Crohn's disease: Difference between revisions
Dollarwizard (talk | contribs) →Complementary and alternative medicine: The study was about cannabis-derived compounds, so I am adjusting this sentence |
m Fix CW Error #61 with GenFixes (T1) |
||
| Line 1: | Line 1: | ||
{{Short description|Type of inflammatory bowel disease}} |
|||
{{Infobox disease |
|||
{{cs1 config|name-list-style=vanc|display-authors=6}} |
|||
| Name = Crohn's disease |
|||
{{Use mdy dates|date=November 2021}} |
|||
| Latin = morbus Leśniowski-Crohn |
|||
{{Infobox medical condition (new) |
|||
| Image = Patterns of CD.svg |
|||
| |
| name = Crohn's disease |
||
| image = CD colitis 2.jpg |
|||
[[ileum|ileal]], [[ileocolic]] and [[Colon (anatomy)|colon]]ic.<ref name=Baumgart/> |
|||
| caption = Endoscopic image of severe Crohn's colitis showing diffuse loss of mucosal architecture, friability of mucosa in sigmoid colon and exudate on wall. |
|||
| DiseasesDB = 3178 |
|||
| |
| field = [[Gastroenterology]] |
||
| synonyms = Crohn disease, Crohn syndrome, granulomatous enteritis, regional enteritis, Leśniowski-Crohn disease |
|||
| ICD9 = {{ICD9|555}} |
|||
| symptoms = [[Diarrhea]], [[abdominal pain]], [[fatigue]], [[weight loss]], [[fever]]<ref name="pmid32242028"/> |
|||
| ICDO = |
|||
| complications = [[Anemia]], [[bowel cancer]], [[bowel obstruction]], [[strictures]], [[fistulas]], [[abscesses]], [[anal fissure]]<ref name="pmid32242028"/> |
|||
| OMIM = 266600 |
|||
| onset = 20–30 years<ref name="pmid28601423"/> |
|||
| MedlinePlus = 000249 |
|||
| duration = Lifelong<ref name="pmid32242028"/> |
|||
| eMedicineSubj = med |
|||
| causes = Uncertain<ref name="pmid32242028"/> |
|||
| eMedicineTopic = 477 |
|||
| risks = [[Genetic predisposition]], living in a [[developed country]], [[smoking]], [[diet (nutrition)|diet]],<ref name="pmid32242028"/> [[antibiotics]], [[oral contraceptives]], [[aspirin]], [[NSAIDS]]<ref name="pmid30611442"/> |
|||
| eMedicine_mult = {{eMedicine2|ped|507}} {{eMedicine2|radio|197}} |
|||
| diagnosis = [[Colonoscopy]], [[capsule endoscopy]], [[medical imaging]], [[histopathology]]<ref name="pmid32242028"/>| differential = [[Ulcerative colitis]], [[Behçet's disease]], [[intestinal lymphoma]], [[intestinal tuberculosis]], [[ischaemic colitis]], [[irritable bowel syndrome]]<ref name="pmid32242028"/> |
|||
| MeshID = D003424 |
|||
| prevention = |
|||
| treatment = |
|||
| medication = [[Biologics]] (especially [[TNF inhibitor|TNF blockers]]), [[immunosuppressants]] ([[thiopurine]]s and [[methotrexate]]), [[corticosteroid]]s,<ref name="pmid32242028"/> |
|||
| prognosis = Slightly reduced life expectancy<ref name="pmid33168761"/> |
|||
| frequency = ~300 in 100,000 ([[North America]] and [[Western Europe]])<ref name="pmid32242028"/> |
|||
| deaths = |
|||
| alt = |
|||
| named after = {{ubl|[[Burrill Bernard Crohn]]}} |
|||
}} |
}} |
||
'''Crohn's disease''' is a chronic [[inflammatory bowel disease]] characterized by recurrent episodes of intestinal inflammation, primarily manifesting as [[diarrhea]] and [[abdominal pain]]. Unlike [[ulcerative colitis]], inflammation can occur anywhere in the gastrointestinal tract, though it most frequently affects the [[ileum]] and [[large intestine|colon]], involving all layers of the intestinal wall. Symptoms may be non-specific and progress gradually, often delaying diagnosis. About one-third of patients have colonic disease, another third have ileocolic disease, and the remaining third have isolated ileal disease. Systemic symptoms such as chronic [[fatigue]], [[unintentional weight loss|weight loss]], and low-grade [[fever]]s are common. Organs such as the skin and joints can also be affected. Complications can include [[bowel obstruction]]s, [[fistula]]s, nutrition problems, and an increased risk of [[intestinal cancer]]s.<ref name="pmid32242028"/> |
|||
Crohn's disease is influenced by genetic, environmental, and immunological factors. [[Smoking]] is a major modifiable risk factor, especially in Western countries, where it doubles the likelihood of developing the disease. Dietary shifts from high-fiber to processed foods may reduce microbiota diversity and increase risk, while high-fiber diets can offer some protection. Genetic predisposition plays a significant role, with first-degree relatives facing a five-fold increased risk, particularly due to mutations in genes like [[NOD2]] that affect immune response. The condition results from a dysregulated immune response to gut bacteria and increased intestinal permeability, alongside changes in the [[gut microbiome]].<ref name="pmid32242028"/> |
|||
'''Crohn's disease''' (also known as '''Crohn-Leśniowski Disease''', '''morbus Leśniowski-Crohn''', '''[[granuloma]]tous [[colitis]]''' and '''regional enteritis''') is an inflammatory disease of the intestines that may affect any part of the [[gastrointestinal tract]] from [[anus]] to [[mouth]], causing a wide variety of [[symptom]]s. It primarily causes [[abdominal pain]], [[diarrhea]]<!-- PLEASE SEE WP:ENGVAR - DO NOT CHANGE THE SPELLING AS IT INTERFERES WITH LINKING AND IS INAPPROPRIATE --> (which may be bloody), [[vomiting]], or [[weight loss]],<ref name=Baumgart> |
|||
{{cite journal |
|||
| author = Baumgart DC, Sandborn WJ |
|||
| year = 2007 |
|||
| date= 12 May 2007 |
|||
| title = Inflammatory bowel disease: clinical aspects and established and evolving therapies. |
|||
| journal = The Lancet |
|||
| volume = 369 |
|||
| issue = 9573 |
|||
| pages = 1641–57 |
|||
| month = May |
|||
| pmid = 17499606 |
|||
| doi = 10.1016/S0140-6736(07)60751-X |
|||
| accessdate = 2009-11-04 |
|||
}}</ref><ref>[http://www.mayoclinic.com/health/crohns-disease/DS00104/DSECTION=symptoms Mayo Clinic: Crohn's Disease]</ref><ref>[http://digestive.niddk.nih.gov/ddiseases/pubs/crohns/ National Digestive Diseases Information Clearinghouse]</ref> but may also cause complications outside of the gastrointestinal tract such as [[skin rashes]], [[arthritis]] and [[uveitis|inflammation of the eye]].<ref name=Baumgart/> |
|||
Diagnosing Crohn's disease can be complex due to symptom overlap with other gastrointestinal disorders. It typically involves a combination of clinical history, physical examination, and various diagnostic tests. Key methods include [[colonoscopy|ileocolonoscopy]], which identifies the disease in about 90% of cases, and imaging techniques like [[Computed tomography enterography|CT]] and [[Magnetic resonance enterography|MRI enterography]], which help assess the extent of the disease and its complications. [[Histopathology|Histological examination]] of biopsy samples is the most reliable method for confirming diagnosis.<ref name="pmid32242028"/> |
|||
Crohn's disease is an [[autoimmune disease]], in which the body's [[immune system]] attacks the gastrointestinal tract, causing [[inflammation]]; it is classified as a type of [[inflammatory bowel disease]]. There has been evidence of a [[genetics|genetic]] link to Crohn's disease, putting individuals with siblings afflicted with the disease at higher risk.<ref name="genetic_link"> |
|||
{{cite journal |
|||
| last = Barrett |
|||
| first = Jeffrey C |
|||
| coauthors = Sarah Hansoul, Dan L Nicolae, Judy H Cho, Richard H Duerr, John D Rioux, Steven R Brant, Mark S Silverberg, Kent D Taylor, M Michael Barmada, Alain Bitton, Themistocles Dassopoulos, Lisa Wu Datta, Todd Green, Anne M Griffiths, Emily O Kistner, Michael T Murtha, Miguel D Regueiro, Jerome I Rotter, L Philip Schumm, A Hillary Steinhart, Stephan R Targan, Ramnik J Xavier, the NIDDK IBD Genetics Consortium, Cécile Libioulle, Cynthia Sandor, Mark Lathrop, Jacques Belaiche, Olivier Dewit, Ivo Gut, Simon Heath, Debby Laukens, Myriam Mni, Paul Rutgeerts, André Van Gossum, Diana Zelenika, Denis Franchimont, Jean-Pierre Hugot, Martine de Vos, Severine Vermeire, Edouard Louis, the Belgian-French IBD Consortium, the Wellcome Trust Case Control Consortium, Lon R Cardon, Carl A Anderson, Hazel Drummond, Elaine Nimmo, Tariq Ahmad, Natalie J Prescott, Clive M Onnie, Sheila A Fisher, Jonathan Marchini, Jilur Ghori, Suzannah Bumpstead, Rhian Gwilliam, Mark Tremelling, Panos Deloukas, John Mansfield, Derek Jewell, Jack Satsangi, Christopher G Mathew, Miles Parkes, Michel Georges, Mark J Daly |
|||
| year = 2008 |
|||
| month = August |
|||
| title = Genome-wide association defines more than 30 distinct susceptibility loci for Crohn's disease |
|||
| journal = Nature Genetics |
|||
| volume = 40 |
|||
| issue = 8 |
|||
| pages = 955–962 |
|||
| doi = 10.1038/ng.175 |
|||
| pmid = 18587394 |
|||
| last1 = Barrett |
|||
| first1 = JC |
|||
| last2 = Hansoul |
|||
| first2 = S |
|||
| last3 = Nicolae |
|||
| first3 = DL |
|||
| last4 = Cho |
|||
| first4 = JH |
|||
| last5 = Duerr |
|||
| first5 = RH |
|||
| last6 = Rioux |
|||
| first6 = JD |
|||
| last7 = Brant |
|||
| first7 = SR |
|||
| last8 = Silverberg |
|||
| first8 = MS |
|||
| last9 = Taylor |
|||
| first9 = KD |
|||
| pmc = 2574810 |
|||
| accessdate = 2009-11-04 |
|||
}}</ref> It is understood to have a large environmental component as evidenced by the higher number of cases in western industrialized nations. Males and females are equally affected. Smokers are three times more likely to develop Crohn's disease.<ref name=Cosnes2004> |
|||
{{cite journal |
|||
| author = Cosnes J |
|||
| title = Tobacco and IBD: relevance in the understanding of disease mechanisms and clinical practice |
|||
| journal = Best Pract Res Clin Gastroenterol |
|||
| volume = 18 |
|||
| issue = 3 |
|||
| pages = 481–96 |
|||
| year = 2004 |
|||
| month = June |
|||
| pmid = 15157822 |
|||
| doi = 10.1016/j.bpg.2003.12.003 |
|||
| accessdate = 2009-11-04 |
|||
}}</ref> Crohn's disease affects between 400,000 and 600,000 people in North America.<ref name=Loftus>{{cite journal | last = Loftus | first = E.V. | coauthors = P. Schoenfeld, W. J. Sandborn | year = 2002 | month = January | title = The epidemiology and natural history of Crohn's disease in population-based patient cohorts from North America: a systematic review | journal = Alimentary Pharmacology & Therapeutics | volume = 16 | issue = 1 | pages = 51–60 | doi =10.1046/j.1365-2036.2002.01140.x | pmid = 11856078 | accessdate = 2009-11-04}}</ref> [[Prevalence]] estimates for Northern Europe have ranged from 27–48 per 100,000.<ref name=Bernstein> |
|||
{{cite journal |
|||
| last = Bernstein |
|||
| first = Charles N. |
|||
| title = The epidemiology of inflammatory bowel disease in Canada: a population-based study |
|||
| journal =The American Journal of Gastroenterology |
|||
| year = 2006 |
|||
| month = July |
|||
| volume = 101 |
|||
| issue = 7 |
|||
| pages = 1559–68 |
|||
| last2 = Wajda |
|||
| first2 = A |
|||
| last3 = Svenson |
|||
| first3 = LW |
|||
| last4 = Mackenzie |
|||
| first4 = A |
|||
| last5 = Koehoorn |
|||
| first5 = M |
|||
| last6 = Jackson |
|||
| first6 = M |
|||
| last7 = Fedorak |
|||
| first7 = R |
|||
| last8 = Israel |
|||
| first8 = D |
|||
| last9 = Blanchard |
|||
| first9 = JF |
|||
| pmid = 16863561 |
|||
| doi =10.1111/j.1572-0241.2006.00603.x |
|||
| accessdate = 2009-11-04 |
|||
| author2 = Wajda |
|||
| author3 = Svenson |
|||
| author4 = MacKenzie |
|||
| author5 = Koehoorn |
|||
| author6 = Jackson |
|||
| author7 = Fedorak |
|||
| author8 = Israel |
|||
| author9 = Blanchard |
|||
}}</ref> Crohn's disease tends to present initially in the teens and twenties, with another peak incidence in the fifties to seventies, although the disease can occur at any age.<ref name=Baumgart/><ref name = emed/> |
|||
Management of Crohn's disease is individualized, focusing on disease severity and location to achieve mucosal healing and improve long-term outcomes. Treatment may include [[corticosteroids]] for quick symptom relief, [[immunosuppressants]] for maintaining remission, and [[biologics]] like [[TNF inhibitors|anti-TNF therapies]], which are effective for both induction and maintenance. [[Bowel resection|Surgery]] may be necessary for complications such as blockages. Despite ongoing treatment, Crohn's disease is a chronic condition with no cure, often leading to a higher risk of related health issues and reduced life expectancy.<ref name="pmid32242028"/> |
|||
There is no known [[Medication|pharmaceutical]] or [[surgery|surgical]] cure for Crohn's disease.<ref> |
|||
{{cite web |
|||
|first= Tri H |
|||
|last= Le |
|||
|publisher=eMedicine |
|||
|title=Ulcerative colitis |
|||
|url=emedicine.medscape.com/article/183084-overview |
|||
| date=Aug 7, 2008 |
|||
| accessdate = 2009-11-04 |
|||
}}</ref> [[Treatment of Crohn's disease|Treatment options]] are restricted to controlling [[symptom]]s, maintaining [[remission (medicine)|remission]] and preventing [[relapse]]. |
|||
The disease is most prevalent in [[North America]] and [[Western Europe]], particularly among [[Ashkenazi Jews]], with prevalence rates of 322 per 100,000 in [[Germany]], 319 in [[Canada]],<ref name="pmid32242028"/> and 300 in the [[United States]].<ref name="pmid37223580"/> There is also a rising prevalence in newly industrialized countries, such as 18.6 per 100,000 in [[Hong Kong]] and 3.9 in [[Taiwan]]. The typical age of onset is between 20 and 30 years, with an increasing number of cases among children.<ref name="pmid32242028"/> |
|||
The disease was named for American [[gastroenterology|gastroenterologist]] [[Burrill Bernard Crohn]], who in 1932, along with two colleagues, described a series of patients with inflammation of the [[terminal ileum]], the area most commonly affected by the illness.<ref name=CrohnBB>{{cite journal |author=Crohn BB, Ginzburg L, Oppenheimer GD |title=Regional ileitis: a pathologic and clinical entity. 1932 |journal=Mt. Sinai J. Med. |volume=67 |issue=3 |pages=263–8 |year=2000 |pmid=10828911 |doi=}}</ref> For this reason, the disease has also been called '''regional ileitis'''<ref name="CrohnBB"/> or regional enteritis. The condition, however, has been independently identified by others in the literature prior, most notably in 1904 by Polish surgeon [[Antoni Leśniowski]] for whom the condition is additionally named (Leśniowski-Crohn's disease) in the Polish literature. |
|||
== Signs and symptoms == |
|||
==Classification== |
|||
[[Image: |
[[Image:Patterns of CD.jpg|right|thumb|alt=Diagram of the three most common sites of intestinal involvement in Crohn's disease.|The three most common sites of intestinal involvement in Crohn's disease are ileal, ileocolic and colonic.<ref name="pmid32242028"/>]] |
||
Crohn's disease is one type of inflammatory bowel disease (IBD). It invariably affects the gastrointestinal tract, and most gastroenterologists categorize the presenting disease by the affected areas. ''[[Ileocolic]] Crohn's disease'', which affects both the [[ileum]] (the last part of the [[small intestine]] that connects to the [[large intestine]]) and the large intestine, accounts for fifty percent of cases. ''Crohn's ileitis'', affecting the ileum only, accounts for thirty percent of cases, and ''Crohn's colitis'', affecting the large intestine, accounts for the remaining twenty percent of cases and may be particularly difficult to distinguish from [[ulcerative colitis]]. The disease can attack any part of the digestive tract, from mouth to anus. However, individuals affected by the disease rarely fall outside these three classifications, being affected in other parts of the gastrointestinal tract such as the [[stomach]] and [[esophagus]].<ref name=Baumgart/> |
|||
Crohn's disease is characterized by recurring flares of intestinal inflammation, with diarrhea and abdominal pain as the primary symptoms. Symptoms may be non-specific and progress gradually, and many people have symptoms for years before diagnosis. Unlike [[ulcerative colitis]], inflammation can occur anywhere in the gastrointestinal tract, most often in the [[ileum]] and [[Large intestine|colon]], and can involve all layers of the intestine. Disease location tends to be stable, with a third of patients having colonic disease, a third having ileocolic disease, and a third having ileal disease. The disease may also involve perianal, upper gastrointestinal, and extraintestinal organs.<ref name="pmid32242028"/> |
|||
Crohn's disease may also be categorized by the behavior of disease as it progresses. This was formalized in the Vienna classification of Crohn's disease.<ref name=Vienna>{{cite journal | author = Gasche C, Scholmerich J, Brynskov J, D'Haens G, Hanauer S, Irvine E, Jewell D, Rachmilewitz D, Sachar D, Sandborn W, Sutherland L | title = A simple classification of Crohn's disease: report of the Working Party for the World Congresses of Gastroenterology, Vienna 1998 | journal = Inflamm Bowel Dis | volume = 6 | issue = 1 | pages = 8–15 | year = 2000 | pmid = 10701144}}</ref> There are three categories of disease presentation in Crohn's disease: stricturing, penetrating, and [[inflammatory]]. ''Stricturing disease'' causes narrowing of the bowel which may lead to [[bowel obstruction]] or changes in the caliber of the [[feces]]. ''Penetrating disease'' creates abnormal passageways ([[fistula]]e) between the bowel and other structures such as the skin. ''[[Inflammatory disease]]'' (or non-stricturing, non-penetrating disease) causes inflammation without causing strictures or fistulae.<ref name=Vienna/><ref name=phenotypes>{{cite journal | author = Dubinsky MC, Fleshner PP. | title = Treatment of Crohn's Disease of Inflammatory, Stenotic, and Fistulizing Phenotypes | journal = Curr Treat Options Gastroenterol | volume = 6 | issue = 3 | pages = 183–200 | year = 2003 | pmid = 12744819 | doi = 10.1007/s11938-003-0001-1}}</ref> |
|||
=== Gastrointestinal === |
|||
==Symptoms== |
|||
* [[Diarrhea]] affects 82% of people at the onset of Crohn's disease, with severity ranging from mild to severe enough to require substitution of water and electrolytes. With Crohn's disease, diarrhea is frequent and urgent rather than voluminous.<ref name="pmid22917170">{{cite journal | vauthors = Wenzl HH | title = Diarrhea in chronic inflammatory bowel diseases | journal = Gastroenterology Clinics of North America | volume = 41 | issue = 3 | pages = 651–675 | pmid = 22917170 | date = September 2012 | doi = 10.1016/j.gtc.2012.06.006 | doi-access = free }}</ref> |
|||
[[Image:CD serpiginous ulcer.jpg|right|thumb|Endoscopy image of [[colon (anatomy)|colon]] showing [[serpiginous]] ulcer, a classic finding in Crohn's disease]] |
|||
* [[Abdominal pain]] affects at least 70% of people during the course of Crohn's disease. It can result directly from intestinal inflammation, or from complications such as strictures and fistulas.<ref name="pmid37867930">{{cite journal | vauthors = Coates MD, Clarke K, Williams E, Jeganathan N, Yadav S, Giampetro D, Gordin V, Smith S, Vrana K, Bobb A, Gazzio TT, Tressler H, Dalessio S | title = Abdominal Pain in Inflammatory Bowel Disease: An Evidence-Based, Multidisciplinary Review | journal = Crohns Colitis 360 | volume = 5 | issue = 4 | pmid = 37867930 | date = September 2023 | pages = otad055 | doi = 10.1093/crocol/otad055 | doi-access = free | pmc = 10588456 }}</ref> Pain most commonly occurs in the lower right abdomen.<ref name="ustekinumab">{{cite web |title=What I need to know about Crohn's Disease |url=http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/crohns-disease/Pages/ez.aspx#symptoms |website=www.niddk.nih.gov|access-date=December 11, 2015 |url-status=dead |archive-url = https://web.archive.org/web/20151121213407/http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/crohns-disease/Pages/ez.aspx#symptoms|archive-date=November 21, 2015}}</ref> |
|||
Many people with Crohn's disease have symptoms for years prior to the diagnosis.<ref name=Pimentel>{{cite journal | last = Pimentel | first = Mark | coauthors = Michael Chang, Evelyn J. Chow, Siamak Tabibzadeh, Viorelia Kirit-Kiriak, Stephan R. Targan, Henry C. Lin | year = 2000 | title = Identification of a prodromal period in Crohn's disease but not ulcerative colitis | journal = American Journal of Gastroenterology | volume = 95 | issue = 12 | pages = 3458–62 | doi =10.1111/j.1572-0241.2000.03361.x | pmid = 11151877 }}</ref> The usual onset is between 15 and 30 years of age but can occur at any age.<ref>[http://www.emedicinehealth.com/crohn_disease/article_em.htm Crohn's Disease Overview]</ref> Because of the 'patchy' nature of the gastrointestinal disease and the depth of tissue involvement, initial symptoms can be more vague than with ulcerative colitis. People with Crohn's disease will go through periods of flare-ups and remission. |
|||
* [[Rectal bleeding]] is less common than in ulcerative colitis, and is more likely to occur with inflammation in the colon or rectum. Bleeding in the colon or rectum is bright red, whereas bleeding in higher segments causes dark or black stools.<ref name="CrohnsColitisCA">{{cite web | url = https://crohnsandcolitis.ca/About-Crohn-s-Colitis/IBD-Journey/Symptom-Management/Bleeding-and-Blood-in-the-Stool | title = Bleeding and Blood in the Stool | website = crohn's and colitis | access-date = 16 October 2024}}</ref> |
|||
* [[Bloating]], [[flatus]], and other symptoms of [[irritable bowel syndrome]] occur in 41% of people in remission.<ref name="pmid31496621">{{cite journal | vauthors = Barros LL, Farias AQ, Rezaie A | title = Gastrointestinal motility and absorptive disorders in patients with inflammatory bowel diseases: Prevalence, diagnosis and treatment | journal = World Journal of Gastroenterology | volume = 25 | issue = 31 | pages = 4414–4426 | pmid = 31496621 | pmc = 6710178 | date = August 2019 | doi = 10.3748/wjg.v25.i31.4414 | doi-access = free }}</ref> |
|||
* Perianal involvement occurs in 18–43% of cases, more frequently if the colon and rectum are inflamed, and can cause [[anal fistula|fistulas]], [[skin tags]], [[hemorrhoids]], [[anal fissure|fissures]], [[ulcers]], and [[anal stricture|strictures]].<ref name="pmid31507348">{{cite journal | vauthors = Pogacnik JS, Salgado G | title = Perianal Crohn's Disease | journal = Clinics in Colon and Rectal Surgery | volume = 32 | issue = 5 | pages = 377–385 | pmid = 31507348 | date = September 2019 | doi = 10.1055/s-0039-1687834 | doi-access = free | pmc = 6731113 }}</ref> |
|||
* Upper gastrointestinal involvement is rare, occurring in 0.5-16% of cases, and may cause symptoms such as [[odynophagia|pain while swallowing]], [[dysphagia|difficulty swallowing]], [[vomiting]], and [[nausea]].<ref name="pmid28708248">{{Cite journal |last1=Laube |first1=Robyn |last2=Liu |first2=Ken |last3=Schifter |first3=Mark |last4=Yang |first4=Jessica L |last5=Suen |first5=Michael K |last6=Leong |first6=Rupert W |date=February 2018 |title=Oral and upper gastrointestinal Crohn's disease |url=https://onlinelibrary.wiley.com/doi/10.1111/jgh.13866 |journal=Journal of Gastroenterology and Hepatology |language=en |volume=33 |issue=2 |pages=355–364 |doi=10.1111/jgh.13866 |pmid=28708248 |issn=0815-9319}}</ref> |
|||
=== |
=== Systemic === |
||
Crohn's disease often presents with systemic symptoms, including: |
|||
* [[Fatigue#Chronic|Chronic fatigue]], which lasts for at least 6 months and cannot be cured by rest, occurs in 80% of people with Crohn's disease, including 30% of people who are in remission.<ref name="pmid37629549">{{cite journal | vauthors = Włodarczyk M, Makaro A, Prusisz M, Włodarczyk J, Nowocień M, Maryńczak K, Fichna J, Dziki Ł | title = The Role of Chronic Fatigue in Patients with Crohn's Disease | journal = Life (Basel) | volume = 13 | issue = 8 | pages = 1692 | pmid = 37629549 | date = August 2023 | doi = 10.3390/life13081692 | doi-access = free | pmc = 10455565 | bibcode = 2023Life...13.1692W }}</ref> |
|||
* [[Fevers]], typically low-grade, are often reported as initial symptoms of Crohn's disease. High-grade fevers are often a result of abscesses.<ref name="StatPearls">{{cite web |title=Crohn Disease |date=2024 |url=https://www.ncbi.nlm.nih.gov/books/NBK436021/| access-date=18 October 2024 | publisher=StatPearls Publishing |pmid=28613792 | vauthors = Ranasinghe IR, Tian C, Hsu R }}</ref> |
|||
* [[Unintentional weight loss|Weight loss]] often occurs due to diarrhea and reduced appetite.<ref name="StatPearls"/> |
|||
=== Extraintestinal === |
|||
Abdominal pain may be the initial symptom of Crohn's disease. It is often accompanied by diarrhea, especially in those who have had surgery. The diarrhea may or may not be bloody. People who have had surgery or multiple surgeries often end up with [[short bowel syndrome]] of the gastrointestinal tract. The nature of the diarrhea in Crohn's disease depends on the part of the small intestine or colon that is involved. Ileitis typically results in large-volume watery feces. Colitis may result in a smaller volume of feces of higher frequency. Fecal consistency may range from solid to watery. In severe cases, an individual may have more than 20 [[bowel movements]] per day and may need to awaken at night to defecate.<ref name=Baumgart/><ref name=emed/><ref name=Podolsky/><ref>{{cite journal | last = Mueller | first = M. H. | coauthors = M. E. Kreis, M. L. Gross, H. D. Becker, T. T. Zittel & E. C. Jehle | year = 2002 | title = Anorectal functional disorders in the absence of anorectal inflammation in patients with Crohn's disease | journal = British Journal of Surgery | volume = 89 | issue = 8 | pages = 1027–31 | doi =10.1046/j.1365-2168.2002.02173.x | pmid = 12153630 }}</ref> Visible bleeding in the feces is less common in Crohn's disease than in ulcerative colitis, but may be seen in the setting of Crohn's colitis.<ref name=Baumgart/> Bloody bowel movements are typically intermittent, and may be bright or dark red in colour. In the setting of severe Crohn's colitis, bleeding may be copious.<ref name=emed/> [[Flatulence]] and bloating may also add to the intestinal discomfort.<ref name=emed/> |
