jones J, Dubois R, Cunningham-Rundles C, Pahwa S | title = Chronic fatigue syndrome: a working case definition. | journal = Ann Intern Med | volume = 108 | issue = 3 | pages = 387-9 | year = 1988 | id = PMID 2829679}} [http://www.medicineau.net.au/clinical/medicine/CFS.html#holmes Details]</ref> Also sometimes called "CDC 1988," to distinguish from the newer CDC system. |
|||
* Oxford criteria (1991)<ref name="oxford"/> |
|||
* Carruthers ''et al'' (2003) Canadian Case definition for ME/CFS<ref name="carr"/> |
|||
* Australian Guidelines (2004)<ref>[http://www.cfids-cab.org/MESA/AU_CFS.pdf Australian Guidelines (2004)]</ref> |
|||
== Prognosis == |
|||
===Issues with the definitions/criteria=== |
|||
Information on the [[prognosis]] of ME/CFS is limited. Complete recovery, partial improvement, and worsening are all possible,<ref name="CDC_Clinical2024" /> but full recovery is uncommon.<ref name="IQWiG-2023" />{{Rp|page=11}} Symptoms generally fluctuate over days, weeks, or longer periods, and some people may experience periods of remission. Overall, many will have to adjust to life with ME/CFS.<ref name="NICE2021"/>{{Rp|pages=20}} |
|||
;Selection bias and inconsistencies |
|||
Several studies have found that using different case definitions ( eg broad vs conservative<ref>{{cite journal | author = Jason LA, Corradi K, Torres-Harding S, Taylor RR, King C | title = Chronic fatigue syndrome: the need for subtypes. | journal = Neuropsychol Rev | volume = 15 | issue = 1 | pages = 29-58 | year = 2005 | id = PMID 15929497}}</ref> ) has major influence on the types of patients selected and have also supported the distinction between specific subgroups of CFS to be identified and/or for the case definition to be further clarified with emphasis on using empirical studies: An international CFS study group for the CDC found ambiguities in the CDC 1994 CFS research case definition which contribute to inconsistent case identification.<ref>{{cite journal | author = Reeves WC, Lloyd A, Vernon SD, Klimas N, Jason LA, Bleijenberg G, Evengard B, White PD, Nisenbaum R, Unger ER | title = Identification of ambiguities in the 1994 chronic fatigue syndrome research case definition and recommendations for resolution. | journal = BMC Health Serv Res | volume = 3 | issue = 1 | pages = 25 | year = 2003 | id = PMID 14702202 | url = http://www.biomedcentral.com/1472-6963/3/25}}</ref> Researchers have found that a difference in the self-reported cause of a patient's CFS is associated with significant differences in clinical measures and outcomes, and concluded it is likely that their response to treatment may vary and the CFS definition should be improved to define more homogeneous groups of patients for the purposes of research and treatment.<ref>{{cite journal | author = Kennedy G, Abbot NC, Spence V, Underwood C, Belch JJ | title = The specificity of the CDC-1994 criteria for chronic fatigue syndrome: comparison of health status in three groups of patients who fulfill the criteria. | journal = Ann Epidemiol | volume = 14 | issue = 2 | pages = 95-100 | year = 2004 | id = PMID 15018881}}</ref> It also may be inappropriate to synthesize results from CFS studies that use different definitions to select study populations.<ref name="PMID_12629919">{{cite journal | author = Jason LA, Helgerson J, Torres-Harding SR, Carrico AW, Taylor RR | title = Variability in diagnostic criteria for chronic fatigue syndrome may result in substantial differences in patterns of symptoms and disability. | journal = Eval Health Prof | volume = 26 | issue = 1 | pages = 3-22 | year = 2003 | id = PMID 12629919}}</ref> It has been found that identification of new diagnostic symptoms, the use of severity ratings for symptomatology, and the identification of standardized measures that differentiate cases of CFS from other conditions; all hold promise for improving the sensitivity, specificity, and reliability of the diagnostic criteria for CFS.<ref>{{cite journal | author = King C, Jason LA | title = Improving the diagnostic criteria and procedures for chronic fatigue syndrome. | journal = Biol Psychol | volume = 68 | issue = 2 | pages = 87-106 | year = 2005 | id = PMID 15450690}}</ref> |
|||
An early diagnosis may improve care and prognosis.<ref name="NICE-2021-D" /> Factors that may make the disease worse over days, but also over longer periods, are physical and mental exertion, a new infection, sleep deprivation, and emotional stress.<ref name="IQWiG-2023" />{{Rp|page=11}} Some people who improve need to manage their activities to prevent a relapse.<ref name="CDC_Clinical2024" /> Children and teenagers are more likely to recover or improve than adults.<ref name="CDC_Clinical2024" /><ref name="NICE2021"/>{{Rp|pages=20}} For instance, a study in Australia among 6- to 18-year-olds found that two-thirds reported recovery after 10 years and that the typical duration of illness was five years.<ref name="IQWiG-2023" />{{Rp|page=11}} |
|||
;Improving accuracy |
|||
A study found that the best predictors for people accurately fitting the CDC 1994 definition of CFS were the presence of postexertional malaise, unrefreshing sleep, and impaired memory-concentration, and this accuracy increased when severity of these symptoms were taken into account.<ref name="PMID_17078775">{{cite journal | author = Hawk C, Jason LA, Torres-Harding S | title = Differential diagnosis of chronic fatigue syndrome and major depressive disorder. | journal = Int J Behav Med | volume = 13 | issue = 3 | pages = 244-51 | year = 2006 | id = PMID 17078775}}</ref> Another examination of the CDC's working case definition(s) of CFS found that the differential accuracy is strengthened when eliminating three symptoms (muscle weakness, joint pain, sleep disturbance) and adding two others (anorexia, nausea).<ref>{{cite journal | author = Komaroff AL, Fagioli LR, Geiger AM, Doolittle TH, Lee J, Kornish RJ, Gleit MA, Guerriero RT | title = An examination of the working case definition of chronic fatigue syndrome. | journal = Am J Med | volume = 100 | issue = 1 | pages = 56-64 | year = 1996 | id = PMID 8579088}}</ref> It has also been found that the Canadian 2003 definition (a less used but stricter criteria) selects cases with less [[psychiatry|psychiatric]] co-morbidity, more physical functional impairment, and more fatigue/weakness, [[neuropsychiatry|neuropsychiatric]], and neurological symptoms.<ref name="DOI_10.1300/J092v12n01_03">{{cite journal | author = Jason LA, Torres-Harding SR, Jurgens A, Helgerson J | title = Comparing the Fukuda et al. Criteria and the Canadian Case Definition for Chronic Fatigue Syndrome. | journal = Journal of Chronic Fatigue Syndrome | volume = 12 | issue = 1 | pages = 37 - 52 | year = 2004 | doi = 10.1300/J092v12n01_03}}</ref> |
|||
The effect of ME/CFS on [[life expectancy]] is poorly studied, and the evidence is mixed. One large retrospective study on the topic found no increase in all-cause mortality due to ME/CFS. Death from suicide was, however, significantly higher among those with ME/CFS.<ref name="BMJbest_practice3" />{{Rp|page=59}} In extreme cases, people can die from the illness.<ref name="Hoffmann_2024">{{cite journal | vauthors = Hoffmann K, Hainzl A, Stingl M, Kurz K, Biesenbach B, Bammer C, Behrends U, Broxtermann W, Buchmayer F, Cavini AM, Fretz GS, Gole M, Grande B, Grande T, Habermann-Horstmeier L, Hackl V, Hamacher J, Hermisson J, King M, Kohl S, Leiss S, Litzlbauer D, Renz-Polster H, Ries W, Sagelsdorff J, Scheibenbogen C, Schieffer B, Schön L, Schreiner C, Thonhofer K, Strasser M, Weber T, Untersmayr E | title = Interdisziplinäres, kollaboratives D-A-CH Konsensus-Statement zur Diagnostik und Behandlung von Myalgischer Enzephalomyelitis/Chronischem Fatigue-Syndrom | trans-title = Interdisciplinary, collaborative D-A-CH (Germany, Austria and Switzerland) consensus statement concerning the diagnostic and treatment of myalgic encephalomyelitis/chronic fatigue syndrome | language = de | journal = Wiener Klinische Wochenschrift | volume = 136 | issue = Suppl 5 | pages = 103–123 | date = August 2024 | pmid = 38743348 | pmc = 11093804 | doi = 10.1007/s00508-024-02372-y }}</ref> |
|||
;Possible subtypes |
|||
Studies suggest the existence of CFS subtypes.<ref>{{cite journal | author = Jason LA, Taylor RR, Kennedy CL, Jordan KM, Song S, Johnson D, Torres-Harding S | title = Chronic fatigue syndrome: symptom subtypes in a community based sample. | journal = Women Health | volume = 37 | issue = 1 | pages = 1-13 | year = 2003 | id = PMID 12627607}}</ref><ref>{{cite journal | author = Jason LA, Taylor RR, Kennedy CL, Song S, Johnson D, Torres S | title = Chronic fatigue syndrome: occupation, medical utilization, and subtypes in a community-based sample. | journal = J Nerv Ment Dis | volume = 188 | issue = 9 | pages = 568-76 | year = 2000 | id = PMID 11009329}}</ref> After examining the 'minor' diagnostic symptoms of CFS in women meeting the CDC 1994 criteria, researchers found that 3 subtypes could be identified; musculoskeletal, infectious and neurological; with associated impairment characteristic of each subtype. "Extreme scores" characterized about 2/3 of the sample, with higher disability in those with the highest scores. Depression and anxiety were not more prevalent in any particular subtype, and did not increase with the severity of specific symptom reports.<ref>{{cite journal | author = Janal MN, Ciccone DS, Natelson BH | title = Sub-typing CFS patients on the basis of 'minor' symptoms. | journal = Biol Psychol | volume = 73 | issue = 2 | pages = 124-31 | year = 2006 | id = PMID 16473456}}</ref> |
|||
== Epidemiology == |
|||
;Diagnosis inaccuracies |
|||
[[File:ME-CFS Incidence Rate by Age.png|alt=Graph showing that females have two incidence peaks (teenagers and 30–39 years old), and males' incidence peaks in the teenager years.|thumb|upright=1.35|Incidence rates by age and sex, from a 2014 study in Norway]] |
|||
A review published in 2006 found that the accurate diagnosis of CFS is low<ref>{{cite journal | author = Maoz D, Shoenfeld Y | title = Chronic fatigue syndrome | journal = Harefuah | volume = 145 | issue = 4 | pages = 272-5, 319, 318 | year = 2006 | id = PMID 16642629}}</ref> and another study found that physicians have a tendency to underrecognize psychiatric illness, especially when assessing patients whose chronic fatigue is fully explainable by a psychiatric disorder and who may be misdiagnosed with CFS.<ref>{{cite journal | author = Torres-Harding SR, Jason LA, Cane V, Carrico A, Taylor RR | title = Physicians' diagnoses of psychiatric disorders for people with chronic fatigue syndrome. | journal = Int J Psychiatry Med | volume = 32 | issue = 2 | pages = 109-24 | year = 2002 | id = PMID 12269593}}</ref> |
|||
Reported prevalence rates vary widely depending on how ME/CFS is defined and diagnosed. Overall, around one in 150 people have ME/CFS. Based on the 1994 CDC diagnostic criteria, the global prevalence rate for CFS is 0.89%. In comparison, estimates using the stricter 1988 CDC criteria or the 2003 Canadian Consensus Criteria for ME/CFS produced a prevalence rate of only 0.17%.<ref name=Lim2020/> |
|||
In England and Wales, over 250,000 people are estimated to be affected.<ref name="NICE2021" />{{Rp|pages=92}} These estimates are based on data before the [[COVID-19 pandemic]]. It is likely that numbers have increased as a large share of people with [[long COVID]] meet the diagnostic criteria of ME/CFS.<ref name="IQWiG-2023" />{{Rp|page=228|pages=}} A 2021–2022 [[National Health Interview Survey|CDC survey]] found that 1.3% of adults in the United States, or 3.3 million, had ME/CFS.<ref>{{Cite report |url=https://www.cdc.gov/nchs/products/databriefs/db488.htm |title=Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in Adults: United States, 2021–2022 |date=8 December 2023 |publisher=[[National Center for Health Statistics]] |issue=488 |doi=10.15620/cdc:134504 |pages=1–8 |pmid=38085820 |id=NCHS Data Brief |access-date=8 December 2023 |archive-url=https://web.archive.org/web/20240217000708/https://www.cdc.gov/nchs/products/databriefs/db488.htm |archive-date=17 February 2024 |url-status=live |doi-access=free |vauthors=Vahratian A, Lin JS, Bertolli J, Unger ER}}</ref> <!-- 2020 census US adult population: 258.3M --> |
|||
;Terminology implications |
|||
Because of the similarity in terminology, CFS is often confused with "chronic fatigue". Fatigue in the perceived absence of disease has traditionally been seen within the purview of psychiatry.<ref>Ryan TA (1944). Varieties of Fatigue. ''Am J Psychol'' '''57''';565-569. {{DOI|10.2307/1417252}}.</ref> A study found that while most medical trainees consider the symptom complex of CFS to be a serious illness resulting in poor quality of life, the "chronic fatigue syndrome" name may be regarded less seriously than the "myalgic encephalopathy" name.<ref>{{cite journal | author = Jason LA, Taylor RR, Plioplys S, Stepanek Z, Shlaes J | title = Evaluating attributions for an illness based upon the name: chronic fatigue syndrome, myalgic encephalopathy and Florence Nightingale disease. | journal = Am J Community Psychol | volume = 30 | issue = 1 | pages = 133-48 | year = 2002 | id = PMID 11928774}}</ref> Another study found that nurses and physician assistants viewed a patient's CFS symptoms as more severe and disabling if they were told the patient had a more medical sounding diagnosis of "chronic neuroendocrineimmune dysfunction syndrome".<ref>{{cite journal | author = Jason LA, Holbert C, Torres-Harding S, Taylor RR, LeVasseur JJ, Breitinger P, LaBarbera D, Siegel L | title = Chronic fatigue syndrome versus neuroendocrineimmune dysfunction syndrome:differential attributions. | journal = J Health Soc Policy | volume = 18 | issue = 1 | pages = 43-55 | year = 2003 | id = PMID 15189800}}</ref> |
|||
Women are diagnosed with ME/CFS about 1.5 to four times more often than men.<ref name=Lim2020/><ref name="CDCEpide2023" /> The prevalence in children and adolescents is slightly lower than in adults,<ref name="Lim2020" /> and children have it less than adolescents.<ref>{{Cite web |date=31 May 2024 |title=Fast Facts: ME/CFS |url=https://www.cdc.gov/me-cfs/about/fast-facts-about-me-cfs.html |access-date=15 June 2024 |publisher=U.S. [[Centers for Disease Control and Prevention]] (CDC) |language=en-us|archive-url=https://web.archive.org/web/20240603101152/https://www.cdc.gov/me-cfs/about/fast-facts-about-me-cfs.html|archive-date=3 June 2024}}</ref> The [[Incidence (epidemiology)|incidence]] rate (the onset of ME/CFS) has two peaks, one at 10–19 and another at 30–39 years,<ref name="pmid31379194">{{cite journal | vauthors = Collard SS, Murphy J | title = Management of chronic fatigue syndrome/myalgic encephalomyelitis in a pediatric population: A scoping review | journal = Journal of Child Health Care | volume = 24 | issue = 3 | pages = 411–431 | date = September 2020 | pmid = 31379194 | pmc = 7863118 | doi = 10.1177/1367493519864747 }}</ref> and the [[prevalence]] is highest in [[middle age]].<ref name="CDC_Basics" /> |
|||
===Testing=== |
|||
There is no generally accepted diagnostic test to reliably diagnose or exclude chronic fatigue syndrome. Research has not identified an association between CFS and one particular virus. |
|||
== History == |
|||
According to the [[CDC]], the main purpose of performing diagnostic tests of any sort is to rule out other causes for fatigue and other symptoms of CFS.<ref name="CDC1994"/> Routine tests recommended by the CDC: |
|||
{{Main|History of ME/CFS}}From 1934 onwards, there were multiple outbreaks globally of an unfamiliar illness, initially mistaken for [[polio]]. A 1950s outbreak at London's [[Royal Free Hospital]] led to the term "benign myalgic encephalomyelitis" (ME). Those affected displayed symptoms such as malaise, [[sore throat]], [[pain]], and signs of [[Encephalomyelitis|nervous system inflammation]]. While its infectious nature was suspected, the exact cause remained elusive.<ref name="IOM2015" />{{rp|28–29}} The syndrome appeared in sporadic as well as epidemic cases.<ref>{{cite journal |vauthors=Price JL |date=April 1961 |title=Myalgic Encephalomyelitis |journal=Lancet |volume=1 |issue=7180 |pages=737–738 |doi=10.1016/s0140-6736(61)92893-8 |pmc=1836797 |pmid=13737972}}</ref> |
|||
* [[Complete blood count]] |
|||
* Blood chemistry ([[electrolyte]]s, [[glucose]], [[renal function]], [[liver enzyme]]s, protein levels and [[calcium in biology|calcium]]) |
|||
* [[Thyroid function test]]s |
|||
* [[Erythrocyte sedimentation rate]] (ESR) |
|||
* [[Urinalysis]] for blood cells, protein and glucose |
|||
In 1970, two UK psychiatrists proposed that these ME outbreaks were [[psychosocial]] phenomena, suggesting [[Mass psychogenic illness|mass hysteria]] or altered medical perception as potential causes. This theory, though challenged, sparked controversy and cast doubt on ME's legitimacy in the medical community.<ref name="IOM2015" />{{rp|28–29}} |
|||
The 2007 UK NICE guideline includes, in addition to the CDC panel: [[C-reactive protein]] (a marker of inflammation), [[creatine kinase]] (a muscle-related enzyme), plasma [[viscosity]] (optional if ESR done) and [[serology]] for [[celiac disease]]. [[Ferritin]] determination may be performed in children and young people, and in adults only if other tests suggest iron deficiency. The guideline recommends clinical judgement in decisions to perform other tests in addition to the standard set. Testing for infections (e.g. Lyme disease, viral hepatitis, HIV, mononucleosis, toxoplasmosis or cytomegalovirus) is only recommended if the patient gives a specific history for this. Routine performance of the head-up tilt test, auditory brainstem responses and electrodermal conductivity is discouraged.<ref name=NICECG53/> |
|||
[[Melvin Ramsay]]'s later research highlighted ME's disabling nature, prompting the removal of "benign" from the name and the creation of diagnostic criteria in 1986. These criteria included the tendency of muscles to tire after minor effort and take multiple days to recover, high symptom variability, and chronicity. Despite Ramsay's work and a UK report affirming that ME was not a psychological condition, scepticism persisted within the medical field, leading to limited research.<ref name="IOM2015" />{{rp|28–29}} |
|||
In contrast, the [[Nightingale Research Foundation]] recommends extensive testing including brain imaging and tests for neuropsychological, sleep, muscle, vascular and cardiac dysfunction to diagnose ME/CFS<ref>Hyde B. (2007), "The Nightingale Myalgic Encephalomyelitis (M.E.) Definition", The Nightingale Research Foundation, Ottawa, Canada</ref>. |
|||
In the United States, Nevada and New York State saw outbreaks of what appeared similar to [[Infectious mononucleosis|mononucleosis]] in the middle of the 1980s. People suffered from "chronic or recurrent fatigue", among a large number of other symptoms.<ref name="IOM2015" />{{rp|28–29}} The initial link between elevated antibodies and the Epstein–Barr virus led to the name "chronic Epstein–Barr virus syndrome". The CDC renamed it chronic fatigue syndrome (CFS), as a viral cause could not be confirmed in studies.<ref name="Packard 2004">{{cite book |url=https://books.google.com/books?id=EGNFPZrKIKMC&pg=PA156 |title=Emerging Illnesses and Society: Negotiating the Public Health Agenda |vauthors=Packard RM |publisher=[[Johns Hopkins University Press]] |year=2004 |isbn=978-0-8018-7942-5 |pages= |access-date=6 February 2024 |archive-url=https://web.archive.org/web/20230518113959/https://books.google.com/books?id=EGNFPZrKIKMC&pg=PA156 |archive-date=18 May 2023 |url-status=live}}</ref>{{Rp|155–158}} An initial case definition of CFS was outlined in 1988;<ref name="IOM2015" />{{rp|28–29}} the CDC published new [[Medical diagnosis|diagnostic criteria]] in 1994, which became widely referenced.<ref name="Brurberg2014rev">{{cite journal |vauthors=Brurberg KG, Fønhus MS, Larun L, Flottorp S, Malterud K |date=February 2014 |title=Case Definitions for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME): A Systematic Review |journal=BMJ Open |volume=4 |issue=2 |pages=e003973 |doi=10.1136/bmjopen-2013-003973 |pmc=3918975 |pmid=24508851}}</ref> |
|||
Suhadolnik, DeMeirleir e.a. developed a test to measure the fragmentation of the enzyme RNAse L. This fragmentation was found to be significant in CFS and has some use as a marker, but the test has limited availability<ref name="Suhadolnik97"/>. |
|||
In the 2010s, ME/CFS began to gain more recognition from health professionals and the public. Two reports proved key in this shift. In 2015, the US [[National Academy of Medicine|Institute of Medicine]] produced a report with new diagnostic criteria that described ME/CFS as a "serious, chronic, complex systemic disease". Following this, the US [[National Institutes of Health]] published their ''Pathways to Prevention'' report, which gave recommendations on research priorities.<ref>{{Cite journal |vauthors=Friedberg F |date=2 January 2020 |title=Legitimizing Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Indications of Change over a Decade |url=https://www.tandfonline.com/doi/full/10.1080/21641846.2020.1718292 |journal=Fatigue: Biomedicine, Health & Behavior |volume=8 |issue=1 |pages=24–31 |doi=10.1080/21641846.2020.1718292 |s2cid=214434278 |issn=2164-1846 |access-date=4 February 2024 |archive-date=4 February 2024 |archive-url=https://web.archive.org/web/20240204175310/https://www.tandfonline.com/doi/full/10.1080/21641846.2020.1718292 |url-status=live }}</ref> |
|||
===Diagnostic controversies=== |
|||
Historically, many doctors have been unfamiliar with CFS, and some have refused to diagnose it. Others minimised the seriousness of CFS.<ref>{{cite journal | author = Jason LA, Richman JA, Friedberg F, Wagner L, Taylor R, Jordan KM | title = Politics, science, and the emergence of a new disease. The case of chronic fatigue syndrome. | journal = Am Psychol | volume = 52 | issue = 9 | pages = 973-83 | year = 1997 | id = PMID 9301342}}</ref> This situation is changing somewhat, with more doctors willing to diagnose it. In the UK, the 2002 [[Chief Medical Officer, United Kingdom|Chief Medical Officer]]'s report stated that all doctors should consider CFS as a serious chronic illness — and treat patients accordingly.<ref name=CMOrept2002>CFS/ME Working Group. ''A report of the CFS/ME working group: report to the chief medical officer of an independent working group.'' London: Department of Health, 2002. [http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4064840 Fulltext at DOH].</ref> Similar progress has been made in the United States.<ref name="CDC-awareness"/><ref name="CDCToolkit">Centers for Disease Control and Prevention (2006), "[http://www.cdc.gov/cfs/toolkit.htm] CFS Toolkit: Fact Sheets for Healthcare Professionals"</ref> |
|||
== Society and culture == |
|||
There remains considerable skepticism amongst some medical professionals about the existence of CFS as a "real" — i.e. medical as opposed to behavioral — condition, possibly due to the extreme uncertainty of its [[etiology]], and the lack of testing for biomedical [[Medical sign|signs]] and its largely exclusionary definition. Many people are inclined to believe that a condition with few or no specific biomedical markers may be psychological in origin. This had led to a frustration in many patients, who feel that their disability is not psychological, but biological, and point to the epidemic history and biomedical research trends. Alternatively, some doctors and patients believe that the illnesses are real, but conceptualising them under a CFS banner amounts to misdiagnosis, largely due to the near-absolute exclusion of physical and laboratory signs required by the popular CFS criteria and the excuse to give up looking for treatable abnormalities. |
|||
[[File:Petition presentation by M.E Support in Glamorgan.jpg|thumb|upright=1.35|Presentation of a petition to the [[Senedd|National Assembly for Wales]] relating to ME support in South East Wales|alt=a group of people offering a petition. The group includes a person on a camp bed holding up a placard that says she is in bed 23 hours a day.]] |
|||
=== Controversy === |
|||
Some patients' groups and experts state that research into CFS (ME) in the UK has been mostly hijacked by a "lobby of psychologists and psychiatrists",<ref name="gibson_report">[http://www.erythos.com/gibsonenquiry/Report.html Report of the Group on Scientific Research into Myalgic Encephalomyelitis] 2006</ref>, who they claim hold significant power within the medical fraternity, with a resultant "gross abuse/neglect of patients."<ref name="hooper_pathol_06"/> The UK and the [[Netherlands]] have particularly seen disagreements between biomedical researchers and their adherents, and psychiatrists (particularly proponents of [[cognitive behavioral therapy]], or CBT) and supporters of the theory that CFS is psychological in origin, and can be "cured" or "rehabilitated" by [[psychotherapy]] and [[exercise]].<ref>{{cite journal | author = Van Houdenhove B | title = What is the aim of cognitive behaviour therapy in patients with chronic fatigue syndrome? | journal = Journal of Psychotherapy and Psychosomatics | volume = 75 | issue = 6 | pages = 396-7 | year = 2006 | id = PMID 17053343}}</ref> |
