Arteriovenous malformation: Difference between revisions
→Society and culture: Removed a second non-notable. |
Shaidarolcz (talk | contribs) m Changed "Computerized tomography" to "Computed tomography" to fix a common error in nomenclature. The imaging modality is so named because the image is computed (reconstructed), not because it is performed by a computer. |
||
| (220 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
{{Short description|Abnormal connection between arteries and veins, bypassing the capillaries}} |
|||
{{See also|Cerebral arteriovenous malformation}} |
|||
{{About|the anomaly generally|its occurrence in the brain|Cerebral arteriovenous malformation}} |
|||
{{Infobox disease |
|||
{{Use mdy dates|date=March 2023}} |
|||
| Name = Arteriovenous malformation |
|||
{{Infobox medical condition |
|||
| Image = Arteriovenous malformation - brain - low mag.jpg |
|||
| name = Arteriovenous malformation |
|||
| Caption = [[Micrograph]] of an arteriovenous malformation in the brain. [[HPS stain]]. |
|||
| synonyms = AVM |
|||
| DiseasesDB = 15235 |
|||
| image = Arteriovenous malformation - brain - low mag.jpg |
|||
| ICD10 = {{ICD10|Q|27|3|q|20}}, {{ICD10|Q|28|0|q|20}}, {{ICD10|Q|28|2|q|20}} |
|||
| caption = [[Micrograph]] of an arteriovenous malformation in the brain. [[HPS stain]]. |
|||
| ICD9 = {{ICD9|747.6}}, {{ICD9|747.81}} |
|||
| pronounce = |
|||
| ICDO = |
|||
| field = [[Neurosurgery]] |
|||
| OMIM = |
|||
| symptoms = |
|||
| MedlinePlus = 000779 |
|||
| complications = |
|||
| eMedicineSubj = search |
|||
| onset = |
|||
| eMedicineTopic = Arteriovenous%20Malformation |
|||
| duration = |
|||
| MeshID = D001165 |
|||
| types = |
|||
| causes = |
|||
| risks = |
|||
| diagnosis = CT, MRI, MRA |
|||
| differential = |
|||
| prevention = |
|||
| treatment = |
|||
| medication = |
|||
| prognosis = |
|||
| frequency = |
|||
| deaths = |
|||
}} |
}} |
||
''' |
An '''arteriovenous malformation''' ('''AVM''') is an abnormal connection between [[arteries]] and [[vein]]s, bypassing the [[capillary]] system. Usually [[congenital]], this [[vascular anomaly]] is widely known because of its occurrence in the [[central nervous system]] (usually as a [[cerebral AVM]]), but can appear anywhere in the body. The symptoms of AVMs can range from [[Asymptomatic|none at all]] to intense pain or bleeding, and they can lead to other serious medical problems.<ref name="NINDS" /> |
||
AVMs are usually [[congenital]] and belong to the [[RASopathy|RASopathies]]. |
|||
The genetic transmission patterns of AVM, if any, are unknown. AVM is not generally thought to be an inherited disorder, unless in the context of a specific hereditary [[syndrome]]. |
|||
== Signs and symptoms == |
== Signs and symptoms == |
||
Symptoms of |
Symptoms of AVMs vary according to their location. Most [[neurological]] AVMs produce few to [[Asymptomatic|no symptoms]]. Often the malformation is discovered as part of an [[autopsy]] or during treatment of an unrelated disorder (an "[[incidental finding]]"); in rare cases, its expansion or a micro-bleed from an AVM in the brain can cause [[epilepsy]], [[neurological deficit]], or [[pain]].<ref>{{cite web|title=Arteriovenous Malformations|url=https://www.hopkinsmedicine.org/health/conditions-and-diseases/arteriovenous-malformations|website=[[Johns Hopkins Medicine]]|access-date=26 October 2022}}</ref> |
||
The most general symptoms of a cerebral AVM include [[headache]] and [[epilepsy]], with more specific symptoms occurring that normally depend on the location of the malformation and the individual. Such possible symptoms include:<ref name=NINDS>{{NINDS|avms|Arteriovenous Malformation Information Page}}</ref> |
|||
The most general symptoms of a [[cerebral AVM]] include [[headache]]s and epileptic [[seizure]]s, with more specific symptoms that normally depend on its location and the individual, including:<ref name=NINDS>{{NINDS|Arteriovenous-Malformation|Arteriovenous Malformation Information Page}}<!--An older form of this page can be found at https://web.archive.org/web/20161205043316/http://www.ninds.nih.gov:80/disorders/avms/detail_avms.htm --></ref> |
|||
* Difficulties with movement or coordination, including [[muscle weakness]] and even [[paralysis]]; |
|||
* Difficulties with movement coordination, including [[muscle weakness]] and even [[paralysis]]; |
|||
* [[Vertigo (medical)|vertigo]] (dizziness); |
|||
* [[Vertigo]] (dizziness); |
|||
* Difficulties of speech ([[dysarthria]]) and communication, such as [[aphasia]]; |
* Difficulties of speech ([[dysarthria]]) and communication, such as [[aphasia]]; |
||
* Difficulties with everyday activities, such as [[apraxia]]; |
* Difficulties with everyday activities, such as [[apraxia]]; |
||
* Abnormal sensations (numbness, tingling, or spontaneous |
* Abnormal sensations (numbness, tingling, or spontaneous pain); |
||
* Memory and thought-related problems, such as [[confusion]], [[dementia]] or [[hallucination]]s. |
* Memory and thought-related problems, such as [[confusion]], [[dementia]], or [[hallucination]]s. |
||
Cerebral AVMs may present in a number of ways |
Cerebral AVMs may present themselves in a number of different ways:{{citation needed|date=March 2023}} |
||
* [[Bleeding]] (45% of cases) |
|||
* "[[parkinsonism]]" 4 symptoms in [[Parkinson's disease]]. |
|||
* Acute onset of severe headache. May be described as the worst headache of the patient's life. Depending on the location of bleeding, may be associated with new fixed neurologic deficit. In unruptured brain AVMs, the risk of spontaneous bleeding may be as low as 1% per year. After a first rupture, the annual bleeding risk may increase to more than 5%.<ref>{{cite journal |last1=Stapf |first1=C. |last2=Mast |first2=H. |last3=Sciacca |first3=R. R. |last4=Choi |first4=J. H. |last5=Khaw |first5=A. V. |author6-link=E. Sander Connolly|last6=Connolly |first6=E. S. |last7=Pile-Spellman |first7=J. |last8=Mohr |first8=J. P. |title=Predictors of hemorrhage in patients with untreated brain arteriovenous malformation |journal=Neurology |volume=66 |issue=9 |pages=1350–5 |year=2006 |pmid=16682666 |doi=10.1212/01.wnl.0000210524.68507.87 |s2cid=22004276 }}</ref> |
|||
* Seizure or brain seizure (46%). Depending on the place of the AVM, it can contribute to [[loss of vision]]. |
|||
* Headache (34%) |
|||
* Progressive neurologic deficit (21%) |
|||
** May be caused by mass effect or venous dilatations. Presence and nature of the deficit depend on location of lesion and the draining veins.<ref>{{cite journal |last1=Choi |first1=J.H. |last2=Mast |first2=H. |last3=Hartmann |first3=A. |last4=Marshall |first4=R.S. |last5=Pile-Spellman |first5=J. |last6=Mohr |first6=J.P. |last7=Stapf |first7=C. |title=Clinical and morphological determinants of focal neurological deficits in patients with unruptured brain arteriovenous malformation |journal=Journal of the Neurological Sciences |volume=287 |issue=1–2 |pages=126–30 |year=2009 |pmid=19729171 |pmc=2783734 |doi=10.1016/j.jns.2009.08.011 }}</ref> |
|||
* Pediatric patients |
|||
** [[Heart failure]] |
|||
** [[Macrocephaly]] |
|||
** Prominent scalp veins |
|||
=== Pulmonary arteriovenous malformations === |
|||
*Hemorrhage (45% of cases) |
|||
**Acute onset of severe headache. May be described as the worst headache of the patient's life. Depending on the location of hemorrhage, may be associated with new fixed neurologic deficit. In unruptured brain AVMs, the risk of spontaneous hemorrhage may be as low as 1% per year. After a first rupture, the annual bleeding risk may increase to more than 5%.<ref>{{cite journal |author=Stapf C, Mast H, Sciacca RR, ''et al.'' |title=Predictors of hemorrhage in patients with untreated brain arteriovenous malformation |journal=Neurology |volume=66 |issue=9 |pages=1350–5 |date=May 2006 |pmid=16682666 |doi=10.1212/01.wnl.0000210524.68507.87 |url=http://www.neurology.org/cgi/pmidlookup?view=long&pmid=16682666}}</ref> |
|||
