Inflammation: Difference between revisions
Mariansavu (talk | contribs) →Inflammatory disorders: linking, arranging words in alphabetical order, removing two ambiguous terms |
rv Oncotarget as an unreliable source, WP:CITEWATCH |
||
| (996 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
{{short description|Physical effects resulting from activation of the immune system}} |
|||
[[File:Wintertenen.jpg|thumb|250px|right|Toes inflamed by [[Chilblains]]]] |
|||
{{cs1 config|name-list-style=vanc|display-authors=6}} |
|||
{{More medical citations needed|date=March 2021}} |
|||
{{Use dmy dates|date=June 2023}} |
|||
{{Infobox medical condition |
|||
|name = |
|||
|synonym = |
|||
|image = Allergy to Antibiotic Cefaclor.JPG |
|||
|image_size = |
|||
|image_thumbtime = |
|||
|alt = |
|||
|caption = An [[allergic reaction]] to [[cefaclor]] has led to inflammation of the skin on the foot. The cardinal signs of inflammation include: pain, heat, redness, swelling, and loss of function. Some of these indicators can be seen here. |
|||
|pronounce = |
|||
|specialty = [[Immunology]], [[rheumatology]] |
|||
|symptoms = Heat, pain, redness, swelling |
|||
|complications = [[Asthma]], [[pneumonia]], [[autoimmune diseases]] |
|||
|onset = |
|||
|duration = '''Acute''': few days<br />'''Chronic''': up to many months, or years |
|||
|types = |
|||
|causes = Infection, [[physical injury]], [[autoimmune disorder]] |
|||
|risks = |
|||
|diagnosis = |
|||
|differential = |
|||
|prevention = |
|||
|treatment = |
|||
|medication = |
|||
|prognosis = |
|||
|frequency = |
|||
|deaths = |
|||
}} |
|||
'''Inflammation''' ([[Latin]] |
'''Inflammation''' (from {{langx|la|[[wikt:en:inflammatio#Latin|inflammatio]]}}) is part of the biological response of body tissues to harmful stimuli, such as [[pathogen]]s, damaged cells, or [[Irritation|irritants]].<ref name="pmid17223962">{{Cite journal |vauthors=Ferrero-Miliani L, Nielsen OH, Andersen PS, Girardin SE |date=February 2007 |title=Chronic inflammation: importance of NOD2 and NALP3 in interleukin-1beta generation |journal=Clinical and Experimental Immunology |volume=147 |issue=2 |pages=227–235 |doi=10.1111/j.1365-2249.2006.03261.x |pmc=1810472 |pmid=17223962}}</ref> The five [[cardinal signs]] are heat, pain, redness, swelling, and [[Functio laesa|loss of function]] (Latin ''calor'', ''dolor'', ''rubor'', ''tumor'', and ''functio laesa''). |
||
Inflammation is a generic response, and therefore is considered a mechanism of [[innate immune system|innate immunity]], whereas [[adaptive immune system|adaptive immunity]] is specific to each pathogen.<ref name="ABBAS">{{Cite book |title=Basic Immunology. Functions and disorders of the immune system |vauthors=Abbas AB, Lichtman AH |publisher=Saunders/Elsevier |year=2009 |isbn=978-1-4160-4688-2 |edition=3rd |chapter=Ch.2 Innate Immunity}}</ref> |
|||
Without inflammation, wounds and infections would never heal. Similarly, progressive destruction of the tissue would compromise the survival of the organism. However, chronic inflammation can also lead to a host of diseases, such as [[hay fever]], [[atherosclerosis]], [[rheumatoid arthritis]], and even cancer (e.g., [[gallbladder carcinoma]]). It is for that reason that inflammation is normally closely regulated by the body. |
|||
Inflammation is a protective response involving [[immune cells]], [[blood vessel]]s, and molecular mediators. The function of inflammation is to eliminate the initial cause of cell injury, clear out damaged cells and tissues, and initiate tissue repair. Too little inflammation could lead to progressive tissue destruction by the harmful stimulus (e.g. bacteria) and compromise the survival of the organism. However inflammation can also have negative effects.<ref>{{Cite web |title=Inflammation and Your Health |url=https://www.cedars-sinai.org/discoveries/inflammation.html |website=Cedars-Sinai}}</ref> Too much inflammation, in the form of chronic inflammation, is associated with various diseases, such as [[hay fever]], [[periodontal disease]], [[atherosclerosis]], and [[osteoarthritis]]. |
|||
Inflammation can be classified as either ''acute'' or ''chronic''. ''Acute inflammation'' is the initial response of the body to harmful stimuli and is achieved by the increased movement of [[blood plasma|plasma]] and [[leukocyte]]s (especially [[granulocyte]]s ) from the blood into the injured tissues. A cascade of biochemical events propagates and matures the inflammatory response, involving the local [[vascular system]], the [[immune system]], and various cells within the injured tissue. Prolonged inflammation, known as ''chronic inflammation'', leads to a progressive shift in the type of cells present at the site of inflammation and is characterized by simultaneous destruction and [[healing]] of the tissue from the inflammatory process. |
|||
Inflammation can be classified as ''acute'' or ''chronic''. Acute inflammation is the initial response of the body to harmful stimuli, and is achieved by the increased movement of [[blood plasma|plasma]] and [[leukocyte]]s (in particular [[granulocyte]]s) from the blood into the injured tissues. A series of biochemical events propagates and matures the inflammatory response, involving the local [[vascular system]], the [[immune system]], and various cells in the injured tissue. Prolonged inflammation, known as ''chronic inflammation'', leads to a progressive shift in the type of cells present at the site of inflammation, such as [[Mononuclear cell infiltration|mononuclear cells]], and involves simultaneous destruction and [[healing]] of the tissue. |
|||
Inflammation has also been classified as Type 1 and Type 2 based on the type of [[cytokines]] and [[helper T cells]] (Th1 and Th2) involved.<ref>{{Cite journal |vauthors=Berger A |date=August 2000 |title=Th1 and Th2 responses: what are they? |url=https://www.bmj.com/content/321/7258/424.1 |url-status=live |journal=BMJ |volume=321 |issue=7258 |pages=424 |doi=10.1136/bmj.321.7258.424 |pmc=27457 |pmid=10938051 |archive-url=https://web.archive.org/web/20210712072427/https://www.bmj.com/content/321/7258/424.1 |archive-date=12 July 2021 |access-date=1 July 2021}}</ref> |
|||
== Meaning == |
|||
The earliest known reference for the term inflammation is around the early 15th century. The word root comes from [[Old French]] ''inflammation'' around the 14th century, which then comes from [[Latin]] ''inflammatio'' or ''inflammationem''. Literally, the term relates to the word "flame", as the property of being "set on fire" or "to burn".<ref name="k027">{{Cite web |date=2017-09-28 |title=inflammation |url=https://www.etymonline.com/word/inflammation |access-date=2024-08-11 |website=Etymology of inflammation by etymonline}}</ref> |
|||
The term ''inflammation'' is not a synonym for ''infection''. ''Infection'' describes the interaction between the action of microbial invasion and the reaction of the body's inflammatory response—the two components are considered together in discussion of infection, and the word is used to imply a microbial invasive cause for the observed inflammatory reaction. ''Inflammation'', on the other hand, describes just the body's immunovascular response, regardless of cause. But, because the two are often [[correlation|correlated]], words ending in the suffix ''[[wikt:-itis|-itis]]'' (which means inflammation) are sometimes informally described as referring to infection: for example, the word ''[[urethritis]]'' strictly means only "urethral inflammation", but clinical [[health care provider]]s usually discuss urethritis as a urethral infection because urethral microbial invasion is the most common cause of urethritis. However, the inflammation–infection distinction is crucial in situations in [[pathology]] and [[medical diagnosis]] that involve inflammation that is not driven by microbial invasion, such as cases of [[atherosclerosis]], [[Trauma (medicine)|trauma]], [[ischemia]], and [[autoimmune diseases]] (including [[type III hypersensitivity]]). |
|||
== Causes == |
== Causes == |
||
{{columns-list|colwidth=30em| |
|||
* [[Burn (injury)|Burns]] |
|||
Physical: |
|||
* Chemical [[Irritation|irritants]] |
|||
* [[Burn (injury)|Burns]]<ref name="Hall">{{Cite book |title=Guyton and Hall textbook of medical physiology |vauthors=Hall J |date=2011 |publisher=Saunders/Elsevier |isbn=978-1-4160-4574-8 |edition=12th |location=Philadelphia, Pa. |page=428}}</ref> |
|||
* [[Frostbite]] |
* [[Frostbite]] |
||
* [[Physical injury]], blunt or penetrating<ref>{{Cite book |url=https://www.ncbi.nlm.nih.gov/books/NBK53373/ |title=Inflammation and the Microcirculation |vauthors=Granger DN, Senchenkova E |date=2010 |publisher=Morgan & Claypool Life Sciences |series=Integrated Systems Physiology—From Cell to Function |volume=2 |pages=1–87 |chapter=Leukocyte–Endothelial Cell Adhesion |doi=10.4199/C00013ED1V01Y201006ISP008 |pmid=21452440 |access-date=1 July 2017 |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK53380/ |archive-url=https://web.archive.org/web/20210121004109/https://www.ncbi.nlm.nih.gov/books/NBK53373/ |archive-date=21 January 2021 |url-status=live}}</ref> |
|||
* [[Toxin]]s |
|||
* Foreign bodies, including [[splinters]], dirt and debris |
|||
* [[Infection]] by [[pathogen]]s |
|||
* Trauma<ref name=Hall/> |
|||
* [[Physical injury]], blunt or penetrating |
|||
* Immune reactions due to [[hypersensitivity]] |
|||
* [[Ionizing radiation]] |
* [[Ionizing radiation]] |
||
Biological: |
|||
* Foreign bodies, including splinters, dirt and debris |
|||
* Infection by [[pathogen]]s<ref name=Hall/> |
|||
* Trauma |
|||
* Immune reactions due to [[hypersensitivity]] |
|||
* Stress |
|||
Chemical:<ref name=Hall/> |
|||
* Chemical [[Irritation|irritants]] |
|||
* [[Toxin]]s |
|||
* Alcohol |
|||
Psychological: |
|||
* Excitement<ref>{{Cite journal |vauthors=Piira OP, Miettinen JA, Hautala AJ, Huikuri HV, Tulppo MP |date=October 2013 |title=Physiological responses to emotional excitement in healthy subjects and patients with coronary artery disease |journal=Autonomic Neuroscience |volume=177 |issue=2 |pages=280–5 |doi=10.1016/j.autneu.2013.06.001 |pmid=23916871 |s2cid=19823098}}</ref>}} |
|||
== Types == |
== Types == |
||
{{Unreferenced section|date=April 2023}} |
|||
{| class="wikitable" style="text-align:center" align="center" |
|||
{{See also|List of inflammatory disorders|List of types of inflammation by location}}{{col-begin}} |
|||
{{Col-2}} |
|||
* [[Appendicitis]] |
|||
* [[Bursitis]] |
|||
* [[Colitis]] |
|||
* [[Cystitis]] |
|||
* [[Dermatitis]] |
|||
* [[Epididymitis]] |
|||
* [[Encephalitis]] |
|||
* [[Gingivitis]] |
|||
* [[Meningitis]] |
|||
* [[Myelitis]] |
|||
* [[Myocarditis]] |
|||
* [[Nephritis]] |
|||
* [[Neuritis]] |
|||
* [[Pancreatitis]] |
|||
* [[Periodontitis]]{{Col-2}} |
|||
* [[Pharyngitis]] |
|||
* [[Phlebitis]] |
|||
* [[Prostatitis]] |
|||
* [[RSD/CRPS]] |
|||
* [[Rhinitis]] |
|||
* [[Sinusitis]] |
|||
* [[Tendonitis]] |
|||
* [[Tonsillitis]] |
|||
* [[Urethritis]] |
|||
* [[Vasculitis]] |
|||
* [[Vaginitis]] |
|||
{{col-end}} |
|||
{| class="wikitable" style="text-align:center" |
|||
|+ Comparison between acute and chronic inflammation: |
|+ Comparison between acute and chronic inflammation: |
||
!width="150" | || |
!width="150" | || Acute || Chronic |
||
|- |
|- |
||
| ''Causative agent'' || |
| ''Causative agent'' || {{small|Bacterial pathogens, injured tissues}} || {{small|Persistent acute inflammation due to non-degradable pathogens, viral infection, persistent foreign bodies, or autoimmune reactions}} |
||
|- |
|- |
||
| ''Major cells involved'' || |
| ''Major cells involved'' || {{small|neutrophils (primarily), basophils (inflammatory response), and eosinophils (response to helminth worms and parasites), mononuclear cells (monocytes, macrophages)}} || {{small|Mononuclear cells (monocytes, macrophages, lymphocytes, plasma cells), fibroblasts}} |
||
|- |
|- |
||
| ''Primary mediators'' || |
| ''Primary mediators'' || {{small|Vasoactive amines, eicosanoids}} || {{small|IFN-γ and other cytokines, growth factors, reactive oxygen species, hydrolytic enzymes}} |
||
|- |
|- |
||
| ''Onset'' || |
| ''Onset'' || {{small|Immediate}} || {{small|Delayed}} |
||
|- |
|- |
||
| ''Duration'' || |
| ''Duration'' || {{small|Few days}} || {{small|Up to many months, or years}} |
||
|- |
|- |
||
| ''Outcomes'' || |
| ''Outcomes'' || {{small|Resolution, abscess formation, chronic inflammation}} || {{small|Tissue destruction, fibrosis, necrosis}} |
||
|} |
|} |
||
=== |
=== Acute === |
||
Acute inflammation is a short-term process, usually appearing within a few minutes or hours and begins to cease upon the removal of the injurious stimulus.<ref name="robspath" /> It involves a coordinated and systemic mobilization response locally of various immune, endocrine and neurological mediators of acute inflammation. In a normal healthy response, it becomes activated, clears the pathogen and begins a repair process and then ceases.<ref>{{Cite journal |vauthors=Kumar R, Clermont G, Vodovotz Y, Chow CC |date=September 2004 |title=The dynamics of acute inflammation |journal=Journal of Theoretical Biology |volume=230 |issue=2 |pages=145–55 |arxiv=q-bio/0404034 |bibcode=2004PhDT.......405K |doi=10.1016/j.jtbi.2004.04.044 |pmid=15321710 |s2cid=16992741}}</ref> |
|||
<!-- This section is linked from [[Pathology]] --> |
|||
{| class="wikitable" width="230px" style="text-align:center; margin-left:0.67em" align="right" |
|||
Acute inflammation occurs immediately upon injury, lasting only a few days.<ref name="pmid32310543">{{Cite journal |vauthors=Hannoodee S, Nasuruddin DN |year=2020 |title=Acute Inflammatory Response |url=https://www.ncbi.nlm.nih.gov/books/NBK556083/ |url-status=live |journal=[[EMedicine#History|StatPearls]] |pmid=32310543 |archive-url=https://web.archive.org/web/20220615132211/https://www.ncbi.nlm.nih.gov/books/NBK556083/ |archive-date=15 June 2022 |access-date=28 December 2020}}</ref> [[Cytokine]]s and [[chemokine]]s promote the migration of [[neutrophil]]s and [[macrophage]]s to the site of inflammation.<ref name="pmid32310543" /> Pathogens, allergens, toxins, burns, and frostbite are some of the typical causes of acute inflammation.<ref name="pmid32310543" /> [[Toll-like receptor]]s (TLRs) recognize microbial pathogens.<ref name="pmid32310543" /> Acute inflammation can be a defensive mechanism to protect tissues against injury.<ref name="pmid32310543" /> Inflammation lasting 2–6 weeks is designated subacute inflammation.<ref name="pmid32310543" /><ref name="pmid29630225" /> |
|||
|+ The classic signs and symptoms of acute inflammation: |
|||
!'''English''' || '''Latin''' |
|||
==== Cardinal signs ==== |
|||
{| width="230" align="right" class="wikitable" style="text-align:center; margin-left:0.67em" |
|||
|+ The classic signs and symptoms of acute inflammation:{{efn|1=All these signs may be observed in specific instances, but no single sign must, as a matter of course, be present.<ref name="Stedman">{{Cite book |title=Stedman's Medical Dictionary |publisher=Williams & Wilkins |year=1990 |edition=Twenty-fifth}}</ref> |
|||
These are the original, or [[cardinal signs]] of inflammation.<ref name="Stedman" />}} |
|||
!English || Latin |
|||
|- |
|- |
||
| Redness || ''[[Rubor]]'' |
| Redness || ''[[Rubor]]'' |
||
|- |
|- |
||
| Swelling || ''[[Tumor]]'' |
| Swelling || ''[[Swelling (medical)|Tumor]]'' |
||
|- |
|- |
||
| Heat || ''[[ |
| Heat || ''[[Human body temperature|Calor]]'' |
||
|- |
|- |
||
| Pain || ''[[Pain|Dolor]]'' |
| Pain || ''[[Pain|Dolor]]'' |
||
|- |
|- |
||
| style="border-bottom:2px solid grey;" | Loss of function|| style="border-bottom:2px solid grey;" | ''[[Functio laesa]]''{{efn|1=''Functio laesa'' is an antiquated notion, as it is not unique to inflammation and is a characteristic of many disease states.<ref name="Rather">{{Cite journal |vauthors=Rather LJ |date=March 1971 |title=Disturbance of function (functio laesa): the legendary fifth cardinal sign of inflammation, added by Claudius Galen to the four cardinal signs of Celsus |journal=Bulletin of the New York Academy of Medicine |volume=47 |issue=3 |pages=303–22 |pmc=1749862 |pmid=5276838}}</ref>}} |
|||
| style="border-bottom:2px solid grey;" | Loss of function|| style="border-bottom:2px solid grey;" | ''[[Functio laesa]]''** |
|||
|- |
|||
| colspan="3" align="center"|<sub>All the above signs may be observed in specific instances, but no single sign must, as a matter of course, be present.<ref name="Stedman">{{cite book |last= |first= |title=Stedman's Medical Dictionary |edition=Twenty-fifth |publisher=Williams & Wilkins |location= |year=1990 |isbn= }}</ref> |
|||
These are the original, or "cardinal signs" of inflammation.<ref name="Stedman"/>* |
|||
''Functio laesa'' is an apocryphal notion, as it is not unique to inflammation and is a characteristic of many disease states.<ref name="Rather">{{cite journal |last=Rather |first=L. J. |title=Disturbance of function (functio laesa): the legendary fifth cardinal sign of inflammation, added by Galen to the four cardinal signs of Celsus |journal=Bull N Y Acad Med |year=1971 |volume=47 |issue=3 |pages=303–322 |pmc=1749862 }}</ref></sub>** |
|||
|} |
|} |
||
Inflammation is characterized by five [[cardinal signs]],<ref name="ConcisePathology-Signs">{{Cite book |url=http://www.accessmedicine.com/resourceTOC.aspx?resourceID=7 |title=Concise Pathology |vauthors=Chandrasoma P, Taylor CR |publisher=McGraw-Hill |year=2005 |isbn=978-0-8385-1499-3 |edition=3rd |chapter=Part A. "General Pathology", Section II. "The Host Response to Injury", Chapter 3. "The Acute Inflammatory Response", sub-section "Cardinal Clinical Signs" |oclc=150148447 |access-date=2008-11-05 |chapter-url=http://www.accessmedicine.com/content.aspx?aID=183351 |archive-url=https://web.archive.org/web/20081005091840/http://accessmedicine.com/resourceTOC.aspx?resourceID=7 |archive-date=5 October 2008 |url-status=live}}</ref><ref name="auto">{{cite journal | vauthors = Rather LJ | title = Disturbance of function (functio laesa): the legendary fifth cardinal sign of inflammation, added by Galen to the four cardinal signs of Celsus | journal = Bulletin of the New York Academy of Medicine | volume = 47 | issue = 3 | pages = 303–322 | date = March 1971 | pmid = 5276838 | pmc = 1749862 }}</ref> (the traditional names of which come from Latin): |
|||
[[Image:Toe.JPG|thumb|right|230px|Infected ingrown toenail showing the characteristic redness and swelling associated with acute inflammation]] |
|||
* [[Pain|Dolor]] ([[pain]]) |
|||
* Calor (heat) |
|||
* [[Rubor]] (redness) |
|||
* Tumor ([[swelling (medical)|swelling]]) |
|||
* [[Functio laesa]] (loss of function)<ref>{{Cite book |url=http://thepoint.lww.com/Book/ShowWithResource/2931?resourceId=16419 |title=A massage Therapist Guide to Pathology |vauthors=Werner R |publisher=Wolters Kluwer |year=2009 |isbn=978-0-7817-6919-8 |edition=4th |access-date=6 October 2010 |archive-url=https://web.archive.org/web/20151221050601/http://thepoint.lww.com/Book/ShowWithResource/2931?resourceId=16419 |archive-date=21 December 2015 |url-status=live}}</ref> |
|||
The first four (classical signs) were described by [[Aulus Cornelius Celsus|Celsus]] ({{circa|30 BC}}–38 AD).<ref>{{Cite book |url=https://books.google.com/books?id=t_5pzrF1QocC&pg=PA97 |title=Brief History of Vision and Ocular Medicine |vauthors=Vogel WH, Berke A |publisher=Kugler Publications |year=2009 |isbn=978-90-6299-220-1 |page=97}}</ref> |
|||
Acute inflammation is a short-term process, usually appearing within a few minutes or hours and ceasing upon the removal of the injurious stimulus.<ref name="robspath" /> It is characterized by five cardinal signs:<ref name="ConcisePathology-Signs">{{cite book|author=Parakrama Chandrasoma, Clive R. Taylor |publisher=McGraw-Hill |location=New York, N.Y. |year=ca. 2005 |title=Concise Pathology |edition=3rd edition (Computer file) |isbn=0838514995 |oclc=150148447 |chapter=Part A. ''General Pathology'', Section II. ''The Host Response to Injury'', Chapter 3. ''The Acute Inflammatory Response'', sub-section '''''Cardinal Clinical Signs''''' |url=http://www.accessmedicine.com/resourceTOC.aspx?resourceID=7 |chapterurl=http://www.accessmedicine.com/content.aspx?aID=183351 |accessdate=2008-11-05 }}</ref> |
|||
[[Pain]] is due to the release of chemicals such as bradykinin and histamine that stimulate nerve endings.<ref name="ConcisePathology-Signs" /> Acute inflammation of the lung (usually in response to [[pneumonia]]) does not cause pain unless the inflammation involves the [[parietal pleura]], which does have [[nociceptor|pain-sensitive nerve endings]].<ref name="ConcisePathology-Signs" /> Heat and redness are due to increased blood flow at body core temperature to the inflamed site. Swelling is caused by accumulation of fluid. |
|||
The acronym that may be used for this is "PRISH" for Pain, Redness, Immobility (loss of function), Swelling and Heat. |
|||
=====Loss of function===== |
|||
The traditional names for signs of inflammation come from Latin: |
|||
The fifth sign, ''loss of function'', is believed to have been added later by [[Galen]],<ref name="isbn0-7817-7087-4">{{Cite book |title=Essentials of pahtophysiology: concepts of altered health states |vauthors=Porth C |publisher=Lippincott Williams & Wilkins |year=2007 |isbn=978-0-7817-7087-3 |location=Hagerstown, MD |pages=270}}</ref> [[Thomas Sydenham]]<ref name="isbn0-300-11322-6">{{Cite book |url=https://archive.org/details/worstofevilsmans00dorm/page/22 |title=The worst of evils: man's fight against pain |vauthors=Dormandy T |publisher=Yale University Press |year=2006 |isbn=978-0-300-11322-8 |location=New Haven, Conn |pages=[https://archive.org/details/worstofevilsmans00dorm/page/22 22] |url-access=registration}}</ref> or [[Rudolf Ludwig Karl Virchow|Rudolf Virchow]].<ref name="robspath">{{Cite book |title=Robbins Pathologic Basis of Disease |vauthors=Robbins SL, Cotran RS, Kumar V, Collins T |publisher=W.B Saunders Company |year=1998 |isbn=978-0-7216-7335-6 |location=Philadelphia}}</ref><ref name="ConcisePathology-Signs" /><ref name="auto" /> Examples of loss of function include pain that inhibits mobility, severe swelling that prevents movement, having a worse sense of smell during a cold, or having difficulty breathing when bronchitis is present.<ref>{{Cite book |url=https://www.ncbi.nlm.nih.gov/books/NBK279298/ |title=InformedHealth.org [Internet] |date=22 February 2018 |publisher=Institute for Quality and Efficiency in Health Care (IQWiG) |via=www.ncbi.nlm.nih.gov}}</ref><ref>{{Cite web |date=11 March 2024 |title=Inflammation | Definition, Symptoms, Treatment, & Facts | Britannica |url=https://www.britannica.com/science/inflammation |website=www.britannica.com}}</ref> Loss of function has multiple causes.<ref name="ConcisePathology-Signs" /> |
|||
* [[Dolor]] ([[pain]]) |
|||
* [[Calor]] ([[heat]]) |
|||
==== Acute process ==== |
|||
* [[Rubor]] (redness) |
|||
{{More medical citations needed|section|date=April 2023}} |
|||
* [[Tumor]] ([[swelling]]) |
|||
[[File:Events in Acute Inflammation.pdf|thumb|569x569px|A flowchart depicting the events of acute inflammation.<ref>{{Cite book |title=Pathologic basis of disease |vauthors=Robbins S, Cotran R, Kumar V, Abbas A, Aster J |date=2020 |publisher=Saunders Elsevier |edition=10th |location=Philadelphia, PA}}</ref>]] |
|||
* [[Functio laesa]] (loss of function)<ref name="Ruth Werner: A massage Therapist Guide to Pathology 4th edition">[http://thepoint.lww.com/Book/ShowWithResource/2931?resourceId=16419 A Massage Therapist Guide to Pathology] {{cite book|author= Ruth Werner |publisher=Wolters Kluwer |location=Philadelphia, PA and Baltimore, MD |year= 2009 |title=A massage Therapist Guide to Pathology |edition=4th}}</ref> |
|||
[[File:Granulation tissue low power.jpg|thumb|[[Micrograph]] showing granulation tissue. [[H&E stain]].]] |
|||
The process of acute inflammation is initiated by resident immune cells already present in the involved tissue, mainly resident [[macrophages]], [[dendritic cells]], [[histiocytes]], [[Kupffer cells]] and [[mast cell]]s. These cells possess surface receptors known as ''[[pattern recognition receptor]]s'' (PRRs), which recognize (i.e., bind) two subclasses of molecules: [[pathogen-associated molecular pattern]]s (PAMPs) and [[damage-associated molecular pattern]]s (DAMPs). PAMPs are compounds that are associated with various [[pathogen]]s, but which are distinguishable from host molecules. DAMPs are compounds that are associated with host-related injury and cell damage. |
|||
At the onset of an infection, burn, or other injuries, these cells undergo activation (one of the PRRs recognize a PAMP or DAMP) and release inflammatory mediators responsible for the clinical signs of inflammation. Vasodilation and its resulting increased blood flow causes the redness (''rubor'') and increased heat (''calor''). Increased permeability of the blood vessels results in an exudation (leakage) of [[blood plasma|plasma]] proteins and fluid into the tissue ([[edema]]), which manifests itself as swelling (''tumor''). Some of the released mediators such as [[bradykinin]] increase the sensitivity to pain ([[hyperalgesia]], ''dolor''). The mediator molecules also alter the blood vessels to permit the migration of leukocytes, mainly [[neutrophils]] and [[macrophages]], to flow out of the blood vessels (extravasation) and into the tissue. The neutrophils migrate along a [[chemotactic]] gradient created by the local cells to reach the site of injury.<ref name="robspath" /> The loss of function (''functio laesa'') is probably the result of a neurological reflex in response to pain. |
|||
In addition to cell-derived mediators, several acellular biochemical cascade systems—consisting of preformed plasma proteins—act in parallel to initiate and propagate the inflammatory response. These include the [[complement system]] activated by bacteria and the [[coagulation system|coagulation]] and [[fibrinolysis system]]s activated by [[necrosis]] (e.g., burn, trauma).<ref name="robspath" /> |
|||
Acute inflammation may be regarded as the first line of defense against injury. Acute inflammatory response requires constant stimulation to be sustained. Inflammatory mediators are short-lived and are quickly degraded in the tissue. Hence, acute inflammation begins to cease once the stimulus has been removed.<ref name="robspath" /> |
|||
The first four (classical signs) were described by [[Aulus Cornelius Celsus|Celsus]] (ca 30 BC–38 AD),<ref>{{cite book |first=Wolfgang H. |last=Vogel |first2=Andreas |last2=Berke |year=2009 |url=http://books.google.com/books?id=t_5pzrF1QocC&pg=PA97&dq&hl=en#v=onepage&q=&f=false |title=Brief History of Vision and Ocular Medicine |publisher=Kugler Publications |page=97 |isbn=90-6299-220-X }}</ref> while ''loss of function'' was added later by [[Galen]]<ref name="isbn0-7817-7087-4">{{cite book |author=Porth, Carol |title=Essentials of pahtophysiology: concepts of altered health states |publisher=Lippincott Williams & Wilkins |location=Hagerstown, MD |year=2007 |pages=270 |isbn=0-7817-7087-4 |oclc= |doi= |accessdate=}}</ref> even though the attribution is disputed and the origination of the fifth sign has also been ascribed to [[Thomas Sydenham]]<ref name="isbn0-300-11322-6">{{cite book |author=Dormandy, Thomas |title=The worst of evils: man's fight against pain |publisher=Yale University Press |location=New Haven, Conn |year=2006 |pages=22 |isbn=0-300-11322-6 |oclc= |doi= |accessdate=}}</ref> and [[Rudolf Ludwig Karl Virchow|Virchow]].<ref name="robspath">{{cite book | title=Robbins Pathologic Basis of Disease| last=Cotran| coauthors=Kumar, Collins| publisher=W.B Saunders Company| location=Philadelphia| isbn=0-7216-7335-X | year=1998}}</ref><ref name="ConcisePathology-Signs" /> |
|||
=== Chronic === |
|||
Redness and heat are due to increased blood flow at body core temperature to the inflamed site; swelling is caused by accumulation of fluid; [[pain]] is due to release of chemicals that stimulate nerve endings. Loss of function has multiple causes.<ref name="ConcisePathology-Signs" /> |
|||
{{main|Chronic inflammation}} |
|||
Chronic inflammation is inflammation that lasts for months or years.<ref name="pmid29630225">{{Cite web|vauthors=Pahwa R, Goyal A, Bansal P, Jialal I |date=7 August 2023 |title=Chronic inflammation |url=https://www.ncbi.nlm.nih.gov/books/NBK493173/ |publisher=StatPearls, US National Library of Medicine |pmid=29630225|access-date=29 December 2024}}</ref> Macrophages, [[lymphocytes]], and [[plasma cells]] predominate in chronic inflammation, in contrast to the neutrophils that predominate in acute inflammation.<ref name="pmid29630225" /> [[Type 2 diabetes|Diabetes]], [[cardiovascular disease]], [[Allergy|allergies]], and [[chronic obstructive pulmonary disease]] are examples of diseases mediated by chronic inflammation.<ref name="pmid29630225" /> [[Obesity]], smoking, stress and insufficient diet are some of the factors that promote chronic inflammation.<ref name="pmid29630225" /> |
