Contact lens: Difference between revisions
| Line 1: | Line 1: | ||
{{Short description|Lenses placed on the eye's surface}} |
|||
{{redirect|Contacts|the software application|Address book}} |
|||
{{Use dmy dates|date=May 2016}} |
|||
[[Image:Contactlenzen Confortissimo.JPG||thumb|right|A pair of contact lenses, positioned with the concave side facing upward.]] |
|||
{{Redirect|Contacts|the software application|Contacts (Apple)}} |
|||
[[Image:ColorContactLens.JPG|thumb|right|One-day disposable blue color contact lens in packaging]] |
|||
{{Redirect|Monovision|the Ray LaMontagne album|Monovision (album)}} |
|||
{{Essay|date=July 2011}} |
|||
A '''contact lens''' (also known simply as a '''contact''') is a [[corrective lens|corrective]], [[cosmetics|cosmetic]], or therapeutic [[lens (optics)|lens]] usually placed on the [[cornea]] of the [[Human eye|eye]]. [[Leonardo da Vinci]] is credited with describing and sketching the first ideas for contact lenses in 1508, but it was more than 300 years later before contact lenses were actually fabricated and worn on the eye. Rigid ones were produced and marketed first.{{Citation needed|date=March 2011}} Modern soft contact lenses were invented by the [[Czech Republic|Czech]] [[chemist]] [[Otto Wichterle]] and his assistant [[Drahoslav Lím]], who also invented the first [[gel]] used for their production. {{Citation needed|date=March 2011}} |
|||
[[File:Contactlenzen Confortissimo.JPG|thumb|alt=See caption|A pair of contact lenses, positioned with the concave side facing upward]] |
|||
Some soft contact lenses are tinted a faint blue to make them more visible when immersed in cleaning and storage solutions. Some cosmetic lenses are deliberately colored to alter the appearance of the eye. Some lenses now have a UV protection surface treatment to reduce UV damage to the eye's natural lens.<ref>http://www.eurograduate.com/arch_article.asp?id=3054</ref> |
|||
[[File:ColorContactLens.JPG|thumb|alt=See caption|One-day [[disposable]] contact lenses with blue handling tint in blister-pack packaging]] |
|||
'''Contact lenses''', or simply '''contacts''', are thin [[lens (optics)|lenses]] placed directly on the surface of the [[Human eye|eyes]]. Contact lenses are ocular prosthetic devices used by over 150 million people worldwide,<ref>{{Cite journal |last=R Moreddu |last2=D Vigolo |last3=AK Yetisen |year=2019 |title=Contact Lens Technology: From fundamentals to Applications. |url=http://pure-oai.bham.ac.uk/ws/files/68302144/Contact_Lens_Technology_From_Fundamentals_to_Applications_1_.pdf |journal=Advanced Healthcare Materials |volume=8 |issue=15 |pages=1900368 |doi=10.1002/adhm.201900368 |pmid=31183972 |s2cid=184488183}}</ref> and they can be worn to [[corrective lens|correct vision]] or for [[cosmetics|cosmetic]] or therapeutic reasons.<ref>{{Cite journal |last=NM Farandos |last2=AK Yetisen |last3=MJ Monteiro |last4=CR Lowe |last5=SH Yun |year=2014 |title=Contact Lens Sensors in Ocular Diagnostics |journal=Advanced Healthcare Materials |volume=4 |issue=6 |pages=792–810 |doi=10.1002/adhm.201400504 |pmid=25400274 |s2cid=35508652}}</ref> In 2010, the worldwide market for contact lenses was estimated at $6.1 billion, while the US soft lens market was estimated at $2.1 billion.<ref name="Nichols">Nichols, Jason J., et al [http://www.clspectrum.com/article.aspx?article=105083 "ANNUAL REPORT: Contact Lenses 2010"]. January 2011.</ref> Multiple analysts estimated that the global market for contact lenses would reach $11.7 billion by 2015.<ref name="Nichols" /> {{As of|2010|post=,}} the average age of contact lens wearers globally was 31 years old, and two-thirds of wearers were female.<ref name="Morgan">Morgan, Philip B., et al. [http://www.clspectrum.com/article.aspx?article=105084 "International Contact Lens Prescribing in 2010"]. ''Contact Lens Spectrum''. October 2011.</ref> |
|||
It has been estimated that 125 million people use contact lenses worldwide (2%),<ref name="Barr">Barr, J. [http://www.clspectrum.com/article.aspx?article=12733 "2004 Annual Report"]. ''Contact Lens Spectrum''. January, 2005.</ref> including 28 to 38 million in the United States<ref name="Barr"/> and 13 million in Japan.<ref>National Consumer Affairs Center of Japan. [http://www.kokusen.go.jp/e-hello/data/ncac_news12_4.pdf NCAC News Vol. 12, No. 4]. ''NCAC News''. March, 2001.</ref> The types of lenses used and prescribed vary markedly among countries, with rigid lenses accounting for over 20% of currently-prescribed lenses in [[Japan]], [[Netherlands|the Netherlands]] and [[Germany]] but less than 5% in [[Scandinavia]].<ref name="Barr"/> |
|||
People choose to wear contact lenses for many reasons, |
People choose to wear contact lenses for many reasons.<ref>Agarwal, R. K. (1969), Contact Lens Notes, Some factors concerning patients' motivation, The Optician, 10 January, pages 32-33 (published in London, England).</ref> Aesthetics and cosmetics are main motivating factors for people who want to avoid wearing [[glasses]] or to change the appearance or color of their eyes.<ref>{{Cite journal |last=Sokol |first=JL |last2=Mier |first2=MG |last3=Bloom |first3=S |last4=Asbell |first4=PA |year=1990 |title=A study of patient compliance in a contact lens-wearing population |journal=CLAO Journal |volume=16 |issue=3 |pages=209–13 |pmid=2379308}}</ref> Others wear contact lenses for functional or optical reasons.<ref>{{Cite web |title=Compare Contacts & Glasses |url=https://www.en.acuvuearabia.com/why-contact-lenses/contact-lenses-vs-glasses |access-date=2021-11-22 |website=ACUVUE® Middle East |language=en}}</ref> When compared with spectacles, contact lenses typically provide better [[peripheral vision]], and do not collect moisture (from rain, snow, condensation, etc.) or perspiration. This can make them preferable for sports and other outdoor activities. Contact lens wearers can also wear sunglasses, goggles, or other eye wear of their choice without having to fit them with prescription lenses or worry about compatibility with glasses. Additionally, there are conditions such as [[keratoconus]] and [[aniseikonia]] that are typically corrected better with contact lenses than with glasses.<ref>{{Cite web |date=February 21, 2018 |title=Contact Lenses for Keratoconus |url=https://www.nkcf.org/keratoconus-contact-lenses/ |website=National Keratoconus Foundation}}</ref> |
||
==History== |
==History== |
||
[[Image:Adolf Fick.png|thumb|In 1888, Adolf Fick was the first to successfully fit contact lenses, which were made from blown glass]] |
|||
Leonardo Da Vinci is frequently credited with introducing the idea of contact lenses in his 1508 ''Codex of the eye, Manual D'', where he described a method of directly altering [[cornea]]l power by submerging the eye in a bowl of water. Leonardo, however, did not suggest his idea be used for correcting vision—he was more interested in learning about the mechanisms of [[accommodation (eye)|accommodation]] of the eye.<ref>Heitz, RF and Enoch, J. M. (1987) "Leonardo da Vinci: An assessment on his discourses on image formation in the eye." ''Advances in Diagnostic Visual Optics'' 19—26, Springer-Verlag.</ref> |
|||
===Origins and first functional prototypes=== |
|||
[[René Descartes]] proposed another idea in 1636, in which a glass tube filled with liquid is placed in direct contact with the cornea. The protruding end was to be composed of clear glass, shaped to correct vision; however the idea was impracticable, since it would make blinking impossible. |
|||
[[File:Da Vinci's method of corneal neutralization.jpg|thumb|left|alt=Illustration of a large lens covering a man's face|Artist's impression of [[Leonardo da Vinci|Leonardo's]] method for neutralizing the refractive power of the cornea]] |
|||
[[Leonardo da Vinci]] is frequently credited with introducing the idea of contact lenses in his 1508 ''Codex of the eye, Manual D'',<ref name="Heitz" /> wherein he described a method of directly altering [[cornea]]l power by either submerging the head in a bowl of water or wearing a water-filled glass hemisphere over the eye. Neither idea was practically implementable in da Vinci's time.<ref name="Schifrin" />{{rp|9}} He did not suggest his idea be used for correcting vision; he was more interested in exploring mechanisms of [[accommodation (eye)|accommodation]].<ref name="Heitz">Heitz, RF and Enoch, J. M. (1987) "Leonardo da Vinci: An assessment on his discourses on image formation in the eye." ''Advances in Diagnostic Visual Optics'' 19—26, Springer-Verlag.</ref> |
|||
In 1801, while conducting experiments concerning the mechanisms of accommodation, scientist [[Thomas Young (scientist)|Thomas Young]] constructed a liquid-filled "eyecup" which could be considered a predecessor to the contact lens. On the eyecup's base, Young fitted a microscope eyepiece. However, like Leonardo's, Young's device was not intended to correct refraction errors. |
|||
Sir [[John Herschel]], in a footnote of the 1845 edition of the ''[[Encyclopedia Metropolitana]]'', posed two ideas for the visual correction: the first "a spherical capsule of glass filled with [[gelatin|animal jelly]]", and "a mould of the cornea" which could be impressed on "some sort of transparent medium".<ref>[http://www.eyetopics.com/articles/18/1/The-History-of-Contact-Lenses "The History of Contact Lenses."] eyeTopics.com. Accessed October 18, 2006.</ref> Though Herschel reportedly never tested these ideas, they were both later advanced by several independent inventors such as Hungarian Dr. Dallos (1929), who perfected a method of making molds from living eyes. This enabled the manufacture of lenses that, for the first time, conformed to the actual shape of the eye. |
|||
[[René Descartes|Descartes]] proposed a device for correcting vision consisting of a liquid-filled glass tube capped with a [[lens]]. However, the idea was impracticable, since the device was to be placed in direct contact with the cornea and thus would have made [[blinking]] impossible.<ref name=":0">{{Cite journal |last=Moreddu |first=Rosalia |last2=Vigolo |first2=Daniele |last3=Yetisen |first3=Ali K. |date=August 2019 |title=Contact Lens Technology: From Fundamentals to Applications |url=http://pure-oai.bham.ac.uk/ws/files/68302144/Contact_Lens_Technology_From_Fundamentals_to_Applications_1_.pdf |journal=Advanced Healthcare Materials |volume=8 |issue=15 |pages=1900368 |doi=10.1002/adhm.201900368 |pmid=31183972 |s2cid=184488183}}</ref> |
|||
It was not until 1887 that a German glassblower, F.E. Muller, produced the first eye covering to be seen through and tolerated.<ref>[http://www.contactlenscouncil.org/scon-history.htm Contact Lens Council]</ref> In 1887, the German ophthalmologist [[Adolf Gaston Eugen Fick]] constructed and fitted the first successful contact lens. While working in [[Zürich]], he described fabricating [[Afocal system|afocal]] [[Scleral lens|scleral]] contact shells, which rested on the less sensitive rim of tissue around the cornea, and experimentally fitting them: initially on rabbits, then on himself, and lastly on a small group of volunteers. These lenses were made from heavy blown glass and were 18–21mm in diameter. Fick filled the empty space between cornea/callosity and glass with a dextrose solution. He published his work, "Contactbrille", in the [[scientific journal|journal]] ''Archiv für Augenheilkunde'' in March 1888. |
|||
In 1801, [[Thomas Young (scientist)|Thomas Young]] fashioned a pair of basic contact lenses based on Descartes' model. He used wax to affix water-filled lenses to his eyes, neutralizing their [[refractive power]], which he corrected with another pair of lenses.<ref name="Schifrin">{{Cite book |last=Leonard G. Schifrin |title=The Contact Lens Industry: Structure, Competition, and Public Policy |last2=William J. Rich |date=December 1984 |publisher=United States [[Office of Technology Assessment]]}}</ref><ref name=":0" /> |
|||
Fick's lens was large, unwieldy, and could only be worn for a couple of hours at a time. [[August Muller|August Müller]] in [[Kiel]], Germany, corrected his own severe myopia with a more convenient glass-blown scleral contact lens of his own manufacture in 1888.<ref>{{cite journal | pmid = 2686057 | year = 1989 | last1 = Pearson | first1 = RM | last2 = Efron | first2 = N | title = Hundredth anniversary of August Müller's inaugural dissertation on contact lenses | volume = 34 | issue = 2 | pages = 133–41 | journal = Survey of ophthalmology}}</ref> |
|||
[[John Herschel]], in a footnote to the 1845 edition of the ''[[Encyclopedia Metropolitana]]'', posed two ideas for the visual correction: the first "a spherical capsule of glass filled with [[gelatin|animal jelly]]",<ref name="SinhaDada2017">{{Cite book |last=Rajesh Sinha |url=https://books.google.com/books?id=Ax8LDgAAQBAJ&pg=PA2 |title=Textbook of Contact Lenses |last2=Vijay Kumar Dada |date=31 January 2017 |publisher=JP Medical Ltd |isbn=978-93-86150-44-8 |pages=2–}}</ref> the second "a mould of the cornea" that could be impressed on "some sort of transparent medium".<ref>[http://www.eyetopics.com/articles/18/1/The-History-of-Contact-Lenses "The History of Contact Lenses."] {{Webarchive|url=https://web.archive.org/web/20081011022433/http://www.eyetopics.com/articles/18/1/The-History-of-Contact-Lenses |date=11 October 2008 }} eyeTopics.com. Accessed 18 October 2006.</ref> Though Herschel reportedly never tested these ideas, they were later advanced by independent inventors, including Hungarian physician Joseph Dallos, who perfected a method of making molds from living eyes.<ref name="mastereyeassoc">{{Cite web |title=History of Contact Lenses and Improved Technology |url=https://www.mastereyeassociates.com/contact-lens-history |access-date=14 September 2019 |website=Master Eye Associates |ref=mastereyeassoc}}</ref> This enabled the manufacture of lenses that, for the first time, conformed to the actual shape of the eye.<ref>{{Cite book |title=Van Nostrand's Scientific Encyclopedia |year=2005 |isbn=0471743984 |chapter=Contact Lenses |doi=10.1002/0471743984.vse2040}}</ref> |
|||
Also in 1887, [[Louis J. Girard]] invented a similar scleral form of contact lens.<ref name="Timetables">{{The Timetables of Science|pages=367}}</ref> |
|||
Glass-blown scleral lenses remained the only form of contact lens until the 1930s when polymethyl methacrylate (PMMA or [[Polymethyl methacrylate|Perspex/Plexiglas]]) was developed, allowing plastic scleral lenses to be manufactured for the first time. In 1936, optometrist [[William Feinbloom]] introduced plastic lenses, making them lighter and more convenient.<ref>Robert B. Mandell. ''Contact Lens Practice'', 4th Edition. Charles C. Thomas, Springfield, IL, 1988.</ref> These lenses were a combination of glass and plastic. |
|||
[[File:Adolf Fick-adjust.png|thumb|upright|In 1888, [[Adolf Gaston Eugen Fick]] was the first to successfully fit contact lenses, which were made from blown glass]] |
|||
In 1949, the first "corneal" lenses were developed.<ref>U.S. Patent No. [http://www.google.com/patents?id=BoBuAAAAEBAJ 2,510,438], filed February 28, 1948.</ref><ref>"The Corneal Lens", ''The Optician'', September 2, 1949, pp. 141–144.</ref><ref>"Corneal Contact Lenses", ''The Optician'', September 9, 1949, p. 185.</ref><ref>"New Contact Lens Fits Pupil Only", ''[[The New York Times]]'', February 11, 1952, p. 27.</ref> These were much smaller than the original scleral lenses, as they sat only on the [[cornea]] rather than across all of the visible ocular surface, and could be worn up to sixteen hours per day. PMMA corneal lenses became the first contact lenses to have mass appeal through the 1960s, as lens designs became more sophisticated with improving manufacturing (lathe) technology. |
|||
Although [[Louis J. Girard]] invented a [[scleral contact lens]] in 1887,<ref name="Timetables">{{The Timetables of Science|pages=367}}</ref> it was German ophthalmologist [[Adolf Gaston Eugen Fick]] who in 1888 fabricated the first successful [[Afocal system|afocal]] scleral contact lens.<ref>{{Cite web |title=Adolf Eugen Fick (1852–1937) |url=http://www.sciencemuseum.org.uk/broughttolife/people/adolfeugenfick.aspx |url-status=dead |archive-url=https://web.archive.org/web/20150517070106/http://www.sciencemuseum.org.uk/broughttolife/people/adolfeugenfick.aspx |archive-date=17 May 2015 |access-date=26 March 2015}}</ref> Approximately {{convert|18–21|mm|abbr=on}} in diameter, the heavy [[Glassblowing|blown-glass]] shells rested on the less sensitive rim of tissue surrounding the cornea and floated on a [[dextrose]] solution. He experimented with fitting the lenses initially on rabbits, then on himself, and lastly on a small group of volunteers, publishing his work, ''"Contactbrille"'', in the March 1888 edition of ''Archiv für Augenheilkunde''.<ref>{{Cite journal |last=Heitz |first=R |date=September 2014 |title=The invention of the contact lenses (1888) |url=https://onlinelibrary.wiley.com/doi/10.1111/j.1755-3768.2014.3773.x |journal=Acta Ophthalmologica |language=en |volume=92 |issue=s253 |pages=0 |doi=10.1111/j.1755-3768.2014.3773.x |issn=1755-375X}}</ref> Large and unwieldy, Fick's lens could be worn only for a couple of hours at a time.<ref>{{Cite book |last=Sinha |first=Rajesh |url=https://www.worldcat.org/title/962009998 |title=Textbook of contact lenses |last2=Dada |first2=Vijay Kumar |date=2017 |publisher=Jaypee Brothers Medical Publishers (P) Ltd |isbn=978-93-86150-44-8 |edition=Fifth |location=New Delhi ; Philadelphia |oclc=962009998}}</ref> [[August Müller (inventor)|August Müller]] of [[Kiel]], Germany, corrected his own severe [[myopia]] with a more convenient blown-glass scleral contact lens of his own manufacture in 1888.<ref>{{Cite journal |last=Pearson |first=Richard M. |last2=Efron |first2=Nathan |date=September 1989 |title=Hundredth anniversary of August Müller's inaugural dissertation on contact lenses |journal=Survey of Ophthalmology |volume=34 |issue=2 |pages=133–141 |doi=10.1016/0039-6257(89)90041-6 |pmid=2686057}}</ref> |
|||
Early corneal lenses in the 1950s and 1960s were relatively expensive and fragile, resulting in the development of a market for contact lens [[insurance]]. Replacement Lens Insurance, Inc. (now known as [[RLI Corp.]]) phased out its original flagship product in 1994 after contacts became more affordable and easier to replace. |
|||
The development of [[polymethyl methacrylate]] (PMMA) in the 1930s paved the way for the manufacture of plastic scleral lenses. In 1936, optometrist [[William Feinbloom]] introduced a hybrid lens composed of glass and plastic,<ref>Robert B. Mandell. ''Contact Lens Practice'', 4th Edition. Charles C. Thomas, Springfield, IL, 1988</ref> and in 1937 it was reported that some 3,000 Americans were already wearing contact lenses.<ref>"Contact Lens for Eyes Now Common; It is Used as Substitute for Spectacles." Nashua (IA) Reporter, 28 April 1937.</ref> In 1939, Hungarian ophthalmologist Dr.István Györffy produced the first fully plastic contact lens.<ref>{{Cite journal |last=Gyorgy |first=Salacz |date=January 2001 |title=Dr István Györffy, 1912–1999 |journal=Contact Lens and Anterior Eye |volume=24 |issue=4 |pages=180–182 |doi=10.1016/S1367-0484(01)80040-0}}</ref> The following year, German optometrist [[Heinrich Wöhlk]] produced his own version of plastic lenses based on experiments performed during the 1930s.<ref>Contact Lens History: How Contact Lenses Have Developed Through the Years. EyeHealth Central. Retrieved from https://www.contactlenses.co.uk/education/history.htm</ref> |
|||
One important disadvantage of PMMA lenses is that no oxygen is transmitted through the lens to the conjunctiva and cornea, which can cause a number of adverse clinical effects. By the end of the 1970s, and through the 1980s and 1990s, a range of [[Oxygen permeability|oxygen-permeable]] but rigid materials were developed to overcome this problem. Chemist [[Norman Gaylord]] played a prominent role in the development of these newer, permeable contact lenses.<ref name=bc>{{cite web |url=http://www.boston.com/news/globe/obituaries/articles/2007/09/23/norman_gaylord_84_helped_develop_type_of_contact_lens/|title=Norman Gaylord, 84; helped develop type of contact lens|accessdate=2007-10-06 |author=Pearce, Jeremy|date=2007-09-23 |work=(New York Times News Service) |publisher=''[[The Boston Globe]]''}}</ref> Collectively, these [[polymers]] are referred to as "rigid gas permeable" or "RGP" materials or lenses. Although all the above lens types—sclerals, PMMA lenses and RGPs—could be correctly referred to as being "hard" or "rigid", the term hard is now used to refer to the original PMMA lenses which are still occasionally fitted and worn, whereas rigid is a generic term which can be used for all these lens types. That is, hard lenses (PMMA lenses) are a sub-set of rigid lenses. Occasionally, the term "gas permeable" is used to describe RGP lenses, but this is potentially misleading, as soft lenses are also gas permeable in that they allow oxygen to move through the lens to the ocular surface. |
|||
===Corneal and rigid lenses (1949–1960s)=== |
|||
The principal breakthrough in soft lenses was made by the [[Czechoslovakia|Czech]] chemists [[Otto Wichterle]] and [[Drahoslav Lim]] who published their work "Hydrophilic gels for biological use" in the journal ''Nature'' in 1959.<ref name="Wichterle">Wichterle O, Lim, D. "Hydrophilic gels for biological use". ''Nature''. 1960; 185:117–118.</ref> This led to the launch of the first soft (hydrogel) lenses in some countries in the 1960s and the first approval of the "Soflens" material by the United States [[Food and Drug Administration]] (FDA) in 1971. These lenses were soon prescribed more often than rigid lenses, mainly due to the immediate comfort of soft lenses; by comparison, rigid lenses require a period of adaptation before full comfort is achieved. The polymers from which soft lenses are manufactured improved over the next 25 years, primarily in terms of increasing the [[oxygen permeability]] by varying the ingredients. In 1972, British optometrist Rishi Agarwal was the first to suggest disposable soft contact lenses.<ref>Agarwal, Rishi K. (1972), Some Thoughts on Soft Lenses, The Contact Lens, volume 4, number 1, page 28.</ref><ref>Editorial note (1988), American Journal of Optometry and Physiological Optics, volume 65, number 9, page 744.</ref> |
|||
In 1949, the first "corneal" lenses were developed.<ref>U.S. Patent No. [https://patents.google.com/patent/US2510438 2,510,438], filed 28 February 1948.</ref><ref>"The Corneal Lens", ''The Optician'', 2 September 1949, pp. 141–144.</ref><ref>"Corneal Contact Lenses", ''The Optician'', 9 September 1949, p. 185.</ref><ref>"New Contact Lens Fits Pupil Only", ''[[The New York Times]]'', 11 February 1952, p. 27.</ref> These were much smaller than the original scleral lenses, as they sat only on the cornea rather than across all of the visible ocular surface and could be worn up to 16 hours a day. PMMA corneal lenses became the first contact lenses to have mass appeal through the 1960s, as lens designs became more sophisticated with improving manufacturing technology.<ref>{{Citation |last=Pal |first=Subrata |title=The Eye and Its Artificial Replacement |date=2014 |work=Design of Artificial Human Joints & Organs |pages=219–249 |url=http://link.springer.com/10.1007/978-1-4614-6255-2_14 |access-date=2024-08-29 |place=Boston, MA |publisher=Springer US |language=en |doi=10.1007/978-1-4614-6255-2_14 |isbn=978-1-4614-6254-5}}</ref> On October 18, 1964, in a television studio in Washington, D.C., [[Lyndon Baines Johnson]] became the first President in the history of the United States to appear in public wearing contact lenses, under the supervision of Dr. Alan Isen, who developed the first commercially viable soft-contact lenses in the United States.<ref>{{Cite book |last=Rosenthal |first=J. William |title=Spectacles and Other Vision Aids: A History and Guide to Collecting |date=1996 |publisher=Norman Publishing |isbn=978-0930405717 |page=379}}</ref><ref>{{Cite news |last=Smith |first=William D. |date=18 April 1971 |title=Soft-Lens Clamor |url=https://www.nytimes.com/1971/04/18/archives/softlens-clamor-tiny-piece-of-plastic-attracts-wall-street-interest.html |access-date=29 November 2018 |work=The New York Times}}</ref><ref>{{Cite news |date=December 6, 1964 |title=nytimes archive |url=https://www.nytimes.com/1964/12/06/archives/but-they-make-marriage-contracts-with-girls-who-wear-contacts.html |access-date=2018-08-24 |work=[[The New York Times]]}}</ref> |
|||
In 1998, an important development was the launch of the first silicone hydrogels onto the market by CIBA VISION (now Alcon) in Mexico. These new materials encapsulated the benefits of silicone—which has extremely high [[oxygen permeability]]—with the comfort and clinical performance of the conventional hydrogels which had been used for the previous 30 years. These lenses were initially advocated primarily for extended (overnight) wear although more recently, daily (no overnight) wear silicone hydrogels have been launched. |
|||
Early corneal lenses of the 1950s and 1960s were relatively expensive and fragile, resulting in the development of a market for contact lens insurance. Replacement Lens Insurance, Inc. (now known as [[RLI Corp.]]) phased out its original flagship product in 1994 after contact lenses became more affordable and easier to replace.{{Citation needed|date=June 2017}} |
|||
In a slightly modified molecule, a polar group is added without changing the structure of the silicone hydrogel. This is referred to as the Tanaka monomer because it was invented and patented by [[Kyoichi Tanaka]] of Menicon Co. of Japan in 1979. Second-generation silicone hydrogels, such as galyfilcon A (Acuvue Advance, Vistakon) and senofilcon A (Acuvue Oasys, Vistakon), use the Tanaka monomer. Vistakon improved the Tanaka monomer even further and added other molecules, which serve as an internal wetting agent.<ref name="Szczotka-Flynn">{{Cite web|work=Optometric Management |title=Looking at Silicone Hydrogels Across Generations |url=http://www.optometric.com/article.aspx?article=101727 |accessdate=April 5, 2009}}</ref> |
|||
===Gas permeable and soft lenses (1959–present)=== |
|||
Comfilcon A (Biofinity, CooperVision) was the first third-generation polymer. The patent claims that the material uses two siloxy macromers of different sizes that, when used in combination, produce very high oxygen permeability (for a given water content). Enfilcon A (Avaira, CooperVision) is another third-generation material that's naturally wettable. The enfilcon A material is 46% water.<ref name="Szczotka-Flynn"/> |
|||
One of the major disadvantages of PMMA lenses is that they allow no oxygen to get through to the [[conjunctiva]] and cornea, causing a number of adverse and potentially serious clinical effects. By the end of the 1970s and through the 1980s and 1990s, a range of [[Oxygen permeability|oxygen-permeable]] but rigid materials were developed to overcome this problem. Chemist [[Norman Gaylord]] played a prominent role in the development of these new oxygen-permeable contact lenses.<ref name="bc">{{Cite web |last=Pearce, Jeremy |date=23 September 2007 |title=Norman Gaylord, 84; helped develop type of contact lens |url=http://www.boston.com/news/globe/obituaries/articles/2007/09/23/norman_gaylord_84_helped_develop_type_of_contact_lens/ |access-date=6 October 2007 |website=(New York Times News Service) |publisher=[[The Boston Globe]]}}</ref> Collectively, these [[polymers]] are referred to as ''[[RGP lens|rigid gas permeable]]'' or RGP materials or lenses. Though all the above contact lens types—sclerals, PMMAs and RGPs—could be correctly referred to as "rigid" or "hard", the latter term is now used for the original PMMAs, which are still occasionally fitted and worn, whereas "rigid" is a generic term for all these lens types; thus, hard lenses (PMMAs) are a subset of rigid contact lenses. Occasionally, the term "gas permeable" is used to describe RGPs, which is somewhat misleading as soft contact lenses are also gas permeable in that they allow oxygen to get through to the ocular surface. |