Pulmonary arteriovenous malformations are abnormal communications between the veins and arteries of the [[pulmonary circulation]], leading to a right-to-left blood shunt.<ref name="Reichert">{{cite journal |last1=Reichert |first1=M |last2=Kerber |first2=S |last3=Alkoudmani |first3=I |last4=Bodner |first4=J |title=Management of a solitary pulmonary arteriovenous malformation by video-assisted thoracoscopic surgery and anatomic lingula resection: video and review. |journal=Surgical Endoscopy |date=April 2016 |volume=30 |issue=4 |pages=1667–9 |doi=10.1007/s00464-015-4337-0 |pmid=26156615|s2cid=22394114 }}</ref><ref name="Tellapuri">{{cite journal |last1=Tellapuri |first1=S |last2=Park |first2=HS |last3=Kalva |first3=SP |title=Pulmonary arteriovenous malformations. |journal=The International Journal of Cardiovascular Imaging |date=August 2019 |volume=35 |issue=8 |pages=1421–1428 |doi=10.1007/s10554-018-1479-x |pmid=30386957|s2cid=53144651 }}</ref> |
|||
*Seizure (46%) |
|||
They have no symptoms in up to 29% of all cases,<ref>{{Cite book | author=Goodenberger DM | title=Fishman's Pulmonary Diseases and Disorders | chapter=Chapter 84 Pulmonary arteriovenous malformations | publisher=McGraw-Hill | year=2008 | page=1470 | edition=4th | isbn=978-0-07-145739-2 }}</ref> however they can give rise to serious complications including [[hemorrhage]], and infection.<ref name="Reichert"/> They are most commonly associated with [[hereditary hemorrhagic telangiectasia]].<ref name="Tellapuri"/> |
|||
*Headache (34%) |
|||
*Progressive neurologic deficit (21%) |
|||
**May be caused by mass effect or venous dilatations. Presence and nature of deficit depend on location of lesion and the draining veins.<ref>{{cite journal |author=Choi JH, Mast H, Hartmann A, ''et al.'' |title=Clinical and morphological determinants of focal neurological deficits in patients with unruptured brain arteriovenous malformation |journal=J. Neurol. Sci. |volume=287 |issue=1-2 |pages=126–30 |date=December 2009 |pmid=19729171 |pmc=2783734 |doi=10.1016/j.jns.2009.08.011 |url=http://linkinghub.elsevier.com/retrieve/pii/S0022-510X(09)00762-X}}</ref> |
|||
*Pediatric patients |
|||
**Heart failure |
|||
**Macrocephaly |
|||
**Prominent scalp veins |
|||
== Genetics == |
== Genetics == |
||
AVMs are usually [[congenital]] and are part of the [[RASopathy]] family of developmental syndromes. |
|||
Can occur due to autosomal dominant diseases, such as [[Hereditary Hemorrhagic Telangiectasia]].{{citation needed|date=August 2012}} |
|||
The understanding of the anomaly's [[genetic transmission]] patterns are incomplete, but there are known genetic [[mutation]]s (for instance in the [[epithelial]] line, tumor suppressor [[PTEN gene]]) which can lead to an increased occurrence throughout the body.{{Citation needed|date=March 2023}} |
|||
The anomaly can occur due to autosomal dominant diseases, such as [[hereditary hemorrhagic telangiectasia]].<ref>{{Cite web |title=Hereditary hemorrhagic telangiectasia: MedlinePlus Genetics |url=https://medlineplus.gov/genetics/condition/hereditary-hemorrhagic-telangiectasia/ |access-date=2022-07-23 |website=medlineplus.gov |language=en}}</ref> |
|||
==Pathophysiology== |
|||
In a normal functioning human body, arteries carry blood away from the heart to the lungs or the rest of the body, where the blood passes through capillaries, and veins return the blood to heart. An AVM interferes with this process by forming a direct connection of the arteries and veins. AVMs can cause intense pain and lead to serious medical problems. Although AVMs are often associated with the brain and spinal cord, they can develop in any part of the body. |
|||
==Pathophysiology== |
|||
Arteries and veins are part of the [[Circulatory system|human cardiovascular system]]. Normally, the arteries in the vascular system carry oxygen-rich blood, except in the case of the pulmonary artery. Structurally, arteries divide and sub-divide repeatedly, eventually forming a sponge-like [[capillary bed]]. Blood moves through the [[Capillary|capillaries]], giving up oxygen and taking up waste products, including {{chem|link=Carbon dioxide|CO|2}}, from the surrounding cells. Capillaries in turn successively join together to form veins that carry blood away. The heart acts to pump blood through arteries and uptake the venous blood. |
|||
In the [[circulatory system]], arteries carry blood away from the heart to the [[lung]]s and the rest of the body, where the blood normally passes through [[capillaries]]—where oxygen is released and waste products like [[carbon dioxide]] ({{CO2}}) absorbed—before veins return blood to the heart.<ref>{{Cite web |date=2021-09-21 |title=Circulatory System: Anatomy and Function |url=https://my.clevelandclinic.org/health/body/21775-circulatory-system |access-date=2023-03-08 |website=[[Cleveland Clinic]] |language=en}}</ref> An AVM interferes with this process by forming a direct connection of the arteries and veins, bypassing the [[capillary bed]].<ref name=":0" /> AVMs can cause intense pain and lead to serious medical problems. Although AVMs are often associated with the brain and spinal cord, they can develop in other parts of the body.<ref name=":0">{{Cite journal |last1=Schimmel |first1=Katharina |last2=Ali |first2=Md Khadem |last3=Tan |first3=Serena Y. |last4=Teng |first4=Joyce |last5=Do |first5=Huy M. |last6=Steinberg |first6=Gary K. |last7=Stevenson |first7=David A. |last8=Spiekerkoetter |first8=Edda |date=2021-08-21 |title=Arteriovenous Malformations—Current Understanding of the Pathogenesis with Implications for Treatment |journal=International Journal of Molecular Sciences |volume=22 |issue=16 |pages=9037 |doi=10.3390/ijms22169037 |issn=1422-0067 |pmc=8396465 |pmid=34445743|doi-access=free }}</ref> |
|||
As an AVM lacks the dampening effect of capillaries on the blood flow, the AVM can get progressively larger over time as the amount of blood flowing through it increases, forcing the heart to work harder to keep up with the extra blood flow. It also causes the surrounding area to be deprived of the functions of the capillaries. The resulting tangle of [[blood vessel]]s, often called a ''nidus'' ([[Latin]] for 'nest'), has no capillaries. It can be extremely fragile and prone to bleeding because of the abnormally direct connections between high-pressure arteries and low-pressure veins.<ref>{{Cite journal |last1=Mouchtouris |first1=Nikolaos |last2=Jabbour |first2=Pascal M. |last3=Starke |first3=Robert M. |last4=Hasan |first4=David M. |last5=Zanaty |first5=Mario |last6=Theofanis |first6=Thana |last7=Ding |first7=Dale |last8=Tjoumakaris |first8=Stavropoula I. |last9=Dumont |first9=Aaron S. |last10=Ghobrial |first10=George M. |last11=Kung |first11=David |date=February 2015 |title=Biology of cerebral arteriovenous malformations with a focus on inflammation |journal=Journal of Cerebral Blood Flow and Metabolism|volume=35 |issue=2 |pages=167–175 |doi=10.1038/jcbfm.2014.179 |pmc=4426734 |pmid=25407267}}</ref> One indicator is a pulsing 'whoosh' sound caused by rapid blood flow through arteries and veins, which has been given the term ''bruit'' ([[French language|French]] for 'noise'). If the AVM is severe, this may produce an audible symptom which can interfere with hearing and sleep as well as cause psychological distress.<ref name="NINDS" /> |
|||
==Diagnosis== |
==Diagnosis== |
||
[[File:PleftkidneyAVM1.png|thumb|An arterial venous malformation of the left kidney and a simple cyst of the right kidney]] |