|||
====Cardinal signs==== |
|||
These five signs appear when acute inflammation occurs on the body's surface, whereas acute inflammation of internal organs may not result in the full set. Pain only happens where the appropriate sensory nerve endings exist in the inflamed area—e.g., acute inflammation of the lung ([[pneumonia]]) does not cause pain unless the inflammation involves the [[parietal pleura]], which does have [[nociceptor|pain-sensitive nerve endings]].<ref name="ConcisePathology-Signs" /> |
|||
Common signs and symptoms that develop during chronic inflammation are:<ref name="pmid29630225"/> |
|||
* Body pain, [[arthralgia]], [[myalgia]] |
|||
* Chronic fatigue and insomnia |
|||
* Depression, anxiety and mood disorders |
|||
* Gastrointestinal complications such as constipation, diarrhea, and acid reflux |
|||
* Weight gain or loss |
|||
* Frequent infections |
|||
== Vascular component == |
|||
=== Process of acute inflammation === |
|||
{{More medical citations needed|section|date=March 2021}} |
|||
=== Vasodilation and increased permeability === |
|||
[[Image:Acute inflammation of prostate.jpg|thumb|[[Micrograph]] showing acute inflammation of the [[prostate gland]] with the characteristic [[neutrophil]]ic infiltrate. [[H&E stain]].]] |
|||
The process of acute inflammation is initiated by cells already present in all tissues, mainly resident [[macrophages]], [[dendritic cells]], histiocytes, Kupffer cells and [[mastocytes]]. At the onset of an infection, burn, or other injuries, these cells undergo activation and release [[inflammatory mediators]] responsible for the clinical signs of inflammation. Vasodilation and its resulting increased blood flow causes the redness (''rubor'') and increased heat (''calor''). Increased permeability of the blood vessels results in an exudation (leakage) of [[blood plasma|plasma]] proteins and fluid into the tissue ([[edema]]), which manifests itself as swelling (''tumor''). Some of the released mediators such as [[bradykinin]] increase the sensitivity to pain ([[hyperalgesia]], ''dolor''). The mediator molecules also alter the blood vessels to permit the migration of leukocytes, mainly [[neutrophils]], outside of the blood vessels (extravasation) into the tissue. The neutrophils migrate along a [[chemotactic]] gradient created by the local cells to reach the site of injury.<ref name="robspath" /> The loss of function (''functio laesa'') is probably the result of a neurological reflex in response to pain. |
|||
As defined, acute inflammation is an immunovascular response to inflammatory stimuli, which can include infection or trauma.<ref name=":1">{{Cite journal |vauthors=Raiten DJ, Sakr Ashour FA, Ross AC, Meydani SN, Dawson HD, Stephensen CB, Brabin BJ, Suchdev PS, van Ommen B |date=May 2015 |title=Inflammation and Nutritional Science for Programs/Policies and Interpretation of Research Evidence (INSPIRE) |journal=The Journal of Nutrition |volume=145 |issue=5 |pages=1039S–1108S |doi=10.3945/jn.114.194571 |pmc=4448820 |pmid=25833893}}</ref><ref>{{Cite journal |vauthors=Taams LS |date=July 2018 |title=Inflammation and immune resolution |journal=Clinical and Experimental Immunology |volume=193 |issue=1 |pages=1–2 |doi=10.1111/cei.13155 |pmc=6037995 |pmid=29987840}}</ref> This means acute inflammation can be broadly divided into a vascular phase that occurs first, followed by a cellular phase involving immune cells (more specifically myeloid [[granulocytes]] in the acute setting).<ref name=":1" /> The vascular component of acute inflammation involves the movement of [[Blood plasma|plasma fluid]], containing important [[protein]]s such as [[fibrin]] and [[immunoglobulin]]s ([[antibodies]]), into inflamed tissue. |
|||
In addition to cell-derived mediators, several acellular biochemical cascade systems consisting of preformed plasma proteins act in parallel to initiate and propagate the inflammatory response. These include the [[complement system]] activated by bacteria, and the [[coagulation system|coagulation]] and [[fibrinolysis system]]s activated by [[necrosis]], e.g. a burn or a trauma.<ref name="robspath" /> |
|||
Upon contact with PAMPs, tissue [[macrophages]] and [[mastocytes]] release vasoactive amines such as [[histamine]] and [[serotonin]], as well as [[eicosanoids]] such as [[prostaglandin E2]] and [[leukotriene B4]] to remodel the local vasculature.<ref name=":2">{{Cite journal |vauthors=Medzhitov R |date=July 2008 |title=Origin and physiological roles of inflammation |journal=Nature |volume=454 |issue=7203 |pages=428–435 |bibcode=2008Natur.454..428M |doi=10.1038/nature07201 |pmid=18650913 |s2cid=205214291}}</ref> Macrophages and endothelial cells release [[nitric oxide]].<ref>{{Cite journal |vauthors=Mantovani A, Garlanda C |date=February 2023 |title=Humoral Innate Immunity and Acute-Phase Proteins |journal=The New England Journal of Medicine |volume=388 |issue=5 |pages=439–452 |doi=10.1056/NEJMra2206346 |pmc=9912245 |pmid=36724330 |veditors=Longo DL}}</ref> These mediators vasodilate and permeabilize the [[blood vessel]]s, which results in the net distribution of [[blood plasma]] from the vessel into the tissue space. The increased collection of fluid into the tissue causes it to swell ([[edema]]).<ref name=":2" /> This exuded tissue fluid contains various antimicrobial mediators from the plasma such as [[complement system|complement]], [[lysozyme]], [[antibodies]], which can immediately deal damage to microbes, and [[Opsonin|opsonise]] the microbes in preparation for the cellular phase. If the inflammatory stimulus is a lacerating wound, exuded [[platelet]]s, [[coagulation system|coagulant]]s, [[plasmin]] and [[kinin]]s can [[clot]] the wounded area using vitamin K-dependent mechanisms<ref>{{cite book | vauthors = Ferland G | chapter = Vitamin K |date=2020 | title = Present Knowledge in Nutrition |pages=137–153 | chapter-url = https://linkinghub.elsevier.com/retrieve/pii/B9780323661621000081 |access-date=2023-02-17 |publisher=Elsevier |language=en |doi=10.1016/b978-0-323-66162-1.00008-1 |isbn=978-0-323-66162-1}}</ref> and provide [[haemostasis]] in the first instance. These clotting mediators also provide a structural staging framework at the inflammatory tissue site in the form of a [[fibrin]] lattice – as would construction [[scaffolding]] at a construction site – for the purpose of aiding phagocytic debridement and [[wound healing|wound repair]] later on. Some of the exuded tissue fluid is also funneled by [[lymphatics]] to the regional lymph nodes, flushing bacteria along to start the recognition and attack phase of the [[adaptive immune system]]. |
|||
The acute inflammatory response requires constant stimulation to be sustained. Inflammatory mediators have short half lives and are quickly degraded in the tissue. Hence, acute inflammation ceases once the stimulus has been removed.<ref name="robspath" /> |
|||
[[File:Toe.JPG|thumb|right|230px|Infected [[ingrown toenail]] showing the characteristic redness and swelling associated with acute inflammation]] |
|||
== Exudative component == |
|||
The ''[[exudative component]]'' involves the movement of [[plasma fluid]], containing important [[protein]]s such as [[fibrin]] and [[immunoglobulin]]s ([[antibodies]]), into inflamed tissue. This movement is achieved via the chemically induced dilation and increased permeability of [[blood vessel]]s, which results in a net loss of [[blood plasma]]. The increased collection of fluid into the tissue causes it to swell ([[edema]]). This extravasated fluid is funneled by [[lymphatics]] to the regional lymph nodes, flushing bacteria along to start the recognition and attack phase of the [[adaptive immune system]] system. |
|||
Acute inflammation is characterized by marked vascular changes, including [[vasodilation]], increased permeability and increased blood flow, which are induced by the actions of various inflammatory mediators.<ref name=":2" /> Vasodilation occurs first at the [[arteriole]] level, progressing to the [[capillary]] level, and brings about a net increase in the amount of blood present, causing the redness and heat of inflammation. Increased permeability of the vessels results in the movement of [[blood plasma|plasma]] into the tissues, with resultant [[Venous stasis|stasis]] due to the increase in the concentration of the cells within blood – a condition characterized by enlarged vessels packed with cells. Stasis allows [[leukocytes]] to marginate (move) along the [[endothelium]], a process critical to their recruitment into the tissues. Normal flowing blood prevents this, as the [[Shear stress|shearing force]] along the periphery of the vessels moves cells in the blood into the middle of the vessel. |
|||
=== Vascular changes === |
|||
Acute inflammation is characterised by marked vascular changes, including [[vasodilation]], increased permeability and the slowing of blood flow, which are induced by the actions of various inflammatory mediators. Vasodilation occurs first at the [[arteriole]] level, progressing to the [[capillary]] level, and brings about a net increase in the amount of blood present, causing the redness and heat of inflammation. Increased permeability of the vessels results in the movement of [[blood plasma|plasma]] into the tissues, with resultant ''[[stasis]]'' due to the increase in the concentration of the cells within blood - a condition characterized by enlarged vessels packed with cells. Stasis allows [[leukocytes]] to marginate (move) along the [[endothelium]], a process critical to their recruitment into the tissues. Normal flowing blood prevents this, as the [[Shear stress|shearing force]] along the periphery of the vessels moves cells in the blood into the middle of the vessel. |
|||
=== Plasma cascade systems === |
=== Plasma cascade systems === |
||
* The [[complement system]], when activated, |
* The [[complement system]], when activated, creates a cascade of chemical reactions that promotes [[Antibody opsonization|opsonization]], [[chemotaxis]], and [[agglutination (biology)|agglutination]], and produces the [[Membrane attack complex|MAC]]. |
||
* The [[kinin system]] generates proteins capable of sustaining vasodilation and other physical inflammatory effects. |
* The [[kinin system]] generates proteins capable of sustaining vasodilation and other physical inflammatory effects. |
||
* The [[coagulation system]] or ''clotting cascade'' which forms a protective protein mesh over sites of injury. |
* The [[coagulation system]] or ''clotting cascade'', which forms a protective protein mesh over sites of injury. |
||
* The [[fibrinolysis system]], which acts in opposition to the ''coagulation system'', to counterbalance clotting and generate several other inflammatory mediators. |
* The [[fibrinolysis system]], which acts in opposition to the ''coagulation system'', to counterbalance clotting and generate several other inflammatory mediators. |
||
=== Plasma |
=== Plasma-derived mediators === |
||
{{small|''* non-exhaustive list''}} |
|||
{| class="wikitable" |
{| class="wikitable" |
||
! |
! Name || Produced by || Description |
||
|- |
|- |
||
| align="center" | '''[[Bradykinin]]''' || align="center" | ''[[Kinin system]]'' || A vasoactive protein |
| align="center" | '''[[Bradykinin]]''' || align="center" | ''[[Kinin system]]'' || A vasoactive protein that is able to induce vasodilation, increase vascular permeability, cause smooth muscle contraction, and induce pain. |
||
|- |
|- |
||
| align="center" | '''[[C3 (complement)|C3]]''' || align="center" | ''[[Complement system]]'' || Cleaves to produce ''C3a'' and ''C3b''. C3a stimulates histamine release by mast cells, thereby producing vasodilation. C3b is able to bind to bacterial cell walls and act as an [[opsonin]], which marks the invader as a target for [[phagocytosis]]. |
| align="center" | '''[[C3 (complement)|C3]]''' || align="center" | ''[[Complement system]]'' || Cleaves to produce ''C3a'' and ''C3b''. C3a stimulates histamine release by mast cells, thereby producing vasodilation. C3b is able to bind to bacterial cell walls and act as an [[opsonin]], which marks the invader as a target for [[phagocytosis]]. |
||
|- |
|- |
||
| align="center" | '''[[C5a]]''' || align="center" | ''[[Complement system]]'' || Stimulates histamine release by mast cells, thereby producing vasodilation. It is also able to act as a [[chemoattractant]] to direct cells via chemotaxis to the site of inflammation. |
| align="center" | '''[[Complement component 5a|C5a]]''' || align="center" | ''[[Complement system]]'' || Stimulates histamine release by mast cells, thereby producing vasodilation. It is also able to act as a [[chemoattractant]] to direct cells via chemotaxis to the site of inflammation. |
||
|- |
|- |
||
| align="center" | '''[[Factor XII]]''' (''Hageman Factor'') || align="center" | ''[[Liver]]'' || A protein |
| align="center" | '''[[Factor XII]]''' (''Hageman Factor'') || align="center" | ''[[Liver]]'' || A protein that circulates inactively, until activated by collagen, platelets, or exposed [[basement membrane]]s via [[conformational change]]. When activated, it in turn is able to activate three plasma systems involved in inflammation: the kinin system, fibrinolysis system, and coagulation system. |
||
|- |
|- |
||
| align="center" | '''[[Membrane attack complex]]''' || align="center" | ''[[Complement system]]'' || A complex of the complement proteins [[C5b]], [[Complement component 6|C6]], [[Complement component 7|C7]], [[C8 complex|C8]], and multiple units of [[Complement component 9|C9]]. The combination and activation of this range of complement proteins forms the ''membrane attack complex'', which is able to insert into bacterial cell walls and causes cell lysis with ensuing death. |
| align="center" | '''[[Membrane attack complex]]''' || align="center" | ''[[Complement system]]'' || A complex of the complement proteins [[C5b]], [[Complement component 6|C6]], [[Complement component 7|C7]], [[C8 complex|C8]], and multiple units of [[Complement component 9|C9]]. The combination and activation of this range of complement proteins forms the ''membrane attack complex'', which is able to insert into bacterial cell walls and causes cell lysis with ensuing bacterial death. |
||
|- |
|- |
||
| align="center" | '''[[Plasmin]]''' || align="center" | ''[[Fibrinolysis system]]'' || Able to break down fibrin clots, cleave complement protein C3, and activate Factor XII. |
| align="center" | '''[[Plasmin]]''' || align="center" | ''[[Fibrinolysis system]]'' || Able to break down fibrin clots, cleave complement protein C3, and activate Factor XII. |
||
| Line 120: | Line 217: | ||
== Cellular component == |
== Cellular component == |
||
The ''cellular component'' involves [[leukocyte]]s, which normally reside in blood and must move into the inflamed tissue via ''extravasation'' to aid in inflammation. Some act as [[phagocyte]]s, ingesting |
The ''cellular component'' involves [[leukocyte]]s, which normally reside in blood and must move into the inflamed tissue via ''extravasation'' to aid in inflammation.<ref name=":1" /> Some act as [[phagocyte]]s, ingesting bacteria, viruses, and cellular debris. Others release enzymatic [[granule (cell biology)|granules]] that damage pathogenic invaders. Leukocytes also release inflammatory mediators that develop and maintain the inflammatory response. In general, acute inflammation is mediated by [[granulocyte]]s, whereas chronic inflammation is mediated by mononuclear cells such as [[monocyte]]s and [[lymphocyte]]s. |
||
=== Leukocyte extravasation === |
=== Leukocyte extravasation === |
||
[[ |
[[File:NeutrophilerAktion.svg|200px|thumb|right|Neutrophils migrate from blood vessels to the infected tissue via chemotaxis, where they remove pathogens through phagocytosis and degranulation]] |
||
[[File:Immune response.svg|thumb|Inflammation is a process by which the body's white blood cells and substances they produce protect us from infection with foreign organisms, such as bacteria and viruses. The (phagocytes) white blood cells are a nonspecific immune response, meaning that they attack any foreign bodies. However, in some diseases, like arthritis, the body's defense system the immune system triggers an inflammatory response when there are no foreign invaders to fight off. In these diseases, called autoimmune diseases, the body's normally protective immune system causes damage to its own tissues. The body responds as if normal tissues are infected or somehow abnormal.]] |
|||
{{Main|Leukocyte extravasation}} |
{{Main|Leukocyte extravasation}} |
||
Various [[leukocyte]]s are critically involved in the initiation and maintenance of inflammation. These cells must be able to |
Various [[leukocyte]]s, particularly neutrophils, are critically involved in the initiation and maintenance of inflammation. These cells must be able to move to the site of injury from their usual location in the blood, therefore mechanisms exist to recruit and direct leukocytes to the appropriate place. The process of leukocyte movement from the blood to the tissues through the blood vessels is known as ''extravasation'' and can be broadly divided up into a number of steps: |
||
# '''Leukocyte |
# '''Leukocyte margination and endothelial adhesion:''' The white blood cells within the vessels which are generally centrally located move peripherally towards the walls of the vessels.<ref name=":0">{{Cite book |title=Muir's Textbook of Pathology |vauthors=Herrington S |publisher=CRC Press |year=2014 |isbn=978-1-4441-8499-0 |edition=15th |pages=59}}</ref> Activated macrophages in the tissue release [[cytokines]] such as [[Interleukin 1|IL-1]] and [[TNFα]], which in turn leads to production of [[chemokine]]s that bind to [[proteoglycan]]s forming gradient in the inflamed tissue and along the [[endothelial]] wall.<ref name=":2" /> Inflammatory cytokines induce the immediate expression of [[P-selectin]] on endothelial cell surfaces and P-selectin binds weakly to carbohydrate ligands on the surface of leukocytes and causes them to "roll" along the endothelial surface as bonds are made and broken. Cytokines released from injured cells induce the expression of [[E-selectin]] on endothelial cells, which functions similarly to P-selectin. Cytokines also induce the expression of [[integrin]] ligands such as [[ICAM-1]] and [[VCAM-1]] on endothelial cells, which mediate the adhesion and further slow leukocytes down. These weakly bound leukocytes are free to detach if not activated by chemokines produced in injured tissue after [[signal transduction]] via respective [[G protein-coupled receptors]] that activates integrins on the leukocyte surface for firm adhesion. Such activation increases the affinity of bound integrin receptors for ICAM-1 and VCAM-1 on the endothelial cell surface, firmly binding the leukocytes to the endothelium. |
||
# '''Migration across the endothelium, known as'' transmigration, ''via the process of diapedesis:''' Chemokine gradients stimulate the adhered leukocytes to move between endothelial cells and pass the basement membrane into the |
# '''Migration across the endothelium, known as'' transmigration, ''via the process of [[diapedesis]]:''' Chemokine gradients stimulate the adhered leukocytes to move between adjacent endothelial cells. The endothelial cells retract and the leukocytes pass through the basement membrane into the surrounding tissue using adhesion molecules such as ICAM-1.<ref name=":0" /> |
||
# '''Movement of leukocytes within the tissue via [[chemotaxis]]:''' Leukocytes reaching the tissue interstitium bind to [[extracellular matrix]] proteins via expressed integrins and [[CD44]] to prevent |
# '''Movement of leukocytes within the tissue via [[chemotaxis]]:''' Leukocytes reaching the tissue interstitium bind to [[extracellular matrix]] proteins via expressed integrins and [[CD44]] to prevent them from leaving the site. A variety of molecules behave as [[chemoattractant]]s, for example, C3a or C5a (the [[anaphylatoxins]]), and cause the leukocytes to move along a chemotactic gradient towards the source of inflammation. |
||
=== |
=== Phagocytosis === |
||
{{Main|Phagocyte}} |
|||
<small>''* non-exhaustive list''</small> |
|||
Extravasated neutrophils in the cellular phase come into contact with microbes at the inflamed tissue. [[Phagocyte]]s express cell-surface endocytic [[pattern recognition receptors]] (PRRs) that have affinity and efficacy against non-specific [[microbe-associated molecular patterns]] (PAMPs). Most PAMPs that bind to endocytic PRRs and initiate [[phagocytosis]] are cell wall components, including complex carbohydrates such as [[mannans]] and β-[[glucans]], [[lipopolysaccharides]] (LPS), [[peptidoglycans]], and surface proteins. Endocytic PRRs on phagocytes reflect these molecular patterns, with [[C-type lectin]] receptors binding to mannans and β-glucans, and [[scavenger receptor (immunology)|scavenger receptor]]s binding to LPS. |
|||
Upon endocytic PRR binding, [[actin]]-[[myosin]] [[cytoskeletal]] rearrangement adjacent to the plasma membrane occurs in a way that [[endocytosis|endocytoses]] the plasma membrane containing the PRR-PAMP complex, and the microbe. [[Phosphatidylinositol]] and [[Vps34]]-[[PIK3R4|Vps15]]-[[BECN1|Beclin1]] signalling pathways have been implicated to traffic the endocytosed phagosome to intracellular [[lysosomes]], where fusion of the phagosome and the lysosome produces a phagolysosome. The [[reactive oxygen species]], [[superoxides]] and [[hypochlorite]] bleach within the phagolysosomes then kill microbes inside the phagocyte. |
|||
Phagocytic efficacy can be enhanced by [[opsonization]]. Plasma derived complement [[C3b]] and antibodies that exude into the inflamed tissue during the vascular phase bind to and coat the microbial antigens. As well as endocytic PRRs, phagocytes also express [[opsonin]] receptors [[Fc receptor]] and [[complement receptor 1]] (CR1), which bind to antibodies and C3b, respectively. The co-stimulation of endocytic PRR and opsonin receptor increases the efficacy of the phagocytic process, enhancing the [[lysosomal]] elimination of the infective agent. |
|||
=== Cell-derived mediators === |
|||
{{small|''* non-exhaustive list''}} |
|||
{| class="wikitable" |
{| class="wikitable" |
||
! |
!Name || Type || Source || Description |
||
|- |
|- |
||
| align="center" | '''[[Granule (cell biology)|Lysosome granules]]''' || align="center" | ''[[Enzyme]]s'' || align="center" | [[Granulocyte]]s || These cells contain a large variety of enzymes |
| align="center" | '''[[Granule (cell biology)|Lysosome granules]]''' || align="center" | ''[[Enzyme]]s'' || align="center" | [[Granulocyte]]s || These cells contain a large variety of enzymes that perform a number of functions. Granules can be classified as either ''[[Specific granules|specific]]'' or ''[[azurophil]]ic'' depending upon the contents, and are able to break down a number of substances, some of which may be plasma-derived proteins that allow these enzymes to act as inflammatory mediators. |
||
|- |
|- |
||
| align="center" | '''[[ |
| align="center" | '''[[Granulocyte-macrophage colony-stimulating factor|GM-CSF]]''' || align="center" | ''[[Glycoprotein]]'' || align="center" | Macrophages, monocytes, T-cells, B-cells, and tissue-resident cells || Elevated GM-CSF has been shown to contribute to inflammation in [[inflammatory arthritis]], [[osteoarthritis]], [[colitis]] [[asthma]], [[obesity]], and [[Coronavirus disease 2019|COVID-19]]. |
||
|- |
|||
| align="center" | '''[[Histamine]]''' || align="center" | ''[[Monoamine]]'' || align="center" | Mast cells and basophils || Stored in preformed granules, histamine is released in response to a number of stimuli. It causes [[arteriole]] dilation, increased [[venous]] permeability, and a wide variety of organ-specific effects. |
|||
|- |
|- |
||
| align="center" | '''[[Interferon gamma|IFN-γ]]''' || align="center" | ''[[Cytokine]]'' || align="center" | T-cells, NK cells || Antiviral, immunoregulatory, and anti-tumour properties. This interferon was originally called macrophage-activating factor, and is especially important in the maintenance of chronic inflammation. |
| align="center" | '''[[Interferon gamma|IFN-γ]]''' || align="center" | ''[[Cytokine]]'' || align="center" | T-cells, NK cells || Antiviral, immunoregulatory, and anti-tumour properties. This interferon was originally called macrophage-activating factor, and is especially important in the maintenance of chronic inflammation. |
||
|- |
|||
| align="center" | '''[[Interleukin 6|IL-6]]''' || align="center" | ''[[Cytokine]]'' and ''[[Myokine]]'' || align="center" | Macrophages, osteoblasts, adipocytes, and smooth muscle cells (cytokine) Skeletal muscle cells (myokine) || Pro-inflammatory cytokine secreted by macrophages in response to [[pathogen-associated molecular pattern]]s (PAMPs); pro-inflammatory cytokine secreted by adipocytes, especially in obesity; anti-inflammatory myokine secreted by skeletal muscle cells in response to exercise. |
|||
|- |
|- |
||
| align="center" | '''[[Interleukin 8|IL-8]]''' || align="center" | ''[[Chemokine]]'' || align="center" | Primarily [[macrophage]]s || Activation and chemoattraction of neutrophils, with a weak effect on monocytes and eosinophils. |
| align="center" | '''[[Interleukin 8|IL-8]]''' || align="center" | ''[[Chemokine]]'' || align="center" | Primarily [[macrophage]]s || Activation and chemoattraction of neutrophils, with a weak effect on monocytes and eosinophils. |
||
|- |
|- |
||
| align="center" | '''[[Leukotriene B4]]''' || align="center" | ''[[Eicosanoid]]'' || align="center" | Leukocytes || Able to mediate leukocyte adhesion and activation, allowing them to bind to the endothelium and migrate across it. In neutrophils, it is also a potent chemoattractant, and is able to induce the formation of reactive oxygen species and the release of |
| align="center" | '''[[Leukotriene B4]]''' || align="center" | ''[[Eicosanoid]]'' || align="center" | [[Leukocytes]], cancer cells || Able to mediate leukocyte adhesion and activation, allowing them to bind to the endothelium and migrate across it. In neutrophils, it is also a potent chemoattractant, and is able to induce the formation of reactive oxygen species and the release of lysosomal enzymes by these cells. |
||
|- |
|||
| align="center" | '''[[LTC4]]''', '''[[LTD4]]''' || align="center" | ''[[Eicosanoid]]'' || align="center" | [[eosinophils]], [[mast cells]], [[macrophages]] || These three [[Cysteine]]-containing leukotrienes contract lung airways, increase micro-vascular permeability, stimulate mucus secretion, and promote eosinophil-based inflammation in the lung, skin, nose, eye, and other tissues. |
|||
|- |
|||
| align="center" | '''[[5-oxo-eicosatetraenoic acid]]''' || align="center" | ''[[Eicosanoid]]'' || align="center" | [[Leukocytes]], cancer cells || Potent stimulator of neutrophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation; monocyte chemotaxis; and with even greater potency eosinophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation. |
|||
|- |
|||
| align="center" | '''[[5-HETE]]''' || align="center" | ''[[Eicosanoid]]'' || align="center" | [[Leukocytes]] || Metabolic precursor to 5-Oxo-eicosatetraenoic acid, it is a less potent stimulator of neutrophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation; monocyte chemotaxis; and eosinophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation. |
|||
|- |
|||
| align="center" | '''[[Prostaglandin]]s''' || align="center" | ''[[Eicosanoid]]'' || align="center" | Mast cells || A group of lipids that can cause vasodilation, fever, and pain. |
|||
|- |
|- |
||
| align="center" | '''[[Nitric oxide]]''' || align="center" | ''Soluble gas'' || align="center" | Macrophages, endothelial cells, some neurons || Potent vasodilator, relaxes smooth muscle, reduces platelet aggregation, aids in leukocyte recruitment, direct antimicrobial activity in high concentrations. |
| align="center" | '''[[Nitric oxide]]''' || align="center" | ''Soluble gas'' || align="center" | Macrophages, endothelial cells, some neurons || Potent vasodilator, relaxes smooth muscle, reduces platelet aggregation, aids in leukocyte recruitment, direct antimicrobial activity in high concentrations. |