|||
==Types of contact lenses== |
|||
Contact lenses are classified in many different manners.<ref>[http://www.pasadenaeye.com/faq/faq14/faq14_text.html "What are the types of contact lenses?"]</ref><ref>[http://www.capioeye.co.uk/eyeinfo/contacts/types/index.html "Different types of contact lenses."]</ref> |
|||
[[File:Prof. Ing. RTDr. Otto Wichterle.jpg|thumb|upright|[[Otto Wichterle]] (pictured) and [[Drahoslav Lím]] introduced modern soft hydrogel lenses in 1959.]] |
|||
The principal breakthrough in soft lenses was made by Czech chemists [[Otto Wichterle]] and [[Drahoslav Lím]], who published their work "Hydrophilic gels for biological use" in the journal ''Nature'' in 1959.<ref name="Wichterle">{{Cite journal |vauthors=Wichterle O, Lim D |year=1960 |title=Hydrophilic gels for biological use |journal=Nature |volume=185 |issue=4706 |pages=117–118 |bibcode=1960Natur.185..117W |doi=10.1038/185117a0 |s2cid=4211987}}</ref> In 1965, [[National Patent Development Corporation]] (NPDC) bought the American rights to produce the lenses and then sublicensed the rights to [[Bausch & Lomb]], which started to manufacture them in the United States.<ref>{{Cite web |title=CONTACT LENS HISTORY – Otto Wichterle |url=http://www.andrewgasson.co.uk/opioneers_wichterle.htm |url-status=dead |archive-url=https://web.archive.org/web/20150129033858/http://www.andrewgasson.co.uk/opioneers_wichterle.htm |archive-date=29 January 2015 |access-date=26 March 2015 |df=dmy-all}}</ref> The Czech scientists' work led to the launch of the first [[hydrogel]] contact lenses in some countries in the 1960s and the first approval of the Soflens material by the US [[Food and Drug Administration]] (FDA) in 1971. These soft lenses were soon prescribed more often than rigid ones, due to the immediate and much greater comfort (rigid lenses require a period of adaptation before full comfort is achieved). Polymers from which soft lenses are manufactured improved over the next 25 years, primarily in terms of increasing oxygen permeability, by varying the ingredients. In 1972, British optometrist Rishi Agarwal was the first to suggest disposable soft contact lenses.<ref>{{Cite journal |last=Agarwal Rishi K |year=1972 |title=Some Thoughts on Soft Lenses |journal=The Contact Lens |volume=4 |issue=1 |page=28}}</ref><ref>{{Cite journal |year=1988 |title=Editorial note |journal=American Journal of Optometry and Physiological Optics |volume=65 |issue=9 |page=744}}</ref> |
|||
In 1998, the first silicone hydrogel contact lenses were released by [[Ciba Vision]] in Mexico. These new materials encapsulated the benefits of silicone which has extremely high [[oxygen permeability]]—with the comfort and clinical performance of the conventional hydrogels that had been used for the previous 30 years. These contact lenses were initially advocated primarily for extended (overnight) wear, although more recently, daily (no overnight) wear silicone hydrogels have been launched. |
|||
In a slightly modified molecule, a polar group is added without changing the structure of the silicone hydrogel. This is referred to as the Tanaka monomer because it was invented and patented by {{ill|Kyoichi Tanaka|ja|田中恭一}} of {{ill|Menicon|ja|メニコン}} Co. of Japan in 1979. Second-generation silicone hydrogels, such as [[galyfilcon A]] ([[Acuvue]] Advance, Vistakon) and [[senofilcon A]] (Acuvue Oasys, Vistakon), use the Tanaka monomer. Vistakon improved the Tanaka monomer even further and added other molecules, which serve as an internal [[wetting agent]].<ref name="szcz" /> |
|||
[[Comfilcon A]] (Biofinity, CooperVision) was the first third-generation polymer. Its patent claims that the material uses two siloxy macromers of diverse sizes that, when used in combination, produce very high oxygen permeability for a given water content. [[Enfilcon A]] (Avaira, CooperVision) is another third-generation material that is naturally wet; its water content is 46%.<ref name="szcz" /> |
|||
==Types== |
|||
Contact lenses are classified in diverse ways, namely, by their primary function, material, wear schedule (how long a lens can be worn), and replacement schedule (how long before a lens needs to be discarded). |
|||
===Functions=== |
===Functions=== |
||
====Corrective contact lenses==== |
|||
Corrective contact lenses are designed to improve vision. For many people, there is a mismatch between the refractive power of the eye and the length of the eye, leading to a [[refraction error]]. A contact lens neutralizes this mismatch and allows for correct focusing of light onto the [[retina]]. Conditions correctable with contact lenses include [[myopia]] (near or short sightedness), [[hypermetropia]] (far or long sightedness), [[Astigmatism (eye)|astigmatism]] and [[presbyopia]]. Contact wearers must usually take their contact lenses out every night or every few days, depending on the brand and style of the contact. Recently, there has been renewed interest in [[orthokeratology]], the correction of [[myopia]] by deliberate overnight flattening of the cornea, leaving the eye without contact lens or eyeglasses correction during the day. |
|||
====Correction of refractive error==== |
|||
For those with certain [[color blindness|color deficiencies]], a red-tinted "X-Chrom" contact lens may be used. Although the lens does not restore normal [[color vision]], it allows some colorblind individuals to distinguish colors better.<ref>{{cite journal | pmid = 9314196 | year = 1997 | last1 = Hartenbaum | first1 = NP | last2 = Stack | first2 = CM | title = Color vision deficiency and the X-Chrom lens | volume = 66 | issue = 9 | pages = 36–40, 42 | journal = Occupational health & safety (Waco, Tex.)}}</ref><ref>{{cite journal | pmid = 6971497 | year = 1981 | last1 = Siegel | first1 = IM | title = The X-Chrom lens. On seeing red | volume = 25 | issue = 5 | pages = 312–24 | journal = Survey of ophthalmology}}</ref> |
|||
[[Corrective lens|Corrective]] contact lenses are designed to improve vision, most commonly by correcting [[refractive error]]. This is done by directly focusing light so it enters the eye with the proper [[Dioptre|power]] for clear vision. |
|||
A spherical contact lens bends light evenly in every direction (horizontally, vertically, etc.). They are typically used to correct [[myopia]] and [[hypermetropia]]. |
|||
There are two ways that contact lenses can correct astigmatism. One way is with [[toric lens|toric]] soft lenses that work essentially the same way as eyeglasses with cylindrical correction; a toric lens has a different focusing power horizontally than vertically, and as a result can correct for [[astigmatism]]. Another way is by using a rigid gas permeable lens; since most astigmatism is caused by the shape of the cornea, rigid lenses can improve vision because the front surface of the optical system is the perfectly spherical lens.<ref>{{Cite web |title=Astigmatism |url=http://www.aoa.org/Astigmatism.xml,%20http://www.aoa.org/Astigmatism.xml |access-date=2020-08-06 |website=www.aoa.org |language=en}}{{Dead link|date=December 2023 |bot=InternetArchiveBot |fix-attempted=yes }}</ref> Both approaches have advantages and drawbacks. Toric lenses must have the proper orientation to correct for astigmatism, so such lenses must have additional design characteristics to prevent them from rotating out of alignment. This can be done by weighting the bottom of the lens or by using other physical characteristics to rotate the lens back into position, but these mechanisms rarely work perfectly, so some misalignment is common and results in somewhat imperfect correction, and blurring of sight after blinking rotates the lens. Toric soft lenses have all the advantages of soft lenses in general, which are low initial cost, ease of fitting, and minimal adjustment period. Rigid gas permeable lenses usually provide superior optical correction but have become less popular relative to soft lenses due to higher initial costs, longer initial adjustment period, and more involved fitting.<ref>{{Cite web |title=Advantages and Disadvantages of Various Types of Contact Lenses |url=https://www.aoa.org/patients-and-public/caring-for-your-vision/contact-lenses/advantages-and-disadvantages-of-various-types-of-contact-lenses |access-date=2020-08-06 |website=www.aoa.org |language=en}}</ref><ref>{{Cite web |date=2013-01-26 |title=A Complete Guide to Gas Permeable Contact Lenses |url=https://www.eyehealthweb.com/rigid-gas-permeable-lenses/ |access-date=2020-08-06 |website=EyeHealthWeb.com |language=en}}</ref> |
|||
====Correction of presbyopia==== |
|||
Correction of [[presbyopia]] (a need for a reading prescription different from the prescription needed for distance) presents an additional challenge in the fitting of contact lenses. Two main strategies exist: multifocal lenses and monovision. |
|||
Multifocal contact lenses (e.g. bifocals or progressives) are comparable to spectacles with [[bifocals]] or [[progressive lens]]es because they have multiple [[focus (optics)|focal points]]. Multifocal contact lenses are typically designed for constant viewing through the center of the lens, but some designs do incorporate a shift in lens position to view through the reading power (similar to bifocal glasses). |
|||
Monovision<ref>{{Cite journal |last=Lebow |first=KA |last2=Goldberg |first2=JB |year=1975 |title=Characteristic of binocular vision found for presbyopic patients wearing single vision contact lenses |journal=Journal of the American Optometric Association |volume=46 |issue=11 |pages=1116–23 |pmid=802938}}</ref> is the use of single-vision lenses (one focal point per lens) to focus an eye (typically the dominant one) for distance vision and the other for near work. The brain then learns to use this setup to see clearly at all distances. A technique called modified monovision uses multifocal lenses and also specializes one eye for distance and the other for near, thus gaining the benefits of both systems. Care is advised for persons with a previous history of [[strabismus]] and those with significant phorias, who are at risk of eye misalignment under monovision.<ref>{{Cite journal |last=Pollard |first=Zane F. |last2=Greenberg |first2=Marc F. |last3=Bordenca |first3=Mark |last4=Elliott |first4=Joshua |last5=Hsu |first5=Victoria |date=September 2011 |title=Strabismus Precipitated by Monovision |journal=American Journal of Ophthalmology |volume=152 |issue=3 |pages=479–482.e1 |doi=10.1016/j.ajo.2011.02.008 |pmid=21669405}}</ref> Studies have shown no adverse effect to driving performance in adapted monovision contact lens wearers.<ref>{{Cite journal |last=Wood |first=Joanne M. |last2=Wick |first2=Kristan |last3=Shuley |first3=Vicki |last4=Pearce |first4=Brendon |last5=Evans |first5=Dean |date=6 May 1998 |title=The effect of monovision contact lens wear on driving performance |journal=Clinical and Experimental Optometry |volume=81 |issue=3 |pages=100–103 |doi=10.1111/j.1444-0938.1998.tb06727.x |pmid=12482258 |s2cid=38392636}}</ref> |
|||
Alternatively, a person may simply wear reading glasses over their distance contact lenses. |
|||
====Other types of vision correction==== |
|||
For those with certain [[color blindness|color deficiencies]], a red-tinted "X-Chrom" contact lens may be used. Although such a lens does not restore normal [[color vision]], it allows some color-blind people to distinguish colors better.<ref>{{Cite journal |last=Hartenbaum |first=NP |last2=Stack |first2=CM |year=1997 |title=Color vision deficiency and the X-Chrom lens |journal=Occupational Health & Safety |volume=66 |issue=9 |pages=36–40, 42 |pmid=9314196}}</ref><ref>{{Cite journal |last=Siegel |first=IM |year=1981 |title=The X-Chrom lens. On seeing red |journal=Survey of Ophthalmology |volume=25 |issue=5 |pages=312–24 |doi=10.1016/S0039-6257(81)80001-X |pmid=6971497}}</ref> Red-filtering contact lenses can also be an option for extreme light sensitivity in some visual deficiencies such as [[achromatopsia]].<ref>http://www.achromatopsia.info/red-contact-lenses/ Red contact lenses for achromats</ref> |
|||
ChromaGen contact lenses have been used and shown to have some limitations with vision at night although otherwise producing significant improvements in color vision.<ref>{{Cite journal |last=Swarbrick |first=HA |last2=Nguyen |first2=P |last3=Nguyen |first3=T |last4=Pham |first4=P |year=2001 |title=The ChromaGen contact lens system: Colour vision test results and subjective responses |journal=Ophthalmic & Physiological Optics |volume=21 |issue=3 |pages=182–96 |doi=10.1046/j.1475-1313.2001.00583.x |pmid=11396392 |s2cid=40409461}}</ref> An earlier study showed very significant improvements in color vision and patient satisfaction.<ref>Harris D "Colouring Sight: A study of CL fittings with colour enhancing lenses" 'Optician' 8 June 1997</ref> |
|||
Later work that used these ChromaGen lenses with [[Dyslexia|people with dyslexia]] in a randomised, double-blind, placebo-controlled trial showed highly significant{{Clarify|reason=vague|date=June 2017}} improvements in reading ability over reading without the lenses.<ref>Harris DA, MacRow-Hill SJ "Application of ChromaGen haploscopic lenses to patients with dyslexia: a double masked placebo controlled trial" Journal of the American Optometric Association 25/10/99.</ref> This system has been granted FDA approval for use in the United States.<ref>{{Cite press release |title=Cision - FDA Cleared ChromaGen Lenses |url=https://www.prnewswire.com/news-releases/fda-cleared-chromagen-lenses-are-a-life-changing-aid-for-people-struggling-with-dyslexia-and-other-reading-problems-200289391.html |url-status=live |archive-url=https://web.archive.org/web/20130703043949/http://www.prnewswire.com/news-releases/fda-cleared-chromagen-lenses-are-a-life-changing-aid-for-people-struggling-with-dyslexia-and-other-reading-problems-200289391.html |archive-date=3 July 2013}}</ref> |
|||
ChromaGen lenses have been used and these have been shown to have some limitations with vision at night although otherwise producing significant improvements in color vision.<ref>{{cite journal | pmid = 11396392 | year = 2001 | last1 = Swarbrick | first1 = HA | last2 = Nguyen | first2 = P | last3 = Nguyen | first3 = T | last4 = Pham | first4 = P | title = The ChromaGen contact lens system: Colour vision test results and subjective responses | volume = 21 | issue = 3 | pages = 182–96 | journal = Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists)}}</ref> An earlier study showed very significant improvements in color vision and patient satisfaction.<ref>Harris D “Colouring Sight: A study of CL fittings with colour enhancing lenses” 'Optician' 8 June 1997</ref> |
|||
[[Magnification]] is another area being researched for future contact lens applications.<ref>{{Cite magazine |title=Telescopic contact lens magnifies vision by 2.8 times on demand |url=https://www.wired.co.uk/news/archive/2013-07/24/magnifying-contact-lenses |url-status=dead |archive-url=https://web.archive.org/web/20150402151345/http://www.wired.co.uk/news/archive/2013-07/24/magnifying-contact-lenses |archive-date=2 April 2015 |access-date=26 March 2015 |magazine=Wired UK}}</ref> Embedding of telescopic lenses and electronic components suggests that future uses of contact lenses may become extremely diverse. |
|||
Later work that used these ChromaGen lenses with [[Dyslexia|dyslexics]] in a randomised, double-blind, placebo controlled trial showed highly significant improvements in reading ability over reading without the lenses<ref>Harris DA, MacRow-Hill SJ “Application of ChromaGen haploscopic lenses to patients with dyslexia: a double masked placebo controlled trial” Journal of the American Optometric Association 25/10/99.</ref> This system has been granted FDA approval in the USA. |
|||
====Cosmetic contact lenses==== |
====Cosmetic contact lenses==== |
||
[[File:Contact Grain.jpg |
[[File:Contact Grain.jpg|thumb|Woman wearing a cosmetic type of contact lens; enlarged detail shows the grain produced during the manufacturing process. Curving of the lines of printed dots suggests these lenses were manufactured by printing onto a flat sheet then shaping it.]] |
||
A cosmetic contact lens is designed to change the appearance of the eye. These lenses may also correct the vision, but some blurring or obstruction of vision may occur as a result of the color or design. In the USA, the [[U.S. Food and Drug Administration|Food and Drug Administration]] frequently calls non-corrective cosmetic contact lenses ''decorative contact lenses''. These types of lenses tend to cause mild irritation on insertion, but after accustoming to the lenses, the eyes are typically well tolerated. As with any contact lens, cosmetic lenses carry risks of mild and serious complications, including ocular redness, irritation, and infection. All individuals who decide to wear cosmetic lenses should check with an eye care provider prior to first use, and periodically over long term use in order to avoid potentially blinding complications. |
|||
A cosmetic contact lens is designed to change the appearance of the eye. These lenses may also correct [[refractive error]]. Although many brands of contact lenses are lightly tinted to make them easier to handle, cosmetic lenses worn to change eye color are far less common, accounting for only 3% of contact lens fits in 2004.<ref>Morgan PB et al.[http://www.clspectrum.com/article.aspx?article=12741 "International Contact Lens Prescribing in 2004: An analysis of more than 17,000 contact lens fits from 14 countries in 2004 reveals the diversity of contact lens practice worldwide."] ''Contact Lens Spectrum.'' January 2005.</ref> |
|||
Theatrical contact lenses are a type of cosmetic contact lens that are used primarily in the [[entertainment industry]] to make the eye appear confusing and arousing in appearance,{{Citation needed|date=February 2010}} most often in horror film and [[zombie]] movies, where lenses can make one's eyes appear demonic, cloudy and lifeless, or even to make the pupils of the wearer appear dilated to simulate the natural appearance of the pupils under the influence of various illicit drugs. |
|||
In the United States, the FDA labels non-corrective cosmetic contact lenses as ''decorative contact lenses''. Like any contact lens, cosmetic lenses carry risks of mild to serious complications, including ocular redness, irritation and infection.<ref>[http://www.mc.vanderbilt.edu/news/releases.php?release=1670 Vanderbilt University Medical Center – Vanderbilt Eye Doctors Warn of the Dangers of Cosmetic Contact Lenses]. Mc.vanderbilt.edu (19 April 2010). Retrieved on 2013-07-21.</ref> |
|||
[[Scleral lens]]es cover the white part of the eye (i.e. [[sclera]]) and are used in many theatrical lenses. Due to their size, these lenses are difficult to insert and do not move very well within the eye. They may also hamper the vision as the lens has a small area for the user to see through. As a result they generally cannot be worn for more than 3 hours as they can cause temporary vision disturbances.<ref>[http://www.eyecontactguide.com/about_theatrical_contact_lenses.htm "A Guide to Theatrical Contact Lenses"] eyecontactguide.com Accessed 31 December 2006</ref> |
|||
Due to their medical nature, colored contact lenses, similar to regular ones, are illegal to purchase in the United States without a valid prescription. Those with perfect vision can buy color contacts for cosmetic reasons, but they still need their eyes to be measured for a "plano" prescription, meaning one with zero vision correction. This is for safety reasons so the lenses will fit the eye without causing irritation or redness. |
|||
Similar lenses have more direct medical applications. For example, some lenses can give the [[Iris (anatomy)|iris]] an enlarged appearance, or mask defects such as absence of ([[aniridia]]) or damage to ([[dyscoria]]) the iris. |
|||
Some colored contact lenses completely cover the iris, thus dramatically changing eye color. Other colored contact lenses merely tint the iris, highlighting its natural color. A new trend in Japan, South Korea and China is the [[circle contact lens]], which extend the appearance of the iris onto the sclera by having a dark tinted area all around. The result is an appearance of a bigger, wider iris, a look reminiscent of dolls' eyes.<ref>{{Cite web |title=How Do You Find the Right Circle Lens? |url=http://www.eyecandys.com/news/finding-the-right-circle-lenses |url-status=dead |archive-url=https://web.archive.org/web/20131213060734/http://www.eyecandys.com/news/finding-the-right-circle-lenses |archive-date=13 December 2013 |access-date=26 March 2015 |website=EyeCandy's}}</ref> |
|||
A new trend in Japan, South Korea and China is the [[circle contact lens]]. Circle lenses appear to be bigger because they are not only tinted in areas that cover the iris of the eye, but tinted prominently in the extra-wide outer ring of the lens. The result is the appearance of a bigger, wider iris. |
|||
Cosmetic lenses can have more direct medical applications. For example, some contact lenses can restore the appearance and, to some extent the function, of a damaged or [[aniridia|missing]] [[Iris (anatomy)|iris]]. |
|||
Although many brands of contact lenses are lightly tinted to make them easier to handle, cosmetic lenses worn to change the color of the eye are far less common, accounting for only 3% of contact lens fits in 2004.<ref>Morgan PB et al.[http://www.clspectrum.com/article.aspx?article=12741 "International Contact Lens Prescribing in 2004: An analysis of more than 17,000 contact lens fits from 14 countries in 2004 reveals the diversity of contact lens practice worldwide."] ''Contact Lens Spectrum.'' January 2005.</ref> |
|||
====Therapeutic scleral lenses==== |
|||
As a specialist's tool, in the hands of the untrained general public, non-prescription cosmetic contact lenses may represent a health risk.<ref>http://www.mc.vanderbilt.edu/news/releases.php?release=1670</ref> |
|||
[[File:Scleral lens worn on an eye.jpg|thumb|upright|alt=See caption|[[Scleral lens]], with visible outer edge resting on the sclera of a patient with severe [[dry eye syndrome]] ]] |
|||
A [[scleral lens]] is a large, firm, transparent, oxygen-permeable contact lens that rests on the sclera and creates a tear-filled vault over the cornea. The cause of this unique positioning is usually relevant to a specific patient whose cornea is too sensitive to support the lens directly. Scleral lenses may be used to improve vision and reduce pain and light sensitivity for people with disorders or injuries to the eye, such as severe [[dry eye syndrome]] (keratoconjunctivitis sicca), [[microphthalmia]], [[keratoconus]], [[corneal ectasia]], [[Stevens–Johnson syndrome]], [[Sjögren's syndrome]], [[aniridia]], neurotrophic keratitis (anesthetic corneas), complications post-LASIK, high order [[aberrations of the eye]], complications post-corneal transplant and [[Pellucid marginal degeneration|pellucid degeneration]]. Injuries to the eye such as surgical complications, distorted corneal implants, as well as chemical and burn injuries also may be treated with scleral lenses.<ref>{{Cite journal |last=Caceres |first=Vanessa |date=June 2009 |title=Taking a second look at scleral lenses |url=http://www.eyeworld.org/article-taking-a-second-look-at-scleral-lenses |url-status=dead |journal=ASCRS EyeWorld |archive-url=https://web.archive.org/web/20190228004334/https://www.eyeworld.org/article-taking-a-second-look-at-scleral-lenses |archive-date=28 February 2019 |access-date=18 May 2014}}</ref> |
|||
====Therapeutic contact lenses==== |
|||
Soft lenses are often used in the treatment and management of non-refractive disorders of the eye. A bandage contact lens protects an injured or diseased cornea from the constant rubbing of blinking eyelids thereby allowing it to heal.<ref>[http://eyemdlink.com/terminology/bandage_contact_lens.htm EyeMDLink.com]</ref> They are used in the treatment of conditions including [[bullous keratopathy]], [[Keratoconjunctivitis sicca|dry eyes]], [[corneal abrasion|corneal ulcers]] and [[recurrent corneal erosion|erosion]], [[keratitis]], corneal [[edema]], [[descemetocele]], corneal ectasis, [[Mooren's ulcer]], anterior corneal dystrophy, and neurotrophic keratoconjunctivitis.<ref>{{cite web | url=http://new.cms.hhs.gov/manuals/downloads/Pub06_PART_45.pdf | title=45 COVERAGE ISSUES – SUPPLIES – DRUGS 11–91 45 | format=PDF | publisher=[[Centers for Medicare and Medicaid Services]] | accessdate=2006-03-01}}</ref> Contact lenses that deliver drugs to the eye have also been developed.<ref>[http://www.devicelink.com/mddi/archive/05/01/011.html "Contact Lenses Employed for Drug Delivery."]</ref> |
|||
====Therapeutic soft lenses==== |
|||
Soft lenses are often used in the treatment and management of non-refractive disorders of the eye. A bandage contact lens allows the patient to see<ref>{{Cite journal |last=Alvarez-Lorenzo |first=Carmen |last2=Anguiano-Igea |first2=Soledad |last3=Varela-García |first3=Angela |last4=Vivero-Lopez |first4=María |last5=Concheiro |first5=Angel |date=January 2019 |title=Bioinspired hydrogels for drug-eluting contact lenses |journal=Acta Biomaterialia |volume=84 |pages=49–62 |doi=10.1016/j.actbio.2018.11.020 |pmid=30448434 |s2cid=53780024}}</ref> while protecting an injured or diseased cornea<ref>{{Cite journal |last=Zidan |first=Ghada |last2=Rupenthal |first2=Ilva D. |last3=Greene |first3=Carol |last4=Seyfoddin |first4=Ali |date=2018 |title=Medicated ocular bandages and corneal health: potential excipients and active pharmaceutical ingredients |journal=Pharmaceutical Development and Technology |volume=23 |issue=3 |pages=255–260 |doi=10.1080/10837450.2017.1377232 |pmid=28875742 |s2cid=32765975}}</ref> from the constant rubbing of blinking eyelids, thereby allowing it to heal.<ref>{{Cite web |title=Eye Health Guide – Eye Diseases, Eye Problems and Eye Conditions |url=http://eyemdlink.com/terminology/bandage_contact_lens.htm |url-status=dead |archive-url=https://web.archive.org/web/20080409214021/http://eyemdlink.com/terminology/bandage_contact_lens.htm |archive-date=9 April 2008 |access-date=26 March 2015 |website=All About Vision}}</ref> They are used in the treatment of conditions including [[bullous keratopathy]], [[Keratoconjunctivitis sicca|dry eyes]], [[corneal abrasion]]s and [[recurrent corneal erosion|erosion]], [[keratitis]], corneal [[edema]], [[descemetocele]], [[corneal ectasia]], [[Mooren's ulcer]], anterior corneal dystrophy, and neurotrophic keratoconjunctivitis.<ref>{{Cite web |title=45 COVERAGE ISSUES – SUPPLIES – DRUGS 11–91 45 |url=http://new.cms.hhs.gov/manuals/downloads/Pub06_PART_45.pdf |url-status=dead |archive-url=https://web.archive.org/web/20060304101146/http://new.cms.hhs.gov/manuals/downloads/Pub06_PART_45.pdf |archive-date=4 March 2006 |access-date=1 March 2006 |publisher=[[Centers for Medicare and Medicaid Services]] |df=dmy-all}}</ref> Contact lenses that deliver drugs to the eye have also been developed.<ref>{{Cite web |title=Qmed is the world's only directory of pre-qualified suppliers to the medical device and in vitro diagnostics industry. - Qmed |url=http://www.devicelink.com/mddi/archive/05/01/011.html |url-status=dead |archive-url=https://web.archive.org/web/20081205140248/http://www.devicelink.com/mddi/archive/05/01/011.html |archive-date=5 December 2008 |access-date=26 March 2015}}</ref> |
|||
===Materials=== |
===Materials=== |
||
[[ |
