Ebola: Difference between revisions
m Moving Category:Biological weapons to Category:Biological agents per Wikipedia:Categories for discussion/Speedy |
|||
| Line 1: | Line 1: | ||
{{Short description|Viral hemorrhagic fever of humans and other primates caused by ebolaviruses}} |
|||
{{pp-vandalism|expiry=19 August 2014|small=yes}} |
|||
{{ |
{{about|the disease}} |
||
{{pp-vandalism|small=yes}} |
|||
{{infobox disease |
|||
{{Use British English|date=February 2020}} |
|||
| Name = Ebola virus disease |
|||
{{Use dmy dates|date=July 2023}} |
|||
| Image = 7042 lores-Ebola-Zaire-CDC Photo.jpg |
|||
{{Infobox medical condition |
|||
| Caption = 1976 photograph of two nurses standing in front of [[Mayinga N'Seka|Mayinga N.]], a person with Ebola virus disease; she died only a few days later due to severe internal hemorrhaging. |
|||
| |
| name = Ebola |
||
| synonyms = Ebola haemorrhagic fever (EHF), Ebola virus disease |
|||
| ICD10 = {{ICD10|A|98|4|a|90}} |
|||
| |
| image = 7042 lores-Ebola-Zaire-CDC Photo.jpg |
||
| caption = Two nurses standing near [[Mayinga N'Seka]], a nurse with Ebola virus disease in the [[1976 Zaire Ebola virus outbreak|1976 outbreak in Zaire]]. N'Seka died a few days later. The nurses are not wearing proper protective equipment. |
|||
| MedlinePlus = 001339 |
|||
| field = [[Infectious disease (medical specialty)|Infectious disease]] |
|||
| eMedicineSubj = med |
|||
| symptoms = [[Fever]], [[sore throat]], [[Myalgia|muscular pain]], [[headaches]], [[diarrhoea]], bleeding<ref name=WHO2014/> |
|||
| eMedicineTopic = 626 |
|||
| complications = [[hypovolemic shock|shock from fluid loss]]<ref name=Ruz2014/> |
|||
| MeshID = D019142 |
|||
| onset = Two days to three weeks post exposure<ref name=WHO2014/> |
|||
| duration = |
|||
| causes = [[Ebolavirus]]es spread by direct contact<ref name=WHO2014/> |
|||
| risks = |
|||
| diagnosis = Finding the virus, viral [[RNA]], or [[antibodies]] in blood<ref name=WHO2014/> |
|||
| differential = [[Malaria]], [[cholera]], [[typhoid fever]], [[meningitis]], other [[viral haemorrhagic fevers]]<ref name=WHO2014/> |
|||
| prevention = Coordinated medical services, careful handling of [[bushmeat]]<ref name=WHO2014/> |
|||
| treatment = [[Supportive care]]<ref name=WHO2014/> |
|||
| medication = [[Atoltivimab/maftivimab/odesivimab]] (Inmazeb) |
|||
| prognosis = 25–90% mortality<ref name=WHO2014/> |
|||
| frequency = |
|||
| deaths = |
|||
| alt = |
|||
| image_size = 200 |
|||
}} |
}} |
||
'''Ebola virus disease''' ('''EVD''') or '''Ebola hemorrhagic fever''' ('''EHF''') is the human disease caused by the [[Ebola virus]].<!-- <ref name=WHO2014/> --> Symptoms typically start two days to three weeks after contracting the virus, with a [[fever]], sore throat, [[Myalgia|muscle pains]], and [[headaches]].<!-- <ref name=WHO2014/> --> Typically [[nausea]], vomiting, and [[diarrhea]] follow, along with decreased functioning of the [[liver]] and [[kidney]]s.<!-- <ref name=WHO2014/> --> At this point, some people begin to have [[bleeding]] problems.<ref name=WHO2014>{{cite web|title=Ebola virus disease Fact sheet N°103|url=http://www.who.int/mediacentre/factsheets/fs103/en/|work=World Health Organization|accessdate=12 April 2014|date=March 2014}}</ref> |
|||
'''Ebola''', also known as '''Ebola virus disease''' ('''EVD''') and '''Ebola hemorrhagic fever''' ('''EHF'''), is a [[viral hemorrhagic fever]] in humans and other [[primate]]s, caused by [[ebolavirus]]es.<ref name=WHO2014/> Symptoms typically start anywhere between two days and three weeks after infection.<ref>{{Cite book | vauthors = Modrow S, Falke D, Truyen U, Schätzl H |title=Molecular Virology |chapter=Viruses: Definition, Structure, Classification |date=2013 |pages=17–30 | veditors = Modrow S, Falke D, Truyen U, Schätzl H |place=Berlin, Heidelberg |publisher=Springer |language=en |doi=10.1007/978-3-642-20718-1_2 |isbn=978-3-642-20718-1 |s2cid=83235976|doi-access=free }}</ref> The first symptoms are usually [[fever]], [[sore throat]], [[Myalgia|muscle pain]], and [[headache]]s.