[[File:PleftkidneyAVM1.png|thumb|An arterial venous malformation of the left kidney and a simple cyst of the right kidney]] |
||
[[File:PleftkidneyAVM2.png|thumb|An arterial venous malformation of the left kidney leading to |
[[File:PleftkidneyAVM2.png|thumb|An arterial venous malformation of the left kidney leading to [[aneurysm]]al dilatation of the left [[renal vein]] and [[inferior vena cava]]]] |
||
AVMs are diagnosed primarily by the following methods: |
|||
AVMs are diagnosed primarily by the following [[Medical imaging|imaging]] methods:<ref>{{cite journal |last1=Mokin |first1=Maxim |title=Novel Multimodality Imaging Techniques for Diagnosis and Evaluation of Arteriovenous Malformations |journal=Neurologic Clinics |date=February 2014 |volume=32 |issue=1 |pages=225–236 |doi=10.1016/j.ncl.2013.07.006 |pmid=24287392 |url=https://www.sciencedirect.com/science/article/pii/S0733861913000893 |access-date=February 11, 2023}}</ref> |
|||
* [[Computerized tomography|Computerized Tomography (CT)]] scan is a noninvasive X-ray to view the anatomical structures within the brain to detect blood in or around the brain. A newer technology called CT angiography involves the injection of contrast into the blood stream to view the arteries of the brain. This type of test provides the best pictures of blood vessels through angiography and soft tissues through CT. |
|||
* [[Computed tomography]] (CT) scan is a noninvasive X-ray to view the anatomical structures within the brain to detect blood in or around the brain. A newer technology called [[CT angiography]] involves the injection of [[Radiocontrast agent|contrast]] into the blood stream to view the arteries of the brain. This type of test provides the best pictures of blood vessels through angiography and soft tissues through CT. |
|||
* [[Magnetic resonance imaging|Magnetic Resonance Imaging (MRI)]] scan is a noninvasive test, which uses a magnetic field and radio-frequency waves to give a detailed view of the soft tissues of the brain. |
|||
* [[Magnetic resonance imaging]] (MRI) scan is a noninvasive test, which uses a magnetic field and radio-frequency waves to give a detailed view of the soft tissues of the brain. |
|||
* An MRA ([[Magnetic resonance angiogram|Magnetic Resonance Angiogram]]) is scan created using magnetic resonance imaging to specifically image the blood vessels, as well as the structures of the brain. A magnetic resonance angiogram can be an invasive procedure, involving the introduction of contrast dyes (e.g., gadolinium MR contrast agents) into the vasculature of a patient using a catheter inserted into an artery and passed through the blood vessels to the brain. Once the catheter is in place, the contrast dye is injected into the bloodstream and the MR images are taken. Additionally or alternatively, flow-dependent or other contrast-free magnetic resonance imaging techniques can be used to determine the location and other properties of the vasculature. |
|||
* [[Magnetic resonance angiography]] (MRA) – scans created using magnetic resonance imaging to specifically image the blood vessels and structures of the brain. A magnetic resonance angiogram can be an invasive procedure, involving the introduction of contrast dyes (e.g., [[gadolinium]] MR [[contrast agent]]s) into the vasculature (circulatory system) of a patient using a [[catheter]] inserted into an artery and passed through the blood vessels to the brain. Once the catheter is in place, the contrast dye is injected into the bloodstream and the MR images are taken. Additionally or alternatively, flow-dependent or other contrast-free magnetic resonance imaging techniques can be used to determine the location and other properties of the vasculature. |
|||
AVMs can occur in various parts of the body: |
AVMs can occur in various parts of the body: |
||
* [[human brain|brain]] |
* [[human brain|brain]] ([[Cerebral arteriovenous malformation|cerebral AV malformation]]) |
||
* [[spleen]]<ref name="pmid17145440">{{cite journal | |
* [[spleen]]<ref name="pmid17145440">{{cite journal |last1=Agrawal |first1=Aditya |last2=Whitehouse |first2=Richard |last3=Johnson |first3=Robert W. |last4=Augustine |first4=Titus |title=Giant splenic artery aneurysm associated with arteriovenous malformation |journal=Journal of Vascular Surgery |volume=44 |issue=6 |pages=1345–9 |year=2006 |pmid=17145440 |doi=10.1016/j.jvs.2006.06.049 |doi-access=free }}</ref> |
||
* [[human lung|lung]]<ref name="pmid18294908">{{cite journal | |
* [[human lung|lung]]<ref name="pmid18294908">{{cite journal |last1=Chowdhury |first1=Ujjwal K. |last2=Kothari |first2=Shyam S. |last3=Bishnoi |first3=Arvind K. |last4=Gupta |first4=Ruchika |last5=Mittal |first5=Chander M. |last6=Reddy |first6=Srikrishna |title=Successful Lobectomy for Pulmonary Arteriovenous Malformation Causing Recurrent Massive Haemoptysis |journal=Heart, Lung and Circulation |volume=18 |issue=2 |pages=135–9 |year=2009 |pmid=18294908 |doi=10.1016/j.hlc.2007.11.142 }}</ref><ref name="dupeRef1">{{Cite journal|last1=Cusumano|first1=Lucas R.|last2=Duckwiler|first2=Gary R.|last3=Roberts|first3=Dustin G.|last4=McWilliams|first4=Justin P.|date=2019-08-30|title=Treatment of Recurrent Pulmonary Arteriovenous Malformations: Comparison of Proximal Versus Distal Embolization Technique|journal=CardioVascular and Interventional Radiology|volume=43|issue=1|pages=29–36|doi=10.1007/s00270-019-02328-0|issn=1432-086X|pmid=31471718|s2cid=201675132}}</ref> |
||
* [[kidney]]<ref name="pmid16794894">{{cite journal | |
* [[kidney]]<ref name="pmid16794894">{{cite journal |last1=Barley |first1=Fay L. |last2=Kessel |first2=David |last3=Nicholson |first3=Tony |last4=Robertson |first4=Iain |title=Selective Embolization of Large Symptomatic Iatrogenic Renal Transplant Arteriovenous Fistula |journal=CardioVascular and Interventional Radiology |volume=29 |issue=6 |pages=1084–7 |year=2006 |pmid=16794894 |doi=10.1007/s00270-005-0265-z |s2cid=9335750 }}</ref> |
||
* [[spinal cord]]<ref name="pmid15730991">{{cite journal | |
* [[spinal cord]]<ref name="pmid15730991">{{cite journal |last1=Kishi |first1=K |last2=Shirai |first2=S |last3=Sonomura |first3=T |last4=Sato |first4=M |title=Selective conformal radiotherapy for arteriovenous malformation involving the spinal cord |journal=The British Journal of Radiology |volume=78 |issue=927 |pages=252–4 |year=2005 |pmid=15730991 |doi=10.1259/bjr/50653404 }}</ref> |
||
* [[liver]]<ref name="pmid7650340">{{cite journal | |
* [[liver]]<ref name="pmid7650340">{{cite journal |last1=Bauer |first1=Tilman |last2=Britton |first2=Peter |last3=Lomas |first3=David |last4=Wight |first4=Derek G.D. |last5=Friend |first5=Peter J. |last6=Alexander |first6=Graeme J.M. |title=Liver transplantation for hepatic arteriovenous malformation in hereditary haemorrhagic telangiectasia |journal=Journal of Hepatology |volume=22 |issue=5 |pages=586–90 |year=1995 |pmid=7650340 |doi=10.1016/0168-8278(95)80455-2 }}</ref> |
||
* [[intercostal space]]<ref name="pmid17056881">{{cite journal | |
* [[intercostal space]]<ref name="pmid17056881">{{cite journal |last1=Rivera |first1=Peter P. |last2=Kole |first2=Max K. |last3=Pelz |first3=David M. |last4=Gulka |first4=Irene B. |last5=McKenzie |first5=F. Neil |last6=Lownie |first6=Stephen P. |title=Congenital Intercostal Arteriovenous Malformation |journal=American Journal of Roentgenology |volume=187 |issue=5 |pages=W503–6 |year=2006 |pmid=17056881 |doi=10.2214/AJR.05.0367 }}</ref> |
||
* [[Iris (anatomy)|iris]]<ref name="pmid16534057">{{cite journal | |
* [[Iris (anatomy)|iris]]<ref name="pmid16534057">{{cite journal |last1=Shields |first1=Jerry A. |last2=Streicher |first2=Theodor F. E. |last3=Spirkova |first3=Jane H. J. |last4=Stubna |first4=Michal |last5=Shields |first5=Carol L. |title=Arteriovenous Malformation of the Iris in 14 Cases |journal=Archives of Ophthalmology |volume=124 |issue=3 |pages=370–5 |year=2006 |pmid=16534057 |doi=10.1001/archopht.124.3.370 |doi-access= }}</ref> |