[[File:Eye with contact lens.jpg|thumb|alt=Closeup of the eye, showing the light tint on the rim of a corrective contact lense|Non-cosmetic contact lenses become almost invisible once inserted in the eye. Most corrective contact lenses come with a light "handling tint" that renders the it slightly more visible on the eye, sometimes visible against the [[sclera]].]] |
||
====Rigid lenses==== |
|||
The first contact lenses were made of [[glass]], which caused eye irritation, and were not wearable for extended periods of time. But when [[William Feinbloom]] introduced lenses made from [[polymethyl methacrylate]] (PMMA or [[Polymethyl methacrylate|Perspex/Plexiglas]]), contact lenses became much more convenient. These PMMA lenses are commonly referred to as "hard" lenses (this term is not used for other types of contact lens). |
|||
Glass lenses were never comfortable enough to gain widespread popularity. The first lenses to do so were those made from [[polymethyl methacrylate]] (PMMA or Perspex/Plexiglas), now commonly referred to as "hard" lenses. Their main disadvantage is they do not allow [[oxygen]] to pass through to the [[cornea]], which can cause a number of adverse, and often serious, clinical events. Starting in the late 1970s, improved rigid materials which were [[Oxygen permeability|oxygen-permeable]] were developed. Contact lenses made from these materials are called [[rigid gas permeable]] lenses (RGPs). |
|||
A rigid lens is able to cover the natural shape of the [[cornea]] with a new refracting surface. This means that a spherical rigid contact lens can correct corneal astigmatism. Rigid lenses can also be made as a front-toric, back-toric, or bitoric. Rigid lenses can also correct corneas with irregular geometries, such as those with [[keratoconus]] or post surgical [[Post-LASIK ectasia|ectasias]]. In most cases, patients with keratoconus see better through rigid lenses than through [[eyeglasses|glasses]]. Rigid lenses are more chemically inert, allowing them to be worn in more challenging environments where chemical inertia is important compared to soft lenses.<ref>{{Cite web |title=Rigid contact lenses |url=http://www.eagleeyeuk.com/rigid-contact-lenses/ |access-date=2022-04-28 |website=Eagle Eyes UK |language=en-US}}</ref> |
|||
PMMA lenses have certain disadvantages: no [[oxygen]] is transmitted through the lens to the [[cornea]], which can cause a number of adverse clinical events. In the late 1970s, and through the 1980s and 1990s, improved rigid materials — which were also [[Oxygen permeability|oxygen-permeable]] — were developed. Lenses made from these materials are called [[rigid gas permeable]] or 'RGP' lenses. RGP lenses are not hydrophilic and do not absorb vapours or liquids, making them suitable for use in some industrial environments. |
|||
====Soft lenses==== |
|||
An RGP lens is able to replace the natural shape of the [[cornea]] with a new refracting surface. This means that a regular (spherical) rigid contact lens can provide good level of vision in people who require strong correction, have astigmatism or suffer from diseases which distort the cornea, such as [[keratoconus]]. |
|||
{{see also|List of soft contact lens materials}} |
|||
Soft lenses are more flexible than rigid lenses and can be gently rolled or folded without damaging the lens. While rigid lenses require a period of adaptation before comfort is achieved, new soft lens wearers typically report lens awareness rather than pain or discomfort. |
|||
Hydrogel lenses rely on their water content to transmit oxygen through the lens to the cornea. As a result, higher water content lenses allowed more oxygen to the cornea. In 1998, [[silicone hydrogel]], or Si-hy lenses became available. These materials have both the extremely high [[oxygen permeability]] of [[silicone]] and the comfort and clinical performance of the conventional hydrogels. Because silicone allows more oxygen permeability than water, oxygen permeability of silicone hydrogels is not tied to the lenses' water content. Lenses have now been developed with so much oxygen permeability that they are approved for overnight wear (extended wear). Lenses approved for daily wear are also available in silicone hydrogel materials.<ref>FDA Premarket Notification for [http://acuvue-now.com/latest-news/news-flash/121-green-light-for-1-day-acuvue-trueye.html "new silicone hydrogel lens for daily wear"] {{webarchive|url=https://web.archive.org/web/20081003075751/http://acuvue-now.com/latest-news/news-flash/121-green-light-for-1-day-acuvue-trueye.html |date=3 October 2008 }} 'July 2008.</ref> |
|||
While rigid lenses have been around for about 120 years, soft lenses are a much more recent development. The principal breakthrough in soft lenses made by [[Otto Wichterle]] led to the launch of the first soft ([[hydrogel]]) lenses in some countries in the 1960s and the approval of the 'Soflens' material (polymacon) by the [[United States]] FDA in 1971. Soft lenses are immediately comfortable, while rigid lenses require a period of adaptation before full comfort is achieved. The [[polymer]]s from which soft lenses are manufactured improved over the next 25 years. The [[oxygen permeability]] has been increased by varying the polymer composition. |
|||
Current brands of soft lenses are either traditional hydrogel or silicone hydrogel. Because of drastic differences in oxygen permeability, replacement schedule, and other design characteristics, it is very important to follow the instructions of the eye care professional prescribing the lenses. When comparing traditional hydrogel soft lens contacts with silicone hydrogel versions, there is no clear evidence to recommend a superior lens.<ref>{{Cite journal |last=Haworth |first=Kristina |last2=Travis |first2=Darian |last3=Leslie |first3=Louis |last4=Fuller |first4=Daniel |last5=Pucker |first5=Andrew D |date=2023-09-19 |editor-last=Cochrane Eyes and Vision Group |title=Silicone hydrogel versus hydrogel soft contact lenses for differences in patient-reported eye comfort and safety |journal=Cochrane Database of Systematic Reviews |language=en |volume=2023 |issue=9 |pages=CD014791 |doi=10.1002/14651858.CD014791.pub2 |pmc=10507745 |pmid=37724689}}</ref> |
|||
A small number of hybrid rigid/soft lenses exist. An alternative technique is piggybacking of contact lenses, a smaller, rigid lens being mounted atop a larger, soft lens. This is done in cases where a single lens will not provide the [[optical power]], fitting characteristics, or comfort required. |
|||
Disadvantages of silicone hydrogels are that they are slightly stiffer and the lens surface can be hydrophobic, thus less "wettable" – factors that can influence comfort of lens use. New manufacturing techniques and changes to multipurpose solutions have minimized these effects. Those new techniques are often broken down into 3 generations:<ref name="szcz">{{Cite web |last=Szczotka-Flynn |first=Loretta |date=1 May 2008 |title=Looking at Silicone Hydrogels Across Generations |url=http://www.optometricmanagement.com/articleviewer.aspx?articleid=101727 |url-status=live |archive-url=https://web.archive.org/web/20110719173206/http://www.optometric.com/article.aspx?article=101727 |archive-date=19 July 2011 |access-date=5 October 2021 |website=www.optometricmanagement.com}}</ref><ref name="chou">{{Cite web |last=Chou |first=Brian |date=1 June 2008 |title=The Evolution of Silicone Hydrogel Lenses |url=https://www.clspectrum.com/issues/2008/june-2008/the-evolution-of-silicone-hydrogel-lenses |url-status=live |archive-url=https://web.archive.org/web/20161230160857/https://www.clspectrum.com/issues/2008/june-2008/the-evolution-of-silicone-hydrogel-lenses |archive-date=30 December 2016 |access-date=5 October 2021 |website=www.clspectrum.com}}</ref> |
|||
In 1998, '[[silicone]] hydrogels' became available. Silicone hydrogels have both the extremely high [[oxygen permeability]] of [[silicone]] and the comfort and clinical performance of the conventional hydrogels. These lenses were initially advocated primarily for extended (overnight) wear, although more recently daily (no overnight) wear silicone hydrogels have been approved<ref>FDA Premarket Notification for [http://acuvue-now.com/latest-news/news-flash/121-green-light-for-1-day-acuvue-trueye.html "new silicone hydrogel lens for daily wear"] 'July 2008.</ref> and launched. |
|||
* 1st generation (plasma coating): A surface modification process called plasma coating alters the lens surface's hydrophobic nature; |
|||
While it provides the [[oxygen permeability]], the silicone also makes the lens surface highly hydrophobic and less "wettable." This frequently results in discomfort and dryness during lens wear. In order to compensate for the hydrophobicity, hydrogels are added (hence the name "silicone hydrogels") to make the lenses more hydrophilic. However the lens surface may still remain hydrophobic. Hence some of the lenses undergo surface modification processes by plasma treatments which alter the hydrophobic nature of the lens surface. Other lens types incorporate internal rewetting agents to make the lens surface hydrophilic. A third process uses longer backbone polymer chains that results in less cross linking and increased wetting without surface alterations or additive agents. |
|||
* 2nd generation (wetting agents): Another technique incorporates internal rewetting agents to make the lens surface hydrophilic; |
|||
* 3rd generation (inherently wettable): A third process uses longer backbone polymer chains that results in less cross linking and increased wetting without surface alterations or additive agents. |
|||
====Hybrid==== |
|||
===Wear Schedule/Wear Indicator=== |
|||
A small number of hybrid lenses exist. Typically, these contact lenses consist of a rigid center and a soft "skirt". A similar technique is the "piggybacking" of a smaller, rigid lens on the surface of a larger, soft lens. These techniques are often chosen to give the vision correction benefits of a rigid lens and the comfort of a soft lens.<ref>{{Cite web |last=White |first=Neal |last2=Jennings |first2=Christopher |last3=Pelka |first3=Kevin |date=16 January 2015 |title=Hybrid contact lens |url=https://patents.google.com/patent/US9625738B2/en |access-date=28 February 2018}}</ref> |
|||
A ''daily wear'' (DW) contact lens is designed to be removed prior to sleeping. An ''extended wear'' (EW) contact lens is designed for continuous overnight wear, typically for 6 or more consecutive nights. Newer materials, such as silicone hydrogels, allow for even longer wear periods of up to 30 consecutive nights; these longer-wear lenses are often referred to as ''continuous wear'' (CW). Generally, extended wear lenses are discarded after the specified length of time, according to the replacement schedule (see next section). Extended- and continuous-wear contact lenses can be worn for such long periods of time because of their high [[oxygen permeability]] to the cornea (typically 5–6 times greater than conventional soft lenses), which allows the eye to remain healthy even when the eyelid is closed. |
|||
===Wear schedule=== |
|||
Extended lens wearers may have an increased risk for corneal infections and [[corneal ulcer]]s, primarily due to poor care and cleaning of the lenses, tear film instability, and bacterial stagnation. [[Corneal neovascularization]] has historically also been a common complication of extended lens wear, though this does not appear to be a problem with silicone hydrogel extended wear. The most common complication of extended lens use is conjunctivitis, usually [[allergy|allergic]] or [[Conjunctivitis|giant papillary conjunctivitis]] (GPC), sometimes associated with a poorly fitting contact lens. |
|||
A "daily wear" (DW) contact lens is designed to be worn for one day and removed before sleeping. An "extended wear" (EW) contact lens is designed for continuous overnight wear, typically for up to 6 consecutive nights.<ref>{{Cite web |title=Contact Lens Types |url=https://www.aao.org/eye-health/glasses-contacts/contact-lens-types |access-date=30 April 2020 |website=American Academy of Ophthalmology}}</ref> Newer materials, such as silicone hydrogels, allow for even longer wear periods of up to 30 consecutive nights; these longer-wear lenses are often referred to as "continuous wear" (CW). EW and CW contact lenses can be worn overnight because of their high [[oxygen permeability]]. While awake, the eyes are mostly open, allowing oxygen from the air to dissolve into the tears and pass through the lens to the cornea. While asleep, oxygen is supplied from the blood vessels in the back of the eyelid. A lens hindering passage of oxygen to the cornea causes corneal hypoxia which can result in serious complications, such as [[corneal ulcer]] that, if left untreated, can permanently decrease vision. EW and CW contact lenses typically allow for a transfer of 5–6 times more oxygen than conventional softs, allowing the cornea to remain healthy, even with closed eyelids. |
|||
Wearing lenses designed for daily wear overnight has an increased risk for corneal infections, corneal ulcers and [[corneal neovascularization]]—this latter condition, once it sets in, cannot be reversed and will eventually spoil vision acuity through diminishing corneal transparency. The most common complication of extended wear is giant papillary conjunctivitis (GPC), sometimes associated with a poorly fitting contact lens. |
|||
===Replacement Schedule=== |
|||
The various soft contact lenses available are often categorized by their replacement schedule. The shortest replacement schedule is single use (1-day or daily disposable) lenses which are disposed of each night. Shorter replacement cycle lenses are commonly thinner and lighter, due to lower requirements for durability against wear and tear, and may be the most comfortable in their respective class and generation. These may be best for patients with ocular [[allergies]] or other conditions because it limits deposits of [[antigens]] and [[protein]], and is considered the healthiest wear schedule due to the most frequent replacement. Single use lenses are also useful for people who use contacts infrequently, or for purposes (e.g. swimming or other sporting activities) where losing a lens is likely. |
|||
===Replacement schedule=== |
|||
More commonly, contact lenses are prescribed to be disposed of on a two-week or 4-week basis. Quarterly or annual lenses, which used to be very common, have lost favor because a more frequent replacement allows for increased comfort and fewer on-lens deposits. Rigid gas permeable lenses are very durable and may last for several years without the need for replacement. PMMA hard lenses were very durable, and were commonly worn for 5 to 10 years. Interestingly, a careful analysis of the materials used to manufacture many 'daily' disposable lenses show that they are often manufactured from the same material as the longer life disposables (4-week replacement for example), from the same company. Although the materials are the same, the manufacturing processes by which the respective contact lenses are made is what differentiates a 'daily disposable' lens from a lens recommended for two-week or 4-week replacement. |
|||
Contact lenses are often categorized by their replacement schedule. Single use lenses (called 1-day or daily disposables) are discarded after one use. Because they do not have to stand up to the wear and tear of repeated uses, these lenses can be made thinner and lighter, greatly improving their comfort. Lenses replaced frequently gather fewer deposits of [[allergens]] and [[pathogen|germs]], making these lenses preferable for patients with ocular [[allergies]] or for those who are prone to infection. Single-use lenses are also useful for people who wear contact lenses infrequently, or when losing a lens is likely or not easily replaced (such as when on vacation). They are also considered useful for children because cleaning or disinfecting is not needed, leading to improved compliance. |
|||
Other disposable contact lenses are designed for replacement every two or four weeks. Quarterly or annual lenses, which used to be very common, are now much less so. Rigid gas permeable lenses are very durable and may last for several years without the need for replacement. PMMA hards were very durable and were commonly worn for 5 to 10 years but had several drawbacks. |
|||
Contrary to popular belief, replacement schedule is not determined by the Food & Drug Administration (FDA). Replacement schedule is recommended only by the manufacturer of that contact lens. The only FDA-approved measure of contact lens wear is the 'wear indication' or 'wear schedule' (extended wear or daily wear) as was discussed in the previous section. |
|||
Lenses with different replacement schedules can be made of the same material. Although the materials are alike, differences in the manufacturing processes determine if the resulting lens will be a "daily disposable" or one recommended for two- or four-week replacement. However, sometimes manufacturers use absolutely identical lenses and just repackage them with different labels.<ref>{{Cite news |date=1993-07-12 |title=The Only Difference Is When You Throw Them Away |url=https://www.bloomberg.com/news/articles/1993-07-11/the-only-difference-is-when-you-throw-them-away |access-date=2016-12-26 |work=Bloomberg.com}}</ref><ref>{{Cite web |title=Contact Lenses – Types of Contact Lenses. Disposable (Replacement Schedule) Contact Lenses |url=https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/HomeHealthandConsumer/ConsumerProducts/ContactLenses/ucm062319.htm#dcl |access-date=2016-12-26 |website=www.fda.gov |language=en}}</ref> |
|||
===Design=== |
|||
A '''spherical''' contact lens is one in which both the inner and outer optical surfaces are portions of a sphere. A [[toric lens]] is one in which either or both of the optical surfaces have the effect of |
|||
a cylindrical lens, usually in combination with the effect of a spherical lens. [[Myopic]] (nearsighted) and [[hypermetropic]] (farsighted) people who also have astigmatism and who have been told they are not suitable for regular contact lenses may be able to use toric lenses. If one eye has [[Astigmatism (eye)|astigmatism]] and the other does not, the patient may be told to use a spherical lens in one eye and a toric lens in the other. Toric lenses are made from the same materials as regular contact lenses but have a few extra characteristics: |
|||
* They correct for both spherical and cylindrical aberration. |
|||
* They may have a specific 'top' and 'bottom', as they are not symmetrical around their centre and must not be rotated. Lenses must be designed to maintain their orientation regardless of eye movement. Often lenses are thicker at the bottom and this thicker zone is pushed down by the upper eyelid during blinking to allow the lens to rotate into the correct position (with this thicker zone at the 6 o'clock position on the eye). Toric lenses are usually marked with tiny striations to assist their fitting. |
|||
* They are usually more expensive to produce than non-toric lenses; therefore they are usually meant for extended wear. The first disposable toric lenses were introduced in 2000 by [[Vistakon]]. |
|||
==Manufacturing== |
|||
Like eyeglasses, contact lenses can have one (single vision) or more (multifocal) [[focus (optics)|focal points]]. |
|||
[[File:Siliconehydrogel.svg|thumb|left|Molecular structure of silicone hydrogel used in flexible, oxygen-permeable contact lenses.<ref>{{Cite book |title=Kirk-Othmer Encyclopedia of Chemical Technology |year=2000 |isbn=9780471484943 |editor-last=John Wiley & Sons, Inc |doi=10.1002/0471238961}}</ref>]] |
|||
Typically, soft contact lenses are mass-produced, while rigids are custom-made to exact specifications for the individual patient. |
|||
* Spin-cast lenses – A soft lens manufactured by whirling liquid silicone in a revolving mold at high speed.<ref name="Cassin">Cassin, B. and Solomon, S. ''Dictionary of Eye Terminology''. Gainesville, Florida: Triad Publishing Company, 1990.</ref> |
|||
* [[Diamond turning]] – This type is cut and polished on a CNC [[lathe]].<ref name="Cassin" /> The lens starts out as a cylindrical disk held in the jaws of the lathe that is equipped with an industrial-grade [[diamond]] as the cutting tool. The CNC lathe may turn at nearly 6000 RPM as the cutter removes the desired amount of material from the inside of the lens. The concave (inner) surface of the lens is then polished with some fine abrasive paste, oil, and a small polyester cotton ball turned at high speeds. To hold the delicate lens in reverse manner, wax is used as an adhesive. The lens' convex (outer) surface is thus cut and polished by the same process. This method can be used to shape rigid as well as soft lenses. In the case of softs, the lens is cut from a dehydrated polymer that is rigid until water is reintroduced. |
|||
* Molded – Molding is used to manufacture some brands of soft contact lenses. Rotating molds are used and the molten material is added and shaped by centripetal forces. Injection molding and computer control are also used to create nearly perfect lenses.<ref>Manufacture of soft contact lenses. [http://www.lensfinder.co.uk/information/contact-lens-manufacturing-process/ "Manufacture of soft contact lenses".]</ref> The lens is kept moist throughout the entire molding process and is never dried and rehydrated. |
|||
==Prescriptions== |
|||
For correction of [[presbyopia]] or [[accommodative insufficiency]] multifocal contact lenses are almost always used; however, single vision lenses may also be used in a process known as ''monovision'':<ref>{{cite journal | pmid = 802938 | year = 1975 | last1 = Lebow | first1 = KA | last2 = Goldberg | first2 = JB | title = Characteristic of binocular vision found for presbyopic patients wearing single vision contact lenses | volume = 46 | issue = 11 | pages = 1116–23 | journal = Journal of the American Optometric Association}}</ref> single vision lenses are used to correct one eye's far vision and the other eye's near vision. Alternatively, a person may wear single vision contact lenses to improve distance vision and reading glasses to improve near vision. |
|||
[[File:Lens Basecurve.jpg|thumb|alt=Diagram of a circle with the diameter labeled "D" and the radius labeled "r" and "BC"|Diameter and base curve radius]] |
|||
The parameters specified in a contact lens prescription may include: |
|||
Some contact lenses have small text written around the edge, such as 123 or AV. These are used to identify if the contact lens is put on correctly or not. |
|||
* Brand name |
|||
Rigid gas permeable bifocal contact lenses most commonly have a small lens on the bottom for the near correction, when the eyes are lowered to read, this lens comes into the optical path. RGPs must translate (move vertically) to work properly, and thus the gaze of the eye can change from the near to the distant sections, much like bifocal eyeglasses. |
|||
* Material |
|||
* [[Base curve radius]] (BC, BCR) |
|||
* [[Diameter]] (D, OAD) |
|||
* [[Optical power]] in [[diopter]]s (dpt) |
|||
* Center thickness (CT) |
|||
Prescriptions for contact lenses and [[glasses]] may be similar but are not interchangeable. Prescribing of contact lenses is usually restricted to various combinations of [[ophthalmologist]]s, [[optometrist]]s and [[optician]]s. An [[eye examination]] is needed to determine an individual's suitability for contact lens wear. This typically includes a [[refraction]] to determine the proper power of the lens and an assessment of the health of the eye's anterior segment. Many eye diseases inhibit contact lens wear, such as active infections, allergies, and dry eye.<ref>Agarwal, R.K. (1970), Some reasons for not fitting contact lenses, The Optician, 4 December, page 623 (published in London, England).</ref> [[Keratometer|Keratometry]] is especially important in the fitting of rigid lenses. |
|||
Multifocal soft contact lenses are more complex to manufacture and require more skill to fit. All soft bifocal contact lenses are considered "simultaneous vision" because both far and near vision corrections are presented simultaneously to the retina, regardless of the position of the eye. Of course, only one correction is correct, the incorrect correction causes blur. Commonly these are designed with distance correction in the center of the lens and near correction in the periphery, or vice versa. |
|||
=== |
===United States=== |
||
Contact lenses are prescribed by [[ophthalmologist]]s, [[optometrist]]s, or specially licensed [[optician]]s under the supervision of an eye doctor. They are typically ordered at the same office that conducts the eye exam and fitting. The [[Fairness to Contact Lens Consumers Act]] guarantees consumers a copy of their contact lens prescription, allowing them to obtain lenses at the provider of their choice.<ref name="FCLCA">[http://www.gpo.gov/fdsys/pkg/PLAW-108publ164/html/PLAW-108publ164.htm "Fairness to Contact Lens Consumers Act"]. 15 October 2003.</ref> |
|||
[[Intraocular lens]]es, also known as an ''implantable contact lenses'', are special small corrective lenses surgically implanted in the eye's [[posterior chamber]] behind the [[iris (anatomy)|iris]] and in front of the [[lens (anatomy)|lens]] to correct higher degrees of myopia and hyperopia. |
|||
==Usage== |
|||
==Manufacturing of contact lenses== |
|||
Before touching the contact lens or the eye, it is important to [[handwashing|wash hands]] thoroughly with [[soap]] and rinse well. Soaps containing [[moisturizer]]s or [[allergen]]s should be avoided as these can cause eye irritation.<ref>{{Cite web |title=How to Put Contacts in Your Eyes |url=http://coopervision.com/about-contacts/how-put-contacts-your-eyes |access-date=20 November 2014 |publisher=CooperVision |quote=use plain soap without any heavy moisturizers or perfumes. Rinse well and dry your hands. Again, this is to prevent transmitting anything unwanted to your eyes.}}</ref> Drying of hands using towels or tissues before handling contact lenses can transfer lint (fluff) to the hands and, subsequently, to the lenses, causing irritation upon insertion. Towels, unless freshly laundered on high temperature wash, are frequently contaminated with large quantities of bacteria and, as such, should be avoided when handling lenses. Dust, lint and other debris may collect on the outside of contact lenses. Again, hand contact with this material, before handling contact lenses, may transfer it to the lenses themselves. Rinsing the case under a source of clean running water, before opening it, can help alleviate this problem. Next the lens should be removed from its case and inspected for defects (e.g. splits, folds, lint). A 'gritty' or rough appearance to the lens surface may indicate that a considerable quantity of proteins, lipids and debris has built up on it and that additional cleaning is required; this is often accompanied and felt by unusually high irritation upon insertion. |
|||
Most contact lenses are mass produced. |
|||
* Spin-cast lenses – A spin-cast lens is a soft contact lens manufactured by whirling liquid silicone in a revolving mold at high speed.<ref name="Cassin">Cassin, B. and Solomon, S. ''Dictionary of Eye Terminology''. Gainsville, Florida: Triad Publishing Company, 1990.</ref> |
|||
* [[Diamond turning]] – A diamond-turned contact lens is cut and polished on a CNC [[lathe]].<ref name="Cassin"/> The lens starts out as a cylindrical disk held in the jaws of the lathe. The lathe is equipped with an industrial-grade [[diamond]] as the cutting tool. The CNC lathe may turn at nearly 6000 RPM as the cutter removes the desired amount of material from the inside of the lens. The [[wikt:concave|concave]] (inner) surface of the lens is then polished with some fine abrasive paste, oil, and a small polyester cotton ball turned at high speeds. In order to hold the delicate lens in reverse manner, wax is used as an adhesive. The [[wikt:convex|convex]] (outer) surface of the lens is thus cut and polished by the same process. |