<ref name=WHO2014/> These are usually followed by [[vomiting]], [[diarrhoea]], [[rash]] and decreased [[liver]] and [[kidney]] function,<ref name=WHO2014/> at which point some people begin to [[bleeding|bleed]] both [[internal bleeding|internally]] and externally.<ref name="WHO2014">{{Cite web |date=September 2014 |title=Ebola virus disease, Fact sheet N°103, Updated September 2014 |url=https://www.who.int/mediacentre/factsheets/fs103/en/ |url-status=deviated |archive-url=https://web.archive.org/web/20141214011751/https://www.who.int/mediacentre/factsheets/fs103/en/ |archive-date=14 December 2014 |access-date=15 December 2014 |publisher=[[World Health Organization]] (WHO)}}</ref> It kills between 25% and 90% of those infected – about 50% on average.<ref name=WHO2014/> Death is often due to [[hypovolemic shock|shock from fluid loss]], and typically occurs between six and 16 days after the first symptoms appear.<ref name="Ruz2014">{{Cite book |url=https://books.google.com/books?id=l5MtJdDhie0C&pg=PA444 |title=Viral hemorrhagic fevers |date=2014 |publisher=CRC Press, Taylor & Francis Group |isbn=978-1439884294 | veditors = Singh SK, Ruzek D |location=Boca Raton |page=444 |archive-url=https://web.archive.org/web/20160429192429/https://books.google.com/books?id=l5MtJdDhie0C&pg=PA444 |archive-date=29 April 2016 }}</ref> Early treatment of symptoms increases the survival rate considerably compared to late start.<ref name="Guiliani 2022">Ebola in Uganda: {{Cite web | vauthors = Guiliani R |title=Our game-changing treatment centres will save more lives |url=https://msf.org.uk/article/ebola-uganda-our-game-changing-treatment-centres-will-save-more-lives |archive-url=https://web.archive.org/web/20221115224626/https://msf.org.uk/article/ebola-uganda-our-game-changing-treatment-centres-will-save-more-lives |archive-date=15 November 2022 |access-date=15 November 2022 |publisher=msf.org.urk}}</ref> An [[Ebola vaccine]] was approved by the US FDA in December 2019. |
|||
<!-- Cause and Diagnosis--> |
|||
The virus may be acquired upon contact with [[blood]] or [[bodily fluid]]s of an infected animal (commonly monkeys or [[fruit bat]]s).<ref name=WHO2014/> It is not naturally transmitted through the air.<ref name=WHOAir2014>{{cite web|title=2014 Ebola Virus Disease (EVD) outbreak in West Africa|url=http://www.who.int/ith/updates/20140421/en/|website=WHO|accessdate=3 August 2014|date=Apr 21 2014}}</ref> Fruit bats are believed to carry and spread the virus without being affected.<!-- <ref name=WHO2014/> --> Once human infection occurs, the disease may spread between people as well.<!-- <ref name=WHO2014/> --> Male survivors may be able to transmit the disease via [[semen]] for nearly two months.<!-- <ref name=WHO2014/> --> In order to make the diagnosis, typically other diseases with similar symptoms such as [[malaria]], [[cholera]] and other [[viral hemorrhagic fever]]s are first excluded.<!-- <ref name=WHO2014/> --> Blood samples may then be tested for viral [[antibodies]], viral [[RNA]], or the virus itself to confirm the diagnosis.<ref name=WHO2014/> |
|||
The virus spreads through direct contact with [[body fluid]]s, such as [[blood]] from infected humans or other animals,<ref name=WHO2014/> or from contact with items that have recently been contaminated with infected body fluids.<ref name=WHO2014/> There have been no documented cases, either in nature or under laboratory conditions, of spread through the air between humans or other [[primate]]s.<ref name="WHOAir2014">{{Cite web |date=21 April 2014 |title=2014 Ebola Virus Disease (EVD) outbreak in West Africa |url=https://www.who.int/ith/updates/20140421/en/ |url-status=dead |archive-url=https://web.archive.org/web/20140729034008/https://www.who.int/ith/updates/20140421/en/ |archive-date=29 July 2014 |access-date=3 August 2014 |publisher=World Health Organization (WHO) }}</ref> After recovering from Ebola, [[semen]] or [[breast milk]] may continue to carry the virus for anywhere between several weeks to several months.