|||
{{Main|Controversies related to ME/CFS}} |
|||
ME/CFS is a contested illness, with debates mainly revolving around the cause of the illness and treatments.<ref name="pmid29971693" /> Historically, there was a heated discussion about whether the condition was psychological or neurological.<ref name="Lim_2020" /> Professionals who subscribed to the psychological model had frequent conflicts with patients, who believed their illness to be organic.<ref name="pmid32601171">{{cite journal |vauthors=O'Leary D |date=December 2020 |title=A Concerning Display of Medical Indifference: Reply to 'Chronic Fatigue Syndrome and an Illness-Focused Approach to Care: Controversy, Morality and Paradox' |url= |journal=Medical Humanities |volume=46 |issue=4 |pages=e4 |doi=10.1136/medhum-2019-011743 |pmid=32601171 |s2cid=220253462}}</ref> While ME/CFS is now generally believed to be a multisystem neuroimmune condition,<ref name="Lim_2020" /> a subset of professionals still see the condition as [[Psychosomatic medicine|psychosomatic]], or an "illness-without-disease".<ref name="pmid32601171" /><ref>{{Cite journal |last=Geraghty |first=Keith |date=2020-07-02 |title=The Negative Impact of the Psychiatric Model of Chronic Fatigue Syndrome on Doctors' Understanding and Management of the Illness |url=https://www.tandfonline.com/doi/full/10.1080/21641846.2020.1834295 |journal=Fatigue: Biomedicine, Health & Behavior |language=en |volume=8 |issue=3 |pages=167–180 |doi=10.1080/21641846.2020.1834295 |issn=2164-1846}}</ref> |
|||
Further controversy persists regarding the redefinition of ME as CFS in 1988 and whether they are in fact essentially different, if perhaps overlapping, entities. This dispute is reflected in debate over nomenclature or definition writ small, with stakes being high for all parties as this informs choice of treatment, research, management and funding policy. Psychiatrists refute the suggestion of the Gibson Report that excessive funding has been given to psychiatric research, despite that extremely few Medical Research Council studies have been into the pathoetiology of the illness. In his submission to the NICE guidelines panel, UK CFS specialist psychologist Peter Denton White disputed needs for disability aids for the severely affected and rejected the possibility of neuropathic pain and other features found in ME. Following a recent BBC radio show Dr White is reported to have contradicted his own broadcast stance by allegedly clarifying to co-guest, Dr William Weir, that ME ''"is an abnormal illness belief”''. Dr White claims to have misinterpreted the question as one of abnormal illness beliefs in general.<ref>Regarding “Whiter than white?” : Response from Prof Peter Denton White [http://meagenda.wordpress.com/2007/11/07/regarding-whiter-than-white-response-from-prof-peter-denton-white/]</ref> |
|||
The possible role of chronic viral infection in ME/CFS has been a subject of disagreement. One study caused considerable controversy by establishing a causal relationship between ME/CFS and a [[retrovirus]] called [[Xenotropic murine leukemia virus–related virus|XMRV]]. Some with the illness began taking [[Management of HIV/AIDS|antiretroviral drugs]] targeted specifically for [[HIV/AIDS]], another retrovirus,<ref>{{Cite web | vauthors = Westly E |date= June 2011 |title=Retrovirus No Longer Thought to Be Cause of Chronic Fatigue Syndrome |url=https://www.scientificamerican.com/article/virus-no-longer-thought-cause-chronic-fatigue-syndrome/ |url-status=live |archive-url=https://web.archive.org/web/20240222054928/https://www.scientificamerican.com/article/virus-no-longer-thought-cause-chronic-fatigue-syndrome/ |archive-date=22 February 2024 |access-date=22 February 2024 |website=Scientific American }}</ref> and national blood supplies were suspected to be tainted with the retrovirus. After several years of study, the XMRV findings were determined to be the result of contamination of the testing materials.<ref name="pmid27358491">{{cite journal |vauthors=Johnson AD, Cohn CS |title=Xenotropic Murine Leukemia Virus-Related Virus (XMRV) and the Safety of the Blood Supply |journal=Clinical Microbiology Reviews |volume=29 |issue=4 |pages=749–57 |date=October 2016 |pmid=27358491 |pmc=5010753 |doi=10.1128/CMR.00086-15 |url=}}</ref> |
|||
Proponents of "lumping" insist there is insufficient evidence as to the existence of a discrete ME, and that they are equivalent. Detractors respond that if they were equivalent, there would be no resistence to referencing the term ME, that the popular CFS definition bears little or no resemblence to ME, and that ever-increasingly vague, misleading criteria and heterogeneity benefit no-one. ME activists insist that medical education of the historical database of published ME findings is suppressed in favour of biased appeals to the psychiatric paradigm such as the criticised 1996 Royal Colleges Report, reviews which cherry-pick study inclusions and a publishing "preference" of some journals such as the BMJ for psychosocial papers revolving around unsupportable psychosomatic explanations such as "interoception". The assertion of equivalency relies on disputing any definitive ME signs and findings, despite advances such as the 2003 Consensus definition which even use compound terminology. |
|||
Treatments based on behavioural and psychological models of the illness have also been the subject of much contention. The largest clinical trial on behavioural interventions, the 2011 [[PACE trial]], concluded that graded exercise therapy and [[Cognitive behavioral therapy|CBT]] are moderately effective. The trial drew heavy criticism.<ref name="pmid29971693">{{cite journal |vauthors=Blease C, Geraghty KJ |date=September 2018 |title=Are ME/CFS Patient Organizations 'Militant'? : Patient Protest in a Medical Controversy |url=|journal=Journal of Bioethical Inquiry |volume=15 |issue=3 |pages=393–401 |doi=10.1007/s11673-018-9866-5 |pmid=29971693 |s2cid=49677273}}</ref> The study authors [[Outcome switching|weakened their definition of recovery]] during the trial: some participants now met a key criterion for recovery before the trial started. A reanalysis under the original [[Protocol (science)|clinical trial protocol]] showed no significant difference in recovery rate between treatment groups and the controls receiving standard care.<ref name="pmid28805517">{{cite journal |vauthors=Geraghty KJ |date=August 2017 |title=Further Commentary on the PACE Trial: Biased Methods and Unreliable Outcomes |url=|journal=Journal of Health Psychology |volume=22 |issue=9 |pages=1209–1216 |doi=10.1177/1359105317714486 |pmid=28805517}}</ref><ref name="pmid31637650">{{cite journal |vauthors=Friedberg F, Sunnquist M, Nacul L |date=March 2020 |title=Rethinking the Standard of Care for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome |url=|journal=Journal of General Internal Medicine |volume=35 |issue=3 |pages=906–909 |doi=10.1007/s11606-019-05375-y |pmc=7080939 |pmid=31637650}}</ref> |
|||
All three ME specialists present at the CDC's naming board refused to endorse the descriptor of CFS and Dr Holmes was unknown for any work in this field previously; since then co-author Professor Komaroff has admitted the CFS definition was "a mistake". Dr Reeves of the CDC has stated that the epidemics described historically as ME were "not CFS". Recently the IACFS has voted to change its name to the IACFSME with a view to phasing out CFS, although they have made no associated changes to definition. Reasons cited for keeping CFS are American insurance claims and easy recognition of recent research carried out under the CFS umbrella. |
|||
=== Doctor–patient relations === |
|||
The UK Department of Health has in parliament recognised the WHO classifaction and ME is recognised in a 1988 Bill of Rights, despite the establishment largely insisting on ME-CFS equivalency. It is debatable whether the NHS recognises ME at all and frequently documentation on CFS refers to "chronic fatigue", insisting that there are no signs or testable abnormalities. |
|||
People with ME/CFS often face stigma in healthcare settings,<ref name="Hussein-2024" /> and the majority of individuals report negative healthcare experiences. They may feel that their doctor inappropriately calls their illness psychological or doubts the severity of their symptoms.<ref name="McManimen-2019">{{cite journal |vauthors=McManimen S, McClellan D, Stoothoff J, Gleason K, Jason LA |date=March 2019 |title=Dismissing Chronic Illness: A Qualitative Analysis of Negative Health Care Experiences |journal=Health Care for Women International |volume=40 |issue=3 |pages=241–258 |doi=10.1080/07399332.2018.1521811 |pmc=6567989 |pmid=30829147}}</ref> They may also feel forced to prove that they are legitimately ill.<ref name="pmid16085344">{{cite journal |vauthors=Dumit J |date=February 2006 |title=Illnesses You Have to Fight to Get: Facts as Forces in Uncertain, Emergent Illnesses |journal=Social Science & Medicine |volume=62 |issue=3 |pages=577–590 |doi=10.1016/j.socscimed.2005.06.018 |pmid=16085344}}</ref> Some may be given outdated treatments that provoke symptoms or assume their illness is due to unhelpful thoughts and deconditioning.<ref name="Bateman-2021" />{{Rp|page=2871}}<ref name="Davis-2023" /> |
|||
Clinicians may be unfamiliar with ME/CFS, as it is often not fully covered in medical school.<ref name="Davis-2023" /> Due to this unfamiliarity, people may go undiagnosed for years<ref name="Bateman-2021" /> or be misdiagnosed with mental health conditions.<ref name="Davis-2023" /> As individuals gain knowledge about their illness over time, their relationship with treating physicians changes. They may feel on a more equal footing with their doctors and able to work in partnership. At times, relationships may deteriorate instead as the previous asymmetry of knowledge breaks down.<ref name="Shortland_2024">{{Cite journal | vauthors = Shortland D, Fazil Q, Lavis A, Hallett N |date=4 April 2024 |title=A Systematic Scoping Review of How People with ME/CFS Use the Internet |journal=Fatigue: Biomedicine, Health & Behavior |language=en |volume=12 |issue=2 |pages=142–176 |doi=10.1080/21641846.2024.2303887 |issn=2164-1846 |doi-access=free}}</ref> |
|||
Recently the CDC has made its position clear, stating on 26th december 2007 that: |
|||
=== Economic and social impact === |
|||
<blockquote> |
|||
ME/CFS negatively impacts people's social lives and relationships. Stress can be compounded by disbelief in the illness from the support network, who can be sceptical due to the subjective nature of diagnosis. Many people with the illness feel [[Social isolation|socially isolated]], and [[Suicidal ideation|thoughts of suicide]] are high, especially in those without a supportive care network.<ref name="Shortland_2024" /> ME/CFS interrupts [[Child development|normal development]] in children, making them more dependent on their family for assistance instead of gaining independence as they age.<ref name="pmid28087544">{{cite journal |vauthors=Parslow RM, Harris S, Broughton J, Alattas A, Crawley E, Haywood K, Shaw A |date=January 2017 |title=Children's Experiences of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME): A Systematic Review and Meta-Ethnography Of Qualitative Studies |url=|journal=BMJ Open |volume=7 |issue=1 |pages=e012633 |doi=10.1136/bmjopen-2016-012633 |pmc=5253584 |pmid=28087544}}</ref> Caring for somebody with ME/CFS can be a full-time role, and the stress of caregiving is made worse by the lack of effective treatments.<ref>{{cite journal |vauthors=O'Dwyer S, Boothby S, Smith G, Biddle L, Muirhead N, Khot S |date=July 2022 |title=Unpaid Carers Are the Missing Piece in Treatment Guidelines and Research Priorities for ME/CFS |url=https://orca.cardiff.ac.uk/id/eprint/156445/1/bmj.o1691.full.pdf |url-status=live |journal=BMJ |volume=378 |pages=o1691 |doi=10.1136/bmj.o1691 |pmid=35835467 |s2cid=250533596 |archive-url=https://web.archive.org/web/20240306063412/https://orca.cardiff.ac.uk/id/eprint/156445/1/bmj.o1691.full.pdf |archive-date=6 March 2024 |access-date=21 February 2024 |hdl-access=free |hdl=10871/130699}}</ref> |
|||
'''"Various terms are incorrectly used interchangeably with CFS. CFS has an internationally accepted case definition that is used in research and clinical settings. ... The name myalgic encephalomyelitis (ME) was coined in the 1950s to clarify well-documented outbreaks of disease; however, ME is accompanied by neurologic and muscular signs and has a case definition distinct from that of CFS"''' <ref>CDC declaration on terminology and definition, on 26th Dec 2007[http://www.cdc.gov/cfs/cme/wb1032/chapter1/overview.html]</ref> |
|||
</blockquote> |
|||
Economic costs due to ME/CFS are significant.<ref>{{cite journal | vauthors = Pheby DF, Araja D, Berkis U, Brenna E, Cullinan J, de Korwin JD, Gitto L, Hughes DA, Hunter RM, Trepel D, Wang-Steverding X | title = The Development of a Consistent Europe-Wide Approach to Investigating the Economic Impact of Myalgic Encephalomyelitis (ME/CFS): A Report from the European Network on ME/CFS (EUROMENE) | journal = Healthcare | volume = 8 | issue = 2 | pages = 88 | date = April 2020 | pmid = 32272608 | pmc = 7349118 | doi = 10.3390/healthcare8020088 | doi-access = free }}</ref> In the United States, estimates range from $36 to $51 billion per year, considering both lost wages and healthcare costs.<ref>{{Cite journal |vauthors=Jason LA, Mirin AA |date=January 2021 |title=Updating the National Academy of Medicine ME/CFS Prevalence and Economic Impact Figures to Account for Population Growth and Inflation |url=https://solvecfs.org/wp-content/uploads/2021/02/Jason-Mirin_Prevalence_econ_update.pdf |url-status=live |journal=Fatigue: Biomedicine, Health & Behavior |volume=9 |issue=1 |pages=9–13 |doi=10.1080/21641846.2021.1878716 |issn=2164-1846 |s2cid=233745601 |archive-url=https://web.archive.org/web/20230315073408/https://solvecfs.org/wp-content/uploads/2021/02/Jason-Mirin_Prevalence_econ_update.pdf |archive-date=15 March 2023 |access-date=21 January 2023}}</ref> A 2017 estimate for the annual economic burden in the United Kingdom was £3.3 billion.<ref name="Dibble McGrath Ponting 2020 p." /> |
|||
==Treatment== |
|||
{{POV-section|date=December 2007}} |
|||
Many patients do not fully recover from CFS, even with treatment<ref>{{cite journal | author = Rimes KA, Chalder T. | title = Treatments for chronic fatigue syndrome. | journal = Occupational Medicine | volume = 55 | issue = 1 | pages = 32-39 | year = 2005 | id = PMID 15699088}}</ref>. Some management strategies are suggested to reduce the consequences of having CFS. A sytematic review has shown that CFS patients are less susceptible to placebo effects than predicted, and have a low placebo response compared to patients with other diseases.<ref>{{cite journal | author = Cho HJ, Hotopf M, Wessely S | title = The placebo response in the treatment of chronic fatigue syndrome: a systematic review and meta-analysis. | journal = Psychosom Med | volume = 67 | issue = 2 | pages = 301-13 | year = 2005 | id = PMID 15784798}}</ref> |
|||
=== |
=== Advocacy === |
||
[[File:Blue awareness ribbon icon with outline.svg|thumb|The blue ribbon is used for ME/CFS awareness.|alt=see caption]] |
|||
Behavioral interventions including [[cognitive behavioral therapy]] (CBT) and [[physical therapy|graded exercise therapy]] (GET) have been shown to be at least partially effective in some people with CFS. A systematic review published in the ''[[Journal of the Royal Society of Medicine]]'' (October 2006)<ref name="cbt_systematic_review">[{{cite journal |author=Chambers D, Bagnall AM, Hempel S, Forbes C |title=Interventions for the treatment, management and rehabilitation of patients with chronic fatigue syndrome/myalgic encephalomyelitis: an updated systematic review |journal=Journal of the Royal Society of Medicine |volume=99 |issue=10 |pages=506-20 |year=2006 |pmid=17021301 |doi=10.1258/jrsm.99.10.506}}</ref> found these are the only two known treatments that seem helpful. The statement of principal findings regarding CBT/GET was: "A number of RCTs (randomised controlled trials) suggest that behavioural interventions, including elements of CBT, GET and rehabilitation, may reduce symptoms and improve physical functioning of people with CFS/ME." However some uncertainty still exists over the efficacy of these treatments, especially GET for severely affected patients, as none were included in studies that passed the inclusion criteria of the review. The review also emphasized the need for more and better conducted studies of both therapies, as well as more research into the adverse affects of treatments in general as they may be under reported or poorly quantified. As mentioned in the review under the 'unanswered questions/further research' section, very few studies assessed the effectiveness of "interventions for children and young people and for severely affected patients." More research is needed on severely affected patients in general; because many treatments and studies require patients to attend a clinic, and those with the worst symptoms often receive the least support from health and social services. The authors also expressed concern about possible bias in the CFS literature, a lack of uniformity in case definitions and study inclusion/exclusion criteria (studies using any CFS criteria were included), and the basic information provided about the participants; which they state makes it difficult to assess the generalizability of the findings of many of these studies. This review found that no intervention had been proved effective in restoring the ability to work. An earlier systematic review published in 2002 also found this, although CBT was "lending a possible association between improvement in the ability to work and an increase in the number of patients employed". This earlier review also found that no specific patient characteristics seemed to serve as best predictors of positive employment outcomes in CFS patients, although did find that depression of greater severity was associated with unemployment.<ref>{{cite journal | author = Ross SD, Levine C, Ganz N, Frame D, Estok R, Stone L, Ludensky V | title = Systematic review of the current literature related to disability and chronic fatigue syndrome. | journal = Evid Rep Technol Assess (Summ) | issue = 66 | pages = 1-3 | year = 2002 | id = PMID 12647509}}</ref> However, another systematic review published in 2004 concluded "Only cognitive behavior therapy, rehabilitation, and exercise therapy interventions were associated with restoring the ability to work."<ref>{{cite journal |author=Ross SD, Estok RP, Frame D, Stone LR, Ludensky V, Levine CB |title=Disability and chronic fatigue syndrome: a focus on function |journal=Arch. Intern. Med. |volume=164 |issue=10 |pages=1098-107 |year=2004 |pmid=15159267 |doi=10.1001/archinte.164.10.1098}}</ref> |
|||
Patient organisations have aimed to involve researchers via activism but also by publishing research themselves—similarly to [[HIV/AIDS activism|AIDS activism]] in the 1980s, which also sought to combat underfunding and stigma. [[Citizen science|Citizen scientists]], for example, helped start discussions about weaknesses in trials of psychological treatments.<ref name="pmid29971693" /> |
|||
[[International May 12th Awareness Day|ME/CFS International Awareness Day]] takes place on 12 May.<ref name="CDC_Awareness">{{cite web |date=10 May 2024 |title=ME/CFS Awareness Day |url=https://www.cdc.gov/me-cfs/awareness-day/ |url-status=live |archive-url=https://web.archive.org/web/20240517200059/https://www.cdc.gov/me-cfs/awareness-day/ |archive-date=17 May 2024 |access-date=17 May 2024 |publisher=U.S. [[Centers for Disease Control and Prevention]]}}</ref> The goal of the day is to raise awareness among the public and health care workers about the diagnosis and treatment of ME/CFS.<ref name="NIH_Awareness">{{cite web |title=Dr. Nancy Lee on International Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Awareness Day|date=12 May 2012|url=https://www.hhs.gov/advcomcfs/cfsac-cfsa-day.html |archive-url=https://web.archive.org/web/20120708024540/http://www.hhs.gov/advcomcfs/cfsac-cfsa-day.html |archive-date=8 July 2012 |access-date=12 October 2013 |publisher=[[United States Department of Health and Human Services|US Department of Health and Human Services]] |vauthors=Lee N}}</ref> The date was chosen because it is the birthday of [[Florence Nightingale]], who had an unidentified illness similar to ME/CFS.<ref name="CDC_Awareness" /> |
|||
The "Gibson Report" (Report of the Group on Scientific Research into Myalgic Encephalomyelitis 2006)<ref name="gibson_report"/>, a political inquiry into the science of CFS provides information about treating CFS with CBT and/or GET. However, the report has been criticised by the ME Association, for: being poorly conducted, misrepresentations, omissions, lack of references, factual inaccuracies or bias, and even potentially damaging implications.<ref>[http://www.afme.org.uk/news.asp?newsid=181] Action for ME's "Review of Gibson Inquiry Report" ([[27 November]] [[2006]])</ref><ref>[http://www.meassociation.org.uk/content/view/135/70] The ME Association's "Gibson Report: key points raised by The ME Association" ([[6 February]] [[2007]])</ref><ref>[http://www.theoneclickgroup.co.uk/documents/ME-CFS_pol/The%20One%20Click%20Group%20Report%20%20-%20The%20Gibson%20Inquiry%20.pdf] The One Click Group's "The One Click Group Report - The Gibson 'Inquiry'" ([[17 January]] [[2007]])</ref> The "25% ME Group", a UK advocacy support group for severely affected M.E. sufferers, state, in their submission to the Gibson report<ref>[http://www.25megroup.org/Campaigning/Gibson%20Inquiry%20Information/25%20final%20sub%20to%20Gibson%20(2).doc]</ref>, that both CBT and GET are unhelpful and may be dangerous/harmful to severely affected CFS patients. The discrepancy between trial results and patient group surveys has been noted by the P.A.C.E. trial group, who are conducting a larger more detailed study into CBT and GET which is currently underway and is due for completion in 2009.<ref>{{cite journal | author = Peter D White, Michael C Sharpe, Trudie Chalder, Julia C DeCesare, Rebecca Walwyn for the PACE trial group | title = Protocol for the PACE trial: A randomised controlled trial of adaptive pacing, cognitive behaviour therapy, and graded exercise as supplements to standardised specialist medical care versus standardised specialist medical care alone for patients with the chronic fatigue syndrome/myalgic encephalomyelitis or encephalopathy. | journal = BMC Neurology 7:6 | year = 2007 | id = DOI 10.1186/1471-2377-7-6 | url = http://www.biomedcentral.com/1471-2377/7/6}}</ref> However, it has without explanation dropped all use of objective measures such as actometers since the original research plan was published. |
|||
== Research == |
|||
====Cognitive Behavioral Therapy (CBT)==== |
|||
[[File:ME-CFS Papers by Year.svg|alt=Graph of ME/CFS papers published by year, showing an increasing trend since about 1985|thumb|upright=1.35|Graph of ME/CFS papers published by year:{{legend|#0062C4|Papers mentioning ME or CFS}}{{legend|#62C400|Papers whose title mentions ME/CFS}}]] Research into ME/CFS seeks to find a better understanding of the disease's causes, biomarkers to aid in diagnosis, and treatments to relieve symptoms.<ref name="IOM2015" />{{Rp|page=10}} The emergence of long COVID has sparked increased interest in ME/CFS, as the two conditions may share pathology and treatment for one may treat the other.<ref name="Marshall-Gradisnik_2022">{{cite journal | vauthors = Marshall-Gradisnik S, Eaton-Fitch N | title = Understanding myalgic encephalomyelitis | journal = Science | volume = 377 | issue = 6611 | pages = 1150–1151 | date = September 2022 | pmid = 36074854 | doi = 10.1126/science.abo1261 | hdl-access = free | s2cid = 252159772 | bibcode = 2022Sci...377.1150M | hdl = 10072/420658 }}</ref><ref name="pmid38443223" /> |
|||