||
* [[spermatic cord]]<ref name="pmid17939869">{{cite journal | |
* [[spermatic cord]]<ref name="pmid17939869">{{cite journal |last1=Sountoulides |first1=Petros |last2=Bantis |first2=Athanasios |last3=Asouhidou |first3=Irene |last4=Aggelonidou |first4=Hellen |title=Arteriovenous malformation of the spermatic cord as the cause of acute scrotal pain: a case report |journal=Journal of Medical Case Reports |volume=1 |pages=110 |year=2007 |pmid=17939869 |pmc=2194703 |doi=10.1186/1752-1947-1-110 |doi-access=free }}</ref> |
||
* extremities – arm, shoulder, etc. |
|||
*limbs |
|||
AVMs may occur in isolation or as a part of another disease (for example, [[ |
AVMs may occur in isolation or as a part of another disease (for example, [[Sturge-Weber syndrome]] or [[hereditary hemorrhagic telangiectasia]]).<ref name="National Institute of Neurological Disorders and Stroke 2024 s064">{{cite web | title=Arteriovenous Malformations (AVMs) | website=National Institute of Neurological Disorders and Stroke, [[NIH]] | date=February 22, 2024 | url=https://www.ninds.nih.gov/health-information/disorders/arteriovenous-malformations-avms | access-date=March 30, 2024}}</ref> |
||
AVMs have been shown to be associated with [[ |
AVMs have been shown to be associated with [[aortic stenosis]].<ref>{{cite journal |last1=Batur |first1=Pelin |last2=Stewart |first2=William J. |last3=Isaacson |first3=J. Harry |title=Increased Prevalence of Aortic Stenosis in Patients With Arteriovenous Malformations of the Gastrointestinal Tract in Heyde Syndrome |journal=Archives of Internal Medicine |volume=163 |issue=15 |pages=1821–4 |year=2003 |pmid=12912718 |doi=10.1001/archinte.163.15.1821 |doi-access= }}</ref> |
||
Bleeding from an AVM can be relatively mild or devastating. It can cause severe and less often fatal [[stroke]]s. |
Bleeding from an AVM can be relatively mild or devastating. It can cause severe and less often fatal [[stroke]]s.<ref name="NINDS" /> |
||
<!-- == Screening == --> |
|||
== Treatment == |
== Treatment == |
||
Treatment for |
[[Cerebral arteriovenous malformation#Treatment|Treatment for AVMs in the brain]] can be symptomatic, and patients should be followed by a neurologist for any seizures, headaches, or focal neurologic deficits. AVM-specific treatment may also involve [[Interventional neuroradiology|endovascular embolization]], neurosurgery or radiosurgery.<ref name=NINDS/> |
||
Embolization, that is, cutting off the blood supply to the AVM with coils |
Embolization, that is, cutting off the blood supply to the AVM with coils, particles, acrylates, or polymers introduced by a radiographically guided catheter, may be used in addition to neurosurgery or radiosurgery, but is rarely successful in isolation except in smaller AVMs.<ref>{{Cite journal|last1=Jafar|first1=Jafar J.|last2=Davis|first2=Adam J.|last3=Berenstein|first3=Alejandro|last4=Choi|first4=In Sup|last5=Kupersmith|first5=Mark J.|date=1993-01-01|title=The effect of embolization with N-butyl cyanoacrylate prior to surgical resection of cerebral arteriovenous malformations|journal=Journal of Neurosurgery|volume=78|issue=1|pages=60–69|doi=10.3171/jns.1993.78.1.0060|pmid=8416244|issn=0022-3085}}</ref> A [[gamma knife]] may also be used.<ref>{{cite web |url=http://www.muh.org.au/ServicesSpecialties/GammaKnife/ForPatients/ConditionsWeTreat.aspx |archive-url=https://web.archive.org/web/20130613164614/http://www.muh.org.au/ServicesSpecialties/GammaKnife/ForPatients/ConditionsWeTreat.aspx |archive-date=2013-06-13 |title=Conditions We Treat |publisher=Macquarie University Hospital }}</ref> |
||
If a cerebral AVM is detected before a stroke occurs, usually the arteries feeding blood into the nidus can be closed off to avert the danger.<ref>{{Cite web |title=Arteriovenous Malformations |url=https://lsom.uthscsa.edu/neurosurgery/clinical-practice/arteriovenous-malformations/ |access-date=2023-06-26 |website=Neurosurgery |language=en-US}}</ref> Interventional therapy may be relatively risky in the short term.<ref name="aruba02">{{cite web |date=January 29, 2014 |title=A Randomized Trial of Unruptured Brain Arteriovenous Malformations (ARUBA) |url=http://www.ninds.nih.gov/news_and_events/news_articles/ARUBA_trial_results.htm |archive-url=https://web.archive.org/web/20160704222521/http://www.ninds.nih.gov/news_and_events/news_articles/ARUBA_trial_results.htm |archive-date=2016-07-04 |access-date=2023-03-06 |website=[[National Institute of Neurological Disorders and Stroke]]}}</ref> |
|||
The Spetzler-Martin grading system developed at the [[Barrow Neurological Institute]] is utilized by neurosurgeons to determine operative versus nonoperative management of AVMs. |
|||
Treatment of lung AVMs is typically performed with endovascular embolization alone, which is considered the standard of care.<ref name="dupeRef1" /> |
|||
== Epidemiology == |
== Epidemiology == |
||
The estimated detection rate of AVM in the US general population is 1.4/100,000 per year.<ref>{{cite journal | |
The estimated detection rate of AVM in the US general population is 1.4/100,000 per year.<ref>{{cite journal |last1=Stapf |first1=C. |last2=Mast |first2=H. |last3=Sciacca |first3=R.R. |last4=Berenstein |first4=A. |last5=Nelson |first5=P.K. |last6=Gobin |first6=Y.P. |last7=Pile-Spellman |first7=J. |last8=Mohr |first8=J.P. |title=The New York Islands AVM Study: Design, Study Progress, and Initial Results |journal=Stroke |volume=34 |issue=5 |pages=e29–33 |year=2003 |pmid=12690217 |doi=10.1161/01.STR.0000068784.36838.19 |doi-access=free }}</ref> This is approximately one-fifth to one-seventh the incidence of [[intracranial aneurysm]]s. An estimated 300,000 Americans have AVMs, of whom 12% (approximately 36,000) will exhibit symptoms of greatly varying severity.<ref name=NINDS/> |
||
==History== |
==History== |
||
[[Hubert von Luschka]] (1820–1875) and [[Rudolf Virchow]] (1821–1902) first described arteriovenous malformations in the mid-1800s. [[Herbert Olivecrona]] (1891–1980) performed the first surgical excision of an intracranial AVM in 1932. |
|||
== |
==Society and culture== |
||
=== Notable cases === |
|||
*American [[basketball]] player [[AJ Price]] nearly died from AVM in 2004 while a student at the [[University of Connecticut]]. |
|||
* Actor [[Ricardo Montalbán]] was born with spinal AVM.<ref>[https://www.youtube.com/watch?v=x39-hR5rGlc "Ricardo Montalban tribute"] YouTube, acceptance speech video of Easter Seals Lifetime Achievement Award</ref> During the filming of the 1951 film ''[[Across the Wide Missouri (film)|Across the Wide Missouri]]'', Montalbán was thrown from his horse, knocked unconscious, and trampled by another horse which aggravated his AVM and resulted in a painful back injury that never healed. The pain increased as he aged, and in 1993, Montalbán underwent {{frac|9|1|2}} hours of spinal surgery which left him paralyzed below the waist and using a wheelchair.<ref>{{cite web |title=Inside |url=http://www.mahalo.com/Ricardo_Montalban |access-date=17 March 2018 |website=mahalo.com}}</ref> |
|||
* Composer and lyricist [[William Finn]] was diagnosed with AVM and underwent gamma knife surgery in September 1992, soon after he won the 1992 [[Tony Award]] for best musical, awarded to "[[Falsettos]]".<ref>{{cite news |last=Pall |first=Ellen |date=14 June 1998 |title=The Long-Running Musical of William Finn's Life |newspaper=The New York Times |url=https://www.nytimes.com/1998/06/14/magazine/the-long-running-musical-of-william-finn-s-life.html |access-date=17 March 2018}}</ref> Finn wrote the 1998 Off-Broadway musical ''[[A New Brain]]'' about the experience. |