<ref name=WHO2014/><ref name="cdc9months">{{Cite web |date=14 October 2015 |title=Preliminary study finds that Ebola virus fragments can persist in the semen of some survivors for at least nine months |url=https://www.cdc.gov/media/releases/2015/p1014-ebola-virus.html |url-status=live |archive-url=https://web.archive.org/web/20170824104650/https://www.cdc.gov/media/releases/2015/p1014-ebola-virus.html |archive-date=24 August 2017 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref><ref name="CDCBreast2014">{{Cite web |date=19 September 2014 |title=Recommendations for Breastfeeding/Infant Feeding in the Context of Ebola |url=https://www.cdc.gov/vhf/ebola/hcp/recommendations-breastfeeding-infant-feeding-ebola.html |url-status=live |archive-url=https://web.archive.org/web/20141024235607/https://www.cdc.gov/vhf/ebola/hcp/recommendations-breastfeeding-infant-feeding-ebola.html |archive-date=24 October 2014 |access-date=26 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> [[Megabat|Fruit bat]]s are believed to be the normal [[natural host|carrier in nature]]; they are able to spread the virus without being affected by it.<ref name=WHO2014/> The symptoms of Ebola may resemble those of several other diseases, including [[malaria]], [[cholera]], [[typhoid fever]], [[meningitis]] and other viral hemorrhagic fevers.<ref name=WHO2014/> Diagnosis is confirmed by testing blood samples for the presence of viral [[RNA]], viral [[antibodies]] or the virus itself.<ref name=WHO2014/><ref name="Bro2016">{{Cite journal |vauthors=Broadhurst MJ, Brooks TJ, Pollock NR |date=13 July 2016 |title=Diagnosis of Ebola Virus Disease: Past, Present, and Future |journal=Clinical Microbiology Reviews |publisher=American Society for Microbiology |volume=29 |issue=4 |pages=773–793 |doi=10.1128/cmr.00003-16 |issn=0893-8512 |lccn=88647279 |oclc=38839512 |pmc=5010747 |pmid=27413095}}</ref> |
|||
<!-- Prevention --> |
|||
Prevention includes decreasing the spread of disease from infected monkeys and pigs to humans.<!-- <ref name=WHO2014/> --> This may be done by checking such animals for infection and killing and properly disposing of the bodies if the disease is discovered.<!-- <ref name=WHO2014/> --> Properly cooking meat and wearing protective clothing when handling meat may also be helpful,<!-- <ref name=WHO2014/> --> as are wearing protective clothing and [[washing hands]] when around a person with the disease.<!-- <ref name=WHO2014/> --> Samples of bodily fluids and tissues from people with the disease should be handled with special caution.<ref name=WHO2014/> |
|||
Control of outbreaks requires coordinated medical services and community engagement,<ref name=WHO2014/> including rapid detection, [[contact tracing]] of those exposed, quick access to laboratory services, care for those infected, and proper disposal of the dead through [[cremation]] or burial.<ref name=WHO2014/><ref>{{Cite web |title=Guidance for Safe Handling of Human Remains of Ebola Patients in U.S. Hospitals and Mortuaries |url=https://www.cdc.gov/vhf/ebola/hcp/guidance-safe-handling-human-remains-ebola-patients-us-hospitals-mortuaries.html |url-status=live |archive-url=https://web.archive.org/web/20141009172209/https://www.cdc.gov/vhf/ebola/hcp/guidance-safe-handling-human-remains-ebola-patients-us-hospitals-mortuaries.html |archive-date=9 October 2014 |access-date=10 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> Prevention measures involve wearing proper protective clothing and [[washing hands]] when in close proximity to patients and while handling potentially infected [[bushmeat]], as well as thoroughly cooking bushmeat.<ref name=WHO2014/> An [[Ebola vaccine]] was approved by the US FDA in December 2019.