Results from clinical studies have suggested that [[cognitive behavioral therapy]] (CBT) is an effective, [[evidence-based]] therapy for CFS<ref name=cbt_bmj_clinical_evidence>[http://www.clinicalevidence.com/ceweb/conditions/msd/1101/1101_I1.jsp]</ref>. The use of psychological therapies such as CBT does not imply that CFS is a psychiatric condition or that physical symptoms are not real. Some CFS patients have comorbid depression and/or anxiety.<ref>{{cite journal | author = Youssefi M, Linkowski P | title = Chronic fatigue syndrome: psychiatric perspectives | journal = Rev Med Brux | volume = 23 | issue = 4 | pages = A299-304 | year = 2002 | id = PMID 12422451}}</ref> In addition, it is argued{{who?}} that CBT may teach patients various "coping strategies" to help them deal with cognitive impairments such as a deterioration of [[short-term memory]] or abbreviated [[attention span]]{{Fact|date=April 2007}}, although it is uncertain how changing one's [[Schema (psychology)|schemas]], as CBT theory contends, would cause improvement in these serious pathological symptoms{{Fact|date=December 2007}}. Dr. David Smith, a former medical advisor to the ME Association in the UK who reports to have successfully treated many children using [[antidepressants]] and therapy<ref>{{cite journal | author = Patel MX, Smith DG, Chalder T, Wessely S | title = Chronic fatigue syndrome in children: a cross sectional survey | journal = Arch Dis Child | volume = 88|issue = 10|pages = 894-8|year = 2003|id = PMID 14500310 }}</ref>, offers a possible explanation on his website.<ref>[http://www.me-cfs-treatment.com] www.me-cfs-treatment.com</ref> Some patients and patient groups{{Who|date=December 2007}} state that this is innaccurate, arguing that CBT is described as an "exposure therapy" e.g. UK mental health charity MIND,<ref>[http://www.mind.org.uk/Information/Booklets/Understanding/Understanding+talking+treatments.htm] www.mind.org.uk</ref> that most of the conditions commonly listed as being suitable for CBT are behavioural and that the 2002 UK CMO's Report describes CBT as "a tool for constructively modifying attitude and behaviour." Carruthers and Van de Sande in their Overview of the Canadian Consensus Guidelines<ref name="carr2"> </ref>, note that to supportive counselling should not be mis-termed CBT to avoid patient confusion between the two treatments. |
|||
=== Funding === |
|||
The Gibson Report <ref name="gibson_report"/> states that CBT in general is helpful to many people with other illnesses; and while it is controversial in regards to CFS, it seems to be most effective in those with less severe forms but much less effective in the severely affected. Commenting on the relevance of CBT for CFS, the report states that it has a role to play in treatment but at best is only a partial answer and more research is needed. A systematic review on CBT<ref name="cbt_systematic_review"/> finds that "CBT was associated with a significant positive effect on fatigue, symptoms, physical functioning and school attendance." The reviewers state that the quality of many recent trails on CBT are lower quality randomized controlled trials or trials that did not involve random allocation. The reviewers also state that one recent, good quality trial of CBT in children and adolscence supports the effectiveness of CBT. The reviewers state that reasons for withdrawals typically remain unreported, and that a degree of publication bias seems to be present in CFS/ME literature as a whole. In one study, the effect of CBT has been demonstrated up to five years after therapy<ref>{{cite journal | author = Deale A, Husain K, Chalder T, Wessely S | title = Long-term outcome of cognitive behavior therapy versus relaxation therapy for chronic fatigue syndrome: a 5-year follow-up study. | journal = Am J Psychiatry | volume = 158|issue = 12|pages = 2038-42|year = 2001|id = PMID 11729022}}</ref>. A large evaluation study in Belgium, however, lead to the conclusion that while on average CBT may cause patients to feel somewhat better, objective measurement shows no reduction in their disability{{Verify source|date=January 2008}}<ref>RIZIV, "Referentiecentra voor het Chronisch vermoeidheidssyndroom (CVS), evaluatierapport 2002-2004", Brussels, July 2006</ref>. Another recent study found that CBT improved self-reported cognitive impairment but not actual neuropsychological test performance.<ref>{{cite journal | author = Knoop H, Prins JB, Stulemeijer M, van der Meer JW, Bleijenberg G | title = The effect of cognitive behaviour therapy for chronic fatigue syndrome on self-reported cognitive impairments and neuropsychological test performance. | journal = J Neurol Neurosurg Psychiatry | volume = 78 | issue = 4 | pages = 434-6 | year = 2007 | id = PMID 17369597}}</ref> According to researchers of one study, CBT usually aims at reducing fatigue but can also reduce pain, although higher pain at baseline was associated with a negative treatment outcome.<ref>{{cite journal | author = Knoop H, Stulemeijer M, Prins JB, van der Meer JW, Bleijenberg G | title = Is cognitive behaviour therapy for chronic fatigue syndrome also effective for pain symptoms? | journal = Behav Res Ther ([[March 14]] [[2007]]) | id = PMID 17451642}}</ref> The place of CBT for children, young people and the severely affected needs to be better established, although some open studies suggest that it is helpful, so long as it is adapted for the individual patient{{Fact|date=April 2007}}. |
|||
Historical research funding for ME/CFS has been far below that of comparable diseases.<ref name="Tyson_2022" /><ref name="meresearch_funding_2016">{{cite web |date=2016 |title=ME/CFS Research Funding – An Overview Of Activity By Major Institutional Funders Included on the Dimensions Database |url=https://www.meresearch.org.uk/wp-content/uploads/2016/09/mecfs-research-funding-report-2016-final.pdf |url-status=live |archive-url=https://web.archive.org/web/20240204230442/https://www.meresearch.org.uk/wp-content/uploads/2016/09/mecfs-research-funding-report-2016-final.pdf |archive-date=4 February 2024 |access-date=6 April 2023 |publisher=UK CFS/ME Research Collaborative and ÜberResearch |vauthors=Radford G, Chowdhury S}}</ref> In a 2015 report, the US National Academy of Sciences said that "remarkably little research funding" had been dedicated to causes, mechanisms, and treatment.<ref name="IOM2015" />{{Rp|9}} Lower funding levels have led to a smaller number and size of studies.<ref>{{cite journal |vauthors=Scheibenbogen C, Freitag H, Blanco J, Capelli E, Lacerda E, Authier J, Meeus M, Castro Marrero J, Nora-Krukle Z, Oltra E, Strand EB, Shikova E, Sekulic S, Murovska M |date=July 2017 |title=The European ME/CFS Biomarker Landscape Project: An Initiative of the European Network EUROMENE |journal=Journal of Translational Medicine |volume=15 |issue=1 |pages=162 |doi=10.1186/s12967-017-1263-z |pmc=5530475 |pmid=28747192 |doi-access=free}}</ref> In addition, drug companies have invested very little in the disease.<ref name="pmid33529750">{{cite journal |vauthors=Toogood PL, Clauw DJ, Phadke S, Hoffman D |date=March 2021 |title=Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Where Will the Drugs Come From? |journal=Pharmacological Research |volume=165 |issue= |pages=105465 |doi=10.1016/j.phrs.2021.105465 |pmid=33529750 |s2cid=231787959 |doi-access=free}}</ref> |
|||
=====Similar and related treatments===== |
|||
Many CFS patients face the stress of economic and legal problems. CFS sufferers may lose jobs, marriages, and the ability to work at all, causing severe financial loss and distress. A lawyer, social worker, or counsellor can be beneficial in helping the patient determine their best course, and may assist the patient with applying for work-related disability, social programs, and other aid. A study which included 45 CFS patients found that [[Psychodynamic_psychotherapy|psychodynamic counselling]] has comparable effectiveness to cognitive behavioral therapy (CBT) in the treatment of chronic fatigue.<ref>{{cite journal | author = Ridsdale L, Godfrey E, Chalder T, Seed P, King M, Wallace P, Wessely S | title = Chronic fatigue in general practice: is counselling as good as cognitive behaviour therapy? A UK randomised trial. | journal = Br J Gen Pract | volume = 51 | issue = 462 | pages = 19-24 | year = 2001 | id = PMID 11271868 | url = http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1313894&blobtype=pdf}}</ref> |
|||
The US National Institutes of Health (NIH) is the largest biomedical funder worldwide.<ref>{{Cite web |title=Grants & Funding |url=https://www.nih.gov/grants-funding |url-status=live |archive-url=https://web.archive.org/web/20231128044038/https://www.nih.gov/grants-funding |archive-date=28 November 2023 |access-date=22 November 2023 |website= |publisher=[[National Institutes of Health]] (NIH)}}</ref> Using rough estimates of disease burden, a study found NIH funding for ME/CFS was only 3% to 7% of the average disease per [[Disability-adjusted life year|healthy life year lost]] between 2015 and 2019.<ref name="Mirin_2021">{{cite journal |vauthors=Mirin AA |date=July 2021 |title=Gender Disparity in the Funding of Diseases by the U.S. National Institutes of Health |journal=Journal of Women's Health |volume=30 |issue=7 |pages=956–963 |doi=10.1089/jwh.2020.8682 |pmc=8290307 |pmid=33232627}}</ref> Worldwide, [[multiple sclerosis]], which affects fewer people and results in disability no worse than ME/CFS, received 20 times as much funding between 2007 and 2015.<ref name="meresearch_funding_2016" /><ref name="Tyson_2022" /> |
|||
====Graded Exercise Therapy (GE, GA or GET)==== |
|||
Several [[Physical medicine and rehabilitation|rehabilitation]] programs have been proposed which involve supervised or self-monitored graded exercise or activity. {{Fact|date=January 2008}} Such programs are designed to overcome [[deconditioning]], increase strength and cardiovascular health. {{Fact|date=January 2008}} The program should incorporate considerable education wherein the sufferer learns to start at an appropriate level of activity (based upon intensity and duration) which is incrementally increased, at a rate which does not substantially increase symptoms. {{Fact|date=January 2008}} |
|||
Multiple reasons have been proposed for the low funding levels. Diseases for which society "blames the victim" are frequently underfunded. This may explain why [[Chronic obstructive pulmonary disease|COPD]], a severe lung disease often caused by smoking, receives low funding per healthy life year lost.<ref>{{cite journal |vauthors=Mirin AA, Dimmock ME, Jason LA |date=2020 |title=Research Update: The Relation Between ME/CFS Disease Burden and Research Funding in the USA |journal=Work |volume=66 |issue=2 |pages=277–282 |doi=10.3233/WOR-203173 |pmid=32568148 |s2cid=219974997 |doi-access=free |veditors=Mooney A}}</ref> Similarly, for ME/CFS, the historical belief that it is caused by psychological factors may have contributed to lower funding. [[Gender disparities in health|Gender bias]] may also play a role; the NIH spends less on diseases that predominantly affect women in relation to disease burden. Less well-funded research areas may also struggle to compete with more mature areas of medicine for the same grants.<ref name="Mirin_2021" /> |
|||
The Gibson Report states GET is one of the most common treatments for CFS in the UK. Dr. Peter White found that in four studies 50-70% of patients improved with GET, and he stated that GET (combined with CBT) has only been shown to be efficacious in small trials. The Gibson Report mentions the 25% ME Group statement that, "only 5% of their members found GET helpful and 95% found it unhelpful". Many patients who submitted personal evidence to the Gibson inquiry said that they had similarly negative experiences which they attributed to their participation in GET.<ref name="gibson_report"/> The authors of the report expressed concern about GET treatment guidelines, arguing that there are be potential risks of GET for CFS patients, "Some of our evidence suggests that GET carries some risk and patients should be advised of this." The authors stated that the CFS guidlines lacked cautions about these possible risks and they said that patients should consider of checking for heart trouble before attempting GET. The authors said that the perception that GET may make severe sufferers feel worse "has lent fuel to their often serious antipathy to the doctors offering it." A [[New Zealand]] study suggests that GET may result in self-reported improvement by reducing the degree to which patients focus on their symptoms.<ref>{{cite journal | author = Moss-Morris R, Sharon C, Tobin R, Baldi JC | title = A randomized controlled graded exercise trial for chronic fatigue syndrome: outcomes and mechanisms of change. | journal = J Health Psychol | volume = 10 | issue = 2 | pages = 245-59 | year = 2005 | id = PMID 15723894}}</ref> |
|||
=== |
=== Directions === |
||
Many biomarkers for ME/CFS have been proposed. Studies on biomarkers have often been too small to draw robust conclusions. Natural killer cells have been identified as an area of interest for biomarker research as they show consistent abnormalities.<ref name="pmid37226227" /> Other proposed markers include [[Electrical impedance|electrical measurements]] of blood cells and [[Raman microscope|Raman microscopy]] of immune cells.<ref name="pmid38443223" /> Several small studies have investigated the genetics of ME/CFS, but none of their findings have been replicated.<ref name="Dibble McGrath Ponting 2020 p." /> A larger study, [[DecodeME]], is currently underway in the United Kingdom.<ref>{{Cite news |date=12 September 2022 |title=Experts Launch World's Largest Genetic Study of ME |work=BBC News |url=https://www.bbc.com/news/uk-scotland-edinburgh-east-fife-62876472 |access-date=20 January 2023 |archive-date=20 January 2023 |archive-url=https://web.archive.org/web/20230120140624/https://www.bbc.com/news/uk-scotland-edinburgh-east-fife-62876472 |url-status=live }}</ref> |
|||
====Antidepressants==== |
|||
[[Antidepressant]]s are often prescribed to CFS patients. Their purpose can be to treat secondary depression or mood swings, but low [[dosage]] tricyclic antidepressants are sometimes prescribed to improve sleep quality and reduce pain.<ref name="isbn: 0201407973">{{cite book | last = Bell | first = Bell David S | authorlink = http://www.davidsbell.com/DSBBooks.htm | title = The Doctor's Guide to Chronic Fatigue Syndrome | publisher = Da Capo Press | date = 1994 | pages = 163 | url = http://books.google.com/books?hl=en&lr=&id=MtKW0xFPs5sC&oi=fnd&pg=PR11&dq=%22Bell%22+%22The+Doctor%27s+Guide+to+Chronic+Fatigue+Syndrome:+...%22+&ots=b1A6hRFIZf&sig=BJMOZ-SdQb7Xk1jlMoAc5VHK_QY#PPP1,M1 | isbn = 0201407973}}</ref>. However, antidepressants often have [[side effect]]s, some of which can increase CFS symptoms, and baseline metabolism differs between patients. Finding antidepressants, if any, that help the individual patient, is therefore a matter of trial and error. |
|||
Various drug treatments for ME/CFS are being explored. Drugs under investigation often target the nervous system, the immune system, autoimmunity, or pain directly. More recently, there has been a growing interest in drugs targeting energy metabolism.<ref name="pmid33529750" /> In several clinical trials of ME/CFS, [[rintatolimod]] showed a small reduction in symptoms, but improvements were not sustained after discontinuation.<ref name="Richman2019">{{cite journal |vauthors=Richman S, Morris MC, Broderick G, Craddock TJ, Klimas NG, Fletcher MA |date=May 2019 |title=Pharmaceutical Interventions in Chronic Fatigue Syndrome: A Literature-Based Commentary |journal=Clinical Therapeutics |volume=41 |issue=5 |pages=798–805 |doi=10.1016/j.clinthera.2019.02.011 |pmc=6543846 |pmid=30871727}}</ref><ref name="pmid33529750" /> Rintatolimod has been approved in Argentina.<ref name="ADVINAT2019">{{cite book |title=Advances in Nucleic Acid Therapeutics |vauthors=Agrawal S, Kandimalla ER |date=February 2019 |publisher=[[Royal Society of Chemistry]] |isbn=978-1-78801-732-9 |veditors=Agrawal S, Gait MJ |pages=306–338 (310) |chapter=Chapter 14: Synthetic agonists of Toll-like receptors and therapeutic applications. |quote=14.2: Agonists of TLR3 |access-date=20 October 2021 |chapter-url=https://books.google.com/books?id=HsCrDwAAQBAJ&q=Rintatolimod+argentina&pg=PA310 |archive-url=https://web.archive.org/web/20220514015202/https://books.google.com/books?id=HsCrDwAAQBAJ&q=Rintatolimod+argentina&pg=PA310 |archive-date=14 May 2022 |url-status=live}}</ref> [[Rituximab]], a drug that depletes [[B cell]]s, was studied and found to be ineffective.<ref name="pmid38443223" /> Another option targeting autoimmunity is [[Immunoadsorption|immune adsorption]], which removes a large set of (auto)antibodies from the blood.<ref name="pmid33529750" /> |
|||
Overall, studies into the use of antidepressants in CFS have had mixed results. Some studies have shown a reduction in symptoms with antidepressant use, while others have shown no benefit.<ref>Thomas MA, Smith AP.An investigation of the long-term benefits of antidepressant medication in the recovery of patients with chronic fatigue syndrome. Hum Psychopharmacol. 2006 Dec;21(8):503-9</ref><ref>Schonfeldt-Lecuona C, Connemann BJ, Wolf RC, Braun M, Freudenmann RW.Bupropion augmentation in the treatment of chronic fatigue syndrome with coexistent major depression episode. Pharmacopsychiatry. 2006 Jul;39(4):152-4.</ref><ref>Goodnick PJ, Sandoval R, Brickman A, Klimas NG.Bupropion treatment of fluoxetine-resistant chronic fatigue syndrome. Biol Psychiatry. 1992 Nov 1;32(9):834-8.</ref><ref>Hickie IB, Wilson AJ, Wright JM, Bennett BK, Wakefield D, Lloyd AR. A randomized, double-blind placebo-controlled trial of moclobemide in patients with chronic fatigue syndrome. |
|||
J Clin Psychiatry. 2000 Sep;61(9):643-8.</ref> |
|||
=== Challenges === |
|||
====Autonomic nervous system stimulants==== |
|||
Symptoms and their severity can widely differ among people with ME/CFS. This poses a challenge for research into the cause and progression of the disease. Dividing people into subtypes may help manage this heterogeneity.<ref name="pmid38443223" /> The existence of multiple diagnostic criteria and variations in how scientists apply them complicate comparisons between studies.<ref name="IOM2015" />{{Rp|page=53}} Definitions also vary in which co-occurring conditions preclude a diagnosis of ME/CFS.<ref name="IOM2015" />{{Rp|page=52}} |
|||
Drugs such as [[atomoxetine]] (Strattera®), which stimulate the [[autonomic nervous system]], appear to have positive effects in some people with CFS symptoms. [[Amphetamine]]s and amphetamine analogs may help some patients. For example, [[methylphenidate]] (Ritalin®) has been found to be significantly better than placebo in relieving fatigue and concentration disturbances in a minority of CFS patients but more research is needed into the long term effects.<ref>{{cite journal | author = Blockmans D, Persoons P, Van Houdenhove B, Bobbaers H | title = Does methylphenidate reduce the symptoms of chronic fatigue syndrome? | journal = Am J Med | volume = 119 | issue = 2 | pages = 167.e23-30 | year = 2006 | id = PMID 16443425}}</ref> [[Modafinil]] (Provigil®), a medication designed to aid in maintaining wakefulness, has had some positive effect on individuals with CFS, but has not been properly studied. A small study suggested that long-term treatment with modafinil may not be beneficial for CFS patients.<ref>{{cite journal | author = Randall DC, Cafferty FH, Shneerson JM, Smith IE, Llewelyn MB, File SE | title = Chronic treatment with modafinil may not be beneficial in patients with chronic fatigue syndrome. | journal = J Psychopharmacol | volume = 19 | issue = 6 | pages = 647-60 | year = 2005 | id = PMID 16272188}}</ref> |
|||
== |
==See also== |
||
Various [[hormone]]s have been tried from time to time, including specifically [[steroids]] (such as [[cortisol]]) and [[thyroid]] hormones. Though conventional steroidal treatment may produce short-term pain relief, it has not been shown to be of any general benefit. Studies performed by Dr. Jacob Teitelbaum incorporating low-dose cortisol therapy have demonstrated positive results,<ref>{{cite journal | author = Teitelbaum J, Bird B, Weiss A, Gould L | title = Low-dose hydrocortisone for chronic fatigue syndrome. | journal = JAMA | volume = 281|issue = 20|pages = 1887-8; author reply 1888-9|year = 1999|id = PMID 10349885}}</ref> but other studies have shown little benefit from cortisol itself{{Fact|date=January 2008}}. |
|||
* [[List of people with ME/CFS]] |
|||
===Other medical treatments=== |
|||
* [[History of ME/CFS]] |
|||
====Allergy identification and treatment==== |
|||
In cases where CFS-like symptoms may be caused by allergies, enzyme deficiencies or [[food intolerance]], such as chronic [[sinusitis]] <ref name="pmid12447232">{{cite journal |author=Naranch K, Park YJ, Repka-Ramirez MS, Velarde A, Clauw D, Baraniuk JN |title=A tender sinus does not always mean rhinosinusitis |journal=Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery |volume=127 |issue=5 |pages=387-97 |year=2002 |pmid=12447232 |doi=10.1067/mhn.2002.129038}}</ref> |
|||
<ref name="pmid9809501">{{cite journal |author=Baraniuk JN, Clauw DJ, Gaumond E |title=Rhinitis symptoms in chronic fatigue syndrome |journal=Ann. Allergy Asthma Immunol. |volume=81 |issue=4 |pages=359-65 |year=1998 |pmid=9809501 |doi=}}</ref> |
|||
, [[coeliac disease]]<ref name="pmid11703165">{{cite journal |author=Logan AC, Wong C |title=Chronic fatigue syndrome: oxidative stress and dietary modifications |journal=Alternative medicine review : a journal of clinical therapeutic |volume=6 |issue=5 |pages=450-9 |year=2001 |pmid=11703165 |doi=}}</ref>, or [[irritable bowel syndrome]]<ref name="pmid16738080">{{cite journal |author=Moss-Morris R, Spence M |title=To "lump" or to "split" the functional somatic syndromes: can infectious and emotional risk factors differentiate between the onset of chronic fatigue syndrome and irritable bowel syndrome? |journal=Psychosomatic medicine |volume=68 |issue=3 |pages=463-9 |year=2006 |pmid=16738080 |doi=10.1097/01.psy.0000221384.07521.05}}</ref><ref name="pmid10647761">{{cite journal |author=Aaron LA, Burke MM, Buchwald D |title=Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder |journal=Arch. Intern. Med. |volume=160 |issue=2 |pages=221-7 |year=2000 |pmid=10647761 |doi=}}</ref>, allergy testing, treatments, or elimination diets may prove beneficial. |
|||
<ref name="pmid11703165">{{cite journal |author=Logan AC, Wong C |title=Chronic fatigue syndrome: oxidative stress and dietary modifications |journal=Alternative medicine review : a journal of clinical therapeutic |volume=6 |issue=5 |pages=450-9 |year=2001 |pmid=11703165 |doi=}}</ref><ref name="isbn0-9695662-0-4">{{cite book |author=Nightingale Research Foundation; Goldstein, Jay E.; Byron M. Hyde |title=The Clinical and scientific basis of myalgic encephalomyelitis/chronic fatigue syndrome |publisher=Nightingale Research Foundation |location=Ogdensburg, N.Y |year=1992 |pages=521-538, chapter57, The Role of Food Intolerance in Chronic Fatigue Syndrome |isbn=0-9695662-0-4 |oclc= |doi=}}</ref> |
|||
== References == |
|||
===Complementary and alternative medicine=== |
|||
{{reflist}} |
|||
====Essential fatty acid treatments==== |
|||
Behan and Horrobin in a 1990 study of individuals diagnosed with postviral fatigue syndrome stated patients given essential fatty acids reported much greater symptom improvement verses patients given placebo.<ref name="pmid2270749">{{cite journal |author=Behan PO, Behan WM, Horrobin D |title=Effect of high doses of essential fatty acids on the postviral fatigue syndrome |journal=Acta Neurol. Scand. |volume=82 |issue=3 |pages=209-16 |year=1990 |pmid=2270749 |doi=}}</ref> A fatty acid supplementation study conducted in 1999 using patients diagnosed by the Oxford criteria (Warren et al.) declared there were no significant differences between treatment and placebo groups.<ref name="pmid10071170">{{cite journal |author=Warren G, McKendrick M, Peet M |title=The role of essential fatty acids in chronic fatigue syndrome. A case-controlled study of red-cell membrane essential fatty acids (EFA) and a placebo-controlled treatment study with high dose of EFA |journal=Acta Neurol. Scand. |volume=99 |issue=2 |pages=112-6 |year=1999 |pmid=10071170 |doi=}}</ref> A review of CFS treatments by Reid et al. in 2000, concluded the Behan and Warren studies showed mixed results, and classified dietary supplements as "unknown effectiveness".<ref name="Reid et al.">{{cite journal |author=Reid S, Chadler T, Cleare A, Hotopf M, Wessely S. |title=Extracts from “Clinical Evidence”: Chronic fatigue syndrome |journal=British Medical Journal |volume=320 |issue=7230 |pages=292–296 |year=2000 |url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1117488 |pmid= |doi=}}</ref> |
|||
== External links == |
|||
====Magnesium==== |
|||
<!-- External links must follow [[WP:EL]] |
|||