|||
* Molded – Molding is used to manufacture some brands of soft contact lenses. Rotating molds are used and the molten material is added and shaped by centrifugal forces. Injection molding and computer control are also used to create nearly perfect lenses.<ref>Manufacture of soft contact lenses. The contact lens is kept moist throughout the entire molding process and is never dried then rehydrated. [http://www.lensfinder.co.uk/information/contact-lens-manufacturing-process/ "Manufacture of soft contact lenses".]</ref> |
|||
* Hybrids |
|||
Care should be taken to ensure the soft lens is not inserted inside-out. The edge of a lens turned inside out has a different appearance, especially when the lens is slightly folded. Insertion of an inside-out lens for a brief time (less than one minute) should not cause any damage to the eye. Some brands of lenses have markings on the rim that make it easier to tell the front of the lens apart from the back. |
|||
Although many companies make contact lenses, in the US there are four major manufacturers:<ref>Federal Trade Commission. [http://www.ftc.gov/reports/contactlens/050214contactlensrpt.pdf "The Strength of Competition in the Sale of Rx Contact Lenses: An FTC Study".] February, 2005.</ref> |
|||
* [[Acuvue]]/[[Vistakon]] ([[Johnson & Johnson]]) |
|||
* [[Ciba Vision]] ([[Novartis]]) |
|||
* [[Bausch & Lomb]] |
|||
* [[CooperVision]] |
|||
===Extended Wear Contacts Lenses=== |
|||
====Silicone Hydrogel Lenses==== |
|||
Silicone is oxygen permeable. Silicone hydrogel lenses use both their water and polymer content to transmit oxygen to the eye. |
|||
===Insertion=== |
|||
The benefits to wearers include comfort and convenience. Silicone hydrogel contact lenses contain less water and deliver more oxygen to the eye than traditional hydrogel lenses. As a result, they aren't as prone to causing dehydration. For some people who wear their lenses for long days, this can mean better end-of-day comfort and allow for overnight wear. Some brands of silicone hydrogel lenses are approved for 30 days of continuous wear. |
|||
[[File:Contact Lens Wiki 2 3.webm|thumb|Video instructions for inserting and removing contact lenses]] |
|||
Contact lenses are typically inserted into the eye by placing them on the pad of the index or middle finger with the concave side upward and then using that finger to place the lens on the eye. Rigid lenses should be placed directly on the cornea. Soft lenses may be placed on the [[sclera]] (white of the eye) and then slid into place. Another finger of the same hand, or a finger of the other hand, is used to keep the eye wide open. Alternatively, the user may close their eyes and then look towards their nose, sliding the lens into place over the cornea. Problems may arise if the lens folds, turns inside-out, slides off the finger prematurely, or adheres more tightly to the finger than the eye surface. A drop of solution may help the lens adhere to the eye. |
|||
===Hydrogel materials=== |
|||
* Alphafilcon A |
|||
* Asmofilcon A |
|||
* Balafilcon A |
|||
* Comfilcon A |
|||
* Enfilcon A |
|||
* Etafilcon A |
|||
* Galyfilcon A |
|||
* Hilafilcon A |
|||
* Hilafilcon B |
|||
* Hioxifilcon A |
|||
* Hioxifilcon D |
|||
* Lotrafilcon B |
|||
* Methafilcon A |
|||
* Omafilcon A |
|||
* Phemfilcon A |
|||
* Polymacon |
|||
* Senofilcon |
|||
* Tetrafilcon A |
|||
* Vifilcon A |
|||
* POLY HEMA |
|||
When the lens first contacts the eye, it should be comfortable. A brief period of irritation may occur, caused by a difference in [[pH]] and/or [[salinity]] between that of the lens solution and the tear.<ref>{{Cite journal |last=Demas GN |year=1989 |title=pH consistency and stability of contact lens solutions |journal=J Am Optom Assoc |volume=60 |issue=10 |pages=732–4 |pmid=2584587 |quote=The pH of contact lens solutions has been implicated in the comfort of contact lenses on insertion.}}</ref><ref>{{Cite web |title=Eye Care |url=http://www.contactlensheaven.com/eyecare.html |access-date=20 November 2014 |publisher=CLH}}</ref> This discomfort fades quickly as the solution drains away and is replaced by the natural tears. However, if irritation persists, the cause could be a dirty, damaged, or inside-out lens. Removing and inspecting it for damage and proper orientation, and re-cleaning if necessary, should correct the problem. If discomfort continues, the lens should not be worn. In some cases, taking a break from lens wear for a day may correct the problem. In case of severe discomfort, or if it does not resolve by the next day, the person should be seen as soon as possible by an eye doctor to rule out potentially serious [[#Complications|complications]]. |
|||
==Contact lens prescriptions== |
|||
The prescribing of contact lenses is usually restricted to appropriately qualified [[eye care professional|eye care practitioners]]. In countries such as the United States (where all contact lenses are deemed to be [[medical device]]s by the Food and Drug Administration), the United Kingdom and Australia, [[optometry|optometrists]] are usually responsible. <!--no FDA in UK, AU. Don't know if contacts considered medical devices-->In France and Eastern European countries, [[ophthalmology|ophthalmologists]] play the major role. In other parts of the world, [[opticians]] usually prescribe contact lenses. Prescriptions for contact lenses and [[glasses]] may be similar, but are not interchangeable. |
|||
===Removal=== |
|||
The practitioner or contact lens fitter typically determines an individual's suitability for contact lenses during an [[eye examination]]. Corneal health is verified; ocular allergies or [[dry eye]]s may affect a person's ability to wear contact lenses successfully. |
|||
Removing contact lenses incorrectly can result in damage to the lens and injury to the eye, so certain precautions must be taken. Rigid contact lenses can best be removed by pulling the eyelid tight and then blinking, whereupon the lens drops out. With one finger on the outer corner of the eyelids, or lateral [[canthus (anatomy)|canthus]], the person stretches the eyelids towards the ear; the increased tension of the eyelid margins against the edge of lens allows the blink to break the [[capillary action]] that adheres the lens to the eye. The other hand is typically cupped underneath the eye to catch the lens as it drops out. For soft lenses, which have a stronger adherence to the eye surface, this technique is less suitable. |
|||
A soft contact lens may be removed by pinching the edge between the thumb and index finger. Moving the lens off the cornea first can improve comfort during removal and reduce risk of scratching the cornea with a fingernail. It is also possible to push or pull a soft lens far enough to the side or bottom of the eyeball to get it to fold then fall out, without pinching and thereby damaging it. If these techniques are used with a rigid lens, it may scratch the cornea. |
|||
The parameters specified in a contact lenses prescription may include: |
|||
* Material (e.g. [[Oxygen Permeability|Oxygen Permeability/Transmissibility (Dk/L, Dk/t)]], water content, modulus; optional) |
|||
* [[Base curve radius]] (BC, BCR; required) |
|||
* [[Diameter]] (D, OAD; required) |
|||
* [[Optical power|Power]] in [[dioptre]]s (Spherical required, cylindrical only for correction of astigmatism, reading addition required only for bifocal prescription) |
|||
* Cylinder axis (Often just "Axis"; required only if a cylindrical correction is present) |
|||
* Center thickness (CT; optional and seldom provided) |
|||
* Brand (Optional) |
|||
There are also small tools specifically for removing lenses. Usually made of flexible plastic, they resemble small tweezers, or [[plunger]]s that suction onto the front of the lens. Typically, these tools are used only with rigid lenses. Extreme care must be exercised when using mechanical tools or fingernails to insert or remove contact lenses. |
|||
Note that while a contact lens prescription may specify diameter and base curve of the ideal lens for a particular individual, many manufacturers only produce lenses at very limited intervals. [[Johnson & Johnson]], which manufactures the "[[Acuvue 2]]" soft lens, only makes such lenses with base curves of either 8.3mm or 8.7mm, and only at a diameter of 14.0mm—such lenses are designed to fit a "target audience" that includes the vast majority of individuals who might fit such lenses or might at least find them sufficiently comfortable to wear. |
|||
===Care=== |
|||
Many people already wear contact lenses ordered over the Internet. In the [[United States]], the [[Fairness to Contact Lens Consumers Act]], which [[Effective date|went into effect]] in 2004, was intended to ensure the availability of contact lens prescriptions to patients.<ref name="FCLCA">[http://www.1800contacts.com/ExternalRelations/docs/ECP/FairnessToContactLensConsumersAct.pdf "Fairness to Contact Lens Consumers Act"]. October 15, 2003.</ref> Under the law consumers have a right to obtain a copy of their contact lens prescription, allowing them to fill that prescription at the business of their choice. Some controversy has arisen over the fact that online vendors are allowed to fill a prescription if the originating prescriber doesn't respond within eight business hours, as verifications are often sent during the prescriber's closed hours, allowing even an expired prescription to be filled.<ref name="FCLCA"/> |
|||
[[File:Lens-cover.jpg|thumb|alt=An open lens care. The lens caps are engraved with the letters L and R to indicate left and right. The case body is shaped as a pair of glasses and contains two holes for the lenses.|Lens case to store contacts]] |
|||
Lens care varies depending on material and wear schedule. Daily disposables are discarded after a single use and thus require no cleaning. Other lenses need regular cleaning and disinfecting to prevent surface coating and infections. |
|||
==Complications== |
|||
[[Complication (medicine)|Complications]] due to contact lens wear affect roughly 5% of contact lens wearers each year.<ref name="Stamler">John Stamler. [http://www.emedicine.com/oph/topic651.htm "Contact Lens Complications."] ''eMedicine.com.'' September 1, 2004.</ref> Excessive wear of contact lenses, particularly overnight wear, is associated with most of the safety concerns. Problems associated with contact lens wear may affect the [[eyelid]], the [[conjunctiva]], the various layers of the [[cornea]],<!-- such as lens hypathnea, where the lens becomes lodged on the opposite side of the pupil. |
|||
There are many ways to clean and care for contact lenses, typically called care systems or lens solutions: |
|||
--><ref name="pmid17498998">{{cite journal |author=Efron N |title=Contact lens-induced changes in the anterior eye as observed in vivo with the confocal microscope |journal=[[Prog Retin Eye Res]] |volume=26 |issue=4 |pages=398–436 |year=2007 |month=July |pmid=17498998 |doi=10.1016/j.preteyeres.2007.03.003 |url=http://linkinghub.elsevier.com/retrieve/pii/S1350-9462(07)00025-0}}</ref><!-- |
|||
;Multipurpose solutions |
|||
--> and even the [[tears|tear film]] that covers the outer surface of the eye.<ref name="Stamler"/> |
|||
:The main attraction of multipurpose solutions is that the same solution can clean, rinse, disinfect and store lenses. Some multipurpose solutions also contain ingredients that improve the surface wettability and comfort of silicone hydrogel lenses. Studies showed that multipurpose solutions are ineffective against ''[[Acanthamoeba]]e''.<ref name="Johnston2009">{{Cite journal |last=Johnston |first=Stephanie P. |last2=Sriram |first2=Rama |last3=Qvarnstrom |first3=Yvonne |last4=Roy |first4=Sharon |last5=Verani |first5=Jennifer |last6=Yoder |first6=Jonathan |last7=Lorick |first7=Suchita |last8=Roberts |first8=Jacquelin |last9=Beach |first9=Michael J. |last10=Visvesvara |first10=Govinda |date=July 2009 |title=Resistance of Acanthamoeba Cysts to Disinfection in Multiple Contact Lens Solutions |journal=Journal of Clinical Microbiology |volume=47 |issue=7 |pages=2040–2045 |doi=10.1128/JCM.00575-09 |pmc=2708465 |pmid=19403771}}</ref><ref name="Padzik2014">{{Cite journal |last=Padzik |first=Marcin |last2=Chomicz |first2=Lidia |last3=Szaflik |first3=Jacek P. |last4=Chruścikowska |first4=Agnieszka |last5=Perkowski |first5=Konrad |last6=Szaflik |first6=Jerzy |date=November 2014 |title=In vitro effects of selected contact lens care solutions on Acanthamoeba castellanii strains in Poland |journal=Experimental Parasitology |volume=145 |pages=S98–S101 |doi=10.1016/j.exppara.2014.06.014 |pmid=24967738}}</ref><ref name="de Aguiar2013">{{Cite journal |last=Aguiar |first=Ana |last2=Oliveira Silveira |first2=Caroline |last3=Todero Winck |first3=Mari |last4=Rott |first4=Marilise |date=1 January 2013 |title=Susceptibility of Acanthamoeba to multipurpose lens-cleaning solutions |journal=Acta Parasitologica |volume=58 |issue=3 |pages=304–308 |doi=10.2478/s11686-013-0143-9 |pmid=23990426 |doi-access=free |hdl-access=free |hdl=10183/179379}}</ref> There is preliminary research on creating a new multipurpose solution that kills amoeba.<ref>{{Cite journal |last=Fears |first=Alyssa C. |last2=Metzinger |first2=Rebecca C. |last3=Killeen |first3=Stephanie Z. |last4=Reimers |first4=Robert S. |last5=Roy |first5=Chad J. |date=December 2018 |title=Comparative in vitro effectiveness of a novel contact lens multipurpose solution on Acanthamoeba castellanii |journal=Journal of Ophthalmic Inflammation and Infection |volume=8 |issue=1 |pages=19 |doi=10.1186/s12348-018-0161-8 |pmc=6200833 |pmid=30357549 |doi-access=free}}</ref> |
|||
[[File:Contact lens case for Hydrogen Peroxide solution showing bubbles.jpg|thumb|upright|Contact lenses soaking in a hydrogen peroxide-based solution.]] |
|||
;[[Hydrogen peroxide contact solutions]] |
|||
:Hydrogen peroxide can be used to disinfect contact lenses.<ref name="hughes">{{Cite journal |last=Hughes |first=Reanne |last2=Kilvington |first2=Simon |date=July 2001 |title=Comparison of Hydrogen Peroxide Contact Lens Disinfection Systems and Solutions against Acanthamoeba polyphaga |journal=Antimicrobial Agents and Chemotherapy |volume=45 |issue=7 |pages=2038–43 |doi=10.1128/AAC.45.7.2038-2043.2001 |pmc=90597 |pmid=11408220}}</ref> Care should be taken not to get hydrogen peroxide in the eye because it is very painful and irritating. With "two-step" products, the hydrogen peroxide must be rinsed away with saline before the lenses may be worn. "One-step" systems allow the hydrogen peroxide to react completely, becoming pure water. Thus "one-step" hydrogen peroxide systems do not require the lenses to be rinsed before insertion, provided the solution has been given enough time to react. |
|||
:An exposure time of 2-3 hours to 3% {{chem|H|2|O|2}} (non neutralized solution) is sufficient to kill bacteria, HIV, fungi, and ''Acanthamoeba''.<ref name="Hiti2002">{{Cite journal |last=Hiti |first=K |last2=Walochnik |first2=J |last3=Haller-Schober |first3=EM |last4=Faschinger |first4=C |last5=Aspöck |first5=H |date=1 February 2002 |title=Viability of Acanthamoeba after exposure to a multipurpose disinfecting contact lens solution and two hydrogen peroxide systems |journal=British Journal of Ophthalmology |volume=86 |issue=2 |pages=144–146 |doi=10.1136/bjo.86.2.144 |pmc=1771011 |pmid=11815336}}</ref><ref name="Hiti2004">{{Cite journal |last=Hiti |first=K |last2=Walochnik |first2=J |last3=Faschinger |first3=C |last4=Haller-Schober |first4=E-M |last5=Aspöck |first5=H |date=December 2005 |title=One- and two-step hydrogen peroxide contact lens disinfection solutions against Acanthamoeba: How effective are they? |journal=Eye |volume=19 |issue=12 |pages=1301–1305 |doi=10.1038/sj.eye.6701752 |pmid=15543174 |doi-access=free}}</ref> This can be achieved by using a "two-step" product or a "one-step" tablet system if the catalytic tablet is not added before 2-3 hours.<ref name="Hiti2004" /> However, the "one-step" catalytic disk systems are not effective against ''Acanthamoeba'' due to insufficient exposure time.<ref name="Hiti2004" /> |
|||
;Enzymatic cleaner |
|||
:Used for cleaning protein deposits off lenses, usually weekly, if the daily cleaner is not sufficient. Typically, this cleaner is in tablet form. |
|||
;Ultraviolet, vibration, or ultrasonic devices |
|||
:These devices intend to disinfect and clean contact lenses. The lenses are inserted inside the portable device (running on batteries and/or plug-in) for 2 to 6 minutes during which both the microorganisms and protein build-up are supposed to be cleaned. However these devices can not be used to replace the manual rub and rinse method because vibration and ultrasound can not create relative motion between contact lens and solution, which is required for proper cleaning of the lens.<ref>{{Cite journal |last=Efron |first=Nathan |last2=Lowe |first2=Russell |last3=Vallas |first3=Vicky |last4=Grusiner |first4=Eugene |date=1991-01-01 |title=Clinical efficacy of standing wave and ultrasound for cleaning and disinfecting contact lenses |url=https://www.contactlensjournal.com/article/0892-8967(91)90040-7/abstract |journal=International Contact Lens Clinic |language=English |volume=18 |issue=1 |pages=24–29 |doi=10.1016/0892-8967(91)90040-7 |issn=0892-8967}}</ref> These devices are not usually available in optic retailers but are in other stores.<ref>{{Cite journal |date=6 April 2019 |title=How Optical Ultrasonic Cleaners Work |url=http://www.tech-faq.com/how-optical-ultrasonic-cleaners-work.html |website=The Tech-FAQ}}</ref><ref>{{Cite journal |last=White |first=Gina |title=Caring for Soft Contact Lenses |url=http://www.allaboutvision.com/contacts/caresoftlens.htm |website=All About Vision}}</ref><ref>{{Cite journal |last=Ward |first=Michael |title=Soft Contact Lens Care Products |url=http://www.clspectrum.com/article.aspx?article=12384 |website=Contact Lens Spectrum}}</ref> |
|||
====Rub and rinse method==== |
|||
Studies conducted on side effects from long-term wearing of contact lenses, i.e. over 5 years, such as by Zuguo Liu et al., 2000,<ref name="pmid10647727">{{cite journal |author=Liu Z, Pflugfelder SC |title=The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity |journal=[[Ophthalmology (journal)|Ophthalmology]] |volume=107 |issue=1 |pages=105–11 |year=2000 |month=January |pmid=10647727 |doi= 10.1016/S0161-6420(99)00027-5|url=http://linkinghub.elsevier.com/retrieve/pii/S0161-6420(99)00027-5}}</ref> concludes that "Long-term contact lens wear appears to decrease the entire corneal thickness and increase the corneal curvature and surface irregularity." |
|||
Contact lenses can be mechanically cleaned of more substantial protein, lipid and debris build up by rubbing them between the clean pad of a finger and the palm of a hand, using a small amount of cleaning fluid as a lubricant; and by rinsing thereafter. This "rub and rinse" method is thought to be the most effective method for multipurpose solutions,<ref name="zhuRub">{{Cite journal |last=Zhu |first=Hua |last2=Bandara |first2=Mahesh B. |last3=Vijay |first3=Ajay K. |last4=Masoudi |first4=Simin |last5=Wu |first5=Duojia |last6=Willcox |first6=Mark D. P. |date=August 2011 |title=Importance of Rub and Rinse in Use of Multipurpose Contact Lens Solution |journal=Optometry and Vision Science |volume=88 |issue=8 |pages=967–972 |doi=10.1097/OPX.0b013e31821bf976 |pmid=21623253 |s2cid=23544740 |doi-access=free}}</ref> and is the method indicated by the [[American Academy of Ophthalmology]] regardless of cleaning solution used.<ref name="aaoRub">{{Cite web |last=Boyd |first=Kierstan |date=4 March 2021 |title=How to Take Care of Contact Lenses |url=https://www.aao.org/eye-health/glasses-contacts/contact-lens-care |access-date=5 October 2021 |website=[[American Academy of Ophthalmology|www.aao.org]]}}</ref> In 2010, the FDA recommended that manufacturers removed the "no rub" from product labeling,<ref name="FDAguide">{{Cite web |date=15 August 2010 |title=Contact Lens Care Products Labeling - Guidance for Industry and FDA Staff |url=https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/contact-lens-care-products-labeling-guidance-industry-and-fda-staff |access-date=5 October 2021 |website=[[FDA|www.fda.gov]]}}</ref> "because {{'}}rub-and-rinse{{'}} regimens help prevent microbial adhesion to the contact lens, help prevent formation of [[biofilm]]s, and generally reduce the microbial load on the lens and the lens case."<ref name="FDArub">{{Cite web |date=19 May 2009 |title=FDA Letter to Firms with Marketing Clearance for No-rub Multipurpose Contact Lens Solutions |url=https://www.fda.gov/medical-devices/contact-lenses/fda-letter-firms-marketing-clearance-no-rub-multipurpose-contact-lens-solutions |access-date=5 October 2021 |website=[[FDA|www.fda.gov]]}}</ref> |
|||
====Physical rubbing devices==== |
|||
Long-term wear of rigid contact lens is associated with decreased [[corneal keratocyte]] density<ref name="pmid16303530">{{cite journal |author=Hollingsworth JG, Efron N |title=Confocal microscopy of the corneas of long-term rigid contact lens wearers |journal=[[Cont Lens Anterior Eye]] |volume=27 |issue=2 |pages=57–64 |year=2004 |month=June |pmid=16303530 |doi=10.1016/j.clae.2004.02.002 |url=http://linkinghub.elsevier.com/retrieve/pii/S1367-0484(04)00018-9}}</ref> and increased number of [[corneal epithelium|epithelial]] [[Langerhans cells]].<ref name="pmid17198013">{{cite journal |author=Zhivov A, Stave J, Vollmar B, Guthoff R |title=''In vivo'' confocal microscopic evaluation of langerhans cell density and distribution in the corneal epithelium of healthy volunteers and contact lens wearers |journal=[[Cornea]] |volume=26 |issue=1 |pages=47–54 |year=2007 |month=January |pmid=17198013 |doi=10.1097/ICO.0b013e31802e3b55 |url=http://meta.wkhealth.com/pt/pt-core/template-journal/lwwgateway/media/landingpage.htm?issn=0277-3740&volume=26&issue=1&spage=47}}</ref> |
|||
[[File:Eyexpert Supermoist lenzenvloeistof twee maten inclusief lenshouder.jpg|thumb|upright|alt=See caption|Saline solution bottles together with contact lens cases]] |
|||
This type of devices mimic digital rubbing. The lenses are sandwiched by silicone parts inside the portable device. The device applies a gentle yet high speed rubbing action on the lens surface and remove debris. |
|||
===Eyelid=== |
|||
* [[Ptosis (eyelid)|Ptosis]] |
|||
;[[Saline solution]] |
|||
===Conjunctiva=== |
|||
:Sterile saline is used for rinsing the lens after cleaning and preparing it for insertion. Saline solutions do not disinfect, so it must be used in conjunction with some type of disinfection system. One advantage to saline is that it cannot cause an allergic response, so it is well suited for individuals with sensitive eyes or strong allergies. |
|||
* [[Giant papillary conjunctivitis]] |
|||
;Daily cleaner |
|||
* [[Superior limbic keratoconjunctivitis]] |
|||
:Used to clean lenses on a daily basis. A few drops of cleaner are applied to the lens while it rests in the palm of the hand; the lens is rubbed for about 20 seconds with a clean fingertip (depending on the product) on each side. Lens must then be rinsed. This system is commonly used to care for rigid lenses. |
|||
Water is not recommended for cleaning contact lenses.<ref name="raz">{{Cite journal |last=Razmaria |first=Aria A. |year=2015 |title=Proper Care of Contact Lenses |journal=JAMA |volume=314 |issue=14 |page=1534 |doi=10.1001/jama.2015.12468 |pmid=26462011}}</ref> Insufficiently chlorinated tap water can lead to lens contamination, particularly by Acanthamoeba. On the other hand, sterile water will not kill any contaminants that get in from the environment.<ref name="Carnt">{{Cite journal |last=Carnt |first=Nicole A. |last2=Subedi |first2=Dinesh |last3=Connor |first3=Sophie |last4=Kilvington |first4=Simon |date=11 March 2020 |title=The relationship between environmental sources and the susceptibility of Acanthamoeba keratitis in the United Kingdom |journal=PLOS ONE |volume=15 |issue=3 |pages=e0229681 |bibcode=2020PLoSO..1529681C |doi=10.1371/journal.pone.0229681 |pmc=7065798 |pmid=32160218 |doi-access=free}}</ref> |
|||
===Cornea=== |
|||
* [[Epithelium]] |
|||
** [[Corneal abrasion]] |
|||
** [[Corneal erosion]] |
|||
** [[Contact lens acute red eye]] (CLARE) |
|||
** [[Keratoconus]] |
|||
* [[Corneal endothelium]] |
|||
Aside from cleaning the contact lenses, contact lens case should also be kept clean and be replaced at minimum every 3 months.<ref name="aaoRub" /> |
|||
==Usage== |
|||
Before touching the contact lens or one's eyes, it is important to thoroughly [[handwashing|wash & rinse hands]] with a [[soap]] that does not contain [[moisturizer]]s or [[allergen]]s such as [[fragrance]]s {{Citation needed|date=April 2011}}. The soap should not be [[antibacterial]] due to risk of improper hand washing and the possibility of destroying the natural bacteria found on the eye. These bacteria keep pathogenic bacteria from colonizing the cornea {{Citation needed|date=April 2011}}. The technique for removing or inserting a contact lens varies slightly depending upon whether the lens is soft or rigid. |
|||
Contact lens solutions often contain [[preservative]]s such as [[benzalkonium chloride]] and [[benzyl alcohol]]. Preservative-free products usually have shorter [[shelf life|shelf lives]], but are better suited for individuals with an allergy or sensitivity to a preservative. In the past, [[thiomersal]] was used as a preservative. In 1989, thiomersal was responsible for about 10% of problems related to contact lenses.<ref>{{Cite journal |last=Wilson-Holt |first=N |last2=Dart |first2=J K G |date=September 1989 |title=Thiomersal keratoconjunctivitis, frequency, clinical spectrum and diagnosis |journal=Eye |volume=3 |issue=5 |pages=581–587 |doi=10.1038/eye.1989.91 |pmid=2630335 |doi-access=free}}</ref> As a result, most products no longer contain thiomersal. |
|||
In all cases, the insertion and removal of lenses requires some training and practice on the part of the user, in part to overcome the instinctive hesitation against actually touching the eyeball with one's fingertip. |
|||
== |
==Complications== |
||
{{Main|List of contact lens complications}} |
|||
[[Image:Contact Lens Ayala.jpg|thumb|200px|Inserting a contact lens]] |
|||
{{Further|Effects of long-term contact lens wear on the cornea}} |
|||
Contact lenses are typically inserted into the eye by placing them on the index finger with the concave side upward and raising them to touch the cornea. The other hand may be employed to keep the eye open. Problems may arise particularly with disposable soft lenses; if the [[surface tension]] between the lens and the finger is too great the lens may turn itself inside out; alternatively it may fold itself in half. When the lens first contacts the eye, a brief period of irritation may ensue as the eye acclimatizes to the lens and also (if a multi-use lens is not correctly cleansed) as dirt on the lens irritates the eye. Irrigation may help during this period, which generally should not exceed one minute. It may be noted that although with some types of contact lenses it is easy to tell if you have inserted the lens backwards (as it is usually painful and vision is impaired) you are able to determine the lens's correct position beforehand by holding the lens on the tip of your finger and squeezing the bottom of it with two fingers from your other hand, you will know you have it the correct way if the edges of the lens curve inward like a taco. If they curve out you need to flip the lens. With some types of lenses however, this is difficult as both sides look very much the same. With many lenses it is hard to tell whether they are inside out or not even when they are in the eye itself. This is because the vision and feel of the lens can be very similar for both sides. For these reasons many people try to ensure they keep visual track of the different sides of the contact lenses from the day they are open, if they suspect the lens is inside out they can always change its orientation at a later stage. It is never advisable to wear the lenses inside-out even if they feel comfortable and vision is good when doing so. |