<ref name="FDA2019Vac">{{Cite press release |title=First FDA-approved vaccine for the prevention of Ebola virus disease, marking a critical milestone in public health preparedness and response |date=20 December 2019 |url=https://www.fda.gov/news-events/press-announcements/first-fda-approved-vaccine-prevention-ebola-virus-disease-marking-critical-milestone-public-health |access-date=22 December 2019 |publisher=U.S. [[Food and Drug Administration]] (FDA) |archive-date=20 December 2019 |archive-url=https://web.archive.org/web/20191220052152/https://www.fda.gov/news-events/press-announcements/first-fda-approved-vaccine-prevention-ebola-virus-disease-marking-critical-milestone-public-health |url-status=live }}</ref> While there is no approved treatment for Ebola {{as of |2019|lc=yes}},<ref name="NIH2019">{{Cite web |title=Ebola Treatment Research |url=https://www.niaid.nih.gov/diseases-conditions/ebola-treatment |access-date=20 August 2019 |publisher=NIH: National Institute of Allergy and Infectious Diseases |archive-date=20 August 2019 |archive-url=https://web.archive.org/web/20190820100501/https://www.niaid.nih.gov/diseases-conditions/ebola-treatment |url-status=live }}</ref> two treatments ([[atoltivimab/maftivimab/odesivimab]] and [[ansuvimab]]) are associated with improved outcomes.<ref name="NIH2019Tx">{{Cite web |title=Independent Monitoring Board Recommends Early Termination of Ebola Therapeutics Trial in DRC Because of Favorable Results with Two of Four Candidates |date=12 August 2019 |url=https://www.niaid.nih.gov/news-events/independent-monitoring-board-recommends-early-termination-ebola-therapeutics-trial-drc |access-date=20 August 2019 |publisher=NIH: National Institute of Allergy and Infectious Diseases |archive-date=19 August 2019 |archive-url=https://web.archive.org/web/20190819184035/https://www.niaid.nih.gov/news-events/independent-monitoring-board-recommends-early-termination-ebola-therapeutics-trial-drc |url-status=live }}</ref> Supportive efforts also improve outcomes.<ref name=WHO2014/> These include [[oral rehydration therapy]] (drinking slightly sweetened and salty water) or giving [[intravenous fluids]], and treating symptoms.<ref name=WHO2014/> In October 2020, atoltivimab/maftivimab/odesivimab (Inmazeb) was approved for medical use in the United States to treat the disease caused by ''Zaire ebolavirus''.<ref name="FDA PR" /> |
|||
<!-- Treatment, Prognosis and Epidemiology--> |
|||
{{TOC limit}} |
|||
There is no specific treatment for the disease; efforts to help persons who are infected include giving either [[oral rehydration therapy]] (slightly sweet and salty water to drink) or [[intravenous fluids]].<ref name=WHO2014/> The disease has high [[mortality rate]]: often killing between 50% and 90% of those infected with the virus.<ref name=WHO2014/><ref name="Elsevier/Academic Press">{{cite book|author1=C.M. Fauquet|title=Virus taxonomy classification and nomenclature of viruses; 8th report of the International Committee on Taxonomy of Viruses|date=2005|publisher=Elsevier/Academic Press|location=Oxford|isbn=9780080575483|page=648|url=http://books.google.ca/books?id=9Wy7Jgy5RWYC&pg=PA648}}</ref> EVD was first identified in [[Sudan]] and the [[Democratic Republic of the Congo]].<!-- <ref name=WHO2014/> --> The disease typically occurs in outbreaks in tropical regions of [[Sub-Saharan Africa]].<ref name=WHO2014/> Between 1976, when it was first identified, through 2013, fewer than 1,000 people per year have been infected.<ref name=WHO2014/><ref name=MMWRJune2014>{{cite web|title=Ebola Viral Disease Outbreak — West Africa, 2014|url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6325a4.htm?s_cid=mm6325a4_w|website=CDC|accessdate=26 June 2014|date=June 27, 2014}}</ref> The largest outbreak to date is the ongoing [[2014 West Africa Ebola outbreak]], which is affecting [[Guinea]], [[Sierra Leone]], [[Liberia]] and likely [[Nigeria]].<ref name=CDC2014/><ref name=CDCAug2014N>{{cite web|title=Outbreak of Ebola in Guinea, Liberia, and Sierra Leone|url=http://www.cdc.gov/vhf/ebola/outbreaks/guinea/index.html|website=CDC|accessdate=5 August 2014|date=August 4, 2014}}</ref> As of July 2014 more than 1320 cases have been identified.<ref name=CDC2014>{{cite web|title=CDC urges all US residents to avoid nonessential travel to Liberia, Guinea, and Sierra Leone because of an unprecedented outbreak of Ebola.|url=http://wwwnc.cdc.gov/travel/notices/warning/ebola-liberia|website=CDC|accessdate=2 August 2014|date=July 31, 2014}}</ref> Efforts are ongoing to develop a [[vaccine]]; however, none yet exists.<ref name=WHO2014/> |