One small randomised controlled trial compared intramuscular injections with magnesium sulphate to placebo. The study stated greater improvement was found in the treatment group compared to the control group, as measured by the Nottingham health profile.<ref name="pmid1672392">{{cite journal |author=Cox IM, Campbell MJ, Dowson D |title=Red blood cell magnesium and chronic fatigue syndrome |journal=Lancet |volume=337 |issue=8744 |pages=757-60 |year=1991 |pmid=1672392 |doi=}}</ref> The previously noted review by Reid et al. determined subsequent studies have failed to find a deficiency of magnesium in people with chronic fatigue syndrome, and classified magnesium treatments in dietary supplements having "unknown effectiveness".<ref name="Reid et al."/> |
|||
Do not include disputed links unless there is a consensus to do so --> |
|||
{{Sister project links|collapsible=collapsed|voy=no|species=no|c=Category:Chronic fatigue syndrome|d=Q209733}} |
|||
{{Medical resources |
|||
====Complementary and alternative medicine usage==== |
|||
| ICD11 = {{ICD11|8E49}} |
|||
Two studies reported increased utilization of alternative treatments by people with CFS vs. without. In one study designed to assess use of alternative medicines and perceived benefits with 63 paired CFS and non-CFS co-twins, 91% of twins with CFS and 71% without CFS used at last one alternative treatment in their life, and a large proportion of all twins considered them helpful. Future research should ascertain the usefulness of alternative practices in the management of CFS.<ref name="pmid17459162">{{cite journal |author=Jones JF, Maloney EM, Boneva RS, Jones AB, Reeves WC |title=Complementary and alternative medical therapy utilization by people with chronic fatiguing illnesses in the United States |journal=BMC Complement Altern Med |volume=7 |issue= |pages=12 |year=2007 |pmid=17459162 |doi=10.1186/1472-6882-7-12}}</ref><ref name="pmid10882883">{{cite journal |author=Afari N, Eisenberg DM, Herrell R, ''et al'' |title=Use of alternative treatments by chronic fatigue syndrome discordant twins |journal=Integr Med |volume=2 |issue=2 |pages=97–103 |year=2000 |pmid=10882883 |doi=}}</ref> |
|||
| ICD10 = {{ICD10|G93.3}} |
|||
| ICD10CM = {{ICD10CM|G93.32}} |
|||
| ICD9 = {{ICD9|323.9}} {{ICD9|780.71}} |
|||
| ICDO = |
|||
| OMIM = |
|||
| MeshID = D015673 |
|||
| DiseasesDB = 1645 |
|||
| SNOMED CT = 52702003 |
|||
| Curlie = |
|||
| MedlinePlus = 001244 |
|||
| eMedicineSubj = med |
|||
| eMedicineTopic = 3392 |
|||
| eMedicine_mult = {{eMedicine2|ped|2795}} |
|||
| PatientUK = |
|||
| NCI = |
|||
| GeneReviewsNBK = |
|||
| GeneReviewsName = |
|||
| NORD = |
|||
| GARDNum = |
|||
| GARDName = |
|||
| RP = 74341 |
|||
| AO = |
|||
| WO = |
|||
| OrthoInfo = |
|||
| Orphanet = |
|||
| Scholia = Q209733 |
|||
| OB = |
|||
}} |
|||
{{Chronic fatigue syndrome}} |
|||
==Prognosis== |
|||
{{CNS diseases of the nervous system}} |
|||
===Recovery=== |
|||
{{Portal bar | Medicine}} |
|||
A systematic review of 14 studies of the outcome of untreated people with CFS found that "the median full recovery rate was 5% (range 0–31%) and the median proportion of patients who improved during follow-up was 39.5% (range 8–63%). Return to work at follow-up ranged from 8 to 30% in the three studies that considered this outcome." .... "In five studies, a worsening of symptoms during the period of follow-up was reported in between 5 and 20% of patients."<ref name=Cairns2005>{{cite journal |author=Cairns R, Hotopf M |title=A systematic review describing the prognosis of chronic fatigue syndrome |journal=Occupational medicine (Oxford, England) |volume=55 |issue=1 |pages=20-31 |year=2005 |pmid=15699087 |doi=10.1093/occmed/kqi013}}</ref> It is not known whether any patients truly "recover" entirely from the illness, or achieve remission from a relapsing, remitting illness{{Fact|date=January 2008}}. Few untreated patients report a total "cure". |
|||
{{Authority control}} |
|||
===Deaths=== |
|||
CFS is unlikely to increase the risk of an early death. A systematic review of 14 studies of the outcome of CFS reported 8 deaths, but none were considered directly attributable to CFS.<ref name=Cairns2005/> To date there have been two studies directly addressing life expectancy in CFS. In a preliminary 2006 study of CFS self-help group members, it was reported that CFS patients were likely to die at a younger than average age for cancer, heart failure, and suicide.<ref>{{cite journal |author=Jason LA, Corradi K, Gress S, Williams S, Torres-Harding S |title=Causes of death among patients with chronic fatigue syndrome |journal=Health care for women international |volume=27 |issue=7 |pages=615-26 |year=2006 |pmid=16844674 |doi=10.1080/07399330600803766}}</ref> However, a much larger study of 641 CDC criteria diagnosed patients with CFS, who were followed up for a mean of 9 years, showed no excess risk of dying from any cause.<ref>{{cite journal |author=Smith WR, Noonan C, Buchwald D |title=Mortality in a cohort of chronically fatigued patients |journal=Psychological medicine |volume=36 |issue=9 |pages=1301-6 |year=2006 |pmid=16893495 |doi=10.1017/S0033291706007975}}</ref> |
|||
People diagnosed with CFS ''may'' die, as in the case in the [[UK]] of [[Sophia Mirza]], where the coroner recorded a verdict of "[[acute renal failure|Acute anuric renal failure]] due to dehydration arising as a result of CFS." According to Sophia's mother, Sophia became intolerant to water and managed only 4 fluid ounces per day<ref>[http://www.25megroup.org/Campaigning/Awareness%202006/Sophia's%20story/sophia's%20story%2006.htm Sophia's story]</ref>. The pathologist said, "ME describes inflammation of the spinal cord and muscles. My work supports the inflammation theory...The changes of [[dorsal root]] ganglionitis seen in 75% of Sophia's [[spinal cord]] were very similar to that seen during active infection by herpes viruses." This was seen as a form of recognition by the ME community.<ref>{{cite news | title=Fatigue syndrome ruling welcomed |url=http://news.bbc.co.uk/1/hi/uk/5112050.stm |format= |work= |publisher= |id= |pages= |page= |date=[[2006-06-23]] |accessdate = 2007-09-03 |language=English}}</ref> Previous cases have listed CFS as the cause of death in the US and Australia<ref>[http://www.meactionuk.org.uk/Inquest_Implications.htm Inquest Implications: Marshall E, Williams, M, June 2006]</ref> |
|||
==Epidemiology== |
|||
Due to problems with the definition of CFS, estimates of its [[prevalence]] vary widely. Studies in the United States have previously found between 75 and 420 cases of CFS for every 100,000 adults. The CDC states that more than 1 million Americans have CFS and approximately 80% of the cases are undiagnosed.<ref name="CDCBasic">{{cite web | title = Chronic Fatigue Syndrome Basic Facts | publisher = Centers for Disease Control and Prevention | date = May 9, 2006 | url = http://www.cdc.gov/cfs/cfsbasicfacts.htm | format = htm | accessdate = 2008-02-07}}</ref> All ethnic and racial groups appear susceptible to the illness, and lower income groups are slightly more likely to develop CFS.<ref name="CDCRisk"/> More women than men get CFS — between 60 and 85% of cases are women; however, there is some indication that the prevalence among men is under reported. The illness is reported to occur more frequently in people between the ages of 40 and 59. Blood relatives of people who have CFS appear to be more predisposed.<ref name="CDCRisk">{{cite web | title = Chronic Fatigue Syndrome Who's at risk? | publisher = Centers for Disease Control and Prevention | date = March 10, 2006 | url = http://www.cdc.gov/cfs/cfscausesHCP.htm | format = htm | accessdate = 2008-02-07}}</ref><ref>{{cite journal | author = Walsh CM, Zainal NZ, Middleton SJ, Paykel ES | title = A family history study of chronic fatigue syndrome. | journal = Psychiatr Genet | volume = 11 | issue = 3 | pages = 123-8 | year = 2001 | id = PMID 11702053}}</ref> However, CFS does not appear directly contagious; caretakers, partners and others in close contact with persons with CFS for years do not develop CFS any more frequently (excluding relatives, as earlier). |
|||
Epidemiological research on children and adolescents has received minimal focus according to a 2006 research review. Among minors, prevalence appears to be lower than for adults and various studies have found a range of 50-80% of the cases occur in girls. The authors hypothesize the differences in estimates of ME/CFS among pediatric studies may result because of the lack of a reliable pediatric case definition.<ref name="DOI : 10.1300/J092v13n02_01"/> |
|||
CFS generally occurs in [[Endemic (epidemiology)|endemic]] cases. In addition, over 50 instances have been documented, such as the [[Royal Free Hospital]] incident, where [[epidemic]] clusters were reported.{{weasel word}}<ref name="Ramsay86"/><ref name="isbn0-9695662-0-4"/> In these instances, significant numbers of people came down with illnesses described{{weasel-inline}} as ME or CFS simultaneously, confined to a local area or even a single building. An infectious origin for these clusters was considered highly likely due tor: |
|||
* transference by inoculation to monkeys which developed symptomology and on post-mortem demonstrated neurological and vascular damage (Fellow and Miles, 1955). |
|||
* human post-mortems or scans demonstrating abnormalities consistent with chronic infection (Wallis 1957, Schwartz et al 1994) |
|||
* serologic evidence of Iceland Disease blocking spread of polio type I spreading northwards (Sigurdsson et al, 1958). |
|||
* the pattern of acute onset with pharyngitis, mild fever, muscular pain, neck stiffness, cervical lymphadenopathy, gastroenteric symptoms, diffuse CNS involvement and photosensitivity were consistent with viral infection with an observed incubation period of 5-7 days. The biphasic clinical picture echoes pathogenesis through the pharynx, spreading through the reticuloendothelial barrier, then the CNS, resulting in morphological changes in mature lymphocytes and antibody creation. (Acheson, Ramsay, RIchardson, Crowley, Dillon et al) |
|||
* A predeliction for residential communities and most outbreaks occurring in summer (Acheson) |
|||
* The isolation of the non-polio enterovirus ECHO-9 in patients (Lyle, Annals of Internal Medicine 1959; 51: 248-269) |
|||
* psychiatric disease was a widely regarded exclusion for M.E. diagnosis (e.g. Acheson) and positive criteria for hysteria were absent (Gosling, Mayne, 1970). |
|||
* At the 1978 RSM Symposium, new evidence was presented of increased anti-complementary activity and the ability of lymphocytes to proliferate and survive in vitro for up to 19 weeks. (Compston 1978). |
|||
Since most current definitions of CFS exclude such findings and signs, it is disputed whether they refer to a differential diagnosis (but see below). |
|||
According to the CDC, CFS itself is not contagious.<ref name="CDCDemographics">{{cite web | title = Chronic Fatigue Syndrome Demographics | publisher = Centers for Disease Control and Prevention | date = May 11, 2005 | url = http://www.cdc.gov/ncidod/diseases/cfs/about/demographics.htm| format = htm | accessdate = 2008-02-07}}</ref> |
|||
===Disease associations=== |
|||
Some diseases show a considerable overlap with CFS. According to an article in ''American Family Physician'' in 2002, [[Multiple Sclerosis]], [[Thyroid|Thyroid disorders]], [[anemia]], and [[diabetes]] are but a few of the diseases that must be ruled out if the patient presents with appropriate symptoms.<ref name="CDC1994"/><ref name="CFSeval">{{cite journal | author = Craig, T and Kakumanu S| title = Chronic fatigue syndrome: evaluation and treatment | journal = Am Fam Physician. | volume = 65 |issue = 6 |pages = 1083-90 |year = Mar 2002 |url = http://www.aafp.org/afp/20020315/1083.html | id = PMID 11925084}}</ref> |
|||
People with [[fibromyalgia]] (FM, or Fibromyalgia Syndrome, FMS) have muscle pain and sleep disturbances. Fatigue and muscle pain occurs frequently in the initial phase of various hereditary muscle disorders and in several autoimmune, endocrine and metabolic syndromes; and are frequently labelled as CFS or fibromyalgia in the absence of obvious biochemical/metabolic abnormalities and neurological symptoms.<ref>{{cite journal | author = van de Glind G, de Vries M, Rodenburg R, Hol F, Smeitink J, Morava E | title = Resting muscle pain as the first clinical symptom in children carrying the MTTK A8344G mutation. | journal = Eur J Paediatr Neurol | year = 2007 | id = PMID 17293137}}</ref> Those with [[multiple chemical sensitivities]] (MCS) are sensitive to chemicals and have sleep disturbances. Many veterans with [[Gulf War syndrome]] (GWS) have symptoms almost identical to CFS.<ref>{{cite journal | author = Vojdani A, Thrasher J | title = Cellular and humoral immune abnormalities in Gulf War veterans. | journal = Environ Health Perspect | volume = 112|issue = 8|pages = 840-6|year = 2004|id = PMID 15175170}}</ref> One study found several parallels when relating the symptoms of [[Post-polio syndrome]] with CFS, and postulates a possible common pathophysiology for the illnesses.<ref name="polio">{{cite journal | author = Bruno RL, Creange SJ, Frick NM | title = Parallels between post-polio fatigue and chronic fatigue syndrome: a common pathophysiology? | journal = Am J Med. | volume = 105 |issue = 3A |pages = 66S-73S |year = 1998 |id = PMID 9790485}}</ref> |
|||
Although post-Lyme syndrome and CFS share many features/symptoms, a study found that patients of the former experience more cognitive impairment and the patients of the latter experience more flu-like symptoms.<ref>{{cite journal | author = Gaudino EA, Coyle PK, Krupp LB | title = Post-Lyme syndrome and chronic fatigue syndrome. Neuropsychiatric similarities and differences. | journal = Arch Neurol | volume = 54 | issue = 11 | pages = 1372-6 | year = 1997 | id = PMID 9362985}}</ref> |
|||
One review (2006) found that there was a lack of literature to establish the [[discriminant validity]] of undifferentiated [[somatoform disorder]] from CFS. The author stated that there is a need for proponents of chronic fatigue syndrome to distinguish it from undifferentiated somatoform disorder. The author also mentioned that the experience of fatigue as exclusively physical and not mental is captured by the definition of somatoform disorder but not CFS.<ref>{{cite journal | author = van Staden WC | title = Conceptual issues in undifferentiated somatoform disorder and chronic fatigue syndrome. | journal = Curr Opin Psychiatry | volume = 19 | issue = 6 | pages = 613-8 | year = 2006 | id = PMID 17012941}}</ref> Hysterical diagnoses are not merely diagnoses of exclusion but require criteria to be met on the positive grounds of both primary and secondary gain. <ref>Jenkins R, Mowbray J, ed. Post-viral Fatigue Syndrome. 1991 John Wiley & Sons Ltd</ref> Primary Depression can be excluded in the [[differential diagnosis]] due to the absence of [[anhedonia]] and [[la belle indifference]], the variability (lability) of mood, and the presence of sensory phenomena and somatic signs such as ataxia, myclonus and most importantly, exercise intolerance with paresis, malaise and general deterioration<ref name="carr">. Feeling depressed is also a commonplace reaction to the losses caused by chronic illness<ref>{{cite journal | author = Frank RG, Chaney JM, Clay DL, Shutty MS, Beck NC, Kay DR, Elliott TR, Grambling S | title = Dysphoria: a major symptom factor in persons with disability or chronic illness. | journal = Psychiatry Res | volume = 43 | issue = 3 | pages = 231-41 | year = 1992 | id = PMID 1438622}}</ref>, which can in some cases become a comorbid situational depression. |
|||
===Co-morbidity=== |
|||
Many CFS patients will also have, or appear to have, other medical problems or related diagnoses. Co-morbid [[fibromyalgia]] is common, although there are differences in pain complaints.<ref>{{cite journal | author = Bradley LA, McKendree-Smith NL, Alarcon GS | title = Pain complaints in patients with fibromyalgia versus chronic fatigue syndrome. | journal = Curr Rev Pain | volume = 4 | issue = 2 | pages = 148-57 | year = 2000 | id = PMID 10998728}}</ref> Fibromyalgia will occur in a large percentage of CFS patients between onset and the second year, and some researchers suggest that fibromyalgia and CFS are related.<ref>{{cite journal | author = Friedberg F, Jason LA | title = Chronic fatigue syndrome and fibromyalgia: clinical assessment and treatment. | journal = J Clin Psychol. | volume = 57 | issue = 4 | pages = 433-55 | year = 2001 | id = PMID 11255201 }}</ref> Similarly, [[multiple chemical sensitivity]] (MCS) is reported by many CFS patients, and it is speculated that these similar conditions may be related by some underlying mechanism, such as elevated nitric oxide/peroxynitrite.<ref>{{cite journal | author = Pall ML, Satterlee JD | title = Elevated nitric oxide/peroxynitrite mechanism for the common etiology of multiple chemical sensitivity, chronic fatigue syndrome, and posttraumatic stress disorder. | journal = Ann N Y Acad Sci | volume = 933 | pages = 323-9 | year = 2001 | id = PMID 12000033}}</ref> As previously mentioned, many CFS sufferers also experience symptoms of [[irritable bowel syndrome]], [[temporomandibular joint]] pain, [[headache]] including [[migraine]]s, and other forms of [[myalgia]]. [[Clinical depression]] and [[anxiety]] are also commonly co-morbid. Compared with the non-fatigued population, male CFS patients are more likely to experience [[Prostatitis#Category III: CP.2FCPPS.2C pelvic myoneuropathy|chronic pelvic pain syndrome (CP/CPPS)]], and female CFS patients are also more likely to experience [[chronic pelvic pain]].<ref>{{cite journal | author = Aaron LA, Herrell R, Ashton S, Belcourt M, Schmaling K, Goldberg J, Buchwald D | title = Comorbid clinical conditions in chronic fatigue: a co-twin control study. | journal = J Gen Intern Med | volume = 16 | issue = 1 | pages = 24-31 | year = 2001 | id = PMID 11251747 | url = http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=11251747}}</ref> CFS is significantly more common in women with [[endometriosis]] compared with women in the general USA population.<ref>{{cite journal | author = Sinaii N, Cleary SD, Ballweg ML, Nieman LK, Stratton P | title = High rates of autoimmune and endocrine disorders, fibromyalgia, chronic fatigue syndrome and atopic diseases among women with endometriosis: a survey analysis. | journal = Hum Reprod | volume = 17 | issue = 10 | pages = 2715-24 | year = 2002 | id = PMID 12351553}}</ref> |
|||
===Social issues=== |
|||
Many patients find that a chronic fatigue syndrome diagnosis carries a considerable stigma, and has frequently been viewed as malingering, hypochondriac, phobic, "wanting attention" or "yuppie flu". As there is no objective test for the condition at this time, it has been argued that it is easy to invent or feign CFS-like symptoms for financial, social, or emotional benefits.<ref name="isbn: 1572301732">{{cite book | last = Rogers | first = Richard | title = Clinical Assessment of Malingering and Deception, Second Edition | publisher = Guilford Press | date = 1997 | location = New York, London | pages = pg 40 of 525 | url = http://books.google.com/books?id=YZ6uK4Cjd_MC&printsec=frontcover&dq=somatoform+deception+chronic+fatigue+syndrome | page = 40 | isbn = 1572301732}}</ref><ref name="isbn: 0773529942">{{cite book | last = Malleson | first = Andrew | title = Whiplash and Other Useful Illnesses | publisher = McGill-Queen's Press | date = 2005 | location = Quebec | pages = pg 59 of 544 | url = http://books.google.com/books?id=naDghccZhEwC&vq=Whiplash+and+Other+Useful+Illnesses | isbn = 0773529942}}</ref> CFS sufferers argue in turn that the perceived "benefits" are hardly as generous as some may believe, and that CFS patients would greatly prefer to be healthy and independent. A study found that CFS patients endure a heavy psychosocial burden.<ref name="PMID_12097786">{{cite journal | author = Van Houdenhove B, Neerinckx E, Onghena P, Vingerhoets A, Lysens R, Vertommen H | title = Daily hassles reported by chronic fatigue syndrome and fibromyalgia patients in tertiary care: a controlled quantitative and qualitative study. | journal = Psychother Psychosom | volume = 71 | issue = 4 | pages = 207-13 | year = 2002 | id = PMID 12097786}}</ref> 2,338 respondents of a survey by a UK patient organization highlights that those with the worst symptoms often receive the least support from health and social services.<ref name="Neglected">[http://www.afme.org.uk/res/img/resources/Severely%20Neglected.pdf Action for M.E. in the UK, Severely Neglected: Membership Survey] London: Action for M.E.; 2001</ref> A study found that CFS patients receive worse social support than disease-free cancer patients or healthy controls, which may perpetuate fatigue severity and functional impairment in CFS.<ref name="nosupport"/> A survey by the Thymes Trust found that children with CFS often state that they struggle for recognition of their needs and/or they feel bullied by medical and educational professionals.<ref name="colby_special">{{cite journal | author = Colby J | title = Special problems of children with myalgic encephalomyelitis/chronic fatigue syndrome and the enteroviral link. | journal = J Clin Pathol | volume = 60 | issue = 2 | pages = 125-8 | year = 2007 | id = 16935964}}</ref> The ambiguity of the status of CFS as a medical condition may cause higher perceived stigma.<ref>{{cite journal | author = Looper KJ, Kirmayer LJ | title = Perceived stigma in functional somatic syndromes and comparable medical conditions. | journal = J Psychosom Res | volume = 57 | issue = 4 | pages = 373-8 | year = 2004 | id = PMID 15518673}}</ref> A study suggests that while there are no gender differences in CFS symptoms, men and women have different perceptions of their illness and are treated differently by the medical profession.<ref>{{cite journal | author = Clarke JN | title = Chronic fatigue syndrome: gender differences in the search for legitimacy. | journal = Aust N Z J Ment Health Nurs | volume = 8 | issue = 4 | pages = 123-33 | year = 1999 | id = PMID 10855087}}</ref> Anxiety and depression often result from the emotional, social and financial crises caused by CFS. While few studies have been made, it is believed that CFS patients are at a high risk of suicide.<ref>{{cite journal | author = Jason L, Corradi K, Gress S, Williams S, Torres-Harding S | title = Causes of death among patients with chronic fatigue syndrome. | journal = Health Care Women Int | volume = 27 | issue = 7 | pages = 615-26 | year = 2006 | id = PMID 16844674}}</ref> |
|||
A lack of information and awareness has led to many patients to feel stigmatized.<ref>Green J, Romei J, Natelson BH (1999) Stigma and Chronic Fatigue Syndrome Journal of Chronic Fatigue Syndrome, Vol. 5, No. 2, 1999</ref> CFS patients may not receive total medical and social acceptance and they state that some people trivialise the illness.<ref name="nosupport">{{cite journal | author = Prins JB, Bos E, Huibers MJ, Servaes P, van der Werf SP, van der Meer JW, Bleijenberg G | title = Social support and the persistence of complaints in chronic fatigue syndrome. | journal = Psychother Psychosom | volume = 73 | issue = 3 | pages = 174-82 | year = 2004 | id = PMID 15031590}}</ref><ref name="hooper_pathol_06">{{cite journal | author = Hooper M | title = Myalgic Encephalomyelitis (ME): a review with emphasis on key findings in biomedical research. | journal = J Clin Pathol | year = 2006 | doi = 10.1136/jcp.2006.042408}}[http://jcp.bmj.com/cgi/content/abstract/jcp.2006.042408v2]</ref> When the illness is coupled with unaccommodating family, friends, colleagues, often due to [[social stigma|stigma]], and social repercussions such as financial needs, housing problems, the struggle to obtain disability benefits or insurance, discrimination and misconception within the care sector, it can put demands on the sufferer exceeding their safe capabilities.{{Fact|date=January 2008}} Many sufferers say that they need to do things for themselves during the time in which they feel better as there is no-one to delegate these tasks to.<ref name="nosupport"/> |
|||
==History== |
|||
===The concept=== |
|||
In 1681, the diagnosis of [[muscular rheumatism]] was introduced by [[Thomas Sydenham]]<ref>Sydenham T, "The Works of Thomas Sydenham, M.D.", (translated from the Latin edition of Greenhill WA by Latham RG), Vol. 1, Londen, Sydenham Society, 1847</ref>, which according to Hyde<ref name="isbn0-9695662-0-4"/> is likely to have included cases of ME. |
|||