|||
===== Insertion of Contact Lenses Tips ===== |
|||
* Place the contact lens on the index finger of the hand you write with. |
|||
* With the same hand take the middle finger and hold the bottom lid open. |
|||
* With the free hand reach over and hold the top lid close to the lashes open.<ref>[http://www.contactlensesexpress.co.uk Contact Lenses Insertion Tips]</ref> |
|||
* You should have created a large enough space for the contact lens to go in without touching anything other then the eyes. |
|||
[[File:Clare-314.jpg|thumb|alt=Closeup of an eye infection after wearing contact lenses|[[Contact lens acute red eye]] (CLARE) is a group of inflammatory complications from lens wear]] |
|||
===Removal=== |
|||
A soft lens may be removed by holding the eyelids open and grasping the lens with opposing digits. This method may cause irritation, could risk damage to the eye and may in many cases be difficult, in part due to the [[Corneal reflex|blink reflex]]. If the lens is pushed off the cornea (by touching the lens with your forefinger and looking towards your nose, moving the lens) it will buckle up (due to the difference in curvature), making it easier to grasp. |
|||
Contact lenses are generally safe as long as they are used correctly. [[Complication (medicine)|Complications]] from contact lens wear affect roughly 5% of wearers yearly.<ref name="Stamler">{{Cite journal |last=Stamler |first=John F. |date=August 1998 |title=The complications of contact lens wear |journal=Current Opinion in Ophthalmology |volume=9 |issue=4 |pages=66–71 |doi=10.1097/00055735-199808000-00012 |pmid=10387472}}</ref> Factors leading to eye damage varies,<ref name="Factors Leading to Eye Damage Caused by Contact Lenses">{{Cite web |title=Do Contact Lenses Damage The Eye? |url=https://www.lensite.co.uk/Lens-Wearing-Guide/Contact-Lenses-Facts |url-status=dead |archive-url=https://web.archive.org/web/20181002020453/https://www.lensite.co.uk/Lens-Wearing-Guide/Contact-Lenses-Facts |archive-date=2 October 2018 |access-date=30 March 2018 |publisher=Lensite}}</ref> and improper use of a contact lens may affect the [[eyelid]], the [[conjunctiva]], and, most of all, the whole structure of the [[cornea]].<ref name="Stamler" /> Poor lens care may lead to infections by various [[microorganism]]s including [[bacteria]], [[fungi]], and the amoeba ''[[Acanthamoeba]]'' ([[Acanthamoeba keratitis|''Acanthamoeba'' keratitis]]). |
|||
As an alternative method to grasping, once the lens is moved off the cornea to the inner corner of the eye, it can be pushed out of the eye by pressing downwards on the upper eyelid with a finger. With this method there is less risk of touching the eye with the fingers, and it may be easier for people with long fingernails. |
|||
Many complications arise when contact lenses are worn not as prescribed (improper wear schedule or lens replacement). Sleeping in lenses not designed or approved for extended wear is a common cause of complications. Many people go too long before replacing their contacts, wearing lenses designed for 1, 14, or 30 days of wear for multiple months or years. While this does save on the cost of lenses, it risks permanent damage to the eye and even loss of sight. |
|||
Rigid contact lenses may be removed by pulling with one finger on the outer or lateral [[canthus (anatomy)|canthus]], then blinking to cause the lens to lose [[adhesion]]. The other hand is typically cupped underneath the eye to catch the lens. There also exist small tools specifically for removing lenses, which resemble small [[plunger]]s made of flexible plastic; the concave end is raised to the eye and touched to the lens, forming a seal stronger than that of the lens with the cornea and allowing the lens to be removed from the eye. |
|||
For non silicone-hydrogel lenses, one of the major factors that causes complications is that the contact lens is an oxygen barrier. The cornea needs a constant supply of oxygen to remain completely transparent and function as it should; it normally gets that oxygen from the surrounding air while awake, and from the blood vessels in the back of the eyelid while asleep. The most prominent risks associated with long-term, chronic low oxygen to the cornea include [[corneal neovascularization]], increased epithelial permeability, bacterial adherence, microcysts, corneal [[edema]], endothelial [[polymegethism]], dry eye and potential increase in myopia.<ref name="What's the Best Prescription for Healthy Contact Lens Wear?">{{Cite web |title=What's the Best Prescription for Healthy Contact Lens Wear? |url=http://www.clspectrum.com/article.aspx?article=12590 |publisher=Contact Lens Spectrum}}</ref> Much of the research into soft and rigid contact lens materials has centered on improving oxygen transmission through the lens. |
|||
===Care=== |
|||
[[Image:Lens-cover.jpg|thumb|right|Lens cover to store contact lens]] |
|||
Silicone-hydrogel lenses available today have effectively eliminated hypoxia for most patients.<ref name="Sweeney2013">{{Cite journal |last=Sweeney |first=Deborah F. |year=2013 |title=Have Silicone Hydrogel Lenses Eliminated Hypoxia? |journal=Eye & Contact Lens: Science & Clinical Practice |volume=39 |issue=1 |pages=53–60 |doi=10.1097/ICL.0b013e31827c7899 |pmid=23271474 |s2cid=205659587}}</ref> |
|||
While daily disposable lenses require no cleaning, other types require regular cleaning and disinfecting in order to retain clear vision and prevent discomfort and infections by various [[microorganism]]s including [[bacteria]], [[fungi]], and ''[[Acanthamoeba]]'', that form a [[biofilm]] on the lens surface. There are a lot of products that are used to cleans contact lenses: |
|||
* Multipurpose solutions – The most popular cleaning solution{{Clarify|date=January 2011}} for contact lenses; these are suitable for rinsing, disinfecting, cleaning and storing lenses, and in most cases eliminate the need for protein removal enzyme tablets. Some multipurpose solutions are not effective at disinfecting ''[[Acanthamoeba]]'' from the lens.<ref name="hiti">{{Cite journal |
|||
| last1 = Hiti| first1 = K |
|||
| last2 = Walochnik| first2 = J |
|||
| last3 = Haller-Schober| first3 = E M |
|||
| last4 = Faschinger | first4 = C |
|||
| last5 = Aspöck | first5 = H |
|||
| title = Viability of Acanthamoeba after exposure to a multipurpose disinfecting contact lens solution and two hydrogen peroxide systems |
|||
| journal = British Journal of Ophthalmology |
|||
| date = February 2002 |
|||
| volume = 86 |
|||
| issue = 2 |
|||
| pages = 144–6 |
|||
| url = http://bjo.bmj.com/cgi/content/abstract/86/2/144 |
|||
| pmid = 11815336 |
|||
| doi = 10.1136/bjo.86.2.144 |
|||
| pmc = 1771011 |
|||
| postscript = <!--None--> |
|||
}}</ref> In May 2007, one brand of multipurpose solution was recalled due to a cluster of ''Acanthamoeba'' infections.<ref name="cdcAMOrecall">[http://www2a.cdc.gov/HAN/ArchiveSys/ViewMsgV.asp?AlertNum=00260 Early Report of Serious Eye Infections Associated with Soft Contact Lens Solution]. [[Centers for Disease Control and Prevention|CDC]] health advisory. May 25, 2007. CDCHAN-00260-2007-05-25-ADV-N</ref><ref name="mmwr">[http://www.cdc.gov/mmwr/preview/mmwrhtml/mm56d526a1.htm Acanthamoeba Keratitis --- Multiple States, 2005–2007]. Center for Disease Control [http://www.cdc.gov/mmwr/index.html MMWR] dispatch. May 26, 2007 / 56(Dispatch);1–3</ref> Newer generations of multipurpose solutions are effective against bacteria, fungi, and acanthamoeba and are designed to condition the lenses while soaking. |
|||
* [[Saline (medicine)|Saline]] solution – Used for rinsing the lens after cleaning and preparing it for insertion. Saline solutions do not disinfect. |
|||
* Daily cleaner – Used to clean lenses on a daily basis. A few drops of cleaner are applied to the lens while it rests in the palm of the hand, and the lens is rubbed for about 20 seconds with a fingertip (depending on the product) on each side. Long fingernails can damage lenses. |
|||
* [[Hydrogen peroxide]] solution – Used for disinfecting the lenses, and available as 'two-step' or 'one-step' systems. With 'two-step' products, the peroxide must be rinsed away with saline before the lenses may be worn, because hydrogen peroxide is an irritant and strong oxidizer.<ref name="hughes">{{Cite journal |
|||
| last1 = Hughes | first1 = Reanne |
|||
| last2 = Kilvington | first2 = Simon |
|||
| title = Comparison of Hydrogen Peroxide Contact Lens Disinfection Systems and Solutions against Acanthamoeba polyphaga |
|||
| journal = Antimicrobial Agents and Chemotherapy |
|||
| date = July 2001 |
|||
| volume = 45 |
|||
| issue = 7 |
|||
| pages = 2038–43 |
|||
| url = http://aac.asm.org/cgi/content/full/45/7/2038 |
|||
| pmid = 11408220 |
|||
| doi = 10.1128/AAC.45.7.2038-2043.2001 |
|||
| pmc = 90597 |
|||
| postscript = <!--None--> |
|||
}}</ref> |
|||
* Enzymatic cleaner – Used for cleaning protein deposits off lenses, usually weekly, if the daily cleaner is not sufficient. Typically, this cleaner is in tablet form. Protein deposits make use of contact lenses uncomfortable, and may lead to various eye problems. |
|||
* Ultraviolet, vibration or ultrasonic devices – Used to both disinfect and clean contact lenses. The lenses are inserted inside the portable device (running on batteries and/or plug-in) for 2 to 6 minutes during which both the microorganisms and protein build-up are thoroughly cleaned. Saline solution is typically used as multi-purpose solutions are not necessary. These devices are not usually available in optic retailers but are in some electro-domestic stores.<ref>{{Cite journal |
|||
| title = How Optical Ultrasonic Cleaners Work |
|||
| url = http://www.tech-faq.com/how-optical-ultrasonic-cleaners-work.html |
|||
}}</ref><ref>{{Cite journal |
|||
| last1 = White | first1 = Gina |
|||
| title = Caring for Soft Contact Lenses |
|||
| url = http://www.allaboutvision.com/contacts/caresoftlens.htm |
|||
}}</ref><ref>{{Cite journal |
|||
| last1 = Ward | first1 = Michael |
|||
| title = Soft Contact Lens Care Products |
|||
| url = http://www.clspectrum.com/article.aspx?article=12384 |
|||
}}</ref> |
|||
Mishandling of contact lenses can also cause problems. [[Corneal abrasion]]s can increase the chances of infection.<ref name="Corneal Abrasion in Emergency Medicine">{{Cite journal |last=Khan |first=Feras H |date=2023-04-13 |title=Emergency Care of Corneal Abrasion: Overview, Clinical Evaluation, ED Treatment Considerations |url=https://emedicine.medscape.com/article/799316-overview |access-date=2024-08-25 |website=Medscape Reference}}</ref> When combined with improper cleaning and disinfection of the lens, a risk of infection further increases. Decreased corneal sensitivity after extended contact lens wear may cause a patient to miss some of the earliest symptoms of such complications.<ref name="The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity">{{Cite journal |last=Liu |first=Z. |last2=Pflugfelder, S. |date=January 2000 |title=The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity |journal=Ophthalmology |volume=107 |issue=1 |pages=105–111 |doi=10.1016/S0161-6420(99)00027-5 |pmid=10647727}}</ref> |
|||
Some products must only be used with certain types of contact lenses. Water alone will not adequately disinfect the lens, and can lead to lens contamination and has been known in some cases to cause irreparable harm to the eye.<ref>[http://www.lenstore.co.uk/lens-wearing-guide Contact Lens Wearing Guide]</ref> Proper lens cleaning is important in warding off biofilm formation. |
|||
The way contact lenses interact with the natural tear layer is a major factor in determining lens comfort and visual clarity. People with [[Keratoconjunctivitis sicca|dry eyes]] are particularly vulnerable to discomfort and episodes of brief blurry vision. Proper lens selection can minimize these effects. |
|||
To keep the cleaning product as clean as possible, and to counteract minor contamination of the product and kill microorganisms on the contact lens, some products contain [[preservative]]s such as [[thiomersal]], [[benzalkonium chloride]], and [[benzyl alcohol]]. In 1989, thiomersal was responsible for about 10% of problems related to contact lenses:<ref>{{cite journal | pmid = 2630335 | year = 1989 | last1 = Wilson-Holt | first1 = N | last2 = Dart | first2 = JK | title = Thiomersal keratoconjunctivitis, frequency, clinical spectrum and diagnosis | volume = 3 ( Pt 5) | pages = 581–7 | journal = Eye (London, England)}}</ref> because of this, many products no longer contain thiomersal. Preservative-free products usually have shorter [[shelf life|shelf lives]]. For example, non-aerosol preservative-free saline solutions can typically be used for only two weeks once opened. The introduction of silicone-hydrogel soft contact lens materials in 1999 made selection of the proper disinfecting solution more important. |
|||
[[Effects of long-term contact lens wear on the cornea|Long-term wear]] (over five years) of contact lenses may "decrease the entire corneal thickness and increase the corneal curvature and surface irregularity."<ref name="pmid10647727">{{Cite journal |vauthors=Liu Z, Pflugfelder SC |date=January 2000 |title=The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity |journal=[[Ophthalmology (journal)|Ophthalmology]] |volume=107 |issue=1 |pages=105–11 |doi=10.1016/S0161-6420(99)00027-5 |pmid=10647727}}</ref> Long-term wear of rigid contacts is associated with decreased [[corneal keratocyte]] density<ref name="pmid16303530">{{Cite journal |vauthors=Hollingsworth JG, Efron N |date=June 2004 |title=Confocal microscopy of the corneas of long-term rigid contact lens wearers |journal=[[Cont Lens Anterior Eye]] |volume=27 |issue=2 |pages=57–64 |doi=10.1016/j.clae.2004.02.002 |pmid=16303530 |doi-access=free}}</ref> and increased number of [[corneal epithelium|epithelial]] [[Langerhans cells]].<ref name="pmid17198013">{{Cite journal |vauthors=Zhivov A, Stave J, Vollmar B, Guthoff R |date=January 2007 |title=''In vivo'' confocal microscopic evaluation of langerhans cell density and distribution in the corneal epithelium of healthy volunteers and contact lens wearers |journal=[[Cornea]] |volume=26 |issue=1 |pages=47–54 |doi=10.1097/ICO.0b013e31802e3b55 |pmid=17198013 |s2cid=22951471}}</ref> |
|||
All contact lenses sold in the United States are studied and approved as safe by the FDA when specific handling and care procedures, wear schedules, and replacement schedules are followed. |
|||
==Current research== |
==Current research== |
||
Contact lens sensors to monitor the ocular temperature have been demonstrated.<ref>{{Cite journal |vauthors=Moreddu R, Elsherif M, Butt H, Vigolo D, Yetisen AK |year=2019 |title=Contact lenses for continuous corneal temperature monitoring |url=http://pure-oai.bham.ac.uk/ws/files/60402992/c9ra00601j.pdf |journal=RSC Advances |volume=9 |issue=20 |pages=11433–11442 |bibcode=2019RSCAd...911433M |doi=10.1039/C9RA00601J |pmc=9063335 |pmid=35520262 |doi-access=free}}</ref> Monitoring [[intraocular pressure]] with contact lens sensors is another area of contact lens research.<ref>{{Cite journal |last=Baghban |first=R |last2=Talebnejad |first2=MR |last3=Meshksar |first3=A |last4=Heydari |first4=M |last5=Khalili |first5=MR |date=2 November 2023 |title=Recent advancements in nanomaterial-laden contact lenses for diagnosis and treatment of glaucoma, review and update. |journal=Journal of Nanobiotechnology |volume=21 |issue=1 |pages=402 |doi=10.1186/s12951-023-02166-w |pmc=10621182 |pmid=37919748 |doi-access=free}}</ref> |
|||
A large segment of current contact lens research is directed towards the treatment and prevention of conditions resulting from contact lens contamination and colonization by foreign organisms. It is generally accepted by clinicians that the most significant complication of contact lens wear is microbial [[keratitis]] and that the most predominant microbial pathogen is ''[[Pseudomonas aeruginosa]]''.<ref>Robertson, DM, Petroll, WM, Jester, JV & Cavanagh, HD: Current concepts: contact lens related Pseudomonas keratitis. ''Cont Lens Anterior Eye'', 30: 94–107, 2007.</ref> Other organisms are also major causative factors in bacterial keratitis associated with contact lens wear, although their prevalence varies across different locations. These include both the ''[[Staphylococcus]]'' species (''aureus'' and ''epidermidis'') and the ''[[Streptococcus]]'' species, among others.<ref>Sharma, S, Kunimoto, D, Rao, N, Garg, P & Rao, G: Trends in antibiotic resistance of corneal pathogens: Part II. An analysis of leading bacterial keratitis isolates, 1999.</ref><ref>Verhelst D, Koppen C, Looveren JV, Meheus A, Tassignon M (2005) Clinical, epidemiological and cost aspects of contact lens related infectious keratitis in Belgium: results of a seven-year retrospective study. ''Bull Soc Belge Ophtalmol'' 297:7–15.</ref> Microbial keratitis is a serious focal point of current research due to its potentially devastating effect on the eye, including severe vision loss.<ref>Burd EM, Ogawa GSH, Hyndiuk RA. Bacterial keratitis and conjunctivitis. In: Smolin G, Thoft RA, editors. '''The Cornea'''. ''Scientific Foundations and Clinical Practice''. 3rd ed. Boston: Little, Brown, & Co, 1994. p 115–67.</ref> |
|||
A large segment of current contact lens research is directed towards the treatment and prevention of conditions resulting from contact lens contamination and colonization by foreign organisms. Clinicians tend to agree that the most significant complication of contact lens wear is microbial [[keratitis]] and that the most predominant microbial pathogen is ''[[Pseudomonas aeruginosa]]''.<ref>Robertson, DM, Petroll, WM, Jester, JV & Cavanagh, HD: Current concepts: contact lens related Pseudomonas keratitis. ''Cont Lens Anterior Eye'', 30: 94–107, 2007.</ref> Other organisms are also major causative factors in bacterial keratitis associated with contact lens wear, although their prevalence varies across different locations. These include both the ''[[Staphylococcus]]'' species (''aureus'' and ''epidermidis'') and the ''[[Streptococcus]]'' species, among others.<ref>Sharma, S, Kunimoto, D, Rao, N, Garg, P & Rao, G: Trends in antibiotic resistance of corneal pathogens: Part II. An analysis of leading bacterial keratitis isolates, 1999.</ref><ref>{{Cite journal |vauthors=Verhelst D, Koppen C, Looveren JV, Meheus A, Tassignon M |year=2005 |title=Clinical, epidemiological and cost aspects of contact lens related infectious keratitis in Belgium: results of a seven-year retrospective study |journal=Bull Soc Belge Ophtalmol |volume=297 |issue=297 |pages=7–15 |pmid=16281729}}</ref> Microbial keratitis is a serious focal point of current research due to its potentially devastating effect on the eye, including severe vision loss.<ref>Burd EM, Ogawa GSH, Hyndiuk RA. Bacterial keratitis and conjunctivitis. In: Smolin G, Thoft RA, editors. '''The Cornea'''. ''Scientific Foundations and Clinical Practice''. 3rd ed. Boston: Little, Brown, & Co, 1994. p 115–67.</ref> |
|||
One specific research topic of interest is how microbes such as ''[[Pseudomonas aeruginosa]]'' invade the eye and cause infection. Although the pathogenesis of microbial keratitis is not well understood, many different factors have been investigated. One group of researchers showed that corneal hypoxia exacerbated ''Pseudomonas'' binding to the corneal epithelium, internalization of the microbes, and induction of the inflammatory response.<ref>Zaidi, T, Mowrey-McKee, M & Pier, GB: Hypoxia increases corneal cell expression of CFTR leading to increased Pseudomonas aeruginosa binding, internalization, and initiation of inflammation. ''Invest Ophthalmol Vis Sci'', 45: 4066–74, 2004.</ref> One way to alleviate [[Hypoxia (medical)|hypoxia]] is to increase the amount of oxygen transmitted to the cornea. Although silicone-hydrogel lenses almost eliminate hypoxia in patients due to their very high levels of oxygen transmissibility,<ref>Sweeney DF, Keay L, Jalbert I. Clinical performance of silicone hydrogel lenses. In Sweeney DF, ed. ''Silicone Hydrogels: The Rebirth of Continuous Wear Contact Lenses.'' Woburn, Ma: Butterworth Heinemann; 2000.</ref> they also seem to provide a more efficient platform for bacterial contamination and corneal infiltration than other conventional hydrogel soft contact lenses. A recent study showed that ''[[Pseudomonas aeruginosa]]'' and ''[[Staphylococcus epidermis]]'' adhere much more strongly to silicone hydrogel contact lenses than conventional hydrogel contact lenses and that adhesion of Pseudomonas aeruginosa was 20 times stronger than adhesion of Staphylococcus epidermidis.<ref>Kodjikian, L, Casoli-Bergeron, E, Malet, F, Janin-Manificat, H, Freney, J, Burillon, C, Colin, J & Steghens, JP: Bacterial adhesion to conventional hydrogel and new silicone hydrogel contact lens materials. ''Graefes Arch Clin Exp Ophthalmol'', 246: 267–73, 2008.</ref> This might help to explain one reason why Pseudomonas infections are the most predominant. |
|||
One specific research topic of interest is how microbes such as ''Pseudomonas aeruginosa'' invade the eye and cause infection. Although the pathogenesis of microbial keratitis is not well understood, many different factors have been investigated. One group of researchers showed that corneal hypoxia exacerbated ''Pseudomonas'' binding to the corneal epithelium, internalization of the microbes, and induction of the inflammatory response.<ref>{{Cite journal |vauthors=Zaidi T, Mowrey-McKee M, Pier GB |year=2004 |title=Hypoxia increases corneal cell expression of CFTR leading to increased Pseudomonas aeruginosa binding, internalization, and initiation of inflammation |journal=Invest Ophthalmol Vis Sci |volume=45 |issue=11 |pages=4066–74 |doi=10.1167/iovs.04-0627 |pmc=1317302 |pmid=15505057}}</ref> One way to alleviate [[Hypoxia (medical)|hypoxia]] is to increase the amount of oxygen transmitted to the cornea. Although silicone-hydrogel lenses almost eliminate hypoxia in patients due to their very high levels of oxygen transmissibility,<ref>Sweeney DF, Keay L, Jalbert I. Clinical performance of silicone hydrogel lenses. In Sweeney DF, ed. ''Silicone Hydrogels: The Rebirth of Continuous Wear Contact Lenses.'' Woburn, Ma: Butterworth Heinemann; 2000.</ref> they also seem to provide a more efficient platform for bacterial contamination and corneal infiltration than other conventional hydrogel soft contact lenses. One study showed that ''Pseudomonas aeruginosa'' and ''[[Staphylococcus epidermidis]]'' adhere much more strongly to unworn silicone hydrogel contact lenses than conventional hydrogel lenses and that adhesion of ''Pseudomonas aeruginosa'' was 20 times stronger than that of ''Staphylococcus epidermidis''.<ref>{{Cite journal |vauthors=Kodjikian L, Casoli-Bergeron E, Malet F, Janin-Manificat H, Freney J, Burillon C, Colin J, Steghens JP |year=2008 |title=Bacterial adhesion to conventional hydrogel and new silicone hydrogel contact lens materials |journal=Graefes Arch Clin Exp Ophthalmol |volume=246 |issue=2 |pages=267–73 |doi=10.1007/s00417-007-0703-5 |pmid=17987309 |s2cid=23218590}}</ref> This might partly explain why ''Pseudomonas'' infections are the most predominant. However, another study conducted with worn and unworn silicone and conventional hydrogel contact lenses showed that worn silicone contact lenses were less prone to ''Staphylococcus epidermidis'' colonization than conventional hydrogel lenses.<ref name="Santos2008">{{Cite journal |last=Santos |first=Lívia |last2=Rodrigues |first2=Diana |last3=Lira |first3=Madalena |last4=Real Oliveira |first4=M Elisabete C. D. |last5=Oliveira |first5=Rosário |last6=Vilar |first6=Eva Yebra-Pimente |last7=Azeredo |first7=Joana |date=July 2008 |title=Bacterial Adhesion to Worn Silicone Hydrogel Contact Lenses |journal=Optometry and Vision Science |volume=85 |issue=7 |pages=520–525 |doi=10.1097/OPX.0b013e31817c92f3 |pmid=18594343 |s2cid=10171270 |hdl-access=free |hdl=1822/8740}}</ref> |
|||
Another important area of contact lens research deals with patient compliance. Compliance is a major issue surrounding the use of contact lenses because patient noncompliance often leads to contamination of the lens, storage case, or both.<ref>Yung MS, Boost M, Cho P, Yap M. Microbial contamination of contact lenses and lens care accessories of soft contact lens wearers (university students) in Hong Kong. ''Ophthalmic and Physiological Optics'', 2007 Jan;27(1):11–21.</ref><ref>J. Midelfart, A. Midelfart and L. Bevanger, Microbial contamination of contact lens cases among medical students, ''CLAO'' J 22 (1996) (1), pp. 21–24.</ref><ref>T.B. Gray, R.T. Cursons, J.F. Sherwan and P.R. Rose, Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases, ''Br J Ophthalmol'' 79 (1995), pp. 601–605.</ref> The introduction of multipurpose solutions and daily disposable lenses have helped to alleviate some of the problems observed from inadequate cleaning but new methods of combating microbial contamination are currently being developed. A [[silver]]-impregnated lens case has been developed which helps to eradicate any potentially contaminating microbes that come in contact with the lens case.<ref>Amos, CF & George, MD: Clinical and laboratory testing of a silver-impregnated lens case. ''Cont Lens Anterior Eye'', 29: 247–55, 2006.</ref> Additionally, a number of [[antimicrobial]] agents are being developed that have been embedded into contact lenses themselves. Contact lenses with covalently attached [[Selenium]] molecules have been shown to reduce bacterial colonization without adversely affecting the cornea of a rabbit eye<ref>Mathews, SM, Spallholz, JE, Grimson, MJ, Dubielzig, RR, Gray, T & Reid, TW: Prevention of bacterial colonization of contact lenses with covalently attached selenium and effects on the rabbit cornea. ''Cornea'', 25: 806–14, 2006.</ref> and octylglucoside used as a contact lens surfactant significantly decreases bacterial adhesion.<ref>Santos, L, Rodrigues, D, Lira, M, Oliveira, R, Real Oliveira, ME, Vilar, EY & Azeredo, J: The effect of octylglucoside and sodium cholate in Staphylococcus epidermidis and Pseudomonas aeruginosa adhesion to soft contact lenses. ''Optom Vis Sci'', 84: 429–34, 2007.</ref> These compounds are of particular interest to contact lens manufacturers and prescribing optometrists because they do not require any patient compliance to effectively attenuate the effects of bacterial colonization. |
|||
Besides bacterial adhesion and cleaning, micro and nano pollutants (biological and manmade) is an area of contact lens research that is growing. Small physical pollutants ranging from [[Microplastics|nanoplastics]] to fungi spores to plant pollen adhere to contact lens surfaces in high concentrations. It has been found that multipurpose solution and rubbing with fingers does not significantly clean the lenses. A group of researchers have suggested an alternative cleaning solution, PoPPR (polymer on polymer pollution removal).<ref>{{Cite journal |last=Burgener |first=Katherine |last2=Bhamla |first2=M. Saad |date=June 2021 |title=A polymer-based technique to remove pollutants from soft contact lenses |journal=Contact Lens and Anterior Eye |volume=44 |issue=3 |pages=101335 |arxiv=2005.08732 |doi=10.1016/j.clae.2020.05.004 |pmid=32444249 |s2cid=218673928}}</ref> This cleaning technique takes advantage of a soft and porous polymer to physically peel pollutants off of contact lenses. |