|||
{{TOC limit|3}} |
|||
==History and name== |
|||
Ebola was first identified in 1976, in two simultaneous outbreaks, one in [[Nzara]] (a town in [[South Sudan]]) and the other in [[Yambuku]] ([[the Democratic Republic of the Congo]]), a village near the [[Ebola River]], for which the disease was named.<ref name="WHO2014" /> [[List of Ebola outbreaks|Ebola outbreaks]] occur intermittently in tropical regions of [[sub-Saharan Africa]].<ref name=WHO2014/> Between 1976 and 2012, according to the [[World Health Organization]], there were 24 outbreaks of Ebola resulting in a total of [[List of Ebola outbreaks|2,387 cases, and 1,590 deaths]].<ref name=WHO2014/><ref name="MMWRJune2014">{{Cite journal |vauthors=Dixon MG, Schafer IJ |date=June 2014 |title=Ebola viral disease outbreak – West Africa, 2014 |url=https://www.cdc.gov/mmwr/pdf/wk/mm6325.pdf |journal=MMWR Morb. Mortal. Wkly. Rep. |volume=63 |issue=25 |pages=548–551 |pmc=5779383 |pmid=24964881 |access-date=7 April 2020 |archive-date=23 October 2020 |archive-url=https://web.archive.org/web/20201023224947/https://www.cdc.gov/mmwr/pdf/wk/mm6325.pdf |url-status=live }}</ref> The largest Ebola outbreak to date was an [[Ebola virus epidemic in West Africa|epidemic in West Africa]] from December 2013 to January 2016, with {{#section:Ebola virus epidemic in West Africa|cases}} cases and {{#section:Ebola virus epidemic in West Africa|deaths}} deaths.{{#section:Ebola virus epidemic in West Africa|caserefs}}<ref name="CDC2014">{{Cite web |date=31 July 2014 |title=CDC urges all US residents to avoid nonessential travel to Liberia, Guinea and Sierra Leone because of an unprecedented outbreak of Ebola |url=https://wwwnc.cdc.gov/travel/notices/warning/ebola-liberia |archive-url=https://web.archive.org/web/20140809181737/https://wwwnc.cdc.gov/travel/notices/warning/ebola-liberia |archive-date=9 August 2014 |access-date=2 August 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC) }}</ref><ref name="CDCAug2014N">{{Cite web |date=4 August 2014 |title=2014 Ebola Outbreak in West Africa |url=https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/ |url-status=live |archive-url=https://web.archive.org/web/20141002134254/https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/ |archive-date=2 October 2014 |access-date=5 August 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> On 29 March 2016, it was declared to no longer be an emergency.<ref name="who.int">{{Cite web |date=29 March 2016 |title=Statement on the 9th meeting of the IHR Emergency Committee regarding the Ebola outbreak in West Africa |url=https://www.who.int/mediacentre/news/statements/2016/end-of-ebola-pheic/en/ |url-status=live |archive-url=https://web.archive.org/web/20160331231040/https://www.who.int/mediacentre/news/statements/2016/end-of-ebola-pheic/en/ |archive-date=31 March 2016 |access-date=30 March 2016 |publisher=[[World Health Organization]] (WHO)}}</ref> Other outbreaks in Africa began in the Democratic Republic of the Congo in May 2017,<ref>{{Cite web |title=Statement on Ebola in the Democratic Republic of the Congo |url=https://www.who.int/mediacentre/news/statements/2017/ebola-drc/en/ |url-status=live |archive-url=https://web.archive.org/web/20170512203522/https://www.who.int/mediacentre/news/statements/2017/ebola-drc/en/ |archive-date=12 May 2017 |access-date=12 May 2017 |publisher=[[World Health Organization]] (WHO)}}</ref><ref>{{Cite news | vauthors = Hodal K |date=12 May 2017 |title=Ebola outbreak declared in Democratic Republic of the Congo after three die |work=[[The Guardian]] |location=United Kingdom |url=https://www.theguardian.com/world/2017/may/12/ebola-outbreak-declared-democratic-republic-of-congo-after-three-die |url-status=live |access-date=12 May 2017 |archive-url=https://web.archive.org/web/20170512161809/https://www.theguardian.com/world/2017/may/12/ebola-outbreak-declared-democratic-republic-of-congo-after-three-die |archive-date=12 May 2017 |issn=1756-3224 |oclc=60623878}}</ref> and 2018.