||
|- |
|- |
||
| align="center" | '''[[Tumor necrosis factor-alpha|TNF-α]] and [[Interleukin 1|IL-1]]''' || align="center" | ''[[Cytokine]]s'' || align="center" | Primarily macrophages || Both affect a wide variety of cells to induce many similar inflammatory reactions: fever, production of cytokines, endothelial gene regulation, chemotaxis, leukocyte adherence, activation of [[fibroblast]]s. Responsible for the systemic effects of inflammation, such as loss of appetite and increased heart rate. TNF-α inhibits osteoblast differentiation. |
|||
| align="center" | '''[[Prostaglandin]]s''' || align="center" | ''[[Eicosanoid]]'' || align="center" | Mast cells || A group of lipids which can cause vasodilation, fever, and pain. |
|||
|- |
|- |
||
| align="center" | '''[[Tryptase]]''' || align="center" | ''[[Enzyme]]s'' || align="center" | Mast Cells || This serine protease is believed to be exclusively stored in mast cells and secreted, along with histamine, during mast cell activation.<ref>{{Cite book |url=https://www.ncbi.nlm.nih.gov/books/NBK200913/ |title=Itch: Mechanisms and Treatment |vauthors=Carstens E, Akiyama T, Cevikbas F, Kempkes C, Buhl T, Mess C, Buddenkotte J, Steinhoff M |date=2014 |publisher=CRC Press/Taylor & Francis |isbn=978-1-4665-0543-8 |veditors=Carstens M, Akiyama T |series=Frontiers in Neuroscience |location=Boca Raton (FL) |chapter=Role of Interleukin-31 and Oncostatin M in Itch and Neuroimmune Communication |pmid=24830021}}</ref><ref>{{Cite journal |vauthors=Caughey GH |date=June 2007 |title=Mast cell tryptases and chymases in inflammation and host defense |journal=Immunological Reviews |volume=217 |issue=1 |pages=141–54 |doi=10.1111/j.1600-065x.2007.00509.x |pmc=2275918 |pmid=17498057}}</ref><ref>{{Cite journal |vauthors=Caughey GH |date=May 2016 |title=Mast cell proteases as pharmacological targets |journal=European Journal of Pharmacology |series=Pharmacological modulation of Mast cells and Basophils |volume=778 |pages=44–55 |doi=10.1016/j.ejphar.2015.04.045 |pmc=4636979 |pmid=25958181}}</ref> |
|||
| align="center" | '''[[Tumor necrosis factor-alpha|TNF-α]] and [[Interleukin 1|IL-1]]''' || align="center" | ''[[Cytokine]]s'' || align="center" | Primarily macrophages || Both affect a wide variety of cells to induce many similar inflammatory reactions: fever, production of cytokines, endothelial gene regulation, chemotaxis, leukocyte adherence, activation of [[fibroblast]]s. Responsible for the systemic effects of inflammation, such as loss of appetite and increased heart rate. |
|||
|} |
|} |
||
| Line 155: | Line 273: | ||
Specific patterns of acute and chronic inflammation are seen during particular situations that arise in the body, such as when inflammation occurs on an [[epithelial]] surface, or [[pyogenic]] bacteria are involved. |
Specific patterns of acute and chronic inflammation are seen during particular situations that arise in the body, such as when inflammation occurs on an [[epithelial]] surface, or [[pyogenic]] bacteria are involved. |
||
* '''Granulomatous inflammation:''' Characterised by the formation of [[granuloma]]s, they are the result of a limited but diverse number of diseases, which include among others [[tuberculosis]], [[leprosy]], [[sarcoidosis]], and [[syphilis]]. |
* '''Granulomatous inflammation:''' Characterised by the formation of [[granuloma]]s, they are the result of a limited but diverse number of diseases, which include among others [[tuberculosis]], [[leprosy]], [[sarcoidosis]], and [[syphilis]]. |
||
* '''Fibrinous inflammation:''' Inflammation resulting in a large increase in vascular permeability allows [[fibrin]] to pass through the blood vessels. If an appropriate ''procoagulative'' stimulus is present, such as cancer cells,<ref name="robspath" /> a fibrinous exudate is deposited. This is commonly seen in [[serous membrane|serous cavities]], where the conversion of fibrinous exudate into a |
* '''Fibrinous inflammation:''' Inflammation resulting in a large increase in vascular permeability allows [[fibrin]] to pass through the blood vessels. If an appropriate ''procoagulative'' stimulus is present, such as cancer cells,<ref name="robspath" /> a fibrinous exudate is deposited. This is commonly seen in [[serous membrane|serous cavities]], where the conversion of fibrinous exudate into a scar can occur between serous membranes, limiting their function. The deposit sometimes forms a pseudomembrane sheet. During inflammation of the intestine ([[pseudomembranous colitis]]), pseudomembranous tubes can be formed. |
||
* '''Purulent inflammation:''' Inflammation resulting in large amount of [[pus]], which consists of neutrophils, dead cells, and fluid. Infection by pyogenic bacteria such as [[staphylococci]] is characteristic of this kind of inflammation. Large, localised collections of pus enclosed by surrounding tissues are called [[abscess]]es. |
* '''Purulent inflammation:''' Inflammation resulting in large amount of [[pus]], which consists of neutrophils, dead cells, and fluid. Infection by pyogenic bacteria such as [[staphylococci]] is characteristic of this kind of inflammation. Large, localised collections of pus enclosed by surrounding tissues are called [[abscess]]es. |
||
* '''Serous inflammation:''' Characterised by the copious effusion of non-viscous serous fluid, commonly produced by [[mesothelial]] cells of [[serous membrane]]s, but may be derived from blood plasma. Skin [[blister]]s exemplify this pattern of inflammation. |
* '''Serous inflammation:''' Characterised by the copious effusion of non-viscous serous fluid, commonly produced by [[mesothelial]] cells of [[serous membrane]]s, but may be derived from blood plasma. Skin [[blister]]s exemplify this pattern of inflammation. |
||
* '''Ulcerative inflammation:''' Inflammation occurring near an epithelium can result in the [[necrotic]] loss of tissue from the surface, exposing lower layers. The subsequent excavation in the epithelium is known as an [[ulcer (dermatology)|ulcer]]. |
* '''Ulcerative inflammation:''' Inflammation occurring near an epithelium can result in the [[necrotic]] loss of tissue from the surface, exposing lower layers. The subsequent excavation in the epithelium is known as an [[ulcer (dermatology)|ulcer]]. |
||
== |
== Disorders == |
||
[[File:Asthma (Lungs).png|thumb|215x215px|Asthma is considered an inflammatory-mediated disorder. On the right is an inflamed airway due to asthma.]] |
|||
Abnormalities associated with inflammation comprise a large, officially unrelated group of disorders which underlie a vast variety of human diseases. The immune system is often involved with inflammatory disorders, demonstrated in both [[allergic reaction]]s and some [[myopathies]], with many [[immune system disorder]]s resulting in abnormal inflammation. Non-immune diseases with etiological origins in inflammatory processes are thought to include cancer, [[atherosclerosis]], and [[ischaemic heart disease]].<ref name="robspath" /> |
|||
[[File:CD colitis 2.jpg|thumb|209x209px|Colitis (inflammation of the colon) caused by [[Crohn's disease]].]] |
|||
Inflammatory abnormalities are a large group of disorders that underlie a vast variety of human diseases. The immune system is often involved with inflammatory disorders, as demonstrated in both [[allergic reaction]]s and some [[myopathies]], with many [[immune system disorder]]s resulting in abnormal inflammation. Non-immune diseases with causal origins in inflammatory processes include cancer, [[atherosclerosis]], and [[ischaemic heart disease|ischemic heart disease]].<ref name="robspath" /> |
|||
A large variety of proteins are involved in inflammation, and any one of them is open to a genetic mutation which impairs or otherwise dysregulates the normal function and expression of that protein. |
|||
Examples of disorders associated with inflammation include: |
Examples of disorders associated with inflammation include: |
||
{{div col|colwidth=25em}} |
|||
<div style="-moz-column-count:3; column-count:2;"> |
|||
* [[Acne vulgaris]] |
* [[Acne vulgaris]] |
||
* [[Alzheimer's ]] |
|||
* [[Amyotrophic lateral sclerosis|Amyotrophic Lateral Sclerosis (ALS) "Lou Gehrig's Disease" ]] |
|||
* [[Anemia ]] |
|||
* [[Arthritis ]] |
|||
* [[Asthma]] |
* [[Asthma]] |
||
* [[ADHD]] |
|||
* [[Autoimmune disease]]s |
* [[Autoimmune disease]]s |
||
* [[Autoinflammatory disease]]s |
|||
* [[Cancer]] |
|||
* [[Celiac |
* [[Celiac disease]] |
||
* [[Chronic prostatitis]] |
* [[Asymptomatic inflammatory prostatitis|Chronic prostatitis]] |
||
* [[ |
* [[Ulcerative colitis|Colitis]] |
||
* [[ |
* [[Diverticulitis]] |
||
* [[Familial Mediterranean Fever]] |
|||
* [[Erectile dysfunction|Erectile Dysfunction (ED) ]] |
|||
* [[Fibromyalgia]] |
|||
* [[Glomerulonephritis]] |
* [[Glomerulonephritis]] |
||
* [[ |
* [[Hidradenitis suppurativa]] |
||
* [[HIV|Human Immunodeficiency Virus (HIV) ]] |
|||
* [[Hypersensitivity|Hypersensitivities]] |
* [[Hypersensitivity|Hypersensitivities]] |
||
* [[Inflammatory bowel disease]]s |
* [[Inflammatory bowel disease]]s |
||
* [[Interstitial cystitis]] |
* [[Interstitial cystitis]] |
||
* [[ |
* [[Lichen planus]] |
||
* [[Mast Cell Activation Syndrome]] |
|||
* [[Lupus]] |
|||
* [[ |
* [[Mastocytosis]] |
||
* [[ |
* [[Otitis]] |
||
* [[Multiple Sclerosis ]] |
|||
* [[Myelitis ]] |
|||
* [[Narcolepsy ]] |
|||
* [[Neuropathy]] |
|||
* [[Obesity ]] |
|||
* [[Pelvic inflammatory disease]] |
* [[Pelvic inflammatory disease]] |
||
* [[Peripheral ulcerative keratitis]] |
|||
* [[Poliomyelitis]] |
|||
* [[Pneumonia]] |
|||
* [[Reperfusion injury]] |
* [[Reperfusion injury]] |
||
* [[ |
* [[Rheumatic fever]] |
||
* [[Rheumatoid arthritis]] |
* [[Rheumatoid arthritis]] |
||
* [[Rhinitis]] |
|||
* [[Sarcoidosis]] |
* [[Sarcoidosis]] |
||
* [[Scleroderma]] |
|||
* [[Sjögren's Syndrome]] |
|||
* [[Sleep Apnea]] |
|||
* [[Small bowel bacterial overgrowth syndrome|Small Intestinal Bacterial Overgrowth]] |
|||
* [[Stroke]] |
|||
* [[Tourette's Syndrome]] |
|||
* [[Transplant rejection]] |
* [[Transplant rejection]] |
||
* [[Vasculitis]] |
* [[Vasculitis]] |
||
{{div col end}} |
|||
</div> |
|||
=== Atherosclerosis === |
=== Atherosclerosis === |
||
{{main|Atherosclerosis}} |
|||
Atherosclerosis, formerly considered a bland lipid storage disease, actually involves an ongoing inflammatory response. Recent advances in basic science have established a fundamental role for inflammation in mediating all stages of this disease from initiation through progression and, ultimately, the thrombotic complications of atherosclerosis. These new findings provide important links between risk factors and the mechanisms of atherogenesis. Clinical studies have shown that this emerging biology of inflammation in atherosclerosis applies directly to human patients. Elevation in markers of inflammation predicts outcomes of patients with acute coronary syndromes, independently of myocardial damage. In addition, low-grade chronic inflammation, as indicated by levels of the inflammatory marker C-reactive protein, prospectively defines risk of atherosclerotic complications, thus adding to prognostic information provided by traditional risk factors. Moreover, certain treatments that reduce coronary risk also limit inflammation. In the case of lipid lowering with statins, this anti-inflammatory effect does not appear to correlate with reduction in low-density lipoprotein levels. These new insights into inflammation in atherosclerosis not only increase our understanding of this disease, but also have practical clinical applications in risk stratification and targeting of therapy for this scourge of growing worldwide importance. http://circ.ahajournals.org/cgi/content/full/105/9/1135 |
|||
Atherosclerosis, formerly considered a [[lipid]] storage disorder, is now understood as a chronic inflammatory condition involving the arterial walls.<ref name="libby2021">{{cite journal |vauthors=Libby P |title=Inflammation during the life cycle of the atherosclerotic plaque |journal=Cardiovascular Research |volume=117 |issue=13 |pages=2525–2536 |date=November 2021 |pmid=34550337 |pmc=8783385 |doi=10.1093/cvr/cvab303}}</ref> Research has established a fundamental role for inflammation in mediating all stages of atherosclerosis from initiation through progression and, ultimately, the thrombotic complications from it.<ref name=libby2021/> These new findings reveal links between traditional risk factors like cholesterol levels and the underlying mechanisms of [[atherogenesis]]. |
|||
Clinical studies have shown that this emerging biology of inflammation in atherosclerosis applies directly to people.<ref name="libby2021" /> For instance, elevation in markers of inflammation predicts outcomes of people with [[acute coronary syndrome]]s, independently of myocardial damage. In addition, low-grade chronic inflammation, as indicated by levels of the inflammatory marker [[C-reactive protein]], prospectively defines risk of atherosclerotic complications, thus adding to prognostic information provided by traditional risk factors, such as LDL levels.<ref>{{cite journal | vauthors = Spagnoli LG, Bonanno E, Sangiorgi G, Mauriello A | title = Role of inflammation in atherosclerosis | journal = Journal of Nuclear Medicine | volume = 48 | issue = 11 | pages = 1800–1815 | date = November 2007 | pmid = 17942804 | doi = 10.2967/jnumed.107.038661 }}</ref><ref name=libby2021/> |
|||
=== Allergies === |
|||
An allergic reaction, formally known as [[Type I hypersensitivity|type 1 hypersensitivity]], is the result of an inappropriate immune response triggering inflammation. A common example is [[hay fever]], which is caused by a hypersensitive response by skin [[mast cell]]s to [[allergen]]s. Pre-sensitised mast cells respond by [[degranulation|degranulating]], releasing [[vasoactive]] chemicals such as histamine. These chemicals propagate an excessive inflammatory response characterised by blood vessel dilation, production of pro-inflammatory molecules, cytokine release, and recruitment of leukocytes.<ref name="robspath" /> Severe inflammatory response may mature into a systemic response known as [[anaphylaxis]]. |
|||
Moreover, certain treatments that reduce coronary risk also limit inflammation. Notably, lipid-lowering medications such as [[statin]]s have shown anti-inflammatory effects, which may contribute to their efficacy beyond just lowering LDL levels.<ref>{{cite journal | vauthors = Morofuji Y, Nakagawa S, Ujifuku K, Fujimoto T, Otsuka K, Niwa M, Tsutsumi K | title = Beyond Lipid-Lowering: Effects of Statins on Cardiovascular and Cerebrovascular Diseases and Cancer | journal = Pharmaceuticals | volume = 15 | issue = 2 | pages = 151 | date = January 2022 | pmid = 35215263 | pmc = 8877351 | doi = 10.3390/ph15020151 | doi-access = free }}</ref> This emerging understanding of inflammation's role in atherosclerosis has had significant clinical implications, influencing both risk stratification and therapeutic strategies. |
|||
Other [[hypersensitivity]] reactions (''[[Type II hypersensitivity|type 2]]'' and ''[[Type III hypersensitivity|type 3]]'') are mediated by antibody reactions and induce inflammation by attracting leukocytes which damage surrounding tissue.<ref name="robspath" /> |
|||
==== Emerging treatments ==== |
|||
Recent developments in the treatment of atherosclerosis have focused on addressing inflammation directly. New anti-inflammatory drugs, such as monoclonal antibodies targeting IL-1β, have been studied in large clinical trials, showing promising results in reducing cardiovascular events.<ref>{{cite journal | vauthors = Szekely Y, Arbel Y | title = A Review of Interleukin-1 in Heart Disease: Where Do We Stand Today? | journal = Cardiology and Therapy | volume = 7 | issue = 1 | pages = 25–44 | date = June 2018 | pmid = 29417406 | pmc = 5986669 | doi = 10.1007/s40119-018-0104-3 }}</ref> These drugs offer a potential new avenue for treatment, particularly for patients who do not respond adequately to statins. However, concerns about long-term safety and cost remain significant barriers to widespread adoption. |
|||
==== Connection to depression ==== |
|||
Inflammatory processes can be triggered by negative cognition or their consequences, such as stress, violence, or deprivation. Negative cognition may therefore contribute to inflammation, which in turn can lead to depression. A 2019 meta-analysis found that chronic inflammation is associated with a 30% increased risk of developing major depressive disorder, supporting the link between inflammation and mental health.<ref>{{cite journal | vauthors = Osimo EF, Pillinger T, Rodriguez IM, Khandaker GM, Pariante CM, Howes OD | title = Inflammatory markers in depression: A meta-analysis of mean differences and variability in 5,166 patients and 5,083 controls | journal = Brain, Behavior, and Immunity | volume = 87 | pages = 901–909 | date = July 2020 | pmid = 32113908 | pmc = 7327519 | doi = 10.1016/j.bbi.2020.02.010 }}</ref> |
|||
=== Allergy === |
|||
An allergic reaction, formally known as [[Type I hypersensitivity|type 1 hypersensitivity]], is the result of an inappropriate immune response triggering inflammation, vasodilation, and nerve irritation. A common example is [[hay fever]], which is caused by a hypersensitive response by [[mast cell]]s to [[allergen]]s. Pre-sensitised mast cells respond by [[degranulation|degranulating]], releasing [[vasoactive]] chemicals such as histamine. These chemicals propagate an excessive inflammatory response characterised by blood vessel dilation, production of pro-inflammatory molecules, cytokine release, and recruitment of leukocytes.<ref name="robspath" /> Severe inflammatory response may mature into a systemic response known as [[anaphylaxis]]. |
|||
=== Myopathies === |
=== Myopathies === |
||
Inflammatory myopathies are caused by the immune system inappropriately attacking components of muscle, leading to signs of muscle inflammation. They may occur in conjunction with other immune disorders, such as [[systemic sclerosis]], and include [[dermatomyositis]], [[polymyositis]], and [[inclusion body myositis]].<ref name="robspath" /> |
[[Inflammatory myopathy|Inflammatory myopathies]] are caused by the immune system inappropriately attacking components of muscle, leading to signs of muscle inflammation. They may occur in conjunction with other immune disorders, such as [[systemic sclerosis]], and include [[dermatomyositis]], [[polymyositis]], and [[inclusion body myositis]].<ref name="robspath" /> |
||
=== Leukocyte defects === |
=== Leukocyte defects === |
||
Due to the central role of leukocytes in the development and propagation of inflammation, defects in leukocyte |
Due to the central role of leukocytes in the development and propagation of inflammation, defects in leukocyte functionality often result in a decreased capacity for inflammatory defense with subsequent vulnerability to infection.<ref name="robspath" /> Dysfunctional leukocytes may be unable to correctly bind to blood vessels due to surface receptor mutations, digest bacteria ([[Chédiak–Higashi syndrome]]), or produce [[microbicide]]s ([[chronic granulomatous disease]]). In addition, diseases affecting the [[bone marrow]] may result in abnormal or few leukocytes. |
||
=== Pharmacological === |
=== Pharmacological === |
||
Certain drugs |
Certain drugs or exogenous chemical compounds are known to affect inflammation. [[Vitamin A]] deficiency, for example, causes an increase in inflammatory responses,<ref>{{Cite journal |vauthors=Wiedermann U, Chen XJ, Enerbäck L, Hanson LA, Kahu H, Dahlgren UI |date=December 1996 |title=Vitamin A deficiency increases inflammatory responses |journal=Scandinavian Journal of Immunology |volume=44 |issue=6 |pages=578–84 |doi=10.1046/j.1365-3083.1996.d01-351.x |pmid=8972739 |s2cid=3079540}}</ref> and [[anti-inflammatory]] drugs work specifically by inhibiting the enzymes that produce inflammatory [[eicosanoids]]. Additionally, certain illicit drugs such as [[cocaine]] and [[Ecstasy (drug)|ecstasy]] may exert some of their detrimental effects by activating transcription factors intimately involved with inflammation (e.g. [[NF-κB]]).<ref>{{Cite journal |vauthors=Hargrave BY, Tiangco DA, Lattanzio FA, Beebe SJ |year=2003 |title=Cocaine, not morphine, causes the generation of reactive oxygen species and activation of NF-kappaB in transiently cotransfected heart cells |journal=Cardiovascular Toxicology |volume=3 |issue=2 |pages=141–51 |doi=10.1385/CT:3:2:141 |pmid=14501032 |s2cid=35240781}}</ref><ref>{{Cite journal |vauthors=Montiel-Duarte C, Ansorena E, López-Zabalza MJ, Cenarruzabeitia E, Iraburu MJ |date=March 2004 |title=Role of reactive oxygen species, glutathione and NF-kappaB in apoptosis induced by 3,4-methylenedioxymethamphetamine ("Ecstasy") on hepatic stellate cells |journal=Biochemical Pharmacology |volume=67 |issue=6 |pages=1025–33 |doi=10.1016/j.bcp.2003.10.020 |pmid=15006539}}</ref> |
||
=== Cancer === |
=== Cancer === |
||
Inflammation orchestrates the microenvironment around tumours, contributing to proliferation, survival and migration. |
Inflammation orchestrates the [[Tumor microenvironment|microenvironment]] around tumours, contributing to proliferation, survival and migration.<ref>{{Cite journal |vauthors=Ungefroren H, Sebens S, Seidl D, Lehnert H, Hass R |date=September 2011 |title=Interaction of tumor cells with the microenvironment |journal=Cell Communication and Signaling |volume=9 |pages=18 |doi=10.1186/1478-811X-9-18 |pmc=3180438 |pmid=21914164 |doi-access=free}}</ref> Cancer cells use [[selectins]], [[chemokines]] and their receptors for invasion, migration and metastasis.<ref name="Coussens" /> On the other hand, many cells of the immune system contribute to [[cancer immunology]], suppressing cancer.<ref name="pmid22914051">{{Cite journal |vauthors=Gunn L, Ding C, Liu M, Ma Y, Qi C, Cai Y, Hu X, Aggarwal D, Zhang HG, Yan J |date=September 2012 |title=Opposing roles for complement component C5a in tumor progression and the tumor microenvironment |journal=Journal of Immunology |volume=189 |issue=6 |pages=2985–94 |doi=10.4049/jimmunol.1200846 |pmc=3436956 |pmid=22914051}}</ref> |
||
Molecular intersection between receptors of steroid hormones, which have important effects on cellular development, and transcription factors that play key roles in inflammation, such as [[NF-κB]], may mediate some of the most critical effects of inflammatory stimuli on cancer cells.<ref name="pmid19382224">{{Cite journal |vauthors=Copland JA, Sheffield-Moore M, Koldzic-Zivanovic N, Gentry S, Lamprou G, Tzortzatou-Stathopoulou F, Zoumpourlis V, Urban RJ, Vlahopoulos SA |date=June 2009 |title=Sex steroid receptors in skeletal differentiation and epithelial neoplasia: is tissue-specific intervention possible? |journal=BioEssays |volume=31 |issue=6 |pages=629–41 |doi=10.1002/bies.200800138 |pmid=19382224 |s2cid=205469320}}</ref> This capacity of a mediator of inflammation to influence the effects of steroid hormones in cells is very likely to affect carcinogenesis. On the other hand, due to the modular nature of many steroid hormone receptors, this interaction may offer ways to interfere with cancer progression, through targeting of a specific protein domain in a specific cell type. Such an approach may limit side effects that are unrelated to the tumor of interest, and may help preserve vital homeostatic functions and developmental processes in the organism. |
|||
There is some evidence from 2009 to suggest that cancer-related inflammation (CRI) may lead to accumulation of random genetic alterations in cancer cells.<ref name="pmid19468060">{{Cite journal |vauthors=Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A |date=July 2009 |title=Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability |journal=Carcinogenesis |type=review |volume=30 |issue=7 |pages=1073–81 |doi=10.1093/carcin/bgp127 |pmid=19468060 |doi-access=free}}</ref>{{Update needed|date=October 2024}} |
|||
====Role in cancer==== |
|||
In 1863, [[Rudolf Virchow]] hypothesized that the origin of cancer was at sites of chronic inflammation.<ref name="Coussens">{{Cite journal |vauthors=Coussens LM, Werb Z |year=2002 |title=Inflammation and cancer |journal=Nature |volume=420 |issue=6917 |pages=860–7 |bibcode=2002Natur.420..860C |doi=10.1038/nature01322 |pmc=2803035 |pmid=12490959}}</ref><ref name="Chiba">{{Cite journal |vauthors=Chiba T, Marusawa H, Ushijima T |date=September 2012 |title=Inflammation-associated cancer development in digestive organs: mechanisms and roles for genetic and epigenetic modulation |url=http://repository.kulib.kyoto-u.ac.jp/dspace/bitstream/2433/160134/1/j.gastro.2012.07.009.pdf |url-status=live |journal=Gastroenterology |volume=143 |issue=3 |pages=550–563 |doi=10.1053/j.gastro.2012.07.009 |pmid=22796521 |s2cid=206226588 |archive-url=https://web.archive.org/web/20220829232437/https://repository.kulib.kyoto-u.ac.jp/dspace/bitstream/2433/160134/1/j.gastro.2012.07.009.pdf |archive-date=29 August 2022 |access-date=9 June 2018 |hdl-access=free |hdl=2433/160134}}</ref> As of 2012, chronic inflammation was estimated to contribute to approximately 15% to 25% of human cancers.<ref name="Chiba" /><ref name="pmid18650914">{{Cite journal |vauthors=Mantovani A, Allavena P, Sica A, Balkwill F |date=July 2008 |title=Cancer-related inflammation |url=https://air.unimi.it/bitstream/2434/145688/2/Cancer-related%20inflammation_Nature.pdf |url-status=live |journal=Nature |volume=454 |issue=7203 |pages=436–44 |bibcode=2008Natur.454..436M |doi=10.1038/nature07205 |pmid=18650914 |s2cid=4429118 |archive-url=https://web.archive.org/web/20221030195610/https://air.unimi.it/bitstream/2434/145688/2/Cancer-related%20inflammation_Nature.pdf |archive-date=30 October 2022 |access-date=9 June 2018 |hdl-access=free |hdl=2434/145688}}</ref> |
|||
====Mediators and DNA damage in cancer==== |
|||
An inflammatory mediator is a messenger that acts on blood vessels and/or cells to promote an inflammatory response.<ref name="pmid6399978">{{Cite journal |vauthors=Larsen GL, Henson PM |year=1983 |title=Mediators of inflammation |journal=Annual Review of Immunology |volume=1 |pages=335–59 |doi=10.1146/annurev.iy.01.040183.002003 |pmid=6399978}}</ref> Inflammatory mediators that contribute to neoplasia include [[prostaglandin]]s, inflammatory [[cytokine]]s such as [[Interleukin 1 beta|IL-1β]], [[tumor necrosis factor alpha|TNF-α]], [[Interleukin 6|IL-6]] and [[Interleukin 15|IL-15]] and [[chemokine]]s such as [[Interleukin 8|IL-8]] and [[CXCL1|GRO-alpha]].<ref name="Shacter">{{Cite journal |vauthors=Shacter E, Weitzman SA |date=February 2002 |title=Chronic inflammation and cancer |journal=Oncology |volume=16 |issue=2 |pages=217–26, 229; discussion 230–2 |pmid=11866137}}</ref><ref name="Chiba" /> These inflammatory mediators, and others, orchestrate an environment that fosters proliferation and survival.<ref name="Coussens" /><ref name="Shacter" /> |
|||
Inflammation also causes DNA damages due to the induction of [[reactive oxygen species]] (ROS) by various intracellular inflammatory mediators.<ref name="Coussens" /><ref name="Shacter" /><ref name="Chiba" /> In addition, [[White blood cell|leukocytes]] and other [[Phagocyte|phagocytic cells]] attracted to the site of inflammation induce DNA damages in proliferating cells through their generation of ROS and [[reactive nitrogen species]] (RNS). ROS and RNS are normally produced by these cells to fight infection.<ref name="Coussens" /> ROS, alone, cause more than 20 types of DNA damage.<ref name="pmid27989142">{{Cite journal |vauthors=Yu Y, Cui Y, Niedernhofer LJ, Wang Y |date=December 2016 |title=Occurrence, Biological Consequences, and Human Health Relevance of Oxidative Stress-Induced DNA Damage |journal=Chemical Research in Toxicology |volume=29 |issue=12 |pages=2008–2039 |doi=10.1021/acs.chemrestox.6b00265 |pmc=5614522 |pmid=27989142}}</ref> Oxidative DNA damages cause both [[mutation]]s<ref name="pmid22293091">{{Cite journal |vauthors=Dizdaroglu M |date=December 2012 |title=Oxidatively induced DNA damage: mechanisms, repair and disease |journal=Cancer Letters |volume=327 |issue=1–2 |pages=26–47 |doi=10.1016/j.canlet.2012.01.016 |pmid=22293091}}</ref> and epigenetic alterations.<ref name="pmid24281019">{{Cite journal |vauthors=Nishida N, Kudo M |year=2013 |title=Oxidative stress and epigenetic instability in human hepatocarcinogenesis |journal=Digestive Diseases |volume=31 |issue=5–6 |pages=447–53 |doi=10.1159/000355243 |pmid=24281019 |doi-access=free}}</ref><ref name="Chiba" /><ref name="Ding">{{Cite journal |vauthors=Ding N, Maiuri AR, O'Hagan HM |year=2017 |title=The emerging role of epigenetic modifiers in repair of DNA damage associated with chronic inflammatory diseases |journal=Mutation Research |volume=780 |pages=69–81 |doi=10.1016/j.mrrev.2017.09.005 |pmc=6690501 |pmid=31395351}}</ref> RNS also cause mutagenic DNA damages.<ref name="pmid28050219">{{Cite journal |vauthors=Kawanishi S, Ohnishi S, Ma N, Hiraku Y, Oikawa S, Murata M |year=2016 |title=Nitrative and oxidative DNA damage in infection-related carcinogenesis in relation to cancer stem cells |journal=Genes and Environment |volume=38 |issue=1 |pages=26 |bibcode=2016GeneE..38...26K |doi=10.1186/s41021-016-0055-7 |pmc=5203929 |pmid=28050219 |doi-access=free}}</ref> |