Sir Richard Manningham in 1750 published his description of febricula or little fever.<ref>Manningham, R. (1750) "The symptoms , nature, causes and cure of the februlica or little fever; commonly called the nervous or hysteric fever; the fever on the spirits; vapours, hypo or spleen," 2nd edition, J. Robertson, London p.52-3.</ref>, an antiquated diagnosis which has also been attributed to some cases of ME by Shepherd. |
|||
In the 19th century, neurologist [[George Miller Beard]] popularised the concept of [[neurasthenia]], in which symptoms included; fatigue, anxiety, headache, impotence, neuralgia and depression.<ref>[[George Miller Beard|Beard, G.]] (1869, Apr. 28). "Neurasthenia, or nervous exhaustion". ''The Boston Medical and Surgical Journal''. (pp. 217-221)</ref> This concept remained popular until well into the 20th century, although by then this diagnosis was viewed as primarily behavioural rather than physical, and to exclude postviral syndromes. It has largely been abandoned as a medical diagnosis. |
|||
In 1938 Gilliam made a detailed description of an illness that resembled [[poliomyelitis]], interviewing patients and reviewing records of one of several clusters which had occurred in Los Angeles, United States in 1934.<ref name="Gilliam38">Gilliam AG (1938) Epidemiological Study on an Epidemic, Diagnosed as Poliomyelitis, Occurring among the Personnel of Los Angeles County General Hospital during the Summer of 1934, United States Treasury Department Public Health Service Public Health Bulletin, No. 240, pp. 1-90. Washington, DC, Government Printing Office.</ref> His common "atypical [[poliomyelitis]]" features of rapid muscle weakness, vasomotor instability, clonic twitches and cramps, ataxia, severe pain usually aggravated by exercise, neck and back stiffness, menstrual disturbance and dominant sensory involvement et cetera, constituted a twenty-point definition which was later viewed as the first recognisable description of ME.<ref name="isbn0-9695662-0-4"/> In the 1950s, the British public eye was caught by several [[outbreak]]s of a polio'-resembling illness<ref name="Ramsay-RF">{{cite book | author=A. Melvin Ramsay | title=Postviral Fatigue Syndrome. The saga of Royal Free disease | location=Londen | year=1986 | ISBN=0-906923-96-4}}</ref> and by now several tens of epidemics had occurred worldwide, including those in Iceland, Norway and New Zealand. Afterwards, it was established that the disorder was primarily found among the general population and the [[epidemic]] form was the exception{{Fact|date=August 2007}}. [[Autopsy]] findings, both on [[monkey]]s<ref>R.A.A. Pellew, J.A.R. Miles, "Further investigations on a disease resembling poliomyelitis seen in Adelaide," Medical Journal of Australia, 42. 480-482</ref> and on the rare human [[casualty (person)|casualties]]<ref>A.L. Wallis, "An investigation into an unusual illness seen in Epidemic and Sporadic Form in a General Practice in Cumberland in 1955 and subsequent years", M.D. Thesis, Edinburgh University, 1957</ref>, led to the conclusion that the disorder was caused by [[inflammation]] of the [[brain]] and the [[spinal cord]], particularly the [[afferent]] nerve roots<ref>Richardson J (2002) Myalgic Encephalomyelitis: Guidelines for Doctors. Journal: J of Chronic Fatigue Syndrome, Vol. 10(1)</ref>, and in 1956 it was named accordingly as ''myalgic encephalomyelitis'', reflecting a presumed [[Neuroimmunology|neuroimmune]] etiology.<ref name=Acheson1956/> |
|||
Although non-epidemic cases were recognised, the disorder was in 1970 dismissed as [[mass hysteria]] by two psychiatrists.<ref>{{cite journal |author=McEvedy CP, Beard AW |title=Concept of benign myalgic encephalomyelitis |journal=British medical journal |volume=1 |issue=5687 |pages=11–5 |year=1970 |pmid=5411596 |url=}} {{PMC|1700895}}</ref> They were strongly criticized (Gosling; Hopkins; Galpine; Scott; Mayne: 1970 BMJ),(Compston, 1978 BMJ) for not adequately investigating the patients they described.<ref name="hooper_pathol_06"/> In a 1978 symposium held at the [[Royal Society of Medicine]] (RSM) where there was clear agreement that ME is a distinct disease entity, and new pathology findings were discussed.<ref>{{cite journal |author= Compston ND|title=Epidemic myalgic encephalomyelitis |journal=British medical journal |volume=1 |issue=6125 |pages=1436–7 |year=1978 |pmid=647324 |doi=}}</ref> |
|||
The illness gained national attention in the United States when the popular magazine Hippocrates ran a cover story of an [[epidemic]] in the mid-1980s at [[Lake Tahoe]], [[Nevada]].<ref name = "Osler'sWeb">{{cite book | last = Johnson | first = Hilary | title = Osler's Web: Inside the Labyrinth of the Chronic Fatigue Syndrome Epidemic | publisher = Penguin Books | date = 1996 | location = New York | pages = 24 | isbn = 0595348742 }}</ref> The designation Chronic Epstein-Barr Virus was in use in the U.S.<ref name="pmid2578268"/><ref name="pmid2578266"/>, but the magazine used the term "Raggedy Ann Syndrome" to note the fatigue and loss of muscle power patients felt.<ref name="Hippocrates">{{Citation | author = Day W | year=1987 | title =Raggedy Ann Syndrome | journal =Hippocrates | volume = | pages = July/August, cover story }}</ref> |
|||
After investigating the Lake Tahoe cluster, [[Centers for Disease Control & Prevention]] researchers attached a different kind of name to the phenomenon: chronic fatigue syndrome, involving some of the symptoms rather than disease taxonomy. They published the first working case definition for CFS in 1988.<ref name=Holmes1988/> Research increased considerably, and more so after the criteria were relaxed in 1994.<ref>{{cite journal |author=Fukuda K, Straus S, Hickie I, Sharpe M, Dobbins J, Komaroff A |title=The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group |journal=Ann. Intern. Med. |volume=121 |issue=12 |pages=953-9 |year=1994 |pmid=7978722}}</ref> |
|||
In the United Kingdom, the [[Chief Medical Officer]] [[Kenneth Calman]] requested a report from the medical Royal Colleges in 1996. This led to the publication of a joint report in which the term "chronic fatigue syndrome" was found to be most representative.<ref>{{cite book |author=Royal Colleges of Physicians, Psychiatrists and General Practitioners |title=Chronic fatigue syndrome; Report of a joint working group of the Royal Colleges of Physicians, Psychiatrists and General Practitioners |year= 1996|publisher=Royal College of Physicians of London |location=London, UK |isbn=1-86016-046-8 }}</ref> This was followed in 2002 by a further report by the new CMO, [[Liam Donaldson]].<ref name=CMOrept2002/> |
|||
The U.S. [[Centers for Disease Control & Prevention]] (CDC) have now recognized CFS as a serious illness and launched a campaign in June 2006 to raise public and medical awareness about it.<ref name="CDC-awareness">[[June 7]] [[2006]] . [http://www.cdc.gov/cfs/PSAs/Gerberding-launch.pdf Dr. Gerberding's address at CFS awareness campaign launch] Department of Health and Human Services. Centers for Disease Control and Prevention.</ref> |
|||
===WHO classification=== |
|||
Since its introduction into the eighth edition of the [[ICD|International Classification of Diseases]] in 1969, CFS/ME has been classified as a disease of the central nervous system. In the [[ICD-10]], ME is the only disorder listed in the tabular classification under G93.3, [[post-viral fatigue syndrome]] (PVFS). In 1993 the term "chronic fatigue syndrome" (CFS) was added to the alphabetic list of the classification with the same designation. |
|||
===Controversy=== |
|||
Two contrasting viewpoints among ME/CFS experts have become apparent. In a letter to the Lancet, psychiatrists David and [[Simon Wessely|Wessely]] contested the WHO classification, arguing that CFS was a form of [[neurasthenia]] to be classified as a psychiatric condition.<ref>{{cite journal |author=David A, Wessely S |title=Chronic fatigue, ME, and ICD-10 |journal=Lancet |volume=342 |issue=8881 |pages=1247–8 |year=1993 |pmid=7901572 |doi=}}</ref> Dutch researchers tested a model where behavioral, cognitive, and affective factors played a role in perpetuating fatigue, and concluded that this was the correct model for CFS.<ref>Vercoulen JHMM, Swanink CMA, Galama JMD, Fennis JFM, Jongen PHJ, Hommes OR, Van der Meer JWM, Bleijenberg G. (1998), "The persistence of fatigue in chronic fatigue syndrome and multiple sclerosis: Development of a model. Journal of Psychosomatic Research", 45, 507 – 517</ref> This result could, however, not be replicated in a population-based study, where fatigue in psychiatric disorders, but not in CFS, proved to be a match.<ref>Song, S, Jason, LA (2005), "A population based study of CFS experienced in differing patient groups. An effort to replicate Vercoulen et al.'s model of CFS", Journal of Mental Health, 14, 3, 277-289</ref> |
|||
===Notable sufferers=== |
|||
Some notable persons who are believed to have suffered from CFS are: |
|||
*[[Olaf Bodden]], former German [[soccer]] player<ref>{{cite web | language = german | url = http://www.probono.tv/sendungen/sendung.php?sendung=30&subnav=reportage| title = Documentary "Der müde Stürmer" }}</ref> |
|||
*[[Clare Francis]], yachtswoman and novelist<ref>Biography at: http://www.clarefrancis.com/biography/ </ref> |
|||
*[[Susan Harris]], television writer and producer, who incorporated her experiences into the fifth season of ''[[The Golden Girls]]''<ref>{{cite web | url = http://www.imdb.com/name/nm0365358/bio | title = Biography for Susan Harris | source = imdb.com | accessdate = 2007-10-16 | language = english }}</ref> |
|||
*[[Laura Hillenbrand]], author of the book ''[[Seabiscuit: An American Legend]]'', the basis for the film ''[[Seabiscuit (film)|Seabiscuit]]''<ref>{{cite web | url = http://www.nndb.com/people/253/000082007/ | title = Laura Hillenbrand | accessdate = 2007-10-16 | source = Notable Names Database | language = english }}</ref> |
|||
*[[Blair Hornstine]], a [[New Jersey]] student<ref>{{cite web | url = http://www.foxnews.com/story/0,2933,86469,00.html | title = Demographics, Nerves, Valedictorian, Vouchers | last = Jacobs | first = Joanne |date=2003-05-09 | accessdate = 2007-10-16 | language = english | format = html | source = Foxnews.com }}</ref> |
|||
*[[Keith Jarrett]], jazz pianist<ref>{{cite web | format = cfm | language = english | url = http://www.immunesupport.com/library/showarticle.cfm?ID=2811 | title = Jazz Great Keith Jarrett Discusses Living with Chronic Fatigue Syndrome |date=2000-09-14 | accessdate = 2007-10-16 }}</ref> |
|||
*[[Peter Marshall (squash player)|Peter Marshall]], former [[United Kingdom|British]] squash player<ref>{{cite web | url = http://www.ayme.org.uk/article.php?sid=13&id=18 | title = Shattered- The Interview | last = Collingridge | first = Emily | language = english |date=2003-08-01 | accessdate = 2007-10-16 | format = php }}; Marshall was diagnosed with myalgic encephalomyelitis.</ref> |
|||
*[[Andrew Oldcorn]], golfer<ref>{{cite web | url = http://www.europeantour.com/publish.sps?pageid=127&pagegid=%7BAB0336D2%2DD3C9%2D469B%2DBCB6%2DBFD443B52A34%7D&playerId=143 | title = Player biography: Andrew Oldcorn | language = english | accessdate = 2007-10-16 |date=2007}}; Oldcorn was diagnosed with myalgic encephalomyelitis.</ref> |
|||
*[[Alastair Lynch]], [[Australian rules football]]er<ref>{{cite web | url = http://www.footballlegends.org/alastair_lynch.htm | format = html | language = english | accessdate = 2007-10-17 | title = Eighties Tasmanian Footbal Legends: Alastair Lynch |date=2007}}</ref> |
|||
*[[Ali Smith]], author<ref>{{cite web | url = http://books.guardian.co.uk/bookerprize2005/story/0,16347,1546471,00.html | title = Life stories: Ali Smith | accessdate = 2007-10-16 | language = english | format = html |date=2005-05-22 | source = Guardian Unlimited | last = France | first = Louise }}</ref> |
|||
===Cultural references=== |
|||
* A 1989 episode of ''[[The Golden Girls]]'' ("Sick and Tired") dealt with [[Dorothy Zbornak|Dorothy]] developing the illness and trying to cope with doctors who told her it was mental. [[Bea Arthur]] (who played Dorothy) wanted to raise social awareness of the issue. |
|||
* In the first series of [[Alan Partridge]], during a meal with the head of the BBC Alan suggests a program he has thought of involving the illness Knowing ME Knowing You. "You've got to keep the energy up." |
|||
* The 2000 film [[I Remember Me]] chronicles a sufferer of CFS. |
|||
* In the premiere episode of ''[[Buffy the Vampire Slayer (TV series)|Buffy the Vampire Slayer]]'' ("[[Welcome to the Hellmouth]]"), popular girl [[Cordelia Chase|Cordelia]] remarks, "My mom doesn't even get out of bed anymore. And the doctor says it's Epstein-Barr. I'm like, pleeease! It's chronic hepatitis, or at least chronic fatigue syndrome. I mean, nobody cool has Epstein-Barr anymore." |
|||
==References== |
|||
{{reflist|3}} |
|||
==External links== |
|||
<!-- BEFORE inserting new links here you should first post it to the talk page, otherwise your edit is likely to be reverted--> |
|||
{{DMOZ|Health/Conditions_and_Diseases/Neurological_Disorders/Chronic_Fatigue_Syndrome/}} |
|||
{{Cleanup|date=September 2007}} |
|||
{{DEFAULTSORT:Myalgic encephalomyelitis/chronic fatigue syndrome}} |
|||
[[Category:Myalgic encephalomyelitis/chronic fatigue syndrome| ]] |
|||
[[Category:Immune system disorders]] |
[[Category:Immune system disorders]] |
||
[[Category:Neurological disorders]] |
[[Category:Neurological disorders]] |
||
[[Category: |
[[Category:Syndromes of unknown causes]] |
||
[[Category:Syndromes]] |
|||
[[ca:Síndrome de fatiga crònica]] |
|||
[[cs:Chronický únavový syndrom]] |
|||
[[de:Chronisches Erschöpfungssyndrom]] |
|||
[[es:Síndrome de fatiga crónica]] |
|||
[[fr:Syndrome de fatigue chronique]] |
|||
[[it:Sindrome da fatica cronica]] |
|||
[[he:תסמונת העייפות הכרונית]] |
|||
[[lb:Chronescht Middegkeetssyndrom]] |
|||
[[lt:Lėtinis nuovargis]] |
|||
[[nl:Chronischevermoeidheidssyndroom]] |
|||
[[ja:慢性疲労症候群]] |
|||
[[no:Kronisk utmattelsessyndrom]] |
|||
[[sk:Chronický únavový syndróm]] |
|||
[[sr:Хронични синдром замора]] |
|||
[[fi:Krooninen väsymysoireyhtymä]] |
|||
[[sv:Kroniskt trötthetssyndrom]] |
|||
[[vi:Hội chứng mệt mỏi kinh niên]] |
|||
Latest revision as of 15:11, 2 January 2025
| Myalgic encephalomyelitis/chronic fatigue syndrome | |
|---|---|
| Other names | Post-viral fatigue syndrome (PVFS), systemic exertion intolerance disease (SEID)[1]: 20 |
| The four primary symptoms of ME/CFS according to the National Institute for Health and Care Excellence | |
| Specialty | Rheumatology, rehabilitation medicine, endocrinology, infectious disease, neurology, immunology, general practice, paediatrics, other specialists in ME/CFS[2]: 58 |
| Symptoms | Worsening of symptoms with activity, long-term fatigue, sleep problems, others[3] |
| Usual onset | Peaks at 10–19 and 30–39 years old[4] |
| Duration | Long-term[5] |
| Causes | Unknown[6] |
| Risk factors | Being female, family history, viral infections[6] |
| Diagnostic method | Based on symptoms[7] |
| Treatment | Symptomatic[8] |
| Prevalence | About 0.17% to 0.89% (pre-COVID-19 pandemic)[9] |
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a disabling chronic illness. People with ME/CFS experience profound fatigue that does not go away with rest, as well as sleep issues and problems with memory or concentration. The hallmark symptom is post-exertional malaise, a worsening of the illness which can start immediately or hours to days after even minor physical or mental activity. This "crash" can last from hours or days to several months. Further common symptoms include dizziness or faintness when upright and pain.[3][10]
The cause of the disease is unknown.[11] ME/CFS often starts after an infection, such as mononucleosis.[12] It can run in families, but no genes that contribute to ME/CFS have been confirmed.[13] ME/CFS is associated with changes in the nervous and immune systems, as well as in energy production.[14] Diagnosis is based on symptoms and a differential diagnosis because no diagnostic test is available.[7][15][16][17]
The illness can improve or worsen over time, but full recovery is uncommon.[12] No therapies or medications are approved to treat the condition, and management is aimed at relieving symptoms.[2]: 29 Pacing of activities can help avoid worsening symptoms, and counselling may help in coping with the illness.[8] Before the COVID-19 pandemic, ME/CFS affected two to nine out of every 1,000 people, depending on the definition.[9] However, many people fit ME/CFS diagnostic criteria after contracting long COVID.[18] ME/CFS occurs more often in women than in men. It is more common in middle age, but can occur at all ages, including childhood.[19]
ME/CFS has a large social and economic impact, and the disease can be socially isolating.[20] About a quarter of those affected are unable to leave their bed or home.[10]: 3 People with ME/CFS often face stigma in healthcare settings, and care is complicated by controversies around the cause and treatments of the illness.[21] Doctors may be unfamiliar with ME/CFS, as it is often not fully covered in medical school.[18] Historically, research funding for ME/CFS has been far below that of diseases with comparable impact.[22]
Classification and terminology
[edit]ME/CFS has been classified as a neurological disease by the World Health Organization (WHO) since 1969, initially under the name benign myalgic encephalomyelitis.[23]: 564 The classification of ME/CFS as a neurological disease is based on symptoms which indicate a central role of the nervous system.[24] Alternatively, on the basis of abnormalities in immune cells, ME/CFS is sometimes labelled a neuroimmune condition.[25] The disease can further be regarded as a post-acute infection syndrome (PAIS) or an infection-associated chronic illness.[11][26] PAISes such as long COVID and post-treatment Lyme disease syndrome share many symptoms with ME/CFS and are suspected to have a similar cause.[26]
Many names have been proposed for the illness. The most commonly used are chronic fatigue syndrome, myalgic encephalomyelitis, and the umbrella term myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Reaching consensus on a name has been challenging because the cause and pathology remain unknown.[1]: 29–30 In the WHO's most recent classification, the ICD-11, chronic fatigue syndrome and myalgic encephalomyelitis are named under post-viral fatigue syndrome.[27] The term post-infectious fatigue syndrome was initially proposed as a subset of "chronic fatigue syndrome" with a documented triggering infection, but might also be used as a synonym of ME/CFS or as a broader set of fatigue conditions after infection.[26]
Many individuals with ME/CFS object to the term chronic fatigue syndrome. They consider the term simplistic and trivialising, which in turn prevents the illness from being taken seriously.[1]: 234 [28] At the same time, there are also issues with the use of myalgic encephalomyelitis (myalgia means muscle pain and encephalomyelitis means brain and spinal cord inflammation), as there is only limited evidence of brain inflammation implied by the name.[29]: 3 The umbrella term ME/CFS would retain the better-known phrase CFS without trivialising the disease, but some people object to this name too, as they see CFS and ME as distinct illnesses.[28]
A 2015 report from the US Institute of Medicine recommended the illness be renamed systemic exertion intolerance disease (SEID) and suggested new diagnostic criteria.[1] While the new name was not widely adopted, the diagnostic criteria were taken over by the CDC. Like CFS, the name SEID only focuses on a single symptom, and opinion from those affected was generally negative.[30]
Signs and symptoms
[edit]ME/CFS causes debilitating fatigue, sleep problems, and post-exertional malaise (PEM, overall symptoms getting worse after mild activity). In addition, cognitive issues, orthostatic intolerance (dizziness or nausea when upright) or other physical symptoms may be present (see also § Diagnostic criteria). Symptoms significantly reduce the ability to function and typically last for three to six months before a diagnosis can be confirmed.[10]: 13 [2]: 11 ME/CFS usually starts after an infection. Onset can be sudden or more gradual over weeks to months.[12]
Core symptoms
[edit]People with ME/CFS experience persistent debilitating fatigue. It is made worse by normal physical, mental, emotional, and social activity, and is not a result of ongoing overexertion.[3][2]: 12 Rest provides limited relief from fatigue. Particularly in the initial period of illness, this fatigue is described as "flu-like". Individuals may feel "physically drained" and unable to start or finish activities. They may also feel restless while fatigued, describing their experience as "wired but tired". When starting an activity, muscle strength may drop rapidly, which can lead to difficulty with coordination, clumsiness or sudden weakness. Mental fatigue may also make cognitive efforts difficult.[2]: 12, 57, 95 [31][32] The fatigue experienced in ME/CFS is of a longer duration and greater severity than in other conditions characterized by fatigue.[10]: 5–6
The hallmark feature of ME/CFS is a worsening of symptoms after exertion, known as post-exertional malaise or post-exertional symptom exacerbation.[6] PEM involves increased fatigue and is disabling. It can also include flu-like symptoms, pain, cognitive difficulties, gastrointestinal issues, nausea, and sleep problems.[10]: 6

All types of activities that require energy, whether physical, cognitive, social, or emotional, can trigger PEM.[33]: 49 Examples include attending a school event, food shopping, or even taking a shower.[3] For some, being in a stimulating environment can be sufficient to trigger PEM.[33]: 49 PEM usually starts 12 to 48 hours after the activity,[34] but can also follow immediately after. PEM can last hours, days, weeks, or months.[10]: 6 Extended periods of PEM, commonly referred to as "crashes" or "flare-ups" by people with the illness, can lead to a prolonged relapse.[33]: 50
Unrefreshing sleep is a further core symptom. People wake up exhausted and stiff rather than restored after a night's sleep. This can be caused by a pattern of sleeping during the day and being awake at night, shallow sleep, or broken sleep. However, even a full night's sleep is typically non-restorative. Some individuals experience insomnia, hypersomnia (excessive sleepiness), or vivid nightmares.[33]: 50
Cognitive dysfunction in ME/CFS can be as disabling as physical symptoms, leading to difficulties at work or school, as well as in social interactions.[10]: 7 People with ME/CFS sometimes describe it as "brain fog",[3] and report a slowdown in information processing.[10]: 7 Individuals may have difficulty speaking, struggling to find words and names. They may have trouble concentrating or multitasking, or may have difficulties with short-term memory.[2] Tests often show problems with short-term visual memory, reaction time and reading speed. There may also be problems with attention and verbal memory.[35]
People with ME/CFS often experience orthostatic intolerance, symptoms that start or worsen with standing or sitting. Symptoms, which include nausea, lightheadedness, and cognitive impairment, often improve again after lying down.[12] Weakness and vision changes may also be triggered by the upright posture.[3] Some have postural orthostatic tachycardia syndrome (POTS), an excessive increase in heart rate after standing up, which can result in fainting.[10]: 7 Additionally, individuals may experience orthostatic hypotension, a drop in blood pressure after standing.[29]: 17
Other common symptoms
[edit]Pain and hyperalgesia (an abnormally increased sensitivity to pain) are common in ME/CFS. The pain is not accompanied by swelling or redness.[29]: 16 The pain can be present in muscles (myalgia) and joints. Individuals with ME/CFS may have chronic pain behind the eyes and in the neck, as well as neuropathic pain (related to disorders of the nervous system).[10]: 8 Headaches and migraines that were not present before the illness can occur as well. However, chronic daily headaches may indicate an alternative diagnosis.[29]: 16
Additional common symptoms include irritable bowel syndrome or other problems with digestion, chills and night sweats, shortness of breath or an irregular heartbeat. Some experience sore lymph nodes and a sore throat. People may also develop allergies or become sensitive to foods, lights, noise, smells or chemicals.[3]
Illness severity
[edit]ME/CFS often leads to serious disability, but the degree varies considerably.[11] ME/CFS is generally classified into four categories of illness severity:[2]: 8 [29]: 10
- People with mild ME/CFS can usually still work and care for themselves, but they will need their free time to recover from these activities rather than engage in social and leisure activities.