<ref>{{Cite news |vauthors=Scutti S, Goldschmidt D |title=Ebola outbreak declared in Democratic Republic of Congo |publisher=CNN |url=https://www.cnn.com/2018/05/08/health/ebola-outbreak-who-bn/index.html |access-date=9 May 2018 |archive-date=8 May 2018 |archive-url=https://web.archive.org/web/20180508212134/https://www.cnn.com/2018/05/08/health/ebola-outbreak-who-bn/index.html |url-status=live }}</ref><ref name="WHO2018DRCOver">{{Cite web |title=Ebola outbreak in DRC ends: WHO calls for international efforts to stop other deadly outbreaks in the country |url=https://www.who.int/news-room/detail/24-07-2018-ebola-outbreak-in-drc-ends-who-calls-for-international-efforts-to-stop-other-deadly-outbreaks-in-the-country |access-date=26 July 2018 |publisher=[[World Health Organization]] (WHO) |archive-date=25 July 2018 |archive-url=https://web.archive.org/web/20180725190657/http://www.who.int/news-room/detail/24-07-2018-ebola-outbreak-in-drc-ends-who-calls-for-international-efforts-to-stop-other-deadly-outbreaks-in-the-country |url-status=live }}</ref> In July 2019, the World Health Organization declared the Congo Ebola outbreak a [[Public health emergency of international concern|world health emergency]].<ref>{{Cite news | vauthors = Grady D |date=17 July 2019 |title=Congo's Ebola Outbreak Is Declared a Global Health Emergency |work=[[The New York Times]] |url=https://www.nytimes.com/2019/07/17/health/ebola-congo-who-emergency.html |access-date=17 July 2019 |archive-url=https://web.archive.org/web/20190717180831/https://www.nytimes.com/2019/07/17/health/ebola-congo-who-emergency.html |archive-date=17 July 2019 |issn=1553-8095 |oclc=1645522}}</ref> |
|||
==Signs and symptoms== |
==Signs and symptoms== |
||
[[File:Symptoms of ebola.png|thumb| |
[[File:Symptoms of ebola.png|thumb|upright=1.3|Signs and symptoms of Ebola<ref name="CDC2014S" />]] |
||
Signs and symptoms of Ebola usually begin suddenly with an [[influenza|flu]]-like stage characterized by fatigue, fever, headaches, and joint, muscle, and abdominal pain.<ref name="Gatherer 2014">{{cite journal | author = Gatherer D | title = The 2014 Ebola virus disease outbreak in West Africa | journal = J. Gen. Virol. | volume = 95 | issue = Pt 8 | pages = 1619–1624 | year = 2014 | pmid = 24795448 | doi = 10.1099/vir.0.067199-0 }}</ref><ref name=CDC2014S/> Vomiting, diarrhea and [[Anorexia (symptom)|loss of appetite]] are also common.<ref name=CDC2014S/> Less common symptoms include the following: sore throat, chest pain, hiccups, [[shortness of breath]] and [[dysphagia|trouble swallowing]].<ref name=CDC2014S/> The average time between contracting the infection and the start of symptoms is 8 to 10 days, but can occur between 2 and 21 days.<ref name=CDC2014S>{{cite web|title=Ebola Hemorrhagic Fever Signs and Symptoms|url=http://www.cdc.gov/vhf/ebola/symptoms/index.html|website=CDC|accessdate=2 August 2014|date=January 28, 2014}}</ref> Skin manifestations may include a [[maculopapular rash]] (in about 50% of cases).<ref name=Hoenen2006 /> Early symptoms of EVD may be similar to those of [[malaria]], [[dengue fever]], or other [[tropical fever]]s, before the disease progresses to the bleeding phase.<ref name="Gatherer 2014"/> |
|||
===Onset=== |
|||
<!-- Incubation --> |
|||