|||
A normal cell may undergo [[carcinogenesis]] to become a cancer cell if it is frequently subjected to DNA damage during long periods of chronic inflammation. DNA damages may cause genetic [[mutation]]s due to [[DNA repair#Translecion synthesis|inaccurate repair]]. In addition, mistakes in the DNA repair process may cause [[Cancer epigenetics|epigenetic]] alterations.<ref name="Chiba" /><ref name="Shacter" /><ref name="Ding" /> Mutations and epigenetic alterations that are replicated and provide a selective advantage during somatic cell proliferation may be carcinogenic. |
|||
Genome-wide analyses of human cancer tissues reveal that a single typical cancer cell may possess roughly 100 mutations in [[coding region]]s, 10–20 of which are [[carcinogenesis|"driver mutations"]] that contribute to cancer development.<ref name="Chiba" /> However, chronic inflammation also causes epigenetic changes such as [[DNA methylation in cancer|DNA methylation]]s, that are often more common than mutations. Typically, several hundreds to thousands of genes are methylated in a cancer cell (see [[DNA methylation in cancer]]). Sites of oxidative damage in [[chromatin]] can recruit complexes that contain [[DNA methyltransferase]]s (DNMTs), a histone deacetylase ([[sirtuin 1|SIRT1]]), and a [[EZH2|histone methyltransferase (EZH2)]], and thus induce DNA methylation.<ref name="Chiba" /><ref name="pmid22094255">{{Cite journal |vauthors=O'Hagan HM, Wang W, Sen S, Destefano Shields C, Lee SS, Zhang YW, Clements EG, Cai Y, Van Neste L, Easwaran H, Casero RA, Sears CL, Baylin SB |date=November 2011 |title=Oxidative damage targets complexes containing DNA methyltransferases, SIRT1, and polycomb members to promoter CpG Islands |journal=Cancer Cell |volume=20 |issue=5 |pages=606–19 |doi=10.1016/j.ccr.2011.09.012 |pmc=3220885 |pmid=22094255}}</ref><ref name="pmid28522752">{{Cite journal |vauthors=Maiuri AR, Peng M, Podicheti R, Sriramkumar S, Kamplain CM, Rusch DB, DeStefano Shields CE, Sears CL, O'Hagan HM |date=July 2017 |title=Mismatch Repair Proteins Initiate Epigenetic Alterations during Inflammation-Driven Tumorigenesis |journal=Cancer Research |volume=77 |issue=13 |pages=3467–3478 |doi=10.1158/0008-5472.CAN-17-0056 |pmc=5516887 |pmid=28522752}}</ref> DNA methylation of a [[CpG site|CpG island]] in a [[Promoter (genetics)|promoter region]] may cause silencing of its downstream gene (see [[CpG site]] and [[regulation of transcription in cancer]]). DNA repair genes, in particular, are frequently inactivated by methylation in various cancers (see [[DNA methylation in cancer#Likely role of hypermethylation of DNA repair genes in cancer|hypermethylation of DNA repair genes in cancer]]). A 2018 report<ref name="pmid29358395">{{Cite journal |vauthors=Yamashita S, Kishino T, Takahashi T, Shimazu T, Charvat H, Kakugawa Y, Nakajima T, Lee YC, Iida N, Maeda M, Hattori N, Takeshima H, Nagano R, Oda I, Tsugane S, Wu MS, Ushijima T |date=February 2018 |title=Genetic and epigenetic alterations in normal tissues have differential impacts on cancer risk among tissues |journal=Proceedings of the National Academy of Sciences of the United States of America |volume=115 |issue=6 |pages=1328–1333 |bibcode=2018PNAS..115.1328Y |doi=10.1073/pnas.1717340115 |pmc=5819434 |pmid=29358395 |doi-access=free}}</ref> evaluated the relative importance of mutations and epigenetic alterations in progression to two different types of cancer. This report showed that epigenetic alterations were much more important than mutations in generating gastric cancers (associated with inflammation).<ref name="pmid24664859">{{Cite journal |vauthors=Raza Y, Khan A, Farooqui A, Mubarak M, Facista A, Akhtar SS, Khan S, Kazi JI, Bernstein C, Kazmi SU |date=October 2014 |title=Oxidative DNA damage as a potential early biomarker of Helicobacter pylori associated carcinogenesis |journal=Pathology & Oncology Research |volume=20 |issue=4 |pages=839–46 |doi=10.1007/s12253-014-9762-1 |pmid=24664859 |s2cid=18727504}}</ref> However, mutations and epigenetic alterations were of roughly equal importance in generating esophageal squamous cell cancers (associated with [[Cigarette#Smokers|tobacco chemicals]] and [[Acetaldehyde#Carcinogenicity|acetaldehyde]], a product of alcohol metabolism). |
|||
===Restless Legs Syndrome=== |
|||
=== HIV and AIDS === |
|||
A literature review indicated that 30 of 40 causes of secondary RLS are associated with inflammation. <ref>{{cite journal |pages=A256 |title=Restless legs syndrome (RLS) is associated with an increased prevalence of small intestinal bacterial overgrowth: is RLS mediated by inflammatory and immunological mechanisms? |year=2010 |last1=Weinstock |first1=LB |last2=Walters|first2=A.|journal=Sleep |volume=33 |issue=S}} </ref> |
|||
It has long been recognized that infection with [[HIV]] is characterized not only by development of profound [[immunodeficiency]] but also by sustained inflammation and immune activation.<ref name="Deeks 141–155">{{Cite journal |vauthors=Deeks SG |date=2011-01-01 |title=HIV infection, inflammation, immunosenescence, and aging |journal=Annual Review of Medicine |volume=62 |pages=141–55 |doi=10.1146/annurev-med-042909-093756 |pmc=3759035 |pmid=21090961}}</ref><ref>{{Cite journal |vauthors=Klatt NR, Chomont N, Douek DC, Deeks SG |date=July 2013 |title=Immune activation and HIV persistence: implications for curative approaches to HIV infection |journal=Immunological Reviews |volume=254 |issue=1 |pages=326–42 |doi=10.1111/imr.12065 |pmc=3694608 |pmid=23772629}}</ref><ref>{{Cite journal |vauthors=Salazar-Gonzalez JF, Martinez-Maza O, Nishanian P, Aziz N, Shen LP, Grosser S, Taylor J, Detels R, Fahey JL |date=August 1998 |title=Increased immune activation precedes the inflection point of CD4 T cells and the increased serum virus load in human immunodeficiency virus infection |journal=The Journal of Infectious Diseases |volume=178 |issue=2 |pages=423–30 |doi=10.1086/515629 |pmid=9697722 |doi-access=free}}</ref> A substantial body of evidence implicates chronic inflammation as a critical driver of immune dysfunction, premature appearance of aging-related diseases, and immune deficiency.<ref name="Deeks 141–155" /><ref>{{Cite journal |vauthors=Ipp H, Zemlin A |date=February 2013 |title=The paradox of the immune response in HIV infection: when inflammation becomes harmful |journal=Clinica Chimica Acta; International Journal of Clinical Chemistry |volume=416 |pages=96–9 |doi=10.1016/j.cca.2012.11.025 |pmid=23228847}}</ref> Many now regard HIV infection not only as an evolving virus-induced immunodeficiency, but also as chronic inflammatory disease.<ref>{{Cite journal |vauthors=Nasi M, Pinti M, Mussini C, Cossarizza A |date=October 2014 |title=Persistent inflammation in HIV infection: established concepts, new perspectives |journal=Immunology Letters |volume=161 |issue=2 |pages=184–8 |doi=10.1016/j.imlet.2014.01.008 |pmid=24487059}}</ref> Even after the introduction of [[Antiretroviral therapy, highly active|effective antiretroviral therapy]] (ART) and effective suppression of viremia in HIV-infected individuals, chronic inflammation persists. Animal studies also support the relationship between immune activation and progressive cellular immune deficiency: [[Simian immunodeficiency virus|SIV]]<nowiki/>sm infection of its natural nonhuman primate hosts, the [[sooty mangabey]], causes high-level viral replication but limited evidence of disease.<ref>{{Cite journal |vauthors=Milush JM, Mir KD, Sundaravaradan V, Gordon SN, Engram J, Cano CA, Reeves JD, Anton E, O'Neill E, Butler E, Hancock K, Cole KS, Brenchley JM, Else JG, Silvestri G, Sodora DL |date=March 2011 |title=Lack of clinical AIDS in SIV-infected sooty mangabeys with significant CD4+ T cell loss is associated with double-negative T cells |journal=The Journal of Clinical Investigation |volume=121 |issue=3 |pages=1102–10 |doi=10.1172/JCI44876 |pmc=3049370 |pmid=21317533}}</ref><ref>{{Cite journal |vauthors=Rey-Cuillé MA, Berthier JL, Bomsel-Demontoy MC, Chaduc Y, Montagnier L, Hovanessian AG, Chakrabarti LA |date=May 1998 |title=Simian immunodeficiency virus replicates to high levels in sooty mangabeys without inducing disease |journal=Journal of Virology |volume=72 |issue=5 |pages=3872–86 |doi=10.1128/JVI.72.5.3872-3886.1998 |pmc=109612 |pmid=9557672}}</ref> This lack of pathogenicity is accompanied by a lack of inflammation, immune activation and cellular proliferation. In sharp contrast, experimental [[Simian immunodeficiency virus|SIV]]<nowiki/>sm infection of [[rhesus macaque]] produces immune activation and AIDS-like disease with many parallels to human HIV infection.<ref>{{Cite journal |vauthors=Chahroudi A, Bosinger SE, Vanderford TH, Paiardini M, Silvestri G |date=March 2012 |title=Natural SIV hosts: showing AIDS the door |journal=Science |volume=335 |issue=6073 |pages=1188–93 |bibcode=2012Sci...335.1188C |doi=10.1126/science.1217550 |pmc=3822437 |pmid=22403383}}</ref> |
|||
In light of the fact that many of the highly RLS associated conditions are also associated with inflammatory/immune changes suggests the possibility that RLS may be mediated or affected through these mechanisms. Inflammation is known to cause iron deficiency and hypothetically could cause CNS iron deficiency-induced RLS. Alternatively, an immune reaction to gastrointestinal bacteria or other antigens could contribute to some cases of RLS by a direct immunological attack on the central or peripheral nervous system. Patients with gastrointestinal (GI) diseases such as celiac disease and Crohn’s disease have a high prevalence of RLS and are also associated with inflammation, immune disturbances, iron deficiency and peripheral neuropathy. <ref>{{cite journal |pages=1667-73 |title=Celiac disease is associated with restless legs syndrome. |year=2010 |last1=Weinstock |first1=LB |last2=Walters|first2=A. |last3=Mullen |first3=G. |last4=Duntley |first4=SP |journal=Journal of Neurology, Neurosurgery & Psychiatry |volume=55 |issue=6 | PMID=19731029}} </ref> <ref>{{cite journal |pages=275-9 | title=Crohn’s disease is associated with restless legs syndrome. |year=2010 |last1=Weinstock |first1=LB |last2=Bosworth |first2=BP |last3=Scherl |first3=EJ |last4=et al. | journal=Inflammatory Bowel Diseases |volume=16 |issue=2 | PMID=19575360 }} </ref> |
|||
Delineating how [[CD4]] T cells are depleted and how chronic inflammation and immune activation are induced lies at the heart of understanding HIV pathogenesis{{emdash}}one of the top priorities for HIV research by the Office of AIDS Research, [[National Institute of Allergy and Infectious Diseases|National Institutes of Health]]. Recent studies demonstrated that [[Caspase 1|caspase-1]]-mediated [[pyroptosis]], a highly inflammatory form of programmed cell death, drives CD4 T-cell depletion and inflammation by HIV.<ref name="Doitsh 509–514">{{Cite journal |vauthors=Doitsh G, Galloway NL, Geng X, Yang Z, Monroe KM, Zepeda O, Hunt PW, Hatano H, Sowinski S, Muñoz-Arias I, Greene WC |date=January 2014 |title=Cell death by pyroptosis drives CD4 T-cell depletion in HIV-1 infection |journal=Nature |volume=505 |issue=7484 |pages=509–14 |bibcode=2014Natur.505..509D |doi=10.1038/nature12940 |pmc=4047036 |pmid=24356306}}</ref><ref>{{Cite journal |vauthors=Monroe KM, Yang Z, Johnson JR, Geng X, Doitsh G, Krogan NJ, Greene WC |date=January 2014 |title=IFI16 DNA sensor is required for death of lymphoid CD4 T cells abortively infected with HIV |journal=Science |volume=343 |issue=6169 |pages=428–32 |bibcode=2014Sci...343..428M |doi=10.1126/science.1243640 |pmc=3976200 |pmid=24356113}}</ref><ref>{{Cite journal |vauthors=Galloway NL, Doitsh G, Monroe KM, Yang Z, Muñoz-Arias I, Levy DN, Greene WC |date=September 2015 |title=Cell-to-Cell Transmission of HIV-1 Is Required to Trigger Pyroptotic Death of Lymphoid-Tissue-Derived CD4 T Cells |journal=Cell Reports |volume=12 |issue=10 |pages=1555–1563 |doi=10.1016/j.celrep.2015.08.011 |pmc=4565731 |pmid=26321639}}</ref> These are the two signature events that propel HIV disease progression to [[HIV/AIDS|AIDS]]. Pyroptosis appears to create a pathogenic vicious cycle in which dying CD4 T cells and other immune cells (including macrophages and neutrophils) release inflammatory signals that recruit more cells into the infected lymphoid tissues to die. The feed-forward nature of this inflammatory response produces chronic inflammation and tissue injury.<ref>{{Cite journal |vauthors=Doitsh G, Greene WC |date=March 2016 |title=Dissecting How CD4 T Cells Are Lost During HIV Infection |journal=Cell Host & Microbe |volume=19 |issue=3 |pages=280–91 |doi=10.1016/j.chom.2016.02.012 |pmc=4835240 |pmid=26962940}}</ref> Identifying pyroptosis as the predominant mechanism that causes CD4 T-cell depletion and chronic inflammation, provides novel therapeutic opportunities, namely caspase-1 which controls the pyroptotic pathway. In this regard, pyroptosis of CD4 T cells and secretion of pro-inflammatory cytokines such as [[Interleukin 1 beta|IL-1β]] and [[Interleukin 18|IL-18]] can be blocked in HIV-infected human lymphoid tissues by addition of the caspase-1 inhibitor VX-765,<ref name="Doitsh 509–514" /> which has already proven to be safe and well tolerated in phase II human clinical trials.<ref>{{Cite journal |date=19 December 2013 |title=Study of VX-765 in Subjects With Treatment-resistant Partial Epilepsy – Full Text View – ClinicalTrials.gov |url=https://clinicaltrials.gov/ct2/show/NCT01048255 |url-status=live |archive-url=https://web.archive.org/web/20220926164557/https://clinicaltrials.gov/ct2/show/NCT01048255 |archive-date=26 September 2022 |access-date=2016-05-21 |website=clinicaltrials.gov}}</ref> These findings could propel development of an entirely new class of "anti-AIDS" therapies that act by targeting the host rather than the virus. Such agents would almost certainly be used in combination with ART. By promoting "tolerance" of the virus instead of suppressing its replication, VX-765 or related drugs may mimic the evolutionary solutions occurring in multiple monkey hosts (e.g. the sooty mangabey) infected with species-specific lentiviruses that have led to a lack of disease, no decline in CD4 T-cell counts, and no chronic inflammation. |
|||
A recent study showed an increase in the incidence of small intestinal bacterial overgrowth and irritable bowel syndrome in RLS patients. <ref>{{cite journal |pages=610-3 | title=Restless legs syndrome is associated with an increased prevalence of small intestinal bacterial overgrowth and irritable bowel syndrome. |year=2011 |last1=Walters |first1=A. | last2=Weinstock |first2=LB | journal=Sleep Medicine |volume=12 |issue=6 | PMID=21570907 }} </ref> |
|||
=== Resolution === |
|||
Both of these gastrointestinal disorders also have immune and inflammatory disorders. Three studies show evidence that antibiotic therapy may be beneficial for RLS patients who have small intestinal bacterial overgrowth. <ref>{{cite journal |pages=1252-6 | title=“Restless legs syndrome in patients with irritable bowel syndrome: response to small intestinal bacterial overgrowth therapy.” |year=2008 |last1=Weinstock |first1=LB |last2=Fern |first2=SE |last3=Duntleyl |first3=SP | journal=Digestive Diseases and Science |volume=53 |issue=5 |PMID=17934858}} </ref> <ref>{{cite journal |pages=S28 |title= Antibiotic therapy improves restless legs syndrome: a double blind, controlled study of short course of rifaximin. |year=2009 |last1=Weinstock |first1=LB |last2=Walters|first2=A. |last3=Duntley |first3=SP |last4=Zeiss |first4=S. |last5=Lewis |first5=N.|journal=Sleep Medicine |volume=10 |issue=S2}} </ref> <ref>{{cite journal |pages=427 | title=Antibiotic therapy may improve idiopathic restless legs syndrome: Prospective, open-label pilot study of rifaximin, a nonsystemic antibiotic. |year=2010 |last1=Weinstock |first1=LB | journal=Sleep Medicine |volume=11 |issue=4 | PMID=20042368 }} </ref> |
|||
The inflammatory response must be actively terminated when no longer needed to prevent unnecessary "bystander" damage to tissues.<ref name="robspath" /> Failure to do so results in chronic inflammation, and cellular destruction. Resolution of inflammation occurs by different mechanisms in different tissues. |
|||
Mechanisms that serve to terminate inflammation include:<ref name="robspath" /><ref>{{Cite journal |vauthors=Eming SA, Krieg T, Davidson JM |date=March 2007 |title=Inflammation in wound repair: molecular and cellular mechanisms |journal=The Journal of Investigative Dermatology |volume=127 |issue=3 |pages=514–25 |doi=10.1038/sj.jid.5700701 |pmid=17299434 |doi-access=free}}</ref> |
|||
{{columns-list|colwidth=30em| |
|||
=== Resolution of inflammation === |
|||
The inflammatory response must be actively terminated when no longer needed to prevent unnecessary "bystander" damage to tissues.<ref name="robspath" /> Failure to do so results in chronic inflammation, and cellular destruction. Resolution of inflammation occurs by different mechanisms in different tissues. |
|||
Mechanisms which serve to terminate inflammation include:<ref name="robspath" /><ref>{{cite journal |last=Eming |first=S. A. |first2=T. |last2=Krieg |first3=J. M. |last3=Davidson |title=Inflammation in wound repair: molecular and cellular mechanisms |journal=Journal of Investigative Dermatology |year=2007 |volume=127 |issue=3 |pages=514–525 |doi=10.1038/sj.jid.5700701 |pmid=17299434 }}</ref> |
|||
* Short [[half-life]] of [[inflammatory mediators]] ''in vivo''. |
* Short [[half-life]] of [[inflammatory mediators]] ''in vivo''. |
||
* Production and release of [[ |
* Production and release of [[transforming growth factor (TGF) beta]] from [[macrophages]]<ref>{{Cite journal |vauthors=Ashcroft GS, Yang X, Glick AB, Weinstein M, Letterio JL, Mizel DE, Anzano M, Greenwell-Wild T, Wahl SM, Deng C, Roberts AB |date=September 1999 |title=Mice lacking Smad3 show accelerated wound healing and an impaired local inflammatory response |journal=Nature Cell Biology |volume=1 |issue=5 |pages=260–6 |doi=10.1038/12971 |pmid=10559937 |s2cid=37216623}}</ref><ref>{{Cite journal |vauthors=Ashcroft GS |date=December 1999 |title=Bidirectional regulation of macrophage function by TGF-beta |url=https://zenodo.org/record/1260212 |url-status=live |journal=Microbes and Infection |volume=1 |issue=15 |pages=1275–82 |doi=10.1016/S1286-4579(99)00257-9 |pmid=10611755 |archive-url=https://web.archive.org/web/20200110215702/https://zenodo.org/record/1260212 |archive-date=10 January 2020 |access-date=11 September 2019}}</ref><ref>{{Cite journal |vauthors=Werner F, Jain MK, Feinberg MW, Sibinga NE, Pellacani A, Wiesel P, Chin MT, Topper JN, Perrella MA, Lee ME |date=November 2000 |title=Transforming growth factor-beta 1 inhibition of macrophage activation is mediated via Smad3 |journal=The Journal of Biological Chemistry |volume=275 |issue=47 |pages=36653–8 |doi=10.1074/jbc.M004536200 |pmid=10973958 |doi-access=free}}</ref> |
||
* Production and release of [[ |
* Production and release of [[interleukin 10]] (IL-10)<ref>{{Cite journal |vauthors=Sato Y, Ohshima T, Kondo T |date=November 1999 |title=Regulatory role of endogenous interleukin-10 in cutaneous inflammatory response of murine wound healing |journal=Biochemical and Biophysical Research Communications |volume=265 |issue=1 |pages=194–9 |doi=10.1006/bbrc.1999.1455 |pmid=10548513}}</ref> |
||
* Production of anti-inflammatory [[lipoxin]]s<ref>{{ |
* Production of anti-inflammatory [[specialized proresolving mediators]], i.e. [[lipoxin]]s, [[resolvin]]s, [[maresin]]s, and [[neuroprotectin]]s<ref>{{Cite journal |vauthors=Serhan CN |date=August 2008 |title=Controlling the resolution of acute inflammation: a new genus of dual anti-inflammatory and proresolving mediators |journal=Journal of Periodontology |volume=79 |issue=8 Suppl |pages=1520–6 |doi=10.1902/jop.2008.080231 |pmid=18673006}}</ref><ref name="pmid25911383">{{Cite journal |vauthors=Headland SE, Norling LV |date=May 2015 |title=The resolution of inflammation: Principles and challenges |journal=Seminars in Immunology |volume=27 |issue=3 |pages=149–60 |doi=10.1016/j.smim.2015.03.014 |pmid=25911383}}</ref> |
||
* Downregulation of pro-inflammatory molecules, such as [[leukotrienes]] |
* Downregulation of pro-inflammatory molecules, such as [[leukotrienes]]. |
||
* Upregulation of anti-inflammatory molecules such as the [[ |
* Upregulation of anti-inflammatory molecules such as the [[interleukin 1 receptor antagonist]] or the soluble [[tumor necrosis factor receptor]] (TNFR) |
||
* [[Apoptosis]] of pro-inflammatory cells<ref>{{ |
* [[Apoptosis]] of pro-inflammatory cells<ref>{{Cite journal |vauthors=Greenhalgh DG |date=September 1998 |title=The role of apoptosis in wound healing |journal=The International Journal of Biochemistry & Cell Biology |volume=30 |issue=9 |pages=1019–30 |doi=10.1016/S1357-2725(98)00058-2 |pmid=9785465}}</ref> |
||
* Desensitization of receptors |
* Desensitization of receptors. |
||
* Increased survival of cells in regions of inflammation due to their interaction with the [[extracellular matrix]] (ECM)<ref>{{ |
* Increased survival of cells in regions of inflammation due to their interaction with the [[extracellular matrix]] (ECM)<ref>{{Cite journal |vauthors=Jiang D, Liang J, Fan J, Yu S, Chen S, Luo Y, Prestwich GD, Mascarenhas MM, Garg HG, Quinn DA, Homer RJ, Goldstein DR, Bucala R, Lee PJ, Medzhitov R, Noble PW |date=November 2005 |title=Regulation of lung injury and repair by Toll-like receptors and hyaluronan |journal=Nature Medicine |volume=11 |issue=11 |pages=1173–9 |doi=10.1038/nm1315 |pmid=16244651 |s2cid=11765495}}</ref><ref>{{Cite journal |vauthors=Teder P, Vandivier RW, Jiang D, Liang J, Cohn L, Puré E, Henson PM, Noble PW |date=April 2002 |title=Resolution of lung inflammation by CD44 |journal=Science |volume=296 |issue=5565 |pages=155–8 |bibcode=2002Sci...296..155T |doi=10.1126/science.1069659 |pmid=11935029 |s2cid=7905603}}</ref> |
||
* Downregulation of receptor activity by high concentrations of [[ligands]] |
* Downregulation of receptor activity by high concentrations of [[ligands]] |
||
* Cleavage of [[chemokine]]s by [[matrix metalloproteinases]] (MMPs) might lead to production of anti-inflammatory factors.<ref>{{ |
* Cleavage of [[chemokine]]s by [[matrix metalloproteinases]] (MMPs) might lead to production of anti-inflammatory factors.<ref>{{Cite journal |vauthors=McQuibban GA, Gong JH, Tam EM, McCulloch CA, Clark-Lewis I, Overall CM |date=August 2000 |title=Inflammation dampened by gelatinase A cleavage of monocyte chemoattractant protein-3 |journal=Science |volume=289 |issue=5482 |pages=1202–6 |bibcode=2000Sci...289.1202M |doi=10.1126/science.289.5482.1202 |pmid=10947989}}</ref> |
||
}} |
|||
{{Cquote|Acute inflammation normally resolves by mechanisms that have remained somewhat elusive. Emerging evidence now suggests that an active, coordinated program of resolution initiates in the first few hours after an inflammatory response begins. After entering tissues, [[granulocyte]]s promote the switch of [[arachidonic acid]]–derived [[prostaglandin]]s and [[leukotriene]]s to lipoxins, which initiate the termination sequence. [[Neutrophil]] recruitment thus ceases and programmed death by [[apoptosis]] is engaged. These events coincide with the biosynthesis, from [[omega-3 fatty acid|omega-3 polyunsaturated fatty acids]], of [[resolvins]] and [[Neuroprotectin|protectins]], which critically shorten the period of neutrophil infiltration by initiating apoptosis. As a consequence, apoptotic neutrophils undergo [[phagocytosis]] by [[macrophage]]s, leading to neutrophil clearance and release of anti-inflammatory and reparative [[cytokines]] such as transforming growth factor-β1. The anti-inflammatory program ends with the departure of macrophages through the [[Lymphatic system|lymphatics]].<ref name="pmid16369558">{{Cite journal |vauthors=Serhan CN, Savill J |date=December 2005 |title=Resolution of inflammation: the beginning programs the end |journal=Nature Immunology |volume=6 |issue=12 |pages=1191–7 |doi=10.1038/ni1276 |pmid=16369558 |s2cid=22379843}}</ref>|30px|30px|[[Charles N. Serhan]] |
|||
}} |
|||
=== Connection to depression === |
|||
{{Cquote|Acute inflammation normally resolves by mechanisms that have remained somewhat elusive. Emerging evidence now suggests that an active, coordinated program of resolution initiates in the first few hours after an inflammatory response begins. After entering tissues, [[granulocyte]]s promote the switch of [[arachidonic acid]]–derived [[prostaglandin]]s and [[leukotriene]]s to lipoxins, which initiate the termination sequence. [[Neutrophil]] recruitment thus ceases and programmed death by [[apoptosis]] is engaged. These events coincide with the biosynthesis, from [[omega-3 fatty acid|omega-3 polyunsaturated fatty acids]], of [[resolvins]] and [[Neuroprotectin|protectins]], which critically shorten the period of neutrophil infiltration by initiating apoptosis. Consequently, apoptotic neutrophils undergo [[phagocytosis]] by [[macrophage]]s, leading to neutrophil clearance and release of anti-inflammatory and reparative [[cytokines]] such as transforming growth factor-β1. The anti-inflammatory program ends with the departure of macrophages through the [[Lymphatic system|lymphatics]].<ref name="pmid16369558">{{cite journal |author=Serhan CN, Savill J |title=Resolution of inflammation: the beginning programs the end |journal=Nat. Immunol. |volume=6 |issue=12 |pages=1191–1197 |year=2005 |pmid=16369558 |url= http://www.nature.com/ni/journal/v6/n12/abs/ni1276.html |doi=10.1038/ni1276}}</ref>|30px|30px|Charles Serhan}} |
|||
There is evidence for a link between [[Depression and immune function#Depression and inflammation|inflammation and depression]].<ref>{{Cite journal |vauthors=Berk M, Williams LJ, Jacka FN, O'Neil A, Pasco JA, Moylan S, Allen NB, Stuart AL, Hayley AC, Byrne ML, Maes M |date=September 2013 |title=So depression is an inflammatory disease, but where does the inflammation come from? |journal=BMC Medicine |volume=11 |pages=200 |doi=10.1186/1741-7015-11-200 |pmc=3846682 |pmid=24228900 |doi-access=free}}</ref> Inflammatory processes can be triggered by negative cognitions or their consequences, such as stress, violence, or deprivation. Thus, negative cognitions can cause inflammation that can, in turn, lead to depression.<ref name="Cox et al. (2012)">{{Cite journal |vauthors=Cox WT, Abramson LY, Devine PG, Hollon SD |date=September 2012 |title=Stereotypes, Prejudice, and Depression: The Integrated Perspective |journal=Perspectives on Psychological Science |volume=7 |issue=5 |pages=427–49 |doi=10.1177/1745691612455204 |pmid=26168502 |s2cid=1512121}}</ref><ref>{{Cite journal |vauthors=Kiecolt-Glaser JK, Derry HM, Fagundes CP |date=November 2015 |title=Inflammation: depression fans the flames and feasts on the heat |journal=The American Journal of Psychiatry |volume=172 |issue=11 |pages=1075–91 |doi=10.1176/appi.ajp.2015.15020152 |pmc=6511978 |pmid=26357876}}</ref>{{Dubious|Depression|reason=Implausible claim apparently not supported by citation.|date=July 2013}} |
|||
In addition, there is increasing evidence that inflammation can cause depression because of the increase of cytokines, setting the brain into a "sickness mode".<ref>{{Cite news |date=2015-01-04 |title=Is depression a kind of allergic reaction? |url=https://www.theguardian.com/lifeandstyle/2015/jan/04/depression-allergic-reaction-inflammation-immune-system |url-status=live |archive-url=https://web.archive.org/web/20221021202426/https://www.theguardian.com/lifeandstyle/2015/jan/04/depression-allergic-reaction-inflammation-immune-system |archive-date=21 October 2022 |access-date=11 December 2016 |work=The Guardian |vauthors=Williams C}}</ref> |
|||