|||
Extraintestinal manifestations occur in 21–47% of cases, and include symptoms such as:<ref name="pmid32242028"/> |
|||
* Mouth ulcers, such as [[canker sores]].<ref name="pmid33477990">{{cite journal |vauthors=Antonelli E, Bassotti G, Tramontana M, Hansel K, Stingeni L, Ardizzone S, Genovese G, Marzano AV, Maconi G |title=Dermatological Manifestations in Inflammatory Bowel Diseases |journal=J Clin Med |volume=10 |issue=2 |date=January 2021 |page=364 |pmid=33477990 |pmc=7835974 |doi=10.3390/jcm10020364 | doi-access = free}}</ref> |
|||
* Eye inflammation, such as [[uveitis]], [[scleritis]], and [[episcleritis]].<ref name="pmid32242028"/> |
|||
* Skin inflammation, such as [[erythema nodosum]] and [[pyoderma gangrenosum]].<ref name="pmid32242028"/> |
|||
* Blood conditions such as [[portal hypertension]], [[thromboembolism]], [[thrombosis]], [[pulmonary embolism]].<ref name="pmid32242028"/> |
|||
* Joint inflammation such as [[arthritis]], [[ankylosing spondylitis]], [[sacroiliitis]].<ref name="pmid32242028"/> |
|||
* Respiratory conditions such as [[obstructive sleep apnea]] and [[chest infections]].<ref name="pmid32242028"/> |
|||
* Liver, bile duct, and gallbladder conditions such as [[primary sclerosing cholangitis]] and [[cirrhosis]].<ref name="pmid32242028"/> |
|||
* Mental disorders such as [[Major depressive disorder|depression]] and [[Anxiety disorder|anxiety]].<ref name="pmid35732730">{{cite journal | vauthors = Bisgaard TH, Allin KH, Keefer L, Ananthakrishnan AN, Jess T | title = Depression and anxiety in inflammatory bowel disease: epidemiology, mechanisms and treatment | journal = Nature Reviews Gastroenterology & Hepatology | volume = 19 | issue = 11 | pages = 717–726 | pmid = 35732730 | date = March 2023 | doi = 10.1038/s41575-022-00634-6 | doi-access = free }}</ref> |
|||
* [[Metabolic bone disease]].<ref name="pmid32242028"/> |
|||
=== Complications === |
|||
Symptoms caused by [[bowel obstruction|intestinal stenosis]] are also common in Crohn's disease. Abdominal pain is often most severe in areas of the bowel with stenoses. In the setting of severe stenosis, vomiting and nausea may indicate the beginnings of small bowel obstruction.<ref name=emed> |
|||
[[Image:Colorectal cancer endo 2.jpg|right|thumb| alt=Image of colon cancer identified during a colonoscopy in Crohn's disease.|Image of colon cancer identified in the sigmoid colon of a person with Crohn's disease during a colonoscopy.]] |
|||
{{cite web |
|||
| first= George Y |
|||
| last= Wu |
|||
| coauthors=Marcy L Coash, Senthil Nachimuthu |
|||
| publisher=eMedicine |
|||
| title=Crohn Disease |
|||
| url=emedicine.medscape.com/article/172940-overview |
|||
| date=Jan 20, 2009 |
|||
| accessdate = 2009-11-04 |
|||
}}</ref> Crohn's disease may also be associated with [[primary sclerosing cholangitis]], a type of inflammation of the bile ducts.<ref>{{cite book|last=Kumar|first=Vinay|coauthors=Abul K. Abbas, Nelson Fausto|title=Robbins and Cotran: Pathologic Basis of Disease|publisher=Elsevier Saunders |location=Philadelphia, Pennsylvania|date=July 30, 2004|edition=7th|pages=847|chapter=Ch 17: The Gastrointestinal Tract|isbn=0-7216-0187-1}}</ref> |
|||
Bowel damage due to inflammation occurs in half of cases within 10 years of diagnosis, and can lead to stricturing or penetrating disease forms. This can cause complications such as: |
|||
Perianal discomfort may also be prominent in Crohn's disease. Itchiness or pain around the [[anus]] may be suggestive of inflammation, [[fistula|fistulization]] or [[abscess]] around the anal area<ref name=Baumgart/> or [[anal fissure]]. Perianal skin [[acrochordon|tags]] are also common in Crohn's disease.<ref>{{cite journal | author = Taylor B, Williams G, Hughes L, Rhodes J | title = The histology of anal skin tags in Crohn's disease: an aid to confirmation of the diagnosis | journal = Int J Colorectal Dis | volume = 4 | issue = 3 | pages = 197–9 | year = 1989 | pmid = 2769004 | doi = 10.1007/BF01649703}}</ref> [[Fecal incontinence]] may accompany peri-anal Crohn's disease. At the opposite end of the gastrointestinal tract, the mouth may be affected by non-healing sores ([[aphthous ulcer]]s). Rarely, the [[esophagus]], and [[stomach]] may be involved in Crohn's disease. These can cause symptoms including difficulty swallowing ([[dysphagia]]), upper abdominal pain, and vomiting.<ref>{{cite journal | last = Fix | first = Oren K. | coauthors = Jorge A. Soto, Charles W. Andrews and Francis A. Farraye | year = 2004 | title = Gastroduodenal Crohn's disease | journal = Gastrointestinel Endoscopy | volume = 60 | issue = 6 | pages = 985 | doi = 10.1016/S0016-5107(04)02200-X | pmid = 15605018 }}</ref> |
|||
* [[Bowel obstruction]]s may occur due to strictures, particularly in the small intestine, and may require surgical removal of the affected segment ([[bowel resection]]) or surgical dilation ([[stricturoplasty]]).<ref name="pmid28601423"/> |
|||
* [[Fistulas]], openings in the gut, result from penetrating disease and can cause diarrhea, [[urinary tract infections]], and stool leakage to the vagina or skin. It is treated by bowel resection or [[fistulotomy]]<ref name="pmid28601423"/> |
|||
* [[Abscesses]], infected pockets, can also result from penetrating disease, causing abdominal pain, fever, and chills. It may be treated by [[Incision and drainage|surgical drainage]].<ref name="pmid28601423">{{cite journal | vauthors = Feuerstein JD, Cheifetz AS | title = Crohn Disease: Epidemiology, Diagnosis, and Management | journal = Mayo Clinic Proceedings | volume = 92 | issue = 7 | pages = 1088–1103 | pmid = 28601423 | date = June 2017 | doi = 10.1016/j.mayocp.2017.04.010 | doi-access = free }}</ref> |
|||
Malnutrition occurs in 38.9% of people in remission and 82.8% of people with active disease due to malabsorption in the small intestine, reduced appetite, and drug interactions.<ref name="pmid37111210"/> This can cause complications such as: |
|||
===Systemic symptoms=== |
|||
* [[Anemia]] occurs in 6–74% of cases as a result of [[iron deficiency]] and blood loss. It is treated by [[oral iron]] or [[intravenous iron]] depending on disease activity.<ref name="pmid37111210"/> |
|||
Crohn's disease, like many other chronic, inflammatory diseases, can cause a variety of [[B symptoms|systemic symptoms]].<ref name=Baumgart/> Among children, [[growth failure]] is common. In addition to these complications, Acute Myelogenous leukemia as well as Lymphoma are two common system cancer that can occur at any age. AML being a cancer of the blood (Myeloid) as well as cancer of the lymph nodes (Lymphoma). Many children are first diagnosed with Crohn's disease based on [[failure to thrive|inability to maintain growth]].<ref name=Beattie/> As Crohn's disease may manifest at the time of the growth spurt in [[puberty]], up to 30% of children with Crohn's disease may have retardation of growth.<ref>{{cite journal | last = Büller | first = H.A. | year = 1997 | title = Problems in diagnosis of IBD in children | journal = The Netherlands Journal of Medicine | volume = 50 | issue = 2 | pages = S8–S11 | doi =10.1016/S0300-2977(96)00064-2 | pmid = 9050326 }}</ref> Fever may also be present, though fevers greater than 38.5 [[Celsius|˚C]] (101.3 [[Fahrenheit|˚F]]) are uncommon unless there is a complication such as an [[abscess]].<ref name=Baumgart/> Among older individuals, Crohn's disease may manifest as weight loss. This is usually related to decreased food intake, since individuals with intestinal symptoms from Crohn's disease often feel better when they do not eat and might lose their appetite.<ref name=Beattie>{{cite journal | last = Beattie | first = R.M. | coauthors = N. M. Croft, J. M. Fell, N. A. Afzal and R. B. Heuschkel | year = 2006 | title = Inflammatory bowel disease | journal = Archives of Disease in Childhood | volume = 91 | issue = 5 | pages = 426–32 | doi =10.1136/adc.2005.080481 | pmid = 16632672 | pmc = 2082730 }}</ref> People with extensive [[small intestine]] disease may also have [[malabsorption]] of [[carbohydrate]]s or [[lipid]]s, which can further exacerbate weight loss.<ref>{{cite journal | last = O'Keefe | first = S. J. | year = 1996 | title = Nutrition and gastrointestinal disease | journal = Scandinavian Journal of Gastroenterology Supplement | issue = 220 | pages = 52–9 | pmid = 8898436 | doi = 10.3109/00365529609094750 | volume = 31 }}</ref> |
|||
* [[Vitamin D deficiency]] is prevalent and can cause [[osteoporosis]], and is treated by oral supplementation.<ref name="pmid37111210"/> |
|||
* [[Folate deficiency|Folic acid]], [[Vitamin B12 deficiency|vitamin B12]], [[Zinc deficiency|zinc]], [[Magnesium deficiency|magnesium]], and [[Selenium deficiency|selenium]] deficiencies may also occur, and are treated through oral supplementation.<ref name="pmid37111210">{{cite journal | vauthors = Jabłońska B, Mrowiec S | title = Nutritional Status and Its Detection in Patients with Inflammatory Bowel Diseases | journal = Nutrients | volume = 15 | issue = 8 | pages = 1991 | pmid = 37111210 | pmc = 10143611 | date = April 2023 | doi = 10.3390/nu15081991 | doi-access = free }}</ref> |
|||
* [[Stunted growth|Impaired growth]] and nutritional deficiency occur in 65–85% of children with Crohn's disease.<ref name="pmid25309059">{{cite journal | vauthors = Gasparetto M, Guariso G | title = Crohn's disease and growth deficiency in children and adolescents | journal = World Journal of Gastroenterology | volume = 20 | issue = 37 | pages = 13219–13233 | pmid = 25309059 | pmc = 4188880 | date = October 2014 | doi = 10.3748/wjg.v20.i37.13219 | doi-access = free }}</ref> |
|||
Intestinal cancers may develop as a result of prolonged or severe inflammation.<ref name="pmid37627182"/> This includes: |
|||
===Extraintestinal symptoms=== |
|||
* [[Colorectal cancer]] has a prevalence of 7% at 30 years after diagnosis and accounts for 15% of deaths in people with Crohn's. Risk is higher if the disease occurs in most of the colon. Endoscopic surveillance is performed to detect and remove polyps, while surgery is required for dysplasia beyond the mucosal surface.<ref name="pmid37627182">{{cite journal | vauthors = Sato Y, Tsujinaka S, Miura T, Kitamura Y, Suzuki H, Shibata C | title = Inflammatory Bowel Disease and Colorectal Cancer: Epidemiology, Etiology, Surveillance, and Management | journal = Cancers (Basel) | volume = 15 | issue = 16 | pages = 4154 | pmid = 37627182 | pmc = 10452690 | date = August 2023 | doi = 10.3390/cancers15164154 | doi-access = free }}</ref> |
|||
[[Image:Crohnie sores 4.JPG|thumb|[[Erythema nodosum]] on the back of a person with Crohn's disease.]] |
|||
* [[Small bowel cancer]] has a prevalence of 1.6%, at least 12-times greater in people with Crohn's disease. Unlike colorectal cancer, endoscopic surveillance is ineffective and not recommended for small bowel cancer.<ref name="pmid38188070">{{cite journal | vauthors = Bhatt H, Mathis KL | title = Small Bowel Carcinoma in the Setting of Inflammatory Bowel Disease | journal = Clinics in Colon and Rectal Surgery | volume = 37 | issue = 1 | pages = 46–52 | pmid = 38188070 | pmc = 10769580 | date = March 2023 | doi = 10.1055/s-0043-1762929 | doi-access = free }}</ref> |
|||
[[Image:Crohnie Pyoderma gangrenosum.jpg|thumb|[[Pyoderma gangrenosum]] on the leg of a person with Crohn's disease.]] |
|||
== Causes == |
|||
In addition to systemic and gastrointestinal involvement, Crohn's disease can affect many other organ systems.<ref name=Danese>{{cite journal | last = Danese | first = Silvio | coauthors = Stefano Semeraro, Alfredo Papa, Italia Roberto, Franco Scaldaferri, Giuseppe Fedeli, Giovanni Gasbarrini, Antonio Gasbarrini | year = 2005 | title = Extraintestinal manifestations in inflammatory bowel disease | journal = World Journal of Gastroenterology | volume = 11 | issue = 46 | pages = 7227–36 | pmid = 16437620 | url = http://www.wjgnet.com/1007-9327/11/7227.asp | accessdate = 2009-11-07 }}</ref> Inflammation of the interior portion of the eye, known as [[uveitis]], can cause eye pain, especially when exposed to light ([[photophobia]]). Inflammation may also involve the white part of the eye ([[sclera]]), a condition called [[Scleritis|episcleritis]]. Both episcleritis and uveitis can lead to loss of vision if untreated. |
|||
=== Risk factors === |
|||
Smoking is a major modifiable risk factor for Crohn's disease, particularly in Western countries, where it doubles the risk. This risk is higher in females and varies with age. Smoking is also linked to earlier disease onset, increased need for immunosuppression, more surgeries, and higher recurrence rates. Ethnic differences have been noted, with studies in Japan linking passive smoking to the disease.<ref name="pmid32242028"/> Proposed mechanisms for smoking's effects include impaired [[autophagy]], direct toxicity to immune cells, and changes in the [[Gut microbiota|microbiome]].<ref name="pmid30611442"/> |
|||
Diet may influence the development of Crohn's disease by affecting the gut microbiome. The shift from high-fiber, low-fat foods to processed foods reduces microbiota diversity, increasing the risk of Crohn's disease.<ref name="pmid32242028"/> Conversely, high-fiber diets may reduce risk by up to 40%, likely due to the production of anti-inflammatory [[short-chain fatty acids]] from fiber metabolism by gut bacteria.<ref name="pmid30611442"/> The [[Mediterranean diet]] is also linked to a lower risk of later-onset Crohn's disease. Since diet's effect on the microbiome is temporary, its role in gut dysbiosis is controversial.<ref name="pmid32242028"/> |
|||
Crohn's disease is associated with a type of [[Rheumatology|rheumatologic disease]] known as [[spondyloarthropathy|seronegative spondyloarthropathy]]. This group of diseases is characterized by inflammation of one or more [[joint]]s ([[arthritis]]) or muscle insertions ([[enthesitis]]). The arthritis can affect larger joints such as the knee or shoulder or may exclusively involve the small joints of the hand and feet. The arthritis may also involve the spine, leading to [[ankylosing spondylitis]] if the entire spine is involved or simply [[sacroiliitis]] if only the lower spine is involved. The symptoms of arthritis include painful, warm, swollen, stiff [[Arthralgia|joints]] and loss of joint mobility or function. {{Citation needed|date=March 2009}} |
|||
Childhood antibiotic exposure is linked to a higher risk of Crohn's disease due to changes in the intestinal microbiome, which shapes the immune system in early life. Other medications, like [[oral contraceptives]], [[aspirin]], and [[NSAIDs]], may also increase risk by up to two-fold. Conversely, [[breastfeeding]] and [[statin]] use may reduce risk, though breastfeeding's effects are inconsistent. Early life factors such as mode of delivery, pet exposure, and infections—related to the [[hygiene hypothesis]]—also significantly influence risk, likely due to influences on the microbiome.<ref name="pmid30611442"/> |
|||
Crohn's disease may also involve the skin, blood, and [[endocrine system]]. One type of skin manifestation, [[erythema nodosum]], presents as red nodules usually appearing on the shins. Erythema nodosum is due to inflammation of the underlying subcutaneous tissue and is characterized by septal [[panniculitis]]. Another skin lesion, [[pyoderma gangrenosum]], is typically a painful ulcerating nodule. Crohn's disease also increases the risk of blood clots; painful swelling of the lower legs can be a sign of [[deep venous thrombosis]], while difficulty breathing may be a result of [[pulmonary embolism]]. [[Autoimmune hemolytic anemia]], a condition in which the immune system attacks the [[red blood cells]], is also more common in Crohn's disease and may cause fatigue, pallor, and other symptoms common in [[anemia]]. [[Clubbing]], a deformity of the ends of the fingers, may also be a result of Crohn's disease. Finally, Crohn's disease may cause [[osteoporosis]], or thinning of the bones. Individuals with osteoporosis are at increased risk of [[bone fracture]]s.<ref name=Bernstein>{{cite journal | last = Bernstein | first = Michael | coauthors = Sue Irwin and Gordon R. Greenberg | year = 2005 | title = Maintenance infliximab treatment is associated with improved bone mineral density in Crohn's disease | journal = The American Journal of Gastroenterology | volume = 100 | issue = 9 | pages = 2031–5. | doi =10.1111/j.1572-0241.2005.50219.x | pmid = 16128948 }}</ref> |
|||
=== Genetics === |
|||
Crohn's disease can also cause neurological complications (reportedly in up to 15% of patients).<ref name="pro">[http://professionals.epilepsy.com/page/inflammatory_crohn.html Crohn's disease]. professionals.epilepsy.com. Retrieved on July 13, 2007.</ref> The most common of these are [[seizures]], [[stroke]], [[myopathy]], [[peripheral neuropathy]], [[headache]] and [[Depression (mood)|depression]].<ref name="pro"/> |
|||
Genetics significantly influences the risk of Crohn's disease. First-degree relatives of affected individuals have a five-fold increased risk, while identical twins have a 38–50% risk if one twin is affected. [[Genome-wide association studies]] have identified around 200 loci linked to Crohn's, most found in non-coding regions that regulate gene expression and overlap with other immune-related conditions, such as [[ankylosing spondylitis]] and [[psoriasis]].<ref name="pmid30611442"/> While genetics can predict disease location, it does not determine complications like stricturing. A substantial portion of inherited risk is attributed to a few key polymorphisms.<ref name="pmid32242028"/> |
|||
* [[NOD2]] mutations are the primary genetic risk factor for ileal Crohn's disease, impairing the function of immune cells, particularly [[Paneth cells]]. These mutations are found in 10–27% of individuals with Crohn's disease, predominantly in Caucasian populations. Heterozygotes (one mutated copy) have a three-fold risk, while homozygotes (two copies) have a 20–40 fold risk.<ref name="pmid38582044">{{cite journal | vauthors = Kayali S, Fantasia S, Gaiani F, Cavallaro LG, de'Angelis GL, Laghi L | title = NOD2 and Crohn's Disease Clinical Practice: From Epidemiology to Diagnosis and Therapy, Rewired | journal = Inflammatory Bowel Diseases | pmid = 38582044 | date = April 2024 | doi = 10.1093/ibd/izae075 | doi-access = free }}</ref> |
|||
Crohn's patients often also have issues with [[small bowel bacterial overgrowth syndrome]], which has similar symptoms.<ref>{{MedlinePlus|000222|Small bowel bacterial overgrowth}}</ref> |
|||
* [[ATG16L1]] mutations impair autophagy and immune defense, and are more common in Caucasians.<ref name="pmid32242028"/> |
|||
* [[IL23R]] mutations increase inflammatory signaling of the [[interleukin-23]] pathway, and are more common in Caucasians.<ref name="pmid32242028"/> |
|||
* [[TNFSF15]] mutations are the primary genetic risk factor in Asian populations.<ref name="pmid32242028"/> |
|||
* [[IL10RA]] mutations impair the anti-inflammatory signaling of [[interleukin-10]], causing early-onset Crohn's disease with high [[penetrance]]. |
|||
== |
== Mechanism == |
||
[[File:Crohn's Disease Mechanism.png|thumb|upright=2|alt=diagram of mechanism of Crohn's disease|The intestinal barrier and immune system in health and during Crohn's disease. In health, immune cells secrete TGFβ and retinoic acid to promote the differentiation of Tregs, which regulate the inflammatory behavior of effector T cells.<ref name="pmid27590281">{{cite journal | vauthors = Plitas G, Rudensky AY | title = Regulatory T Cells: Differentiation and Function | journal = Cancer Immunology Research | volume = 4 | issue = 9 | pages = 721–725 | pmid = 27590281 | date = September 2016 | doi = 10.1158/2326-6066.CIR-16-0193 | doi-access = free | pmc = 5026325 }}</ref> During Crohn's disease, microbiome alterations, intestinal barrier permeability, and deficient innate immunity enable pathogens to enter the gut tissue. This causes antigen-presenting cells to upregulate IL-12, IL-18, and IL-23, increasing the differentiation of Th1 and Th17 cells. These cells secrete inflammatory cytokines such as IL-17, IFNγ, and TNF to perpetuate inflammation.<ref name="pmid30611442"/>]] |
|||
[[Image:Colorectal cancer endo 2.jpg|right|thumb|[[Colonoscopy|Endoscopic]] image of '''colon cancer''' identified in the sigmoid colon on screening [[colonoscopy]] for Crohn's disease.]] |
|||
Crohn's disease can lead to several mechanical complications within the intestines, including [[obstruction]], fistulae, and abscesses. Obstruction typically occurs from [[strictures]] or [[adhesions]] which narrow the lumen, blocking the passage of the intestinal contents. Fistulae can develop between two loops of bowel, between the bowel and bladder, between the bowel and vagina, and between the bowel and skin. Abscesses are walled off collections of [[infection]], which can occur in the [[abdomen]] or in the [[wiktionary:perianal|perianal]] area in Crohn's disease sufferers. |
|||
Crohn's disease is believed to be caused by a dysregulated immune response to gut bacteria, though the exact mechanism is unknown. This is evidenced by the disease's links to genes involved in bacteria defense and its occurrence in the [[ileum]] and [[Large intestine|colon]], the most bacteria-dense segments of the intestine.<ref name="pmid25234148">{{cite journal | vauthors = Mowat AM, Agace WW | title = Regional specialization within the intestinal immune system | journal = Nature Reviews Immunology | volume = 14 | issue = 10 | pages = 667–85 | pmid = 25234148 | date = October 2014 | doi = 10.1038/nri3738 | doi-access = free }}</ref> In Crohn's disease, a permeable intestinal barrier and a deficient [[innate immune response]] enable bacteria to enter intestinal tissue, causing an excessive inflammatory response from [[T helper 1]] (Th1) and [[T helper 17]] (Th17) cells. An altered [[microbiome]] may also be causatory and serve as the link to environmental factors.<ref name="pmid30611442">{{cite journal | vauthors = Ramos GP, Papadakis KA | title = Mechanisms of Disease: Inflammatory Bowel Diseases | journal = Mayo Clinic Proceedings | volume = 94 | issue = 1 | pages = 155–165 | pmid = 30611442 | pmc = 6386158 | date = January 2019 | doi = 10.1016/j.mayocp.2018.09.013 | doi-access = free }}</ref> |
|||
Crohn's disease also increases the risk of cancer in the area of inflammation. For example, individuals with Crohn's disease involving the [[small bowel]] are at higher risk for [[small intestinal cancer]]. Similarly, people with Crohn's colitis have a [[relative risk]] of 5.6 for developing [[colon cancer]].<ref>{{cite journal |author=Ekbom A, Helmick C, Zack M, Adami H |title=Increased risk of large-bowel cancer in Crohn's disease with colonic involvement |journal=Lancet |volume=336 |issue=8711 |pages=357–9 |year=1990 |pmid=1975343 | doi = 10.1016/0140-6736(90)91889-I}}</ref> Screening for colon cancer with [[colonoscopy]] is recommended for anyone who has had Crohn's colitis for at least eight years.<ref>{{cite journal | author = Collins P, Mpofu C, Watson A, Rhodes J | title = Strategies for detecting colon cancer and/or dysplasia in patients with inflammatory bowel disease | journal = Cochrane Database Syst Rev | volume = | issue = 2| pages = CD000279 | year = 2006| pmid = 16625534 | doi = 10.1002/14651858.CD000279.pub3}}</ref> Some studies suggest that there is a role for chimioprotection in the prevention of colorectal cancer in Crohn's involving the colon; two agents have been suggested, [[folate]] and [[mesalamine]] preparations.<ref>{{cite journal | author = Lynne V McFarland | title = Colorectal cancer and dysplasia in inflammatory bowel disease | journal = World Journal of Gastroenterology | volume = | issue = | pages = 2665 | year = 2008| pmid = | doi = }}</ref> |
|||
=== Intestinal barrier === |
|||
Individuals with Crohn's disease are at risk of [[malnutrition]] for many reasons, including decreased food intake and [[malabsorption]]. The risk increases following resection of the [[small bowel]]. Such individuals may require oral supplements to increase their caloric intake, or in severe cases, [[total parenteral nutrition]] (TPN). Most people with moderate or severe Crohn's disease are referred to a [[dietitian]] for assistance in nutrition.<ref>{{cite journal | author = Evans J, Steinhart A, Cohen Z, McLeod R | title = Home total parenteral nutrition: an alternative to early surgery for complicated inflammatory bowel disease | journal = J Gastrointest Surg | volume = 7 | issue = 4 | pages = 562–6 | year = 2003 | pmid = 12763417 | doi = 10.1016/S1091-255X(02)00132-4}}</ref> |
|||