- Moderate severity impedes activities of daily living (self-care activities, such as making a meal). People are usually unable to work and require frequent rest.
- Those with severe ME/CFS are homebound and can do only limited activities of daily living, for instance brushing their teeth. They may be wheelchair-dependent and spend the majority of their time in bed.
- With very severe ME/CFS, people are mostly bed-bound and cannot care for themselves.
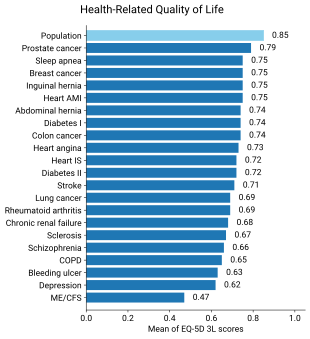
Roughly a quarter of those living with ME/CFS fall into the mild category, and half fall into the moderate or moderate-to-severe categories.[6] The final quarter falls into the severe or very severe category.[10]: 3 Severity may change over time. Symptoms might get worse, improve, or the illness may go into remission for a period of time.[11] People who feel better for a period of time may overextend their activities, triggering PEM and a worsening of symptoms.[34]
Those with severe and very severe ME/CFS experience more extreme and diverse symptoms. They may face severe weakness and greatly limited ability to move. They can lose the ability to speak, swallow, or communicate completely due to cognitive issues. They can further experience severe pain and hypersensitivities to touch, light, sound, and smells.[2]: 50 Minor day-to-day activities can be sufficient to trigger PEM.[12]
Individuals with ME/CFS have decreased quality of life when evaluated by the SF-36 questionnaire, especially in the domains of physical and social functioning, general health, and vitality. However, their emotional functioning and mental health are not much lower than those of healthy individuals.[17] Functional impairment in ME/CFS can be greater than multiple sclerosis, heart disease, or lung cancer.[12] Fewer than half of people with ME/CFS are employed, and roughly one in five have a full-time job.[9]
Causes
[edit]The cause of ME/CFS is not yet known.[12] Between 60% and 80% of cases start after an infection, usually a viral infection.[29]: 5 [6] A genetic factor is believed to contribute, but there is no single gene known to be responsible for increased risk. Instead, many gene variants probably have a small individual effect, but their combined effect can be strong.[13] Other factors may include problems with the nervous and immune systems, as well as energy metabolism.[12] ME/CFS is a biological disease, not a psychological condition,[17][11] and is not due to deconditioning.[17][12]
Besides viruses, other reported triggers include stress, traumatic events, and environmental exposures such as to mould.[10]: 21 Bacterial infections such as Q-fever are other potential triggers.[29]: 5 ME/CFS may further occur after physical trauma, such as an accident or surgery.[11] Pregnancy has been reported in around 3% to 10% of cases as a trigger.[36] ME/CFS can also begin with multiple minor triggering events, followed by a final trigger that leads to a clear onset of symptoms.[6]
Risk factors
[edit]ME/CFS can affect people of all ages, ethnicities, and income levels, but it is more common in women than men.[9] People with a history of frequent infections are more likely to develop it.[14] Those with family members who have ME/CFS are also at higher risk, suggesting a genetic factor.[13] In the United States, white Americans are diagnosed more frequently than other groups,[19] but the illness is probably at least as prevalent among African Americans and Hispanics.[37] It used to be thought that ME/CFS was more common among those with higher incomes. Instead, people in minority groups or lower income groups may have increased risks due to poorer nutrition, lower healthcare access, and increased work stress.[9]
Viral infections
[edit]Viral infections have long been suspected to cause ME/CFS, based on the observation that ME/CFS sometimes occurs in outbreaks and is possibly connected to autoimmune diseases.[38] How viral infections cause ME/CFS is unclear; it could be via viral persistence or via a "hit and run" mechanism, in which infections dysregulate the immune system or cause autoimmunity.[39]
Different types of viral infection have been implicated in ME/CFS, including airway infections, bronchitis, gastroenteritis, or an acute "flu-like illness".[10]: 226 Between 15% and 50% of people with long COVID also meet the diagnostic criteria for ME/CFS.[10]: 228 Of people who get infectious mononucleosis, which is caused by the Epstein–Barr virus (EBV), around 8% to 15% develop ME/CFS, depending on criteria.[10]: 226 Other viral infections that can trigger ME/CFS are the H1N1 influenza virus, varicella zoster (the virus that causes chickenpox and shingles), and SARS-CoV-1.[40]
Reactivation of latent viruses, in particular EBV and human herpesvirus 6, has also been hypothesised to drive symptoms. EBV is present in about 90% of people, usually in a latent state.[41][42]: 13 The levels of antibodies to EBV are commonly higher in people with ME/CFS, indicating possible viral reactivation.[43]
Pathophysiology
[edit]ME/CFS is associated with changes in several areas, including the nervous and immune systems, as well as disturbances in energy metabolism.[11][14] Neurological differences include autonomic nervous system dysfunction and a change in brain structure and metabolism.[44] Observed changes in the immune system include decreased natural killer cell function and, in some cases, autoimmunity.[14]
Neurological
[edit]A range of structural, biochemical, and functional abnormalities are found in brain imaging studies of people with ME/CFS.[25][44] Common findings are changes in the brainstem and the use of additional brain areas for cognitive tasks. Other consistent findings, based on a smaller number of studies, are low metabolism in some areas, reduced serotonin transporters, and problems with neurovascular coupling.[24]
Neuroinflammation has been proposed as an underlying mechanism of ME/CFS that could explain a large set of symptoms. Several studies suggest neuroinflammation in the cortical and limbic regions of the brain. Individuals with ME/CFS, for instance, have higher brain lactate and choline levels, which are signs of neuroinflammation. More direct evidence from two small positron emission tomography studies of microglia, a type of immune cell in the brain, were contradictory, however.[45][46]
ME/CFS affects sleep. Individuals experience decreased sleep efficiency, take longer to fall asleep, and take longer to achieve REM sleep, a phase of sleep characterised by rapid eye movement. Changes to non-REM sleep have also been found, together suggesting a role of the autonomic nervous system.[47] Individuals often have a blunted heart rate response to exercise, but a higher heart rate during a tilt table test when the body is rotated from lying flat to an upright position. This again suggests dysfunction in the autonomic nervous system.[48]
Immunological
[edit]People with ME/CFS often have immune system abnormalities. A consistent finding in studies is a decreased function of natural killer cells, a type of immune cell that targets virus-infected and tumour cells.[49] They are also more likely to have active viral infections, correlating with cognitive issues and fatigue. T cells show less metabolic activity. This may reflect they have reached an exhausted state and cannot respond effectively against pathogens.[14]
Autoimmunity has been proposed to be a factor in ME/CFS. There is a subset of people with ME/CFS with increased levels of autoantibodies, possibly as a result of viral mimicry.[50] Some may have higher levels of autoantibodies to muscarinic acetylcholine receptors as well as to β2 adrenergic receptors.[50][14] Problems with these receptors can lead to impaired blood flow.[51]
Energy
[edit]
Objective signs of PEM have been found with the 2-day cardiopulmonary exercise test.[52] People with ME/CFS have lower performance compared to healthy controls on the first test. On the second test, healthy people's scores stay roughly the same or increase slightly, while those with ME/CFS have a clinically significant decrease in work rate at the anaerobic threshold. Potential causes include mitochondrial dysfunction, and issues with the transport and use of oxygen.[53] Some of the usual recovery processes following exercise may be lacking, providing an alternative explanation for PEM.[14]
Studies have observed mitochondrial abnormalities in cellular energy production, but differences between studies make it hard to draw clear conclusions.[54] ATP, the primary energy carrier in cells, is likely more frequently produced from lipids and amino acids than from carbohydrates.[14]
Other
[edit]Some people with ME/CFS have abnormalities in their hypothalamic–pituitary–adrenal axis hormones. This can include lower cortisol levels, less change in cortisol levels throughout the day, and a weaker reaction to stress and stimuli.[55] Other proposed abnormalities are reduced blood flow to the brain under orthostatic stress (as found in a tilt table test), small-fibre neuropathy, and an increase in the amount of gut microbes entering the blood.[29]: 9 The diversity of gut microbes is reduced compared to healthy controls.[14] Women with ME/CFS are more likely to experience endometriosis, early menopause, and other menstrual irregularities compared to women without the condition.[11]
Diagnosis
[edit]Diagnosis of ME/CFS is based on symptoms[7] and involves taking a medical history and a mental and physical examination.[56] No specific lab tests are approved for diagnosis; while physical abnormalities can be found, no single finding is considered sufficient for diagnosis.[12][7] Blood and urine tests are used to rule out other conditions that could be responsible for the symptoms.[56] People with ME/CFS often face significant delays in obtaining a diagnosis, and diagnoses may be missed altogether.[2]: 66 Specialists in ME/CFS may be asked to confirm the diagnosis, as primary care physicians often lack a good understanding of the illness.[2]: 68
Diagnostic criteria
[edit]| Symptom M: Mandatory O: Optional |
CDC/Fukuda
|
CCC
|
ICC
|
IOM
|
NICE
|
|---|---|---|---|---|---|
| Fatigue | M | M | M | M | M |
| Functional impairment | M | M | M | M | M |
| PEM | O | M | M | M | M |
| Sleep problems | O | M | O | M | M |
| Cognitive issues | O | O | O | O | M |
| Pain or headaches | O | M | O | ||
| Orthostatic intolerance | O | O | O | ||
| Flu or cold symptoms | O | O | O | ||
| Nausea | O | O | |||
| Cardiovascular problems | O | O | |||
| Hypersensitivities | O | O | |||
| Susceptibility to infection | O |
Multiple research and clinical criteria exist to diagnose ME/CFS. These include the NICE guidelines, Institute of Medicine (IOM) criteria, the International Consensus Criteria (ICC), the Canadian Consensus Criteria (CCC), and CDC criteria. The criteria sets were all developed based on expert consensus and differ in the required symptoms and which conditions preclude a diagnosis of ME/CFS.[29]: 14 The definitions differ in their conceptualisation of the cause and mechanisms of ME/CFS.[57]
As there is no single known biomarker for ME/CFS, it is not possible to determine which set of criteria is the most accurate. A trade-off must be made between overdiagnosis and missing more diagnoses. The broad Fukuda criteria have a higher risk of overdiagnosis, whereas the strict ICC criteria have a higher risk of missing people. The IOM and NICE criteria fall in the middle.[33]: 47–48
The 1994 CDC criteria, sometimes called the Fukuda criteria, require six months of persistent or relapsing fatigue for diagnosis, as well as the persistent presence of four out of eight other symptoms.[29]: 35 While used frequently, the Fukuda criteria have limitations: PEM and cognitive issues are not mandatory. The large variety of optional symptoms can lead to diagnosis of individuals who differ significantly from each other.[10]: 15
The Canadian Consensus Criteria, another commonly used criteria set, was developed in 2003.[29]: 14 In addition to PEM, fatigue and sleep problems, pain and neurological or cognitive issues are required for diagnosis. Furthermore, three categories of symptoms are defined (orthostatic, thermal instability, and immunological). At least one symptom in two of these categories needs to be present.[10]: 15 [29]: 34 People diagnosed under the CCC have more severe symptoms compared to those diagnosed under the Fukuda criteria. The 2011 International Consensus Criteria defines ME using symptom clusters and has no minimum duration of symptoms. Similarly to the CCC criteria, ICC is stricter than the Fukuda criteria and selects more severely ill people.[29]: 14
The 2015 IOM criteria share significant similarities with the CCC but were developed to be easy to use for clinicians. Diagnosis requires fatigue, PEM, non-restorative sleep, and either cognitive issues (such as memory impairment) or orthostatic intolerance. Additionally, fatigue must persist for at least six months, substantially impair activities in all areas of life, and have a clearly defined onset.[10]: 16–17 Symptoms must be present at least half of the time, and be of moderate severity or worse; previous criteria just required symptoms to be present.[29]: 14 In 2021, NICE revised its criteria based on the IOM criteria. The updated criteria require fatigue, PEM, non-restorative sleep, and cognitive difficulties persisting for at least three months.[10]: 16–17
Separate diagnostic criteria have been developed for children and young people. A diagnosis for children often requires a shorter symptom duration. For example, the CCC definition only requires three months of persistent symptoms in children compared to six months for adults.[10]: 17–18 NICE requires only four weeks of symptoms to suspect ME/CFS in children, compared to six weeks in adults.[29]: 15 Exclusionary diagnoses also differ; for instance, children and teenagers may have anxiety related to school attendance, which could explain symptoms.[10]: 17–18
Clinical assessment
[edit]
Screening can be done using the DePaul Symptom Questionnaire, which assesses the frequency and severity of ME/CFS symptoms.[29]: 24 Individuals may struggle to answer questions related to PEM, if they are unfamiliar with the symptom. To find patterns in symptoms, they may be asked to keep a diary.[12]
A physical exam may appear completely normal, particularly if the individual has rested substantially before a doctor's visit.[12] There may be tenderness in the lymph nodes and abdomen or signs of hypermobility.[29]: 17 Answers to questions may show a temporary difficulty with finding words or other cognitive problems.[6] Cognitive tests and a two-day cardiopulmonary exercise test (CPET) can be helpful to document aspects of the illness, but they may be risky as they can cause severe PEM. They may be warranted to support a disability claim.[12] Orthostatic intolerance can be measured with a tilt table test. If that is unavailable, it can also be assessed with the simpler NASA 10-minute lean test, which tests the response to prolonged standing.[6]
Standard laboratory findings are usually normal. Standard tests when suspecting ME/CFS include an HIV test, and blood tests to determine full blood count, red blood cell sedimentation rate (ESR), C-reactive protein, blood glucose and thyroid-stimulating hormone. Tests for antinuclear antibodies may come back positive, but below the levels that suggest the individual may have lupus. C-reactive protein levels are often at the high end of normal. Serum ferritin levels may be useful to test, as borderline anaemia can make some ME/CFS symptoms worse.[29]: 18
Differential diagnosis
[edit]Some medical conditions have symptoms similar to ME/CFS. Diagnosis often involves clinical evaluation, testing, and specialist referrals to identify the correct condition. During the time other possible diagnoses are explored, advice can be given on symptom management to help prevent the condition from getting worse.[2]: 66–67 Before a diagnosis of ME/CFS is confirmed, a waiting period is used to exclude acute medical conditions or symptoms which may resolve within that time frame.[12][58]
Possible differential diagnoses span a large set of specialties and depend on the medical history.[12] Examples are infectious diseases, such as Epstein–Barr virus and Lyme disease, and neuroendocrine disorders, including diabetes and hypothyroidism. Blood disorders, such as anaemia, and some cancers may also present similar symptoms.[12][33]: 57 Various rheumatological and autoimmune diseases, such as Sjögren's syndrome, lupus, and arthritis, may have overlapping symptoms with ME/CFS. Furthermore, it may be necessary to evaluate psychiatric diseases, such as depression or substance use disorder, as well as neurological disorders, such as narcolepsy, multiple sclerosis, and craniocervical instability.[12][33]: 57 Finally, sleep disorders, coeliac disease, and side effects of medications may also explain symptoms.[12]
Joint and muscle pain without swelling or inflammation is a common feature of ME/CFS, but is more closely associated with fibromyalgia. Modern definitions of fibromyalgia not only include widespread pain but also fatigue, sleep disturbances, and cognitive issues. This makes it difficult to distinguish ME/CFS from fibromyalgia[59]: 13, 26 and the two are often co-diagnosed.[29]: 28
Another common condition that often co-occurs with ME/CFS is hypermobile Ehlers–Danlos syndrome (EDS).[33]: 57 Unlike ME/CFS, EDS is present from birth. People with ME/CFS are more often hypermobile compared to the general population.[29]: 28–29 Sleep apnoea may also co-occur with ME/CFS.[29]: 16 However, many diagnostic criteria require ruling out sleep disorders before confirming a diagnosis of ME/CFS.[10]: 7
Like with other chronic illnesses, depression and anxiety co-occur frequently with ME/CFS. Depression may be differentially diagnosed by the presence of feelings of worthlessness, the inability to feel pleasure, loss of interest, and/or guilt, and the absence of ME/CFS bodily symptoms such as autonomic dysfunction, pain, migraines, and PEM.[29]: 27 People with chronic fatigue, which is not due to ME/CFS or other chronic illnesses, may be diagnosed with idiopathic (unexplained) chronic fatigue.[29]: 32
Management
[edit]There is no approved drug treatment or cure for ME/CFS, although some symptoms can be treated or managed. Care for ME/CFS involves multidisciplinary healthcare professionals. Usually, the primary care clinician plays an important role in coordinating health care, social care and educational support for those still in school. This coordinator can help provide access to community resources such as occupational therapy and district nursing. Management may start with treating the most disabling symptom first, and tackle symptoms one by one in further health care visits.[29]: 46
Pacing, or managing one's activities to stay within energy limits, can reduce episodes of PEM. Addressing sleep problems with good sleep hygiene, or medication if required, may be beneficial. Chronic pain is common in ME/CFS, and the CDC recommends consulting with a pain management specialist if over-the-counter painkillers are insufficient. For cognitive impairment, adaptations like organisers and calendars may be helpful.[8]
Co-occurring conditions that may interact with and worsen ME/CFS symptoms are common, and treating these may help manage ME/CFS.[12] Commonly diagnosed ones include fibromyalgia, irritable bowel syndrome, migraines and mast cell activation syndrome.[29]: 19 The debilitating nature of ME/CFS can cause depression, anxiety, or other psychological problems, which can be treated.[8] People with ME/CFS may be unusually sensitive to medications, especially ones that affect the central nervous system.[60]
Pacing and energy management
[edit]
Pacing, or activity management, involves balancing periods of rest with periods of activity.[34] The goal of pacing is to stabilize the illness and avoid triggering PEM.[61] This involves staying within an individual's available energy envelope to reduce the PEM "payback" caused by overexertion.[62] The technique was developed for ME/CFS in the 1980s.[63]
Pacing can involve breaking up large tasks into smaller ones and taking extra breaks, or creating easier ways to do activities. For example, this might include sitting down while doing the laundry. The decision to stop an activity (and rest or change an activity) is determined by self-awareness of a worsening of symptoms. Use of a heart rate monitor may help some individuals with pacing.[8]
Research on pacing and energy envelope theory typically shows positive effects.[62][64] However, these studies have often had a low number of participants and have rarely included methods to check if study participants implemented pacing well.[64] Pacing is difficult to apply for people with very severe ME/CFS, as the activities that trigger PEM in this group, such as eating, cannot be avoided completely.[61]
Those with a stable illness who understand how to "listen to their body" may be able to carefully and flexibly increase their activity levels.[34] The goal of an exercise programme would be to increase stamina, while not interfering with everyday tasks or making the illness more severe.[29]: 56 In many chronic illnesses, intense exercise is beneficial, but in ME/CFS it is not recommended. The CDC states:[8]
Vigorous aerobic exercise can benefit people with many chronic illnesses. But people with ME/CFS do not tolerate such exercise routines. Standard exercise recommendations for healthy people can be harmful for patients with ME/CFS. However, it is important that patients with ME/CFS undertake activities that they can tolerate.