Classical symptoms of being physically sick, such as lethargy, show a large overlap in behaviors that characterize depression. Levels of cytokines tend to increase sharply during the depressive episodes of people with bipolar disorder and drop off during remission.<ref>{{Cite journal |vauthors=Brietzke E, Stertz L, Fernandes BS, Kauer-Sant'anna M, Mascarenhas M, Escosteguy Vargas A, Chies JA, Kapczinski F |date=August 2009 |title=Comparison of cytokine levels in depressed, manic and euthymic patients with bipolar disorder |journal=Journal of Affective Disorders |volume=116 |issue=3 |pages=214–7 |doi=10.1016/j.jad.2008.12.001 |pmid=19251324}}</ref> Furthermore, it has been shown in clinical trials that anti-inflammatory medicines taken in addition to antidepressants not only significantly improves symptoms but also increases the proportion of subjects positively responding to treatment.<ref>{{Cite journal |vauthors=Müller N, Schwarz MJ, Dehning S, Douhe A, Cerovecki A, Goldstein-Müller B, Spellmann I, Hetzel G, Maino K, Kleindienst N, Möller HJ, Arolt V, Riedel M |date=July 2006 |title=The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine |journal=Molecular Psychiatry |volume=11 |issue=7 |pages=680–4 |doi=10.1038/sj.mp.4001805 |pmid=16491133 |doi-access=free}}</ref> |
|||
Inflammations that lead to serious depression could be caused by common infections such as those caused by a virus, bacteria or even parasites.<ref>{{Cite journal |vauthors=Canli T |year=2014 |title=Reconceptualizing major depressive disorder as an infectious disease |journal=Biology of Mood & Anxiety Disorders |volume=4 |pages=10 |doi=10.1186/2045-5380-4-10 |pmc=4215336 |pmid=25364500 |doi-access=free}}</ref> |
|||
=== Connection to delirium === |
|||
There is evidence for a link between inflammation and [[delirium]] based on the results of a recent longitudinal study investigating CRP in COVID-19 patients.<ref>{{Cite journal |vauthors=Saini A, Oh TH, Ghanem DA, Castro M, Butler M, Sin Fai Lam CC, Posporelis S, Lewis G, David AS, Rogers JP |date=October 2022 |title=Inflammatory and blood gas markers of COVID-19 delirium compared to non-COVID-19 delirium: a cross-sectional study |url=https://discovery.ucl.ac.uk/id/eprint/10136824/ |url-status=live |journal=Aging & Mental Health |volume=26 |issue=10 |pages=2054–2061 |doi=10.1080/13607863.2021.1989375 |pmid=34651536 |s2cid=238990849 |archive-url=https://web.archive.org/web/20211022093940/https://discovery.ucl.ac.uk/id/eprint/10136824/ |archive-date=22 October 2021 |access-date=20 February 2023 |doi-access=free}}</ref> |
|||
== Systemic effects == |
== Systemic effects == |
||
An [[infectious organism]] can escape the confines of the immediate tissue via the [[circulatory system]] or [[lymphatic system]], where it may spread to other parts of the body. If an organism is not contained by the actions of acute inflammation it may gain access to the lymphatic system via nearby [[lymph vessel]]s. An infection of the lymph vessels is known as [[lymphangitis]], and infection of a lymph node is known as [[lymphadenitis]]. A pathogen can gain access to the bloodstream through lymphatic drainage into the circulatory system. |
An [[infectious organism]] can escape the confines of the immediate tissue via the [[circulatory system]] or [[lymphatic system]], where it may spread to other parts of the body. If an organism is not contained by the actions of acute inflammation, it may gain access to the lymphatic system via nearby [[lymph vessel]]s. An infection of the lymph vessels is known as [[lymphangitis]], and infection of a lymph node is known as [[lymphadenitis]]. When lymph nodes cannot destroy all pathogens, the infection spreads further. A pathogen can gain access to the bloodstream through lymphatic drainage into the circulatory system. |
||
When inflammation overwhelms the host, [[systemic inflammatory response syndrome]] is diagnosed. When it is due to |
When inflammation overwhelms the host, [[systemic inflammatory response syndrome]] is diagnosed. When it is due to infection, the term [[sepsis]] is applied, with the terms [[bacteremia]] being applied specifically for bacterial sepsis and [[viremia]] specifically to viral sepsis. [[Vasodilation]] and organ dysfunction are serious problems associated with widespread infection that may lead to [[septic shock]] and death.<ref>{{Cite book |title=StatPearls |vauthors=Ramanlal R, Gupta V |date=2021 |publisher=StatPearls Publishing |location=Treasure Island (FL) |chapter=Physiology, Vasodilation |pmid=32491494 |access-date=22 September 2021 |chapter-url=http://www.ncbi.nlm.nih.gov/books/NBK557562/ |archive-url=https://web.archive.org/web/20210511162804/https://www.ncbi.nlm.nih.gov/books/NBK557562/ |archive-date=11 May 2021 |url-status=live}}</ref> |
||
=== Acute-phase proteins === |
=== Acute-phase proteins === |
||
Inflammation also |
Inflammation also is characterized by high systemic levels of [[acute-phase protein]]s. In acute inflammation, these proteins prove beneficial; however, in chronic inflammation, they can contribute to [[amyloidosis]].<ref name="robspath" /> These proteins include [[C-reactive protein]], [[serum amyloid A]], and [[serum amyloid P]], which cause a range of systemic effects including:<ref name="robspath" /> |
||
{{div col|colwidth=25em}} |
|||
<div style="-moz-column-count:3; column-count:2;"> |
|||
* |
* Fever |
||
* Increased [[blood pressure]] |
* Increased [[blood pressure]] |
||
* Decreased [[sweating]] |
* Decreased [[sweating]] |
||
| Line 275: | Line 413: | ||
* [[Anorexia (symptom)|Loss of appetite]] |
* [[Anorexia (symptom)|Loss of appetite]] |
||
* [[Somnolence]] |
* [[Somnolence]] |
||
{{div col end}} |
|||
</div> |
|||
=== Leukocyte numbers === |
=== Leukocyte numbers === |
||
Inflammation often affects the numbers of leukocytes present in the body: |
Inflammation often affects the numbers of leukocytes present in the body: |
||
* [[Leukocytosis]] is often seen during inflammation induced by infection, where it results in a large increase in the amount of leukocytes in the blood, especially immature cells. Leukocyte numbers usually increase to between 15 000 and 20 000 cells per microliter, but extreme cases can see it approach 100 000 cells per microliter.<ref name="robspath" /> Bacterial infection usually results in an increase of [[neutrophil]]s, creating [[neutrophilia]], whereas diseases such as [[asthma]], [[hay fever]], and parasite infestation result in an increase in [[eosinophil]]s, creating [[eosinophilia]].<ref name="robspath" /> |
* [[Leukocytosis]] is often seen during inflammation induced by infection, where it results in a large increase in the amount of leukocytes in the blood, especially immature cells. Leukocyte numbers usually increase to between 15 000 and 20 000 cells per microliter, but extreme cases can see it approach 100 000 cells per microliter.<ref name="robspath" /> Bacterial infection usually results in an increase of [[neutrophil]]s, creating [[neutrophilia]], whereas diseases such as [[asthma]], [[hay fever]], and parasite infestation result in an increase in [[eosinophil]]s, creating [[eosinophilia]].<ref name="robspath" /> |
||
* [[Leukopenia]] can be induced by certain infections and diseases, including viral infection, ''[[Rickettsia]]'' infection, some [[protozoa]], [[tuberculosis]], and some |
* [[Leukopenia]] can be induced by certain infections and diseases, including viral infection, ''[[Rickettsia]]'' infection, some [[protozoa]], [[tuberculosis]], and some cancers.<ref name="robspath" /> |
||
=== |
=== Interleukins and obesity === |
||
With the discovery of [[interleukin]]s (IL), the concept of [[systemic inflammation]] developed. Although the processes involved are identical to tissue inflammation, systemic inflammation is not confined to a particular tissue but involves the [[endothelium]] and other organ systems. |
With the discovery of [[interleukin]]s (IL), the concept of [[systemic inflammation]] developed. Although the processes involved are identical to tissue inflammation, systemic inflammation is not confined to a particular tissue but involves the [[endothelium]] and other organ systems. |
||
Chronic inflammation is widely observed in obesity.<ref>{{ |
Chronic inflammation is widely observed in [[obesity]].<ref name="ParimisettyDorsemans2016">{{Cite journal |vauthors=Parimisetty A, Dorsemans AC, Awada R, Ravanan P, Diotel N, Lefebvre d'Hellencourt C |date=March 2016 |title=Secret talk between adipose tissue and central nervous system via secreted factors-an emerging frontier in the neurodegenerative research |journal=Journal of Neuroinflammation |type=Review |volume=13 |issue=1 |pages=67 |doi=10.1186/s12974-016-0530-x |pmc=4806498 |pmid=27012931 |doi-access=free}}</ref><ref>{{Cite journal |vauthors=Kershaw EE, Flier JS |date=June 2004 |title=Adipose tissue as an endocrine organ |journal=The Journal of Clinical Endocrinology and Metabolism |volume=89 |issue=6 |pages=2548–56 |doi=10.1210/jc.2004-0395 |pmid=15181022 |doi-access=free}}</ref> Obese people commonly have many elevated markers of inflammation, including:<ref>{{Cite journal |vauthors=Bastard JP, Jardel C, Bruckert E, Blondy P, Capeau J, Laville M, Vidal H, Hainque B |date=September 2000 |title=Elevated levels of interleukin 6 are reduced in serum and subcutaneous adipose tissue of obese women after weight loss |journal=The Journal of Clinical Endocrinology and Metabolism |volume=85 |issue=9 |pages=3338–42 |doi=10.1210/jcem.85.9.6839 |pmid=10999830 |doi-access=free}}</ref><ref>{{Cite journal |vauthors=Mohamed-Ali V, Flower L, Sethi J, Hotamisligil G, Gray R, Humphries SE, York DA, Pinkney J |date=December 2001 |title=beta-Adrenergic regulation of IL-6 release from adipose tissue: in vivo and in vitro studies |journal=The Journal of Clinical Endocrinology and Metabolism |volume=86 |issue=12 |pages=5864–9 |doi=10.1210/jcem.86.12.8104 |pmid=11739453 |s2cid=73100391 |doi-access=free}}</ref> |
||
* [[Interleukin-6|IL-6 (Interleukin-6)]]<ref name="Loffreda S 1998">{{Cite journal |vauthors=Loffreda S, Yang SQ, Lin HZ, Karp CL, Brengman ML, Wang DJ, Klein AS, Bulkley GB, Bao C, Noble PW, Lane MD, Diehl AM |date=January 1998 |title=Leptin regulates proinflammatory immune responses |journal=FASEB Journal |volume=12 |issue=1 |pages=57–65 |doi=10.1096/fasebj.12.1.57 |pmid=9438411 |doi-access=free}}</ref><ref name="Esposito K 2002">{{Cite journal |vauthors=Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M, Quagliaro L, Ceriello A, Giugliano D |date=October 2002 |title=Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress |journal=Circulation |volume=106 |issue=16 |pages=2067–72 |doi=10.1161/01.CIR.0000034509.14906.AE |pmid=12379575 |doi-access=free}}</ref> |
|||
{{columns-list|colwidth=30em| |
|||
* [[Interleukin-6|IL-6 (Interleukin-6)]]<ref name="Loffreda S 1998">{{cite journal |last=Loffreda |first=S. |last2=''et al.'' |title=Leptin regulates proinflammatory immune responses |journal=FASEB J |year=1998 |volume=12 |issue=1 |pages=57–65 |doi= |pmid=9438411 }}</ref><ref name ="Esposito K 2002">{{cite journal |last=Esposito |first=K. |last2=''et al.'' |title=Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress |journal=Circulation |year=2002 |volume=106 |issue=16 |pages=2067–2072 |doi=10.1161/01.CIR.0000034509.14906.AE |pmid=12379575 }}</ref> |
|||
* [[Interleukin-8|IL-8 (Interleukin-8)]] |
* [[Interleukin-8|IL-8 (Interleukin-8)]] |
||
* [[Interleukin-18|IL-18 (Interleukin-18)]]<ref name="Loffreda S 1998"/><ref name="Esposito K 2002"/> |
* [[Interleukin-18|IL-18 (Interleukin-18)]]<ref name="Loffreda S 1998" /><ref name="Esposito K 2002" /> |
||
* [[Tumor necrosis factor-alpha|TNF-α (Tumor necrosis factor-alpha)]]<ref name="Loffreda S 1998"/><ref name="Esposito K 2002"/> |
* [[Tumor necrosis factor-alpha|TNF-α (Tumor necrosis factor-alpha)]]<ref name="Loffreda S 1998" /><ref name="Esposito K 2002" /> |
||
* [[C-reactive protein|CRP (C-reactive protein)]]<ref name="Loffreda S 1998"/><ref name="Esposito K 2002"/> |
* [[C-reactive protein|CRP (C-reactive protein)]]<ref name="Loffreda S 1998" /><ref name="Esposito K 2002" /> |
||
* [[Insulin]]<ref name="Loffreda S 1998"/><ref name="Esposito K 2002"/> |
* [[Insulin]]<ref name="Loffreda S 1998" /><ref name="Esposito K 2002" /> |
||
* [[Blood sugar|Blood glucose]]<ref name="Loffreda S 1998"/><ref name="Esposito K 2002"/> |
* [[Blood sugar|Blood glucose]]<ref name="Loffreda S 1998" /><ref name="Esposito K 2002" /> |
||
* [[Leptin]]<ref name="Loffreda S 1998"/><ref name="Esposito K 2002"/> |
* [[Leptin]]<ref name="Loffreda S 1998" /><ref name="Esposito K 2002" /> |
||
}} |
|||
Low-grade chronic inflammation is characterized by a two- to threefold increase in the systemic concentrations of cytokines such as TNF-α, IL-6, and CRP.<ref>{{ |
Low-grade chronic inflammation is characterized by a two- to threefold increase in the systemic concentrations of cytokines such as TNF-α, IL-6, and CRP.<ref>{{Cite journal |vauthors=Petersen AM, Pedersen BK |date=April 2005 |title=The anti-inflammatory effect of exercise |journal=Journal of Applied Physiology |volume=98 |issue=4 |pages=1154–62 |doi=10.1152/japplphysiol.00164.2004 |pmid=15772055 |s2cid=4776835}}</ref> Waist circumference correlates significantly with systemic inflammatory response.<ref>{{Cite journal |vauthors=Rogowski O, Shapira I, Bassat OK, Chundadze T, Finn T, Berliner S, Steinvil A |date=July 2010 |title=Waist circumference as the predominant contributor to the micro-inflammatory response in the metabolic syndrome: a cross sectional study |journal=Journal of Inflammation |volume=7 |pages=35 |doi=10.1186/1476-9255-7-35 |pmc=2919526 |pmid=20659330 |doi-access=free}}</ref> |
||
Loss of [[white adipose tissue]] reduces levels of inflammation markers.<ref name="ParimisettyDorsemans2016" /> As of 2017 the association of systemic inflammation with [[insulin resistance]] and [[type 2 diabetes]], and with [[atherosclerosis]] was under preliminary research, although rigorous [[clinical trial]]s had not been conducted to confirm such relationships.<ref name="Goldfine">{{Cite journal |vauthors=Goldfine AB, Shoelson SE |date=January 2017 |title=Therapeutic approaches targeting inflammation for diabetes and associated cardiovascular risk |journal=The Journal of Clinical Investigation |volume=127 |issue=1 |pages=83–93 |doi=10.1172/jci88884 |pmc=5199685 |pmid=28045401 |doi-access=free}}</ref> |
|||
During clinical studies, inflammatory-related molecule levels were reduced and increased levels of anti-inflammatory molecules were seen within four weeks after patients began a very low calorie diet.<ref>{{cite journal |author=Clément K |title=Weight loss regulates inflammation-related genes in white adipose tissue of obese subjects |journal=FASEB J |volume=18 |issue=14 |pages=1657–1669 |year=2004 |pmid=15522911 |url=http://www.fasebj.org/cgi/content/full/18/14/1657 | doi = 10.1096/fj.04-2204com |author-separator=, |display-authors=1 |last2=Viguerie |first2=N |last3=Poitou |first3=C |last4=Carette |first4=C |last5=Pelloux |first5=V |last6=Curat |first6=CA |last7=Sicard |first7=A |last8=Rome |first8=S |last9=Benis |first9=A}}</ref> The association of systemic inflammation with [[insulin resistance]] and [[atherosclerosis]] is the subject of intense |
|||
research.<ref name=Stitzinger>{{cite web |url=https://openaccess.leidenuniv.nl/dspace/bitstream/1887/9729/11/01.pdf |publisher= The digital repository of Leiden University |title= Lipids, inflammation and atherosclerosis |author=M Stitzinger |year=2007 |accessdate=2007-11-02 |format= pdf|work=}}</ref> |
|||
[[C-reactive protein]] (CRP) is generated at a higher level in obese people, and may increase the risk for [[cardiovascular diseases]].<ref name="Choi">{{Cite journal |vauthors=Choi J, Joseph L, Pilote L |date=March 2013 |title=Obesity and C-reactive protein in various populations: a systematic review and meta-analysis |journal=Obesity Reviews |volume=14 |issue=3 |pages=232–44 |doi=10.1111/obr.12003 |pmid=23171381 |s2cid=206227739}}</ref> |
|||
Studies{{Which?|date=November 2010}} have shown in obesity that inflammation and [[macrophage]]-specific genes are unregulated in white adipose tissue (WAT). There were also signs of dramatic increase in circulating [[insulin]] level, adipocyte lipolysis and formation of multinucleate [[giant cell]]s. The fat-derived protein called [[angiopoietin]]-like protein 2 (Angptl2) elevates in fat tissues. Higher than normal Angptl2 level in fat tissues develop inflammation as well as insulin and leptin resistance. [[Leptin]] is a hormone protein secreted by stored fat that signals satiety. Leptin resistance plays a role in the process where appetite overrules the message of satiety. Angptl2 then starts an inflammatory cascade causing blood vessels to remodel and attract macrophages. Angptl2 is an adipocyte-derived inflammatory mediator linking obesity to systemic insulin resistance.{{Citation needed|date=November 2010}} It is possible that, as an inflammatory marker, [[Leptin#Clinical significance| leptin responds specifically to adipose-derived inflammatory cytokines]]. |
|||
== Outcomes == |
|||
[[C-reactive protein]] (CRP) is generated at a higher level in obese people. It raises when there is inflammation throughout the body. Mild elevation in CRP increase risk of heart attacks, strokes, high blood pressure, muscle weakness and fragility.{{Citation needed|date=November 2010}} |
|||
The outcome in a particular circumstance will be determined by the tissue in which the injury has occurred—and the injurious agent that is causing it. Here are the possible outcomes to inflammation:<ref name="robspath" /> |
|||
=== Systemic inflammation and overeating === |
|||
# '''Resolution'''<br />The complete restoration of the inflamed tissue back to a normal status. Inflammatory measures such as vasodilation, chemical production, and leukocyte infiltration cease, and damaged [[parenchyma]]l cells regenerate. Such is usually the outcome when limited or short-lived inflammation has occurred. |
|||
[[Hyperglycemia]] induces IL-6 production from endothelial cells and macrophages.<ref>Shoelson, Steven E., Jongsoon Lee, and Allison B. Goldfine. "Inflammation and Insulin Resistance." Journal of Clinical Investigation 116.7 (2006): 1793-801. Print.</ref> Meals high in [[saturated fat]], as well as meals high in [[calories]] irrespective of [[nutrient|macronutrient]] composition, have also been associated with increases in inflammatory markers.<ref>Blackburn P, Després JP, Lamarche B, Tremblay A, Bergeron J, Lemieux I, Couillard C. Impact of postprandial variation in triglyceridemia on low-density lipoprotein particle size. Metabolism. 2003 Nov;52(11):1379-86.</ref><ref>van Dijk SJ, Feskens EJ, Bos MB, Hoelen DW, Heijligenberg R, Bromhaar MG, de Groot LC, de Vries JH, Müller M, Afman LA. A saturated fatty acid-rich diet induces an obesity-linked proinflammatory gene expression profile in adipose tissue of subjects at risk of metabolic syndrome. Am J Clin Nutr. 2009 Dec;90(6):1656-64. Epub 2009 Oct 14.</ref> While the inflammatory responses are acute and arise in response to [[overeating]], the response may become chronic if the overeating is chronic. |
|||
# '''[[Fibrosis]]'''<br />Large amounts of tissue destruction, or damage in tissues unable to regenerate, cannot be regenerated completely by the body. Fibrous [[scarring]] occurs in these areas of damage, forming a scar composed primarily of [[collagen]]. The scar will not contain any specialized structures, such as [[parenchyma]]l cells, hence functional impairment may occur. |
|||
# '''Abscess formation'''<br />A cavity is formed containing pus, an opaque liquid containing dead white blood cells and bacteria with general debris from destroyed cells. |
|||
== Outcomes == |
|||
# '''Chronic inflammation'''<br />In acute inflammation, if the injurious agent persists then chronic inflammation will ensue. This process, marked by inflammation lasting many days, months or even years, may lead to the formation of a [[chronic wound]]. Chronic inflammation is characterised by the dominating presence of macrophages in the injured tissue. These cells are powerful defensive agents of the body, but the [[toxin]]s they release—including [[reactive oxygen species]]—are injurious to the organism's own tissues as well as invading agents. As a consequence, chronic inflammation is almost always accompanied by tissue destruction. |
|||
[[Image:Scar (xndr).jpg|250px|thumb|right|Scars present on the skin, evidence of fibrosis and healing of a wound]] |
|||
The outcome in a particular circumstance will be determined by the tissue in which the injury has occurred and the injurious agent that is causing it. Here are the possible outcomes to inflammation:<ref name="robspath" /> |
|||
# '''Resolution'''<br />The complete restoration of the inflamed tissue back to a normal status. Inflammatory measures such as vasodilation, chemical production, and leukocyte infiltration cease, and damaged [[parenchyma]]l cells regenerate. In situations where limited or short lived inflammation has occurred this is usually the outcome. |
|||
# '''Fibrosis'''<br />Large amounts of tissue destruction, or damage in tissues unable to regenerate, can not be regenerated completely by the body. Fibrous [[scarring]] occurs in these areas of damage, forming a scar composed primarily of [[collagen]]. The scar will not contain any specialized structures, such as [[parenchyma]]l cells, hence functional impairment may occur. |
|||
# '''Abscess Formation'''<br />A cavity is formed containing pus, an opaque liquid containing dead white blood cells and bacteria with general debris from destroyed cells. |
|||
# '''Chronic inflammation'''<br />In acute inflammation, if the injurious agent persists then chronic inflammation will ensue. This process, marked by inflammation lasting many days, months or even years, may lead to the formation of a [[chronic wound]]. Chronic inflammation is characterised by the dominating presence of macrophages in the injured tissue. These cells are powerful defensive agents of the body, but the [[toxin]]s they release (including [[reactive oxygen species]]) are injurious to the organism's own tissues as well as invading agents. Consequently, chronic inflammation is almost always accompanied by tissue destruction. |
|||
== Examples == |
== Examples == |
||
Inflammation is usually indicated by adding the suffix "[[wikt:-itis| |
Inflammation is usually indicated by adding the suffix "[[wikt:-itis|itis]]", as shown below. However, some conditions, such as [[asthma]] and [[pneumonia]], do not follow this convention. More examples are available at [[List of types of inflammation]]. |
||
<gallery> |
<gallery> |
||
File:Acute_Appendicitis.jpg|Acute [[appendicitis]] |
|||
File:Dermatitis.jpg|Acute [[dermatitis]] |
|||
File:Streptococcus pneumoniae meningitis, gross pathology 33 lores.jpg|Acute infective [[meningitis]] |
|||
File:Tonsillitis.jpg|Acute [[tonsillitis]] |
|||
</gallery> |
</gallery> |
||
== Exercise and Inflammation == |
|||
===Exercise-induced acute inflammation=== |
|||
Acute inflammation of the [[muscle cells]], as understood in [http://www.sport-fitness-advisor.com/exercise-physiology.html exercise] physiology,<ref>{{cite book|last=Wilmore|first=Jack|title=Physiology of Sport and Exercise|year=2008|publisher=Human Kinetics|location=Champaign, IL|isbn=978-0-7360-5583-3|pages=26–36, 98–120, 186–250, 213–218}}</ref> can result after [[Muscle contraction|induced]] [[Eccentric contraction|eccentric]] and [[Concentric contraction|concentric]] muscle training. Participation in eccentric training and conditioning, including resistance training and activities that emphasize eccentric lengthening of the [[muscle]] including downhill running on a moderate to high incline can result in considerable soreness within 24 to 48 hours, even though [[blood lactate]] levels, previously thought to cause muscle soreness, were much higher with level running. This [[delayed onset muscle soreness]] (DOMS) results from structural damage to the contractile filaments and [[Muscle cells|z-disks]], which has been noted especially in marathon runners whose muscle fibers revealed [[Marathon runner|remarkable damage]] to the muscle fibers after both training and marathon competition. The onset and timing of this [[Resistance training|gradient damage]] to the muscle parallels the degree of muscle soreness experienced by the runners. |
|||
Z-disks are the point of contact for the contractile proteins. They provide structural support for the transmission of force when the muscle fibers are activated to shorten. However, in marathon runners and those who prescribe to the [http://www.sport-fitness-advisor.com/fitt-principle.html overload principle] to enhance their muscles, show moderate Z-disk streaming and major disruption of the thick and thin filaments in parallel groups of sarcomeres as a result of the force of eccentric actions or stretching of the tightened muscle fibers. |
|||
This disruption of the muscle fibers triggers white blood cells to increase following the induced muscle soreness, leading to the inflammatory response observation from the induced muscle soreness. Elevations in plasma enzymes, myoglobinemia, and abnormal muscle histology and ultrastructure are concluded to be associated with the inflammatory response in [http://www.sport-fitness-advisor.com/delayed-onset-muscle-soreness.html DOMS]. High tension in the contractile-elastic system of muscle results in structural damage to the muscle fiber and plasmalemma and its epimysium, perimysium, and/or endomysium. The mysium damage disrupts calcium homeostasis in the injured fiber and fiber bundles, resulting in necrosis that peaks about 48 hours after exercise. The products of the macrophage activity and intracellular contents (such as histamines, kinins, and K<sup>+</sup>) accumulate outside the cells. These substances then stimulate the free nerve endings in the muscle; a process that appears accentuated by eccentric exercise, in which large forces are distributed over relatively small cross-sectional area of the muscle. |
|||
===Post-inflammatory muscle growth and repair=== |
|||
There is a known relationship between inflammation and muscle growth.<ref name="ReferenceA">Toth MJ, Matthews DE, Tracy RP, Previs MJ. Age-related differences in skeletal muscle protein synthesis: relation to markers of immune activation. Am J Physiol Endocrinol Metab. 2005 May;288(5):E883-91. Epub 2004 Dec 21.</ref> For instance, high doses of anti-inflammatory medicines (e.g., [[NSAID]]s) are able to blunt muscle growth.<ref name="ReferenceB">Mikkelsen UR, Langberg H, Helmark IC, Skovgaard D, Andersen LL, Kjaer M, Mackey AL. Local NSAID infusion inhibits satellite cell proliferation in human skeletal muscle after eccentric exercise. J Appl Physiol. 2009 Nov;107(5):1600-11. Epub 2009 Aug 27.</ref><ref name="ReferenceC">Trappe TA, White F, Lambert CP, Cesar D, Hellerstein M, Evans WJ. Effect of ibuprofen and acetaminophen on postexercise muscle protein synthesis. Am J Physiol Endocrinol Metab. 2002 Mar;282(3):E551-6.</ref> |
|||
It has been further theorized that the acute localized inflammatory responses to muscular contraction during exercise, as described above, are a necessary precursor to muscle growth.<ref>Marimuthu K, Murton AJ, Greenhaff PL. Mechanisms regulating muscle mass during disuse atrophy and rehabilitation in humans. J Appl Physiol. 2011 Feb;110(2):555-60.</ref> As a response to muscular contractions, the acute inflammatory response initiates the breakdown and removal of damaged muscle tissue.<ref name="Cannon">Cannon JG, St Pierre BA. Cytokines in exertion-induced skeletal muscle injury. Mol Cell Biochem. 1998 Feb;179(1-2):159-67. Review.</ref> Muscles can synthesize cytokines in response to contractions,<ref name="Lang_a">Lang CH, Hong-Brown L, Frost RA. Cytokine inhibition of JAK-STAT signaling: a new mechanism of growth hormone resistance. Pediatr Nephrol. 2005 Mar;20(3):306-12. Epub 2004 Nov 10. Review.</ref><ref>Pedersen BK, Toft AD. Effects of exercise on lymphocytes and cytokines. Br J Sports Med. 2000 Aug;34(4):246-51. Review.</ref><ref name="Bruunsgaard">Bruunsgaard H, Galbo H, Halkjaer-Kristensen J, Johansen TL, MacLean DA, Pedersen BK. Exercise-induced increase in serum interleukin-6 in humans is related to muscle damage. J Physiol. 1997 Mar 15;499 ( Pt 3):833-41.</ref> such that the cytokines [[IL1B|Interleukin-1 beta (IL-1β)]], TNF-α, and IL-6 are expressed in skeletal muscle up to 5 days after exercise.<ref name="Cannon" /> |
|||
In particular, the increase in levels of IL-6 can reach up to one hundred times that of resting levels.<ref name="Bruunsgaard" /> Depending on volume, intensity, and other training factors, the IL-6 increase associated with |
|||