|||
* [[Phoenix Suns]] point guard [[AJ Price]] nearly died from AVM in 2004 while a student at the [[University of Connecticut]]. |
|||
* On December 13, 2006, Senator [[Tim Johnson (South Dakota politician)|Tim Johnson]] of South Dakota was diagnosed with AVM and treated at [[George Washington University Hospital]].<ref>{{cite news |title=Sen. Johnson recovering after brain surgery |agency=AP |date=December 14, 2006 |url=https://www.nbcnews.com/id/wbna16199440}}</ref> |
|||
* Actor/comedian [[T. J. Miller]] was diagnosed with AVM in 2010; Miller had a seizure and was unable to sleep for a period. He successfully underwent surgery that had a mortality rate of 10%.<ref>{{cite podcast |host=[[Pete Holmes|Holmes, Pete]] |title=''You Made It Weird with Pete Holmes'' |website=[[You Made It Weird]] #2: TJ Miller |publisher=Nerdist Industries |date=October 27, 2011 |url=http://www.nerdist.com/2011/10/you-made-it-weird-2-tj-miller/ |time=37:45 |access-date=December 5, 2012 |archive-url=https://web.archive.org/web/20130212035323/http://www.nerdist.com/2011/10/you-made-it-weird-2-tj-miller/ |archive-date=February 12, 2013 |url-status=dead}}</ref> |
|||
* On August 3, 2011, [[Mike Patterson (American football)|Mike Patterson]] of the [[Philadelphia Eagles]] collapsed on the field and had a seizure during a practice, leading to him being diagnosed with AVM.<ref>{{cite web |date=2011-08-04 |title=Mike Patterson's Collapse Reportedly Related To Brain AVM |url=https://www.sbnation.com/2011/8/4/2343821/mike-patterson-collapse-eagles-practice |access-date=17 March 2018 |website=sbnation.com}}</ref> |
|||
* Former Florida Gators and Oakland Raiders linebacker [[Neiron Ball]] was diagnosed with AVM in 2011 while playing for [[University of florida gators football|Florida]], but recovered and was cleared to play. On September 16, 2018, Ball was placed in a medically induced coma due to complications of the disease, which lasted until his death on September 10, 2019.<ref>{{cite news |date=September 26, 2018 |title=Neiron Ball, former Raiders LB, in medically induced coma after aneurysm |work=ESPN |url=https://www.espn.com/nfl/story/_/id/24796861/neiron-ball-former-oakland-raiders-lb-medically-induced-coma-aneurysm}}</ref> |
|||
* Indonesian actress {{illm|Egidia Savitri|id}} died from complications of AVM on November 29, 2013.<ref>{{cite news |last1=Suhendra |first1=Ichsan |title=Pesinetron Egidia Savitri Telah Pergi |language=id |work=KOMPAS.com |agency=Kompas Cyber Media |url=https://entertainment.kompas.com/read/2013/11/29/1920142/Pesinetron.Egidia.Savitri.Telah.Pergi |access-date=15 May 2019}}</ref> |
|||
* Jazz guitarist [[Pat Martino]] experienced an AVM and subsequently developed [[amnesia]] and [[manic depression]]. He eventually re-learned to play the guitar by listening to his own recordings from before the [[aneurysm]].<ref>Vida, Vendela. Confidence, or the Appearance of Confidence: The Best of the Believer Music Interviews. No ed. San Francisco, CA: Believer, a Tiny Division of McSweeney's Which Is Also Tiny, 2014. Print.</ref> |
|||
* YouTube vlogger [[Nikki Lilly]] (Nikki Christou), winner of the [[Junior Bake Off (series 4)|2016 season]] of ''[[Junior Bake Off]]'' was born with AVM, which has resulted in some facial disfigurement.<ref>{{cite news|title = Junior Bake Off 2016 Winner announced|date = 25 November 2016|access-date = 9 April 2017|url = http://www.bbc.co.uk/mediacentre/latestnews/2016/junior-bake-off-winner|publisher = [[BBC Online]]|website = [[BBC Media Centre]]}}</ref> |
|||
* Country music singer [[Drake White]] was diagnosed with AVM in January 2019, and is undergoing treatment. |
|||
=== Cultural depictions === |
|||
*On December 13, 2006, [[United States Senate|Senator]] [[Tim Johnson (Politician)|Tim Johnson]] was diagnosed with AVM and treated at [[George Washington University Hospital]].<ref>{{cite news |title=Sen. Johnson recovering after brain surgery |agency=AP |date=December 14, 2006 |url=http://www.msnbc.msn.com/id/16199440/}}</ref> |
|||
* In the HBO series ''[[Six Feet Under (TV series)|Six Feet Under]]'' (2001), main character [[Nate Fisher (Six Feet Under)|Nate Fisher]] discovers he has an AVM after being in a car accident and getting a precautionary cat scan at the hospital during Season 1. His AVM becomes a key focus during Season 2 and again in Season 5. |
|||
* In season 1 episode 9 of ''[[House (TV series)|House]]'' (2004), titled "DNR", a jazz musician has an AVM and is misdiagnosed with [[ALS]]. Two season three episodes also involve AVM - "Top Secret" (episode 16), in which a veteran who believes himself to be suffering from [[Gulf War syndrome]] is found to have spinal and pulmonary AVM from hereditary hemorrhagic telangiectasia; and "Resignation" (episode 22), where the patient developed AVM in her intestines after drinking pipe cleaner fluid in a suicide attempt. |
|||
*On August 3, 2011, [[Mike Patterson (American football)|Mike Patterson]] of the [[Philadelphia Eagles]] collapsed on the field and suffered a seizure during a practice. After he collapsed, Patterson was rushed to the hospital where he was diagnosed with AVM.<ref>[http://www.sbnation.com/2011/8/4/2343821/mike-patterson-collapse-eagles-practice "Mike Patterson's Collapse Reportedly Related To Brain AVM"]</ref> |
|||
* In the 2005 Lifetime film [[Dawn Anna]], the titular character learns she has AVM, and undergoes a serious operation and subsequent rehabilitation, which she recovers from. |
|||
*''[[Six Feet Under (TV series)|Six Feet Under]]'', an American television series that ran on HBO from 2001–2005, featured a protagonist, [[Nate Fisher]], who suffered from AVM, a recurring feature in the storyline of this character. |
|||
*In the episode [[DNR (House)|"DNR"]] of the TV series ''[[House M.D.]]'', the patient was finally diagnosed with an AVM. |
|||
*In the episode "Save Me" of season 1 of the TV series ''[[Grey's Anatomy]]'', a psychic was diagnosed with an AVM in his left temporal lobe. |
|||
*On August 1, 2007, NIH/NINDS decides to launch the first international study evaluating the best treatment strategy for patients with unruptured brain AVMs: ARUBA — A Randomized trial of Unruptured Brain AVMs, which was stopped in spring of 2013.<ref>{{ClinicalTrialsGov|NCT00389181|A Randomized Trial of Unruptured Brain AVMs (ARUBA)}}</ref> |
|||
*Actor [[Ricardo Montalbán]] was born with spinal AVM.<ref>[http://www.youtube.com/watch?NR=1&feature=endscreen&v=x39-hR5rGlc "Ricardo Montalban tribute"] YouTube, acceptance speech video of Easter Seals Lifetime Achievement Award</ref> During the filming of the 1951 film ''[[Across the Wide Missouri (film)|Across the Wide Missouri]]'', Montalbán was thrown from his horse, knocked unconscious, and trampled by another horse which aggravated his AVM and resulted in a painful back injury that never healed. The pain increased as he aged, and in 1993, Montalbán underwent 9½ hours of spinal surgery which left him paralysed below the waist and using a wheelchair.<ref>[http://www.mahalo.com/Ricardo_Montalban Mahalo Answers: Ricardo Montalban]</ref><ref>[http://www.nndb.com/people/748/000022682/ NNDB: Ricardo Montalban]</ref>{{verify credibility|date=September 2013}} |
|||
*Actor/comedian [[T. J. Miller]] was diagnosed with AVM while on the set of ''[[Yogi Bear (film)|Yogi Bear]]'' in New Zealand in 2010; Miller described his experience with the disease on the Pete Holmes podcast You Made It Weird on October 28, 2011, shedding his comedian side for a moment and becoming more philosophical, narrating his behaviors and inability to sleep during that time. He was soon flown back to Los Angeles and successfully underwent surgery that had a mortality rate of ten percent.<ref>{{cite podcast |host=[[Pete Holmes]] |title=''You Made It Weird with Pete Holmes'' |website=You Made It Weird #2: TJ Miller |publisher=Nerdist Industries |date=October 27, 2011 |url=http://www.nerdist.com/2011/10/you-made-it-weird-2-tj-miller/ |time=37:45 |accessdate=December 5, 2012}}</ref> |