The epithelial barrier is a single layer of [[epithelial cells]] covered in antimicrobial mucus that protects the intestine from gut bacteria.<ref name="pmid25234148"/> Epithelial cells are joined by [[tight junction proteins]], which are reduced by Crohn's-linked polymorphisms. In particular, [[claudin-5]] and [[CLDN8|claudin-8]] are reduced, while pore-forming [[claudin-2]] is increased, causing intestinal permeability. Epithelial cells under stress emit inflammatory signals such as the [[unfolded protein response]] to stimulate the immune system, and Crohn's-linked polymorphisms to the [[ATG16L1]] gene lower the threshold at which this response is triggered.<ref name="pmid32242028">{{cite journal | vauthors = Roda G, Chien Ng S, Kotze PG, Argollo M, Panaccione R, Spinelli A, Kaser A, Peyrin-Biroulet L, Danese S | title = Crohn's Disease | journal = Nature Reviews Disease Primers | volume = 6 | issue = 1 | pages = 22 | pmid = 32242028 | date = April 2020 | doi = 10.1038/s41572-020-0156-2 | doi-access = free }}</ref> |
|||
In a functional state, the intestinal epithelium and IgA dimers work together to manage and keep the luminal microflora distinct from the mucosal immune system.<ref>{{cite journal | url=https://doi.org/10.1016/S0140-6736(16)31711-1 | doi=10.1016/S0140-6736(16)31711-1 | title=Crohn's disease | date=2017 | journal=The Lancet | volume=389 | issue=10080 | pages=1741–1755 | pmid=27914655 | vauthors = Torres J, Mehandru S, Colombel J, Peyrin-Biroulet L }}</ref> [[Paneth cells]] exist in the epithelial barrier of the small intestine and secrete [[Alpha defensin|α-defensins]] to prevent bacteria from entering gut tissue.<ref name="pmid25234148"/> Genetic polymorphisms associated with Crohn's disease can impair this ability and lead to Crohn's disease in the ileum. [[NOD2]] is a receptor produced by Paneth cells to sense bacteria, and mutations to NOD2 can inhibit the antimicrobial activity of Paneth cells. ATG16L1, [[IRGM]], and [[LRRK2]] are proteins involved in selective [[autophagy]], the mechanism by which Paneth cells secrete α-defensins, and mutations to these genes also impair the antimicrobial activity of Paneth cells.<ref name="pmid32242028"/> |
|||
Crohn's disease can cause significant complications including [[bowel obstruction]], abscesses, free [[Bowel perforation|perforation]] and [[hemorrhage]].<ref>{{cite web|url=https://www.livingwithcrohnsdisease.com/livingwithcrohnsdisease/crohns_disease/complications_of_crohns.html|title=Complications of Crohn's Disease| accessdate = 2009-11-07 }}</ref> |
|||
[[Intraepithelial lymphocytes]] (IELs) are immune cells that exist in the epithelial barrier, consisting mostly of activated [[T cells]]. They interact with gut bacteria directly and emit signals to regulate the intestinal immune system. IELs in Crohn's disease produce increased levels of inflammatory cytokines [[Interleukin 17|IL-17]], [[IFNγ]], and [[TNF]].<ref name="pmid32242028"/> It is hypothesized that inflammatory signals from the immune system and alterations to the gut microbiome influence IELs to produce inflammatory signals, contributing to Crohn's disease.<ref name="pmid29242771">{{cite journal | vauthors = Hu MD, Edelblum KL | title = Sentinels at the frontline: the role of intraepithelial lymphocytes in inflammatory bowel disease | journal = Current Pharmacology Reports | volume = 3 | issue = 6 | pages = 321–334 | pmid = 29242771 | date = August 2017 | doi = 10.1007/s40495-017-0105-2 | doi-access = free | pmc = 5724577 }}</ref> |
|||
Crohn's disease can be problematic during [[pregnancy]], and some medications can cause adverse outcomes for the [[fetus]] or mother. Consultation with an obstetrician and gastroenterologist about Crohn's disease and all medications allows preventative measures to be taken. In some cases, remission can occur during pregnancy. Certain medications can also impact [[sperm count]] or may otherwise adversely affect a man's ability to [[Fertilisation|conceive]].<ref>{{cite web | url = http://www.ccfa.org/about/news/pregnancy | publisher = [[Crohn's and Colitis Foundation of America]] | date = 2005-10-21 | title = IBD and Pregnancy: What You Need to Know | last = Kaplan | first = C | accessdate = 2009-11-07 }}</ref> |
|||
=== Immune system === |
|||
==Cause== |
|||
Normally, intestinal [[macrophages]] have reduced inflammatory behavior while retaining their ability to consume and destroy pathogens. In Crohn's disease, the number and activity of macrophages is reduced, enabling the entrance of pathogens into intestinal tissue.<ref name="pmid30611442"/> Macrophages degrade internal pathogens through autophagy, which is impaired by Crohn's-linked polymorphisms in genes such as NOD2 and ATG16L1.<ref name="pmid32242028"/> Additionally, people with Crohn's tend to have a separate abnormal population of macrophages that secrete proinflammatory cytokines such as TNF and [[Interleukin 6|IL-6]].<ref name="pmid30611442"/> |
|||
The exact cause of Crohn's disease is still unknown, although more and more details are emerging and has become clear that the interplay of environmental factors and in a genetically predisposed host ignites disease.<ref> |
|||
{{cite journal |
|||
| author = Braat H, Peppelenbosch MP, Hommes DW |
|||
| title = Immunology of Crohn's disease |
|||
| journal = Ann. N. Y. Acad. Sci. |
|||
| volume = 1072 |
|||
| issue = |
|||
| pages = 135–54 |
|||
| year = 2006 |
|||
| month = August |
|||
| accessdate = 2009-11-04 |
|||
| doi = 10.1196/annals.1326.039 |
|||
| pmid = 17057196 |
|||
}}</ref> The genetic risk factors have now more or less been comprehensively elucidated, making Crohn's disease the first genetically complex disease of which the genetic background has been resolved.<ref>{{cite journal |
|||
| author = Henckaerts L, Figueroa C, Vermeire S, Sans M |
|||
| title = The role of genetics in inflammatory bowel disease |
|||
| journal = Curr Drug Targets |
|||
| volume = 9 |
|||
| issue = 5 |
|||
| pages = 361–8 |
|||
| year = 2008 |
|||
| month = May |
|||
| accessdate = 2009-11-04 |
|||
| doi = 10.2174/138945008784221161 |
|||
| pmid = 18473763 |
|||
}}</ref> The relative risks of contracting the disease when one has a mutation in one of the risk genes, however, are actually very low (approximately 1:200). Broadly speaking, the genetic data indicate that innate immune systems in patients with Crohn's disease malfunction, and direct assessment of patient immunity confirms this notion.<ref name=Marks2006> |
|||
{{cite journal |
|||
|author= Marks DJ, Harbord MW, MacAllister R, Rahman FZ, Young J, Al-Lazikani B, Lees W, Novelli M, Bloom S, Segal AW |
|||
|title= Defective acute inflammation in Crohn's disease: a clinical investigation |
|||
|journal= Lancet |
|||
|volume= 367 |
|||
|issue= 9511 |
|||
|pages= 668–78 |
|||
|year= 2006 |
|||
|pmid= 16503465 |
|||
|doi= 10.1016/S0140-6736(06)68265-2 |
|||
|pmc= 2092405 |
|||
}}</ref> This had led to the notion that Crohn's disease should be viewed as innate immune deficiency, chronic inflammation being caused by adaptive immunity trying to compensate for the reduced function of the innate immune system.<ref> |
|||
{{cite journal |
|||
| author = Comalada M, Peppelenbosch MP |
|||
| title = Impaired innate immunity in Crohn's disease |
|||
| journal = Trends Mol Med |
|||
| volume = 12 |
|||
| issue = 9 |
|||
| pages = 397–9 |
|||
| year = 2006 |
|||
| month = September |
|||
| accessdate = 2009-11-04 |
|||
| doi = 10.1016/j.molmed.2006.07.005 |
|||
| pmid = 16890491 |
|||
}}</ref> |
|||
[[Neutrophils]] are recruited from the bloodstream in response to inflammatory signals, and defend tissue by secreting antimicrobial substances and consuming pathogens.<ref name="pmid25234148"/> In Crohn's disease, neutrophil recruitment is delayed and autophagy is impaired, allowing bacteria to survive in intestinal tissue.<ref name="pmid30611442"/> Dysfunction in neutrophil secretion of [[reactive oxygen species]], which are toxic to bacteria, is associated with very early onset Crohn's disease. Although neutrophils are important in bacterial defense, their subsequent accumulation in Crohn's disease damages the epithelial barrier and perpetuates inflammation.<ref name="pmid32242028"/> |
|||
===Genetics=== |
|||
[[Image:NOD2 CARD15.svg|right|thumb|Schematic of NOD2 CARD15 gene, which is associated with certain disease patterns in Crohn's disease.]] |
|||
Some research has indicated that Crohn's disease may have a genetic link.<ref>{{cite web | url = http://www.ccfa.org/reuters/geneticlink | title = Crohn's disease has strong genetic link: study | publisher = [[Crohn's and Colitis Foundation of America]] | date = 2007-04-16 | accessdate = 2009-11-07 }}</ref> The disease runs in families and those with a sibling with the disease are 30 times more likely to develop it than the normal population. |
|||
[[Innate lymphoid cell]]s (ILCs) consist of subtypes including ILC1s, ILC2s, and ILC3s. ILC3s are particularly important for regenerating the epithelial barrier through secretion of IL-17 by NCR- ILC3s and [[Interleukin 22|IL-22]] by NCR+ ILC3s. During Crohn's disease, inflammatory signals from antigen-presenting cells, such as IL-23, cause excessive IL-17 and IL-22 secretion. Although these cytokines protect the intestinal barrier, excessive production damages the barrier through increased inflammation and neutrophil recruitment. Additionally, [[Interleukin 12|IL-12]] from activated dendritic cells influence NCR+ ILC3s to transform into inflammatory [[IFNγ]]-producing ILC1s.<ref name="pmid30962426">{{cite journal | vauthors = Zeng B, Shi S, Ashworth G, Dong C, Liu J, Xing F | title = ILC3 function as a double-edged sword in inflammatory bowel diseases | journal = Cell Death & Disease | volume = 10 | issue = 4 | pages = 315 | pmid = 30962426 | pmc = 6453898 | date = April 2019 | doi = 10.1038/s41419-019-1540-2 | doi-access = free }}</ref> |
|||
[[Mutation]]s in the [[CARD15]] gene (also known as the NOD2 [[gene]]) are associated with Crohn's disease<!-- --><ref>{{cite journal |author=Ogura Y, Bonen DK, Inohara N, ''et al.'' |title=A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease |journal=Nature |volume=411 |issue=6837 |pages=603–6 |year=2001 |pmid=11385577 |doi=10.1038/35079114 |url= |last12=Brant |first12=SR |last13=Bayless |first13=TM |last14=Kirschner |first14=BS |last15=Hanauer |first15=SB |last16=Nuñez |first16=G |last17=Cho |first17=JH}}</ref> and with susceptibility to certain phenotypes of disease location and activity.<ref><!-- |
|||
-->{{cite journal | author = Cuthbert A, Fisher S, Mirza M, ''et al.'' | title = The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease | journal = Gastroenterology | volume = 122 | issue = 4 | pages = 867–74 | year = 2002 | pmid = 11910337 | doi = 10.1053/gast.2002.32415 | last12 = Lewis | first12 = CM | last13 = Mathew | first13 = CG}}</ref> In earlier studies, only two genes were linked to Crohn's, but scientists now believe there are over thirty genes that show genetics play a role in the disease, either directly through causation or indirectly as with a [[mediator variable]]. Anomalies in the [[XBP1]] gene have recently been identified as a factor, pointing towards a role for the [[unfolded protein response]] pathway of the [[endoplasmatic reticulum]] in inflammatory bowel diseases.<ref>{{cite journal|url=http://www.cell.com/content/article/abstract?uid=PIIS0092867408009410|title=XBP1 Links ER Stress to Intestinal Inflammation and Confers Genetic Risk for Human Inflammatory Bowel Disease|journal=Cell|volume=134|pages=743–756|publisher=Cell Press|author=Kaser et al.|date=5 September 2008|doi=10.1016/j.cell.2008.07.021|pmid=18775308|last1=Kaser|first1=A|last2=Lee|first2=AH|last3=Franke|first3=A|last4=Glickman|first4=JN|last5=Zeissig|first5=S|last6=Tilg|first6=H|last7=Nieuwenhuis|first7=EE|last8=Higgins|first8=DE|last9=Schreiber|first9=S|issue=5|author2=Lee|author3=Franke|author4=Glickman|author5=Zeissig|author6=Tilg|author7=Nieuwenhuis|author8=Higgins|author9=Schreiber|first10=LH|pmc=2586148}}</ref><ref>{{cite journal |author=Clevers H |title=Inflammatory Bowel Disease, Stress, and the Endoplasmic Reticulum |journal=N Engl J Med |volume=360 |issue=7 |pages=726–727 |year=2009|doi= 10.1056/NEJMcibr0809591|url=http://content.nejm.org/cgi/content/full/360/7/726 |pmid=19213688 |last1=Clevers |first1=H}}</ref> |
|||
Naive T cells are activated primarily by dendritic cells, which then differentiate into anti-inflammatory [[Regulatory T cell|T regulatory cells]] (Tregs) or inflammatory T helper cells to maintain balance. In Crohn's disease, macrophages and antigen-presenting cells secrete IL-12, [[Interleukin 18|IL-18]], and IL-23 in response to pathogens, increasing Th1 and T17 differentiation and promoting inflammation via [[Interleukin 17|IL-17]], IFNγ and TNF. IL-23 is particularly important, and IL-23 receptor polymorphisms that increase activity are linked with Crohn's disease. Tregs suppress inflammation via [[Interleukin 10|IL-10]], and mutations to IL-10 and its receptor cause very early onset Crohn's disease.<ref name="pmid32242028"/> |
|||
===Environmental factors=== |
|||
Diet is believed to be linked to its higher prevalence in industrialized parts of the world. [[Tobacco smoking|Smoking]] has been shown to increase the risk of the return of active disease, or "flares".<ref name=Cosnes2004/> The introduction of [[hormonal contraception]] in the United States in the 1960s is linked with a dramatic increase in the incidence rate of Crohn's disease. Although a causal linkage has not been effectively shown, there remain fears that these drugs work on the digestive system in ways similar to smoking.<ref><!-- |
|||
-->{{cite journal | author = Lesko S, Kaufman D, Rosenberg L, ''et al.'' | title = Evidence for an increased risk of Crohn's disease in oral contraceptive users | journal = Gastroenterology | volume = 89 | issue = 5 | pages = 1046–9 | year = 1985 | pmid = 4043662}}</ref> |
|||
=== |
=== Microbiome === |
||
People with Crohn's disease tend to have altered microbiomes, although no disease-specific microorganisms have been identified. An altered microbiome may link environmental factors with Crohn's, though causality is uncertain. [[Firmicutes]] tend to be reduced, particularly [[Faecalibacterium prausnitzii]], which produces [[short-chain fatty acids]] that reduce inflammation. [[Bacteroidetes]] and [[proteobacteria]] tend to be increased, particularly adherent-invasive [[E. coli]], which attaches to intestinal epithelial cells. Additionally, mucolytic and sulfate-reducing bacteria are elevated, contributing to damage to the intestinal barrier.<ref name="pmid30611442"/> |
|||
Abnormalities in the [[immune]] system have often been invoked as being causes of Crohn's disease. Crohn's disease is thought to be an autoimmune disease, with inflammation stimulated by an over-active [[T helper cell#Th1/Th2 Model for helper T cells|T<sub>h</sub>1]] [[cytokine]] response.<ref>{{cite journal |author=Cobrin GM, Abreu MT |title=Defects in mucosal immunity leading to Crohn's disease |journal=Immunol. Rev. |volume=206 |issue= |pages=277–95 |year=2005 |pmid=16048555 |doi=10.1111/j.0105-2896.2005.00293.x |url=}}</ref> However, more recent evidence has shown that [[Th17|T<sub>h</sub>17]] is of greater importance in the disease.<ref name=Elson2007>{{Cite journal |
|||
| last = Elson | first = C. |
|||
| year = 2007 |
|||
| title = Monoclonal Anti–Interleukin 23 Reverses Active Colitis in a T Cell–Mediated Model in Mice |
|||
| journal = Gastroenterology |
|||
| volume = 132 |
|||
| pages = 2359 |
|||
| doi = 10.1053/j.gastro.2007.03.104 |
|||
| pmid = 17570211 |
|||
| last1 = Elson |
|||
| first1 = CO |
|||
| last2 = Cong |
|||
| first2 = Y |
|||
| last3 = Weaver |
|||
| first3 = CT |
|||
| last4 = Schoeb |
|||
| first4 = TR |
|||
| last5 = Mcclanahan |
|||
| first5 = TK |
|||
| last6 = Fick |
|||
| first6 = RB |
|||
| last7 = Kastelein |
|||
| first7 = RA |
|||
| issue = 7 |
|||
| author2 = Cong |
|||
| author3 = Weaver |
|||
| author4 = Schoeb |
|||
| author5 = McClanahan |
|||
| author6 = Fick |
|||
| author7 = Kastelein |
|||
}}</ref> The most recent gene to be implicated in Crohn's disease is ATG16L1, which may induce [[Autophagy (cellular)|autophagy]] and hinder the body's ability to attack invasive bacteria.<ref>{{cite journal |author=Prescott NJ, Fisher SA, Franke A, ''et al.'' |title=A nonsynonymous SNP in ATG16L1 predisposes to ileal Crohn's disease and is independent of CARD15 and IBD5 |journal=Gastroenterology |volume=132 |issue=5 |pages=1665–71 |year=2007 |pmid=17484864 |doi=10.1053/j.gastro.2007.03.034 |url= |last12=Lewis |first12=CM |last13=Schreiber |first13=S |last14=Mathew |first14=CG}}</ref> |
|||
Alterations in gut viral and fungal communities may contribute to Crohn's disease. [[Caudovirales]] bacteriophage sequences found in children with Crohn's suggest a potential biomarker for early-onset disease. A meta-analysis showed lower viral diversity in Crohn's patients compared to healthy individuals, with increased [[Synechococcus phage S CBS1]] and [[Retroviridae]] viruses. Additionally, a Japanese study found that the fungal microbiota in Crohn's patients differs significantly from that of healthy individuals, particularly with an abundance of [[Candida albicans|Candida]].<ref name="pmid32242028"/> |
|||
Contrary to the prevailing view that Crohn's disease is a primary T cell autoimmune disorder, there is an increasing body of evidence in favour of the hypothesis that Crohn's disease results from an impaired innate immunity.<ref>{{cite journal| author= Marks DJ, Segal AW. |title=Innate immunity in inflammatory bowel disease: a disease hypothesis|journal= J Pathol. |volume =214 |issue= 2 |pages=260–6 |year=2008 | month = January | doi= 10.1002/path.2291| pmc= 2635948 | accessdate = 2009-11-04| pmid= 18161747}}</ref> The immunodeficiency, which has been shown to be due to (at least in part) impaired cytokine secretion by macrophages, is thought to lead to a sustained microbial-induced inflammatory response, particularly in the colon where the bacterial load is especially high.<ref name=Marks2006/><ref> |
|||
{{cite journal| author= Dessein R, Chamaillard M, Danese S |title=Innate immunity in Crohn's disease: the reverse side of the medal |journal= J Clin Gastroenterol |volume =42 |issue= Suppl 3 Pt 1 |pages=S144–7 |year=2008 |month= September |pmid= 18806708 | doi= 10.1097/MCG.0b013e3181662c90| doi_brokendate= 2009-09-20| accessdate = 2009-11-04}}</ref> |
|||
== |
== Diagnosis == |
||
Diagnosis of Crohn's disease may be challenging since its symptoms overlap with other gastrointestinal diseases. An accurate diagnosis requires a combined assessment of clinical history, physical examination, and diagnostic tests. |
|||
A variety of pathogenic bacteria were initially suspected of being causative agents of Crohn's disease.<ref>{{cite web |url=http://www.crohns.org/research/index.htm |title=OVERVIEW: MAP and Crohn's Disease Research |work= | accessdate = 2009-11-07 }}</ref> However, most health care professionals now believe that a variety of microorganisms are taking advantage of their host's weakened mucosal layer and inability to clear bacteria from the intestinal walls, both symptoms of the disease.<ref><!-- |
|||
-->{{cite journal | author = Sartor, R. | title = Mechanisms of Disease: pathogenesis of Crohn's disease and ulcerative colitis | journal = Nature Clinical Practice Gastroenterology & Hepatology | year = 2006 | month = July | volume = 3 | issue = 7 | pages = 390–407 | url=www.nature.com/nrgastro/journal/v3/n7/full/ncpgasthep0528.html | doi = 10.1038/ncpgasthep0528 }} PMID 16819502</ref> Some studies have suggested that ''[[Mycobacterium avium subspecies paratuberculosis]]'' plays a role in Crohn's disease, in part because it causes a very similar disease, [[Johne's disease]], in cattle.<ref>{{cite journal |author=Naser SA, Collins MT |title=Debate on the lack of evidence of Mycobacterium avium subsp. paratuberculosis in Crohn's disease |journal=Inflamm. Bowel Dis. |volume=11 |issue=12 |pages=1123 |year=2005 |pmid=16306778 |doi= 10.1097/01.MIB.0000191609.20713.ea|url=}}</ref> The [[mannose]] bearing antigens (mannins) from yeast may also elicit an [[antibody]] response.<ref name="pmid1398231">{{cite journal | author = Giaffer MH, Clark A, Holdsworth CD | title = Antibodies to Saccharomyces cerevisiae in patients with Crohn's disease and their possible pathogenic importance | journal = Gut | volume = 33 | issue = 8 | pages = 1071–5 | year = 1992 | pmid = 1398231 | doi = 10.1136/gut.33.8.1071 | pmc = 1379444}}</ref> Other studies have linked specific strains of enteroadherent ''[[E. coli]]'' to the disease.<ref>{{cite journal | author = Baumgart M ''et al.'' | title = Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn's disease involving the ileum | pmid = 18043660 | journal = The ISME Journal | year = 2007 | url = http://www.nature.com/ismej/journal/v1/n5/full/ismej200752a.html | doi = 10.1038/ismej.2007.52 | volume = 1 | pages = 403 | last12 = Schukken | first12 = Y | last13 = Scherl | first13 = E | last14 = Simpson | first14 = KW | issue = 5 }}</ref> Still, this relationship between specific types of bacteria and Crohn's disease remains unclear.<ref name=scah_out38>{{cite web |url=http://ec.europa.eu/food/fs/sc/scah/out38_en.pdf |title=Possible links between Crohn’s disease and Paratuberculosis |format=PDF |work=EUROPEAN COMMISSION DIRECTORATE-GENERAL HEALTH & CONSUMER PROTECTION | accessdate = 2009-11-07}}</ref><ref>{{cite journal |author=Gui GP, Thomas PR, Tizard ML, Lake J, Sanderson JD, Hermon-Taylor J |title=Two-year-outcomes analysis of Crohn's disease treated with rifabutin and macrolide antibiotics |journal=J. Antimicrob. Chemother. |volume=39 |issue=3 |pages=393–400 |year=1997 |month=March |pmid=9096189 |doi= 10.1093/jac/39.3.393|url=http://jac.oxfordjournals.org/cgi/reprint/39/3/393 | format = PDF }}</ref> |
|||
=== Endoscopy === |
|||
Some studies have suggested that some symptoms of Crohn's disease, ulcerative colitis and [[irritable bowel syndrome]] have the same underlying cause. Biopsy samples taken from the colons of all three patient groups were found to produce elevated levels of a serine protease.<ref>{{cite journal |author=Cenac N, Andrews CN, Holzhausen M, ''et al.'' |title=Role for protease activity in visceral pain in irritable bowel syndrome |journal=J. Clin. Invest. |volume=117 |issue=3 |pages=636–47 |year=2007 |month=March |pmid=17304351 |doi=10.1172/JCI29255 |url= |last12=Ferraz |first12=JG |last13=Shaffer |first13=E |last14=Vergnolle |first14=N |pmc=1794118}}</ref> Experimental introduction of the serine protease into mice has been found to produce widespread pain associated with irritable bowel syndrome as well as colitis, which is associated with all three diseases.<ref>{{cite journal |author=Cenac N, Coelho AM, Nguyen C, ''et al.'' |title=Induction of intestinal inflammation in mouse by activation of proteinase-activated receptor-2 |journal=Am. J. Pathol. |volume=161 |issue=5 |pages=1903–15 |year=2002 |month=November |pmid=12414536 |doi= |url=http://ajp.amjpathol.org/cgi/pmidlookup?view=long&pmid=12414536 |last12=Vergnolle |first12=N |pmc=1850779}}</ref> The authors of that study were unable to identify the source of the protease, but a separate review noted that regional and temporal variations in those illnesses follow those associated with infection with a poorly understood protozoan, [[Blastocystis]].<ref>{{cite journal |author=Boorom KF, Smith H, Nimri L, ''et al.'' |title=Oh my aching gut: irritable bowel syndrome, Blastocystis, and asymptomatic infection |journal=Parasit Vectors |volume=1 |issue=1 |pages=40 |year=2008 |month=October |pmid=18937874 |doi=10.1186/1756-3305-1-40 |url= |pmc=2627840}}</ref> |
|||
[[Image:CD colitis.jpg|thumb|right|alt=Image of deep ulcers in the colon of a person with Crohn's colitis.|Image of a colon showing deep ulceration due to Crohn's disease.]] |
|||
[[Image:CD serpiginous ulcer.jpg|thumb|right|alt=Image of a serpiginous ulcer due to Crohn's disease found during a colonoscopy.|Image of a serpiginous ulcer in the colon, a classic finding in Crohn's disease]] |
|||
A study in 2003 put forth the "cold-chain" hypothesis, that [[psychrotrophic bacteria]] such as Yersinia spp and Listeria spp contribute to the disease. A statistical correlation was found between the advent of the use of refrigeration in the United States and various parts of Europe and the rise of the disease.<ref>{{Cite journal |
|||
| last1 = Hugot |
|||
| first1 = Jean-Pierre |
|||
| last2 = Alberti |
|||
| first2 = Corinne |
|||
| last3 = Berrebi |
|||
| first3 = Dominique |
|||
| last4 = Bingen |
|||
| first4 = Edouard |
|||
| last5 = Cezard |
|||
| first5 = Jean-Pierre |
|||
| title = Crohn's disease: the cold chain hypothesis |
|||
| journal = The Lancet |
|||
| volume = 362 |
|||
| issue = 9400 |
|||
| pages = 2012–2015 |
|||
| date = 2003-12-13 |
|||
| year = 2003 |
|||
| url = http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(03)15024-6 |
|||
| doi = 10.1016/S0140-6736(03)15024-6 }}</ref><ref>{{Cite news |
|||
| title = Fridges blamed for Crohn's disease rise |
|||
| newspaper = Medical News TODAY |