training initiates about 4 hours after resistance training and remains elevated for up to 24 hours.<ref name="McKay">McKay BR, De Lisio M, Johnston AP, O’Reilly CE, Phillips SM, Tarnopolsky MA, Parise G. Association of interleukin-6 signalling with the muscle stem cell response following muscle-lengthening contractions in humans. PLoS One. 2009 Jun 24;4(6):e6027.</ref><ref>MacIntyre DL, Sorichter S, Mair J, Berg A, McKenzie DC. Markers of inflammation and myofibrillar proteins following eccentric exercise in humans. Eur J Appl Physiol. 2001 Mar;84(3):180-6.</ref><ref name="Louis 2007"/> |
|||
These acute increases in cytokines, as a response to muscle contractions, help initiate the process of muscle repair and growth by activating [[satellite cell]]s within the inflamed muscle. Satellite cells are crucial for skeletal muscle adaption to exercise.<ref name="Serrano">Serrano AL, Baeza-Raja B, Perdiguero E, Jardí M, Muñoz-Cánoves P. Interleukin-6 is an essential regulator of satellite cell-mediated skeletal muscle hypertrophy. Cell Metab. 2008 Jan;7(1):33-44.</ref> They contribute to hypertrophy by providing new myonuclei and repair damaged segments of mature myofibers for successful regeneration following injury- or exercise-induced muscle damage;<ref>Grounds MD, White JD, Rosenthal N, Bogoyevitch MA. The role of stem cells in skeletal and cardiac muscle repair. J Histochem Cytochem. 2002 May;50(5):589-610. Review.</ref><ref>Hawke TJ, Garry DJ. Myogenic satellite cells: physiology to molecular biology. J Appl Physiol. 2001 Aug;91(2):534-51. Review. Erratum in: J Appl Physiol 2001 Dec;91(6):2414.</ref><ref>Hawke TJ. Muscle stem cells and exercise training. Exerc Sport Sci Rev. 2005 Apr;33(2):63-8. Review.</ref> high-level [[powerlifting|powerlifters]] can have up to 100% more satellite cells than untrained controls.<ref>Kadi F, Eriksson A, Holmner S, Butler-Browne GS, Thornell LE. Cellular adaptation of the trapezius muscle in strength-trained athletes. Histochem Cell Biol. 1999 Mar;111(3):189-95.</ref><ref>Eriksson A, Kadi F, Malm C, Thornell LE. Skeletal muscle morphology in power-lifters with and without anabolic steroids. Histochem Cell Biol. 2005 Aug;124(2):167-75. Epub 2005 Sep 29.</ref> |
|||
A rapid and transient localization of the IL-6 receptor and increased IL-6 expression occurs in satellite cells following contractions.<ref name="McKay" /> IL-6 has been shown to mediate |
|||
hypertrophic muscle growth both ''[[in vitro]]'' and ''[[in vivo]]''.<ref name="Serrano" /> Unaccustomed exercise can increase IL-6 by up to sixfold at 5 hours post-exercise and threefold 8 days after exercise.<ref>Mikkelsen UR, Schjerling P, Helmark IC, Reitelseder S, Holm L, Skovgaard D, Langberg H, Kjær M, Heinemeier KM. Local NSAID infusion does not affect protein synthesis and gene expression in human muscle after eccentric exercise. Scand J Med Sci Sports. 2010 Aug 24. [Epub ahead of print]</ref> Also telling is the fact that NSAIDs can decrease satellite cell response to exercise<ref name="ReferenceB"/>, thereby reducing exercise-induced protein synthesis.<ref name="ReferenceC"/> |
|||
The increase in cytokines after resistance exercise coincides with the decrease in levels of [[myostatin]], a protein that inhibits muscle differentiation and growth.<ref name="Louis 2007">Louis E, Raue U, Yang Y, Jemiolo B, Trappe S. Time course of proteolytic, cytokine, and myostatin gene expression after acute exercise in human skeletal muscle. J Appl Physiol. 2007 Nov;103(5):1744-51. Epub 2007 Sep 6.</ref> The cytokine response to resistance exercise and moderate-intensity running occur differently, with the latter causing a more prolonged response, especially at the 12-24 hour mark.<ref name="Louis 2007"/> |
|||
=== Chronic inflammation and muscle loss === |
|||
Both chronic and extreme inflammation are associated with disruptions of anabolic signals initiating muscle growth. Chronic inflammation has been implicated as part of the cause of the [[sarcopenia|muscle loss that occurs with aging]].<ref name="ReferenceA"/><ref>Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, Nevitt M, Harris TB. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci. 2002 May;57(5):M326-32.</ref> Increased protein levels of myostatin have been described in patients with diseases characterized by chronic low-grade inflammation.<ref>Reardon KA, Davis J, Kapsa RM, Choong P, Byrne E. Myostatin, insulin-like growth factor-1, and leukemia inhibitory factor mRNAs are upregulated in chronic human disuse muscle atrophy. Muscle Nerve. 2001 Jul;24(7):893-9.</ref> Increased levels of TNF-α can suppress the AKT/mTOR pathway, a crucial pathway for regulating skeletal muscle hypertrophy,<ref>Shih, Michael. "Skeletal Muscle Hypertrophy Is Regulated via AKT/mTOR Pathway." BioCarta. Web. 21 Mar. 2011. [http://www.biocarta.com/pathfiles/m_igf1mtorpathway.asp].</ref> thereby increasing muscle [[catabolism]].<ref>Lang CH, Frost RA. Sepsis-induced suppression of skeletal muscle translation initiation mediated by tumor necrosis factor alpha. Metabolism. 2007 Jan;56(1):49-57.</ref><ref>Garcia-Martinez C, Lopez-Soriano FJ, and Argiles JM. Acute treatment with tumor-necrosis-factor-alpha induces changes in protein metabolism in rat skeletal-muscle. Molecular and Cellular Biochemistry 125: 11-18, 1993.</ref><ref>Janssen SPM, Gayan-Ramirez G, Van Den Bergh A, Herijgers P, Maes K, Verbeken E, and Decramer M. Interleukin-6 causes myocardial failure and skeletal muscle atrophy in rats. Circulation 111: 996-1005, 2005.</ref> Cytokines may [[receptor antagonist|antagonize]] the [[anabolic]] effects of [[Insulin-like growth factor 1| Insulin-like growth factor 1 (IGF-1)]].<ref name="Lang">Lang CH, Frost RA, Vary TC. Regulation of muscle protein synthesis during sepsis and inflammation. Am J Physiol Endocrinol Metab. 2007 Aug;293(2):E453-9. Epub 2007 May 15. Review.</ref><ref>Jurasinski CV, Vary TC. Insulin-like growth factor I accelerates protein synthesis in skeletal muscle during sepsis. Am J Physiol. 1995 Nov;269(5 Pt 1):E977-81.</ref> In the case of [[sepsis]], an extreme whole body inflammatory state, the synthesis of both [[myofibrillar hypertrophy|myofibrillar]] and [[sarcoplasmic hypertrophy|sarcoplasmic]] proteins are inhibited, with the inhibition taking place preferentially in [[skeletal muscle|fast-twitch muscle fibers]].<ref>Vary TC, Kimball SR. Regulation of hepatic protein synthesis in chronic inflammation and sepsis. Am J Physiol. 1992 Feb;262(2 Pt 1):C445-52.</ref><ref name="Lang" /> Sepsis is also able to prevent [[leucine]] from stimulating muscle protein synthesis.<ref name="Lang_a" /> In animal models, when inflammation is created, [[mTOR]] loses its ability to be stimulated by muscle growth.<ref>Lang CH, Frost RA, Bronson SK, Lynch CJ, Vary TC. Skeletal muscle protein balance in mTOR heterozygous mice in response to inflammation and leucine. Am J Physiol Endocrinol Metab. 2010 Jun;298(6):E1283-94. Epub 2010 Apr 13.</ref> |
|||
===Exercise as a treatment for inflammation=== |
|||
Regular physical activity is reported to decrease markers of inflammation{{Quantify|date=June 2011}},<ref>Smith JK, Dykes R, Douglas JE, Krishnaswamy G, Berk S. Long-term exercise and atherogenic activity of blood mononuclear cells in persons at risk of developing ischemic heart disease. JAMA. 1999 May 12;281(18):1722-7.</ref><ref>McFarlin BK, Flynn MG, Phillips MD, Stewart LK, Timmerman KL. Chronic resistance exercise training improves natural killer cell activity in older women. J Gerontol A Biol Sci Med Sci. 2005 Oct;60(10):1315-8.</ref><ref>Stewart LK, Flynn MG, Campbell WW, Craig BA, Robinson JP, McFarlin BK, Timmerman KL, Coen PM, Felker J, Talbert E. Influence of exercise training and age on CD14+ cell-surface expression of toll-like receptor 2 and 4. Brain Behav Immun. 2005 Sep;19(5):389-97.</ref> although the correlation is imperfect and seems to reveal differing results contingent upon training intensity. For instance, while baseline measurements of circulating inflammatory markers do not seem to differ greatly between healthy trained and untrained adults,<ref name="Gleeson 2006">Gleeson M. Immune system adaptation in elite athletes. Curr Opin Clin Nutr Metab Care. 2006 Nov;9(6):659-65. Review.</ref><ref>Pedersen BK, Hoffman-Goetz L. Exercise and the immune system: regulation, integration, and adaptation. Physiol Rev. 2000 Jul;80(3):1055-81. Review.</ref> long-term chronic training may help reduce chronic low-grade inflammation.<ref name="Ploeger 2009">Ploeger HE, Takken T, de Greef MH, Timmons BW. The effects of acute and chronic exercise on inflammatory markers in children and adults with a chronic inflammatory disease: a systematic review. Exerc Immunol Rev. 2009;15:6-41. Review.</ref> On the other hand, levels of inflammatory markers (IL-6) remained elevated longer into the recovery period following an acute bout of exercise in patients with inflammatory diseases, relative to the recovery of healthy controls.<ref name="Ploeger 2009"/> It may well be that low-intensity training can reduce resting pro-inflammatory markers (CRP, IL-6), while moderate-intensity training has milder and less-established anti-inflammatory benefits.<ref name="Gleeson 2006"/><ref>Nicklas BJ, Hsu FC, Brinkley TJ, Church T, Goodpaster BH, Kritchevsky SB, Pahor M. . Exercise training and plasma C-reactive protein and interleukin-6 in elderly people. J Am Geriatr Soc. 2008 Nov;56(11):2045-52.</ref><ref>Timmerman KL, Flynn MG, Coen PM, Markofski MM, Pence BD. Exercise training-induced lowering of inflammatory (CD14+CD16+) monocytes: a role in the anti-inflammatory influence of exercise? J Leukoc Biol. 2008 Nov;84(5):1271-8. Epub 2008 Aug 12.</ref><ref>Mackinnon LT. Chronic exercise training effects on immune function. Med Sci Sports Exerc. 2000 Jul;32(7 Suppl):S369-76. Review.</ref> There is a strong relationship between exhaustive exercise and chronic low-grade inflammation.<ref name="Suzuki 2003">Suzuki K, Nakaji S, Yamada M, Liu Q, Kurakake S, Okamura N, Kumae T, Umeda T, Sugawara K. Impact of a competitive marathon race on systemic cytokine and neutrophil responses. Med Sci Sports Exerc. 2003 Feb;35(2):348-55.</ref> Marathon running may enhance IL-6 levels as much as 100 times over normal and increases total leuckocyte count and neturophil mobilization.<ref name="Suzuki 2003"/> As such, individuals pursuing exercise as a means to treat the other factors behind chronic inflammation may wish to balance their exercise protocol with bouts of low-intensity training, while striving to avoid chronic over-exertion. |
|||
===Signal-to-noise theory=== |
|||
Given that localized acute inflammation is a necessary component for muscle growth, and that chronic low-grade inflammation is associated with a disruption of anabolic signals initiating muscle growth, it has been theorized that a [[signal-to-noise]] model may best describe the relationship between inflammation and muscle growth.<ref>Pilon, Brad. "Inflammation Affects Your Ability to Build Muscle." Inflammation Theory | Inflammation, Chronic Inflammation, Muscle Building, Health. Web. 27 Mar. 2011. <http://www.inflammationtheory.com/#2>.</ref> By keeping the "noise" of chronic inflammation to a minimum, the localized acute inflammatory response signals a stronger anabolic response than could be achieved with higher levels of chronic inflammation. |
|||
== See also == |
== See also == |
||
{{columns-list|colwidth=30em| |
|||
{{commons category|Inflammation}} |
|||
* [[Anaphylatoxin]] |
* [[Anaphylatoxin]] |
||
* [[Anti-inflammatory|Anti-inflammatories]] |
* [[Anti-inflammatory|Anti-inflammatories]] |
||
* [[Essential fatty acid interactions]] |
* [[Essential fatty acid interactions]] |
||
* [[Healing]] |
* [[Healing]] |
||
* [[Inflammaging]] |
|||
* [[Inflammatory cytokine]] |
|||
* [[Inflammatory reflex]] |
|||
* [[Interleukin]] |
* [[Interleukin]] |
||
* [[Lipoxin]] |
* [[Lipoxin]] |
||
* [[Neurogenic inflammation]] |
|||
* [[Substance P]] |
* [[Substance P]] |
||
* [[Stress (biology)]] |
|||
* [[Endothelial Cell Tropism]]}} |
|||
== Notes == |
|||
{{notelist}} |
|||
== References == |
== References == |
||
{{reflist |
{{reflist}} |
||
== External links == |
== External links == |
||
{{commons category|Inflammations}} |
|||
* [http://www.clevelandclinic.org/health/health-info/docs/0200/0217.asp?index=4857 What You Need to Know About Inflammation] at [[Cleveland Clinic]] |
|||
* [http://nutrition.about.com/od/dietsformedicaldisorders/a/antiinflamfood.htm Anti-Inflammatory Diet - Foods and Inflammation] at [[About.com]] |
|||
* {{MeshName|Inflammation}} |
* {{MeshName|Inflammation}} |
||
* [http://www.naturalantiinflammatory.org Information on Natural Anti Inflammatory - Herbs, Diets and Inflammation] |
|||
{{Inflammation}} |
{{Inflammation}} |
||
{{Immune system}} |
{{Immune system}} |
||
{{Pathology}} |
|||
{{Authority control}} |
|||
{{pathology}} |
|||
{{Use dmy dates|date=November 2010}} |
|||
[[Category: |
[[Category:Immunology]] |
||
[[Category:Animal physiology]] |
[[Category:Animal physiology]] |
||
[[Category:Pathology]] |
|||
[[Category:Inflammations]] |
[[Category:Inflammations]] |
||
[[Category:Human physiology]] |
|||
[[ar:التهاب]] |
|||
[[bs:Upala]] |
|||
[[bg:Възпаление]] |
|||
[[ca:Inflamació]] |
|||
[[cs:Zánět]] |
|||
[[cy:Llid (meddygaeth)]] |
|||
[[da:Betændelse]] |
|||
[[de:Entzündung]] |
|||
[[et:Põletik]] |
|||
[[el:Φλεγμονή]] |
|||
[[es:Inflamación]] |
|||
[[eo:Inflamo]] |
|||
[[eu:Hantura]] |
|||
[[fa:التهاب]] |
|||
[[fr:Inflammation]] |
|||
[[ko:염증]] |
|||
[[hr:Upala]] |
|||
[[io:Inflamo]] |
|||
[[id:Radang]] |
|||
[[it:Infiammazione]] |
|||
[[he:דלקת]] |
|||
[[la:Inflammatio]] |
|||
[[lt:Uždegimas]] |
|||
[[hu:Gyulladás]] |
|||
[[ml:കോശജ്വലനം]] |
|||
[[ms:Keradangan]] |
|||
[[nl:Ontsteking (geneeskunde)]] |
|||
[[ja:炎症]] |
|||
[[no:Betennelse]] |
|||
[[nds:Sweer (Medizin)]] |
|||
[[pl:Zapalenie]] |
|||
[[pt:Inflamação]] |
|||
[[ru:Воспаление]] |
|||
[[simple:Inflammation]] |
|||
[[sk:Zápal]] |
|||
[[sl:Vnetje]] |
|||
[[ckb:ھەوکردن]] |
|||
[[sr:Запаљење]] |
|||
[[sh:Upala]] |
|||
[[fi:Tulehdus]] |
|||
[[sv:Inflammation]] |
|||
[[ta:அழற்சி]] |
|||
[[th:การอักเสบ]] |
|||
[[tr:Enflamasyon]] |
|||
[[uk:Запалення]] |
|||
[[ur:التہاب]] |
|||
[[vi:Viêm]] |
|||
[[wa:Efouwaedje (medcene)]] |
|||
[[yi:אנצינדונג]] |
|||
[[zh:炎症]] |
|||
Latest revision as of 20:07, 29 December 2024
This article needs more reliable medical references for verification or relies too heavily on primary sources. (March 2021) |  |
| Inflammation | |
|---|---|
 | |
| An allergic reaction to cefaclor has led to inflammation of the skin on the foot. The cardinal signs of inflammation include: pain, heat, redness, swelling, and loss of function. Some of these indicators can be seen here. | |
| Specialty | Immunology, rheumatology |
| Symptoms | Heat, pain, redness, swelling |
| Complications | Asthma, pneumonia, autoimmune diseases |
| Duration | Acute: few days Chronic: up to many months, or years |
| Causes | Infection, physical injury, autoimmune disorder |
Inflammation (from Latin: inflammatio) is part of the biological response of body tissues to harmful stimuli, such as pathogens, damaged cells, or irritants.[1] The five cardinal signs are heat, pain, redness, swelling, and loss of function (Latin calor, dolor, rubor, tumor, and functio laesa).
Inflammation is a generic response, and therefore is considered a mechanism of innate immunity, whereas adaptive immunity is specific to each pathogen.[2]
Inflammation is a protective response involving immune cells, blood vessels, and molecular mediators. The function of inflammation is to eliminate the initial cause of cell injury, clear out damaged cells and tissues, and initiate tissue repair. Too little inflammation could lead to progressive tissue destruction by the harmful stimulus (e.g. bacteria) and compromise the survival of the organism. However inflammation can also have negative effects.[3] Too much inflammation, in the form of chronic inflammation, is associated with various diseases, such as hay fever, periodontal disease, atherosclerosis, and osteoarthritis.
Inflammation can be classified as acute or chronic. Acute inflammation is the initial response of the body to harmful stimuli, and is achieved by the increased movement of plasma and leukocytes (in particular granulocytes) from the blood into the injured tissues. A series of biochemical events propagates and matures the inflammatory response, involving the local vascular system, the immune system, and various cells in the injured tissue. Prolonged inflammation, known as chronic inflammation, leads to a progressive shift in the type of cells present at the site of inflammation, such as mononuclear cells, and involves simultaneous destruction and healing of the tissue.
Inflammation has also been classified as Type 1 and Type 2 based on the type of cytokines and helper T cells (Th1 and Th2) involved.[4]
Meaning
[edit]The earliest known reference for the term inflammation is around the early 15th century. The word root comes from Old French inflammation around the 14th century, which then comes from Latin inflammatio or inflammationem. Literally, the term relates to the word "flame", as the property of being "set on fire" or "to burn".[5]
The term inflammation is not a synonym for infection. Infection describes the interaction between the action of microbial invasion and the reaction of the body's inflammatory response—the two components are considered together in discussion of infection, and the word is used to imply a microbial invasive cause for the observed inflammatory reaction. Inflammation, on the other hand, describes just the body's immunovascular response, regardless of cause. But, because the two are often correlated, words ending in the suffix -itis (which means inflammation) are sometimes informally described as referring to infection: for example, the word urethritis strictly means only "urethral inflammation", but clinical health care providers usually discuss urethritis as a urethral infection because urethral microbial invasion is the most common cause of urethritis. However, the inflammation–infection distinction is crucial in situations in pathology and medical diagnosis that involve inflammation that is not driven by microbial invasion, such as cases of atherosclerosis, trauma, ischemia, and autoimmune diseases (including type III hypersensitivity).
Causes
[edit]- Burns[6]
- Frostbite
- Physical injury, blunt or penetrating[7]
- Foreign bodies, including splinters, dirt and debris
- Trauma[6]
- Ionizing radiation
Biological:
- Infection by pathogens[6]
- Immune reactions due to hypersensitivity
- Stress
Chemical:[6]
Psychological:
- Excitement[8]
Types
[edit]
|
| Acute | Chronic | |
|---|---|---|
| Causative agent | Bacterial pathogens, injured tissues | Persistent acute inflammation due to non-degradable pathogens, viral infection, persistent foreign bodies, or autoimmune reactions |
| Major cells involved | neutrophils (primarily), basophils (inflammatory response), and eosinophils (response to helminth worms and parasites), mononuclear cells (monocytes, macrophages) | Mononuclear cells (monocytes, macrophages, lymphocytes, plasma cells), fibroblasts |
| Primary mediators | Vasoactive amines, eicosanoids | IFN-γ and other cytokines, growth factors, reactive oxygen species, hydrolytic enzymes |
| Onset | Immediate | Delayed |
| Duration | Few days | Up to many months, or years |
| Outcomes | Resolution, abscess formation, chronic inflammation | Tissue destruction, fibrosis, necrosis |
Acute
[edit]Acute inflammation is a short-term process, usually appearing within a few minutes or hours and begins to cease upon the removal of the injurious stimulus.[9] It involves a coordinated and systemic mobilization response locally of various immune, endocrine and neurological mediators of acute inflammation. In a normal healthy response, it becomes activated, clears the pathogen and begins a repair process and then ceases.[10]
Acute inflammation occurs immediately upon injury, lasting only a few days.[11] Cytokines and chemokines promote the migration of neutrophils and macrophages to the site of inflammation.[11] Pathogens, allergens, toxins, burns, and frostbite are some of the typical causes of acute inflammation.[11] Toll-like receptors (TLRs) recognize microbial pathogens.[11] Acute inflammation can be a defensive mechanism to protect tissues against injury.[11] Inflammation lasting 2–6 weeks is designated subacute inflammation.[11][12]
Cardinal signs
[edit]| English | Latin |
|---|---|
| Redness | Rubor |
| Swelling | Tumor |
| Heat | Calor |
| Pain | Dolor |
| Loss of function | Functio laesa[b] |
Inflammation is characterized by five cardinal signs,[15][16] (the traditional names of which come from Latin):
The first four (classical signs) were described by Celsus (c. 30 BC–38 AD).[18]
Pain is due to the release of chemicals such as bradykinin and histamine that stimulate nerve endings.[15] Acute inflammation of the lung (usually in response to pneumonia) does not cause pain unless the inflammation involves the parietal pleura, which does have pain-sensitive nerve endings.[15] Heat and redness are due to increased blood flow at body core temperature to the inflamed site. Swelling is caused by accumulation of fluid.
Loss of function
[edit]The fifth sign, loss of function, is believed to have been added later by Galen,[19] Thomas Sydenham[20] or Rudolf Virchow.[9][15][16] Examples of loss of function include pain that inhibits mobility, severe swelling that prevents movement, having a worse sense of smell during a cold, or having difficulty breathing when bronchitis is present.[21][22] Loss of function has multiple causes.[15]
Acute process
[edit]This section needs more reliable medical references for verification or relies too heavily on primary sources. (April 2023) |  |
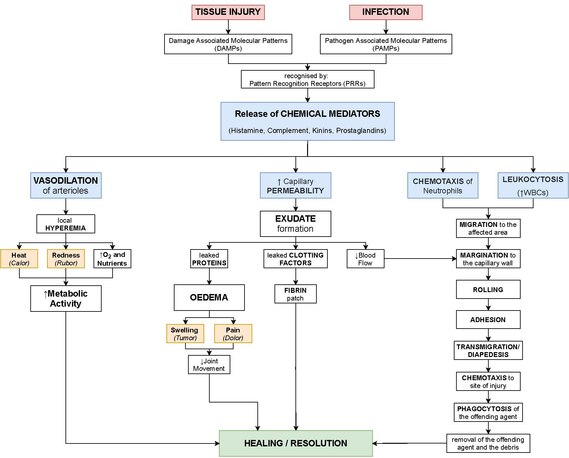

The process of acute inflammation is initiated by resident immune cells already present in the involved tissue, mainly resident macrophages, dendritic cells, histiocytes, Kupffer cells and mast cells. These cells possess surface receptors known as pattern recognition receptors (PRRs), which recognize (i.e., bind) two subclasses of molecules: pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). PAMPs are compounds that are associated with various pathogens, but which are distinguishable from host molecules. DAMPs are compounds that are associated with host-related injury and cell damage.
At the onset of an infection, burn, or other injuries, these cells undergo activation (one of the PRRs recognize a PAMP or DAMP) and release inflammatory mediators responsible for the clinical signs of inflammation. Vasodilation and its resulting increased blood flow causes the redness (rubor) and increased heat (calor). Increased permeability of the blood vessels results in an exudation (leakage) of plasma proteins and fluid into the tissue (edema), which manifests itself as swelling (tumor). Some of the released mediators such as bradykinin increase the sensitivity to pain (hyperalgesia, dolor). The mediator molecules also alter the blood vessels to permit the migration of leukocytes, mainly neutrophils and macrophages, to flow out of the blood vessels (extravasation) and into the tissue. The neutrophils migrate along a chemotactic gradient created by the local cells to reach the site of injury.[9] The loss of function (functio laesa) is probably the result of a neurological reflex in response to pain.
In addition to cell-derived mediators, several acellular biochemical cascade systems—consisting of preformed plasma proteins—act in parallel to initiate and propagate the inflammatory response. These include the complement system activated by bacteria and the coagulation and fibrinolysis systems activated by necrosis (e.g., burn, trauma).[9]
Acute inflammation may be regarded as the first line of defense against injury. Acute inflammatory response requires constant stimulation to be sustained. Inflammatory mediators are short-lived and are quickly degraded in the tissue. Hence, acute inflammation begins to cease once the stimulus has been removed.[9]
Chronic
[edit]Chronic inflammation is inflammation that lasts for months or years.[12] Macrophages, lymphocytes, and plasma cells predominate in chronic inflammation, in contrast to the neutrophils that predominate in acute inflammation.[12] Diabetes, cardiovascular disease, allergies, and chronic obstructive pulmonary disease are examples of diseases mediated by chronic inflammation.[12] Obesity, smoking, stress and insufficient diet are some of the factors that promote chronic inflammation.[12]
Cardinal signs
[edit]Common signs and symptoms that develop during chronic inflammation are:[12]
- Body pain, arthralgia, myalgia
- Chronic fatigue and insomnia
- Depression, anxiety and mood disorders
- Gastrointestinal complications such as constipation, diarrhea, and acid reflux
- Weight gain or loss
- Frequent infections
Vascular component
[edit]This section needs more reliable medical references for verification or relies too heavily on primary sources. (March 2021) |  |
Vasodilation and increased permeability
[edit]As defined, acute inflammation is an immunovascular response to inflammatory stimuli, which can include infection or trauma.[24][25] This means acute inflammation can be broadly divided into a vascular phase that occurs first, followed by a cellular phase involving immune cells (more specifically myeloid granulocytes in the acute setting).[24] The vascular component of acute inflammation involves the movement of plasma fluid, containing important proteins such as fibrin and immunoglobulins (antibodies), into inflamed tissue.
Upon contact with PAMPs, tissue macrophages and mastocytes release vasoactive amines such as histamine and serotonin, as well as eicosanoids such as prostaglandin E2 and leukotriene B4 to remodel the local vasculature.[26] Macrophages and endothelial cells release nitric oxide.[27] These mediators vasodilate and permeabilize the blood vessels, which results in the net distribution of blood plasma from the vessel into the tissue space. The increased collection of fluid into the tissue causes it to swell (edema).[26] This exuded tissue fluid contains various antimicrobial mediators from the plasma such as complement, lysozyme, antibodies, which can immediately deal damage to microbes, and opsonise the microbes in preparation for the cellular phase. If the inflammatory stimulus is a lacerating wound, exuded platelets, coagulants, plasmin and kinins can clot the wounded area using vitamin K-dependent mechanisms[28] and provide haemostasis in the first instance. These clotting mediators also provide a structural staging framework at the inflammatory tissue site in the form of a fibrin lattice – as would construction scaffolding at a construction site – for the purpose of aiding phagocytic debridement and wound repair later on. Some of the exuded tissue fluid is also funneled by lymphatics to the regional lymph nodes, flushing bacteria along to start the recognition and attack phase of the adaptive immune system.

Acute inflammation is characterized by marked vascular changes, including vasodilation, increased permeability and increased blood flow, which are induced by the actions of various inflammatory mediators.[26] Vasodilation occurs first at the arteriole level, progressing to the capillary level, and brings about a net increase in the amount of blood present, causing the redness and heat of inflammation. Increased permeability of the vessels results in the movement of plasma into the tissues, with resultant stasis due to the increase in the concentration of the cells within blood – a condition characterized by enlarged vessels packed with cells. Stasis allows leukocytes to marginate (move) along the endothelium, a process critical to their recruitment into the tissues. Normal flowing blood prevents this, as the shearing force along the periphery of the vessels moves cells in the blood into the middle of the vessel.
Plasma cascade systems
[edit]- The complement system, when activated, creates a cascade of chemical reactions that promotes opsonization, chemotaxis, and agglutination, and produces the MAC.
- The kinin system generates proteins capable of sustaining vasodilation and other physical inflammatory effects.
- The coagulation system or clotting cascade, which forms a protective protein mesh over sites of injury.
- The fibrinolysis system, which acts in opposition to the coagulation system, to counterbalance clotting and generate several other inflammatory mediators.