|||
Another important area of contact lens research deals with patient compliance. Compliance is a major issue<ref>{{Cite journal |last=Agarwal R.K. |year=1971 |title=A legally problematical but clinically interesting contact lens case |journal=The Contact Lens |volume=3 |issue=3 |page=13}}</ref> pertaining to the use of contact lenses because patient noncompliance often leads to contamination of the lens, storage case, or both.<ref>{{Cite journal |vauthors=Yung MS, Boost M, Cho P, Yap M |year=2007 |title=Microbial contamination of contact lenses and lens care accessories of soft contact lens wearers (university students) in Hong Kong |journal=Ophthalmic and Physiological Optics |volume=27 |issue=1 |pages=11–21 |doi=10.1111/j.1475-1313.2006.00427.x |pmid=17239186 |s2cid=6552480 |hdl-access=free |hdl=10397/22844}}</ref><ref>{{Cite journal |last=Midelfart J. |last2=Midelfart A. |last3=Bevanger L. |year=1996 |title=Microbial contamination of contact lens cases among medical students |journal=CLAO J |volume=22 |issue=1 |pages=21–24 |pmid=8835064}}</ref><ref>{{Cite journal |last=Gray T.B. |last2=Cursons R.T. |last3=Sherwan J.F. |last4=Rose P.R. |year=1995 |title=Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases |journal=Br J Ophthalmol |volume=79 |issue=6 |pages=601–605 |doi=10.1136/bjo.79.6.601 |pmc=505174 |pmid=7626578}}</ref> However, careful users can extend the wear of lenses through proper handling: there is, unfortunately, no disinterested research on the issue of "compliance" or the length of time a user can safely wear a lens beyond its stated use. The introduction of multipurpose solutions and daily disposable lenses have helped to alleviate some of the problems observed from inadequate cleaning but new methods of combating microbial contamination are currently being developed. A [[silver]]-impregnated lens case has been developed which helps to eradicate any potentially contaminating microbes that come in contact with the lens case.<ref>{{Cite journal |vauthors=Amos CF, George MD |year=2006 |title=Clinical and laboratory testing of a silver-impregnated lens case |journal=Cont Lens Anterior Eye |volume=29 |issue=5 |pages=247–55 |doi=10.1016/j.clae.2006.09.007 |pmid=17084102}}</ref> Additionally, a number of [[antimicrobial]] agents are being developed that have been embedded into contact lenses themselves. Lenses with covalently attached [[selenium]] molecules have been shown to reduce bacterial colonization without adversely affecting the cornea of a rabbit eye<ref>{{Cite journal |vauthors=Mathews SM, Spallholz JE, Grimson MJ, Dubielzig RR, Gray T, Reid TW |year=2006 |title=Prevention of bacterial colonization of contact lenses with covalently attached selenium and effects on the rabbit cornea |journal=Cornea |volume=25 |issue=7 |pages=806–14 |doi=10.1097/01.ico.0000224636.57062.90 |pmid=17068458 |s2cid=25006245}}</ref> and [[octyl glucoside]] used as a lens surfactant significantly decreases bacterial adhesion.<ref>{{Cite journal |last=Santos L |last2=Rodrigues D |last3=Lira M |last4=Oliveira R |last5=Oliveira Real, ME |last6=Vilar EY |last7=Azeredo J |year=2007 |title=The effect of octylglucoside and sodium cholate in Staphylococcus epidermidis and Pseudomonas aeruginosa adhesion to soft contact lenses |journal=Optom Vis Sci |volume=84 |issue=5 |pages=429–34 |doi=10.1097/opx.0b013e318058a0cc |pmid=17502827 |s2cid=2509161 |hdl-access=free |hdl=1822/6663}}</ref> These compounds are of particular interest to contact lens manufacturers and prescribing optometrists because they do not require any patient compliance to effectively attenuate the effects of bacterial colonization. |
|||
One area of research is in the field of [[Bionic contact lens|bionic lenses]]. These are visual displays that include built-in electric circuits and [[light-emitting diodes]] and can harvest radio waves for their electric power. Bionic lenses can display information beamed from a mobile device overcoming the small display size problem. The technology involves embedding nano and microscale electronic devices in lenses. These lenses will also need to have an array of microlenses to focus the image so that it appears suspended in front of the wearer's eyes. The lens could also serve as a head-up display for pilots or gamers.<ref name="lc" /> |
|||
Drug administration through contact lenses is also becoming an area of research. One application is a lens that releases anesthesia to the eye for post-surgery pain relief, especially after PRK ([[photorefractive keratectomy]]) in which the healing process takes several days. One experiment shows that silicone contact lenses that contain vitamin E deliver pain medication for up to seven days compared with less than two hours in usual lenses.<ref name="lc">{{Cite web |title=Contacts Release Anesthesia to Eyes of Post-Surgery Patients |url=http://www.lenscompare.co.uk/compare-contact-lenses-latest-research/ |url-status=dead |archive-url=https://archive.today/20130421013228/http://www.lenscompare.co.uk/compare-contact-lenses-latest-research/ |archive-date=21 April 2013 |access-date=4 April 2013 |df=dmy-all}}</ref> |
|||
Another study of the usage of contact lens is aimed to address the issue of [[macular degeneration]] (AMD or age-related macular degeneration). An international collaboration of researchers was able to develop a contact lens that can shift between magnified and normal vision. Previous solutions to AMD included bulky glasses or surgical implants. But the development of this new contact lens, which is made of polymethyl methacrylate, could offer an unobtrusive solution.<ref>{{Cite web |title=First Ever Switchable Telescopic Contact Lens |url=https://www.forbes.com/sites/meriameberboucha/2018/02/28/first-ever-switchable-telescopic-contact-lens/ |access-date=23 March 2018 |website=[[Forbes]]}}</ref> |
|||
==In popular culture== |
|||
===Films=== |
|||
[[File:Dracula 1958 c.jpg|thumb|alt=Film still of Christopher Lee wearing red contact lenses|[[Christopher Lee]] as the title character in ''[[Dracula (1958 film)|Dracula]]'' (1958) in one of the first uses of contact lens with makeup in films]] |
|||
One of the earliest known [[motion pictures]] to introduce the use of contact lenses as a [[make-up artist]]'s device for enhancing the eyes was by the innovative actor [[Lon Chaney]] in the 1926 film ''[[The Road to Mandalay (1926 film)|The Road to Mandalay]]'' to create the effect of a character who had a blind eye.<ref>{{Cite book |last=Klepper |first=Robert K. |title=Silent Films, 1877–1996: A Critical Guide to 646 Movies |publisher=McFarland |year=2005 |pages=373}}</ref> Dr. [[Rueben Greenspoon]] applied them to Orson Welles for the film ''[[Citizen Kane]]'' in 1940. In the 1950s, contact lenses were starting to be used in British color horror films. An early example of this is the British actor [[Christopher Lee]] as the [[Dracula]] character in the 1958 color horror film ''[[Dracula (1958 film)|Dracula]]'', which helped to emphasize his horrific looking black [[pupils]] and red [[red eye (medicine)|bloodshot eyes]]. [[Tony Curtis]] wore them in the 1968 film ''[[The Boston Strangler (film)|The Boston Strangler]]''. Contact lenses were also used to better emphasize the sinister gaze of the demonic characters in 1968's ''[[Rosemary's Baby (film)|Rosemary's Baby]]'' and 1973's ''[[The Exorcist (film)|The Exorcist]]''. Colored custom-made contact lenses are now standard makeup for a number of special effects-based movies.<ref>{{Cite news |last=Yazigi |first=Monique P. |date=July 17, 1994 |title=On Film, Them There Eyes Are Often Contact Lenses. |url=https://www.nytimes.com/1994/07/17/movies/film-on-film-them-there-eyes-are-often-contact-lenses.html |work=New York Times}}</ref> |
|||
==Further reading== |
|||
* {{Cite journal |last=Demas GN |year=1989 |title=pH consistency and stability of contact lens solutions |journal=J Am Optom Assoc |volume=60 |issue=10 |pages=732–4 |pmid=2584587 |quote=The pH of contact lens solutions has been implicated in the comfort of contact lenses on insertion.}} |
|||
* {{Cite web |title=Eye Care |url=http://www.contactlensheaven.com/eyecare.html |access-date=20 November 2014 |publisher=CLH}} |
|||
* {{Cite web |title=How to Put Contacts in Your Eyes |url=http://coopervision.com/about-contacts/how-put-contacts-your-eyes |access-date=20 November 2014 |publisher=CooperVision |quote=use plain soap without any heavy moisturizers or perfumes. Rinse well and dry your hands. Again, this is to prevent transmitting anything unwanted to your eyes.}} |
|||
==See also== |
==See also== |
||
{{Columns-list|colwidth=30em| |
|||
* [[Augmented reality contact lens]] |
|||
* [[Bionic contact lens]] |
* [[Bionic contact lens]] |
||
* [[Effects of long-term contact lens wear on the cornea]] |
|||
* [[Corrective lens]] |
|||
* [[Eyeglass prescription]] |
* [[Eyeglass prescription]] |
||
* [[Fungal contamination of contact lenses]] |
|||
* [[List of soft contact lens materials]] |
|||
* [[Visual acuity]] |
* [[Visual acuity]] |
||
}} |
|||
* [[Bates method]] |
|||
{{Clear}} |
|||
* [[Effects of Long-Term Contact Lens Wear on the Cornea]] |
|||
* [http://bodywonders.com/advantage-and-disadvantage-of-contact-lenses Advantage and Disadvantage of contact lenses] |
|||
==References== |
==References== |
||
{{Reflist| |
{{Reflist|30em}} |
||
==Further reading== |
==Further reading== |
||
* Efron, Nathan (2002). ''Contact Lens Practice'' |
* [[Nathan Efron|Efron, Nathan]] (2002). ''[https://books.google.com/books?id=U9Q6NK661pwC Contact Lens Practice]''. Elsevier Health Sciences. {{ISBN|0-7506-4690-X}}. |
||
* Heitz, Robert (2003, 2005 and 2014). "The History of Contact Lenses". In: Julius Hirschberg, ''History of Ophthalmology'', vols. 11/3a, 11/3b, and 11/3c. Ostend, Belgium: Wayenborgh Publishing; Paraguay: Piribebuy. {{ISBN|978-90-6299-463-2}}. |
|||
==External links== |
==External links== |
||
{{Commons}} |
|||
{{commons|Contact lens}} |
|||
<!-- Do not add links to commercial organisations here. They will be removed. For more information, see Wikipedia's policy on external links at [[WP:EL]] --> |
<!-- Do not add links to commercial organisations here. They will be removed. For more information, see Wikipedia's policy on external links at [[WP:EL]] --> |
||
* [http://www.bcla.org.uk/home.asp British Contact Lens Association] |
|||
* [http://www.contactlenseswithoutprescription.org/ Contact Lenses without Prescription] |
|||
* [http://intl.elsevierhealth.com/journals/clae/ ''Contact Lens & Anterior Eye'' Journal] |
|||
* [http://youtube.com/watch?v=62tha1Kxa2c Video] How Contact Lenses are Manufactured |
|||
* [http://www.andrewgasson.co.uk/contact_lens_history.htm Contact Lens History] |
|||
* [http://www.healthlinksbc.org/kb/content/otherdetail/aa126875.html Contact lenses treatment overview] |
|||
* [http://www.journals.elsevier.com/contact-lens-and-anterior-eye Contact lens and anterior eye journal] |
|||
{{DEFAULTSORT:Contact Lens}} |
|||
* [https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm048893.htm Focusing on Contact Lens Safety] from [[Food and Drug Administration]] |
|||
{{Eyewear}} |
|||
{{Authority control}} |
|||
[[Category:Contact lenses| ]] |
[[Category:Contact lenses| ]] |
||
[[Category:1965 introductions]] |
|||
[[Category:Articles containing video clips]] |
|||
[[Category:Corrective lenses]] |
[[Category:Corrective lenses]] |
||
[[Category:Optometry]] |
[[Category:Optometry]] |
||
[[Category: |
[[Category:19th-century inventions]] |
||
[[ar:عدسات لاصقة]] |
|||
[[bg:Контактна леща]] |
|||
[[ca:Lent de contacte]] |
|||
[[cs:Kontaktní čočka]] |
|||
[[da:Kontaktlinse]] |
|||
[[de:Kontaktlinse]] |
|||
[[el:Φακός επαφής]] |
|||
[[es:Lente de contacto]] |
|||
[[eo:Kontaktlenso]] |
|||
[[fa:عدسک]] |
|||
[[fr:Lentilles de contact]] |
|||
[[ko:콘택트 렌즈]] |
|||
[[hi:कॉण्टैक्ट लैंस]] |
|||
[[hr:Kontaktne leće]] |
|||
[[id:Lensa kontak]] |
|||
[[it:Lente a contatto]] |
|||
[[he:עדשות מגע]] |
|||
[[kn:ಕಾಂಟ್ಯಾಕ್ಟ್ ಲೆನ್ಸ್(ಸಂಪರ್ಕ ಮಸೂರ)]] |
|||
[[lt:Kontaktiniai lęšiai]] |
|||
[[hu:Kontaktlencse]] |
|||
[[ms:Kanta lekap]] |
|||
[[nl:Contactlens]] |
|||
[[ja:コンタクトレンズ]] |
|||
[[no:Kontaktlinse]] |
|||
[[nn:Kontaktlinse]] |
|||
[[pl:Soczewka kontaktowa]] |
|||
[[pt:Lente de contato]] |
|||
[[ru:Контактные линзы]] |
|||
[[simple:Contact lens]] |
|||
[[sk:Kontaktná šošovka]] |
|||
[[sr:Контактна сочива]] |
|||
[[sh:Kontaktne leće]] |
|||
[[fi:Piilolinssi]] |
|||
[[sv:Kontaktlins]] |
|||
[[ta:தொடு வில்லை]] |
|||
[[th:เลนส์สัมผัส]] |
|||
[[tr:Kontakt lens]] |
|||
[[vi:Kính áp tròng]] |
|||
[[zh:隱形眼鏡]] |
|||
Latest revision as of 20:18, 1 December 2024


Contact lenses, or simply contacts, are thin lenses placed directly on the surface of the eyes. Contact lenses are ocular prosthetic devices used by over 150 million people worldwide,[1] and they can be worn to correct vision or for cosmetic or therapeutic reasons.[2] In 2010, the worldwide market for contact lenses was estimated at $6.1 billion, while the US soft lens market was estimated at $2.1 billion.[3] Multiple analysts estimated that the global market for contact lenses would reach $11.7 billion by 2015.[3] As of 2010,[update] the average age of contact lens wearers globally was 31 years old, and two-thirds of wearers were female.[4]
People choose to wear contact lenses for many reasons.[5] Aesthetics and cosmetics are main motivating factors for people who want to avoid wearing glasses or to change the appearance or color of their eyes.[6] Others wear contact lenses for functional or optical reasons.[7] When compared with spectacles, contact lenses typically provide better peripheral vision, and do not collect moisture (from rain, snow, condensation, etc.) or perspiration. This can make them preferable for sports and other outdoor activities. Contact lens wearers can also wear sunglasses, goggles, or other eye wear of their choice without having to fit them with prescription lenses or worry about compatibility with glasses. Additionally, there are conditions such as keratoconus and aniseikonia that are typically corrected better with contact lenses than with glasses.[8]
History
[edit]Origins and first functional prototypes
[edit]
Leonardo da Vinci is frequently credited with introducing the idea of contact lenses in his 1508 Codex of the eye, Manual D,[9] wherein he described a method of directly altering corneal power by either submerging the head in a bowl of water or wearing a water-filled glass hemisphere over the eye. Neither idea was practically implementable in da Vinci's time.[10]: 9 He did not suggest his idea be used for correcting vision; he was more interested in exploring mechanisms of accommodation.[9]
Descartes proposed a device for correcting vision consisting of a liquid-filled glass tube capped with a lens. However, the idea was impracticable, since the device was to be placed in direct contact with the cornea and thus would have made blinking impossible.[11]
In 1801, Thomas Young fashioned a pair of basic contact lenses based on Descartes' model. He used wax to affix water-filled lenses to his eyes, neutralizing their refractive power, which he corrected with another pair of lenses.[10][11]
John Herschel, in a footnote to the 1845 edition of the Encyclopedia Metropolitana, posed two ideas for the visual correction: the first "a spherical capsule of glass filled with animal jelly",[12] the second "a mould of the cornea" that could be impressed on "some sort of transparent medium".[13] Though Herschel reportedly never tested these ideas, they were later advanced by independent inventors, including Hungarian physician Joseph Dallos, who perfected a method of making molds from living eyes.[14] This enabled the manufacture of lenses that, for the first time, conformed to the actual shape of the eye.[15]

Although Louis J. Girard invented a scleral contact lens in 1887,[16] it was German ophthalmologist Adolf Gaston Eugen Fick who in 1888 fabricated the first successful afocal scleral contact lens.[17] Approximately 18–21 mm (0.71–0.83 in) in diameter, the heavy blown-glass shells rested on the less sensitive rim of tissue surrounding the cornea and floated on a dextrose solution. He experimented with fitting the lenses initially on rabbits, then on himself, and lastly on a small group of volunteers, publishing his work, "Contactbrille", in the March 1888 edition of Archiv für Augenheilkunde.[18] Large and unwieldy, Fick's lens could be worn only for a couple of hours at a time.[19] August Müller of Kiel, Germany, corrected his own severe myopia with a more convenient blown-glass scleral contact lens of his own manufacture in 1888.[20]
The development of polymethyl methacrylate (PMMA) in the 1930s paved the way for the manufacture of plastic scleral lenses. In 1936, optometrist William Feinbloom introduced a hybrid lens composed of glass and plastic,[21] and in 1937 it was reported that some 3,000 Americans were already wearing contact lenses.[22] In 1939, Hungarian ophthalmologist Dr.István Györffy produced the first fully plastic contact lens.[23] The following year, German optometrist Heinrich Wöhlk produced his own version of plastic lenses based on experiments performed during the 1930s.[24]
Corneal and rigid lenses (1949–1960s)
[edit]In 1949, the first "corneal" lenses were developed.[25][26][27][28] These were much smaller than the original scleral lenses, as they sat only on the cornea rather than across all of the visible ocular surface and could be worn up to 16 hours a day. PMMA corneal lenses became the first contact lenses to have mass appeal through the 1960s, as lens designs became more sophisticated with improving manufacturing technology.[29] On October 18, 1964, in a television studio in Washington, D.C., Lyndon Baines Johnson became the first President in the history of the United States to appear in public wearing contact lenses, under the supervision of Dr. Alan Isen, who developed the first commercially viable soft-contact lenses in the United States.[30][31][32]
Early corneal lenses of the 1950s and 1960s were relatively expensive and fragile, resulting in the development of a market for contact lens insurance. Replacement Lens Insurance, Inc. (now known as RLI Corp.) phased out its original flagship product in 1994 after contact lenses became more affordable and easier to replace.[citation needed]
Gas permeable and soft lenses (1959–present)
[edit]One of the major disadvantages of PMMA lenses is that they allow no oxygen to get through to the conjunctiva and cornea, causing a number of adverse and potentially serious clinical effects. By the end of the 1970s and through the 1980s and 1990s, a range of oxygen-permeable but rigid materials were developed to overcome this problem. Chemist Norman Gaylord played a prominent role in the development of these new oxygen-permeable contact lenses.[33] Collectively, these polymers are referred to as rigid gas permeable or RGP materials or lenses. Though all the above contact lens types—sclerals, PMMAs and RGPs—could be correctly referred to as "rigid" or "hard", the latter term is now used for the original PMMAs, which are still occasionally fitted and worn, whereas "rigid" is a generic term for all these lens types; thus, hard lenses (PMMAs) are a subset of rigid contact lenses. Occasionally, the term "gas permeable" is used to describe RGPs, which is somewhat misleading as soft contact lenses are also gas permeable in that they allow oxygen to get through to the ocular surface.

The principal breakthrough in soft lenses was made by Czech chemists Otto Wichterle and Drahoslav Lím, who published their work "Hydrophilic gels for biological use" in the journal Nature in 1959.[34] In 1965, National Patent Development Corporation (NPDC) bought the American rights to produce the lenses and then sublicensed the rights to Bausch & Lomb, which started to manufacture them in the United States.[35] The Czech scientists' work led to the launch of the first hydrogel contact lenses in some countries in the 1960s and the first approval of the Soflens material by the US Food and Drug Administration (FDA) in 1971. These soft lenses were soon prescribed more often than rigid ones, due to the immediate and much greater comfort (rigid lenses require a period of adaptation before full comfort is achieved). Polymers from which soft lenses are manufactured improved over the next 25 years, primarily in terms of increasing oxygen permeability, by varying the ingredients. In 1972, British optometrist Rishi Agarwal was the first to suggest disposable soft contact lenses.[36][37]
In 1998, the first silicone hydrogel contact lenses were released by Ciba Vision in Mexico. These new materials encapsulated the benefits of silicone which has extremely high oxygen permeability—with the comfort and clinical performance of the conventional hydrogels that had been used for the previous 30 years. These contact lenses were initially advocated primarily for extended (overnight) wear, although more recently, daily (no overnight) wear silicone hydrogels have been launched.
In a slightly modified molecule, a polar group is added without changing the structure of the silicone hydrogel. This is referred to as the Tanaka monomer because it was invented and patented by Kyoichi Tanaka of Menicon Co. of Japan in 1979. Second-generation silicone hydrogels, such as galyfilcon A (Acuvue Advance, Vistakon) and senofilcon A (Acuvue Oasys, Vistakon), use the Tanaka monomer. Vistakon improved the Tanaka monomer even further and added other molecules, which serve as an internal wetting agent.[38]
Comfilcon A (Biofinity, CooperVision) was the first third-generation polymer. Its patent claims that the material uses two siloxy macromers of diverse sizes that, when used in combination, produce very high oxygen permeability for a given water content. Enfilcon A (Avaira, CooperVision) is another third-generation material that is naturally wet; its water content is 46%.[38]
Types
[edit]Contact lenses are classified in diverse ways, namely, by their primary function, material, wear schedule (how long a lens can be worn), and replacement schedule (how long before a lens needs to be discarded).
Functions
[edit]Correction of refractive error
[edit]Corrective contact lenses are designed to improve vision, most commonly by correcting refractive error. This is done by directly focusing light so it enters the eye with the proper power for clear vision.
A spherical contact lens bends light evenly in every direction (horizontally, vertically, etc.). They are typically used to correct myopia and hypermetropia.
There are two ways that contact lenses can correct astigmatism. One way is with toric soft lenses that work essentially the same way as eyeglasses with cylindrical correction; a toric lens has a different focusing power horizontally than vertically, and as a result can correct for astigmatism. Another way is by using a rigid gas permeable lens; since most astigmatism is caused by the shape of the cornea, rigid lenses can improve vision because the front surface of the optical system is the perfectly spherical lens.[39] Both approaches have advantages and drawbacks. Toric lenses must have the proper orientation to correct for astigmatism, so such lenses must have additional design characteristics to prevent them from rotating out of alignment. This can be done by weighting the bottom of the lens or by using other physical characteristics to rotate the lens back into position, but these mechanisms rarely work perfectly, so some misalignment is common and results in somewhat imperfect correction, and blurring of sight after blinking rotates the lens. Toric soft lenses have all the advantages of soft lenses in general, which are low initial cost, ease of fitting, and minimal adjustment period. Rigid gas permeable lenses usually provide superior optical correction but have become less popular relative to soft lenses due to higher initial costs, longer initial adjustment period, and more involved fitting.[40][41]
Correction of presbyopia
[edit]Correction of presbyopia (a need for a reading prescription different from the prescription needed for distance) presents an additional challenge in the fitting of contact lenses. Two main strategies exist: multifocal lenses and monovision.
Multifocal contact lenses (e.g. bifocals or progressives) are comparable to spectacles with bifocals or progressive lenses because they have multiple focal points. Multifocal contact lenses are typically designed for constant viewing through the center of the lens, but some designs do incorporate a shift in lens position to view through the reading power (similar to bifocal glasses).
Monovision[42] is the use of single-vision lenses (one focal point per lens) to focus an eye (typically the dominant one) for distance vision and the other for near work. The brain then learns to use this setup to see clearly at all distances. A technique called modified monovision uses multifocal lenses and also specializes one eye for distance and the other for near, thus gaining the benefits of both systems. Care is advised for persons with a previous history of strabismus and those with significant phorias, who are at risk of eye misalignment under monovision.[43] Studies have shown no adverse effect to driving performance in adapted monovision contact lens wearers.[44]
Alternatively, a person may simply wear reading glasses over their distance contact lenses.
Other types of vision correction
[edit]For those with certain color deficiencies, a red-tinted "X-Chrom" contact lens may be used. Although such a lens does not restore normal color vision, it allows some color-blind people to distinguish colors better.[45][46] Red-filtering contact lenses can also be an option for extreme light sensitivity in some visual deficiencies such as achromatopsia.[47]
ChromaGen contact lenses have been used and shown to have some limitations with vision at night although otherwise producing significant improvements in color vision.[48] An earlier study showed very significant improvements in color vision and patient satisfaction.[49]
Later work that used these ChromaGen lenses with people with dyslexia in a randomised, double-blind, placebo-controlled trial showed highly significant[clarification needed] improvements in reading ability over reading without the lenses.[50] This system has been granted FDA approval for use in the United States.[51]
Magnification is another area being researched for future contact lens applications.[52] Embedding of telescopic lenses and electronic components suggests that future uses of contact lenses may become extremely diverse.
Cosmetic contact lenses
[edit]
A cosmetic contact lens is designed to change the appearance of the eye. These lenses may also correct refractive error. Although many brands of contact lenses are lightly tinted to make them easier to handle, cosmetic lenses worn to change eye color are far less common, accounting for only 3% of contact lens fits in 2004.[53]
In the United States, the FDA labels non-corrective cosmetic contact lenses as decorative contact lenses. Like any contact lens, cosmetic lenses carry risks of mild to serious complications, including ocular redness, irritation and infection.[54]
Due to their medical nature, colored contact lenses, similar to regular ones, are illegal to purchase in the United States without a valid prescription. Those with perfect vision can buy color contacts for cosmetic reasons, but they still need their eyes to be measured for a "plano" prescription, meaning one with zero vision correction. This is for safety reasons so the lenses will fit the eye without causing irritation or redness.