|||
| year = 2003 |
|||
| date = 2003-12-12 |
|||
| url = http://www.medicalnewstoday.com/articles/4849.php}}</ref> Later studies have provided support for this hypothesis.<ref>{{Cite journal |
|||
| last1 = Forbes |
|||
| first1 = Alastair |
|||
| last2 = Kalantzis |
|||
| first2 = Tommy |
|||
| title = Crohn's disease : the cold chain hypothesis |
|||
| journal = International Journal of Colorectal Disease |
|||
| volume = 21 |
|||
| issue = 5 |
|||
| pages = 399–401 |
|||
| publisher = Springer Berlin / Heidelberg |
|||
| issn = 0179-1958 |
|||
| year = 2006 |
|||
| month = July |
|||
| url = www.springerlink.com/content/p6q21tp76x013u51/ |
|||
| doi = 10.1007/s00384-005-0003-7 |
|||
| pmid = 16059694 |
|||
| accessdate = 2009-11-04 |
|||
| author2 = Kalantzis |
|||
}}</ref> |
|||
[[Colonoscopy|Ileocolonoscopy]] is the primary procedure for diagnosing Crohn's disease in the ileum and colon, accurately identifying it in about 90% of cases.<ref name="pmid29972402">{{Cite journal |last1=Passos |first1=Márcio Alexandre Terra |last2=Chaves |first2=Fernanda Correa |last3=Chaves-Junior |first3=Nilson |date=2018 |title=The Importance of Colonoscopy in Inflammatory Bowel Diseases |journal=Arquivos Brasileiros de Cirurgia Digestiva |volume=31 |issue=2 |pages=e1374 |doi=10.1590/0102-672020180001e1374 |pmc=6044200 |pmid=29972402 |doi-access=free}}</ref> During this exam, doctors closely examine the intestinal lining and take small tissue samples for further testing. Signs of Crohn's disease include uneven inflammation and 'skip lesions', which are patches of inflammation separated by healthy tissue. The ulcers can be small (less than 5 mm) or larger (over 5 mm), often appearing cobblestone-like. Their depth helps determine disease severity. Unlike [[ulcerative colitis]], Crohn's disease usually does not affect the rectum or cause continuous inflammation around the bowel.<ref name="pmid32242028"/> |
|||
Studies done at the University of Liverpool have offered ideas that would explain the apparent connection between Crohn's disease, Mycobacterium, other pathogenic bacteria, and genetic markers.<ref>{{Cite journal |
|||
| last1 = Subramanian | first1 = Sreedhar | last2 = Carol | first2 = L. Roberts | last3 = Hart | first3 = C. Anthony | last4 = Martin | first4 = Helen M. | first5 = Steve W. | last6 = Rhodes | first6 = Jonathan M. | last7 = Campbell | first7 = Barry J. | title = Replication of Colonic Crohn's Disease Mucosal Escherichia coli Isolates within Macrophages and Their Susceptibility to Antibiotics | journal = Antimicrobial Agents and Chemotherapy | volume = 52 | pages = 427–434 | year = 2008 | url = http://aac.asm.org/cgi/content/abstract/52/2/427 | doi = 10.1128/AAC.00375-07 |
|||
| pmid = 18070962 |
|||
| last5 = Edwards |
|||
| issue = 2 |
|||
| author2 = Roberts |
|||
| author3 = Hart |
|||
| author4 = Martin |
|||
| author5 = Edwards |
|||
| author6 = Rhodes |
|||
| author7 = Campbell |
|||
| pmc = 2224732 |
|||
| unused_data = |last5 Edwards }}</ref><ref>{{Cite journal | last1 = Mpofu | first1 = Chiedzo M. | last2 = Cambell | first2 = Barry J. | last3 = Subramanin | first3 = Sreedhar | last4 = Marshall-Clarke | first4 = Stuart | last5 = Hart | first5 = Anthony C. | last6 = Cross | first6 = Andy | last7 = Roberts | first7 = Carol L. | last8 = McGoldrick | first8 = Adrian | last9 = Edwards | first9 = Steven W. | title = Microbial Mannan Inhibits Bacterial Killing by Macrophages: A Possible Pathogenic Mechanism for Crohn’s Disease | journal = Gastroenterology, the official journal of the AGA Institute | volume = 133 | issue = 5 | pages = 1487–1498 | year = 2007 | url = http://www.gastrojournal.org/article/S0016-5085(07)01450-3/abstract | doi = 10.1053/j.gastro.2007.08.004 | pmid = 17919633 | author2 = Campbell | author3 = Subramanian | author4 = Marshall-clarke | author5 = Hart | author6 = Cross | author7 = Roberts | author8 = McGoldrick | author9 = Edwards | first10 = JM }}</ref> In many individuals genetic factors predispose individuals to Mycobacterium avium subsp. paratuberculosis infection. This bacteria then produce mannins which protect both itself and various bacteria from phagocytosis, which causes a variety of secondary infections.<ref>{{Cite web | url = http://www.liv.ac.uk/researchintelligence/issue33/crohns.htm |title=New insights into Crohn's Disease}}</ref> Other mycobacterial diseases, such as [[leprosy]] and [[Tuberculosis]] could be considered similar in that they have strong genetic components, but are not genetic per se. |
|||
In certain cases, such as disease in the upper small bowel, standard colonoscopy may be ineffective. Physicians may then opt for [[Enteroscopy|device-assisted enteroscopy]] or [[capsule endoscopy]]. While capsule endoscopy is effective in detecting abnormalities, it may not reliably diagnose Crohn's disease and carries a risk of retention, which is about 1.6% when Crohn's disease is suspected and increases to 13% if already diagnosed. To reduce this risk, physicians typically perform small-bowel imaging and use a [[patency capsule]] that disintegrates within 48 to 72 hours. Once the patency capsule has passed through the intestine, capsule endoscopy may be performed.<ref name="pmid28601423"/> |
|||
==Pathophysiology== |
|||
[[Image:Crohn's transmural path.jpg|thumb|80px|left|Section of [[colectomy]] showing transmural inflammation]] |
|||
During a [[colonoscopy]], [[Biopsy|biopsies]] of the colon are often taken in order to confirm the diagnosis. There are certain characteristic features of the [[pathology]] seen that point toward Crohn's disease. Crohn's disease shows a transmural pattern of [[inflammation]], meaning that the inflammation may span the entire depth of the intestinal wall.<ref name=Baumgart/> Grossly, [[Peptic ulcer|ulceration]] is an outcome seen in highly active disease. There is usually an abrupt transition between unaffected tissue and the ulcer. Under a microscope, biopsies of the affected colon may show [[mucosa]]l inflammation. This inflammation is characterized by focal infiltration of [[neutrophils]], a type of inflammatory cell, into the [[epithelium]]. This typically occurs in the area overlying [[lymphoid tissue|lymphoid]] aggregates. These neutrophils, along with [[lymphocyte|mononuclear cells]], may infiltrate into the [[Crypts of Lieberkuhn|crypts]] leading to inflammation (crypititis) or abscess (crypt abscess). [[Granuloma]]s, aggregates of [[macrophage]] derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. The granulomas of Crohn's disease do not show "caseation", a cheese-like appearance on microscopic examination that is characteristic of granulomas associated with infections such as [[tuberculosis]]. Biopsies may also show chronic mucosal damage as evidenced by blunting of the intestinal [[villus|villi]], atypical branching of the crypts, and change in the tissue type ([[metaplasia]]). One example of such metaplasia, ''Paneth cell metaplasia'', involves development of Paneth cells (typically found in the small intestine) in other parts of the gastrointestinal system.<ref name=Robbins>Crawford JM. "The Gastrointestinal tract, Chapter 17". In Cotran RS, Kumar V, Robbins SL. ''Robbins Pathologic Basis of Disease: 5th Edition''. W.B. Saunders and Company, Philadelphia, 1994.</ref> |
|||
[[Enteroscopy|Device-assisted enteroscopy]] is not typically the first choice for diagnosing small-bowel Crohn's disease due to its invasiveness and higher costs.<ref name="pmid32242028"/> The procedure closely examines the small intestine using specialized tools, such as longer endoscopes or balloon-assisted devices, making it easier for doctors to visualize and treat issues.<ref name="pmid31367155">{{Cite journal |vauthors=Schneider M, Höllerich J, Beyna T |date=July 2019 |title=Device-assisted enteroscopy: A review of available techniques and upcoming new technologies |journal=World Journal of Gastroenterology |volume=25 |issue=27 |pages=3538–3545 |doi=10.3748/wjg.v25.i27.3538 |pmc=6658397 |pmid=31367155 |doi-access=free}}</ref> It often requires sedation and is generally reserved for patients needing a tissue sample or immediate treatment.<ref name="pmid32242028"/> |
|||
==Diagnosis== |
|||
[[Image:CD colitis.jpg|thumb|right|[[Colonoscopy|Endoscopic]] image of Crohn's colitis showing deep ulceration]] |
|||
[[Image:CT scan gastric CD.jpg|thumb|right|[[CT scan]] showing Crohn's disease in the fundus of the [[stomach]]]] |
|||
[[Image:CD colitis 2.jpg|thumb|Crohn's disease can mimic ulcerative colitis on endoscopy. This [[Colonoscopy|endoscopic]] image is of Crohn's colitis showing diffuse loss of [[mucosa]]l architecture, [[friable|friability]] of mucosa in sigmoid colon and exudate on wall, all of which can be found with ulcerative colitis.]] |
|||
=== Cross-sectional Imaging === |
|||
The diagnosis of Crohn's disease can sometimes be challenging,<ref name=Pimentel/> and a number of tests are often required to assist the physician in making the diagnosis.<ref name=emed/> Even with a full battery of tests it may not be possible to diagnose Crohn's with complete certainty; a colonoscopy is approximately 70% effective in diagnosing the disease with further tests being less effective. Disease in the small bowel is particularly difficult to diagnose as a traditional colonoscopy only allows access to the colon and lower portions of the small intestines; introduction of the [[Capsule endoscopy]]<ref>[http://www.givenimaging.com/en-us/HealthcareProfessionals/Pages/pageHCP.aspx HCP: Pill Cam, Capsule Endoscopy, Esophageal Endoscopy<!-- Bot generated title -->]</ref> aids in endoscopic diagnosis. |
|||
[[Image:CT scan gastric CD.jpg|thumb|right|alt=CT scan of Crohn's disease in the fundus of the stomach.|CT scan showing Crohn's disease in the stomach]] |
|||
Cross-sectional imaging techniques, like [[Abdominal ultrasonography|bowel ultrasonography]] (BUS), [[Computed tomography enterography|CT enterography]] (CTE), and [[Magnetic resonance enterography|MRI enterography]] (MRE), are essential for understanding how extensive Crohn's disease is and whether there are any complications, like blockages or abnormal connections between organs. All three methods are quite accurate for diagnosing Crohn's disease and spotting these complications.<ref name="pmid32242028"/> |
|||
===Endoscopy=== |
|||
A [[colonoscopy]] is the best test for making the diagnosis of Crohn's disease as it allows direct visualization of the colon and the [[terminal ileum]], identifying the pattern of disease involvement. Occasionally, the colonoscope can travel past the terminal ileum but it varies from patient to patient. During the procedure, the [[gastroenterologist]] can also perform a [[biopsy]], taking small samples of tissue for laboratory analysis which may help confirm a diagnosis. As 30% of Crohn's disease involves only the ileum,<ref name=Baumgart/> [[cannula]]tion of the terminal ileum is required in making the diagnosis. Finding a patchy distribution of disease, with involvement of the colon or ileum but not the [[rectum]], is suggestive of Crohn's disease, as are other endoscopic stigmata.<!-- is passed in the patient's faeces. It has been used in the search for Crohn's disease in the small bowel, which cannot be reached with colonoscopy or gastroscopy.<!-- |
|||
--><ref name="Hara2006"/><!-- |
|||
-->The utility of capsule endoscopy for this, however, is still uncertain.<!-- |
|||
--><ref>{{cite journal | last = Triester | first = Stuart L. | coauthors = Jonathan A. Leighton, Grigoris I. Leontiadis, Suryakanth R. Gurudu, David E. Fleischer, Amy K. Hara, Russell I. Heigh, Arthur D. Shiff, and Virender K. Sharma | year = 2006 | title = A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn's disease | journal = The American Journal of Gastroenterology | volume = 101 | issue = 5 | pages = 954–64 | doi =10.1111/j.1572-0241.2006.00506.x | pmid = 16696781 | accessdate = 2009-11-04}}</ref> |
|||
* CTE involves [[radiation]] and requires the use of [[contrast agents]] (substances that help show details in images). Despite this, CTE is very effective, with over 80% accuracy in diagnosing the disease and its complications, including blockages and fistulas (abnormal connections).<ref name="pmid32242028"/> |
|||
===Radiologic tests=== |
|||
* MRE is particularly good for detecting intestinal narrowing, with 89% sensitivity and 94% specificity. It is the preferred option for examining fistulas and abscesses in the pelvic area.<ref name="pmid32242028"/> |
|||
A [[barium follow-through|small bowel follow-through]] may suggest the diagnosis of Crohn's disease and is useful when the disease involves only the small intestine. Because colonoscopy and [[Esophagogastroduodenoscopy|gastroscopy]] allow direct visualization of only the terminal ileum and beginning of the [[duodenum]], they cannot be used to evaluate the remainder of the small intestine. As a result, a [[barium follow-through]] x-ray, wherein [[barium sulfate]] suspension is ingested and [[fluoroscopy|fluoroscopic]] images of the bowel are taken over time, is useful for looking for inflammation and narrowing of the small bowel.<!-- |
|||
* BUS is a non-invasive method that doesn't involve radiation and is effective for assessing the intestinal wall and related issues, such as fistulas and abscesses. Despite its limitations, it can accurately identify signs of Crohn's disease when the bowel wall thickens to more than 3 mm, achieving high accuracy rates (88–100%) when also considering factors like fistulas and abscesses.<ref name="pmid32242028"/> |
|||
--><ref name="Hara2006">{{cite journal | last = Hara | first = Amy K. | coauthors = Jonathan A. Leighton, Russell I. Heigh, Virender K. Sharma, Alvin C. Silva, Giovanni De Petris, Joseph G. Hentz and David E. Fleischer | year = 2006 | month = January | title = Crohn disease of the small bowel: preliminary comparison among CT enterography, capsule endoscopy, small-bowel follow-through, and ileoscopy | journal = Radiology | volume = 238 | issue = 1 | pages = 128–34 | doi =10.1148/radiol.2381050296 | pmid = 16373764 | accessdate = 2009-11-04}}</ref><!-- |
|||
--><ref>{{cite journal | last = Dixon | first = P.M. | coauthors = M.E. Roulston and D.J. Nolan | year = 1993 | title = The small bowel enema: a ten year review | journal = Clinical Radiology | volume = 47 | issue = 1 | pages = 46–8 | doi =10.1016/S0009-9260(05)81213-9 | pmid = 8428417 }}</ref> Barium enemas, in which barium is inserted into the rectum and fluoroscopy used to image the bowel, are rarely used in the work-up of Crohn's disease due to the advent of colonoscopy. They remain useful for identifying anatomical abnormalities when strictures of the colon are too small for a colonoscope to pass through, or in the detection of colonic fistulae.<!-- |
|||
--><ref>{{cite journal | last = Carucci | first = L. R. | coauthors = M. S. Levine | year = 2002 | title = Radiographic imaging of inflammatory bowel disease | journal = Gastroenterology Clinics of North America | volume = 31 | issue = 1 | pages = 93–117 | pmid = 12122746 | doi = 10.1016/S0889-8553(01)00007-3 }}</ref> |
|||
=== Histology === |
|||
[[Computed tomography|CT]] and [[MRI]] scans are useful for evaluating the small bowel with [[enteroclysis]] protocols.<!-- |
|||
[[File:Histopathology of granuloma of colonic mucosa.jpg|thumb|alt=Tissue stain of a granuloma due to Crohn's disease.|Tissue stain of a granuloma in the colonic mucosa due to Crohn's disease, consisting of an aggregate of [[histiocytes]] in the center of the image.]] |
|||
--><ref>{{cite journal | last = Rajesh | first = A. | coauthors = D.D.T. Maglinte | year = 2006 | title = Multislice CT enteroclysis: technique and clinical applications | journal = Clinical Radiology | volume = 61 | issue = 1 | pages = 31–9 | doi =10.1016/j.crad.2005.08.006 | pmid = 16356814 }}</ref><!-- |
|||
-->They are additionally useful for looking for intra-abdominal complications of Crohn's disease such as [[abscess]]es, small bowel obstruction, or fistulae.<!-- |
|||
--><ref>{{cite journal | last = Zissin | first = Rivka | coauthors = Marjorie Hertz, Alexandra Osadchy, Ben Novis and Gabriela Gayer | year = 2005 | title = Computed Tomographic Findings of Abdominal Complications of Crohn’s Disease—Pictorial Essay | journal = Canadian Association of Radiologists Journal | volume = 56 | issue = 1 | pages = 25–35 | pmid = 15835588 | url =http://www.carj.ca/issues/2005-Feb/25/pg25.pdf | format = PDF | accessdate = 2009-11-07 }}</ref> [[Magnetic resonance imaging]] (MRI) are another option for imaging the [[small bowel]] as well as looking for complications, though it is more expensive and less readily available<!-- |
|||
--><ref>{{cite journal | last = MacKalski | first = B. A. | coauthors = C. N. Bernstein | year = 2005 | title = New diagnostic imaging tools for inflammatory bowel disease | journal = Gut | volume = 55 | issue = 5 | pages = 733–41 | doi =10.1136/gut.2005.076612 | pmid = 16609136 | pmc = 1856109 }}</ref> |
|||
[[Image:Crohn's transmural path.jpg|thumb|right|alt=Tissue stain of colon showing deep inflammation across all layers.|Tissue stain of colon showing deep inflammation across all layers.]] |
|||
===Blood tests=== |
|||
A [[complete blood count]] may reveal [[anemia]], which may be caused either by blood loss or [[Cyanocobalamin|vitamin B{{ssub|12}}]] deficiency. The latter may be seen with ileitis because vitamin B{{ssub|12}} is absorbed in the [[ileum]].<!-- |
|||
--><ref name=Goh>{{cite journal | last = Goh | first = Jason | coauthors = C. A. O'Morain | year = 2003 | title = Review article: nutrition and adult inflammatory bowel disease | journal = Alimentary Pharmacology & Therapeutics | volume = 17 | issue = 3 | pages = 307–20 | doi =10.1046/j.1365-2036.2003.01482.x | pmid = 12562443 }}</ref><!-- |
|||
--> [[Erythrocyte sedimentation rate]], or ESR, and [[C-reactive protein]] measurements can also be useful to gauge the degree of inflammation.<!-- |
|||
--><ref>{{cite journal | last = Chamouard | first = Patrick | coauthors = Zoe Richert, Nicolas Meyer, Gabriel Rahmi, René Baumann | year = 2006 | title = Diagnostic Value of C-Reactive Protein for Predicting Activity Level of Crohn's Disease | journal = Clinical Gastroenterology and Hepatology | doi =10.1016/j.cgh.2006.02.003 | pmid = 16630759 | volume = 4 | pages = 882 | issue = 7}} Epub ahead of print</ref> It is also true in patient with ilectomy done in response to the complication. Another cause of anaemia is anaemia of chronic disease, characterized by its microcytic and hypochromic anaemia. There can be various reasons for anaemia, including medication used in treatment of inflammatory bowel disease like azathioprine which can lead to cytopenia and sulfasalazine which can also result in folate malabsorption, etc. Testing for anti-''[[Saccharomyces cerevisiae]]'' antibodies (ASCA) and [[anti-neutrophil cytoplasmic antibody|anti-neutrophil cytoplasmic antibodies]] (ANCA) has been evaluated to identify inflammatory diseases of the intestine<ref>{{cite journal | last = Kaila | first = B | coauthors = K Orr and C N Bernstein | year = 2005 | title = The anti-Saccharomyces cerevisiae antibody assay in a province-wide practice: accurate in identifying cases of Crohn's disease and predicting inflammatory disease | journal = The Canadian Journal of Gastroenterology | volume = 19 | issue = 12 | pages = 717–21 | pmid = 16341311 | url =www.pulsus.com/journals/abstract.jsp?sCurrPg=journal&jnlKy=2&atlKy=743&isuKy=263&isArt=t | accessdate = 2006-07-02 }}</ref><!-- |
|||
--> and to differentiate Crohn's disease from ulcerative colitis.<!----><ref>{{cite journal | last = Israeli | first = E. | coauthors = I. Grotto, B. Gilburd, R. D. Balicer, E. Goldin, A. Wiik and Y. Shoenfeld | year = 2005 | title = Anti-Saccharomyces cerevisiae and antineutrophil cytoplasmic antibodies as predictors of inflammatory bowel disease | journal = Gut | volume = 54 | issue = 9 | pages = 1232–6 | doi =10.1136/gut.2004.060228 | pmid = 16099791 | pmc = 1774672 }}</ref> Furthermore, increasing amounts and levels of serological antibodies such as ASCA, anti-laminaribioside [Glc(β1,3)Glb(β); ALCA], anti-chitobioside (GlcNAc(β1,4)GlcNAc(β); ACCA], anti-mannobioside [Man(α1,3)Man(α)AMCA], anti-Laminarin [Glc(β1,3))3n(Glc(β1,6))n; anti-L] and anti-Chitin [(GlcNAc(β1,4)n; anti-C] associate with disease behavior and surgery, and may aid in the prognosis of Crohn's disease.<!----><ref>{{cite journal | last = Ferrante | first = M. | coauthors = L. Henckaerts, M. Joossens, M. Pierik, S. Joossens, N. Dotan, G.L. Norman , R.T. Altstock , K. Van Steen , P. Rutgeerts , G. Van Assche and S.Vermeire | year = 2007 | title = New serological markers in inflammatory bowel disease are associated with complicated disease behaviour | journal = Gut | volume = 56 | issue = 10 | pages = 1394–403 | doi =10.1136/gut.2006.108043 | pmid = 17456509 | last12 = Vermeire | first12 = S }}</ref><ref>{{cite journal | last = Papp | first = M. | coauthors = I. Altorjay, N. Dotan, K. Palatka, I. Foldi, J. Tumpek, S. Sipka, M. Udvardy, T. Dinya, L. Lakatos, A. Kovacs, T. Molnar, Z. Tulassay, P. Mihelle, G.L. Norman, T. Szamosi , J. Papp; Hungarian IBD Study Group and P.L. Lakatos | year = 2008 | title = New serological markers for inflammatory bowel disease are associated with earlier age at onset, complicated disease behavior, risk for surgery, and NOD2/CARD15 genotype in a Hungarian IBD cohort | journal = Am J Gastroenterol | volume = 104 | issue = 6 | pages = 1426–34 | doi =10.1111/j.1572-0241.2007.01652.x | pmid = 18047543 | last12 = Molnar | first12 = T | last13 = Tulassay | first13 = Z | last14 = Miheller | first14 = P | last15 = Norman | first15 = GL | last16 = Szamosi | first16 = T | last17 = Papp | first17 = J | last18 = Hungarian Ibd Study | first18 = Group | last19 = Lakatos | first19 = PL }}</ref><ref>{{cite journal | last = Seow | first = C.H. | coauthors = J.M. Stempak, W. Xu, H. Lan, A.M. Griffiths, G.R. Greenberg, A.H. Steinhart, N. Dotan and M.S. Silverberg | year = 2009 | title = Novel anti-glycan antibodies related to inflammatory bowel disease diagnosis and phenotype | journal = Am J Gastroenterol | volume = 104 | issue = 6 | pages = 1426–34 | doi =10.1038/ajg.2009.79 | pmid = 19491856 }}</ref><ref>{{cite journal | last = Dotan | first = I. | year = 2007 | title = Serologic markers in inflammatory bowel disease: tools for better diagnosis and disease stratification | journal = Expert Rev Gastroenterol Hepatol | volume = 1| issue = 2 | pages = 265–74 | doi =10.1586/17474124.1.2.265 | pmid = 19072419}}</ref> |
|||
The most reliable way to confirm a diagnosis of Crohn's disease is through a [[histopathology|histological examination]] of biopsy samples or tissue removed during surgery. This process helps distinguish Crohn's disease from ulcerative colitis and other types of colitis, particularly infections. While no features are unique to Crohn's disease, typical signs include patchy chronic inflammation, irregularities in the intestinal lining, [[granulomas]] (not related to tissue injury), and abnormal [[intestinal villus|villi]] structure in the terminal ileum. A pathologist specializing in inflammatory bowel disease is important for accurate Crohn's disease diagnoses. Even if biopsy results are unclear, doctors can still suggest a Crohn's disease diagnosis based on clinical symptoms, endoscopic findings, and imaging results.<ref name="pmid32242028"/> |
|||
===Comparison with ulcerative colitis=== |
|||
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the [[colon (anatomy)|colon]] with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as '''indeterminate colitis'''.<ref name=Baumgart/><ref name=emed/><ref name=Podolsky/> |
|||
=== Disease activity indexes === |
|||
{| class="wikitable" cellpadding=1 style="text-align:left" |
|||
The Crohn's Disease Activity Index (CDAI) is a scoring system to assess the symptoms associated with Crohn's disease. It assigns a score based on eight clinical factors, including overall well-being, frequency of loose stools, abdominal pain, presence of abdominal masses, changes in weight, low [[hemoglobin]] levels, and use of opiates for diarrhea. The CDAI is primarily used in clinical trials to evaluate the effectiveness of treatments and to determine whether the disease is in remission. This is particularly significant, as approximately 50% of patients who report feeling well may still exhibit signs of active disease in the intestine, while some patients with symptoms may present with normal intestinal findings.<ref name="pmid32242028"/> |
|||
|+ '''Comparisons of various factors in Crohn's disease and ulcerative colitis''' |
|||
|- |
|||
! !! Crohn's disease !! Ulcerative colitis |
|||
|- |
|||
| [[Terminal ileum]] involvement || Commonly || Seldom |
|||
|- |
|||
| Colon involvement || Usually || Always |
|||
|- |
|||
| Rectum involvement || Seldom || Usually<ref name="Kornbluth-Sachar2004">{{cite journal | last = Kornbluth | first = Asher | coauthors = David B. Sachar | year = 2004 | month = July | title = Ulcerative colitis practice guidelines in adults (update): American College of Gastroenterology, Practice Parameters Committee | journal = American Journal of Gastroenterology | volume = 99 | issue = 7 | pages = 1371–85 | doi = 10.1111/j.1572-0241.2004.40036.x | pmid = 15233681 | url = http://www.acg.gi.org/physicians/guidelines/UlcerativeColitisUpdate.pdf | format = PDF | accessdate = 2009-11-07}}</ref> |