Plasma-derived mediators
[edit]* non-exhaustive list
| Name | Produced by | Description |
|---|---|---|
| Bradykinin | Kinin system | A vasoactive protein that is able to induce vasodilation, increase vascular permeability, cause smooth muscle contraction, and induce pain. |
| C3 | Complement system | Cleaves to produce C3a and C3b. C3a stimulates histamine release by mast cells, thereby producing vasodilation. C3b is able to bind to bacterial cell walls and act as an opsonin, which marks the invader as a target for phagocytosis. |
| C5a | Complement system | Stimulates histamine release by mast cells, thereby producing vasodilation. It is also able to act as a chemoattractant to direct cells via chemotaxis to the site of inflammation. |
| Factor XII (Hageman Factor) | Liver | A protein that circulates inactively, until activated by collagen, platelets, or exposed basement membranes via conformational change. When activated, it in turn is able to activate three plasma systems involved in inflammation: the kinin system, fibrinolysis system, and coagulation system. |
| Membrane attack complex | Complement system | A complex of the complement proteins C5b, C6, C7, C8, and multiple units of C9. The combination and activation of this range of complement proteins forms the membrane attack complex, which is able to insert into bacterial cell walls and causes cell lysis with ensuing bacterial death. |
| Plasmin | Fibrinolysis system | Able to break down fibrin clots, cleave complement protein C3, and activate Factor XII. |
| Thrombin | Coagulation system | Cleaves the soluble plasma protein fibrinogen to produce insoluble fibrin, which aggregates to form a blood clot. Thrombin can also bind to cells via the PAR1 receptor to trigger several other inflammatory responses, such as production of chemokines and nitric oxide. |
Cellular component
[edit]The cellular component involves leukocytes, which normally reside in blood and must move into the inflamed tissue via extravasation to aid in inflammation.[24] Some act as phagocytes, ingesting bacteria, viruses, and cellular debris. Others release enzymatic granules that damage pathogenic invaders. Leukocytes also release inflammatory mediators that develop and maintain the inflammatory response. In general, acute inflammation is mediated by granulocytes, whereas chronic inflammation is mediated by mononuclear cells such as monocytes and lymphocytes.
Leukocyte extravasation
[edit]

Various leukocytes, particularly neutrophils, are critically involved in the initiation and maintenance of inflammation. These cells must be able to move to the site of injury from their usual location in the blood, therefore mechanisms exist to recruit and direct leukocytes to the appropriate place. The process of leukocyte movement from the blood to the tissues through the blood vessels is known as extravasation and can be broadly divided up into a number of steps:
- Leukocyte margination and endothelial adhesion: The white blood cells within the vessels which are generally centrally located move peripherally towards the walls of the vessels.[29] Activated macrophages in the tissue release cytokines such as IL-1 and TNFα, which in turn leads to production of chemokines that bind to proteoglycans forming gradient in the inflamed tissue and along the endothelial wall.[26] Inflammatory cytokines induce the immediate expression of P-selectin on endothelial cell surfaces and P-selectin binds weakly to carbohydrate ligands on the surface of leukocytes and causes them to "roll" along the endothelial surface as bonds are made and broken. Cytokines released from injured cells induce the expression of E-selectin on endothelial cells, which functions similarly to P-selectin. Cytokines also induce the expression of integrin ligands such as ICAM-1 and VCAM-1 on endothelial cells, which mediate the adhesion and further slow leukocytes down. These weakly bound leukocytes are free to detach if not activated by chemokines produced in injured tissue after signal transduction via respective G protein-coupled receptors that activates integrins on the leukocyte surface for firm adhesion. Such activation increases the affinity of bound integrin receptors for ICAM-1 and VCAM-1 on the endothelial cell surface, firmly binding the leukocytes to the endothelium.
- Migration across the endothelium, known as transmigration, via the process of diapedesis: Chemokine gradients stimulate the adhered leukocytes to move between adjacent endothelial cells. The endothelial cells retract and the leukocytes pass through the basement membrane into the surrounding tissue using adhesion molecules such as ICAM-1.[29]
- Movement of leukocytes within the tissue via chemotaxis: Leukocytes reaching the tissue interstitium bind to extracellular matrix proteins via expressed integrins and CD44 to prevent them from leaving the site. A variety of molecules behave as chemoattractants, for example, C3a or C5a (the anaphylatoxins), and cause the leukocytes to move along a chemotactic gradient towards the source of inflammation.
Phagocytosis
[edit]Extravasated neutrophils in the cellular phase come into contact with microbes at the inflamed tissue. Phagocytes express cell-surface endocytic pattern recognition receptors (PRRs) that have affinity and efficacy against non-specific microbe-associated molecular patterns (PAMPs). Most PAMPs that bind to endocytic PRRs and initiate phagocytosis are cell wall components, including complex carbohydrates such as mannans and β-glucans, lipopolysaccharides (LPS), peptidoglycans, and surface proteins. Endocytic PRRs on phagocytes reflect these molecular patterns, with C-type lectin receptors binding to mannans and β-glucans, and scavenger receptors binding to LPS.
Upon endocytic PRR binding, actin-myosin cytoskeletal rearrangement adjacent to the plasma membrane occurs in a way that endocytoses the plasma membrane containing the PRR-PAMP complex, and the microbe. Phosphatidylinositol and Vps34-Vps15-Beclin1 signalling pathways have been implicated to traffic the endocytosed phagosome to intracellular lysosomes, where fusion of the phagosome and the lysosome produces a phagolysosome. The reactive oxygen species, superoxides and hypochlorite bleach within the phagolysosomes then kill microbes inside the phagocyte.
Phagocytic efficacy can be enhanced by opsonization. Plasma derived complement C3b and antibodies that exude into the inflamed tissue during the vascular phase bind to and coat the microbial antigens. As well as endocytic PRRs, phagocytes also express opsonin receptors Fc receptor and complement receptor 1 (CR1), which bind to antibodies and C3b, respectively. The co-stimulation of endocytic PRR and opsonin receptor increases the efficacy of the phagocytic process, enhancing the lysosomal elimination of the infective agent.
Cell-derived mediators
[edit]* non-exhaustive list
| Name | Type | Source | Description |
|---|---|---|---|
| Lysosome granules | Enzymes | Granulocytes | These cells contain a large variety of enzymes that perform a number of functions. Granules can be classified as either specific or azurophilic depending upon the contents, and are able to break down a number of substances, some of which may be plasma-derived proteins that allow these enzymes to act as inflammatory mediators. |
| GM-CSF | Glycoprotein | Macrophages, monocytes, T-cells, B-cells, and tissue-resident cells | Elevated GM-CSF has been shown to contribute to inflammation in inflammatory arthritis, osteoarthritis, colitis asthma, obesity, and COVID-19. |
| Histamine | Monoamine | Mast cells and basophils | Stored in preformed granules, histamine is released in response to a number of stimuli. It causes arteriole dilation, increased venous permeability, and a wide variety of organ-specific effects. |
| IFN-γ | Cytokine | T-cells, NK cells | Antiviral, immunoregulatory, and anti-tumour properties. This interferon was originally called macrophage-activating factor, and is especially important in the maintenance of chronic inflammation. |
| IL-6 | Cytokine and Myokine | Macrophages, osteoblasts, adipocytes, and smooth muscle cells (cytokine) Skeletal muscle cells (myokine) | Pro-inflammatory cytokine secreted by macrophages in response to pathogen-associated molecular patterns (PAMPs); pro-inflammatory cytokine secreted by adipocytes, especially in obesity; anti-inflammatory myokine secreted by skeletal muscle cells in response to exercise. |
| IL-8 | Chemokine | Primarily macrophages | Activation and chemoattraction of neutrophils, with a weak effect on monocytes and eosinophils. |
| Leukotriene B4 | Eicosanoid | Leukocytes, cancer cells | Able to mediate leukocyte adhesion and activation, allowing them to bind to the endothelium and migrate across it. In neutrophils, it is also a potent chemoattractant, and is able to induce the formation of reactive oxygen species and the release of lysosomal enzymes by these cells. |
| LTC4, LTD4 | Eicosanoid | eosinophils, mast cells, macrophages | These three Cysteine-containing leukotrienes contract lung airways, increase micro-vascular permeability, stimulate mucus secretion, and promote eosinophil-based inflammation in the lung, skin, nose, eye, and other tissues. |
| 5-oxo-eicosatetraenoic acid | Eicosanoid | Leukocytes, cancer cells | Potent stimulator of neutrophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation; monocyte chemotaxis; and with even greater potency eosinophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation. |
| 5-HETE | Eicosanoid | Leukocytes | Metabolic precursor to 5-Oxo-eicosatetraenoic acid, it is a less potent stimulator of neutrophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation; monocyte chemotaxis; and eosinophil chemotaxis, lysosome enzyme release, and reactive oxygen species formation. |
| Prostaglandins | Eicosanoid | Mast cells | A group of lipids that can cause vasodilation, fever, and pain. |
| Nitric oxide | Soluble gas | Macrophages, endothelial cells, some neurons | Potent vasodilator, relaxes smooth muscle, reduces platelet aggregation, aids in leukocyte recruitment, direct antimicrobial activity in high concentrations. |
| TNF-α and IL-1 | Cytokines | Primarily macrophages | Both affect a wide variety of cells to induce many similar inflammatory reactions: fever, production of cytokines, endothelial gene regulation, chemotaxis, leukocyte adherence, activation of fibroblasts. Responsible for the systemic effects of inflammation, such as loss of appetite and increased heart rate. TNF-α inhibits osteoblast differentiation. |
| Tryptase | Enzymes | Mast Cells | This serine protease is believed to be exclusively stored in mast cells and secreted, along with histamine, during mast cell activation.[30][31][32] |
Morphologic patterns
[edit]Specific patterns of acute and chronic inflammation are seen during particular situations that arise in the body, such as when inflammation occurs on an epithelial surface, or pyogenic bacteria are involved.
- Granulomatous inflammation: Characterised by the formation of granulomas, they are the result of a limited but diverse number of diseases, which include among others tuberculosis, leprosy, sarcoidosis, and syphilis.
- Fibrinous inflammation: Inflammation resulting in a large increase in vascular permeability allows fibrin to pass through the blood vessels. If an appropriate procoagulative stimulus is present, such as cancer cells,[9] a fibrinous exudate is deposited. This is commonly seen in serous cavities, where the conversion of fibrinous exudate into a scar can occur between serous membranes, limiting their function. The deposit sometimes forms a pseudomembrane sheet. During inflammation of the intestine (pseudomembranous colitis), pseudomembranous tubes can be formed.
- Purulent inflammation: Inflammation resulting in large amount of pus, which consists of neutrophils, dead cells, and fluid. Infection by pyogenic bacteria such as staphylococci is characteristic of this kind of inflammation. Large, localised collections of pus enclosed by surrounding tissues are called abscesses.
- Serous inflammation: Characterised by the copious effusion of non-viscous serous fluid, commonly produced by mesothelial cells of serous membranes, but may be derived from blood plasma. Skin blisters exemplify this pattern of inflammation.
- Ulcerative inflammation: Inflammation occurring near an epithelium can result in the necrotic loss of tissue from the surface, exposing lower layers. The subsequent excavation in the epithelium is known as an ulcer.
Disorders
[edit]

Inflammatory abnormalities are a large group of disorders that underlie a vast variety of human diseases. The immune system is often involved with inflammatory disorders, as demonstrated in both allergic reactions and some myopathies, with many immune system disorders resulting in abnormal inflammation. Non-immune diseases with causal origins in inflammatory processes include cancer, atherosclerosis, and ischemic heart disease.[9]
Examples of disorders associated with inflammation include:
- Acne vulgaris
- Asthma
- Autoimmune diseases
- Autoinflammatory diseases
- Celiac disease
- Chronic prostatitis
- Colitis
- Diverticulitis
- Familial Mediterranean Fever
- Glomerulonephritis
- Hidradenitis suppurativa
- Hypersensitivities
- Inflammatory bowel diseases
- Interstitial cystitis
- Lichen planus
- Mast Cell Activation Syndrome
- Mastocytosis
- Otitis
- Pelvic inflammatory disease
- Peripheral ulcerative keratitis
- Pneumonia
- Reperfusion injury
- Rheumatic fever
- Rheumatoid arthritis
- Rhinitis
- Sarcoidosis
- Transplant rejection
- Vasculitis
Atherosclerosis
[edit]Atherosclerosis, formerly considered a lipid storage disorder, is now understood as a chronic inflammatory condition involving the arterial walls.[33] Research has established a fundamental role for inflammation in mediating all stages of atherosclerosis from initiation through progression and, ultimately, the thrombotic complications from it.[33] These new findings reveal links between traditional risk factors like cholesterol levels and the underlying mechanisms of atherogenesis.
Clinical studies have shown that this emerging biology of inflammation in atherosclerosis applies directly to people.[33] For instance, elevation in markers of inflammation predicts outcomes of people with acute coronary syndromes, independently of myocardial damage. In addition, low-grade chronic inflammation, as indicated by levels of the inflammatory marker C-reactive protein, prospectively defines risk of atherosclerotic complications, thus adding to prognostic information provided by traditional risk factors, such as LDL levels.[34][33]
Moreover, certain treatments that reduce coronary risk also limit inflammation. Notably, lipid-lowering medications such as statins have shown anti-inflammatory effects, which may contribute to their efficacy beyond just lowering LDL levels.[35] This emerging understanding of inflammation's role in atherosclerosis has had significant clinical implications, influencing both risk stratification and therapeutic strategies.
Emerging treatments
[edit]Recent developments in the treatment of atherosclerosis have focused on addressing inflammation directly. New anti-inflammatory drugs, such as monoclonal antibodies targeting IL-1β, have been studied in large clinical trials, showing promising results in reducing cardiovascular events.[36] These drugs offer a potential new avenue for treatment, particularly for patients who do not respond adequately to statins. However, concerns about long-term safety and cost remain significant barriers to widespread adoption.
Connection to depression
[edit]Inflammatory processes can be triggered by negative cognition or their consequences, such as stress, violence, or deprivation. Negative cognition may therefore contribute to inflammation, which in turn can lead to depression. A 2019 meta-analysis found that chronic inflammation is associated with a 30% increased risk of developing major depressive disorder, supporting the link between inflammation and mental health.[37]
Allergy
[edit]An allergic reaction, formally known as type 1 hypersensitivity, is the result of an inappropriate immune response triggering inflammation, vasodilation, and nerve irritation. A common example is hay fever, which is caused by a hypersensitive response by mast cells to allergens. Pre-sensitised mast cells respond by degranulating, releasing vasoactive chemicals such as histamine. These chemicals propagate an excessive inflammatory response characterised by blood vessel dilation, production of pro-inflammatory molecules, cytokine release, and recruitment of leukocytes.[9] Severe inflammatory response may mature into a systemic response known as anaphylaxis.
Myopathies
[edit]Inflammatory myopathies are caused by the immune system inappropriately attacking components of muscle, leading to signs of muscle inflammation. They may occur in conjunction with other immune disorders, such as systemic sclerosis, and include dermatomyositis, polymyositis, and inclusion body myositis.[9]
Leukocyte defects
[edit]Due to the central role of leukocytes in the development and propagation of inflammation, defects in leukocyte functionality often result in a decreased capacity for inflammatory defense with subsequent vulnerability to infection.[9] Dysfunctional leukocytes may be unable to correctly bind to blood vessels due to surface receptor mutations, digest bacteria (Chédiak–Higashi syndrome), or produce microbicides (chronic granulomatous disease). In addition, diseases affecting the bone marrow may result in abnormal or few leukocytes.
Pharmacological
[edit]Certain drugs or exogenous chemical compounds are known to affect inflammation. Vitamin A deficiency, for example, causes an increase in inflammatory responses,[38] and anti-inflammatory drugs work specifically by inhibiting the enzymes that produce inflammatory eicosanoids. Additionally, certain illicit drugs such as cocaine and ecstasy may exert some of their detrimental effects by activating transcription factors intimately involved with inflammation (e.g. NF-κB).[39][40]
Cancer
[edit]Inflammation orchestrates the microenvironment around tumours, contributing to proliferation, survival and migration.[41] Cancer cells use selectins, chemokines and their receptors for invasion, migration and metastasis.[42] On the other hand, many cells of the immune system contribute to cancer immunology, suppressing cancer.[43] Molecular intersection between receptors of steroid hormones, which have important effects on cellular development, and transcription factors that play key roles in inflammation, such as NF-κB, may mediate some of the most critical effects of inflammatory stimuli on cancer cells.[44] This capacity of a mediator of inflammation to influence the effects of steroid hormones in cells is very likely to affect carcinogenesis. On the other hand, due to the modular nature of many steroid hormone receptors, this interaction may offer ways to interfere with cancer progression, through targeting of a specific protein domain in a specific cell type. Such an approach may limit side effects that are unrelated to the tumor of interest, and may help preserve vital homeostatic functions and developmental processes in the organism.
There is some evidence from 2009 to suggest that cancer-related inflammation (CRI) may lead to accumulation of random genetic alterations in cancer cells.[45][needs update]
Role in cancer
[edit]In 1863, Rudolf Virchow hypothesized that the origin of cancer was at sites of chronic inflammation.[42][46] As of 2012, chronic inflammation was estimated to contribute to approximately 15% to 25% of human cancers.[46][47]
Mediators and DNA damage in cancer
[edit]An inflammatory mediator is a messenger that acts on blood vessels and/or cells to promote an inflammatory response.[48] Inflammatory mediators that contribute to neoplasia include prostaglandins, inflammatory cytokines such as IL-1β, TNF-α, IL-6 and IL-15 and chemokines such as IL-8 and GRO-alpha.[49][46] These inflammatory mediators, and others, orchestrate an environment that fosters proliferation and survival.[42][49]
Inflammation also causes DNA damages due to the induction of reactive oxygen species (ROS) by various intracellular inflammatory mediators.[42][49][46] In addition, leukocytes and other phagocytic cells attracted to the site of inflammation induce DNA damages in proliferating cells through their generation of ROS and reactive nitrogen species (RNS). ROS and RNS are normally produced by these cells to fight infection.[42] ROS, alone, cause more than 20 types of DNA damage.[50] Oxidative DNA damages cause both mutations[51] and epigenetic alterations.[52][46][53] RNS also cause mutagenic DNA damages.[54]
A normal cell may undergo carcinogenesis to become a cancer cell if it is frequently subjected to DNA damage during long periods of chronic inflammation. DNA damages may cause genetic mutations due to inaccurate repair. In addition, mistakes in the DNA repair process may cause epigenetic alterations.[46][49][53] Mutations and epigenetic alterations that are replicated and provide a selective advantage during somatic cell proliferation may be carcinogenic.
Genome-wide analyses of human cancer tissues reveal that a single typical cancer cell may possess roughly 100 mutations in coding regions, 10–20 of which are "driver mutations" that contribute to cancer development.[46] However, chronic inflammation also causes epigenetic changes such as DNA methylations, that are often more common than mutations. Typically, several hundreds to thousands of genes are methylated in a cancer cell (see DNA methylation in cancer). Sites of oxidative damage in chromatin can recruit complexes that contain DNA methyltransferases (DNMTs), a histone deacetylase (SIRT1), and a histone methyltransferase (EZH2), and thus induce DNA methylation.[46][55][56] DNA methylation of a CpG island in a promoter region may cause silencing of its downstream gene (see CpG site and regulation of transcription in cancer). DNA repair genes, in particular, are frequently inactivated by methylation in various cancers (see hypermethylation of DNA repair genes in cancer). A 2018 report[57] evaluated the relative importance of mutations and epigenetic alterations in progression to two different types of cancer. This report showed that epigenetic alterations were much more important than mutations in generating gastric cancers (associated with inflammation).[58] However, mutations and epigenetic alterations were of roughly equal importance in generating esophageal squamous cell cancers (associated with tobacco chemicals and acetaldehyde, a product of alcohol metabolism).
HIV and AIDS
[edit]It has long been recognized that infection with HIV is characterized not only by development of profound immunodeficiency but also by sustained inflammation and immune activation.[59][60][61] A substantial body of evidence implicates chronic inflammation as a critical driver of immune dysfunction, premature appearance of aging-related diseases, and immune deficiency.[59][62] Many now regard HIV infection not only as an evolving virus-induced immunodeficiency, but also as chronic inflammatory disease.[63] Even after the introduction of effective antiretroviral therapy (ART) and effective suppression of viremia in HIV-infected individuals, chronic inflammation persists. Animal studies also support the relationship between immune activation and progressive cellular immune deficiency: SIVsm infection of its natural nonhuman primate hosts, the sooty mangabey, causes high-level viral replication but limited evidence of disease.[64][65] This lack of pathogenicity is accompanied by a lack of inflammation, immune activation and cellular proliferation. In sharp contrast, experimental SIVsm infection of rhesus macaque produces immune activation and AIDS-like disease with many parallels to human HIV infection.[66]
Delineating how CD4 T cells are depleted and how chronic inflammation and immune activation are induced lies at the heart of understanding HIV pathogenesis—one of the top priorities for HIV research by the Office of AIDS Research, National Institutes of Health. Recent studies demonstrated that caspase-1-mediated pyroptosis, a highly inflammatory form of programmed cell death, drives CD4 T-cell depletion and inflammation by HIV.[67][68][69] These are the two signature events that propel HIV disease progression to AIDS. Pyroptosis appears to create a pathogenic vicious cycle in which dying CD4 T cells and other immune cells (including macrophages and neutrophils) release inflammatory signals that recruit more cells into the infected lymphoid tissues to die. The feed-forward nature of this inflammatory response produces chronic inflammation and tissue injury.[70] Identifying pyroptosis as the predominant mechanism that causes CD4 T-cell depletion and chronic inflammation, provides novel therapeutic opportunities, namely caspase-1 which controls the pyroptotic pathway. In this regard, pyroptosis of CD4 T cells and secretion of pro-inflammatory cytokines such as IL-1β and IL-18 can be blocked in HIV-infected human lymphoid tissues by addition of the caspase-1 inhibitor VX-765,[67] which has already proven to be safe and well tolerated in phase II human clinical trials.[71] These findings could propel development of an entirely new class of "anti-AIDS" therapies that act by targeting the host rather than the virus. Such agents would almost certainly be used in combination with ART. By promoting "tolerance" of the virus instead of suppressing its replication, VX-765 or related drugs may mimic the evolutionary solutions occurring in multiple monkey hosts (e.g. the sooty mangabey) infected with species-specific lentiviruses that have led to a lack of disease, no decline in CD4 T-cell counts, and no chronic inflammation.
Resolution
[edit]The inflammatory response must be actively terminated when no longer needed to prevent unnecessary "bystander" damage to tissues.[9] Failure to do so results in chronic inflammation, and cellular destruction. Resolution of inflammation occurs by different mechanisms in different tissues. Mechanisms that serve to terminate inflammation include:[9][72]
- Short half-life of inflammatory mediators in vivo.
- Production and release of transforming growth factor (TGF) beta from macrophages[73][74][75]
- Production and release of interleukin 10 (IL-10)[76]
- Production of anti-inflammatory specialized proresolving mediators, i.e. lipoxins, resolvins, maresins, and neuroprotectins[77][78]
- Downregulation of pro-inflammatory molecules, such as leukotrienes.
- Upregulation of anti-inflammatory molecules such as the interleukin 1 receptor antagonist or the soluble tumor necrosis factor receptor (TNFR)
- Apoptosis of pro-inflammatory cells[79]
- Desensitization of receptors.
- Increased survival of cells in regions of inflammation due to their interaction with the extracellular matrix (ECM)[80][81]
- Downregulation of receptor activity by high concentrations of ligands
- Cleavage of chemokines by matrix metalloproteinases (MMPs) might lead to production of anti-inflammatory factors.[82]
Acute inflammation normally resolves by mechanisms that have remained somewhat elusive. Emerging evidence now suggests that an active, coordinated program of resolution initiates in the first few hours after an inflammatory response begins. After entering tissues, granulocytes promote the switch of arachidonic acid–derived prostaglandins and leukotrienes to lipoxins, which initiate the termination sequence. Neutrophil recruitment thus ceases and programmed death by apoptosis is engaged. These events coincide with the biosynthesis, from omega-3 polyunsaturated fatty acids, of resolvins and protectins, which critically shorten the period of neutrophil infiltration by initiating apoptosis. As a consequence, apoptotic neutrophils undergo phagocytosis by macrophages, leading to neutrophil clearance and release of anti-inflammatory and reparative cytokines such as transforming growth factor-β1. The anti-inflammatory program ends with the departure of macrophages through the lymphatics.[83]
Connection to depression
[edit]There is evidence for a link between inflammation and depression.[84] Inflammatory processes can be triggered by negative cognitions or their consequences, such as stress, violence, or deprivation. Thus, negative cognitions can cause inflammation that can, in turn, lead to depression.[85][86][dubious – discuss] In addition, there is increasing evidence that inflammation can cause depression because of the increase of cytokines, setting the brain into a "sickness mode".[87]
Classical symptoms of being physically sick, such as lethargy, show a large overlap in behaviors that characterize depression. Levels of cytokines tend to increase sharply during the depressive episodes of people with bipolar disorder and drop off during remission.[88] Furthermore, it has been shown in clinical trials that anti-inflammatory medicines taken in addition to antidepressants not only significantly improves symptoms but also increases the proportion of subjects positively responding to treatment.[89] Inflammations that lead to serious depression could be caused by common infections such as those caused by a virus, bacteria or even parasites.[90]
Connection to delirium
[edit]There is evidence for a link between inflammation and delirium based on the results of a recent longitudinal study investigating CRP in COVID-19 patients.[91]
Systemic effects
[edit]An infectious organism can escape the confines of the immediate tissue via the circulatory system or lymphatic system, where it may spread to other parts of the body. If an organism is not contained by the actions of acute inflammation, it may gain access to the lymphatic system via nearby lymph vessels. An infection of the lymph vessels is known as lymphangitis, and infection of a lymph node is known as lymphadenitis. When lymph nodes cannot destroy all pathogens, the infection spreads further. A pathogen can gain access to the bloodstream through lymphatic drainage into the circulatory system.
When inflammation overwhelms the host, systemic inflammatory response syndrome is diagnosed. When it is due to infection, the term sepsis is applied, with the terms bacteremia being applied specifically for bacterial sepsis and viremia specifically to viral sepsis. Vasodilation and organ dysfunction are serious problems associated with widespread infection that may lead to septic shock and death.[92]
Acute-phase proteins
[edit]Inflammation also is characterized by high systemic levels of acute-phase proteins. In acute inflammation, these proteins prove beneficial; however, in chronic inflammation, they can contribute to amyloidosis.[9] These proteins include C-reactive protein, serum amyloid A, and serum amyloid P, which cause a range of systemic effects including:[9]
- Fever
- Increased blood pressure
- Decreased sweating
- Malaise
- Loss of appetite
- Somnolence
Leukocyte numbers
[edit]Inflammation often affects the numbers of leukocytes present in the body:
- Leukocytosis is often seen during inflammation induced by infection, where it results in a large increase in the amount of leukocytes in the blood, especially immature cells. Leukocyte numbers usually increase to between 15 000 and 20 000 cells per microliter, but extreme cases can see it approach 100 000 cells per microliter.[9] Bacterial infection usually results in an increase of neutrophils, creating neutrophilia, whereas diseases such as asthma, hay fever, and parasite infestation result in an increase in eosinophils, creating eosinophilia.[9]
- Leukopenia can be induced by certain infections and diseases, including viral infection, Rickettsia infection, some protozoa, tuberculosis, and some cancers.[9]
Interleukins and obesity
[edit]With the discovery of interleukins (IL), the concept of systemic inflammation developed. Although the processes involved are identical to tissue inflammation, systemic inflammation is not confined to a particular tissue but involves the endothelium and other organ systems.
Chronic inflammation is widely observed in obesity.[93][94] Obese people commonly have many elevated markers of inflammation, including:[95][96]
Low-grade chronic inflammation is characterized by a two- to threefold increase in the systemic concentrations of cytokines such as TNF-α, IL-6, and CRP.[99] Waist circumference correlates significantly with systemic inflammatory response.[100]
Loss of white adipose tissue reduces levels of inflammation markers.[93] As of 2017 the association of systemic inflammation with insulin resistance and type 2 diabetes, and with atherosclerosis was under preliminary research, although rigorous clinical trials had not been conducted to confirm such relationships.[101]
C-reactive protein (CRP) is generated at a higher level in obese people, and may increase the risk for cardiovascular diseases.[102]
Outcomes
[edit]The outcome in a particular circumstance will be determined by the tissue in which the injury has occurred—and the injurious agent that is causing it. Here are the possible outcomes to inflammation:[9]
- Resolution
The complete restoration of the inflamed tissue back to a normal status. Inflammatory measures such as vasodilation, chemical production, and leukocyte infiltration cease, and damaged parenchymal cells regenerate. Such is usually the outcome when limited or short-lived inflammation has occurred. - Fibrosis
Large amounts of tissue destruction, or damage in tissues unable to regenerate, cannot be regenerated completely by the body. Fibrous scarring occurs in these areas of damage, forming a scar composed primarily of collagen. The scar will not contain any specialized structures, such as parenchymal cells, hence functional impairment may occur. - Abscess formation
A cavity is formed containing pus, an opaque liquid containing dead white blood cells and bacteria with general debris from destroyed cells. - Chronic inflammation
In acute inflammation, if the injurious agent persists then chronic inflammation will ensue. This process, marked by inflammation lasting many days, months or even years, may lead to the formation of a chronic wound. Chronic inflammation is characterised by the dominating presence of macrophages in the injured tissue. These cells are powerful defensive agents of the body, but the toxins they release—including reactive oxygen species—are injurious to the organism's own tissues as well as invading agents. As a consequence, chronic inflammation is almost always accompanied by tissue destruction.
Examples
[edit]Inflammation is usually indicated by adding the suffix "itis", as shown below. However, some conditions, such as asthma and pneumonia, do not follow this convention. More examples are available at List of types of inflammation.