Graded exercise therapy (GET), a proposed treatment for ME/CFS that assumes deconditioning and a fear of activity play important roles in maintaining the illness, is no longer recommended for people with ME/CFS.[6][29]: 38 Reviews of GET either see weak evidence of a small to moderate effect[65][66] or no evidence of effectiveness.[67][68] GET can have serious adverse effects.[61] Similarly, a form of cognitive behavioural therapy (CBT) that assumed the illness is maintained by unhelpful beliefs about the illness and avoidance of activity is no longer recommended.[12]
Symptom relief
[edit]The first management step for sleep problems in ME/CFS is improving sleep habits. If sleep problems remain after implementing sleep hygiene routines, cognitive behavioural therapy for insomnia can be offered. Avoiding naps during the day can further improve sleep,[29]: 41 but there may be a trade-off with needed rest during the day.[2]: 36 Drugs that help with insomnia in fibromyalgia, such as trazodone or suvorexant, may help in ME/CFS too.[6]
Pain is initially managed with over-the-counter pain medication, such as ibuprofen or paracetamol (acetaminophen). If this is insufficient, referral to a pain specialist or counselling on pain management can be the next step. Heat treatment, hydrotherapy and gentle massage can sometimes help. In addition, stretching and exercise may help with pain, but a balance must be struck, as they can trigger PEM.[34] While there is lack of evidence on pharmaceutical options for pain management in ME/CFS, medication that works for fibromyalgia may be tried, such as pregabalin.[29]: 42 [6]
Like in other chronic illnesses, those with ME/CFS often experience mental health issues like anxiety and depression.[12] Psychotherapy, such as CBT may help manage the stress of being ill and teach self-management strategies.[2]: 42 Family sessions may be useful to educate people close to those with ME/CFS about the severity of the illness.[29]: 41 Antidepressants can be useful, but there may be more side effects than in the general population. For instance, it may be difficult to stop weight gain due to exercise intolerance.[29]: 52
Bowel issues are a common symptom of ME/CFS. For some, eliminating specific foods, such as caffeine, alcohol, gluten, or dairy, can alleviate symptoms.[12] Those with orthostatic intolerance can benefit from increased salt and fluid intake.[12] Compression stockings can help with orthostatic intolerance.[12]
Severe ME/CFS
[edit]People with moderate to severe ME/CFS may benefit from home adaptations and mobility aids, such as wheelchairs, disability parking, shower chairs, or stair lifts. To manage sensitivities to environmental stimuli, these stimuli can be limited. For instance, the surroundings can be made perfume-free, or an eye mask or earplugs can be used.[29]: 39–40 Those with severe ME/CFS may have significant trouble getting nutrition. Intravenous feeding (via blood) or tube feeding may be necessary to address this or to address electrolyte imbalances.[6]
Patients who cannot move easily in bed may need help to prevent pressure sores. Regular repositioning is important to keep their joints flexible and prevent contractures and stiffness. Osteoporosis may pose a risk over the long term.[69] Symptoms of severe ME/CFS may be misunderstood as neglect or abuse during well-being evaluations, and NICE recommends that professionals with experience in ME/CFS should be involved in any type of assessment for safeguarding.[2]: 22
Prognosis
[edit]Information on the prognosis of ME/CFS is limited. Complete recovery, partial improvement, and worsening are all possible,[11] but full recovery is uncommon.[10]: 11 Symptoms generally fluctuate over days, weeks, or longer periods, and some people may experience periods of remission. Overall, many will have to adjust to life with ME/CFS.[2]: 20
An early diagnosis may improve care and prognosis.[33] Factors that may make the disease worse over days, but also over longer periods, are physical and mental exertion, a new infection, sleep deprivation, and emotional stress.[10]: 11 Some people who improve need to manage their activities to prevent a relapse.[11] Children and teenagers are more likely to recover or improve than adults.[11][2]: 20 For instance, a study in Australia among 6- to 18-year-olds found that two-thirds reported recovery after 10 years and that the typical duration of illness was five years.[10]: 11
The effect of ME/CFS on life expectancy is poorly studied, and the evidence is mixed. One large retrospective study on the topic found no increase in all-cause mortality due to ME/CFS. Death from suicide was, however, significantly higher among those with ME/CFS.[29]: 59 In extreme cases, people can die from the illness.[61]
Epidemiology
[edit]
Reported prevalence rates vary widely depending on how ME/CFS is defined and diagnosed. Overall, around one in 150 people have ME/CFS. Based on the 1994 CDC diagnostic criteria, the global prevalence rate for CFS is 0.89%. In comparison, estimates using the stricter 1988 CDC criteria or the 2003 Canadian Consensus Criteria for ME/CFS produced a prevalence rate of only 0.17%.[9]
In England and Wales, over 250,000 people are estimated to be affected.[2]: 92 These estimates are based on data before the COVID-19 pandemic. It is likely that numbers have increased as a large share of people with long COVID meet the diagnostic criteria of ME/CFS.[10]: 228 A 2021–2022 CDC survey found that 1.3% of adults in the United States, or 3.3 million, had ME/CFS.[70]
Women are diagnosed with ME/CFS about 1.5 to four times more often than men.[9][37] The prevalence in children and adolescents is slightly lower than in adults,[9] and children have it less than adolescents.[71] The incidence rate (the onset of ME/CFS) has two peaks, one at 10–19 and another at 30–39 years,[4] and the prevalence is highest in middle age.[19]
History
[edit]From 1934 onwards, there were multiple outbreaks globally of an unfamiliar illness, initially mistaken for polio. A 1950s outbreak at London's Royal Free Hospital led to the term "benign myalgic encephalomyelitis" (ME). Those affected displayed symptoms such as malaise, sore throat, pain, and signs of nervous system inflammation. While its infectious nature was suspected, the exact cause remained elusive.[1]: 28–29 The syndrome appeared in sporadic as well as epidemic cases.[72]
In 1970, two UK psychiatrists proposed that these ME outbreaks were psychosocial phenomena, suggesting mass hysteria or altered medical perception as potential causes. This theory, though challenged, sparked controversy and cast doubt on ME's legitimacy in the medical community.[1]: 28–29
Melvin Ramsay's later research highlighted ME's disabling nature, prompting the removal of "benign" from the name and the creation of diagnostic criteria in 1986. These criteria included the tendency of muscles to tire after minor effort and take multiple days to recover, high symptom variability, and chronicity. Despite Ramsay's work and a UK report affirming that ME was not a psychological condition, scepticism persisted within the medical field, leading to limited research.[1]: 28–29
In the United States, Nevada and New York State saw outbreaks of what appeared similar to mononucleosis in the middle of the 1980s. People suffered from "chronic or recurrent fatigue", among a large number of other symptoms.[1]: 28–29 The initial link between elevated antibodies and the Epstein–Barr virus led to the name "chronic Epstein–Barr virus syndrome". The CDC renamed it chronic fatigue syndrome (CFS), as a viral cause could not be confirmed in studies.[73]: 155–158 An initial case definition of CFS was outlined in 1988;[1]: 28–29 the CDC published new diagnostic criteria in 1994, which became widely referenced.[74]
In the 2010s, ME/CFS began to gain more recognition from health professionals and the public. Two reports proved key in this shift. In 2015, the US Institute of Medicine produced a report with new diagnostic criteria that described ME/CFS as a "serious, chronic, complex systemic disease". Following this, the US National Institutes of Health published their Pathways to Prevention report, which gave recommendations on research priorities.[75]
Society and culture
[edit]
Controversy
[edit]ME/CFS is a contested illness, with debates mainly revolving around the cause of the illness and treatments.[76] Historically, there was a heated discussion about whether the condition was psychological or neurological.[57] Professionals who subscribed to the psychological model had frequent conflicts with patients, who believed their illness to be organic.[77] While ME/CFS is now generally believed to be a multisystem neuroimmune condition,[57] a subset of professionals still see the condition as psychosomatic, or an "illness-without-disease".[77][78]
The possible role of chronic viral infection in ME/CFS has been a subject of disagreement. One study caused considerable controversy by establishing a causal relationship between ME/CFS and a retrovirus called XMRV. Some with the illness began taking antiretroviral drugs targeted specifically for HIV/AIDS, another retrovirus,[79] and national blood supplies were suspected to be tainted with the retrovirus. After several years of study, the XMRV findings were determined to be the result of contamination of the testing materials.[80]
Treatments based on behavioural and psychological models of the illness have also been the subject of much contention. The largest clinical trial on behavioural interventions, the 2011 PACE trial, concluded that graded exercise therapy and CBT are moderately effective. The trial drew heavy criticism.[76] The study authors weakened their definition of recovery during the trial: some participants now met a key criterion for recovery before the trial started. A reanalysis under the original clinical trial protocol showed no significant difference in recovery rate between treatment groups and the controls receiving standard care.[81][82]
Doctor–patient relations
[edit]People with ME/CFS often face stigma in healthcare settings,[21] and the majority of individuals report negative healthcare experiences. They may feel that their doctor inappropriately calls their illness psychological or doubts the severity of their symptoms.[83] They may also feel forced to prove that they are legitimately ill.[84] Some may be given outdated treatments that provoke symptoms or assume their illness is due to unhelpful thoughts and deconditioning.[12]: 2871 [18]
Clinicians may be unfamiliar with ME/CFS, as it is often not fully covered in medical school.[18] Due to this unfamiliarity, people may go undiagnosed for years[12] or be misdiagnosed with mental health conditions.[18] As individuals gain knowledge about their illness over time, their relationship with treating physicians changes. They may feel on a more equal footing with their doctors and able to work in partnership. At times, relationships may deteriorate instead as the previous asymmetry of knowledge breaks down.[85]
Economic and social impact
[edit]ME/CFS negatively impacts people's social lives and relationships. Stress can be compounded by disbelief in the illness from the support network, who can be sceptical due to the subjective nature of diagnosis. Many people with the illness feel socially isolated, and thoughts of suicide are high, especially in those without a supportive care network.[85] ME/CFS interrupts normal development in children, making them more dependent on their family for assistance instead of gaining independence as they age.[86] Caring for somebody with ME/CFS can be a full-time role, and the stress of caregiving is made worse by the lack of effective treatments.[87]
Economic costs due to ME/CFS are significant.[88] In the United States, estimates range from $36 to $51 billion per year, considering both lost wages and healthcare costs.[89] A 2017 estimate for the annual economic burden in the United Kingdom was £3.3 billion.[13]
Advocacy
[edit]
Patient organisations have aimed to involve researchers via activism but also by publishing research themselves—similarly to AIDS activism in the 1980s, which also sought to combat underfunding and stigma. Citizen scientists, for example, helped start discussions about weaknesses in trials of psychological treatments.[76]
ME/CFS International Awareness Day takes place on 12 May.[90] The goal of the day is to raise awareness among the public and health care workers about the diagnosis and treatment of ME/CFS.[91] The date was chosen because it is the birthday of Florence Nightingale, who had an unidentified illness similar to ME/CFS.[90]
Research
[edit]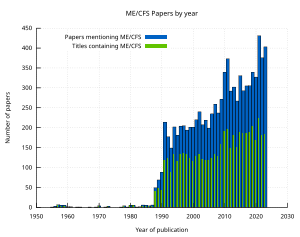
Research into ME/CFS seeks to find a better understanding of the disease's causes, biomarkers to aid in diagnosis, and treatments to relieve symptoms.[1]: 10 The emergence of long COVID has sparked increased interest in ME/CFS, as the two conditions may share pathology and treatment for one may treat the other.[25][14]
Funding
[edit]Historical research funding for ME/CFS has been far below that of comparable diseases.[22][92] In a 2015 report, the US National Academy of Sciences said that "remarkably little research funding" had been dedicated to causes, mechanisms, and treatment.[1]: 9 Lower funding levels have led to a smaller number and size of studies.[93] In addition, drug companies have invested very little in the disease.[94]
The US National Institutes of Health (NIH) is the largest biomedical funder worldwide.[95] Using rough estimates of disease burden, a study found NIH funding for ME/CFS was only 3% to 7% of the average disease per healthy life year lost between 2015 and 2019.[96] Worldwide, multiple sclerosis, which affects fewer people and results in disability no worse than ME/CFS, received 20 times as much funding between 2007 and 2015.[92][22]
Multiple reasons have been proposed for the low funding levels. Diseases for which society "blames the victim" are frequently underfunded. This may explain why COPD, a severe lung disease often caused by smoking, receives low funding per healthy life year lost.[97] Similarly, for ME/CFS, the historical belief that it is caused by psychological factors may have contributed to lower funding. Gender bias may also play a role; the NIH spends less on diseases that predominantly affect women in relation to disease burden. Less well-funded research areas may also struggle to compete with more mature areas of medicine for the same grants.[96]
Directions
[edit]Many biomarkers for ME/CFS have been proposed. Studies on biomarkers have often been too small to draw robust conclusions. Natural killer cells have been identified as an area of interest for biomarker research as they show consistent abnormalities.[7] Other proposed markers include electrical measurements of blood cells and Raman microscopy of immune cells.[14] Several small studies have investigated the genetics of ME/CFS, but none of their findings have been replicated.[13] A larger study, DecodeME, is currently underway in the United Kingdom.[98]
Various drug treatments for ME/CFS are being explored. Drugs under investigation often target the nervous system, the immune system, autoimmunity, or pain directly. More recently, there has been a growing interest in drugs targeting energy metabolism.[94] In several clinical trials of ME/CFS, rintatolimod showed a small reduction in symptoms, but improvements were not sustained after discontinuation.[99][94] Rintatolimod has been approved in Argentina.[100] Rituximab, a drug that depletes B cells, was studied and found to be ineffective.[14] Another option targeting autoimmunity is immune adsorption, which removes a large set of (auto)antibodies from the blood.[94]
Challenges
[edit]Symptoms and their severity can widely differ among people with ME/CFS. This poses a challenge for research into the cause and progression of the disease. Dividing people into subtypes may help manage this heterogeneity.[14] The existence of multiple diagnostic criteria and variations in how scientists apply them complicate comparisons between studies.[1]: 53 Definitions also vary in which co-occurring conditions preclude a diagnosis of ME/CFS.[1]: 52
See also
[edit]References
[edit]- ^ a b c d e f g h i j k l m Committee on the Diagnostic Criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, Board on the Health of Select Populations, Institute of Medicine (10 February 2015). Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness (PDF). National Academies Press. ISBN 978-0-309-31689-7. PMID 25695122. Archived (PDF) from the original on 20 January 2017. Retrieved 28 July 2020.
- ^ a b c d e f g h i j k l m n o p q "Myalgic Encephalomyelitis (Or Encephalopathy)/Chronic Fatigue Syndrome: Diagnosis and Management: NICE Guideline". National Institute for Health and Care Excellence (NICE). 29 October 2021. Archived from the original on 8 February 2024. Retrieved 9 March 2024.
- ^ a b c d e f g "Symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". U.S. Centers for Disease Control and Prevention (CDC). 10 May 2024. Archived from the original on 17 May 2024. Retrieved 17 May 2024.
- ^ a b Collard SS, Murphy J (September 2020). "Management of chronic fatigue syndrome/myalgic encephalomyelitis in a pediatric population: A scoping review". Journal of Child Health Care. 24 (3): 411–431. doi:10.1177/1367493519864747. PMC 7863118. PMID 31379194.
- ^ "Myalgic Encephalomyelitis (Or Encephalopathy)/Chronic Fatigue Syndrome: Diagnosis and Management: Information for the Public". National Institute for Health and Care Excellence (NICE). 29 October 2021. Archived from the original on 4 April 2024. Retrieved 24 March 2024.
- ^ a b c d e f g h i j k l Grach SL, Seltzer J, Chon TY, Ganesh R (October 2023). "Diagnosis and Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Mayo Clinic Proceedings. 98 (10): 1544–1551. doi:10.1016/j.mayocp.2023.07.032. PMID 37793728. S2CID 263665180.
- ^ a b c d e Maksoud R, Magawa C, Eaton-Fitch N, Thapaliya K, Marshall-Gradisnik S (May 2023). "Biomarkers for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): a systematic review". BMC Medicine. 21 (1): 189. doi:10.1186/s12916-023-02893-9. PMC 10206551. PMID 37226227.
- ^ a b c d e f "Manage Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". U.S. Centers for Disease Control and Prevention (CDC). 10 May 2024. Archived from the original on 18 May 2024. Retrieved 18 May 2024.
- ^ a b c d e f g h Lim EJ, Ahn YC, Jang ES, Lee SW, Lee SH, Son CG (February 2020). "Systematic Review and Meta-Analysis Of the Prevalence of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME)". Journal of Translational Medicine. 18 (1): 100. doi:10.1186/s12967-020-02269-0. PMC 7038594. PMID 32093722.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) (17 April 2023). Myalgische Enzephalomyelitis / Chronic Fatigue Syndrome (ME/CFS): Aktueller Kenntnisstand [Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): current state of knowledge] (PDF) (in German). Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. ISSN 1864-2500. Archived (PDF) from the original on 2 November 2023. Retrieved 8 November 2023.
- ^ a b c d e f g h i j k "Clinical Overview of ME/CFS". U.S. Centers for Disease Control and Prevention (CDC). 10 May 2024. Archived from the original on 17 May 2024. Retrieved 17 May 2024.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z Bateman L, Bested AC, Bonilla HF, Chheda BV, Chu L, Curtin JM, et al. (November 2021). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Essentials of Diagnosis and Management". Mayo Clinic Proceedings. 96 (11): 2861–2878. doi:10.1016/j.mayocp.2021.07.004. PMID 34454716. S2CID 237419583.
- ^ a b c d e Dibble JJ, McGrath SJ, Ponting CP (September 2020). "Genetic Risk Factors of ME/CFS: A Critical Review". Human Molecular Genetics. 29 (R1): R117 – R124. doi:10.1093/hmg/ddaa169. PMC 7530519. PMID 32744306.
- ^ a b c d e f g h i j k l m Annesley SJ, Missailidis D, Heng B, Josev EK, Armstrong CW (March 2024). "Unravelling Shared Mechanisms: Insights from Recent ME/CFS Research to Illuminate Long COVID Pathologies". Trends in Molecular Medicine. 30 (5): 443–458. doi:10.1016/j.molmed.2024.02.003. PMID 38443223.
- ^ "Myalgic encephalomyelitis (Chronic fatigue syndrome) - Symptoms, diagnosis and treatment | BMJ Best Practice US". bestpractice.bmj.com. Retrieved 21 October 2024.
- ^ "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (CFS) | Diseases & Conditions | 5MinuteConsult". 5minuteconsult.com. Retrieved 25 November 2024.
- ^ a b c d Unger ER, Lin JS, Brimmer DJ, Lapp CW, Komaroff AL, Nath A, et al. (December 2016). "CDC Grand Rounds: Chronic Fatigue Syndrome – Advancing Research and Clinical Education" (PDF). MMWR. Morbidity and Mortality Weekly Report. 65 (50–51): 1434–1438. doi:10.15585/mmwr.mm655051a4. PMID 28033311. Archived (PDF) from the original on 6 January 2017. Retrieved 5 January 2017.
- ^ a b c d e Davis HE, McCorkell L, Vogel JM, Topol EJ (March 2023). "Long COVID: Major Findings, Mechanisms and Recommendations". Nature Reviews. Microbiology. 21 (3): 133–146. doi:10.1038/s41579-022-00846-2. PMC 9839201. PMID 36639608.
- ^ a b c "ME/CFS Basics". U.S. Centers for Disease Control and Prevention (CDC). 10 May 2024. Archived from the original on 23 May 2024. Retrieved 25 May 2024.
- ^ Boulazreg, S, Rokach A (17 July 2020). "The Lonely, Isolating, and Alienating Implications of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Healthcare. 8 (4): 413–433. doi:10.3390/healthcare8040413. ISSN 2164-1846. PMC 7711762. PMID 33092097.
- ^ a b Hussein S, Eiriksson L, MacQuarrie M, Merriam S, Dalton M, Stein E, et al. (2024). "Healthcare System Barriers Impacting the Care of Canadians with Myalgic Encephalomyelitis: A Scoping Review". Journal of Evaluation in Clinical Practice. 30 (7): 1337–1360. doi:10.1111/jep.14047. ISSN 1356-1294. PMID 39031904.
- ^ a b c Tyson S, Stanley K, Gronlund TA, Leary S, Emmans Dean M, Dransfield C, et al. (2022). "Research Priorities for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): The Results of a James Lind Alliance Priority Setting Exercise". Fatigue: Biomedicine, Health & Behavior. 10 (4): 200–211. doi:10.1080/21641846.2022.2124775. ISSN 2164-1846. S2CID 252652429.
- ^ Bateman L (2022). "Fibromyalgia and myalgic encephalomyelitis/chronic fatigue syndrome". In Zigmond M, Wiley C, Chesselet MF (eds.). Neurobiology of Brain Disorders : Biological Basis of Neurological and Psychiatric Disorders (2nd ed.). Elsevier. ISBN 978-0-323-85654-6.
- ^ a b Shan ZY, Barnden LR, Kwiatek RA, Bhuta S, Hermens DF, Lagopoulos J (September 2020). "Neuroimaging Characteristics of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Systematic Review". Journal of Translational Medicine. 18 (1): 335. doi:10.1186/s12967-020-02506-6. PMC 7466519. PMID 32873297.
- ^ a b c Marshall-Gradisnik S, Eaton-Fitch N (September 2022). "Understanding myalgic encephalomyelitis". Science. 377 (6611): 1150–1151. Bibcode:2022Sci...377.1150M. doi:10.1126/science.abo1261. hdl:10072/420658. PMID 36074854. S2CID 252159772.
- ^ a b c Choutka J, Jansari V, Hornig M, Iwasaki A (May 2022). "Unexplained Post-Acute Infection Syndromes". Nature Medicine. 28 (5): 911–923. doi:10.1038/s41591-022-01810-6. PMID 35585196. S2CID 248889597.