|||
|- |
|||
| Involvement around the [[anus]] || Common<ref name="HanauerCrohns">{{cite journal | last = Hanauer | first = Stephen B. | coauthors = William Sandborn | year = 2001 | month = March | date=2001-03-01 | title = Management of Crohn's disease in adults | journal=American Journal of Gastroenterology | volume = 96 | issue = 3 | pages = 635–43 | doi = 10.1111/j.1572-0241.2001.03671.x | pmid = 11280528 | url = http://www.acg.gi.org/physicians/guidelines/CrohnsDiseaseinAdults.pdf | format = PDF | accessdate = 2009-11-07}}</ref> |
|||
|| Seldom |
|||
|- |
|||
| Bile duct involvement || No increase in rate of [[primary sclerosing cholangitis]] || Higher rate<ref>{{cite journal | last = Broomé | first = Ulrika | coauthors = Annika Bergquist | year = 2006 | month = February | title = Primary sclerosing cholangitis, inflammatory bowel disease, and colon cancer | journal = Seminars in Liver Disease | volume = 26 | issue = 1 | pages = 31–41 | doi =10.1055/s-2006-933561 | pmid = 16496231 }}</ref> |
|||
|- |
|||
| Distribution of Disease || Patchy areas of inflammation (Skip lesions) || Continuous area of inflammation<ref name="Kornbluth-Sachar2004"/> |
|||
|- |
|||
| Endoscopy || Deep geographic and serpiginous (snake-like) [[Peptic ulcer|ulcers]] |
|||
|| Continuous ulcer |
|||
|- |
|||
| Depth of inflammation || May be transmural, deep into tissues<ref name=Baumgart/><ref name="HanauerCrohns"/> |
|||
|| Shallow, mucosal |
|||
|- |
|||
| [[Fistula]]e || Common<ref name="HanauerCrohns"/> |
|||
|| Seldom |
|||
|- |
|||
| [[Stenosis]] || Common || Seldom |
|||
|- |
|||
| [[Autoimmunity|Autoimmune disease]] || Widely regarded as an autoimmune disease || No consensus |
|||
|- |
|||
| [[Cytokine]] response || Associated with [[Th17|T<sub>h</sub>17]] <ref name=Elson2007/> || Vaguely associated with T<sub>h</sub>2 |
|||
|- |
|||
| [[Granuloma]]s on biopsy || May have non-[[necrosis|necrotizing]] non-peri-[[intestinal crypt]] granulomas<ref name="HanauerCrohns"/><ref name=pmid12147095>{{Cite journal | last1 = Shepherd | first1 = NA. | title = Granulomas in the diagnosis of intestinal Crohn's disease: a myth exploded? | journal = Histopathology | volume = 41 | issue = 2 | pages = 166-8 | month = Aug | year = 2002 | doi = | PMID = 12147095 }}</ref><ref name=pmid12121237 >{{Cite journal | last1 = Mahadeva | first1 = U. | last2 = Martin | first2 = JP. | last3 = Patel | first3 = NK. | last4 = Price | first4 = AB. | title = Granulomatous ulcerative colitis: a re-appraisal of the mucosal granuloma in the distinction of Crohn's disease from ulcerative colitis. | journal = Histopathology | volume = 41 | issue = 1 | pages = 50-5 | month = Jul | year = 2002 | doi = | PMID = 12121237 }}</ref> |
|||
|| Non-peri-[[intestinal crypt]] granulomas not seen<ref name="Kornbluth-Sachar2004"/> |
|||
|- |
|||
| Surgical cure || Often returns following removal of affected part || Usually cured by removal of colon |
|||
|- |
|||
| [[Tobacco smoking|Smoking]] || Higher risk for smokers || Lower risk for smokers<ref name="Kornbluth-Sachar2004"/> |
|||
|} |
|||
The Harvey–Bradshaw Index (HBI) provides a more streamlined approach by assessing only clinical factors, thus eliminating the need for laboratory tests. Neither the CDAI nor the HBI incorporates diagnostic procedures such as endoscopies or imaging studies; instead, they focus exclusively on symptom tracking. The HBI is generally considered easier to apply than the CDAI and may be more suitable for certain clinical trials and routine practice due to its simplicity in calculation and reduced reliance on patient recall of symptoms.<ref name="pmid32242028"/> |
|||
==Treatment== |
|||
{{Main|Treatment of Crohn's disease|Biological therapy for inflammatory bowel disease}} |
|||
Currently there is no cure for Crohn's disease and [[remission (medicine)|remission]] may not be possible or prolonged if achieved.<ref>{{cite web | url = http://www.ccfa.org/ccfaprof/research-grant-opps/documents/May-2007-Newsletter.pdf | format = PDF | title = Clinical Research Alliance Update | publisher = [[Crohn's and Colitis Foundation of America]] | date = 2007-05-01 | accessdate = 2008-02-14 }}</ref> In cases where remission is possible, [[relapse]] can be prevented and [[symptom]]s controlled with medication, lifestyle changes and in some cases, surgery. Adequately controlled, Crohn's disease may not significantly restrict daily living.<ref name = WebMD>{{cite web | url = http://www.webmd.com/digestive-disorders/features/crohns-disease-54-tips-to-help-you-manage?ecd=wnl_gid_120607 |title=Crohn's Disease: 54 Tips to Help You Manage | publisher = [[WebMD]] | last = Fries | first = WS | coauthor = Nazario, B | date = 2007-05-16 | accessdate = 2008-02-14 }}</ref> Treatment for Crohn's disease is only when symptoms are active and involve first treating the [[acute (medical)|acute]] problem, then maintaining [[remission (medicine)|remission]]. |
|||
The Crohn's Disease Endoscopic Index of Severity (CDEIS) is a scoring system used during endoscopy to evaluate Crohn's disease severity. It assesses six factors: deep and shallow ulcers, nonulcerated and ulcerated stenosis, the area covered by ulcers, and the overall disease-affected area across five intestinal sections. Scores range from 0 to 44, with higher scores indicating more severe disease. While often seen as the standard for measuring severity, CDEIS can be complex to calculate and may underestimate severity if only one segment, particularly the ileum, is affected. There are also no clear score cutoffs for specific outcomes or treatment responses, limiting its effectiveness in determining remission.<ref name="pmid27184635">{{cite journal | vauthors = Koutroumpakis E, Katsanos KH | title = Implementation of the simple endoscopic activity score in crohn's disease | journal = Saudi Journal of Gastroenterology | volume = 22 | issue = 3 | pages = 183–191 | pmid = 31367155 | pmc = 4898086 | date = May 2016 | doi = 10.4103/1319-3767.182455 | doi-access = free }}</ref> |
|||
===Medication=== |
|||
Acute treatment uses medications to treat any infection (normally [[antibiotic]]s) and to reduce inflammation (normally [[Aminosalicylic acid|aminosalicylate]] anti-inflammatory drugs and [[corticosteroid]]s). When symptoms are in remission, treatment enters maintenance with a goal of avoiding the recurrence of symptoms. Prolonged use of corticosteroids has significant [[Adverse effect (medicine)|side-effects]]; as a result they are generally not used for long-term treatment. Alternatives include aminosalicylates alone, though only a minority are able to maintain the treatment, and many require immunosuppressive drugs.<ref name="HanauerCrohns"/> |
|||
The Simple Endoscopic Score for Crohn's Disease (SES-CD) offers a more straightforward approach than the CDEIS scoring system, using four key factors to evaluate Crohn's disease during an endoscopy. These factors include the presence and size of ulcers, the area affected by ulcers, the overall extent of the disease, and any narrowing of the intestine (stenosis). The first three factors are scored from 0 to 3 in each of the five sections of the intestine, with a maximum score of 15 for each section. Stenosis is scored separately, ranging from 0 to 11. This results in a total SES-CD score that can range from 0 to 56, with higher scores indicating more severe disease.<ref name="pmid27184635"/> |
|||
Medications used to treat the symptoms of Crohn's disease include [[mesalazine|5-aminosalicylic acid]] (5-ASA) formulations, [[prednisone]], immunomodulators such as [[azathioprine]], [[mercaptopurine]], [[methotrexate]], [[infliximab]], [[adalimumab]]<ref name=Podolsky>{{Cite journal|last=Podolsky|first= Daniel K.|title=Inflammatory bowel disease|journal=New England Journal of Medicine|year=2002|volume=346|issue=6|pages=417–29 |
|||
|url=http://content.nejm.org/cgi/content/extract/347/6/417|accessdate=2006-07-02|pmid=12167685|doi=10.1056/NEJMra020831}}</ref>, [[certolizumab]]<ref> |
|||
{{cite press release |
|||
| url=www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116882.htm |
|||
| title=FDA Approves Cimzia to Treat Crohn's Disease |
|||
| publisher=[[Food and Drug Administration (United States)|Food and Drug Administration]] |
|||
| date=April 22, 2008 |
|||
| accessdate = 2009-11-04 |
|||
}}</ref> and [[natalizumab]].<ref name=Sandborn2005>{{cite journal | author = Sandborn, W.J. | coauthors = Colombel, J.F.; Enns, R.; Feagan, B.G.; Hanauer, S.B.; Lawrance, I.C.; Panaccione, R.; Sanders, M.; Schreiber, S.; Targan, S.; Others, | year = 2005 | title = Natalizumab Induction and Maintenance Therapy for Crohn's Disease | journal = New England Journal of Medicine | volume = 353 | issue = 18 | pages = 1912 | doi = 10.1056/NEJMoa043335 | pmid = 16267322 | last12 = Goldblum | first12 = R | last13 = Despain | first13 = D | last14 = Hogge | first14 = GS | last15 = Rutgeerts | first15 = P | last16 = International Efficacy Of Natalizumab As Active Crohn's Therapy (Enact-1) Trial | first16 = Group | last17 = Evaluation Of Natalizumab As Continuous Therapy (Enact-2) Trial | first17 = Group }}</ref><ref name=MacDonald2006>{{cite journal | author = MacDonald, J.K. | coauthors = McDonald, J.W.D. | year = 2006 | title = Natalizumab for induction of remission in Crohn's disease (Cochrane Review) | journal = The Cochrane Database of Systematic Reviews | pages = 1465–858 | url = http://dellboy.update-software.com/abstracts/AB006097.htm | accessdate = 2008-02-15 | doi = 10.1002/14651858.CD006097 | pmid = 16856112 | last1 = Macdonald | first1 = JK | last2 = Mcdonald | first2 = JW | volume = 3 | issue = }}</ref> [[Hydrocortisone]] should be used in severe attacks of Crohn's disease.<ref name="OHCM">{{cite book | last=Longmore | first=Murray | coauthors=Ian Wilkinson, Tom Turmezei, Chee Kay Cheung | title=Oxford Handbook of Clinicial Medicine, 7th edition | publisher=Oxford University Press | year=2007 | pages=266–7 | isbn=0-19-856837-1 }}</ref> |
|||
=== Laboratory testing === |
|||
Low doses of the opiate receptor antagonist [[Naltrexone]] (also [[Low dose naltrexone]]) have been found to be effective in inducing remission in 67% of patients with Crohn's disease in a small study conducted at Pennsylvania State University. Dr. Jill Smith, Professor of Gastroenterology at Pennsylvania State University's College of Medicine concluded that "LDN therapy appears effective and safe in subjects with active Crohn’s disease."<ref>*{{cite journal | author = Smith JP, Stock H, Bingaman S, Mauger D, Rogosnitzky M, Zagon IS | title = Low-dose naltrexone therapy improves active Crohn's disease. | journal = Am J Gastroenterol | pages = 820–8 | volume = 102 | issue = 4 | month = April | year = 2007 | pmid = 17222320 | doi = 10.1111/j.1572-0241.2007.01045.x}}</ref> Smith and her colleagues have since received a NIH grant and are proceeding with a definitive Phase II placebo-controlled [[clinical trial]]. |
|||
While no lab test can definitively confirm or rule out Crohn's disease, results from serum and stool tests can help support the diagnosis:<ref name="pmid28601423"/> |
|||
* The antimicrobial [[antibody]] [[Anti–Saccharomyces cerevisiae antibody|ASCA]] is a well-known blood test marker used in the diagnosis of Crohn's disease. Approximately 60–70% of individuals with Crohn's disease test positive for ASCA, while only 10–15% of those with ulcerative colitis and less than 5% of patients with other types of colitis have positive results.<ref name="pmid32242028"/> |
|||
*The [[autoantibody]] [[P-ANCA|pANCA]] is found in 10–15% of Crohn's disease cases, in 60–70% of ulcerative colitis cases, and in less than 5% of patients with other types of colitis that aren't inflammatory bowel disease. Additionally, patients with Crohn's disease who test positive for pANCA often show symptoms similar to those of ulcerative colitis.<ref name="pmid32242028"/> |
|||
*[[C-reactive protein]] (CRP) is a blood marker that indicates inflammation and can help monitor Crohn's disease activity. However, about one third of patients with active disease may have normal CRP levels, while one third with high levels of CRP have inactive disease. Moreover, CRP's ability to predict disease progression is not well established.<ref name="pmid32242028"/> |
|||
*[[Fecal calprotectin]] is a stool test used to differentiate inflammatory bowel disease, like Crohn's disease, from irritable bowel syndrome. While there are no official cut-off values, it is commonly used to assess disease activity in Crohn's.<ref name="pmid32242028"/> Elevated levels may also indicate other intestinal infections or inflammatory conditions, not just Crohn's disease.<ref name="pmid28601423"/> |
|||
=== Differential diagnosis === |
|||
===Lifestyle changes=== |
|||
Crohn's disease has similar endoscopic, radiographic and histological features with other inflammatory or infectious diseases. 10% of people with Crohn's disease are initially diagnosed with indeterminate colitis.<ref name="pmid32242028"/> |
|||
Certain lifestyle changes can reduce symptoms, including [[Diet (nutrition)|dietary]] adjustments, proper [[hydration]] and [[smoking cessation]]. Eating small meals frequently instead of big meals may also help with a low appetite. To manage symptoms have a balanced diet with proper portion control. [[Fatigue (medical)|Fatigue]] can be helped with regular exercise, a healthy diet and enough sleep. A [[food diary]] may help with identifying foods that trigger symptoms. Some patients should follow a low [[dietary fiber]] diet to control symptoms especially if fiberous foods cause symptoms.<ref name = WebMD/> |
|||
* [[Behçet’s disease]] can cause intestinal inflammation, primarily featuring single ulcers and symptoms outside the intestines, which differ from Crohn's disease. Recurrent sores in the mouth and genitals raise suspicion for Behçet's. A pathergy test, where the skin is lightly pricked to check for a red bump or ulcer, can help confirm the diagnosis. Eye inflammation (uveitis) and skin issues are also common in Behçet's disease.<ref name="pmid32242028"/> |
|||
* [[Intestinal lymphoma]] lacks symptoms that differentiate it from other conditions; diagnosis can only be confirmed through histological examination of tissue samples.<ref name="pmid32242028"/> |
|||
* [[Intestinal tuberculosis]] can cause symptoms such as fever, night sweats, and ulcers in the transverse colon, along with a swollen ileocecal valve. Key tissue changes include granulomas, which may be caseating, confluent, or large. A positive smear test for acid-fast bacillus and imaging that detects necrotic lymph nodes are also important indicators of the disease.<ref name="pmid32242028"/> |
|||
* [[Ischemic colitis]] is also a possible alternative diagnosis to Crohn's disease. It often shows swelling and redness of the inner lining of the colon, while the rectum usually remains unaffected.<ref name="pmid32242028"/> |
|||
=== |
=== Classification === |
||
The [[Montreal classification system]] is a widely used framework for categorizing the phenotypes of Crohn's disease. It considers three primary factors: the age at diagnosis (divided into three groups: less than 16 years, 17 to 40 years, and over 40 years), the location of the disease (which can be ileal, colonic, ileocolonic, or isolated upper), and the behavior of the disease (including non-stricturing/non-penetrating, stricturing, penetrating, and perianal types).<ref name="pmid38065612">{{cite journal | vauthors = Cockburn E, Kamal S, Chan A, Rao V, Liu T, Huang JY, Segal JP | title = Crohn's disease: an update | journal = Clinical Medicine (London) | volume = 23 | issue = 6 | pages = 549–557 | pmid = 38065612 | pmc = 11298500 | date = November 2023 | doi = 10.7861/clinmed.2023-0493 | doi-access = free }}</ref> |
|||
Crohn's cannot be cured by [[surgery]], though it is used when partial or a full blockage of the intestine occurs. Surgery may also be required for complications such as obstructions, fistulas and/or abscesses, or if the disease does not respond to drugs. After the first surgery, Crohn's usually shows up at the site of the resection though it can appear in other locations. After a resection, scar tissue builds up which can cause [[stenosis|stricture]]s. A stricture is when the intestines become too small to allow excrement to pass through easily which can lead to a blockage. After the first resection, another resection may be necessary within five years.<ref>{{cite web | url = http://ibdcrohns.about.com/od/surgeryprocedures/a/resectioncrohns.htm | title = Resection Surgery for Crohn's Disease | publisher = [[About.com]] | accessdate = 2008-02-14 | date = 2007-01-12 | last = Tresca | first = AJ }}</ref> For patients with an obstruction due to a stricture, two options for treatment are [[strictureplasty]] and resection of that portion of bowel. There is no [[statistical significance]] between strictureplasty alone versus strictureplasty and resection in cases of [[Duodenum|duodenal]] involvement. In these cases, re-operation rates were 31% and 27%, respectively, indicating that strictureplasty is a safe and effective treatment for selected patients with duodenal involvement.<ref name="pmid8918424">{{cite journal | author = Ozuner G, Fazio VW, Lavery IC, Milsom JW, Strong SA | title = Reoperative rates for Crohn's disease following strictureplasty. Long-term analysis | journal = Dis. Colon Rectum | volume = 39 | issue = 11 | pages = 1199–203 | year = 1996 | pmid = 8918424| doi = 10.1007/BF02055108}}</ref> |
|||
== Management == |
|||
[[Short bowel syndrome]] (SBS, also short gut syndrome or simply short gut) can be caused by the surgical removal of the small intestines. It usually develops if a person has had half or more of their small intestines removed.<ref>[http://digestive.niddk.nih.gov/ddiseases/pubs/shortbowel/ Short Bowel Syndrome] as defined by the [[National Institute of Diabetes and Digestive and Kidney Diseases]]</ref> Diarrhea is the main symptom of short bowel syndrome though other symptoms may include cramping, bloating and heartburn. Short bowel syndrome is treated with changes in diet, intravenous feeding, vitamin and mineral supplements and treatment with medications. Another complication following surgery for Crohn's disease where the terminal ileum has been removed is the development of excessive watery diarrhea. This is due to an inability to reabsorb bile acids after resection of the terminal ileum. {{Citation needed|date=March 2009}} |
|||
{{Main|Management of Crohn's disease}} |
|||
The management of Crohn's disease is customized based on the severity, location, and behavior of the disease. Providers also assess the risk of aggressive disease to determine the need for more intensive treatment. Risk factors include diagnosis before age 30, extensive disease involvement, perianal complications, deep ulcers, and history of surgery. A key goal of treatment is to achieve mucosal healing, which restores the intestinal lining. Mucosal healing is linked to better outcomes, such as fewer flare-ups, reduced hospitalizations, steroid-free remission, and a longer interval without surgery.<ref name="pmid32242028"/> |
|||
=== Corticosteroids === |
|||
In some cases of SBS, intestinal transplant surgery may be considered; though the number of transplant centres offering this procedure is quite small and it comes with a high risk due to the chance of infection and rejection of the transplanted intestine.<ref>{{cite web | url = http://www.revolutionhealth.com/conditions/digestive/crohns-disease/surgery/intestinal-transplant | title = Intestinal transplant for Crohn's disease | publisher [[revolutionhealth.com]] | accessdate = 2009-03-22 | date = 2006-10-24 | last = Rhodes | first = M }}</ref> |
|||
[[Corticosteroids|Steroids]] are often used to quickly induce remission and relieve symptoms in Crohn's disease, but they are ineffective for maintaining remission. Options include intravenous steroids, [[prednisone]], and [[budesonide]], with budesonide preferred for its safety, though it's limited to mild to moderate cases in the ileum and right colon. Patients on systemic steroids should switch to other medications for long-term remission, as prolonged use can cause adrenal issues, [[weight gain]], [[cataracts]], [[hypertension]], and [[Type 2 diabetes|diabetes]]. Additionally, systemic steroids may increase the risk of serious infections and mortality in moderate to severe Crohn's disease.<ref name="pmid27184635"/> |
|||
=== Conventional immunosuppressants === |
|||
===Prospective treatments=== |
|||
[[Thiopurine]]s, like [[azathioprine]] and [[6-mercaptopurine]], maintain remission in Crohn's disease but do not induce it initially. Since thiopurines take 6 to 12 weeks to work, steroids are often used to manage symptoms during this time. Before starting thiopurines, liver metabolism is assessed and [[Epstein-Barr]] virus is tested in patients under 25. Around 15% to 20% of patients stop thiopurines due to side effects, including low blood cell counts, liver problems, nausea, vomiting, allergic reactions, and acute pancreatitis. Thiopurines also raise the risk of certain cancers and serious conditions, necessitating regular lab monitoring.<ref name="pmid27184635"/> |
|||
Researchers at [[University College London]] have questioned the wisdom of suppressing the immune system in Crohn's, as the problem may be an under-active rather than an over-active immune system: their study found that Crohn's patients showed an abnormally low response to an introduced infection, marked by a poor flow of blood to the wound, and the response improved when the patients were given [[sildenafil|sildenafil citrate]].<ref name=Marks2006/> |
|||
[[Methotrexate]] is used to induce and maintain remission in Crohn's disease, being slightly more effective than thiopurines and taking 8 to 16 weeks to work. About 17% of patients stop taking it due to side effects like nausea, vomiting, headaches, and fatigue. It can affect liver health and, rarely, lower blood cell counts, requiring regular blood tests. Methotrexate may also cause anemia and mouth sores, so daily folic acid is recommended. Additionally, it may increase the risk of certain [[skin cancer]]s and [[lymphoma]]. Methotrexate is discontinued during pregnancy due to the risks of [[miscarriage]] and [[birth defect]]s.<ref name="pmid27184635"/> |
|||
Recent studies using [[helminthic therapy]] or [[hookworms]] to treat Crohn's Disease and other (non-viral) auto-immune diseases seem to yield promising results.<ref>{{cite journal |author=Croese J, O'neil J, Masson J, ''et al.'' |title=A proof of concept study establishing ''[[Necator americanus]]'' in Crohn's patients and reservoir donors |journal=Gut |volume=55 |issue=1 |pages=136–7 |year=2006 |pmid=16344586 |doi=10.1136/gut.2005.079129 |pmc=1856386}}</ref> |
|||
=== Biologics === |
|||
===Complementary and alternative medicine=== |
|||
[[TNF inhibitor|Anti-TNF therapy]] is the most effective treatment for inducing and maintaining remission, with FDA-approved agents including [[infliximab]], [[adalimumab]], and [[certolizumab pegol]].<ref name="pmid27184635"/> It blocks the inflammatory protein [[TNF]] and induces cell death in activated [[T cells]].<ref name="pmid26896086">{{cite journal | vauthors = Levin AD, Wildenberg ME, van den Brink GR | title = Mechanism of Action of Anti-TNF Therapy in Inflammatory Bowel Disease | journal = Journal of Crohn's and Colitis | volume = 10 | issue = 8 | pages = 989–997 | pmid = 29242771 | date = August 2016 | doi = 10.1093/ecco-jcc/jjw053 | doi-access = free | pmc = 5724577 }}</ref> Responses may occur within a week, but full effects can take up to six weeks. Loss of response can happen due to the development of [[Immunogenicity|antidrug antibodies]], necessitating a switch in agents or drug classes. Anti-TNF agents are often combined with thiopurines or methotrexate to minimize antibody development. Side effects include injection-site reactions, a higher risk of infection, a slight increase in melanoma risk, and rare cases of [[cytopenias]] and [[liver toxicity]].<ref name="pmid27184635"/> |
|||
More than half of Crohn's disease sufferers have tried complementary or alternative therapy.<ref>{{cite journal | author = Caprilli R, Gassull M, Escher J ''et al.'' | title = European evidence based consensus on the diagnosis and management of Crohn's disease: special situations | journal = Gut | volume = 55 Suppl 1 | issue = | pages = i36–58 | year = 2006| pmid = 16481630 | last12 = Hildebrand | first12 = H | last13 = Kolacek | first13 = S | last14 = Riis | first14 = L | last15 = Lukas | first15 = M | last16 = De Franchis | first16 = R | last17 = Hamilton | first17 = M | last18 = Jantschek | first18 = G | last19 = Michetti | first19 = P | last20 = O'morain | first20 = C | last21 = Anwar | first21 = MM | last22 = Freitas | first22 = JL | last23 = Mouzas | first23 = IA | last24 = Baert | first24 = F | last25 = Mitchell | first25 = R | last26 = Hawkey | first26 = CJ | last27 = European Crohn's And Colitis | first27 = Organisation | doi = 10.1136/gut.2005.081950c | pmc = 1859996}}</ref> These include diets, [[probiotics]], fish oil and other [[Herbalism|herbal]] and nutritional supplements. The benefit of these medications is uncertain. |