-
Acute appendicitis
-
Acute dermatitis
-
Acute infective meningitis
-
Acute tonsillitis
See also
[edit]Notes
[edit]- ^ All these signs may be observed in specific instances, but no single sign must, as a matter of course, be present.[13] These are the original, or cardinal signs of inflammation.[13]
- ^ Functio laesa is an antiquated notion, as it is not unique to inflammation and is a characteristic of many disease states.[14]
References
[edit]- ^ Ferrero-Miliani L, Nielsen OH, Andersen PS, Girardin SE (February 2007). "Chronic inflammation: importance of NOD2 and NALP3 in interleukin-1beta generation". Clinical and Experimental Immunology. 147 (2): 227–235. doi:10.1111/j.1365-2249.2006.03261.x. PMC 1810472. PMID 17223962.
- ^ Abbas AB, Lichtman AH (2009). "Ch.2 Innate Immunity". Basic Immunology. Functions and disorders of the immune system (3rd ed.). Saunders/Elsevier. ISBN 978-1-4160-4688-2.
- ^ "Inflammation and Your Health". Cedars-Sinai.
- ^ Berger A (August 2000). "Th1 and Th2 responses: what are they?". BMJ. 321 (7258): 424. doi:10.1136/bmj.321.7258.424. PMC 27457. PMID 10938051. Archived from the original on 12 July 2021. Retrieved 1 July 2021.
- ^ "inflammation". Etymology of inflammation by etymonline. 28 September 2017. Retrieved 11 August 2024.
- ^ a b c d Hall J (2011). Guyton and Hall textbook of medical physiology (12th ed.). Philadelphia, Pa.: Saunders/Elsevier. p. 428. ISBN 978-1-4160-4574-8.
- ^ Granger DN, Senchenkova E (2010). "Leukocyte–Endothelial Cell Adhesion". Inflammation and the Microcirculation. Integrated Systems Physiology—From Cell to Function. Vol. 2. Morgan & Claypool Life Sciences. pp. 1–87. doi:10.4199/C00013ED1V01Y201006ISP008. PMID 21452440. Archived from the original on 21 January 2021. Retrieved 1 July 2017.
- ^ Piira OP, Miettinen JA, Hautala AJ, Huikuri HV, Tulppo MP (October 2013). "Physiological responses to emotional excitement in healthy subjects and patients with coronary artery disease". Autonomic Neuroscience. 177 (2): 280–5. doi:10.1016/j.autneu.2013.06.001. PMID 23916871. S2CID 19823098.
- ^ a b c d e f g h i j k l m n o p q r Robbins SL, Cotran RS, Kumar V, Collins T (1998). Robbins Pathologic Basis of Disease. Philadelphia: W.B Saunders Company. ISBN 978-0-7216-7335-6.
- ^ Kumar R, Clermont G, Vodovotz Y, Chow CC (September 2004). "The dynamics of acute inflammation". Journal of Theoretical Biology. 230 (2): 145–55. arXiv:q-bio/0404034. Bibcode:2004PhDT.......405K. doi:10.1016/j.jtbi.2004.04.044. PMID 15321710. S2CID 16992741.
- ^ a b c d e f Hannoodee S, Nasuruddin DN (2020). "Acute Inflammatory Response". StatPearls. PMID 32310543. Archived from the original on 15 June 2022. Retrieved 28 December 2020.
- ^ a b c d e f Pahwa R, Goyal A, Bansal P, Jialal I (7 August 2023). "Chronic inflammation". StatPearls, US National Library of Medicine. PMID 29630225. Retrieved 29 December 2024.
- ^ a b Stedman's Medical Dictionary (Twenty-fifth ed.). Williams & Wilkins. 1990.
- ^ Rather LJ (March 1971). "Disturbance of function (functio laesa): the legendary fifth cardinal sign of inflammation, added by Claudius Galen to the four cardinal signs of Celsus". Bulletin of the New York Academy of Medicine. 47 (3): 303–22. PMC 1749862. PMID 5276838.
- ^ a b c d e Chandrasoma P, Taylor CR (2005). "Part A. "General Pathology", Section II. "The Host Response to Injury", Chapter 3. "The Acute Inflammatory Response", sub-section "Cardinal Clinical Signs"". Concise Pathology (3rd ed.). McGraw-Hill. ISBN 978-0-8385-1499-3. OCLC 150148447. Archived from the original on 5 October 2008. Retrieved 5 November 2008.
- ^ a b Rather LJ (March 1971). "Disturbance of function (functio laesa): the legendary fifth cardinal sign of inflammation, added by Galen to the four cardinal signs of Celsus". Bulletin of the New York Academy of Medicine. 47 (3): 303–322. PMC 1749862. PMID 5276838.
- ^ Werner R (2009). A massage Therapist Guide to Pathology (4th ed.). Wolters Kluwer. ISBN 978-0-7817-6919-8. Archived from the original on 21 December 2015. Retrieved 6 October 2010.
- ^ Vogel WH, Berke A (2009). Brief History of Vision and Ocular Medicine. Kugler Publications. p. 97. ISBN 978-90-6299-220-1.
- ^ Porth C (2007). Essentials of pahtophysiology: concepts of altered health states. Hagerstown, MD: Lippincott Williams & Wilkins. p. 270. ISBN 978-0-7817-7087-3.
- ^ Dormandy T (2006). The worst of evils: man's fight against pain. New Haven, Conn: Yale University Press. pp. 22. ISBN 978-0-300-11322-8.
- ^ InformedHealth.org [Internet]. Institute for Quality and Efficiency in Health Care (IQWiG). 22 February 2018 – via www.ncbi.nlm.nih.gov.
- ^ "Inflammation | Definition, Symptoms, Treatment, & Facts | Britannica". www.britannica.com. 11 March 2024.
- ^ Robbins S, Cotran R, Kumar V, Abbas A, Aster J (2020). Pathologic basis of disease (10th ed.). Philadelphia, PA: Saunders Elsevier.
- ^ a b c Raiten DJ, Sakr Ashour FA, Ross AC, Meydani SN, Dawson HD, Stephensen CB, et al. (May 2015). "Inflammation and Nutritional Science for Programs/Policies and Interpretation of Research Evidence (INSPIRE)". The Journal of Nutrition. 145 (5): 1039S – 1108S. doi:10.3945/jn.114.194571. PMC 4448820. PMID 25833893.
- ^ Taams LS (July 2018). "Inflammation and immune resolution". Clinical and Experimental Immunology. 193 (1): 1–2. doi:10.1111/cei.13155. PMC 6037995. PMID 29987840.
- ^ a b c d Medzhitov R (July 2008). "Origin and physiological roles of inflammation". Nature. 454 (7203): 428–435. Bibcode:2008Natur.454..428M. doi:10.1038/nature07201. PMID 18650913. S2CID 205214291.
- ^ Mantovani A, Garlanda C (February 2023). Longo DL (ed.). "Humoral Innate Immunity and Acute-Phase Proteins". The New England Journal of Medicine. 388 (5): 439–452. doi:10.1056/NEJMra2206346. PMC 9912245. PMID 36724330.
- ^ Ferland G (2020). "Vitamin K". Present Knowledge in Nutrition. Elsevier. pp. 137–153. doi:10.1016/b978-0-323-66162-1.00008-1. ISBN 978-0-323-66162-1. Retrieved 17 February 2023.
- ^ a b Herrington S (2014). Muir's Textbook of Pathology (15th ed.). CRC Press. p. 59. ISBN 978-1-4441-8499-0.
- ^ Carstens E, Akiyama T, Cevikbas F, Kempkes C, Buhl T, Mess C, et al. (2014). "Role of Interleukin-31 and Oncostatin M in Itch and Neuroimmune Communication". In Carstens M, Akiyama T (eds.). Itch: Mechanisms and Treatment. Frontiers in Neuroscience. Boca Raton (FL): CRC Press/Taylor & Francis. ISBN 978-1-4665-0543-8. PMID 24830021.
- ^ Caughey GH (June 2007). "Mast cell tryptases and chymases in inflammation and host defense". Immunological Reviews. 217 (1): 141–54. doi:10.1111/j.1600-065x.2007.00509.x. PMC 2275918. PMID 17498057.
- ^ Caughey GH (May 2016). "Mast cell proteases as pharmacological targets". European Journal of Pharmacology. Pharmacological modulation of Mast cells and Basophils. 778: 44–55. doi:10.1016/j.ejphar.2015.04.045. PMC 4636979. PMID 25958181.
- ^ a b c d Libby P (November 2021). "Inflammation during the life cycle of the atherosclerotic plaque". Cardiovascular Research. 117 (13): 2525–2536. doi:10.1093/cvr/cvab303. PMC 8783385. PMID 34550337.
- ^ Spagnoli LG, Bonanno E, Sangiorgi G, Mauriello A (November 2007). "Role of inflammation in atherosclerosis". Journal of Nuclear Medicine. 48 (11): 1800–1815. doi:10.2967/jnumed.107.038661. PMID 17942804.
- ^ Morofuji Y, Nakagawa S, Ujifuku K, Fujimoto T, Otsuka K, Niwa M, et al. (January 2022). "Beyond Lipid-Lowering: Effects of Statins on Cardiovascular and Cerebrovascular Diseases and Cancer". Pharmaceuticals. 15 (2): 151. doi:10.3390/ph15020151. PMC 8877351. PMID 35215263.
- ^ Szekely Y, Arbel Y (June 2018). "A Review of Interleukin-1 in Heart Disease: Where Do We Stand Today?". Cardiology and Therapy. 7 (1): 25–44. doi:10.1007/s40119-018-0104-3. PMC 5986669. PMID 29417406.
- ^ Osimo EF, Pillinger T, Rodriguez IM, Khandaker GM, Pariante CM, Howes OD (July 2020). "Inflammatory markers in depression: A meta-analysis of mean differences and variability in 5,166 patients and 5,083 controls". Brain, Behavior, and Immunity. 87: 901–909. doi:10.1016/j.bbi.2020.02.010. PMC 7327519. PMID 32113908.
- ^ Wiedermann U, Chen XJ, Enerbäck L, Hanson LA, Kahu H, Dahlgren UI (December 1996). "Vitamin A deficiency increases inflammatory responses". Scandinavian Journal of Immunology. 44 (6): 578–84. doi:10.1046/j.1365-3083.1996.d01-351.x. PMID 8972739. S2CID 3079540.
- ^ Hargrave BY, Tiangco DA, Lattanzio FA, Beebe SJ (2003). "Cocaine, not morphine, causes the generation of reactive oxygen species and activation of NF-kappaB in transiently cotransfected heart cells". Cardiovascular Toxicology. 3 (2): 141–51. doi:10.1385/CT:3:2:141. PMID 14501032. S2CID 35240781.
- ^ Montiel-Duarte C, Ansorena E, López-Zabalza MJ, Cenarruzabeitia E, Iraburu MJ (March 2004). "Role of reactive oxygen species, glutathione and NF-kappaB in apoptosis induced by 3,4-methylenedioxymethamphetamine ("Ecstasy") on hepatic stellate cells". Biochemical Pharmacology. 67 (6): 1025–33. doi:10.1016/j.bcp.2003.10.020. PMID 15006539.
- ^ Ungefroren H, Sebens S, Seidl D, Lehnert H, Hass R (September 2011). "Interaction of tumor cells with the microenvironment". Cell Communication and Signaling. 9: 18. doi:10.1186/1478-811X-9-18. PMC 3180438. PMID 21914164.
- ^ a b c d e Coussens LM, Werb Z (2002). "Inflammation and cancer". Nature. 420 (6917): 860–7. Bibcode:2002Natur.420..860C. doi:10.1038/nature01322. PMC 2803035. PMID 12490959.
- ^ Gunn L, Ding C, Liu M, Ma Y, Qi C, Cai Y, et al. (September 2012). "Opposing roles for complement component C5a in tumor progression and the tumor microenvironment". Journal of Immunology. 189 (6): 2985–94. doi:10.4049/jimmunol.1200846. PMC 3436956. PMID 22914051.
- ^ Copland JA, Sheffield-Moore M, Koldzic-Zivanovic N, Gentry S, Lamprou G, Tzortzatou-Stathopoulou F, et al. (June 2009). "Sex steroid receptors in skeletal differentiation and epithelial neoplasia: is tissue-specific intervention possible?". BioEssays. 31 (6): 629–41. doi:10.1002/bies.200800138. PMID 19382224. S2CID 205469320.
- ^ Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A (July 2009). "Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability". Carcinogenesis (review). 30 (7): 1073–81. doi:10.1093/carcin/bgp127. PMID 19468060.
- ^ a b c d e f g h Chiba T, Marusawa H, Ushijima T (September 2012). "Inflammation-associated cancer development in digestive organs: mechanisms and roles for genetic and epigenetic modulation" (PDF). Gastroenterology. 143 (3): 550–563. doi:10.1053/j.gastro.2012.07.009. hdl:2433/160134. PMID 22796521. S2CID 206226588. Archived (PDF) from the original on 29 August 2022. Retrieved 9 June 2018.
- ^ Mantovani A, Allavena P, Sica A, Balkwill F (July 2008). "Cancer-related inflammation" (PDF). Nature. 454 (7203): 436–44. Bibcode:2008Natur.454..436M. doi:10.1038/nature07205. hdl:2434/145688. PMID 18650914. S2CID 4429118. Archived (PDF) from the original on 30 October 2022. Retrieved 9 June 2018.
- ^ Larsen GL, Henson PM (1983). "Mediators of inflammation". Annual Review of Immunology. 1: 335–59. doi:10.1146/annurev.iy.01.040183.002003. PMID 6399978.
- ^ a b c d Shacter E, Weitzman SA (February 2002). "Chronic inflammation and cancer". Oncology. 16 (2): 217–26, 229, discussion 230–2. PMID 11866137.
- ^ Yu Y, Cui Y, Niedernhofer LJ, Wang Y (December 2016). "Occurrence, Biological Consequences, and Human Health Relevance of Oxidative Stress-Induced DNA Damage". Chemical Research in Toxicology. 29 (12): 2008–2039. doi:10.1021/acs.chemrestox.6b00265. PMC 5614522. PMID 27989142.
- ^ Dizdaroglu M (December 2012). "Oxidatively induced DNA damage: mechanisms, repair and disease". Cancer Letters. 327 (1–2): 26–47. doi:10.1016/j.canlet.2012.01.016. PMID 22293091.
- ^ Nishida N, Kudo M (2013). "Oxidative stress and epigenetic instability in human hepatocarcinogenesis". Digestive Diseases. 31 (5–6): 447–53. doi:10.1159/000355243. PMID 24281019.
- ^ a b Ding N, Maiuri AR, O'Hagan HM (2017). "The emerging role of epigenetic modifiers in repair of DNA damage associated with chronic inflammatory diseases". Mutation Research. 780: 69–81. doi:10.1016/j.mrrev.2017.09.005. PMC 6690501. PMID 31395351.
- ^ Kawanishi S, Ohnishi S, Ma N, Hiraku Y, Oikawa S, Murata M (2016). "Nitrative and oxidative DNA damage in infection-related carcinogenesis in relation to cancer stem cells". Genes and Environment. 38 (1): 26. Bibcode:2016GeneE..38...26K. doi:10.1186/s41021-016-0055-7. PMC 5203929. PMID 28050219.
- ^ O'Hagan HM, Wang W, Sen S, Destefano Shields C, Lee SS, Zhang YW, et al. (November 2011). "Oxidative damage targets complexes containing DNA methyltransferases, SIRT1, and polycomb members to promoter CpG Islands". Cancer Cell. 20 (5): 606–19. doi:10.1016/j.ccr.2011.09.012. PMC 3220885. PMID 22094255.
- ^ Maiuri AR, Peng M, Podicheti R, Sriramkumar S, Kamplain CM, Rusch DB, et al. (July 2017). "Mismatch Repair Proteins Initiate Epigenetic Alterations during Inflammation-Driven Tumorigenesis". Cancer Research. 77 (13): 3467–3478. doi:10.1158/0008-5472.CAN-17-0056. PMC 5516887. PMID 28522752.
- ^ Yamashita S, Kishino T, Takahashi T, Shimazu T, Charvat H, Kakugawa Y, et al. (February 2018). "Genetic and epigenetic alterations in normal tissues have differential impacts on cancer risk among tissues". Proceedings of the National Academy of Sciences of the United States of America. 115 (6): 1328–1333. Bibcode:2018PNAS..115.1328Y. doi:10.1073/pnas.1717340115. PMC 5819434. PMID 29358395.
- ^ Raza Y, Khan A, Farooqui A, Mubarak M, Facista A, Akhtar SS, et al. (October 2014). "Oxidative DNA damage as a potential early biomarker of Helicobacter pylori associated carcinogenesis". Pathology & Oncology Research. 20 (4): 839–46. doi:10.1007/s12253-014-9762-1. PMID 24664859. S2CID 18727504.
- ^ a b Deeks SG (1 January 2011). "HIV infection, inflammation, immunosenescence, and aging". Annual Review of Medicine. 62: 141–55. doi:10.1146/annurev-med-042909-093756. PMC 3759035. PMID 21090961.
- ^ Klatt NR, Chomont N, Douek DC, Deeks SG (July 2013). "Immune activation and HIV persistence: implications for curative approaches to HIV infection". Immunological Reviews. 254 (1): 326–42. doi:10.1111/imr.12065. PMC 3694608. PMID 23772629.
- ^ Salazar-Gonzalez JF, Martinez-Maza O, Nishanian P, Aziz N, Shen LP, Grosser S, et al. (August 1998). "Increased immune activation precedes the inflection point of CD4 T cells and the increased serum virus load in human immunodeficiency virus infection". The Journal of Infectious Diseases. 178 (2): 423–30. doi:10.1086/515629. PMID 9697722.
- ^ Ipp H, Zemlin A (February 2013). "The paradox of the immune response in HIV infection: when inflammation becomes harmful". Clinica Chimica Acta; International Journal of Clinical Chemistry. 416: 96–9. doi:10.1016/j.cca.2012.11.025. PMID 23228847.
- ^ Nasi M, Pinti M, Mussini C, Cossarizza A (October 2014). "Persistent inflammation in HIV infection: established concepts, new perspectives". Immunology Letters. 161 (2): 184–8. doi:10.1016/j.imlet.2014.01.008. PMID 24487059.
- ^ Milush JM, Mir KD, Sundaravaradan V, Gordon SN, Engram J, Cano CA, et al. (March 2011). "Lack of clinical AIDS in SIV-infected sooty mangabeys with significant CD4+ T cell loss is associated with double-negative T cells". The Journal of Clinical Investigation. 121 (3): 1102–10. doi:10.1172/JCI44876. PMC 3049370. PMID 21317533.
- ^ Rey-Cuillé MA, Berthier JL, Bomsel-Demontoy MC, Chaduc Y, Montagnier L, Hovanessian AG, et al. (May 1998). "Simian immunodeficiency virus replicates to high levels in sooty mangabeys without inducing disease". Journal of Virology. 72 (5): 3872–86. doi:10.1128/JVI.72.5.3872-3886.1998. PMC 109612. PMID 9557672.
- ^ Chahroudi A, Bosinger SE, Vanderford TH, Paiardini M, Silvestri G (March 2012). "Natural SIV hosts: showing AIDS the door". Science. 335 (6073): 1188–93. Bibcode:2012Sci...335.1188C. doi:10.1126/science.1217550. PMC 3822437. PMID 22403383.
- ^ a b Doitsh G, Galloway NL, Geng X, Yang Z, Monroe KM, Zepeda O, et al. (January 2014). "Cell death by pyroptosis drives CD4 T-cell depletion in HIV-1 infection". Nature. 505 (7484): 509–14. Bibcode:2014Natur.505..509D. doi:10.1038/nature12940. PMC 4047036. PMID 24356306.
- ^ Monroe KM, Yang Z, Johnson JR, Geng X, Doitsh G, Krogan NJ, et al. (January 2014). "IFI16 DNA sensor is required for death of lymphoid CD4 T cells abortively infected with HIV". Science. 343 (6169): 428–32. Bibcode:2014Sci...343..428M. doi:10.1126/science.1243640. PMC 3976200. PMID 24356113.
- ^ Galloway NL, Doitsh G, Monroe KM, Yang Z, Muñoz-Arias I, Levy DN, et al. (September 2015). "Cell-to-Cell Transmission of HIV-1 Is Required to Trigger Pyroptotic Death of Lymphoid-Tissue-Derived CD4 T Cells". Cell Reports. 12 (10): 1555–1563. doi:10.1016/j.celrep.2015.08.011. PMC 4565731. PMID 26321639.
- ^ Doitsh G, Greene WC (March 2016). "Dissecting How CD4 T Cells Are Lost During HIV Infection". Cell Host & Microbe. 19 (3): 280–91. doi:10.1016/j.chom.2016.02.012. PMC 4835240. PMID 26962940.
- ^ "Study of VX-765 in Subjects With Treatment-resistant Partial Epilepsy – Full Text View – ClinicalTrials.gov". clinicaltrials.gov. 19 December 2013. Archived from the original on 26 September 2022. Retrieved 21 May 2016.
- ^ Eming SA, Krieg T, Davidson JM (March 2007). "Inflammation in wound repair: molecular and cellular mechanisms". The Journal of Investigative Dermatology. 127 (3): 514–25. doi:10.1038/sj.jid.5700701. PMID 17299434.
- ^ Ashcroft GS, Yang X, Glick AB, Weinstein M, Letterio JL, Mizel DE, et al. (September 1999). "Mice lacking Smad3 show accelerated wound healing and an impaired local inflammatory response". Nature Cell Biology. 1 (5): 260–6. doi:10.1038/12971. PMID 10559937. S2CID 37216623.
- ^ Ashcroft GS (December 1999). "Bidirectional regulation of macrophage function by TGF-beta". Microbes and Infection. 1 (15): 1275–82. doi:10.1016/S1286-4579(99)00257-9. PMID 10611755. Archived from the original on 10 January 2020. Retrieved 11 September 2019.
- ^ Werner F, Jain MK, Feinberg MW, Sibinga NE, Pellacani A, Wiesel P, et al. (November 2000). "Transforming growth factor-beta 1 inhibition of macrophage activation is mediated via Smad3". The Journal of Biological Chemistry. 275 (47): 36653–8. doi:10.1074/jbc.M004536200. PMID 10973958.
- ^ Sato Y, Ohshima T, Kondo T (November 1999). "Regulatory role of endogenous interleukin-10 in cutaneous inflammatory response of murine wound healing". Biochemical and Biophysical Research Communications. 265 (1): 194–9. doi:10.1006/bbrc.1999.1455. PMID 10548513.
- ^ Serhan CN (August 2008). "Controlling the resolution of acute inflammation: a new genus of dual anti-inflammatory and proresolving mediators". Journal of Periodontology. 79 (8 Suppl): 1520–6. doi:10.1902/jop.2008.080231. PMID 18673006.
- ^ Headland SE, Norling LV (May 2015). "The resolution of inflammation: Principles and challenges". Seminars in Immunology. 27 (3): 149–60. doi:10.1016/j.smim.2015.03.014. PMID 25911383.
- ^ Greenhalgh DG (September 1998). "The role of apoptosis in wound healing". The International Journal of Biochemistry & Cell Biology. 30 (9): 1019–30. doi:10.1016/S1357-2725(98)00058-2. PMID 9785465.
- ^ Jiang D, Liang J, Fan J, Yu S, Chen S, Luo Y, et al. (November 2005). "Regulation of lung injury and repair by Toll-like receptors and hyaluronan". Nature Medicine. 11 (11): 1173–9. doi:10.1038/nm1315. PMID 16244651. S2CID 11765495.
- ^ Teder P, Vandivier RW, Jiang D, Liang J, Cohn L, Puré E, et al. (April 2002). "Resolution of lung inflammation by CD44". Science. 296 (5565): 155–8. Bibcode:2002Sci...296..155T. doi:10.1126/science.1069659. PMID 11935029. S2CID 7905603.
- ^ McQuibban GA, Gong JH, Tam EM, McCulloch CA, Clark-Lewis I, Overall CM (August 2000). "Inflammation dampened by gelatinase A cleavage of monocyte chemoattractant protein-3". Science. 289 (5482): 1202–6. Bibcode:2000Sci...289.1202M. doi:10.1126/science.289.5482.1202. PMID 10947989.
- ^ Serhan CN, Savill J (December 2005). "Resolution of inflammation: the beginning programs the end". Nature Immunology. 6 (12): 1191–7. doi:10.1038/ni1276. PMID 16369558. S2CID 22379843.
- ^ Berk M, Williams LJ, Jacka FN, O'Neil A, Pasco JA, Moylan S, et al. (September 2013). "So depression is an inflammatory disease, but where does the inflammation come from?". BMC Medicine. 11: 200. doi:10.1186/1741-7015-11-200. PMC 3846682. PMID 24228900.
- ^ Cox WT, Abramson LY, Devine PG, Hollon SD (September 2012). "Stereotypes, Prejudice, and Depression: The Integrated Perspective". Perspectives on Psychological Science. 7 (5): 427–49. doi:10.1177/1745691612455204. PMID 26168502. S2CID 1512121.
- ^ Kiecolt-Glaser JK, Derry HM, Fagundes CP (November 2015). "Inflammation: depression fans the flames and feasts on the heat". The American Journal of Psychiatry. 172 (11): 1075–91. doi:10.1176/appi.ajp.2015.15020152. PMC 6511978. PMID 26357876.
- ^ Williams C (4 January 2015). "Is depression a kind of allergic reaction?". The Guardian. Archived from the original on 21 October 2022. Retrieved 11 December 2016.
- ^ Brietzke E, Stertz L, Fernandes BS, Kauer-Sant'anna M, Mascarenhas M, Escosteguy Vargas A, et al. (August 2009). "Comparison of cytokine levels in depressed, manic and euthymic patients with bipolar disorder". Journal of Affective Disorders. 116 (3): 214–7. doi:10.1016/j.jad.2008.12.001. PMID 19251324.
- ^ Müller N, Schwarz MJ, Dehning S, Douhe A, Cerovecki A, Goldstein-Müller B, et al. (July 2006). "The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine". Molecular Psychiatry. 11 (7): 680–4. doi:10.1038/sj.mp.4001805. PMID 16491133.
- ^ Canli T (2014). "Reconceptualizing major depressive disorder as an infectious disease". Biology of Mood & Anxiety Disorders. 4: 10. doi:10.1186/2045-5380-4-10. PMC 4215336. PMID 25364500.
- ^ Saini A, Oh TH, Ghanem DA, Castro M, Butler M, Sin Fai Lam CC, et al. (October 2022). "Inflammatory and blood gas markers of COVID-19 delirium compared to non-COVID-19 delirium: a cross-sectional study". Aging & Mental Health. 26 (10): 2054–2061. doi:10.1080/13607863.2021.1989375. PMID 34651536. S2CID 238990849. Archived from the original on 22 October 2021. Retrieved 20 February 2023.
- ^ Ramanlal R, Gupta V (2021). "Physiology, Vasodilation". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32491494. Archived from the original on 11 May 2021. Retrieved 22 September 2021.
- ^ a b Parimisetty A, Dorsemans AC, Awada R, Ravanan P, Diotel N, Lefebvre d'Hellencourt C (March 2016). "Secret talk between adipose tissue and central nervous system via secreted factors-an emerging frontier in the neurodegenerative research". Journal of Neuroinflammation (Review). 13 (1): 67. doi:10.1186/s12974-016-0530-x. PMC 4806498. PMID 27012931.
- ^ Kershaw EE, Flier JS (June 2004). "Adipose tissue as an endocrine organ". The Journal of Clinical Endocrinology and Metabolism. 89 (6): 2548–56. doi:10.1210/jc.2004-0395. PMID 15181022.
- ^ Bastard JP, Jardel C, Bruckert E, Blondy P, Capeau J, Laville M, et al. (September 2000). "Elevated levels of interleukin 6 are reduced in serum and subcutaneous adipose tissue of obese women after weight loss". The Journal of Clinical Endocrinology and Metabolism. 85 (9): 3338–42. doi:10.1210/jcem.85.9.6839. PMID 10999830.
- ^ Mohamed-Ali V, Flower L, Sethi J, Hotamisligil G, Gray R, Humphries SE, et al. (December 2001). "beta-Adrenergic regulation of IL-6 release from adipose tissue: in vivo and in vitro studies". The Journal of Clinical Endocrinology and Metabolism. 86 (12): 5864–9. doi:10.1210/jcem.86.12.8104. PMID 11739453. S2CID 73100391.
- ^ a b c d e f g Loffreda S, Yang SQ, Lin HZ, Karp CL, Brengman ML, Wang DJ, et al. (January 1998). "Leptin regulates proinflammatory immune responses". FASEB Journal. 12 (1): 57–65. doi:10.1096/fasebj.12.1.57. PMID 9438411.
- ^ a b c d e f g Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M, et al. (October 2002). "Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress". Circulation. 106 (16): 2067–72. doi:10.1161/01.CIR.0000034509.14906.AE. PMID 12379575.
- ^ Petersen AM, Pedersen BK (April 2005). "The anti-inflammatory effect of exercise". Journal of Applied Physiology. 98 (4): 1154–62. doi:10.1152/japplphysiol.00164.2004. PMID 15772055. S2CID 4776835.
- ^ Rogowski O, Shapira I, Bassat OK, Chundadze T, Finn T, Berliner S, et al. (July 2010). "Waist circumference as the predominant contributor to the micro-inflammatory response in the metabolic syndrome: a cross sectional study". Journal of Inflammation. 7: 35. doi:10.1186/1476-9255-7-35. PMC 2919526. PMID 20659330.
- ^ Goldfine AB, Shoelson SE (January 2017). "Therapeutic approaches targeting inflammation for diabetes and associated cardiovascular risk". The Journal of Clinical Investigation. 127 (1): 83–93. doi:10.1172/jci88884. PMC 5199685. PMID 28045401.
- ^ Choi J, Joseph L, Pilote L (March 2013). "Obesity and C-reactive protein in various populations: a systematic review and meta-analysis". Obesity Reviews. 14 (3): 232–44. doi:10.1111/obr.12003. PMID 23171381. S2CID 206227739.
External links
[edit]- Inflammation at the U.S. National Library of Medicine Medical Subject Headings (MeSH)