- ^ "8E49 Postviral Fatigue Syndrome". ICD-11 – Mortality and Morbidity Statistics. World Health Organization. Archived from the original on 1 August 2018. Retrieved 20 May 2020.
- ^ a b Bhatia S, Jason LA (24 February 2023). "Using Data Mining and Time Series to Investigate ME and CFS Naming Preferences". Journal of Disability Policy Studies. 35: 65–72. doi:10.1177/10442073231154027. ISSN 1044-2073. S2CID 257198201. Archived from the original on 6 November 2023. Retrieved 15 October 2023.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah Baraniuk JN, Marshall-Gradisnik S, Eaton-Fitch N (January 2024). BMJ Best Practice: Myalgic Encephalomyelitis (Chronic Fatigue Syndrome). BMJ Publishing Group. Archived from the original on 19 February 2024. Retrieved 19 January 2024.
- ^ Jason LA, Johnson M (2 April 2020). "Solving the ME/CFS Criteria and Name Conundrum: The Aftermath of IOM". Fatigue: Biomedicine, Health & Behavior. 8 (2): 97–107. doi:10.1080/21641846.2020.1757809. ISSN 2164-1846. S2CID 219011696.
- ^ Jason L, Jessen T, Porter N, Boulton A, Gloria-Njoku M (16 July 2009). "Examining Types of Fatigue Among Individuals with ME/CFS". Disability Studies Quarterly. 29 (3). doi:10.18061/dsq.v29i3.938. ISSN 2159-8371.
- ^ Jason LA, Boulton A, Porter NS, Jessen T, Njoku MG, Friedberg F (24 February 2010). "Classification of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome by Types of Fatigue". Behavioral Medicine. 36 (1): 24–31. doi:10.1080/08964280903521370. ISSN 0896-4289. PMC 4852700. PMID 20185398.
- ^ a b c d e f g h i National Guideline Centre (UK) (2021). Identifying and Diagnosing ME/CFS: Myalgic Encephalomyelitis (Or Encephalopathy) / Chronic Fatigue Syndrome: Diagnosis and Management: Evidence Review D (PDF). NICE Evidence Reviews Collection. London: National Institute for Health and Care Excellence (NICE). ISBN 978-1-4731-4221-3. PMID 35438857. Archived from the original on 19 February 2024. Retrieved 23 September 2023.
- ^ a b c d e "Strategies to Prevent Worsening of Symptoms". U.S. Centers for Disease Control and Prevention (CDC). 10 May 2024. Archived from the original on 18 May 2024. Retrieved 18 May 2024.
- ^ Aoun Sebaiti M, Hainselin M, Gounden Y, Sirbu CA, Sekulic S, Lorusso L, et al. (February 2022). "Systematic Review and Meta-Analysis Of Cognitive Impairment in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Scientific Reports. 12 (1): 2157. Bibcode:2022NatSR..12.2157A. doi:10.1038/s41598-021-04764-w. PMC 8828740. PMID 35140252.
- ^ Pollack B, von Saltza E, McCorkell L, Santos L, Hultman A, Cohen AK, et al. (2023). "Female Reproductive Health Impacts of Long COVID and Associated Illnesses Including ME/CFS, POTS, And Connective Tissue Disorders: A Literature Review". Frontiers in Rehabilitation Sciences. 4: 1122673. doi:10.3389/fresc.2023.1122673. PMC 10208411. PMID 37234076.
- ^ a b "Epidemiology". U.S. Centers for Disease Control and Prevention (CDC). 21 March 2023. Archived from the original on 6 March 2024. Retrieved 13 April 2024.
- ^ Hwang JH, Lee JS, Oh HM, Lee EJ, Lim EJ, Son CG (October 2023). "Evaluation of Viral Infection as an Etiology of ME/CFS: A Systematic Review and Meta-Analysis". Journal of Translational Medicine. 21 (1): 763. doi:10.1186/s12967-023-04635-0. PMC 10612276. PMID 37898798.
- ^ Rasa S, Nora-Krukle Z, Henning N, Eliassen E, Shikova E, Harrer T, et al. (October 2018). "Chronic Viral Infections in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Journal of Translational Medicine. 16 (1): 268. doi:10.1186/s12967-018-1644-y. PMC 6167797. PMID 30285773.
- ^ Altmann DM, Whettlock EM, Liu S, Arachchillage DJ, Boyton RJ (October 2023). "The Immunology of Long COVID". Nature Reviews. Immunology. 23 (10): 618–634. doi:10.1038/s41577-023-00904-7. PMID 37433988. S2CID 259831825.
- ^ Ruiz-Pablos M, Paiva B, Zabaleta A (September 2023). "Epstein-Barr Virus-Acquired Immunodeficiency in Myalgic encephalomyelitis-Is It Present in Long COVID?". Journal of Translational Medicine. 21 (1): 633. doi:10.1186/s12967-023-04515-7. PMC 10506247. PMID 37718435.
- ^ Bateman L, Hanson M (15 May 2024). Report of the ME/CFS Research Roadmap Working Group of Council (PDF) (Report). National Institutes of Health (NIH). Archived (PDF) from the original on 22 May 2024. Retrieved 25 May 2024.
- ^ Eriksen W (16 August 2018). "ME/CFS, Case Definition, And Serological Response to Epstein–Barr Virus. A Systematic Literature Review". Fatigue: Biomedicine, Health & Behavior. 6 (4): 220–34. doi:10.1080/21641846.2018.1503125. S2CID 80898744.
- ^ a b Maksoud R, du Preez S, Eaton-Fitch N, Thapaliya K, Barnden L, Cabanas H, et al. (2020). "A Systematic Review of Neurological Impairments in Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome Using Neuroimaging Techniques". PLOS ONE. 15 (4): e0232475. Bibcode:2020PLoSO..1532475M. doi:10.1371/journal.pone.0232475. PMC 7192498. PMID 32353033.
- ^ Lee JS, Sato W, Son CG (November 2023). "Brain-Regional Characteristics and Neuroinflammation in ME/CFS Patients from Neuroimaging: A Systematic Review and Meta-Analysis". Autoimmunity Reviews. 23 (2): 103484. doi:10.1016/j.autrev.2023.103484. PMID 38016575.
- ^ VanElzakker MB, Brumfield SA, Lara Mejia PS (2019). "Neuroinflammation and Cytokines in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): A Critical Review of Research Methods". Frontiers in Neurology. 9: 1033. doi:10.3389/fneur.2018.01033. PMC 6335565. PMID 30687207.
- ^ Mohamed AZ, Andersen T, Radovic S, Del Fante P, Kwiatek R, Calhoun V, et al. (June 2023). "Objective Sleep Measures in Chronic Fatigue Syndrome Patients: A Systematic Review and Meta-Analysis". Sleep Medicine Reviews. 69: 101771. doi:10.1016/j.smrv.2023.101771. PMC 10281648. PMID 36948138.
- ^ Nelson MJ, Bahl JS, Buckley JD, Thomson RL, Davison K (October 2019). "Evidence of Altered Cardiac Autonomic Regulation in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Systematic Review and Meta-Analysis". Medicine. 98 (43): e17600. doi:10.1097/MD.0000000000017600. PMC 6824690. PMID 31651868.
- ^ Eaton-Fitch N, du Preez S, Cabanas H, Staines D, Marshall-Gradisnik S (November 2019). "A Systematic Review of Natural Killer Cells Profile and Cytotoxic Function in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Systematic Reviews. 8 (1): 279. doi:10.1186/s13643-019-1202-6. PMC 6857215. PMID 31727160.
- ^ a b Sotzny F, Blanco J, Capelli E, Castro-Marrero J, Steiner S, Murovska M, et al. (European Network on ME/CFS (EUROMENE)) (June 2018). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome – Evidence for an Autoimmune Disease". Autoimmunity Reviews. 17 (6): 601–609. doi:10.1016/j.autrev.2018.01.009. PMID 29635081.
- ^ Wirth K, Scheibenbogen C (June 2020). "A Unifying Hypothesis of the Pathophysiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Recognitions from the Finding of Autoantibodies Against Β2-Adrenergic Receptors". Autoimmunity Reviews. 19 (6): 102527. doi:10.1016/j.autrev.2020.102527. PMID 32247028.
- ^ Lim EJ, Kang EB, Jang ES, Son CG (December 2020). "The Prospects of the Two-Day Cardiopulmonary Exercise Test (CPET) in ME/CFS Patients: A Meta-Analysis". Journal of Clinical Medicine. 9 (12): 4040. doi:10.3390/jcm9124040. PMC 7765094. PMID 33327624.
- ^ Franklin JD, Graham M (3 July 2022). "Repeated Maximal Exercise Tests of Peak Oxygen Consumption in People with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Systematic Review and Meta-Analysis". Fatigue: Biomedicine, Health & Behavior. 10 (3): 119–135. doi:10.1080/21641846.2022.2108628. ISSN 2164-1846. S2CID 251636593.
- ^ Holden S, Maksoud R, Eaton-Fitch N, Cabanas H, Staines D, Marshall-Gradisnik S (July 2020). "A Systematic Review of Mitochondrial Abnormalities in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome/Systemic Exertion Intolerance Disease". Journal of Translational Medicine. 18 (1): 290. doi:10.1186/s12967-020-02452-3. PMC 7392668. PMID 32727475.
- ^ Morris G, Anderson G, Maes M (November 2017). "Hypothalamic-Pituitary-Adrenal Hypofunction in Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS) as a Consequence of Activated Immune-Inflammatory And Oxidative and Nitrosative Pathways". Molecular Neurobiology. 54 (9): 6806–6819. doi:10.1007/s12035-016-0170-2. PMID 27766535. S2CID 3524276.
- ^ a b "Diagnosing ME/CFS". U.S. Centers for Disease Control and Prevention (CDC). 13 May 2024. Archived from the original on 17 May 2024. Retrieved 17 May 2024.
- ^ a b c Lim EJ, Son CG (July 2020). "Review of Case Definitions for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Journal of Translational Medicine. 18 (1): 289. doi:10.1186/s12967-020-02455-0. PMC 7391812. PMID 32727489.
- ^ Kingdon C, Lowe A, Shepherd C, Nacul L (2022). "What Primary Care Practitioners Need to Know about the New NICE Guideline for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in Adults". Healthcare. 10 (12): 2438. doi:10.3390/healthcare10122438. ISSN 2227-9032. PMC 9778354. PMID 36553962.
- ^ Baraniuk JN (January 2022). Myalgic Encephalomyelitis (Chronic Fatigue Syndrome) (PDF). BMJ Best Practice. Archived (PDF) from the original on 9 October 2023. Retrieved 30 September 2023.
- ^ "Monitoring the Use of Medicines and Supplements". U.S. Centers for Disease Control and Prevention (CDC). 10 May 2024. Archived from the original on 25 May 2024. Retrieved 25 May 2024.
- ^ a b c d Hoffmann K, Hainzl A, Stingl M, Kurz K, Biesenbach B, Bammer C, et al. (August 2024). "Interdisziplinäres, kollaboratives D-A-CH Konsensus-Statement zur Diagnostik und Behandlung von Myalgischer Enzephalomyelitis/Chronischem Fatigue-Syndrom" [Interdisciplinary, collaborative D-A-CH (Germany, Austria and Switzerland) consensus statement concerning the diagnostic and treatment of myalgic encephalomyelitis/chronic fatigue syndrome]. Wiener Klinische Wochenschrift (in German). 136 (Suppl 5): 103–123. doi:10.1007/s00508-024-02372-y. PMC 11093804. PMID 38743348.
- ^ a b O'Connor K, Sunnquist M, Nicholson L, Jason LA, Newton JL, Strand EB (March 2019). "Energy Envelope Maintenance Among Patients with Myalgic Encephalomyelitis and Chronic Fatigue Syndrome: Implications of Limited Energy Reserves". Chronic Illness. 15 (1): 51–60. doi:10.1177/1742395317746470. PMC 5750135. PMID 29231037.
- ^ Goudsmit EM, Nijs J, Jason LA, Wallman KE (19 December 2011). "Pacing as a strategy to improve energy management in myalgic encephalomyelitis/chronic fatigue syndrome: a consensus document". Disability and Rehabilitation. 34 (13): 1140–1147. doi:10.3109/09638288.2011.635746. PMID 22181560. S2CID 22457926. Archived from the original on 28 July 2020. Retrieved 23 May 2020.
- ^ a b Sanal-Hayes NE, Mclaughlin M, Hayes LD, Mair JL, Ormerod J, Carless D, et al. (October 2023). "A Scoping Review of 'Pacing' for Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Lessons Learned for the Long COVID Pandemic". Journal of Translational Medicine. 21 (1): 720. doi:10.1186/s12967-023-04587-5. PMC 10576275. PMID 37838675.
- ^ Chou R, McDonagh M, Griffins J, Grusing S (2022). Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): An Updated Systematic Evidence Review (PDF). U.S. Centers for Disease Control and Prevention. Archived from the original (PDF) on 14 February 2024. Retrieved 30 March 2023.
- ^ Larun L, Brurberg KG, Odgaard-Jensen J, Price JR (October 2019). "Exercise Therapy for Chronic Fatigue Syndrome". The Cochrane Database of Systematic Reviews. 10 (10): CD003200. doi:10.1002/14651858.CD003200.pub8. PMC 6953363. PMID 31577366.
- ^ Geraghty K, Jason L, Sunnquist M, Tuller D, Blease C, Adeniji C (23 April 2019). "The 'Cognitive Behavioural Model' of Chronic Fatigue Syndrome: Critique of a Flawed Model". Health Psychology Open. 6 (1): 2055102919838907. doi:10.1177/2055102919838907. PMC 6482658. PMID 31041108.
- ^ Ahmed SA, Mewes JC, Vrijhoef H (February 2020). "Assessment of the Scientific Rigour of Randomized Controlled Trials on the Effectiveness of Cognitive Behavioural Therapy and Graded Exercise Therapy for Patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Systematic Review". Journal of Health Psychology. 25 (2): 240–255. doi:10.1177/1359105319847261. PMID 31072121. S2CID 149443976.
- ^ "ME/CFS Clinical Care for Severely Affected Patients". U.S. Centers for Disease Control and Prevention (CDC). 13 May 2024. Archived from the original on 28 May 2024. Retrieved 15 June 2024.
- ^ Vahratian A, Lin JS, Bertolli J, Unger ER (8 December 2023). Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in Adults: United States, 2021–2022 (Report). National Center for Health Statistics. pp. 1–8. doi:10.15620/cdc:134504. PMID 38085820. NCHS Data Brief. Archived from the original on 17 February 2024. Retrieved 8 December 2023.
- ^ "Fast Facts: ME/CFS". U.S. Centers for Disease Control and Prevention (CDC). 31 May 2024. Archived from the original on 3 June 2024. Retrieved 15 June 2024.
- ^ Price JL (April 1961). "Myalgic Encephalomyelitis". Lancet. 1 (7180): 737–738. doi:10.1016/s0140-6736(61)92893-8. PMC 1836797. PMID 13737972.
- ^ Packard RM (2004). Emerging Illnesses and Society: Negotiating the Public Health Agenda. Johns Hopkins University Press. ISBN 978-0-8018-7942-5. Archived from the original on 18 May 2023. Retrieved 6 February 2024.
- ^ Brurberg KG, Fønhus MS, Larun L, Flottorp S, Malterud K (February 2014). "Case Definitions for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME): A Systematic Review". BMJ Open. 4 (2): e003973. doi:10.1136/bmjopen-2013-003973. PMC 3918975. PMID 24508851.
- ^ Friedberg F (2 January 2020). "Legitimizing Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Indications of Change over a Decade". Fatigue: Biomedicine, Health & Behavior. 8 (1): 24–31. doi:10.1080/21641846.2020.1718292. ISSN 2164-1846. S2CID 214434278. Archived from the original on 4 February 2024. Retrieved 4 February 2024.
- ^ a b c Blease C, Geraghty KJ (September 2018). "Are ME/CFS Patient Organizations 'Militant'? : Patient Protest in a Medical Controversy". Journal of Bioethical Inquiry. 15 (3): 393–401. doi:10.1007/s11673-018-9866-5. PMID 29971693. S2CID 49677273.
- ^ a b O'Leary D (December 2020). "A Concerning Display of Medical Indifference: Reply to 'Chronic Fatigue Syndrome and an Illness-Focused Approach to Care: Controversy, Morality and Paradox'". Medical Humanities. 46 (4): e4. doi:10.1136/medhum-2019-011743. PMID 32601171. S2CID 220253462.
- ^ Geraghty K (2 July 2020). "The Negative Impact of the Psychiatric Model of Chronic Fatigue Syndrome on Doctors' Understanding and Management of the Illness". Fatigue: Biomedicine, Health & Behavior. 8 (3): 167–180. doi:10.1080/21641846.2020.1834295. ISSN 2164-1846.
- ^ Westly E (June 2011). "Retrovirus No Longer Thought to Be Cause of Chronic Fatigue Syndrome". Scientific American. Archived from the original on 22 February 2024. Retrieved 22 February 2024.
- ^ Johnson AD, Cohn CS (October 2016). "Xenotropic Murine Leukemia Virus-Related Virus (XMRV) and the Safety of the Blood Supply". Clinical Microbiology Reviews. 29 (4): 749–57. doi:10.1128/CMR.00086-15. PMC 5010753. PMID 27358491.
- ^ Geraghty KJ (August 2017). "Further Commentary on the PACE Trial: Biased Methods and Unreliable Outcomes". Journal of Health Psychology. 22 (9): 1209–1216. doi:10.1177/1359105317714486. PMID 28805517.
- ^ Friedberg F, Sunnquist M, Nacul L (March 2020). "Rethinking the Standard of Care for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Journal of General Internal Medicine. 35 (3): 906–909. doi:10.1007/s11606-019-05375-y. PMC 7080939. PMID 31637650.
- ^ McManimen S, McClellan D, Stoothoff J, Gleason K, Jason LA (March 2019). "Dismissing Chronic Illness: A Qualitative Analysis of Negative Health Care Experiences". Health Care for Women International. 40 (3): 241–258. doi:10.1080/07399332.2018.1521811. PMC 6567989. PMID 30829147.
- ^ Dumit J (February 2006). "Illnesses You Have to Fight to Get: Facts as Forces in Uncertain, Emergent Illnesses". Social Science & Medicine. 62 (3): 577–590. doi:10.1016/j.socscimed.2005.06.018. PMID 16085344.
- ^ a b Shortland D, Fazil Q, Lavis A, Hallett N (4 April 2024). "A Systematic Scoping Review of How People with ME/CFS Use the Internet". Fatigue: Biomedicine, Health & Behavior. 12 (2): 142–176. doi:10.1080/21641846.2024.2303887. ISSN 2164-1846.
- ^ Parslow RM, Harris S, Broughton J, Alattas A, Crawley E, Haywood K, et al. (January 2017). "Children's Experiences of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME): A Systematic Review and Meta-Ethnography Of Qualitative Studies". BMJ Open. 7 (1): e012633. doi:10.1136/bmjopen-2016-012633. PMC 5253584. PMID 28087544.
- ^ O'Dwyer S, Boothby S, Smith G, Biddle L, Muirhead N, Khot S (July 2022). "Unpaid Carers Are the Missing Piece in Treatment Guidelines and Research Priorities for ME/CFS" (PDF). BMJ. 378: o1691. doi:10.1136/bmj.o1691. hdl:10871/130699. PMID 35835467. S2CID 250533596. Archived (PDF) from the original on 6 March 2024. Retrieved 21 February 2024.
- ^ Pheby DF, Araja D, Berkis U, Brenna E, Cullinan J, de Korwin JD, et al. (April 2020). "The Development of a Consistent Europe-Wide Approach to Investigating the Economic Impact of Myalgic Encephalomyelitis (ME/CFS): A Report from the European Network on ME/CFS (EUROMENE)". Healthcare. 8 (2): 88. doi:10.3390/healthcare8020088. PMC 7349118. PMID 32272608.
- ^ Jason LA, Mirin AA (January 2021). "Updating the National Academy of Medicine ME/CFS Prevalence and Economic Impact Figures to Account for Population Growth and Inflation" (PDF). Fatigue: Biomedicine, Health & Behavior. 9 (1): 9–13. doi:10.1080/21641846.2021.1878716. ISSN 2164-1846. S2CID 233745601. Archived (PDF) from the original on 15 March 2023. Retrieved 21 January 2023.
- ^ a b "ME/CFS Awareness Day". U.S. Centers for Disease Control and Prevention. 10 May 2024. Archived from the original on 17 May 2024. Retrieved 17 May 2024.
- ^ Lee N (12 May 2012). "Dr. Nancy Lee on International Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Awareness Day". US Department of Health and Human Services. Archived from the original on 8 July 2012. Retrieved 12 October 2013.
- ^ a b Radford G, Chowdhury S (2016). "ME/CFS Research Funding – An Overview Of Activity By Major Institutional Funders Included on the Dimensions Database" (PDF). UK CFS/ME Research Collaborative and ÜberResearch. Archived (PDF) from the original on 4 February 2024. Retrieved 6 April 2023.
- ^ Scheibenbogen C, Freitag H, Blanco J, Capelli E, Lacerda E, Authier J, et al. (July 2017). "The European ME/CFS Biomarker Landscape Project: An Initiative of the European Network EUROMENE". Journal of Translational Medicine. 15 (1): 162. doi:10.1186/s12967-017-1263-z. PMC 5530475. PMID 28747192.
- ^ a b c d Toogood PL, Clauw DJ, Phadke S, Hoffman D (March 2021). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Where Will the Drugs Come From?". Pharmacological Research. 165: 105465. doi:10.1016/j.phrs.2021.105465. PMID 33529750. S2CID 231787959.
- ^ "Grants & Funding". National Institutes of Health (NIH). Archived from the original on 28 November 2023. Retrieved 22 November 2023.
- ^ a b Mirin AA (July 2021). "Gender Disparity in the Funding of Diseases by the U.S. National Institutes of Health". Journal of Women's Health. 30 (7): 956–963. doi:10.1089/jwh.2020.8682. PMC 8290307. PMID 33232627.
- ^ Mirin AA, Dimmock ME, Jason LA (2020). Mooney A (ed.). "Research Update: The Relation Between ME/CFS Disease Burden and Research Funding in the USA". Work. 66 (2): 277–282. doi:10.3233/WOR-203173. PMID 32568148. S2CID 219974997.
- ^ "Experts Launch World's Largest Genetic Study of ME". BBC News. 12 September 2022. Archived from the original on 20 January 2023. Retrieved 20 January 2023.
- ^ Richman S, Morris MC, Broderick G, Craddock TJ, Klimas NG, Fletcher MA (May 2019). "Pharmaceutical Interventions in Chronic Fatigue Syndrome: A Literature-Based Commentary". Clinical Therapeutics. 41 (5): 798–805. doi:10.1016/j.clinthera.2019.02.011. PMC 6543846. PMID 30871727.
- ^ Agrawal S, Kandimalla ER (February 2019). "Chapter 14: Synthetic agonists of Toll-like receptors and therapeutic applications.". In Agrawal S, Gait MJ (eds.). Advances in Nucleic Acid Therapeutics. Royal Society of Chemistry. pp. 306–338 (310). ISBN 978-1-78801-732-9. Archived from the original on 14 May 2022. Retrieved 20 October 2021.
14.2: Agonists of TLR3