|||
[[Vedolizumab]] is the first treatment designed specifically for the gut in moderate to severe Crohn's disease. It blocks the molecule [[LPAM-1|α4β7]] that helps white blood cells enter the gut, reducing inflammation. Unlike [[natalizumab]], it does not carry a risk of the serious brain infection [[Progressive multifocal leukoencephalopathy|PML]]. While vedolizumab can induce remission, it works slowly, taking about 12 weeks to show effects, and its overall effectiveness is limited. However, patients who respond well can maintain remission for up to a year. Since it specifically targets the gut, it does not significantly increase the risk of serious side effects or infections, except for mild [[Sinusitis|nasal infections]].<ref name="pmid27184635"/> |
|||
*[[Acupuncture]] is used to treat inflammatory bowel disease in [[China]], and is being used more frequently in [[Western world|Western society]].<ref name=Joos>{{cite journal |author=Joos S, Brinkhaus B, Maluche C, ''et al.'' |title=Acupuncture and moxibustion in the treatment of active Crohn's disease: a randomized controlled study |journal=Digestion |volume=69 |issue=3 |pages=131–9 |year=2004 |pmid=15114043 |doi=10.1159/000078151}}</ref> However, there is little evidence that acupuncture has benefits beyond the [[placebo effect]], improving quality of life, general well-being and a small decrease in blood-bound inflammatory markers.<ref name = Joos/> |
|||
*[[Methotrexate]] is a [[folate]] anti-metabolite drug which is also used for [[chemotherapy]]. It is useful in maintenance of remission for those no longer taking corticosteroids.<ref>{{cite journal |author=Feagan BG, Fedorak RN, Irvine EJ, ''et al.'' |title=A comparison of methotrexate with placebo for the maintenance of remission in Crohn's disease. North American Crohn's Study Group Investigators |journal=N. Engl. J. Med. |volume=342 |issue=22 |pages=1627–32 |year=2000 |pmid=10833208 |doi=10.1056/NEJM200006013422202 |last12=Mcdonald |first12=JW}}</ref> |
|||
*[[Metronidazole]] and [[ciprofloxacin]] are antibiotics which are used to treat Crohn's that have colonic or perianal involvement, although, in the United States, this use has not been approved by the [[Food and Drug Administration]].<ref>{{cite journal |author=Ursing B, Alm T, Bárány F, ''et al.'' |title=A comparative study of metronidazole and sulfasalazine for active Crohn's disease: the cooperative Crohn's disease study in Sweden. II. Result |journal=Gastroenterology |volume=83 |issue=3 |pages=550–62 |year=1982 |pmid=6124474 |doi= |last12=Nordle |first12=O |last13=Rosén |first13=A}}</ref> They are also used for treatment of complications, including abscesses and other infections accompanying Crohn's disease.<ref name=emed/> |
|||
*[[Thalidomide]] has shown response in reversing [[endoscopy|endoscopic]] evidence of disease.<ref>{{cite journal |author=Cohen LB |title=Re: Disappearance of Crohn's ulcers in the terminal ileum after thalidomide therapy. Can J Gastroenterol 2004; 18(2): 101-104 |journal=Can. J. Gastroenterol. |volume=18 |issue=6 |pages=419; author reply 419 |year=2004 |pmid=15230268 |doi=}}</ref> |
|||
*[[Medical Cannabis|Cannabis]]-derived drugs may be used to treat Crohn's Disease with its anti-inflammatory properties. Cannabis-derived drugs may also help to heal the gut lining.<ref>[http://www.medicalnewstoday.com/articles/28584.php Cannabis-based drugs could offer new hope for inflammatory bowel disease patients]</ref> |
|||
*[[Soluble Fiber]] has been used by some to treat symptoms.^ a b c Tungland BC, Meyer D, Nondigestible oligo- and polysaccharides (dietary fiber): their physiology and role in human health and food, Comp Rev Food Sci Food Safety, 3:73-92, 2002 (Table 3)[1] |
|||
[[Ustekinumab]], approved for moderate to severe Crohn's disease in October 2016, has been FDA-approved for [[psoriasis]] since 2009.<ref name="pmid38877997">{{cite journal |vauthors=Gordon H, Minozzi S, Kopylov U, Verstockt B, Chaparro M, Buskens C, Warusavitarne J, Agrawal M, Allocca M, Atreya R, Battat R, Bettenworth D, Bislenghi G, Brown SR, Burisch J, Casanova MJ, Czuber-Dochan W, de Groof J, El-Hussuna A, Ellul P, Fidalgo C, Fiorino G, Gisbert JP, Sabino JG, Hanzel J, Holubar S, Iacucci M, Iqbal N, Kapizioni C, Karmiris K, Kobayashi T, Kotze PG, Luglio G, Maaser C, Moran G, Noor N, Papamichael K, Peros G, Reenaers C, Sica G, Sigall-Boneh R, Vavricka SR, Yanai H, Myrelid P, Adamina M, Raine T |title=ECCO Guidelines on Therapeutics in Crohn's Disease: Medical Treatment |journal=J Crohns Colitis |volume=18 |issue=10 |pages=1531–1555 |date=October 2024 |pmid=38877997 |doi=10.1093/ecco-jcc/jjae091 |url=}}</ref> It appears to be comparable to anti-TNF therapy in both the induction and maintenance of remission, functioning by blocking the inflammatory molecules [[interleukin-12|IL-12]] and [[interleukin-13|IL-23]]. The onset of action is similar to that of anti-TNF treatments, with responses typically observed within six weeks. Notably, Ustekinumab does not seem to increase the risk of serious infections, although the studies conducted in Crohn's disease have been relatively short-term.<ref name="pmid27184635"/> |
|||
==Prognosis== |
|||
{{Expand section|date=October 2009}} |
|||
Crohn's disease is a [[Chronic (medicine)|chronic]] condition for which there is currently no cure. It is characterised by periods of improvement followed by episodes when symptoms flare up. With treatment, most people achieve a healthy height and weight, and the mortality rate for the disease is relatively low. However, Crohn's disease is associated with an increased risk of small bowel and colorectal carcinoma, including bowel cancer.<ref name=Canavan>{{cite journal | last = Canavan | first = C. | coauthors = K. R. Abrams, J. Mayberry | year = 2006 | title = Meta-analysis : colorectal and small bowel cancer risk in patients with Crohn's disease | journal = Alimentary pharmacology & therapeutics | volume = 23 | issue = 8 | pages = 1097–104 | id = ISSN 0269-2813 | url = http://cat.inist.fr/?aModele=afficheN&cpsidt=17660183 | accessdate = 2007-05-23 | doi = 10.1111/j.1365-2036.2006.02854.x | pmid = 16611269 | last1 = Canavan | first1 = C | last2 = Abrams | first2 = KR | last3 = Mayberry | first3 = J }}</ref> |
|||
===[[Small molecule]]s=== |
|||
==Epidemiology== |
|||
The [[JAK inhibitor]] such as [[upadacitinib]] is approved for treatment of moderate to severe Crohn's disease, with a large multi-centre [[randomized control trial]] demonstrating its effectiveness in induction and maintenance of disease.<ref name=pmid38877997 /><ref name="pmid37224198">{{cite journal| author=Loftus EV, Panés J, Lacerda AP, Peyrin-Biroulet L, D'Haens G, Panaccione R | display-authors=etal| title=Upadacitinib Induction and Maintenance Therapy for Crohn's Disease. | journal=N Engl J Med | year= 2023 | volume= 388 | issue= 21 | pages= 1966–1980 | pmid=37224198 | doi=10.1056/NEJMoa2212728 | pmc= | hdl=2268/304716| url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=37224198 | hdl-access=free }} [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=37665995 Review in: Ann Intern Med. 2023 Sep;176(9):JC103. doi: 10.7326/J23-0069]</ref> |
|||
The incidence of Crohn's disease has been ascertained from population studies in [[Norway]] and the [[United States]] and is similar at 6 to 7.1:100,000.<ref name=Hiatt>{{cite journal | last = Hiatt | first = Robert A. | coauthors = Leon Kaufman | year = 1988 | title = Epidemiology of inflammatory bowel disease in a defined northern California population | journal = Western Journal of Medicine | volume = 149 | issue = 5 | pages = 541–6 | pmid = 3250100 | url = | accessdate = 2006-07-02 | pmc = 1026530 }}</ref><ref>{{cite journal | last = Moum | first = B. | coauthors =M. H. Vatn, A. Ekbom, E. Aadland, O. Fausa, I. Lygren, N. Stray, J. Sauar, T. Schulz | year = 1996 | title = Incidence of Crohn's disease in four counties in southeastern Norway, 1990-93. A prospective population-based study. The Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of Gastroenterologists | journal = Scandinavian Journal of Gastroenterology | volume = 31 | issue = 4 | pages = 355–61 | pmid = 8726303 | doi = 10.3109/00365529609006410 }}</ref> Crohn's disease is more common in northern countries, and shows a higher preponderance in northern areas of the same country.<ref>{{cite journal | last = Shivananda | first = S. | coauthors = J. Lennard-Jones, R. Logan, N. Fear, A. Price, L. Carpenter and M. van Blankenstein | year = 1996 | title = Incidence of inflammatory bowel disease across Europe: is there a difference between north and south? Results of the European Collaborative Study on Inflammatory Bowel Disease (EC-IBD) | journal = Gut | volume = 39 | issue = 5 | pages = 690–7 | pmid = 9014768 | doi = 10.1136/gut.39.5.690 | pmc = 1383393 }}</ref> The incidence of Crohn's disease is thought to be similar in [[Europe]] but lower in [[Asia]] and [[Africa]].<ref name=Hiatt/> It also has a higher incidence in [[Ashkenazi Jews]].<ref name=Podolsky/> |
|||
=== Surgery === |
|||
Crohn's disease has a [[bimodal distribution]] in [[incidence (epidemiology)|incidence]] as a function of age: the disease tends to strike people in their teens and 20s, and people in their 50s through to their 70s, and ages in between due to not being diagnosed with Crohn's and being diagnosed instead with [[irritable bowel syndrome]] (IBS).<ref name=Baumgart/><ref name=emed/> It is rarely diagnosed in early childhood. It usually strikes females who are pediatric patients more severely than males.<ref>{{cite web |url=http://www.ccfa.org/reuters/ibdboysgirls |title=Crohn's disease manifests differently in boys and girls |format= |work=CCFA.org |accessdate=}}</ref> However, only slightly more women than men have Crohn's disease.<ref>{{cite web |url=http://www.webmd.com/hw-popup/who-is-affected-by-crohns-disease |title=Who is affected by Crohn's disease |format= |work=WebMD.com |accessdate=}}</ref> Parents, siblings or children of people with Crohn's disease are 3 to 20 times more likely to develop the disease.<ref>{{cite journal |author=Satsangi J, Jewell DP, Bell JI |title=The genetics of inflammatory bowel disease |journal=Gut |volume=40 |issue=5 |pages=572–4 |year=1997 |pmid=9203931 |pmc=1027155 |doi= |url=http://gut.bmj.com/cgi/pmidlookup?view=long&pmid=9203931}}</ref> Twin studies show a concordance of greater than 55% for Crohn's disease.<ref>{{cite journal |author=Tysk C, Lindberg E, Järnerot G, Flodérus-Myrhed B |title=Ulcerative colitis and Crohn's disease in an unselected population of monozygotic and dizygotic twins. A study of heritability and the influence of smoking |journal=Gut |volume=29 |issue=7 |pages=990–6 |year=1988 |pmid=3396969 |pmc=1433769 |doi= 10.1136/gut.29.7.990|url=http://gut.bmj.com/cgi/pmidlookup?view=long&pmid=3396969}}</ref> |
|||
[[Image:ResectedIleum.jpg|thumb|right|Resected ileum from a person with Crohn's disease]] |
|||
Many individuals with Crohn's disease may require a [[bowel resection]] to remove part of the intestine due to blockages, lesions, infections, or ineffective medications. Since surgery is not a cure, the goal is to preserve as much of the small bowel as possible,<ref name="pmid27184635"/> and extensive resections can lead to [[short bowel syndrome]].<ref name="pmid34239262">{{cite journal | vauthors = Aksan A, Farrag K, Blumenstein I, Schröder O, Dignass AU, Stein J | title = Chronic intestinal failure and short bowel syndrome in Crohn's disease | journal = World Journal of Gastroenterology | volume = 27 | issue = 24 | pages = 3440–3465 | pmid = 34239262 | pmc = 8240052 | date = June 2021 | doi = 10.3748/wjg.v27.i24.3440 | doi-access = free }}</ref> In cases with widespread strictures, only the most prominent stricture is typically resected, while minor strictures may be dilated through [[strictureplasty]]. After a resection, the healthy ends of the intestine are rejoined in a primary [[surgical anastomosis|anastomosis]].<ref name="pmid27184635"/> |
|||
==History== |
|||
{{stub-sect|date=October 2009}} |
|||
Inflammatory bowel diseases were described by [[Giovanni Battista Morgagni]] (1682-1771), by Polish surgeon [[Antoni Leśniowski]] in 1904 (leading to the use of the eponym "'''Leśniowski-Crohn disease'''" in [[Poland]]) and by [[Scotland|Scottish]] physician T. Kennedy Dalziel in 1913.<ref>{{cite journal |author=Kirsner JB |title=Historical aspects of inflammatory bowel disease |journal=J. Clin. Gastroenterol. |volume=10 |issue=3 |pages=286–97 |year=1988 |pmid=2980764 |doi= 10.1097/00004836-198806000-00012|url=}}</ref> |
|||
Approximately six to twelve months after surgery, patients usually undergo a colonoscopy to check for inflammation, using the [[Rutgeerts scoring system]] to assess the likelihood of recurrence. About 50% may experience a return of symptoms within five years, and nearly 40% may need a second surgery within ten years,<ref name="pmid27184635"/> often due to inflammation near the anastomosis.<ref name="pmid21088749">{{cite journal | vauthors = Lewis RT, Maron DJ | title = Efficacy and complications of surgery for Crohn's disease | journal = Gastroenterology and Hepatology | volume = 6 | issue = 9 | pages = 587–596 | pmid = 21088749 | pmc = 2976865 | date = September 2010 }}</ref> While drug therapy aims to prevent recurrences, its effectiveness remains uncertain.<ref name="pmid27184635"/> |
|||
[[Burrill Bernard Crohn]], an American gastroenterologist at [[New York City]]'s [[Mount Sinai Hospital, New York|Mount Sinai Hospital]], described fourteen cases in 1932, and submitted them to the [[American Medical Association]] under the rubric of "Terminal ileitis: A new clinical entity". Later that year, he, along with colleagues Leon Ginzburg and Gordon Oppenheimer published the case series as "Regional ileitis: a pathologic and clinical entity".<ref name=CrohnBB/> |
|||
== |
=== Diet === |
||
* [[Enteral nutrition]], which administers nutrients as a powder or liquid, is the primary method for inducing remission in children with Crohn's disease. It can induce remission in up to 80% of cases. Outside of Japan, it is not used to treat Crohn's disease in adults due to unpalatable formulations.<ref name="pmid31540038">{{cite journal | vauthors = Di Caro S, Fragkos KC, Keetarut K, Koo HF, Sebepos-Rogers G, Saravanapavan H, Barragry J, Rogers J, Mehta SJ, Rahman F | title = Enteral Nutrition in Adult Crohn's Disease: Toward a Paradigm Shift | journal = Nutrients | volume = 11 | issue = 4 | pages = 2222 | doi = 10.3390/nu11092222 | pmid = 31540038 | pmc = 6770416 | date = September 2019 | doi-access = free }}</ref> |
|||
{{Reflist|2}} |
|||
* [[Parenteral nutrition]], which administers nutrients directly into the bloodstream, may be used to supply nutrients to patients when there is extensive inflammation that impairs absorption. Parenteral nutrition has the same effectiveness as enteral nutrition in inducing remission.<ref name="pmid31766687">{{cite journal | vauthors = Comeche JM, Comino I, Altavilla C, Tuells J, Gutierrez-Hervas A, Caballero P | title = Parenteral Nutrition in Patients with Inflammatory Bowel Disease Systematic Review, Meta-Analysis and Meta-Regression | journal = Nutrients | volume = 11 | issue = 12 | pages = 2865 | doi = 10.3390/nu11122865 | pmid = 31766687 | pmc = 6950216 | date = November 2019 | doi-access = free }}</ref> |
|||
* The [[Mediterranean diet]], rich in fruits, vegetables, unsaturated fats, and lean protein, is beneficial to general health but has not been found to reduce the rate of flares in Crohn's disease.<ref name="pmid38276922">{{cite journal | vauthors = Hashash JG, Elkins J, Lewis JD, Binion DG | title = AGA Clinical Practice Update on Diet and Nutritional Therapies in Patients With Inflammatory Bowel Disease: Expert Review | journal = Gastroenterology | volume = 166 | issue = 3 | pages = 521–532 | doi = 10.1053/j.gastro.2023.11.303 | pmid = 38276922 | date = January 2024 | doi-access = free }}</ref> |
|||
* Cooking and processing fruits and vegetables to reduce fibrousness increases tolerance of those foods in people with intestinal strictures.<ref name="pmid38276922"/> |
|||
=== Other treatments === |
|||
==External links== |
|||
* [[Mesalamine]] is not effective for inducing or maintaining remission in Crohn's disease, but is nevertheless commonly used as a treatment due to its perceived benefits and low risk of side effects.<ref name="pmid32242028"/> |
|||
{{DMOZ|/Health/Conditions_and_Diseases/Digestive_Disorders/Intestinal/Inflammatory_Bowel_Disease/Crohn%27s_Disease/}} |
|||
* [[Antibiotics]] are not effective in inducing or maintaining remission in Crohn's disease. However, they are effective in treating perianal fistulas and inflammation when used alongside anti-TNF therapy.<ref name="pmid32242028"/> |
|||
* [http://www.crohnsdiseaselibrary.org/ Crohn's Disease] |
|||
* [[Fecal microbiota transplants]] have shown potential effectiveness in preliminary studies. However, larger studies are needed to verify its efficacy.<ref name="pmid34169565">{{cite journal | vauthors = Fehily SR, Basnayake C, Wright EK, Kamm MA | title = Fecal microbiota transplantation therapy in Crohn's disease: Systematic review | journal = Journal of Gastroenterology and Hepatology | volume = 36 | issue = 10 | pages = 2672–2686 | doi = 10.1111/jgh.15598 | pmid = 34169565 | date = July 2021 | hdl = 11343/298722 }}</ref> |
|||
* [http://www.ccfa.org/ Crohn's & Colitis Foundation of America] |
|||
* [[Acupuncture]] influences the immune system by stimulating the [[vagus nerve]]. Early studies have shown efficacy in improving clinical symptoms, but larger studies are needed.<ref name="pmid30535303">{{cite journal | vauthors = Song G, Fiocchi C, Achkar JP | title = Acupuncture in Inflammatory Bowel Disease | journal = Inflammatory Bowel Diseases | volume = 25 | issue = 7 | pages = 1129–1139 | doi = 10.1093/ibd/izy371 | pmid = 30535303 | date = June 2019 }}</ref> |
|||
* [http://www.myibd.org/ The Foundation for Clinical Research in Inflammatory Bowel Disease] |
|||
* [[Cannabis]] is a potential therapy for Crohn's disease by targeting the endocannabinoid system. Although it has shown benefits in animal models, its efficacy as a treatment is uncertain.<ref>{{cite journal |vauthors=Kafil TS, Nguyen TM, MacDonald JK, Chande N |title=Cannabis for the treatment of Crohn's disease |journal=The Cochrane Database of Systematic Reviews |volume=11 |pages=CD012853 |date=November 2018 |issue=11 |pmid=30407616 |pmc=6517156 |doi=10.1002/14651858.CD012853.pub2}}</ref> |
|||
* [[Cognitive behavioral therapy]] has shown short-term positive psychological effects in people with Crohn's disease, but it has no long-term effect on physical or psychological health.<ref name="pmid34911469">{{cite journal | vauthors = Chen J, Chen X, Sun Y, Xie Y, Wang X, Li R, Hesketh T | title = The physiological and psychological effects of cognitive behavior therapy on patients with inflammatory bowel disease before COVID-19: a systematic review | journal = BMC Gastroenterology | volume = 21 | issue = 1 | pages = 469 | date = December 2021 | pmid = 34911469 | pmc = 8672154 | doi = 10.1186/s12876-021-02003-0| doi-access = free }}</ref> |
|||
== Outlook == |
|||
Crohn's disease is a chronic condition requiring ongoing management, as there is currently no cure. Inflammation is typically controlled through medications such as [[corticosteroids|steroids]] and [[immunosuppressants]], and in severe cases, [[bowel resection|surgery]] may be necessary. The clinical course of the disease is classified into four patterns:<ref name="pmid34456186">{{cite journal | vauthors = Cho CW, You MW, Oh CH, Lee CK, Moon SK | title = Long-term Disease Course of Crohn's Disease: Changes in Disease Location, Phenotype, Activities, and Predictive Factors | journal = Gut and Liver | volume = 16 | issue = 2 | pages = 157–170 | pmid = 34456186 | pmc = 8924800 | date = March 2022 | doi = 10.5009/gnl210118 | doi-access = free }}</ref> |
|||
* Remission: Severity decreases in response to treatment, leading to sustained remission.<ref name="pmid34456186"/> |
|||
* Improved and Stable: Severity lessens, but mild inflammation persists.<ref name="pmid34456186"/> |
|||
* Relapsing: The disease fluctuates between periods of remission and severe inflammation.<ref name="pmid34456186"/> |
|||
* Refractory: Severe inflammation continues without respite.<ref name="pmid34456186"/> |
|||
Approximately 40% to 56% of individuals with Crohn's disease achieve clinical remission after one year of [[infliximab]] treatment, increasing to 56% to 58% when combined with an immunosuppressant. Furthermore, 16% to 39% attain both clinical and endoscopic remission, showing no signs of inflammation in the intestine. Once in remission, individuals have an 80% chance of maintaining this state for the following year. Conversely, 10% to 15% of individuals may experience ongoing active disease without remission.<ref name="pmid34456186"/> |
|||
Chronic inflammation from Crohn's disease increases the risk of heart problems, [[cancer]]s, [[arthritis]], [[osteoporosis]] (weakened bones), and mental health issues. Some medications can also raise the chances of infections and cancers. Because of these combined risks, people with Crohn's disease tend to have a shorter lifespan compared to those who are healthy. In Canada, studies show that women affected with Crohn's disease live about 7.7 years less than unaffected women, and affected men live about 7.7 years less than otherwise expected.<ref name="pmid33168761">{{cite journal | vauthors = Kuenzig ME, Manuel DG, Donelle J, Benchimol EI | title = Life expectancy and health-adjusted life expectancy in people with inflammatory bowel disease Factors | journal = Canadian Medical Association Journal | volume = 192 | issue = 45 | pages = E1394–E1402 | pmid = 33168761 | pmc = 7669301 | date = November 2020 | doi = 10.1503/cmaj.190976 | doi-access = free }}</ref> |
|||
== Epidemiology == |
|||
Crohn's disease is most prevalent in [[North America]] and [[Western Europe]], particularly among [[Ashkenazi jew]]s and possibly more common in women.<ref name="pmid27184635"/> The annual incidence in North America is 0–20.2 new cases per 100,000 people, while incidence in Europe is 0.3–12.7 per 100,000. The prevalence of Crohn's disease is 322 per 100,000 in [[Germany]], 319 per 100,000 in [[Canada]],<ref name="pmid32242028"/> and 300 per 100,000 in the [[United States]].<ref name="pmid37223580">{{cite journal | vauthors = Weisman MH, Stens O, Kim SH, Hou JK, Miller FW, Dillon CF | title = Inflammatory Bowel Disease Prevalence: Surveillance data from the U.S. National Health and Nutrition Examination Survey | journal = Preventive Medicine Reports | volume = 9 | issue = 33 | pages = 102173 | date = March 2023 | pmid = 37223580 | pmc = 10201824 | doi = 10.1016/j.pmedr.2023.102173 | doi-access = free}}</ref> The prevalence of Crohn's disease has risen in newly industrialized countries, with rates of 18.6 per 100,000 in [[Hong Kong]] and 3.9 per 100,000 in [[Taiwan]].<ref name="pmid32242028"/> |
|||
The typical age of onset is between 20 and 30 years, with a smaller peak around 50 years, leading to a median onset age of 30.<ref name="pmid27184635"/> About 20 to 25% of patients presenting with [[inflammatory bowel disease]] are children under 18 years old, while 80% are adolescents. Additionally, the incidence of Crohn's disease in children is on the rise, with 2.5–11.4 new cases per 100,000 and a prevalence of 58 per 100,000.<ref name="pmid29487490">{{cite journal | vauthors = von Allmen D | title = ediatric Crohn's Disease | journal = Clinics in Colon and Rectal Surgery | volume = 31 | issue = 2 | pages = 80–88 | date = February 2018 | pmid = 29487490 | pmc = 5825885 | doi = 10.1055/s-0037-1609022 | doi-access = free}}</ref> |
|||
== History == |
|||
[[Giovanni Battista Morgagni]], often referred to as the father of [[anatomic pathology]], provided one of the earliest detailed accounts of the disease in his 1761 treatise, noting specific autopsy findings in a young patient who suffered from severe gastrointestinal symptoms.<ref name="pmid24094598">{{cite journal | vauthors = Mulder DJ, Noble AJ, Justinich CJ, Duffin JM | title = A tale of two diseases: the history of inflammatory bowel disease | journal = Journal of Crohn's and Colitis | volume = 8 | issue = 5 | pages = 341–348 | pmid = 24094598 | date = May 2014 | doi = 10.1016/j.crohns.2013.09.009 | doi-access = free }}</ref> |
|||