Some colored contact lenses completely cover the iris, thus dramatically changing eye color. Other colored contact lenses merely tint the iris, highlighting its natural color. A new trend in Japan, South Korea and China is the circle contact lens, which extend the appearance of the iris onto the sclera by having a dark tinted area all around. The result is an appearance of a bigger, wider iris, a look reminiscent of dolls' eyes.[55]
Cosmetic lenses can have more direct medical applications. For example, some contact lenses can restore the appearance and, to some extent the function, of a damaged or missing iris.
Therapeutic scleral lenses
[edit]
A scleral lens is a large, firm, transparent, oxygen-permeable contact lens that rests on the sclera and creates a tear-filled vault over the cornea. The cause of this unique positioning is usually relevant to a specific patient whose cornea is too sensitive to support the lens directly. Scleral lenses may be used to improve vision and reduce pain and light sensitivity for people with disorders or injuries to the eye, such as severe dry eye syndrome (keratoconjunctivitis sicca), microphthalmia, keratoconus, corneal ectasia, Stevens–Johnson syndrome, Sjögren's syndrome, aniridia, neurotrophic keratitis (anesthetic corneas), complications post-LASIK, high order aberrations of the eye, complications post-corneal transplant and pellucid degeneration. Injuries to the eye such as surgical complications, distorted corneal implants, as well as chemical and burn injuries also may be treated with scleral lenses.[56]
Therapeutic soft lenses
[edit]Soft lenses are often used in the treatment and management of non-refractive disorders of the eye. A bandage contact lens allows the patient to see[57] while protecting an injured or diseased cornea[58] from the constant rubbing of blinking eyelids, thereby allowing it to heal.[59] They are used in the treatment of conditions including bullous keratopathy, dry eyes, corneal abrasions and erosion, keratitis, corneal edema, descemetocele, corneal ectasia, Mooren's ulcer, anterior corneal dystrophy, and neurotrophic keratoconjunctivitis.[60] Contact lenses that deliver drugs to the eye have also been developed.[61]
Materials
[edit]
Rigid lenses
[edit]Glass lenses were never comfortable enough to gain widespread popularity. The first lenses to do so were those made from polymethyl methacrylate (PMMA or Perspex/Plexiglas), now commonly referred to as "hard" lenses. Their main disadvantage is they do not allow oxygen to pass through to the cornea, which can cause a number of adverse, and often serious, clinical events. Starting in the late 1970s, improved rigid materials which were oxygen-permeable were developed. Contact lenses made from these materials are called rigid gas permeable lenses (RGPs).
A rigid lens is able to cover the natural shape of the cornea with a new refracting surface. This means that a spherical rigid contact lens can correct corneal astigmatism. Rigid lenses can also be made as a front-toric, back-toric, or bitoric. Rigid lenses can also correct corneas with irregular geometries, such as those with keratoconus or post surgical ectasias. In most cases, patients with keratoconus see better through rigid lenses than through glasses. Rigid lenses are more chemically inert, allowing them to be worn in more challenging environments where chemical inertia is important compared to soft lenses.[62]
Soft lenses
[edit]Soft lenses are more flexible than rigid lenses and can be gently rolled or folded without damaging the lens. While rigid lenses require a period of adaptation before comfort is achieved, new soft lens wearers typically report lens awareness rather than pain or discomfort.
Hydrogel lenses rely on their water content to transmit oxygen through the lens to the cornea. As a result, higher water content lenses allowed more oxygen to the cornea. In 1998, silicone hydrogel, or Si-hy lenses became available. These materials have both the extremely high oxygen permeability of silicone and the comfort and clinical performance of the conventional hydrogels. Because silicone allows more oxygen permeability than water, oxygen permeability of silicone hydrogels is not tied to the lenses' water content. Lenses have now been developed with so much oxygen permeability that they are approved for overnight wear (extended wear). Lenses approved for daily wear are also available in silicone hydrogel materials.[63]
Current brands of soft lenses are either traditional hydrogel or silicone hydrogel. Because of drastic differences in oxygen permeability, replacement schedule, and other design characteristics, it is very important to follow the instructions of the eye care professional prescribing the lenses. When comparing traditional hydrogel soft lens contacts with silicone hydrogel versions, there is no clear evidence to recommend a superior lens.[64]
Disadvantages of silicone hydrogels are that they are slightly stiffer and the lens surface can be hydrophobic, thus less "wettable" – factors that can influence comfort of lens use. New manufacturing techniques and changes to multipurpose solutions have minimized these effects. Those new techniques are often broken down into 3 generations:[38][65]
- 1st generation (plasma coating): A surface modification process called plasma coating alters the lens surface's hydrophobic nature;
- 2nd generation (wetting agents): Another technique incorporates internal rewetting agents to make the lens surface hydrophilic;
- 3rd generation (inherently wettable): A third process uses longer backbone polymer chains that results in less cross linking and increased wetting without surface alterations or additive agents.
Hybrid
[edit]A small number of hybrid lenses exist. Typically, these contact lenses consist of a rigid center and a soft "skirt". A similar technique is the "piggybacking" of a smaller, rigid lens on the surface of a larger, soft lens. These techniques are often chosen to give the vision correction benefits of a rigid lens and the comfort of a soft lens.[66]
Wear schedule
[edit]A "daily wear" (DW) contact lens is designed to be worn for one day and removed before sleeping. An "extended wear" (EW) contact lens is designed for continuous overnight wear, typically for up to 6 consecutive nights.[67] Newer materials, such as silicone hydrogels, allow for even longer wear periods of up to 30 consecutive nights; these longer-wear lenses are often referred to as "continuous wear" (CW). EW and CW contact lenses can be worn overnight because of their high oxygen permeability. While awake, the eyes are mostly open, allowing oxygen from the air to dissolve into the tears and pass through the lens to the cornea. While asleep, oxygen is supplied from the blood vessels in the back of the eyelid. A lens hindering passage of oxygen to the cornea causes corneal hypoxia which can result in serious complications, such as corneal ulcer that, if left untreated, can permanently decrease vision. EW and CW contact lenses typically allow for a transfer of 5–6 times more oxygen than conventional softs, allowing the cornea to remain healthy, even with closed eyelids.
Wearing lenses designed for daily wear overnight has an increased risk for corneal infections, corneal ulcers and corneal neovascularization—this latter condition, once it sets in, cannot be reversed and will eventually spoil vision acuity through diminishing corneal transparency. The most common complication of extended wear is giant papillary conjunctivitis (GPC), sometimes associated with a poorly fitting contact lens.
Replacement schedule
[edit]Contact lenses are often categorized by their replacement schedule. Single use lenses (called 1-day or daily disposables) are discarded after one use. Because they do not have to stand up to the wear and tear of repeated uses, these lenses can be made thinner and lighter, greatly improving their comfort. Lenses replaced frequently gather fewer deposits of allergens and germs, making these lenses preferable for patients with ocular allergies or for those who are prone to infection. Single-use lenses are also useful for people who wear contact lenses infrequently, or when losing a lens is likely or not easily replaced (such as when on vacation). They are also considered useful for children because cleaning or disinfecting is not needed, leading to improved compliance.
Other disposable contact lenses are designed for replacement every two or four weeks. Quarterly or annual lenses, which used to be very common, are now much less so. Rigid gas permeable lenses are very durable and may last for several years without the need for replacement. PMMA hards were very durable and were commonly worn for 5 to 10 years but had several drawbacks.
Lenses with different replacement schedules can be made of the same material. Although the materials are alike, differences in the manufacturing processes determine if the resulting lens will be a "daily disposable" or one recommended for two- or four-week replacement. However, sometimes manufacturers use absolutely identical lenses and just repackage them with different labels.[68][69]
Manufacturing
[edit]
Typically, soft contact lenses are mass-produced, while rigids are custom-made to exact specifications for the individual patient.
- Spin-cast lenses – A soft lens manufactured by whirling liquid silicone in a revolving mold at high speed.[71]
- Diamond turning – This type is cut and polished on a CNC lathe.[71] The lens starts out as a cylindrical disk held in the jaws of the lathe that is equipped with an industrial-grade diamond as the cutting tool. The CNC lathe may turn at nearly 6000 RPM as the cutter removes the desired amount of material from the inside of the lens. The concave (inner) surface of the lens is then polished with some fine abrasive paste, oil, and a small polyester cotton ball turned at high speeds. To hold the delicate lens in reverse manner, wax is used as an adhesive. The lens' convex (outer) surface is thus cut and polished by the same process. This method can be used to shape rigid as well as soft lenses. In the case of softs, the lens is cut from a dehydrated polymer that is rigid until water is reintroduced.
- Molded – Molding is used to manufacture some brands of soft contact lenses. Rotating molds are used and the molten material is added and shaped by centripetal forces. Injection molding and computer control are also used to create nearly perfect lenses.[72] The lens is kept moist throughout the entire molding process and is never dried and rehydrated.
Prescriptions
[edit]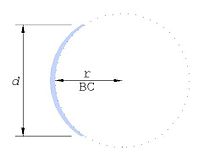
The parameters specified in a contact lens prescription may include:
- Brand name
- Material
- Base curve radius (BC, BCR)
- Diameter (D, OAD)
- Optical power in diopters (dpt)
- Center thickness (CT)
Prescriptions for contact lenses and glasses may be similar but are not interchangeable. Prescribing of contact lenses is usually restricted to various combinations of ophthalmologists, optometrists and opticians. An eye examination is needed to determine an individual's suitability for contact lens wear. This typically includes a refraction to determine the proper power of the lens and an assessment of the health of the eye's anterior segment. Many eye diseases inhibit contact lens wear, such as active infections, allergies, and dry eye.[73] Keratometry is especially important in the fitting of rigid lenses.
United States
[edit]Contact lenses are prescribed by ophthalmologists, optometrists, or specially licensed opticians under the supervision of an eye doctor. They are typically ordered at the same office that conducts the eye exam and fitting. The Fairness to Contact Lens Consumers Act guarantees consumers a copy of their contact lens prescription, allowing them to obtain lenses at the provider of their choice.[74]
Usage
[edit]Before touching the contact lens or the eye, it is important to wash hands thoroughly with soap and rinse well. Soaps containing moisturizers or allergens should be avoided as these can cause eye irritation.[75] Drying of hands using towels or tissues before handling contact lenses can transfer lint (fluff) to the hands and, subsequently, to the lenses, causing irritation upon insertion. Towels, unless freshly laundered on high temperature wash, are frequently contaminated with large quantities of bacteria and, as such, should be avoided when handling lenses. Dust, lint and other debris may collect on the outside of contact lenses. Again, hand contact with this material, before handling contact lenses, may transfer it to the lenses themselves. Rinsing the case under a source of clean running water, before opening it, can help alleviate this problem. Next the lens should be removed from its case and inspected for defects (e.g. splits, folds, lint). A 'gritty' or rough appearance to the lens surface may indicate that a considerable quantity of proteins, lipids and debris has built up on it and that additional cleaning is required; this is often accompanied and felt by unusually high irritation upon insertion.
Care should be taken to ensure the soft lens is not inserted inside-out. The edge of a lens turned inside out has a different appearance, especially when the lens is slightly folded. Insertion of an inside-out lens for a brief time (less than one minute) should not cause any damage to the eye. Some brands of lenses have markings on the rim that make it easier to tell the front of the lens apart from the back.
Insertion
[edit]Contact lenses are typically inserted into the eye by placing them on the pad of the index or middle finger with the concave side upward and then using that finger to place the lens on the eye. Rigid lenses should be placed directly on the cornea. Soft lenses may be placed on the sclera (white of the eye) and then slid into place. Another finger of the same hand, or a finger of the other hand, is used to keep the eye wide open. Alternatively, the user may close their eyes and then look towards their nose, sliding the lens into place over the cornea. Problems may arise if the lens folds, turns inside-out, slides off the finger prematurely, or adheres more tightly to the finger than the eye surface. A drop of solution may help the lens adhere to the eye.
When the lens first contacts the eye, it should be comfortable. A brief period of irritation may occur, caused by a difference in pH and/or salinity between that of the lens solution and the tear.[76][77] This discomfort fades quickly as the solution drains away and is replaced by the natural tears. However, if irritation persists, the cause could be a dirty, damaged, or inside-out lens. Removing and inspecting it for damage and proper orientation, and re-cleaning if necessary, should correct the problem. If discomfort continues, the lens should not be worn. In some cases, taking a break from lens wear for a day may correct the problem. In case of severe discomfort, or if it does not resolve by the next day, the person should be seen as soon as possible by an eye doctor to rule out potentially serious complications.
Removal
[edit]Removing contact lenses incorrectly can result in damage to the lens and injury to the eye, so certain precautions must be taken. Rigid contact lenses can best be removed by pulling the eyelid tight and then blinking, whereupon the lens drops out. With one finger on the outer corner of the eyelids, or lateral canthus, the person stretches the eyelids towards the ear; the increased tension of the eyelid margins against the edge of lens allows the blink to break the capillary action that adheres the lens to the eye. The other hand is typically cupped underneath the eye to catch the lens as it drops out. For soft lenses, which have a stronger adherence to the eye surface, this technique is less suitable.
A soft contact lens may be removed by pinching the edge between the thumb and index finger. Moving the lens off the cornea first can improve comfort during removal and reduce risk of scratching the cornea with a fingernail. It is also possible to push or pull a soft lens far enough to the side or bottom of the eyeball to get it to fold then fall out, without pinching and thereby damaging it. If these techniques are used with a rigid lens, it may scratch the cornea.
There are also small tools specifically for removing lenses. Usually made of flexible plastic, they resemble small tweezers, or plungers that suction onto the front of the lens. Typically, these tools are used only with rigid lenses. Extreme care must be exercised when using mechanical tools or fingernails to insert or remove contact lenses.
Care
[edit]
Lens care varies depending on material and wear schedule. Daily disposables are discarded after a single use and thus require no cleaning. Other lenses need regular cleaning and disinfecting to prevent surface coating and infections.
There are many ways to clean and care for contact lenses, typically called care systems or lens solutions:
- Multipurpose solutions
- The main attraction of multipurpose solutions is that the same solution can clean, rinse, disinfect and store lenses. Some multipurpose solutions also contain ingredients that improve the surface wettability and comfort of silicone hydrogel lenses. Studies showed that multipurpose solutions are ineffective against Acanthamoebae.[78][79][80] There is preliminary research on creating a new multipurpose solution that kills amoeba.[81]

- Hydrogen peroxide contact solutions
- Hydrogen peroxide can be used to disinfect contact lenses.[82] Care should be taken not to get hydrogen peroxide in the eye because it is very painful and irritating. With "two-step" products, the hydrogen peroxide must be rinsed away with saline before the lenses may be worn. "One-step" systems allow the hydrogen peroxide to react completely, becoming pure water. Thus "one-step" hydrogen peroxide systems do not require the lenses to be rinsed before insertion, provided the solution has been given enough time to react.
- An exposure time of 2-3 hours to 3% H
2O
2 (non neutralized solution) is sufficient to kill bacteria, HIV, fungi, and Acanthamoeba.[83][84] This can be achieved by using a "two-step" product or a "one-step" tablet system if the catalytic tablet is not added before 2-3 hours.[84] However, the "one-step" catalytic disk systems are not effective against Acanthamoeba due to insufficient exposure time.[84] - Enzymatic cleaner
- Used for cleaning protein deposits off lenses, usually weekly, if the daily cleaner is not sufficient. Typically, this cleaner is in tablet form.
- Ultraviolet, vibration, or ultrasonic devices
- These devices intend to disinfect and clean contact lenses. The lenses are inserted inside the portable device (running on batteries and/or plug-in) for 2 to 6 minutes during which both the microorganisms and protein build-up are supposed to be cleaned. However these devices can not be used to replace the manual rub and rinse method because vibration and ultrasound can not create relative motion between contact lens and solution, which is required for proper cleaning of the lens.[85] These devices are not usually available in optic retailers but are in other stores.[86][87][88]
Rub and rinse method
[edit]Contact lenses can be mechanically cleaned of more substantial protein, lipid and debris build up by rubbing them between the clean pad of a finger and the palm of a hand, using a small amount of cleaning fluid as a lubricant; and by rinsing thereafter. This "rub and rinse" method is thought to be the most effective method for multipurpose solutions,[89] and is the method indicated by the American Academy of Ophthalmology regardless of cleaning solution used.[90] In 2010, the FDA recommended that manufacturers removed the "no rub" from product labeling,[91] "because 'rub-and-rinse' regimens help prevent microbial adhesion to the contact lens, help prevent formation of biofilms, and generally reduce the microbial load on the lens and the lens case."[92]
Physical rubbing devices
[edit]
This type of devices mimic digital rubbing. The lenses are sandwiched by silicone parts inside the portable device. The device applies a gentle yet high speed rubbing action on the lens surface and remove debris.
- Saline solution
- Sterile saline is used for rinsing the lens after cleaning and preparing it for insertion. Saline solutions do not disinfect, so it must be used in conjunction with some type of disinfection system. One advantage to saline is that it cannot cause an allergic response, so it is well suited for individuals with sensitive eyes or strong allergies.
- Daily cleaner
- Used to clean lenses on a daily basis. A few drops of cleaner are applied to the lens while it rests in the palm of the hand; the lens is rubbed for about 20 seconds with a clean fingertip (depending on the product) on each side. Lens must then be rinsed. This system is commonly used to care for rigid lenses.
Water is not recommended for cleaning contact lenses.[93] Insufficiently chlorinated tap water can lead to lens contamination, particularly by Acanthamoeba. On the other hand, sterile water will not kill any contaminants that get in from the environment.[94]
Aside from cleaning the contact lenses, contact lens case should also be kept clean and be replaced at minimum every 3 months.[90]
Contact lens solutions often contain preservatives such as benzalkonium chloride and benzyl alcohol. Preservative-free products usually have shorter shelf lives, but are better suited for individuals with an allergy or sensitivity to a preservative. In the past, thiomersal was used as a preservative. In 1989, thiomersal was responsible for about 10% of problems related to contact lenses.[95] As a result, most products no longer contain thiomersal.
Complications
[edit]
Contact lenses are generally safe as long as they are used correctly. Complications from contact lens wear affect roughly 5% of wearers yearly.[96] Factors leading to eye damage varies,[97] and improper use of a contact lens may affect the eyelid, the conjunctiva, and, most of all, the whole structure of the cornea.[96] Poor lens care may lead to infections by various microorganisms including bacteria, fungi, and the amoeba Acanthamoeba (Acanthamoeba keratitis).
Many complications arise when contact lenses are worn not as prescribed (improper wear schedule or lens replacement). Sleeping in lenses not designed or approved for extended wear is a common cause of complications. Many people go too long before replacing their contacts, wearing lenses designed for 1, 14, or 30 days of wear for multiple months or years. While this does save on the cost of lenses, it risks permanent damage to the eye and even loss of sight.
For non silicone-hydrogel lenses, one of the major factors that causes complications is that the contact lens is an oxygen barrier. The cornea needs a constant supply of oxygen to remain completely transparent and function as it should; it normally gets that oxygen from the surrounding air while awake, and from the blood vessels in the back of the eyelid while asleep. The most prominent risks associated with long-term, chronic low oxygen to the cornea include corneal neovascularization, increased epithelial permeability, bacterial adherence, microcysts, corneal edema, endothelial polymegethism, dry eye and potential increase in myopia.[98] Much of the research into soft and rigid contact lens materials has centered on improving oxygen transmission through the lens.
Silicone-hydrogel lenses available today have effectively eliminated hypoxia for most patients.[99]
Mishandling of contact lenses can also cause problems. Corneal abrasions can increase the chances of infection.[100] When combined with improper cleaning and disinfection of the lens, a risk of infection further increases. Decreased corneal sensitivity after extended contact lens wear may cause a patient to miss some of the earliest symptoms of such complications.[101]
The way contact lenses interact with the natural tear layer is a major factor in determining lens comfort and visual clarity. People with dry eyes are particularly vulnerable to discomfort and episodes of brief blurry vision. Proper lens selection can minimize these effects.
Long-term wear (over five years) of contact lenses may "decrease the entire corneal thickness and increase the corneal curvature and surface irregularity."[102] Long-term wear of rigid contacts is associated with decreased corneal keratocyte density[103] and increased number of epithelial Langerhans cells.[104]
All contact lenses sold in the United States are studied and approved as safe by the FDA when specific handling and care procedures, wear schedules, and replacement schedules are followed.
Current research
[edit]Contact lens sensors to monitor the ocular temperature have been demonstrated.[105] Monitoring intraocular pressure with contact lens sensors is another area of contact lens research.[106]
A large segment of current contact lens research is directed towards the treatment and prevention of conditions resulting from contact lens contamination and colonization by foreign organisms. Clinicians tend to agree that the most significant complication of contact lens wear is microbial keratitis and that the most predominant microbial pathogen is Pseudomonas aeruginosa.[107] Other organisms are also major causative factors in bacterial keratitis associated with contact lens wear, although their prevalence varies across different locations. These include both the Staphylococcus species (aureus and epidermidis) and the Streptococcus species, among others.[108][109] Microbial keratitis is a serious focal point of current research due to its potentially devastating effect on the eye, including severe vision loss.[110]
One specific research topic of interest is how microbes such as Pseudomonas aeruginosa invade the eye and cause infection. Although the pathogenesis of microbial keratitis is not well understood, many different factors have been investigated. One group of researchers showed that corneal hypoxia exacerbated Pseudomonas binding to the corneal epithelium, internalization of the microbes, and induction of the inflammatory response.[111] One way to alleviate hypoxia is to increase the amount of oxygen transmitted to the cornea. Although silicone-hydrogel lenses almost eliminate hypoxia in patients due to their very high levels of oxygen transmissibility,[112] they also seem to provide a more efficient platform for bacterial contamination and corneal infiltration than other conventional hydrogel soft contact lenses. One study showed that Pseudomonas aeruginosa and Staphylococcus epidermidis adhere much more strongly to unworn silicone hydrogel contact lenses than conventional hydrogel lenses and that adhesion of Pseudomonas aeruginosa was 20 times stronger than that of Staphylococcus epidermidis.[113] This might partly explain why Pseudomonas infections are the most predominant. However, another study conducted with worn and unworn silicone and conventional hydrogel contact lenses showed that worn silicone contact lenses were less prone to Staphylococcus epidermidis colonization than conventional hydrogel lenses.[114]
Besides bacterial adhesion and cleaning, micro and nano pollutants (biological and manmade) is an area of contact lens research that is growing. Small physical pollutants ranging from nanoplastics to fungi spores to plant pollen adhere to contact lens surfaces in high concentrations. It has been found that multipurpose solution and rubbing with fingers does not significantly clean the lenses. A group of researchers have suggested an alternative cleaning solution, PoPPR (polymer on polymer pollution removal).[115] This cleaning technique takes advantage of a soft and porous polymer to physically peel pollutants off of contact lenses.
Another important area of contact lens research deals with patient compliance. Compliance is a major issue[116] pertaining to the use of contact lenses because patient noncompliance often leads to contamination of the lens, storage case, or both.[117][118][119] However, careful users can extend the wear of lenses through proper handling: there is, unfortunately, no disinterested research on the issue of "compliance" or the length of time a user can safely wear a lens beyond its stated use. The introduction of multipurpose solutions and daily disposable lenses have helped to alleviate some of the problems observed from inadequate cleaning but new methods of combating microbial contamination are currently being developed. A silver-impregnated lens case has been developed which helps to eradicate any potentially contaminating microbes that come in contact with the lens case.[120] Additionally, a number of antimicrobial agents are being developed that have been embedded into contact lenses themselves. Lenses with covalently attached selenium molecules have been shown to reduce bacterial colonization without adversely affecting the cornea of a rabbit eye[121] and octyl glucoside used as a lens surfactant significantly decreases bacterial adhesion.[122] These compounds are of particular interest to contact lens manufacturers and prescribing optometrists because they do not require any patient compliance to effectively attenuate the effects of bacterial colonization.
One area of research is in the field of bionic lenses. These are visual displays that include built-in electric circuits and light-emitting diodes and can harvest radio waves for their electric power. Bionic lenses can display information beamed from a mobile device overcoming the small display size problem. The technology involves embedding nano and microscale electronic devices in lenses. These lenses will also need to have an array of microlenses to focus the image so that it appears suspended in front of the wearer's eyes. The lens could also serve as a head-up display for pilots or gamers.[123]
Drug administration through contact lenses is also becoming an area of research. One application is a lens that releases anesthesia to the eye for post-surgery pain relief, especially after PRK (photorefractive keratectomy) in which the healing process takes several days. One experiment shows that silicone contact lenses that contain vitamin E deliver pain medication for up to seven days compared with less than two hours in usual lenses.[123]
Another study of the usage of contact lens is aimed to address the issue of macular degeneration (AMD or age-related macular degeneration). An international collaboration of researchers was able to develop a contact lens that can shift between magnified and normal vision. Previous solutions to AMD included bulky glasses or surgical implants. But the development of this new contact lens, which is made of polymethyl methacrylate, could offer an unobtrusive solution.[124]
In popular culture
[edit]Films
[edit]
One of the earliest known motion pictures to introduce the use of contact lenses as a make-up artist's device for enhancing the eyes was by the innovative actor Lon Chaney in the 1926 film The Road to Mandalay to create the effect of a character who had a blind eye.[125] Dr. Rueben Greenspoon applied them to Orson Welles for the film Citizen Kane in 1940. In the 1950s, contact lenses were starting to be used in British color horror films. An early example of this is the British actor Christopher Lee as the Dracula character in the 1958 color horror film Dracula, which helped to emphasize his horrific looking black pupils and red bloodshot eyes. Tony Curtis wore them in the 1968 film The Boston Strangler. Contact lenses were also used to better emphasize the sinister gaze of the demonic characters in 1968's Rosemary's Baby and 1973's The Exorcist. Colored custom-made contact lenses are now standard makeup for a number of special effects-based movies.[126]
Further reading
[edit]- Demas GN (1989). "pH consistency and stability of contact lens solutions". J Am Optom Assoc. 60 (10): 732–4. PMID 2584587.
The pH of contact lens solutions has been implicated in the comfort of contact lenses on insertion.
- "Eye Care". CLH. Retrieved 20 November 2014.
- "How to Put Contacts in Your Eyes". CooperVision. Retrieved 20 November 2014.
use plain soap without any heavy moisturizers or perfumes. Rinse well and dry your hands. Again, this is to prevent transmitting anything unwanted to your eyes.
See also
[edit]References
[edit]- ^ R Moreddu; D Vigolo; AK Yetisen (2019). "Contact Lens Technology: From fundamentals to Applications" (PDF). Advanced Healthcare Materials. 8 (15): 1900368. doi:10.1002/adhm.201900368. PMID 31183972. S2CID 184488183.
- ^ NM Farandos; AK Yetisen; MJ Monteiro; CR Lowe; SH Yun (2014). "Contact Lens Sensors in Ocular Diagnostics". Advanced Healthcare Materials. 4 (6): 792–810. doi:10.1002/adhm.201400504. PMID 25400274. S2CID 35508652.