|||
== Research directions == |
|||
Despite many years of research, the central question of whether to treat AVMs has not been answered. All treatments, whether involving surgery, radiation, or drugs, have risks and side-effects. Therefore, it might be better in some cases to avoid treatment altogether and simply accept a small risk of coming to harm from the AVM itself. This question is currently being addressed in clinical trials.<ref>[http://www.cliniclog.com/arterio-venous_malformations.php Research trials in arterio-venous malformations; Rustam Al-Shahi Salman]</ref>{{dead link|date=October 2012}} |
|||
<!-- == In other animals == --> |
|||
==See also== |
==See also== |
||
* [[ |
* [[Foix–Alajouanine syndrome]] |
||
* [[Haemangioma]] |
* [[Haemangioma]] |
||
* [[Klippel–Trénaunay syndrome]] |
|||
* [[Klippel-Trenaunay Syndrome]] |
|||
* [[Parkes Weber syndrome]] |
* [[Parkes Weber syndrome]] |
||
==References== |
==References== |
||
{{ |
{{Reflist}} |
||
<!-- == Further reading == --> |
|||
==External links== |
|||
*[http://www.dmoz.org/Health/Conditions_and_Diseases/Neurological_Disorders/Stroke/Support_Groups/Chats_and_Forums/ AVM Support Groups] from the DMOZ Open Directory. |
|||
*[http://avm.ucsf.edu University of California San Francisco AVM research.] |
|||
{{Medical resources |
|||
| DiseasesDB = 15235 |
|||
| ICD11 = {{ICD11|LA90.3}}, {{ICD11|8B22.40}}, {{ICD11|BD52.1}}, {{ICD11|BA82}} |
|||
| ICD10 = {{ICD10|Q27.3}}, {{ICD10|Q28.0}}, {{ICD10|Q28.2}}, {{ICD10|I77.0}}, {{ICD10|I25.4}} |
|||
| ICD9 = {{ICD9|747.6}}, {{ICD9|747.81}} |
|||
| ICDO = |
|||
| OMIM = |
|||
| MedlinePlus = 000779 |
|||
| eMedicineSubj = search |
|||
| eMedicineTopic = Arteriovenous%20Malformation |
|||
| MeshID = D001165 |
|||
}} |
|||
{{Vascular anomalies}} |
|||
{{Congenital vascular defects}} |
{{Congenital vascular defects}} |
||
{{Vascular diseases}} |
{{Vascular diseases}} |
||
{{DEFAULTSORT:Arteriovenous Malformation}} |
{{DEFAULTSORT:Arteriovenous Malformation}} |
||
[[Category:Angiogenesis]] |
|||
[[Category:Congenital vascular defects]] |
[[Category:Congenital vascular defects]] |
||
[[Category:Gross pathology]] |
[[Category:Gross pathology]] |
||
[[Category:RASopathies]] |
[[Category:RASopathies]] |
||
[[Category:Vascular anomalies]] |
|||
Latest revision as of 19:04, 30 October 2024
| Arteriovenous malformation | |
|---|---|
| Other names | AVM |
 | |
| Micrograph of an arteriovenous malformation in the brain. HPS stain. | |
| Specialty | Neurosurgery |
| Diagnostic method | CT, MRI, MRA |
An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system (usually as a cerebral AVM), but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.[1]
Signs and symptoms
[edit]Symptoms of AVMs vary according to their location. Most neurological AVMs produce few to no symptoms. Often the malformation is discovered as part of an autopsy or during treatment of an unrelated disorder (an "incidental finding"); in rare cases, its expansion or a micro-bleed from an AVM in the brain can cause epilepsy, neurological deficit, or pain.[2]
The most general symptoms of a cerebral AVM include headaches and epileptic seizures, with more specific symptoms that normally depend on its location and the individual, including:[1]
- Difficulties with movement coordination, including muscle weakness and even paralysis;
- Vertigo (dizziness);
- Difficulties of speech (dysarthria) and communication, such as aphasia;
- Difficulties with everyday activities, such as apraxia;
- Abnormal sensations (numbness, tingling, or spontaneous pain);
- Memory and thought-related problems, such as confusion, dementia, or hallucinations.
Cerebral AVMs may present themselves in a number of different ways:[citation needed]
- Bleeding (45% of cases)
- "parkinsonism" 4 symptoms in Parkinson's disease.
- Acute onset of severe headache. May be described as the worst headache of the patient's life. Depending on the location of bleeding, may be associated with new fixed neurologic deficit. In unruptured brain AVMs, the risk of spontaneous bleeding may be as low as 1% per year. After a first rupture, the annual bleeding risk may increase to more than 5%.[3]
- Seizure or brain seizure (46%). Depending on the place of the AVM, it can contribute to loss of vision.
- Headache (34%)
- Progressive neurologic deficit (21%)
- May be caused by mass effect or venous dilatations. Presence and nature of the deficit depend on location of lesion and the draining veins.[4]
- Pediatric patients
- Heart failure
- Macrocephaly
- Prominent scalp veins
Pulmonary arteriovenous malformations
[edit]Pulmonary arteriovenous malformations are abnormal communications between the veins and arteries of the pulmonary circulation, leading to a right-to-left blood shunt.[5][6] They have no symptoms in up to 29% of all cases,[7] however they can give rise to serious complications including hemorrhage, and infection.[5] They are most commonly associated with hereditary hemorrhagic telangiectasia.[6]
Genetics
[edit]AVMs are usually congenital and are part of the RASopathy family of developmental syndromes. The understanding of the anomaly's genetic transmission patterns are incomplete, but there are known genetic mutations (for instance in the epithelial line, tumor suppressor PTEN gene) which can lead to an increased occurrence throughout the body.[citation needed]
The anomaly can occur due to autosomal dominant diseases, such as hereditary hemorrhagic telangiectasia.[8]
Pathophysiology
[edit]In the circulatory system, arteries carry blood away from the heart to the lungs and the rest of the body, where the blood normally passes through capillaries—where oxygen is released and waste products like carbon dioxide (CO2) absorbed—before veins return blood to the heart.[9] An AVM interferes with this process by forming a direct connection of the arteries and veins, bypassing the capillary bed.[10] AVMs can cause intense pain and lead to serious medical problems. Although AVMs are often associated with the brain and spinal cord, they can develop in other parts of the body.[10]
As an AVM lacks the dampening effect of capillaries on the blood flow, the AVM can get progressively larger over time as the amount of blood flowing through it increases, forcing the heart to work harder to keep up with the extra blood flow. It also causes the surrounding area to be deprived of the functions of the capillaries. The resulting tangle of blood vessels, often called a nidus (Latin for 'nest'), has no capillaries. It can be extremely fragile and prone to bleeding because of the abnormally direct connections between high-pressure arteries and low-pressure veins.[11] One indicator is a pulsing 'whoosh' sound caused by rapid blood flow through arteries and veins, which has been given the term bruit (French for 'noise'). If the AVM is severe, this may produce an audible symptom which can interfere with hearing and sleep as well as cause psychological distress.[1]
Diagnosis
[edit]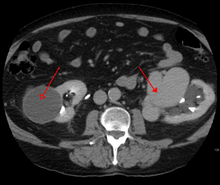

AVMs are diagnosed primarily by the following imaging methods:[12]
- Computed tomography (CT) scan is a noninvasive X-ray to view the anatomical structures within the brain to detect blood in or around the brain. A newer technology called CT angiography involves the injection of contrast into the blood stream to view the arteries of the brain. This type of test provides the best pictures of blood vessels through angiography and soft tissues through CT.