The length of time between exposure to the virus and the development of symptoms ([[incubation period]]) is between 2 and 21 days,<ref name=WHO2014/><ref name="CDC2014S">{{Cite web |date=28 January 2014 |title=Ebola Hemorrhagic Fever Signs and Symptoms |url=https://www.cdc.gov/vhf/ebola/symptoms/index.html |url-status=live |archive-url=https://web.archive.org/web/20140801015854/https://www.cdc.gov/vhf/ebola/symptoms/index.html |archive-date=1 August 2014 |access-date=2 August 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC) }}</ref> and usually between 4 and 10 days.<ref name="Goeijenbier2014">{{Cite journal |vauthors=Goeijenbier M, van Kampen JJ, Reusken CB, Koopmans MP, van Gorp EC |date=November 2014 |title=Ebola virus disease: a review on epidemiology, symptoms, treatment and pathogenesis |url=http://www.njmonline.nl/getpdf.php?t=a&id=10001148 |url-status=live |journal=Neth J Med |volume=72 |issue=9 |pages=442–448 |pmid=25387613 |archive-url=https://web.archive.org/web/20141129144852/http://www.njmonline.nl/getpdf.php?t=a&id=10001148 |archive-date=29 November 2014}}</ref> However, recent estimates based on mathematical models predict that around 5% of cases may take longer than 21 days to develop.<ref>{{Cite journal |vauthors=Haas CN |date=14 October 2014 |title=On the Quarantine Period for Ebola Virus |journal=PLOS Currents Outbreaks |volume=6 |doi=10.1371/currents.outbreaks.2ab4b76ba7263ff0f084766e43abbd89 |pmc=4205154 |pmid=25642371 |doi-access=free |issn=2157-3999}}</ref> |
|||
<!-- Early --> |
|||
Symptoms usually begin with a sudden [[influenza]]-like stage characterised by [[fatigue (medical)|fatigue]], [[fever]], [[asthenia|weakness]], [[anorexia (symptom)|decreased appetite]], [[myalgia|muscular pain]], [[arthralgia|joint pain]], headache, and sore throat.<ref name=WHO2014/><ref name="Goeijenbier2014" /><ref name="Gatherer 2014">{{Cite journal |vauthors=Gatherer D |date=August 2014 |title=The 2014 Ebola virus disease outbreak in West Africa |journal=J Gen Virol |volume=95 |issue=Pt 8 |pages=1619–1624 |doi=10.1099/vir.0.067199-0 |pmid=24795448 |doi-access=free}}</ref><ref name="Hun2012">{{Cite book | vauthors = Magill A |url= https://books.google.com/books?id=UgvdM8WRld4C&pg=PA332 |title=Hunter's tropical medicine and emerging infectious diseases |date=2013 |publisher=Saunders |isbn=978-1416043904 |edition=9th |location=New York |page=332 |author-link=Alan Magill |archive-url=https://web.archive.org/web/20160320072816/https://books.google.com/books?id=UgvdM8WRld4C&pg=PA332 |archive-date=20 March 2016 |url-status=live |name-list-style=vanc}}</ref> The fever is usually higher than {{convert|38.3|°C|°F|0}}.<ref name="Hoenen2006">{{Cite journal |vauthors=Hoenen T, Groseth A, Falzarano D, Feldmann H |date=May 2006 |title=Ebola virus: unravelling pathogenesis to combat a deadly disease |journal=Trends in Molecular Medicine |volume=12 |issue=5 |pages=206–215 |doi=10.1016/j.molmed.2006.03.006 |pmid=16616875}}</ref> This is often followed by nausea, vomiting, [[diarrhoea]], abdominal pain, and sometimes [[hiccups]].<ref name=Hun2012/><ref name="Brown2017">{{Cite journal |vauthors=Brown CS, Mepham S, Shorten RJ |date=June 2017 |title=Ebola Virus Disease: An Update on Epidemiology, Symptoms, Laboratory Findings, Diagnostic Issues, and Infection Prevention and Control Issues for Laboratory Professionals |journal=Clinical Laboratory Medicine |type=Review |volume=37 |issue=2 |pages=269–284 |doi=10.1016/j.cll.2017.01.003 |pmid=28457350}}</ref> The combination of severe vomiting and diarrhoea often leads to severe [[dehydration]].<ref name="Sharma2015">{{Cite journal |vauthors=Sharma N, Cappell MS |date=September 2015 |title=Gastrointestinal and Hepatic Manifestations of Ebola Virus Infection |journal=Digestive Diseases and Sciences |type=Review |volume=60 |issue=9 |pages=2590–2603 |doi=10.1007/s10620-015-3691-z |pmid=25972150 |s2cid=5674317|doi-access=free }}</ref> Next, [[shortness of breath]] and [[chest pain]] may occur, along with [[oedema|swelling]], [[headaches]], and [[decreased level of consciousness|confusion]].<ref name=Hun2012/> In about half of the cases, the skin may develop a [[maculopapular rash]], a flat red area covered with small bumps, five to seven days after symptoms begin.<ref name="Goeijenbier2014" /><ref name="Hoenen2006" /> |