- ^ a b Nichols, Jason J., et al "ANNUAL REPORT: Contact Lenses 2010". January 2011.
- ^ Morgan, Philip B., et al. "International Contact Lens Prescribing in 2010". Contact Lens Spectrum. October 2011.
- ^ Agarwal, R. K. (1969), Contact Lens Notes, Some factors concerning patients' motivation, The Optician, 10 January, pages 32-33 (published in London, England).
- ^ Sokol, JL; Mier, MG; Bloom, S; Asbell, PA (1990). "A study of patient compliance in a contact lens-wearing population". CLAO Journal. 16 (3): 209–13. PMID 2379308.
- ^ "Compare Contacts & Glasses". ACUVUE® Middle East. Retrieved 22 November 2021.
- ^ "Contact Lenses for Keratoconus". National Keratoconus Foundation. 21 February 2018.
- ^ a b Heitz, RF and Enoch, J. M. (1987) "Leonardo da Vinci: An assessment on his discourses on image formation in the eye." Advances in Diagnostic Visual Optics 19—26, Springer-Verlag.
- ^ a b Leonard G. Schifrin; William J. Rich (December 1984). The Contact Lens Industry: Structure, Competition, and Public Policy. United States Office of Technology Assessment.
- ^ a b Moreddu, Rosalia; Vigolo, Daniele; Yetisen, Ali K. (August 2019). "Contact Lens Technology: From Fundamentals to Applications" (PDF). Advanced Healthcare Materials. 8 (15): 1900368. doi:10.1002/adhm.201900368. PMID 31183972. S2CID 184488183.
- ^ Rajesh Sinha; Vijay Kumar Dada (31 January 2017). Textbook of Contact Lenses. JP Medical Ltd. pp. 2–. ISBN 978-93-86150-44-8.
- ^ "The History of Contact Lenses." Archived 11 October 2008 at the Wayback Machine eyeTopics.com. Accessed 18 October 2006.
- ^ "History of Contact Lenses and Improved Technology". Master Eye Associates. Retrieved 14 September 2019.
- ^ "Contact Lenses". Van Nostrand's Scientific Encyclopedia. 2005. doi:10.1002/0471743984.vse2040. ISBN 0471743984.
- ^ Hellemans, Alexander; Bunch, Bryan (1988). The Timetables of Science. Simon & Schuster. p. 367. ISBN 0671621300.
- ^ "Adolf Eugen Fick (1852–1937)". Archived from the original on 17 May 2015. Retrieved 26 March 2015.
- ^ Heitz, R (September 2014). "The invention of the contact lenses (1888)". Acta Ophthalmologica. 92 (s253): 0. doi:10.1111/j.1755-3768.2014.3773.x. ISSN 1755-375X.
- ^ Sinha, Rajesh; Dada, Vijay Kumar (2017). Textbook of contact lenses (Fifth ed.). New Delhi ; Philadelphia: Jaypee Brothers Medical Publishers (P) Ltd. ISBN 978-93-86150-44-8. OCLC 962009998.
- ^ Pearson, Richard M.; Efron, Nathan (September 1989). "Hundredth anniversary of August Müller's inaugural dissertation on contact lenses". Survey of Ophthalmology. 34 (2): 133–141. doi:10.1016/0039-6257(89)90041-6. PMID 2686057.
- ^ Robert B. Mandell. Contact Lens Practice, 4th Edition. Charles C. Thomas, Springfield, IL, 1988
- ^ "Contact Lens for Eyes Now Common; It is Used as Substitute for Spectacles." Nashua (IA) Reporter, 28 April 1937.
- ^ Gyorgy, Salacz (January 2001). "Dr István Györffy, 1912–1999". Contact Lens and Anterior Eye. 24 (4): 180–182. doi:10.1016/S1367-0484(01)80040-0.
- ^ Contact Lens History: How Contact Lenses Have Developed Through the Years. EyeHealth Central. Retrieved from https://www.contactlenses.co.uk/education/history.htm
- ^ U.S. Patent No. 2,510,438, filed 28 February 1948.
- ^ "The Corneal Lens", The Optician, 2 September 1949, pp. 141–144.
- ^ "Corneal Contact Lenses", The Optician, 9 September 1949, p. 185.
- ^ "New Contact Lens Fits Pupil Only", The New York Times, 11 February 1952, p. 27.
- ^ Pal, Subrata (2014), "The Eye and Its Artificial Replacement", Design of Artificial Human Joints & Organs, Boston, MA: Springer US, pp. 219–249, doi:10.1007/978-1-4614-6255-2_14, ISBN 978-1-4614-6254-5, retrieved 29 August 2024
- ^ Rosenthal, J. William (1996). Spectacles and Other Vision Aids: A History and Guide to Collecting. Norman Publishing. p. 379. ISBN 978-0930405717.
- ^ Smith, William D. (18 April 1971). "Soft-Lens Clamor". The New York Times. Retrieved 29 November 2018.
- ^ "nytimes archive". The New York Times. 6 December 1964. Retrieved 24 August 2018.
- ^ Pearce, Jeremy (23 September 2007). "Norman Gaylord, 84; helped develop type of contact lens". (New York Times News Service). The Boston Globe. Retrieved 6 October 2007.
- ^ Wichterle O, Lim D (1960). "Hydrophilic gels for biological use". Nature. 185 (4706): 117–118. Bibcode:1960Natur.185..117W. doi:10.1038/185117a0. S2CID 4211987.
- ^ "CONTACT LENS HISTORY – Otto Wichterle". Archived from the original on 29 January 2015. Retrieved 26 March 2015.
- ^ Agarwal Rishi K (1972). "Some Thoughts on Soft Lenses". The Contact Lens. 4 (1): 28.
- ^ "Editorial note". American Journal of Optometry and Physiological Optics. 65 (9): 744. 1988.
- ^ a b c Szczotka-Flynn, Loretta (1 May 2008). "Looking at Silicone Hydrogels Across Generations". www.optometricmanagement.com. Archived from the original on 19 July 2011. Retrieved 5 October 2021.
- ^ "Astigmatism". www.aoa.org. Retrieved 6 August 2020.[permanent dead link]
- ^ "Advantages and Disadvantages of Various Types of Contact Lenses". www.aoa.org. Retrieved 6 August 2020.
- ^ "A Complete Guide to Gas Permeable Contact Lenses". EyeHealthWeb.com. 26 January 2013. Retrieved 6 August 2020.
- ^ Lebow, KA; Goldberg, JB (1975). "Characteristic of binocular vision found for presbyopic patients wearing single vision contact lenses". Journal of the American Optometric Association. 46 (11): 1116–23. PMID 802938.
- ^ Pollard, Zane F.; Greenberg, Marc F.; Bordenca, Mark; Elliott, Joshua; Hsu, Victoria (September 2011). "Strabismus Precipitated by Monovision". American Journal of Ophthalmology. 152 (3): 479–482.e1. doi:10.1016/j.ajo.2011.02.008. PMID 21669405.
- ^ Wood, Joanne M.; Wick, Kristan; Shuley, Vicki; Pearce, Brendon; Evans, Dean (6 May 1998). "The effect of monovision contact lens wear on driving performance". Clinical and Experimental Optometry. 81 (3): 100–103. doi:10.1111/j.1444-0938.1998.tb06727.x. PMID 12482258. S2CID 38392636.
- ^ Hartenbaum, NP; Stack, CM (1997). "Color vision deficiency and the X-Chrom lens". Occupational Health & Safety. 66 (9): 36–40, 42. PMID 9314196.
- ^ Siegel, IM (1981). "The X-Chrom lens. On seeing red". Survey of Ophthalmology. 25 (5): 312–24. doi:10.1016/S0039-6257(81)80001-X. PMID 6971497.
- ^ http://www.achromatopsia.info/red-contact-lenses/ Red contact lenses for achromats
- ^ Swarbrick, HA; Nguyen, P; Nguyen, T; Pham, P (2001). "The ChromaGen contact lens system: Colour vision test results and subjective responses". Ophthalmic & Physiological Optics. 21 (3): 182–96. doi:10.1046/j.1475-1313.2001.00583.x. PMID 11396392. S2CID 40409461.
- ^ Harris D "Colouring Sight: A study of CL fittings with colour enhancing lenses" 'Optician' 8 June 1997
- ^ Harris DA, MacRow-Hill SJ "Application of ChromaGen haploscopic lenses to patients with dyslexia: a double masked placebo controlled trial" Journal of the American Optometric Association 25/10/99.
- ^ "Cision - FDA Cleared ChromaGen Lenses" (Press release). Archived from the original on 3 July 2013.
- ^ "Telescopic contact lens magnifies vision by 2.8 times on demand". Wired UK. Archived from the original on 2 April 2015. Retrieved 26 March 2015.
- ^ Morgan PB et al."International Contact Lens Prescribing in 2004: An analysis of more than 17,000 contact lens fits from 14 countries in 2004 reveals the diversity of contact lens practice worldwide." Contact Lens Spectrum. January 2005.
- ^ Vanderbilt University Medical Center – Vanderbilt Eye Doctors Warn of the Dangers of Cosmetic Contact Lenses. Mc.vanderbilt.edu (19 April 2010). Retrieved on 2013-07-21.
- ^ "How Do You Find the Right Circle Lens?". EyeCandy's. Archived from the original on 13 December 2013. Retrieved 26 March 2015.
- ^ Caceres, Vanessa (June 2009). "Taking a second look at scleral lenses". ASCRS EyeWorld. Archived from the original on 28 February 2019. Retrieved 18 May 2014.
- ^ Alvarez-Lorenzo, Carmen; Anguiano-Igea, Soledad; Varela-García, Angela; Vivero-Lopez, María; Concheiro, Angel (January 2019). "Bioinspired hydrogels for drug-eluting contact lenses". Acta Biomaterialia. 84: 49–62. doi:10.1016/j.actbio.2018.11.020. PMID 30448434. S2CID 53780024.
- ^ Zidan, Ghada; Rupenthal, Ilva D.; Greene, Carol; Seyfoddin, Ali (2018). "Medicated ocular bandages and corneal health: potential excipients and active pharmaceutical ingredients". Pharmaceutical Development and Technology. 23 (3): 255–260. doi:10.1080/10837450.2017.1377232. PMID 28875742. S2CID 32765975.
- ^ "Eye Health Guide – Eye Diseases, Eye Problems and Eye Conditions". All About Vision. Archived from the original on 9 April 2008. Retrieved 26 March 2015.
- ^ "45 COVERAGE ISSUES – SUPPLIES – DRUGS 11–91 45" (PDF). Centers for Medicare and Medicaid Services. Archived from the original (PDF) on 4 March 2006. Retrieved 1 March 2006.
- ^ "Qmed is the world's only directory of pre-qualified suppliers to the medical device and in vitro diagnostics industry. - Qmed". Archived from the original on 5 December 2008. Retrieved 26 March 2015.
- ^ "Rigid contact lenses". Eagle Eyes UK. Retrieved 28 April 2022.
- ^ FDA Premarket Notification for "new silicone hydrogel lens for daily wear" Archived 3 October 2008 at the Wayback Machine 'July 2008.
- ^ Haworth, Kristina; Travis, Darian; Leslie, Louis; Fuller, Daniel; Pucker, Andrew D (19 September 2023). Cochrane Eyes and Vision Group (ed.). "Silicone hydrogel versus hydrogel soft contact lenses for differences in patient-reported eye comfort and safety". Cochrane Database of Systematic Reviews. 2023 (9): CD014791. doi:10.1002/14651858.CD014791.pub2. PMC 10507745. PMID 37724689.
- ^ Chou, Brian (1 June 2008). "The Evolution of Silicone Hydrogel Lenses". www.clspectrum.com. Archived from the original on 30 December 2016. Retrieved 5 October 2021.
- ^ White, Neal; Jennings, Christopher; Pelka, Kevin (16 January 2015). "Hybrid contact lens". Retrieved 28 February 2018.
- ^ "Contact Lens Types". American Academy of Ophthalmology. Retrieved 30 April 2020.
- ^ "The Only Difference Is When You Throw Them Away". Bloomberg.com. 12 July 1993. Retrieved 26 December 2016.
- ^ "Contact Lenses – Types of Contact Lenses. Disposable (Replacement Schedule) Contact Lenses". www.fda.gov. Retrieved 26 December 2016.
- ^ John Wiley & Sons, Inc, ed. (2000). Kirk-Othmer Encyclopedia of Chemical Technology. doi:10.1002/0471238961. ISBN 9780471484943.
- ^ a b Cassin, B. and Solomon, S. Dictionary of Eye Terminology. Gainesville, Florida: Triad Publishing Company, 1990.
- ^ Manufacture of soft contact lenses. "Manufacture of soft contact lenses".
- ^ Agarwal, R.K. (1970), Some reasons for not fitting contact lenses, The Optician, 4 December, page 623 (published in London, England).
- ^ "Fairness to Contact Lens Consumers Act". 15 October 2003.
- ^ "How to Put Contacts in Your Eyes". CooperVision. Retrieved 20 November 2014.
use plain soap without any heavy moisturizers or perfumes. Rinse well and dry your hands. Again, this is to prevent transmitting anything unwanted to your eyes.
- ^ Demas GN (1989). "pH consistency and stability of contact lens solutions". J Am Optom Assoc. 60 (10): 732–4. PMID 2584587.
The pH of contact lens solutions has been implicated in the comfort of contact lenses on insertion.
- ^ "Eye Care". CLH. Retrieved 20 November 2014.
- ^ Johnston, Stephanie P.; Sriram, Rama; Qvarnstrom, Yvonne; Roy, Sharon; Verani, Jennifer; Yoder, Jonathan; Lorick, Suchita; Roberts, Jacquelin; Beach, Michael J.; Visvesvara, Govinda (July 2009). "Resistance of Acanthamoeba Cysts to Disinfection in Multiple Contact Lens Solutions". Journal of Clinical Microbiology. 47 (7): 2040–2045. doi:10.1128/JCM.00575-09. PMC 2708465. PMID 19403771.
- ^ Padzik, Marcin; Chomicz, Lidia; Szaflik, Jacek P.; Chruścikowska, Agnieszka; Perkowski, Konrad; Szaflik, Jerzy (November 2014). "In vitro effects of selected contact lens care solutions on Acanthamoeba castellanii strains in Poland". Experimental Parasitology. 145: S98–S101. doi:10.1016/j.exppara.2014.06.014. PMID 24967738.
- ^ Aguiar, Ana; Oliveira Silveira, Caroline; Todero Winck, Mari; Rott, Marilise (1 January 2013). "Susceptibility of Acanthamoeba to multipurpose lens-cleaning solutions". Acta Parasitologica. 58 (3): 304–308. doi:10.2478/s11686-013-0143-9. hdl:10183/179379. PMID 23990426.
- ^ Fears, Alyssa C.; Metzinger, Rebecca C.; Killeen, Stephanie Z.; Reimers, Robert S.; Roy, Chad J. (December 2018). "Comparative in vitro effectiveness of a novel contact lens multipurpose solution on Acanthamoeba castellanii". Journal of Ophthalmic Inflammation and Infection. 8 (1): 19. doi:10.1186/s12348-018-0161-8. PMC 6200833. PMID 30357549.
- ^ Hughes, Reanne; Kilvington, Simon (July 2001). "Comparison of Hydrogen Peroxide Contact Lens Disinfection Systems and Solutions against Acanthamoeba polyphaga". Antimicrobial Agents and Chemotherapy. 45 (7): 2038–43. doi:10.1128/AAC.45.7.2038-2043.2001. PMC 90597. PMID 11408220.
- ^ Hiti, K; Walochnik, J; Haller-Schober, EM; Faschinger, C; Aspöck, H (1 February 2002). "Viability of Acanthamoeba after exposure to a multipurpose disinfecting contact lens solution and two hydrogen peroxide systems". British Journal of Ophthalmology. 86 (2): 144–146. doi:10.1136/bjo.86.2.144. PMC 1771011. PMID 11815336.
- ^ a b c Hiti, K; Walochnik, J; Faschinger, C; Haller-Schober, E-M; Aspöck, H (December 2005). "One- and two-step hydrogen peroxide contact lens disinfection solutions against Acanthamoeba: How effective are they?". Eye. 19 (12): 1301–1305. doi:10.1038/sj.eye.6701752. PMID 15543174.
- ^ Efron, Nathan; Lowe, Russell; Vallas, Vicky; Grusiner, Eugene (1 January 1991). "Clinical efficacy of standing wave and ultrasound for cleaning and disinfecting contact lenses". International Contact Lens Clinic. 18 (1): 24–29. doi:10.1016/0892-8967(91)90040-7. ISSN 0892-8967.
- ^ "How Optical Ultrasonic Cleaners Work". The Tech-FAQ. 6 April 2019.
- ^ White, Gina. "Caring for Soft Contact Lenses". All About Vision.
- ^ Ward, Michael. "Soft Contact Lens Care Products". Contact Lens Spectrum.
- ^ Zhu, Hua; Bandara, Mahesh B.; Vijay, Ajay K.; Masoudi, Simin; Wu, Duojia; Willcox, Mark D. P. (August 2011). "Importance of Rub and Rinse in Use of Multipurpose Contact Lens Solution". Optometry and Vision Science. 88 (8): 967–972. doi:10.1097/OPX.0b013e31821bf976. PMID 21623253. S2CID 23544740.
- ^ a b Boyd, Kierstan (4 March 2021). "How to Take Care of Contact Lenses". www.aao.org. Retrieved 5 October 2021.
- ^ "Contact Lens Care Products Labeling - Guidance for Industry and FDA Staff". www.fda.gov. 15 August 2010. Retrieved 5 October 2021.
- ^ "FDA Letter to Firms with Marketing Clearance for No-rub Multipurpose Contact Lens Solutions". www.fda.gov. 19 May 2009. Retrieved 5 October 2021.
- ^ Razmaria, Aria A. (2015). "Proper Care of Contact Lenses". JAMA. 314 (14): 1534. doi:10.1001/jama.2015.12468. PMID 26462011.
- ^ Carnt, Nicole A.; Subedi, Dinesh; Connor, Sophie; Kilvington, Simon (11 March 2020). "The relationship between environmental sources and the susceptibility of Acanthamoeba keratitis in the United Kingdom". PLOS ONE. 15 (3): e0229681. Bibcode:2020PLoSO..1529681C. doi:10.1371/journal.pone.0229681. PMC 7065798. PMID 32160218.
- ^ Wilson-Holt, N; Dart, J K G (September 1989). "Thiomersal keratoconjunctivitis, frequency, clinical spectrum and diagnosis". Eye. 3 (5): 581–587. doi:10.1038/eye.1989.91. PMID 2630335.
- ^ a b Stamler, John F. (August 1998). "The complications of contact lens wear". Current Opinion in Ophthalmology. 9 (4): 66–71. doi:10.1097/00055735-199808000-00012. PMID 10387472.
- ^ "Do Contact Lenses Damage The Eye?". Lensite. Archived from the original on 2 October 2018. Retrieved 30 March 2018.
- ^ "What's the Best Prescription for Healthy Contact Lens Wear?". Contact Lens Spectrum.
- ^ Sweeney, Deborah F. (2013). "Have Silicone Hydrogel Lenses Eliminated Hypoxia?". Eye & Contact Lens: Science & Clinical Practice. 39 (1): 53–60. doi:10.1097/ICL.0b013e31827c7899. PMID 23271474. S2CID 205659587.
- ^ Khan, Feras H (13 April 2023). "Emergency Care of Corneal Abrasion: Overview, Clinical Evaluation, ED Treatment Considerations". Medscape Reference. Retrieved 25 August 2024.
- ^ Liu, Z.; Pflugfelder, S. (January 2000). "The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity". Ophthalmology. 107 (1): 105–111. doi:10.1016/S0161-6420(99)00027-5. PMID 10647727.
- ^ Liu Z, Pflugfelder SC (January 2000). "The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity". Ophthalmology. 107 (1): 105–11. doi:10.1016/S0161-6420(99)00027-5. PMID 10647727.
- ^ Hollingsworth JG, Efron N (June 2004). "Confocal microscopy of the corneas of long-term rigid contact lens wearers". Cont Lens Anterior Eye. 27 (2): 57–64. doi:10.1016/j.clae.2004.02.002. PMID 16303530.
- ^ Zhivov A, Stave J, Vollmar B, Guthoff R (January 2007). "In vivo confocal microscopic evaluation of langerhans cell density and distribution in the corneal epithelium of healthy volunteers and contact lens wearers". Cornea. 26 (1): 47–54. doi:10.1097/ICO.0b013e31802e3b55. PMID 17198013. S2CID 22951471.
- ^ Moreddu R, Elsherif M, Butt H, Vigolo D, Yetisen AK (2019). "Contact lenses for continuous corneal temperature monitoring" (PDF). RSC Advances. 9 (20): 11433–11442. Bibcode:2019RSCAd...911433M. doi:10.1039/C9RA00601J. PMC 9063335. PMID 35520262.
- ^ Baghban, R; Talebnejad, MR; Meshksar, A; Heydari, M; Khalili, MR (2 November 2023). "Recent advancements in nanomaterial-laden contact lenses for diagnosis and treatment of glaucoma, review and update". Journal of Nanobiotechnology. 21 (1): 402. doi:10.1186/s12951-023-02166-w. PMC 10621182. PMID 37919748.
- ^ Robertson, DM, Petroll, WM, Jester, JV & Cavanagh, HD: Current concepts: contact lens related Pseudomonas keratitis. Cont Lens Anterior Eye, 30: 94–107, 2007.
- ^ Sharma, S, Kunimoto, D, Rao, N, Garg, P & Rao, G: Trends in antibiotic resistance of corneal pathogens: Part II. An analysis of leading bacterial keratitis isolates, 1999.
- ^ Verhelst D, Koppen C, Looveren JV, Meheus A, Tassignon M (2005). "Clinical, epidemiological and cost aspects of contact lens related infectious keratitis in Belgium: results of a seven-year retrospective study". Bull Soc Belge Ophtalmol. 297 (297): 7–15. PMID 16281729.
- ^ Burd EM, Ogawa GSH, Hyndiuk RA. Bacterial keratitis and conjunctivitis. In: Smolin G, Thoft RA, editors. The Cornea. Scientific Foundations and Clinical Practice. 3rd ed. Boston: Little, Brown, & Co, 1994. p 115–67.
- ^ Zaidi T, Mowrey-McKee M, Pier GB (2004). "Hypoxia increases corneal cell expression of CFTR leading to increased Pseudomonas aeruginosa binding, internalization, and initiation of inflammation". Invest Ophthalmol Vis Sci. 45 (11): 4066–74. doi:10.1167/iovs.04-0627. PMC 1317302. PMID 15505057.
- ^ Sweeney DF, Keay L, Jalbert I. Clinical performance of silicone hydrogel lenses. In Sweeney DF, ed. Silicone Hydrogels: The Rebirth of Continuous Wear Contact Lenses. Woburn, Ma: Butterworth Heinemann; 2000.
- ^ Kodjikian L, Casoli-Bergeron E, Malet F, Janin-Manificat H, Freney J, Burillon C, Colin J, Steghens JP (2008). "Bacterial adhesion to conventional hydrogel and new silicone hydrogel contact lens materials". Graefes Arch Clin Exp Ophthalmol. 246 (2): 267–73. doi:10.1007/s00417-007-0703-5. PMID 17987309. S2CID 23218590.
- ^ Santos, Lívia; Rodrigues, Diana; Lira, Madalena; Real Oliveira, M Elisabete C. D.; Oliveira, Rosário; Vilar, Eva Yebra-Pimente; Azeredo, Joana (July 2008). "Bacterial Adhesion to Worn Silicone Hydrogel Contact Lenses". Optometry and Vision Science. 85 (7): 520–525. doi:10.1097/OPX.0b013e31817c92f3. hdl:1822/8740. PMID 18594343. S2CID 10171270.
- ^ Burgener, Katherine; Bhamla, M. Saad (June 2021). "A polymer-based technique to remove pollutants from soft contact lenses". Contact Lens and Anterior Eye. 44 (3): 101335. arXiv:2005.08732. doi:10.1016/j.clae.2020.05.004. PMID 32444249. S2CID 218673928.
- ^ Agarwal R.K. (1971). "A legally problematical but clinically interesting contact lens case". The Contact Lens. 3 (3): 13.
- ^ Yung MS, Boost M, Cho P, Yap M (2007). "Microbial contamination of contact lenses and lens care accessories of soft contact lens wearers (university students) in Hong Kong". Ophthalmic and Physiological Optics. 27 (1): 11–21. doi:10.1111/j.1475-1313.2006.00427.x. hdl:10397/22844. PMID 17239186. S2CID 6552480.
- ^ Midelfart J.; Midelfart A.; Bevanger L. (1996). "Microbial contamination of contact lens cases among medical students". CLAO J. 22 (1): 21–24. PMID 8835064.
- ^ Gray T.B.; Cursons R.T.; Sherwan J.F.; Rose P.R. (1995). "Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases". Br J Ophthalmol. 79 (6): 601–605. doi:10.1136/bjo.79.6.601. PMC 505174. PMID 7626578.
- ^ Amos CF, George MD (2006). "Clinical and laboratory testing of a silver-impregnated lens case". Cont Lens Anterior Eye. 29 (5): 247–55. doi:10.1016/j.clae.2006.09.007. PMID 17084102.
- ^ Mathews SM, Spallholz JE, Grimson MJ, Dubielzig RR, Gray T, Reid TW (2006). "Prevention of bacterial colonization of contact lenses with covalently attached selenium and effects on the rabbit cornea". Cornea. 25 (7): 806–14. doi:10.1097/01.ico.0000224636.57062.90. PMID 17068458. S2CID 25006245.
- ^ Santos L; Rodrigues D; Lira M; Oliveira R; Oliveira Real, ME; Vilar EY; Azeredo J (2007). "The effect of octylglucoside and sodium cholate in Staphylococcus epidermidis and Pseudomonas aeruginosa adhesion to soft contact lenses". Optom Vis Sci. 84 (5): 429–34. doi:10.1097/opx.0b013e318058a0cc. hdl:1822/6663. PMID 17502827. S2CID 2509161.
- ^ a b "Contacts Release Anesthesia to Eyes of Post-Surgery Patients". Archived from the original on 21 April 2013. Retrieved 4 April 2013.
- ^ "First Ever Switchable Telescopic Contact Lens". Forbes. Retrieved 23 March 2018.
- ^ Klepper, Robert K. (2005). Silent Films, 1877–1996: A Critical Guide to 646 Movies. McFarland. p. 373.
- ^ Yazigi, Monique P. (17 July 1994). "On Film, Them There Eyes Are Often Contact Lenses". New York Times.
Further reading
[edit]- Efron, Nathan (2002). Contact Lens Practice. Elsevier Health Sciences. ISBN 0-7506-4690-X.
- Heitz, Robert (2003, 2005 and 2014). "The History of Contact Lenses". In: Julius Hirschberg, History of Ophthalmology, vols. 11/3a, 11/3b, and 11/3c. Ostend, Belgium: Wayenborgh Publishing; Paraguay: Piribebuy. ISBN 978-90-6299-463-2.