- Magnetic resonance imaging (MRI) scan is a noninvasive test, which uses a magnetic field and radio-frequency waves to give a detailed view of the soft tissues of the brain.
- Magnetic resonance angiography (MRA) – scans created using magnetic resonance imaging to specifically image the blood vessels and structures of the brain. A magnetic resonance angiogram can be an invasive procedure, involving the introduction of contrast dyes (e.g., gadolinium MR contrast agents) into the vasculature (circulatory system) of a patient using a catheter inserted into an artery and passed through the blood vessels to the brain. Once the catheter is in place, the contrast dye is injected into the bloodstream and the MR images are taken. Additionally or alternatively, flow-dependent or other contrast-free magnetic resonance imaging techniques can be used to determine the location and other properties of the vasculature.
AVMs can occur in various parts of the body:
- brain (cerebral AV malformation)
- spleen[13]
- lung[14][15]
- kidney[16]
- spinal cord[17]
- liver[18]
- intercostal space[19]
- iris[20]
- spermatic cord[21]
- extremities – arm, shoulder, etc.
AVMs may occur in isolation or as a part of another disease (for example, Sturge-Weber syndrome or hereditary hemorrhagic telangiectasia).[22]
AVMs have been shown to be associated with aortic stenosis.[23]
Bleeding from an AVM can be relatively mild or devastating. It can cause severe and less often fatal strokes.[1]
Treatment
[edit]Treatment for AVMs in the brain can be symptomatic, and patients should be followed by a neurologist for any seizures, headaches, or focal neurologic deficits. AVM-specific treatment may also involve endovascular embolization, neurosurgery or radiosurgery.[1] Embolization, that is, cutting off the blood supply to the AVM with coils, particles, acrylates, or polymers introduced by a radiographically guided catheter, may be used in addition to neurosurgery or radiosurgery, but is rarely successful in isolation except in smaller AVMs.[24] A gamma knife may also be used.[25]
If a cerebral AVM is detected before a stroke occurs, usually the arteries feeding blood into the nidus can be closed off to avert the danger.[26] Interventional therapy may be relatively risky in the short term.[27]
Treatment of lung AVMs is typically performed with endovascular embolization alone, which is considered the standard of care.[15]
Epidemiology
[edit]The estimated detection rate of AVM in the US general population is 1.4/100,000 per year.[28] This is approximately one-fifth to one-seventh the incidence of intracranial aneurysms. An estimated 300,000 Americans have AVMs, of whom 12% (approximately 36,000) will exhibit symptoms of greatly varying severity.[1]
History
[edit]Hubert von Luschka (1820–1875) and Rudolf Virchow (1821–1902) first described arteriovenous malformations in the mid-1800s. Herbert Olivecrona (1891–1980) performed the first surgical excision of an intracranial AVM in 1932.
Society and culture
[edit]Notable cases
[edit]- Actor Ricardo Montalbán was born with spinal AVM.[29] During the filming of the 1951 film Across the Wide Missouri, Montalbán was thrown from his horse, knocked unconscious, and trampled by another horse which aggravated his AVM and resulted in a painful back injury that never healed. The pain increased as he aged, and in 1993, Montalbán underwent 9+1⁄2 hours of spinal surgery which left him paralyzed below the waist and using a wheelchair.[30]
- Composer and lyricist William Finn was diagnosed with AVM and underwent gamma knife surgery in September 1992, soon after he won the 1992 Tony Award for best musical, awarded to "Falsettos".[31] Finn wrote the 1998 Off-Broadway musical A New Brain about the experience.
- Phoenix Suns point guard AJ Price nearly died from AVM in 2004 while a student at the University of Connecticut.
- On December 13, 2006, Senator Tim Johnson of South Dakota was diagnosed with AVM and treated at George Washington University Hospital.[32]
- Actor/comedian T. J. Miller was diagnosed with AVM in 2010; Miller had a seizure and was unable to sleep for a period. He successfully underwent surgery that had a mortality rate of 10%.[33]
- On August 3, 2011, Mike Patterson of the Philadelphia Eagles collapsed on the field and had a seizure during a practice, leading to him being diagnosed with AVM.[34]
- Former Florida Gators and Oakland Raiders linebacker Neiron Ball was diagnosed with AVM in 2011 while playing for Florida, but recovered and was cleared to play. On September 16, 2018, Ball was placed in a medically induced coma due to complications of the disease, which lasted until his death on September 10, 2019.[35]
- Indonesian actress Egidia Savitri died from complications of AVM on November 29, 2013.[36]
- Jazz guitarist Pat Martino experienced an AVM and subsequently developed amnesia and manic depression. He eventually re-learned to play the guitar by listening to his own recordings from before the aneurysm.[37]
- YouTube vlogger Nikki Lilly (Nikki Christou), winner of the 2016 season of Junior Bake Off was born with AVM, which has resulted in some facial disfigurement.[38]
- Country music singer Drake White was diagnosed with AVM in January 2019, and is undergoing treatment.
Cultural depictions
[edit]- In the HBO series Six Feet Under (2001), main character Nate Fisher discovers he has an AVM after being in a car accident and getting a precautionary cat scan at the hospital during Season 1. His AVM becomes a key focus during Season 2 and again in Season 5.
- In season 1 episode 9 of House (2004), titled "DNR", a jazz musician has an AVM and is misdiagnosed with ALS. Two season three episodes also involve AVM - "Top Secret" (episode 16), in which a veteran who believes himself to be suffering from Gulf War syndrome is found to have spinal and pulmonary AVM from hereditary hemorrhagic telangiectasia; and "Resignation" (episode 22), where the patient developed AVM in her intestines after drinking pipe cleaner fluid in a suicide attempt.
- In the 2005 Lifetime film Dawn Anna, the titular character learns she has AVM, and undergoes a serious operation and subsequent rehabilitation, which she recovers from.
See also
[edit]References
[edit]- ^ a b c d e f Arteriovenous Malformation Information Page at NINDS
- ^ "Arteriovenous Malformations". Johns Hopkins Medicine. Retrieved October 26, 2022.
- ^ Stapf, C.; Mast, H.; Sciacca, R. R.; Choi, J. H.; Khaw, A. V.; Connolly, E. S.; Pile-Spellman, J.; Mohr, J. P. (2006). "Predictors of hemorrhage in patients with untreated brain arteriovenous malformation". Neurology. 66 (9): 1350–5. doi:10.1212/01.wnl.0000210524.68507.87. PMID 16682666. S2CID 22004276.
- ^ Choi, J.H.; Mast, H.; Hartmann, A.; Marshall, R.S.; Pile-Spellman, J.; Mohr, J.P.; Stapf, C. (2009). "Clinical and morphological determinants of focal neurological deficits in patients with unruptured brain arteriovenous malformation". Journal of the Neurological Sciences. 287 (1–2): 126–30. doi:10.1016/j.jns.2009.08.011. PMC 2783734. PMID 19729171.
- ^ a b Reichert, M; Kerber, S; Alkoudmani, I; Bodner, J (April 2016). "Management of a solitary pulmonary arteriovenous malformation by video-assisted thoracoscopic surgery and anatomic lingula resection: video and review". Surgical Endoscopy. 30 (4): 1667–9. doi:10.1007/s00464-015-4337-0. PMID 26156615. S2CID 22394114.
- ^ a b Tellapuri, S; Park, HS; Kalva, SP (August 2019). "Pulmonary arteriovenous malformations". The International Journal of Cardiovascular Imaging. 35 (8): 1421–1428. doi:10.1007/s10554-018-1479-x. PMID 30386957. S2CID 53144651.
- ^ Goodenberger DM (2008). "Chapter 84 Pulmonary arteriovenous malformations". Fishman's Pulmonary Diseases and Disorders (4th ed.). McGraw-Hill. p. 1470. ISBN 978-0-07-145739-2.
- ^ "Hereditary hemorrhagic telangiectasia: MedlinePlus Genetics". medlineplus.gov. Retrieved July 23, 2022.