The first notable series of cases of Crohn's disease was reported by Polish surgeon [[Antoni Leśniowski]] in 1903,<ref name="pmid31701137">{{cite journal | vauthors = Van Hootegem P, Travis S | title = Is Crohn's Disease a Rightly Used Eponym? | journal = Journal of Crohn's and Colitis | volume = 14 | issue = 6 | pages = 867–871 | pmid = 31701137 | date = July 2020 | doi = 10.1093/ecco-jcc/jjz183 | doi-access = free }}</ref> followed by Scottish surgeon [[Thomas Kennedy Dalziel]] in 1913, who described nine patients exhibiting significant pathological features treated by [[bowel resection|surgical resection]]. However, the disease only gained widespread recognition with a landmark 1932 article by [[Burrill B. Crohn]], [[Leon Ginzburg]], and [[Gordon D. Oppenheimer]]. In this publication, they introduced the term "regional ileitis" based on their observations of chronic inflammation in the terminal [[ileum]] of 14 patients.<ref name="pmid24094598"/> |
|||
Over the following decades, Crohn's disease was recognized as affecting various parts of the gastrointestinal tract, with reports of involvement from the [[esophagus]] to the [[large intestine|colon]]. This period also marked the identification of skip lesions—areas of healthy bowel between diseased sections—adding to the understanding of the disease's pathology. Public awareness of Crohn's disease increased significantly after [[President Eisenhower]] underwent surgery for the condition in 1956, which highlighted its impact on quality of life and encouraged discussions about the disease.<ref name="pmid24094598"/> |
|||
In 1960, [[ulcerative colitis]] and Crohn's colitis were officially classified as distinct diseases, despite lingering beliefs that Crohn's disease could not manifest in the colon. During this decade, advancements such as [[fiberscope|fiberoptic]] [[colonoscopy]] and the capability to perform [[biopsies]] significantly enhanced the diagnosis and management of Crohn's disease, facilitating improved visualization of the gastrointestinal tract and more accurate assessments of disease severity. Subsequent decades saw the testing of various medications for Crohn's disease in clinical trials, including the identification of [[methotrexate]]'s efficacy in 1989.<ref name="pmid24094598"/> |
|||
In the 1990s, the focus of treatment for Crohn's disease began to shift towards [[biologics|biologic therapies]], particularly [[TNF inhibitor|anti-TNF agents]]. Concurrently, [[Clinical nutrition|nutritional therapy]] gained prominence in managing pediatric cases and instances of malnutrition. The introduction of [[Magnetic resonance enterography|MRI enterography]] emerged as a safe and effective method for monitoring disease activity. This was further augmented by the FDA's approval of [[capsule endoscopy]] in 2001, which allowed for improved imaging of the small intestine. Since the inception of [[genome-wide association studies]] in 2005, several genetic markers associated with Crohn's disease have been identified, contributing to a deeper understanding of the condition.<ref name="pmid24094598"/> |
|||
Support organizations such as the [[Crohn's & Colitis Foundation]] have also emerged, providing resources and community for patients, helping to raise awareness and funding for research initiatives.<ref name="pmid24094598"/> Today, Crohn's disease continues to be a focus of extensive research, aiming to improve treatment outcomes and enhance the quality of life for those affected.<ref name="pmid24094598"/> |
|||
=== Etymology === |
|||
Crohn's disease is named after Dr. Burrill Crohn, though its eponymous association arose from complex circumstances. Initially, researchers Ginzburg and Oppenheimer identified a pattern of the disease and compiled 12 cases, all linked to surgeon A. A. Berg. However, Berg declined authorship due to his lack of prior involvement. Ginzburg and Oppenheimer then connected with Crohn, who received the manuscript, which was later published with his name listed first and two additional cases included.<ref name="pmid24094598"/> |
|||
Originally, the disease was referred to as "regional ileitis," reflecting the findings of the time, but subsequent reports revealed its presence throughout the gastrointestinal tract, leading to the adoption of the eponym.<ref name="pmid24094598"/> In Poland, it was historically called “Lesniowski-Crohn's disease.”<ref name="pmid31701137"/> There has been growing criticism of medical eponyms for their inaccuracies, prompting a movement towards using non-possessive forms, such as "Crohn disease," which has gained traction in recent years among academic and medical publications.<ref name="pmid24094598"/> |
|||
== References == |
|||
{{Reflist}} |
|||
== Further reading == |
|||
* {{cite journal |vauthors=Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE |title=ACG Clinical Guideline: Management of Crohn's Disease in Adults |journal=Am. J. Gastroenterol. |volume=113 |issue=4 |pages=481–517 |date=April 2018 |pmid=29610508 |doi=10.1038/ajg.2018.27 |doi-access=free}} |
|||
== External links == |
|||
* {{cite web |url=https://medlineplus.gov/crohnsdisease.html |publisher=U.S. National Library of Medicine |work=MedlinePlus |title=Crohn's disease}} |
|||
*{{commons category-inline}} |
|||
{{Medical condition classification and resources |
|||
| ICD11 = {{ICD11|DD70}} |
|||
| ICD10 = {{ICD10|K50}} |
|||
| ICD9 = {{ICD9|555}} |
|||
| ICDO = |
|||
| OMIM = 266600 |
|||
| MeshID = D003424 |
|||
| DiseasesDB = 3178 |
|||
| MedlinePlus = 000249 |
|||
| eMedicineSubj = med |
|||
| eMedicineTopic = 477 |
|||
| eMedicine_mult = {{eMedicine2|ped|507}} {{eMedicine2|radio|197}} |
|||
}} |
|||
{{Crohn's}} |
{{Crohn's}} |
||
{{Gastroenterology}} |
{{Gastroenterology}} |
||
{{Oral pathology}} |
|||
{{Solute carrier disorders}} |
|||
{{Portal bar | Medicine | Viruses}} |
|||
{{Authority control}} |
|||
{{Good article}} |
|||
{{DEFAULTSORT:Crohn's Disease}} |
{{DEFAULTSORT:Crohn's Disease}} |
||
[[Category:Abdominal pain]] |
|||
[[Category:Articles containing video clips]] |
|||
[[Category:Autoimmune diseases]] |
[[Category:Autoimmune diseases]] |
||
[[Category:Digestive diseases]] |
|||
[[Category:Gastroenterology]] |
|||
[[Category:Genetic disorders]] |
|||
[[Category:Inflammations]] |
[[Category:Inflammations]] |
||
[[Category: |
[[Category:Membrane transport protein disorders]] |
||
[[Category: |
[[Category:Noninfective enteritis and colitis]] |
||
[[Category:Wikipedia medicine articles ready to translate]] |
|||
[[Category:Wikipedia emergency medicine articles ready to translate]] |
|||
[[ar:داء كرون]] |
|||
[[Category:Steroid-responsive inflammatory conditions]] |
|||
[[ca:Malaltia de Crohn]] |
|||
[[ |
[[Category:Crohn's disease]] |
||
[[da:Crohns sygdom]] |
|||
[[de:Morbus Crohn]] |
|||
[[es:Enfermedad de Crohn]] |
|||
[[eo:Crohn-malsano]] |
|||
[[eu:Crohn gaitza]] |
|||
[[fr:Maladie de Crohn]] |
|||
[[fy:Sykte fan Crohn]] |
|||
[[gl:Mal de Crohn]] |
|||
[[hr:Crohnova bolest]] |
|||
[[it:Malattia di Crohn]] |
|||
[[he:מחלת קרוהן]] |
|||
[[hu:Crohn-betegség]] |
|||
[[nl:Ziekte van Crohn]] |
|||
[[ja:クローン病]] |
|||
[[no:Crohns sykdom]] |
|||
[[pl:Choroba Leśniowskiego-Crohna]] |
|||
[[pt:Doença de Crohn]] |
|||
[[ru:Болезнь Крона]] |
|||
[[simple:Crohn's disease]] |
|||
[[sk:Crohnova choroba]] |
|||
[[sl:Crohnova bolezen]] |
|||
[[sr:Кронова болест]] |
|||
[[fi:Crohnin tauti]] |
|||
[[sv:Crohns sjukdom]] |
|||
[[tr:Crohn hastalığı]] |
|||
[[zh:克隆氏症]] |
|||
Latest revision as of 12:13, 10 December 2024
Crohn's disease is a chronic inflammatory bowel disease characterized by recurrent episodes of intestinal inflammation, primarily manifesting as diarrhea and abdominal pain. Unlike ulcerative colitis, inflammation can occur anywhere in the gastrointestinal tract, though it most frequently affects the ileum and colon, involving all layers of the intestinal wall. Symptoms may be non-specific and progress gradually, often delaying diagnosis. About one-third of patients have colonic disease, another third have ileocolic disease, and the remaining third have isolated ileal disease. Systemic symptoms such as chronic fatigue, weight loss, and low-grade fevers are common. Organs such as the skin and joints can also be affected. Complications can include bowel obstructions, fistulas, nutrition problems, and an increased risk of intestinal cancers.[1]
Crohn's disease is influenced by genetic, environmental, and immunological factors. Smoking is a major modifiable risk factor, especially in Western countries, where it doubles the likelihood of developing the disease. Dietary shifts from high-fiber to processed foods may reduce microbiota diversity and increase risk, while high-fiber diets can offer some protection. Genetic predisposition plays a significant role, with first-degree relatives facing a five-fold increased risk, particularly due to mutations in genes like NOD2 that affect immune response. The condition results from a dysregulated immune response to gut bacteria and increased intestinal permeability, alongside changes in the gut microbiome.[1]
Diagnosing Crohn's disease can be complex due to symptom overlap with other gastrointestinal disorders. It typically involves a combination of clinical history, physical examination, and various diagnostic tests. Key methods include ileocolonoscopy, which identifies the disease in about 90% of cases, and imaging techniques like CT and MRI enterography, which help assess the extent of the disease and its complications. Histological examination of biopsy samples is the most reliable method for confirming diagnosis.[1]
Management of Crohn's disease is individualized, focusing on disease severity and location to achieve mucosal healing and improve long-term outcomes. Treatment may include corticosteroids for quick symptom relief, immunosuppressants for maintaining remission, and biologics like anti-TNF therapies, which are effective for both induction and maintenance. Surgery may be necessary for complications such as blockages. Despite ongoing treatment, Crohn's disease is a chronic condition with no cure, often leading to a higher risk of related health issues and reduced life expectancy.[1]
The disease is most prevalent in North America and Western Europe, particularly among Ashkenazi Jews, with prevalence rates of 322 per 100,000 in Germany, 319 in Canada,[1] and 300 in the United States.[5] There is also a rising prevalence in newly industrialized countries, such as 18.6 per 100,000 in Hong Kong and 3.9 in Taiwan. The typical age of onset is between 20 and 30 years, with an increasing number of cases among children.[1]
Signs and symptoms
[edit]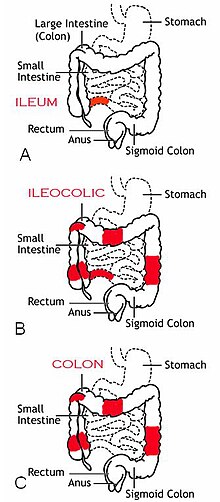
Crohn's disease is characterized by recurring flares of intestinal inflammation, with diarrhea and abdominal pain as the primary symptoms. Symptoms may be non-specific and progress gradually, and many people have symptoms for years before diagnosis. Unlike ulcerative colitis, inflammation can occur anywhere in the gastrointestinal tract, most often in the ileum and colon, and can involve all layers of the intestine. Disease location tends to be stable, with a third of patients having colonic disease, a third having ileocolic disease, and a third having ileal disease. The disease may also involve perianal, upper gastrointestinal, and extraintestinal organs.[1]
Gastrointestinal
[edit]- Diarrhea affects 82% of people at the onset of Crohn's disease, with severity ranging from mild to severe enough to require substitution of water and electrolytes. With Crohn's disease, diarrhea is frequent and urgent rather than voluminous.[6]
- Abdominal pain affects at least 70% of people during the course of Crohn's disease. It can result directly from intestinal inflammation, or from complications such as strictures and fistulas.[7] Pain most commonly occurs in the lower right abdomen.[8]
- Rectal bleeding is less common than in ulcerative colitis, and is more likely to occur with inflammation in the colon or rectum. Bleeding in the colon or rectum is bright red, whereas bleeding in higher segments causes dark or black stools.[9]
- Bloating, flatus, and other symptoms of irritable bowel syndrome occur in 41% of people in remission.[10]
- Perianal involvement occurs in 18–43% of cases, more frequently if the colon and rectum are inflamed, and can cause fistulas, skin tags, hemorrhoids, fissures, ulcers, and strictures.[11]
- Upper gastrointestinal involvement is rare, occurring in 0.5-16% of cases, and may cause symptoms such as pain while swallowing, difficulty swallowing, vomiting, and nausea.[12]
Systemic
[edit]Crohn's disease often presents with systemic symptoms, including:
- Chronic fatigue, which lasts for at least 6 months and cannot be cured by rest, occurs in 80% of people with Crohn's disease, including 30% of people who are in remission.[13]
- Fevers, typically low-grade, are often reported as initial symptoms of Crohn's disease. High-grade fevers are often a result of abscesses.[14]
- Weight loss often occurs due to diarrhea and reduced appetite.[14]
Extraintestinal
[edit]Extraintestinal manifestations occur in 21–47% of cases, and include symptoms such as:[1]
- Mouth ulcers, such as canker sores.[15]
- Eye inflammation, such as uveitis, scleritis, and episcleritis.[1]
- Skin inflammation, such as erythema nodosum and pyoderma gangrenosum.[1]
- Blood conditions such as portal hypertension, thromboembolism, thrombosis, pulmonary embolism.[1]
- Joint inflammation such as arthritis, ankylosing spondylitis, sacroiliitis.[1]
- Respiratory conditions such as obstructive sleep apnea and chest infections.[1]
- Liver, bile duct, and gallbladder conditions such as primary sclerosing cholangitis and cirrhosis.[1]
- Mental disorders such as depression and anxiety.[16]
- Metabolic bone disease.[1]
Complications
[edit]
Bowel damage due to inflammation occurs in half of cases within 10 years of diagnosis, and can lead to stricturing or penetrating disease forms. This can cause complications such as:
- Bowel obstructions may occur due to strictures, particularly in the small intestine, and may require surgical removal of the affected segment (bowel resection) or surgical dilation (stricturoplasty).[2]
- Fistulas, openings in the gut, result from penetrating disease and can cause diarrhea, urinary tract infections, and stool leakage to the vagina or skin. It is treated by bowel resection or fistulotomy[2]
- Abscesses, infected pockets, can also result from penetrating disease, causing abdominal pain, fever, and chills. It may be treated by surgical drainage.[2]
Malnutrition occurs in 38.9% of people in remission and 82.8% of people with active disease due to malabsorption in the small intestine, reduced appetite, and drug interactions.[17] This can cause complications such as:
- Anemia occurs in 6–74% of cases as a result of iron deficiency and blood loss. It is treated by oral iron or intravenous iron depending on disease activity.[17]
- Vitamin D deficiency is prevalent and can cause osteoporosis, and is treated by oral supplementation.[17]
- Folic acid, vitamin B12, zinc, magnesium, and selenium deficiencies may also occur, and are treated through oral supplementation.[17]
- Impaired growth and nutritional deficiency occur in 65–85% of children with Crohn's disease.[18]
Intestinal cancers may develop as a result of prolonged or severe inflammation.[19] This includes:
- Colorectal cancer has a prevalence of 7% at 30 years after diagnosis and accounts for 15% of deaths in people with Crohn's. Risk is higher if the disease occurs in most of the colon. Endoscopic surveillance is performed to detect and remove polyps, while surgery is required for dysplasia beyond the mucosal surface.[19]
- Small bowel cancer has a prevalence of 1.6%, at least 12-times greater in people with Crohn's disease. Unlike colorectal cancer, endoscopic surveillance is ineffective and not recommended for small bowel cancer.[20]
Causes
[edit]Risk factors
[edit]Smoking is a major modifiable risk factor for Crohn's disease, particularly in Western countries, where it doubles the risk. This risk is higher in females and varies with age. Smoking is also linked to earlier disease onset, increased need for immunosuppression, more surgeries, and higher recurrence rates. Ethnic differences have been noted, with studies in Japan linking passive smoking to the disease.[1] Proposed mechanisms for smoking's effects include impaired autophagy, direct toxicity to immune cells, and changes in the microbiome.[3]
Diet may influence the development of Crohn's disease by affecting the gut microbiome. The shift from high-fiber, low-fat foods to processed foods reduces microbiota diversity, increasing the risk of Crohn's disease.[1] Conversely, high-fiber diets may reduce risk by up to 40%, likely due to the production of anti-inflammatory short-chain fatty acids from fiber metabolism by gut bacteria.[3] The Mediterranean diet is also linked to a lower risk of later-onset Crohn's disease. Since diet's effect on the microbiome is temporary, its role in gut dysbiosis is controversial.[1]
Childhood antibiotic exposure is linked to a higher risk of Crohn's disease due to changes in the intestinal microbiome, which shapes the immune system in early life. Other medications, like oral contraceptives, aspirin, and NSAIDs, may also increase risk by up to two-fold. Conversely, breastfeeding and statin use may reduce risk, though breastfeeding's effects are inconsistent. Early life factors such as mode of delivery, pet exposure, and infections—related to the hygiene hypothesis—also significantly influence risk, likely due to influences on the microbiome.[3]
Genetics
[edit]Genetics significantly influences the risk of Crohn's disease. First-degree relatives of affected individuals have a five-fold increased risk, while identical twins have a 38–50% risk if one twin is affected. Genome-wide association studies have identified around 200 loci linked to Crohn's, most found in non-coding regions that regulate gene expression and overlap with other immune-related conditions, such as ankylosing spondylitis and psoriasis.[3] While genetics can predict disease location, it does not determine complications like stricturing. A substantial portion of inherited risk is attributed to a few key polymorphisms.[1]
- NOD2 mutations are the primary genetic risk factor for ileal Crohn's disease, impairing the function of immune cells, particularly Paneth cells. These mutations are found in 10–27% of individuals with Crohn's disease, predominantly in Caucasian populations. Heterozygotes (one mutated copy) have a three-fold risk, while homozygotes (two copies) have a 20–40 fold risk.[21]
- ATG16L1 mutations impair autophagy and immune defense, and are more common in Caucasians.[1]
- IL23R mutations increase inflammatory signaling of the interleukin-23 pathway, and are more common in Caucasians.[1]
- TNFSF15 mutations are the primary genetic risk factor in Asian populations.[1]
- IL10RA mutations impair the anti-inflammatory signaling of interleukin-10, causing early-onset Crohn's disease with high penetrance.
Mechanism
[edit]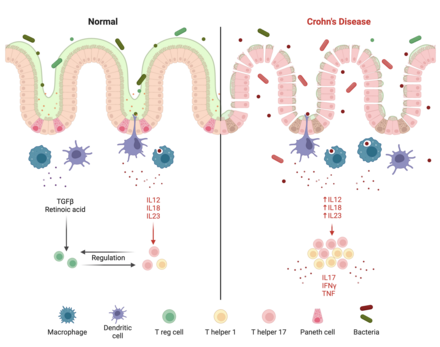
Crohn's disease is believed to be caused by a dysregulated immune response to gut bacteria, though the exact mechanism is unknown. This is evidenced by the disease's links to genes involved in bacteria defense and its occurrence in the ileum and colon, the most bacteria-dense segments of the intestine.[23] In Crohn's disease, a permeable intestinal barrier and a deficient innate immune response enable bacteria to enter intestinal tissue, causing an excessive inflammatory response from T helper 1 (Th1) and T helper 17 (Th17) cells. An altered microbiome may also be causatory and serve as the link to environmental factors.[3]
Intestinal barrier
[edit]The epithelial barrier is a single layer of epithelial cells covered in antimicrobial mucus that protects the intestine from gut bacteria.[23] Epithelial cells are joined by tight junction proteins, which are reduced by Crohn's-linked polymorphisms. In particular, claudin-5 and claudin-8 are reduced, while pore-forming claudin-2 is increased, causing intestinal permeability. Epithelial cells under stress emit inflammatory signals such as the unfolded protein response to stimulate the immune system, and Crohn's-linked polymorphisms to the ATG16L1 gene lower the threshold at which this response is triggered.[1]
In a functional state, the intestinal epithelium and IgA dimers work together to manage and keep the luminal microflora distinct from the mucosal immune system.[24] Paneth cells exist in the epithelial barrier of the small intestine and secrete α-defensins to prevent bacteria from entering gut tissue.[23] Genetic polymorphisms associated with Crohn's disease can impair this ability and lead to Crohn's disease in the ileum. NOD2 is a receptor produced by Paneth cells to sense bacteria, and mutations to NOD2 can inhibit the antimicrobial activity of Paneth cells. ATG16L1, IRGM, and LRRK2 are proteins involved in selective autophagy, the mechanism by which Paneth cells secrete α-defensins, and mutations to these genes also impair the antimicrobial activity of Paneth cells.[1]
Intraepithelial lymphocytes (IELs) are immune cells that exist in the epithelial barrier, consisting mostly of activated T cells. They interact with gut bacteria directly and emit signals to regulate the intestinal immune system. IELs in Crohn's disease produce increased levels of inflammatory cytokines IL-17, IFNγ, and TNF.[1] It is hypothesized that inflammatory signals from the immune system and alterations to the gut microbiome influence IELs to produce inflammatory signals, contributing to Crohn's disease.[25]
Immune system
[edit]Normally, intestinal macrophages have reduced inflammatory behavior while retaining their ability to consume and destroy pathogens. In Crohn's disease, the number and activity of macrophages is reduced, enabling the entrance of pathogens into intestinal tissue.[3] Macrophages degrade internal pathogens through autophagy, which is impaired by Crohn's-linked polymorphisms in genes such as NOD2 and ATG16L1.[1] Additionally, people with Crohn's tend to have a separate abnormal population of macrophages that secrete proinflammatory cytokines such as TNF and IL-6.[3]
Neutrophils are recruited from the bloodstream in response to inflammatory signals, and defend tissue by secreting antimicrobial substances and consuming pathogens.[23] In Crohn's disease, neutrophil recruitment is delayed and autophagy is impaired, allowing bacteria to survive in intestinal tissue.[3] Dysfunction in neutrophil secretion of reactive oxygen species, which are toxic to bacteria, is associated with very early onset Crohn's disease. Although neutrophils are important in bacterial defense, their subsequent accumulation in Crohn's disease damages the epithelial barrier and perpetuates inflammation.[1]
Innate lymphoid cells (ILCs) consist of subtypes including ILC1s, ILC2s, and ILC3s. ILC3s are particularly important for regenerating the epithelial barrier through secretion of IL-17 by NCR- ILC3s and IL-22 by NCR+ ILC3s. During Crohn's disease, inflammatory signals from antigen-presenting cells, such as IL-23, cause excessive IL-17 and IL-22 secretion. Although these cytokines protect the intestinal barrier, excessive production damages the barrier through increased inflammation and neutrophil recruitment. Additionally, IL-12 from activated dendritic cells influence NCR+ ILC3s to transform into inflammatory IFNγ-producing ILC1s.[26]
Naive T cells are activated primarily by dendritic cells, which then differentiate into anti-inflammatory T regulatory cells (Tregs) or inflammatory T helper cells to maintain balance. In Crohn's disease, macrophages and antigen-presenting cells secrete IL-12, IL-18, and IL-23 in response to pathogens, increasing Th1 and T17 differentiation and promoting inflammation via IL-17, IFNγ and TNF. IL-23 is particularly important, and IL-23 receptor polymorphisms that increase activity are linked with Crohn's disease. Tregs suppress inflammation via IL-10, and mutations to IL-10 and its receptor cause very early onset Crohn's disease.[1]
Microbiome
[edit]People with Crohn's disease tend to have altered microbiomes, although no disease-specific microorganisms have been identified. An altered microbiome may link environmental factors with Crohn's, though causality is uncertain. Firmicutes tend to be reduced, particularly Faecalibacterium prausnitzii, which produces short-chain fatty acids that reduce inflammation. Bacteroidetes and proteobacteria tend to be increased, particularly adherent-invasive E. coli, which attaches to intestinal epithelial cells. Additionally, mucolytic and sulfate-reducing bacteria are elevated, contributing to damage to the intestinal barrier.[3]
Alterations in gut viral and fungal communities may contribute to Crohn's disease. Caudovirales bacteriophage sequences found in children with Crohn's suggest a potential biomarker for early-onset disease. A meta-analysis showed lower viral diversity in Crohn's patients compared to healthy individuals, with increased Synechococcus phage S CBS1 and Retroviridae viruses. Additionally, a Japanese study found that the fungal microbiota in Crohn's patients differs significantly from that of healthy individuals, particularly with an abundance of Candida.[1]
Diagnosis
[edit]Diagnosis of Crohn's disease may be challenging since its symptoms overlap with other gastrointestinal diseases. An accurate diagnosis requires a combined assessment of clinical history, physical examination, and diagnostic tests.