- ^ "Circulatory System: Anatomy and Function". Cleveland Clinic. September 21, 2021. Retrieved March 8, 2023.
- ^ a b Schimmel, Katharina; Ali, Md Khadem; Tan, Serena Y.; Teng, Joyce; Do, Huy M.; Steinberg, Gary K.; Stevenson, David A.; Spiekerkoetter, Edda (August 21, 2021). "Arteriovenous Malformations—Current Understanding of the Pathogenesis with Implications for Treatment". International Journal of Molecular Sciences. 22 (16): 9037. doi:10.3390/ijms22169037. ISSN 1422-0067. PMC 8396465. PMID 34445743.
- ^ Mouchtouris, Nikolaos; Jabbour, Pascal M.; Starke, Robert M.; Hasan, David M.; Zanaty, Mario; Theofanis, Thana; Ding, Dale; Tjoumakaris, Stavropoula I.; Dumont, Aaron S.; Ghobrial, George M.; Kung, David (February 2015). "Biology of cerebral arteriovenous malformations with a focus on inflammation". Journal of Cerebral Blood Flow and Metabolism. 35 (2): 167–175. doi:10.1038/jcbfm.2014.179. PMC 4426734. PMID 25407267.
- ^ Mokin, Maxim (February 2014). "Novel Multimodality Imaging Techniques for Diagnosis and Evaluation of Arteriovenous Malformations". Neurologic Clinics. 32 (1): 225–236. doi:10.1016/j.ncl.2013.07.006. PMID 24287392. Retrieved February 11, 2023.
- ^ Agrawal, Aditya; Whitehouse, Richard; Johnson, Robert W.; Augustine, Titus (2006). "Giant splenic artery aneurysm associated with arteriovenous malformation". Journal of Vascular Surgery. 44 (6): 1345–9. doi:10.1016/j.jvs.2006.06.049. PMID 17145440.
- ^ Chowdhury, Ujjwal K.; Kothari, Shyam S.; Bishnoi, Arvind K.; Gupta, Ruchika; Mittal, Chander M.; Reddy, Srikrishna (2009). "Successful Lobectomy for Pulmonary Arteriovenous Malformation Causing Recurrent Massive Haemoptysis". Heart, Lung and Circulation. 18 (2): 135–9. doi:10.1016/j.hlc.2007.11.142. PMID 18294908.
- ^ a b Cusumano, Lucas R.; Duckwiler, Gary R.; Roberts, Dustin G.; McWilliams, Justin P. (August 30, 2019). "Treatment of Recurrent Pulmonary Arteriovenous Malformations: Comparison of Proximal Versus Distal Embolization Technique". CardioVascular and Interventional Radiology. 43 (1): 29–36. doi:10.1007/s00270-019-02328-0. ISSN 1432-086X. PMID 31471718. S2CID 201675132.
- ^ Barley, Fay L.; Kessel, David; Nicholson, Tony; Robertson, Iain (2006). "Selective Embolization of Large Symptomatic Iatrogenic Renal Transplant Arteriovenous Fistula". CardioVascular and Interventional Radiology. 29 (6): 1084–7. doi:10.1007/s00270-005-0265-z. PMID 16794894. S2CID 9335750.
- ^ Kishi, K; Shirai, S; Sonomura, T; Sato, M (2005). "Selective conformal radiotherapy for arteriovenous malformation involving the spinal cord". The British Journal of Radiology. 78 (927): 252–4. doi:10.1259/bjr/50653404. PMID 15730991.
- ^ Bauer, Tilman; Britton, Peter; Lomas, David; Wight, Derek G.D.; Friend, Peter J.; Alexander, Graeme J.M. (1995). "Liver transplantation for hepatic arteriovenous malformation in hereditary haemorrhagic telangiectasia". Journal of Hepatology. 22 (5): 586–90. doi:10.1016/0168-8278(95)80455-2. PMID 7650340.
- ^ Rivera, Peter P.; Kole, Max K.; Pelz, David M.; Gulka, Irene B.; McKenzie, F. Neil; Lownie, Stephen P. (2006). "Congenital Intercostal Arteriovenous Malformation". American Journal of Roentgenology. 187 (5): W503–6. doi:10.2214/AJR.05.0367. PMID 17056881.
- ^ Shields, Jerry A.; Streicher, Theodor F. E.; Spirkova, Jane H. J.; Stubna, Michal; Shields, Carol L. (2006). "Arteriovenous Malformation of the Iris in 14 Cases". Archives of Ophthalmology. 124 (3): 370–5. doi:10.1001/archopht.124.3.370. PMID 16534057.
- ^ Sountoulides, Petros; Bantis, Athanasios; Asouhidou, Irene; Aggelonidou, Hellen (2007). "Arteriovenous malformation of the spermatic cord as the cause of acute scrotal pain: a case report". Journal of Medical Case Reports. 1: 110. doi:10.1186/1752-1947-1-110. PMC 2194703. PMID 17939869.
- ^ "Arteriovenous Malformations (AVMs)". National Institute of Neurological Disorders and Stroke, NIH. February 22, 2024. Retrieved March 30, 2024.
- ^ Batur, Pelin; Stewart, William J.; Isaacson, J. Harry (2003). "Increased Prevalence of Aortic Stenosis in Patients With Arteriovenous Malformations of the Gastrointestinal Tract in Heyde Syndrome". Archives of Internal Medicine. 163 (15): 1821–4. doi:10.1001/archinte.163.15.1821. PMID 12912718.
- ^ Jafar, Jafar J.; Davis, Adam J.; Berenstein, Alejandro; Choi, In Sup; Kupersmith, Mark J. (January 1, 1993). "The effect of embolization with N-butyl cyanoacrylate prior to surgical resection of cerebral arteriovenous malformations". Journal of Neurosurgery. 78 (1): 60–69. doi:10.3171/jns.1993.78.1.0060. ISSN 0022-3085. PMID 8416244.
- ^ "Conditions We Treat". Macquarie University Hospital. Archived from the original on June 13, 2013.
- ^ "Arteriovenous Malformations". Neurosurgery. Retrieved June 26, 2023.
- ^ "A Randomized Trial of Unruptured Brain Arteriovenous Malformations (ARUBA)". National Institute of Neurological Disorders and Stroke. January 29, 2014. Archived from the original on July 4, 2016. Retrieved March 6, 2023.
- ^ Stapf, C.; Mast, H.; Sciacca, R.R.; Berenstein, A.; Nelson, P.K.; Gobin, Y.P.; Pile-Spellman, J.; Mohr, J.P. (2003). "The New York Islands AVM Study: Design, Study Progress, and Initial Results". Stroke. 34 (5): e29–33. doi:10.1161/01.STR.0000068784.36838.19. PMID 12690217.
- ^ "Ricardo Montalban tribute" YouTube, acceptance speech video of Easter Seals Lifetime Achievement Award
- ^ "Inside". mahalo.com. Retrieved March 17, 2018.
- ^ Pall, Ellen (June 14, 1998). "The Long-Running Musical of William Finn's Life". The New York Times. Retrieved March 17, 2018.
- ^ "Sen. Johnson recovering after brain surgery". AP. December 14, 2006.
- ^ Holmes, Pete (October 27, 2011). "You Made It Weird with Pete Holmes". You Made It Weird #2: TJ Miller (Podcast). Nerdist Industries. Event occurs at 37:45. Archived from the original on February 12, 2013. Retrieved December 5, 2012.
- ^ "Mike Patterson's Collapse Reportedly Related To Brain AVM". sbnation.com. August 4, 2011. Retrieved March 17, 2018.
- ^ "Neiron Ball, former Raiders LB, in medically induced coma after aneurysm". ESPN. September 26, 2018.
- ^ Suhendra, Ichsan. "Pesinetron Egidia Savitri Telah Pergi". KOMPAS.com (in Indonesian). Kompas Cyber Media. Retrieved May 15, 2019.
- ^ Vida, Vendela. Confidence, or the Appearance of Confidence: The Best of the Believer Music Interviews. No ed. San Francisco, CA: Believer, a Tiny Division of McSweeney's Which Is Also Tiny, 2014. Print.
- ^ "Junior Bake Off 2016 Winner announced". BBC Media Centre. BBC Online. November 25, 2016. Retrieved April 9, 2017.