Endoscopy
[edit]

Ileocolonoscopy is the primary procedure for diagnosing Crohn's disease in the ileum and colon, accurately identifying it in about 90% of cases.[27] During this exam, doctors closely examine the intestinal lining and take small tissue samples for further testing. Signs of Crohn's disease include uneven inflammation and 'skip lesions', which are patches of inflammation separated by healthy tissue. The ulcers can be small (less than 5 mm) or larger (over 5 mm), often appearing cobblestone-like. Their depth helps determine disease severity. Unlike ulcerative colitis, Crohn's disease usually does not affect the rectum or cause continuous inflammation around the bowel.[1]
In certain cases, such as disease in the upper small bowel, standard colonoscopy may be ineffective. Physicians may then opt for device-assisted enteroscopy or capsule endoscopy. While capsule endoscopy is effective in detecting abnormalities, it may not reliably diagnose Crohn's disease and carries a risk of retention, which is about 1.6% when Crohn's disease is suspected and increases to 13% if already diagnosed. To reduce this risk, physicians typically perform small-bowel imaging and use a patency capsule that disintegrates within 48 to 72 hours. Once the patency capsule has passed through the intestine, capsule endoscopy may be performed.[2]
Device-assisted enteroscopy is not typically the first choice for diagnosing small-bowel Crohn's disease due to its invasiveness and higher costs.[1] The procedure closely examines the small intestine using specialized tools, such as longer endoscopes or balloon-assisted devices, making it easier for doctors to visualize and treat issues.[28] It often requires sedation and is generally reserved for patients needing a tissue sample or immediate treatment.[1]
Cross-sectional Imaging
[edit]
Cross-sectional imaging techniques, like bowel ultrasonography (BUS), CT enterography (CTE), and MRI enterography (MRE), are essential for understanding how extensive Crohn's disease is and whether there are any complications, like blockages or abnormal connections between organs. All three methods are quite accurate for diagnosing Crohn's disease and spotting these complications.[1]
- CTE involves radiation and requires the use of contrast agents (substances that help show details in images). Despite this, CTE is very effective, with over 80% accuracy in diagnosing the disease and its complications, including blockages and fistulas (abnormal connections).[1]
- MRE is particularly good for detecting intestinal narrowing, with 89% sensitivity and 94% specificity. It is the preferred option for examining fistulas and abscesses in the pelvic area.[1]
- BUS is a non-invasive method that doesn't involve radiation and is effective for assessing the intestinal wall and related issues, such as fistulas and abscesses. Despite its limitations, it can accurately identify signs of Crohn's disease when the bowel wall thickens to more than 3 mm, achieving high accuracy rates (88–100%) when also considering factors like fistulas and abscesses.[1]
Histology
[edit]
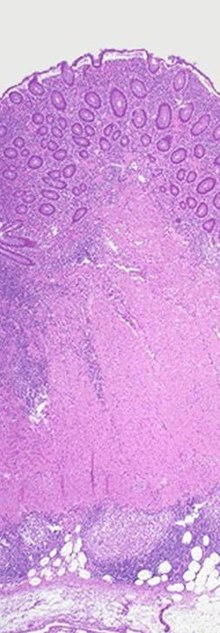
The most reliable way to confirm a diagnosis of Crohn's disease is through a histological examination of biopsy samples or tissue removed during surgery. This process helps distinguish Crohn's disease from ulcerative colitis and other types of colitis, particularly infections. While no features are unique to Crohn's disease, typical signs include patchy chronic inflammation, irregularities in the intestinal lining, granulomas (not related to tissue injury), and abnormal villi structure in the terminal ileum. A pathologist specializing in inflammatory bowel disease is important for accurate Crohn's disease diagnoses. Even if biopsy results are unclear, doctors can still suggest a Crohn's disease diagnosis based on clinical symptoms, endoscopic findings, and imaging results.[1]
Disease activity indexes
[edit]The Crohn's Disease Activity Index (CDAI) is a scoring system to assess the symptoms associated with Crohn's disease. It assigns a score based on eight clinical factors, including overall well-being, frequency of loose stools, abdominal pain, presence of abdominal masses, changes in weight, low hemoglobin levels, and use of opiates for diarrhea. The CDAI is primarily used in clinical trials to evaluate the effectiveness of treatments and to determine whether the disease is in remission. This is particularly significant, as approximately 50% of patients who report feeling well may still exhibit signs of active disease in the intestine, while some patients with symptoms may present with normal intestinal findings.[1]
The Harvey–Bradshaw Index (HBI) provides a more streamlined approach by assessing only clinical factors, thus eliminating the need for laboratory tests. Neither the CDAI nor the HBI incorporates diagnostic procedures such as endoscopies or imaging studies; instead, they focus exclusively on symptom tracking. The HBI is generally considered easier to apply than the CDAI and may be more suitable for certain clinical trials and routine practice due to its simplicity in calculation and reduced reliance on patient recall of symptoms.[1]
The Crohn's Disease Endoscopic Index of Severity (CDEIS) is a scoring system used during endoscopy to evaluate Crohn's disease severity. It assesses six factors: deep and shallow ulcers, nonulcerated and ulcerated stenosis, the area covered by ulcers, and the overall disease-affected area across five intestinal sections. Scores range from 0 to 44, with higher scores indicating more severe disease. While often seen as the standard for measuring severity, CDEIS can be complex to calculate and may underestimate severity if only one segment, particularly the ileum, is affected. There are also no clear score cutoffs for specific outcomes or treatment responses, limiting its effectiveness in determining remission.[29]
The Simple Endoscopic Score for Crohn's Disease (SES-CD) offers a more straightforward approach than the CDEIS scoring system, using four key factors to evaluate Crohn's disease during an endoscopy. These factors include the presence and size of ulcers, the area affected by ulcers, the overall extent of the disease, and any narrowing of the intestine (stenosis). The first three factors are scored from 0 to 3 in each of the five sections of the intestine, with a maximum score of 15 for each section. Stenosis is scored separately, ranging from 0 to 11. This results in a total SES-CD score that can range from 0 to 56, with higher scores indicating more severe disease.[29]
Laboratory testing
[edit]While no lab test can definitively confirm or rule out Crohn's disease, results from serum and stool tests can help support the diagnosis:[2]
- The antimicrobial antibody ASCA is a well-known blood test marker used in the diagnosis of Crohn's disease. Approximately 60–70% of individuals with Crohn's disease test positive for ASCA, while only 10–15% of those with ulcerative colitis and less than 5% of patients with other types of colitis have positive results.[1]
- The autoantibody pANCA is found in 10–15% of Crohn's disease cases, in 60–70% of ulcerative colitis cases, and in less than 5% of patients with other types of colitis that aren't inflammatory bowel disease. Additionally, patients with Crohn's disease who test positive for pANCA often show symptoms similar to those of ulcerative colitis.[1]
- C-reactive protein (CRP) is a blood marker that indicates inflammation and can help monitor Crohn's disease activity. However, about one third of patients with active disease may have normal CRP levels, while one third with high levels of CRP have inactive disease. Moreover, CRP's ability to predict disease progression is not well established.[1]
- Fecal calprotectin is a stool test used to differentiate inflammatory bowel disease, like Crohn's disease, from irritable bowel syndrome. While there are no official cut-off values, it is commonly used to assess disease activity in Crohn's.[1] Elevated levels may also indicate other intestinal infections or inflammatory conditions, not just Crohn's disease.[2]
Differential diagnosis
[edit]Crohn's disease has similar endoscopic, radiographic and histological features with other inflammatory or infectious diseases. 10% of people with Crohn's disease are initially diagnosed with indeterminate colitis.[1]
- Behçet’s disease can cause intestinal inflammation, primarily featuring single ulcers and symptoms outside the intestines, which differ from Crohn's disease. Recurrent sores in the mouth and genitals raise suspicion for Behçet's. A pathergy test, where the skin is lightly pricked to check for a red bump or ulcer, can help confirm the diagnosis. Eye inflammation (uveitis) and skin issues are also common in Behçet's disease.[1]
- Intestinal lymphoma lacks symptoms that differentiate it from other conditions; diagnosis can only be confirmed through histological examination of tissue samples.[1]
- Intestinal tuberculosis can cause symptoms such as fever, night sweats, and ulcers in the transverse colon, along with a swollen ileocecal valve. Key tissue changes include granulomas, which may be caseating, confluent, or large. A positive smear test for acid-fast bacillus and imaging that detects necrotic lymph nodes are also important indicators of the disease.[1]
- Ischemic colitis is also a possible alternative diagnosis to Crohn's disease. It often shows swelling and redness of the inner lining of the colon, while the rectum usually remains unaffected.[1]
Classification
[edit]The Montreal classification system is a widely used framework for categorizing the phenotypes of Crohn's disease. It considers three primary factors: the age at diagnosis (divided into three groups: less than 16 years, 17 to 40 years, and over 40 years), the location of the disease (which can be ileal, colonic, ileocolonic, or isolated upper), and the behavior of the disease (including non-stricturing/non-penetrating, stricturing, penetrating, and perianal types).[30]
Management
[edit]The management of Crohn's disease is customized based on the severity, location, and behavior of the disease. Providers also assess the risk of aggressive disease to determine the need for more intensive treatment. Risk factors include diagnosis before age 30, extensive disease involvement, perianal complications, deep ulcers, and history of surgery. A key goal of treatment is to achieve mucosal healing, which restores the intestinal lining. Mucosal healing is linked to better outcomes, such as fewer flare-ups, reduced hospitalizations, steroid-free remission, and a longer interval without surgery.[1]
Corticosteroids
[edit]Steroids are often used to quickly induce remission and relieve symptoms in Crohn's disease, but they are ineffective for maintaining remission. Options include intravenous steroids, prednisone, and budesonide, with budesonide preferred for its safety, though it's limited to mild to moderate cases in the ileum and right colon. Patients on systemic steroids should switch to other medications for long-term remission, as prolonged use can cause adrenal issues, weight gain, cataracts, hypertension, and diabetes. Additionally, systemic steroids may increase the risk of serious infections and mortality in moderate to severe Crohn's disease.[29]
Conventional immunosuppressants
[edit]Thiopurines, like azathioprine and 6-mercaptopurine, maintain remission in Crohn's disease but do not induce it initially. Since thiopurines take 6 to 12 weeks to work, steroids are often used to manage symptoms during this time. Before starting thiopurines, liver metabolism is assessed and Epstein-Barr virus is tested in patients under 25. Around 15% to 20% of patients stop thiopurines due to side effects, including low blood cell counts, liver problems, nausea, vomiting, allergic reactions, and acute pancreatitis. Thiopurines also raise the risk of certain cancers and serious conditions, necessitating regular lab monitoring.[29]
Methotrexate is used to induce and maintain remission in Crohn's disease, being slightly more effective than thiopurines and taking 8 to 16 weeks to work. About 17% of patients stop taking it due to side effects like nausea, vomiting, headaches, and fatigue. It can affect liver health and, rarely, lower blood cell counts, requiring regular blood tests. Methotrexate may also cause anemia and mouth sores, so daily folic acid is recommended. Additionally, it may increase the risk of certain skin cancers and lymphoma. Methotrexate is discontinued during pregnancy due to the risks of miscarriage and birth defects.[29]
Biologics
[edit]Anti-TNF therapy is the most effective treatment for inducing and maintaining remission, with FDA-approved agents including infliximab, adalimumab, and certolizumab pegol.[29] It blocks the inflammatory protein TNF and induces cell death in activated T cells.[31] Responses may occur within a week, but full effects can take up to six weeks. Loss of response can happen due to the development of antidrug antibodies, necessitating a switch in agents or drug classes. Anti-TNF agents are often combined with thiopurines or methotrexate to minimize antibody development. Side effects include injection-site reactions, a higher risk of infection, a slight increase in melanoma risk, and rare cases of cytopenias and liver toxicity.[29]
Vedolizumab is the first treatment designed specifically for the gut in moderate to severe Crohn's disease. It blocks the molecule α4β7 that helps white blood cells enter the gut, reducing inflammation. Unlike natalizumab, it does not carry a risk of the serious brain infection PML. While vedolizumab can induce remission, it works slowly, taking about 12 weeks to show effects, and its overall effectiveness is limited. However, patients who respond well can maintain remission for up to a year. Since it specifically targets the gut, it does not significantly increase the risk of serious side effects or infections, except for mild nasal infections.[29]
Ustekinumab, approved for moderate to severe Crohn's disease in October 2016, has been FDA-approved for psoriasis since 2009.[32] It appears to be comparable to anti-TNF therapy in both the induction and maintenance of remission, functioning by blocking the inflammatory molecules IL-12 and IL-23. The onset of action is similar to that of anti-TNF treatments, with responses typically observed within six weeks. Notably, Ustekinumab does not seem to increase the risk of serious infections, although the studies conducted in Crohn's disease have been relatively short-term.[29]
The JAK inhibitor such as upadacitinib is approved for treatment of moderate to severe Crohn's disease, with a large multi-centre randomized control trial demonstrating its effectiveness in induction and maintenance of disease.[32][33]
Surgery
[edit]
Many individuals with Crohn's disease may require a bowel resection to remove part of the intestine due to blockages, lesions, infections, or ineffective medications. Since surgery is not a cure, the goal is to preserve as much of the small bowel as possible,[29] and extensive resections can lead to short bowel syndrome.[34] In cases with widespread strictures, only the most prominent stricture is typically resected, while minor strictures may be dilated through strictureplasty. After a resection, the healthy ends of the intestine are rejoined in a primary anastomosis.[29]
Approximately six to twelve months after surgery, patients usually undergo a colonoscopy to check for inflammation, using the Rutgeerts scoring system to assess the likelihood of recurrence. About 50% may experience a return of symptoms within five years, and nearly 40% may need a second surgery within ten years,[29] often due to inflammation near the anastomosis.[35] While drug therapy aims to prevent recurrences, its effectiveness remains uncertain.[29]
Diet
[edit]- Enteral nutrition, which administers nutrients as a powder or liquid, is the primary method for inducing remission in children with Crohn's disease. It can induce remission in up to 80% of cases. Outside of Japan, it is not used to treat Crohn's disease in adults due to unpalatable formulations.[36]
- Parenteral nutrition, which administers nutrients directly into the bloodstream, may be used to supply nutrients to patients when there is extensive inflammation that impairs absorption. Parenteral nutrition has the same effectiveness as enteral nutrition in inducing remission.[37]
- The Mediterranean diet, rich in fruits, vegetables, unsaturated fats, and lean protein, is beneficial to general health but has not been found to reduce the rate of flares in Crohn's disease.[38]
- Cooking and processing fruits and vegetables to reduce fibrousness increases tolerance of those foods in people with intestinal strictures.[38]
Other treatments
[edit]- Mesalamine is not effective for inducing or maintaining remission in Crohn's disease, but is nevertheless commonly used as a treatment due to its perceived benefits and low risk of side effects.[1]
- Antibiotics are not effective in inducing or maintaining remission in Crohn's disease. However, they are effective in treating perianal fistulas and inflammation when used alongside anti-TNF therapy.[1]
- Fecal microbiota transplants have shown potential effectiveness in preliminary studies. However, larger studies are needed to verify its efficacy.[39]
- Acupuncture influences the immune system by stimulating the vagus nerve. Early studies have shown efficacy in improving clinical symptoms, but larger studies are needed.[40]
- Cannabis is a potential therapy for Crohn's disease by targeting the endocannabinoid system. Although it has shown benefits in animal models, its efficacy as a treatment is uncertain.[41]
- Cognitive behavioral therapy has shown short-term positive psychological effects in people with Crohn's disease, but it has no long-term effect on physical or psychological health.[42]
Outlook
[edit]Crohn's disease is a chronic condition requiring ongoing management, as there is currently no cure. Inflammation is typically controlled through medications such as steroids and immunosuppressants, and in severe cases, surgery may be necessary. The clinical course of the disease is classified into four patterns:[43]
- Remission: Severity decreases in response to treatment, leading to sustained remission.[43]
- Improved and Stable: Severity lessens, but mild inflammation persists.[43]
- Relapsing: The disease fluctuates between periods of remission and severe inflammation.[43]
- Refractory: Severe inflammation continues without respite.[43]
Approximately 40% to 56% of individuals with Crohn's disease achieve clinical remission after one year of infliximab treatment, increasing to 56% to 58% when combined with an immunosuppressant. Furthermore, 16% to 39% attain both clinical and endoscopic remission, showing no signs of inflammation in the intestine. Once in remission, individuals have an 80% chance of maintaining this state for the following year. Conversely, 10% to 15% of individuals may experience ongoing active disease without remission.[43]
Chronic inflammation from Crohn's disease increases the risk of heart problems, cancers, arthritis, osteoporosis (weakened bones), and mental health issues. Some medications can also raise the chances of infections and cancers. Because of these combined risks, people with Crohn's disease tend to have a shorter lifespan compared to those who are healthy. In Canada, studies show that women affected with Crohn's disease live about 7.7 years less than unaffected women, and affected men live about 7.7 years less than otherwise expected.[4]
Epidemiology
[edit]Crohn's disease is most prevalent in North America and Western Europe, particularly among Ashkenazi jews and possibly more common in women.[29] The annual incidence in North America is 0–20.2 new cases per 100,000 people, while incidence in Europe is 0.3–12.7 per 100,000. The prevalence of Crohn's disease is 322 per 100,000 in Germany, 319 per 100,000 in Canada,[1] and 300 per 100,000 in the United States.[5] The prevalence of Crohn's disease has risen in newly industrialized countries, with rates of 18.6 per 100,000 in Hong Kong and 3.9 per 100,000 in Taiwan.[1]
The typical age of onset is between 20 and 30 years, with a smaller peak around 50 years, leading to a median onset age of 30.[29] About 20 to 25% of patients presenting with inflammatory bowel disease are children under 18 years old, while 80% are adolescents. Additionally, the incidence of Crohn's disease in children is on the rise, with 2.5–11.4 new cases per 100,000 and a prevalence of 58 per 100,000.[44]
History
[edit]Giovanni Battista Morgagni, often referred to as the father of anatomic pathology, provided one of the earliest detailed accounts of the disease in his 1761 treatise, noting specific autopsy findings in a young patient who suffered from severe gastrointestinal symptoms.[45]
The first notable series of cases of Crohn's disease was reported by Polish surgeon Antoni Leśniowski in 1903,[46] followed by Scottish surgeon Thomas Kennedy Dalziel in 1913, who described nine patients exhibiting significant pathological features treated by surgical resection. However, the disease only gained widespread recognition with a landmark 1932 article by Burrill B. Crohn, Leon Ginzburg, and Gordon D. Oppenheimer. In this publication, they introduced the term "regional ileitis" based on their observations of chronic inflammation in the terminal ileum of 14 patients.[45]
Over the following decades, Crohn's disease was recognized as affecting various parts of the gastrointestinal tract, with reports of involvement from the esophagus to the colon. This period also marked the identification of skip lesions—areas of healthy bowel between diseased sections—adding to the understanding of the disease's pathology. Public awareness of Crohn's disease increased significantly after President Eisenhower underwent surgery for the condition in 1956, which highlighted its impact on quality of life and encouraged discussions about the disease.[45]
In 1960, ulcerative colitis and Crohn's colitis were officially classified as distinct diseases, despite lingering beliefs that Crohn's disease could not manifest in the colon. During this decade, advancements such as fiberoptic colonoscopy and the capability to perform biopsies significantly enhanced the diagnosis and management of Crohn's disease, facilitating improved visualization of the gastrointestinal tract and more accurate assessments of disease severity. Subsequent decades saw the testing of various medications for Crohn's disease in clinical trials, including the identification of methotrexate's efficacy in 1989.[45]
In the 1990s, the focus of treatment for Crohn's disease began to shift towards biologic therapies, particularly anti-TNF agents. Concurrently, nutritional therapy gained prominence in managing pediatric cases and instances of malnutrition. The introduction of MRI enterography emerged as a safe and effective method for monitoring disease activity. This was further augmented by the FDA's approval of capsule endoscopy in 2001, which allowed for improved imaging of the small intestine. Since the inception of genome-wide association studies in 2005, several genetic markers associated with Crohn's disease have been identified, contributing to a deeper understanding of the condition.[45]
Support organizations such as the Crohn's & Colitis Foundation have also emerged, providing resources and community for patients, helping to raise awareness and funding for research initiatives.[45] Today, Crohn's disease continues to be a focus of extensive research, aiming to improve treatment outcomes and enhance the quality of life for those affected.[45]
Etymology
[edit]Crohn's disease is named after Dr. Burrill Crohn, though its eponymous association arose from complex circumstances. Initially, researchers Ginzburg and Oppenheimer identified a pattern of the disease and compiled 12 cases, all linked to surgeon A. A. Berg. However, Berg declined authorship due to his lack of prior involvement. Ginzburg and Oppenheimer then connected with Crohn, who received the manuscript, which was later published with his name listed first and two additional cases included.[45]
Originally, the disease was referred to as "regional ileitis," reflecting the findings of the time, but subsequent reports revealed its presence throughout the gastrointestinal tract, leading to the adoption of the eponym.[45] In Poland, it was historically called “Lesniowski-Crohn's disease.”[46] There has been growing criticism of medical eponyms for their inaccuracies, prompting a movement towards using non-possessive forms, such as "Crohn disease," which has gained traction in recent years among academic and medical publications.[45]
References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk Roda G, Chien Ng S, Kotze PG, Argollo M, Panaccione R, Spinelli A, et al. (April 2020). "Crohn's Disease". Nature Reviews Disease Primers. 6 (1): 22. doi:10.1038/s41572-020-0156-2. PMID 32242028.
- ^ a b c d e f g Feuerstein JD, Cheifetz AS (June 2017). "Crohn Disease: Epidemiology, Diagnosis, and Management". Mayo Clinic Proceedings. 92 (7): 1088–1103. doi:10.1016/j.mayocp.2017.04.010. PMID 28601423.
- ^ a b c d e f g h i j k Ramos GP, Papadakis KA (January 2019). "Mechanisms of Disease: Inflammatory Bowel Diseases". Mayo Clinic Proceedings. 94 (1): 155–165. doi:10.1016/j.mayocp.2018.09.013. PMC 6386158. PMID 30611442.
- ^ a b Kuenzig ME, Manuel DG, Donelle J, Benchimol EI (November 2020). "Life expectancy and health-adjusted life expectancy in people with inflammatory bowel disease Factors". Canadian Medical Association Journal. 192 (45): E1394–E1402. doi:10.1503/cmaj.190976. PMC 7669301. PMID 33168761.
- ^ a b Weisman MH, Stens O, Kim SH, Hou JK, Miller FW, Dillon CF (March 2023). "Inflammatory Bowel Disease Prevalence: Surveillance data from the U.S. National Health and Nutrition Examination Survey". Preventive Medicine Reports. 9 (33): 102173. doi:10.1016/j.pmedr.2023.102173. PMC 10201824. PMID 37223580.
- ^ Wenzl HH (September 2012). "Diarrhea in chronic inflammatory bowel diseases". Gastroenterology Clinics of North America. 41 (3): 651–675. doi:10.1016/j.gtc.2012.06.006. PMID 22917170.
- ^ Coates MD, Clarke K, Williams E, Jeganathan N, Yadav S, Giampetro D, et al. (September 2023). "Abdominal Pain in Inflammatory Bowel Disease: An Evidence-Based, Multidisciplinary Review". Crohns Colitis 360. 5 (4): otad055. doi:10.1093/crocol/otad055. PMC 10588456. PMID 37867930.
- ^ "What I need to know about Crohn's Disease". www.niddk.nih.gov. Archived from the original on November 21, 2015. Retrieved December 11, 2015.
- ^ "Bleeding and Blood in the Stool". crohn's and colitis. Retrieved October 16, 2024.
- ^ Barros LL, Farias AQ, Rezaie A (August 2019). "Gastrointestinal motility and absorptive disorders in patients with inflammatory bowel diseases: Prevalence, diagnosis and treatment". World Journal of Gastroenterology. 25 (31): 4414–4426. doi:10.3748/wjg.v25.i31.4414. PMC 6710178. PMID 31496621.
- ^ Pogacnik JS, Salgado G (September 2019). "Perianal Crohn's Disease". Clinics in Colon and Rectal Surgery. 32 (5): 377–385. doi:10.1055/s-0039-1687834. PMC 6731113. PMID 31507348.
- ^ Laube R, Liu K, Schifter M, Yang JL, Suen MK, Leong RW (February 2018). "Oral and upper gastrointestinal Crohn's disease". Journal of Gastroenterology and Hepatology. 33 (2): 355–364. doi:10.1111/jgh.13866. ISSN 0815-9319. PMID 28708248.
- ^ Włodarczyk M, Makaro A, Prusisz M, Włodarczyk J, Nowocień M, Maryńczak K, et al. (August 2023). "The Role of Chronic Fatigue in Patients with Crohn's Disease". Life (Basel). 13 (8): 1692. Bibcode:2023Life...13.1692W. doi:10.3390/life13081692. PMC 10455565. PMID 37629549.
- ^ a b Ranasinghe IR, Tian C, Hsu R (2024). "Crohn Disease". StatPearls Publishing. PMID 28613792. Retrieved October 18, 2024.
- ^ Antonelli E, Bassotti G, Tramontana M, Hansel K, Stingeni L, Ardizzone S, et al. (January 2021). "Dermatological Manifestations in Inflammatory Bowel Diseases". J Clin Med. 10 (2): 364. doi:10.3390/jcm10020364. PMC 7835974. PMID 33477990.
- ^ Bisgaard TH, Allin KH, Keefer L, Ananthakrishnan AN, Jess T (March 2023). "Depression and anxiety in inflammatory bowel disease: epidemiology, mechanisms and treatment". Nature Reviews Gastroenterology & Hepatology. 19 (11): 717–726. doi:10.1038/s41575-022-00634-6. PMID 35732730.
- ^ a b c d Jabłońska B, Mrowiec S (April 2023). "Nutritional Status and Its Detection in Patients with Inflammatory Bowel Diseases". Nutrients. 15 (8): 1991. doi:10.3390/nu15081991. PMC 10143611. PMID 37111210.
- ^ Gasparetto M, Guariso G (October 2014). "Crohn's disease and growth deficiency in children and adolescents". World Journal of Gastroenterology. 20 (37): 13219–13233. doi:10.3748/wjg.v20.i37.13219. PMC 4188880. PMID 25309059.
- ^ a b Sato Y, Tsujinaka S, Miura T, Kitamura Y, Suzuki H, Shibata C (August 2023). "Inflammatory Bowel Disease and Colorectal Cancer: Epidemiology, Etiology, Surveillance, and Management". Cancers (Basel). 15 (16): 4154. doi:10.3390/cancers15164154. PMC 10452690. PMID 37627182.
- ^ Bhatt H, Mathis KL (March 2023). "Small Bowel Carcinoma in the Setting of Inflammatory Bowel Disease". Clinics in Colon and Rectal Surgery. 37 (1): 46–52. doi:10.1055/s-0043-1762929. PMC 10769580. PMID 38188070.
- ^ Kayali S, Fantasia S, Gaiani F, Cavallaro LG, de'Angelis GL, Laghi L (April 2024). "NOD2 and Crohn's Disease Clinical Practice: From Epidemiology to Diagnosis and Therapy, Rewired". Inflammatory Bowel Diseases. doi:10.1093/ibd/izae075. PMID 38582044.
- ^ Plitas G, Rudensky AY (September 2016). "Regulatory T Cells: Differentiation and Function". Cancer Immunology Research. 4 (9): 721–725. doi:10.1158/2326-6066.CIR-16-0193. PMC 5026325. PMID 27590281.
- ^ a b c d Mowat AM, Agace WW (October 2014). "Regional specialization within the intestinal immune system". Nature Reviews Immunology. 14 (10): 667–85. doi:10.1038/nri3738. PMID 25234148.
- ^ Torres J, Mehandru S, Colombel J, Peyrin-Biroulet L (2017). "Crohn's disease". The Lancet. 389 (10080): 1741–1755. doi:10.1016/S0140-6736(16)31711-1. PMID 27914655.
- ^ Hu MD, Edelblum KL (August 2017). "Sentinels at the frontline: the role of intraepithelial lymphocytes in inflammatory bowel disease". Current Pharmacology Reports. 3 (6): 321–334. doi:10.1007/s40495-017-0105-2. PMC 5724577. PMID 29242771.
- ^ Zeng B, Shi S, Ashworth G, Dong C, Liu J, Xing F (April 2019). "ILC3 function as a double-edged sword in inflammatory bowel diseases". Cell Death & Disease. 10 (4): 315. doi:10.1038/s41419-019-1540-2. PMC 6453898. PMID 30962426.
- ^ Passos MA, Chaves FC, Chaves-Junior N (2018). "The Importance of Colonoscopy in Inflammatory Bowel Diseases". Arquivos Brasileiros de Cirurgia Digestiva. 31 (2): e1374. doi:10.1590/0102-672020180001e1374. PMC 6044200. PMID 29972402.
- ^ Schneider M, Höllerich J, Beyna T (July 2019). "Device-assisted enteroscopy: A review of available techniques and upcoming new technologies". World Journal of Gastroenterology. 25 (27): 3538–3545. doi:10.3748/wjg.v25.i27.3538. PMC 6658397. PMID 31367155.
- ^ a b c d e f g h i j k l m n o Koutroumpakis E, Katsanos KH (May 2016). "Implementation of the simple endoscopic activity score in crohn's disease". Saudi Journal of Gastroenterology. 22 (3): 183–191. doi:10.4103/1319-3767.182455. PMC 4898086. PMID 31367155.
- ^ Cockburn E, Kamal S, Chan A, Rao V, Liu T, Huang JY, et al. (November 2023). "Crohn's disease: an update". Clinical Medicine (London). 23 (6): 549–557. doi:10.7861/clinmed.2023-0493. PMC 11298500. PMID 38065612.
- ^ Levin AD, Wildenberg ME, van den Brink GR (August 2016). "Mechanism of Action of Anti-TNF Therapy in Inflammatory Bowel Disease". Journal of Crohn's and Colitis. 10 (8): 989–997. doi:10.1093/ecco-jcc/jjw053. PMC 5724577. PMID 29242771.
- ^ a b Gordon H, Minozzi S, Kopylov U, Verstockt B, Chaparro M, Buskens C, et al. (October 2024). "ECCO Guidelines on Therapeutics in Crohn's Disease: Medical Treatment". J Crohns Colitis. 18 (10): 1531–1555. doi:10.1093/ecco-jcc/jjae091. PMID 38877997.
- ^ Loftus EV, Panés J, Lacerda AP, Peyrin-Biroulet L, D'Haens G, Panaccione R, et al. (2023). "Upadacitinib Induction and Maintenance Therapy for Crohn's Disease". N Engl J Med. 388 (21): 1966–1980. doi:10.1056/NEJMoa2212728. hdl:2268/304716. PMID 37224198.
{{cite journal}}: CS1 maint: multiple names: authors list (link) Review in: Ann Intern Med. 2023 Sep;176(9):JC103. doi: 10.7326/J23-0069 - ^ Aksan A, Farrag K, Blumenstein I, Schröder O, Dignass AU, Stein J (June 2021). "Chronic intestinal failure and short bowel syndrome in Crohn's disease". World Journal of Gastroenterology. 27 (24): 3440–3465. doi:10.3748/wjg.v27.i24.3440. PMC 8240052. PMID 34239262.
- ^ Lewis RT, Maron DJ (September 2010). "Efficacy and complications of surgery for Crohn's disease". Gastroenterology and Hepatology. 6 (9): 587–596. PMC 2976865. PMID 21088749.
- ^ Di Caro S, Fragkos KC, Keetarut K, Koo HF, Sebepos-Rogers G, Saravanapavan H, et al. (September 2019). "Enteral Nutrition in Adult Crohn's Disease: Toward a Paradigm Shift". Nutrients. 11 (4): 2222. doi:10.3390/nu11092222. PMC 6770416. PMID 31540038.
- ^ Comeche JM, Comino I, Altavilla C, Tuells J, Gutierrez-Hervas A, Caballero P (November 2019). "Parenteral Nutrition in Patients with Inflammatory Bowel Disease Systematic Review, Meta-Analysis and Meta-Regression". Nutrients. 11 (12): 2865. doi:10.3390/nu11122865. PMC 6950216. PMID 31766687.
- ^ a b Hashash JG, Elkins J, Lewis JD, Binion DG (January 2024). "AGA Clinical Practice Update on Diet and Nutritional Therapies in Patients With Inflammatory Bowel Disease: Expert Review". Gastroenterology. 166 (3): 521–532. doi:10.1053/j.gastro.2023.11.303. PMID 38276922.
- ^ Fehily SR, Basnayake C, Wright EK, Kamm MA (July 2021). "Fecal microbiota transplantation therapy in Crohn's disease: Systematic review". Journal of Gastroenterology and Hepatology. 36 (10): 2672–2686. doi:10.1111/jgh.15598. hdl:11343/298722. PMID 34169565.
- ^ Song G, Fiocchi C, Achkar JP (June 2019). "Acupuncture in Inflammatory Bowel Disease". Inflammatory Bowel Diseases. 25 (7): 1129–1139. doi:10.1093/ibd/izy371. PMID 30535303.
- ^ Kafil TS, Nguyen TM, MacDonald JK, Chande N (November 2018). "Cannabis for the treatment of Crohn's disease". The Cochrane Database of Systematic Reviews. 11 (11): CD012853. doi:10.1002/14651858.CD012853.pub2. PMC 6517156. PMID 30407616.
- ^ Chen J, Chen X, Sun Y, Xie Y, Wang X, Li R, et al. (December 2021). "The physiological and psychological effects of cognitive behavior therapy on patients with inflammatory bowel disease before COVID-19: a systematic review". BMC Gastroenterology. 21 (1): 469. doi:10.1186/s12876-021-02003-0. PMC 8672154. PMID 34911469.
- ^ a b c d e f Cho CW, You MW, Oh CH, Lee CK, Moon SK (March 2022). "Long-term Disease Course of Crohn's Disease: Changes in Disease Location, Phenotype, Activities, and Predictive Factors". Gut and Liver. 16 (2): 157–170. doi:10.5009/gnl210118. PMC 8924800. PMID 34456186.
- ^ von Allmen D (February 2018). "ediatric Crohn's Disease". Clinics in Colon and Rectal Surgery. 31 (2): 80–88. doi:10.1055/s-0037-1609022. PMC 5825885. PMID 29487490.
- ^ a b c d e f g h i j Mulder DJ, Noble AJ, Justinich CJ, Duffin JM (May 2014). "A tale of two diseases: the history of inflammatory bowel disease". Journal of Crohn's and Colitis. 8 (5): 341–348. doi:10.1016/j.crohns.2013.09.009. PMID 24094598.
- ^ a b Van Hootegem P, Travis S (July 2020). "Is Crohn's Disease a Rightly Used Eponym?". Journal of Crohn's and Colitis. 14 (6): 867–871. doi:10.1093/ecco-jcc/jjz183. PMID 31701137.
Further reading
[edit]- Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE (April 2018). "ACG Clinical Guideline: Management of Crohn's Disease in Adults". Am. J. Gastroenterol. 113 (4): 481–517. doi:10.1038/ajg.2018.27. PMID 29610508.
External links
[edit]- "Crohn's disease". MedlinePlus. U.S. National Library of Medicine.
 Media related to Crohn's disease at Wikimedia Commons
Media related to Crohn's disease at Wikimedia Commons