|||
===Bleeding=== |
===Bleeding=== |
||
In some cases, internal and external bleeding may occur.<ref name="WHO2014" /> This typically begins five to seven days after the first symptoms.<ref name="urlwhqlibdoc.who.int">{{Cite book |title=Marburg and Ebola virus infections: a guide for their diagnosis, management, and control |vauthors=Simpson DI |publisher=World Health Organization |year=1977 |isbn=924170036X |page=10f |hdl=10665/37138 |id=WHO offset publication; no. 36 |hdl-access=free}}</ref> All infected people show some [[bleeding disorder|decreased blood clotting]].<ref name="Hoenen2006" /> Bleeding from mucous membranes or from sites of needle punctures has been reported in 40–50% of cases.<ref>{{Cite web | vauthors = King JW, Rafeek H | date = 14 January 2021 | veditors = Chandrasekar PH |title=Ebola Virus, Clinical Presentation |url=http://emedicine.medscape.com/article/216288-clinical#showall |url-status=live |archive-url=https://web.archive.org/web/20120101205843/http://emedicine.medscape.com/article/216288-clinical#showall |archive-date=1 January 2012 |access-date=30 July 2012 |publisher=Medscape }}</ref> This may cause [[haematemesis|vomiting blood]], [[haemoptysis|coughing up of blood]], or [[blood in stool]].<ref>{{Cite web |title=Appendix A: Disease-Specific Chapters – Chapter: Hemorrhagic fevers caused by: i) Ebola virus and ii) Marburg virus and iii) Other viral causes including bunyaviruses, arenaviruses, and flaviviruses |url=http://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/hemorrhagic_fevers_chapter.pdf |url-status=live |archive-url=https://web.archive.org/web/20141015081924/http://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/hemorrhagic_fevers_chapter.pdf |archive-date=15 October 2014 |access-date=9 October 2014 |publisher=[[Ministry of Health and Long-Term Care]]}}</ref> Bleeding into the skin may create [[petechia]]e, [[purpura]], [[Ecchymosis|ecchymoses]] or [[haematoma]]s (especially around needle injection sites).<ref name="Feldmann2011" /> [[Subconjunctival haemorrhage|Bleeding into the whites of the eyes]] may also occur.<ref name="ShanthaEye2016">{{cite journal | vauthors = Shantha JG, Yeh S, Nguyen QD | title = Ebola virus disease and the eye | journal = Current Opinion in Ophthalmology | volume = 27 | issue = 6 | pages = 538–544 | date = November 2016 | pmid = 27585217 | doi = 10.1097/ICU.0000000000000313 | type = Review | s2cid = 34367099 }}</ref> Heavy bleeding is uncommon; if it occurs, it is usually in the [[gastrointestinal tract]].<ref name="West2014">{{cite journal | vauthors = West TE, von Saint André-von Arnim A | title = Clinical presentation and management of severe Ebola virus disease | journal = Annals of the American Thoracic Society | volume = 11 | issue = 9 | pages = 1341–1350 | date = November 2014 | pmid = 25369317 | doi = 10.1513/AnnalsATS.201410-481PS | type = Review }}</ref> The incidence of bleeding into the gastrointestinal tract was reported to be ~58% in the 2001 outbreak in Gabon,<ref>{{cite journal | vauthors = Sharma N, Cappell MS | title = Gastrointestinal and Hepatic Manifestations of Ebola Virus Infection | journal = Digestive Diseases and Sciences | volume = 60 | issue = 9 | pages = 2590–2603 | date = September 2015 | pmid = 25972150 | doi = 10.1007/s10620-015-3691-z | s2cid = 5674317 | doi-access = free }}</ref> but in the 2014–15 outbreak in the US it was ~18%,<ref>{{Cite web |date=6 January 2020 |title=Ebola virus disease Information for Clinicians in U.S. Healthcare Settings {{!}} For Clinicians {{!}} Ebola (Ebola Virus Disease) {{!}} Ebola Hemorrhagic Fever {{!}} CDC |url=https://www.cdc.gov/vhf/ebola/clinicians/evd/clinicians.html |access-date=22 March 2020 |website=www.cdc.gov |language=en-us |archive-date=1 April 2020 |archive-url=https://web.archive.org/web/20200401143748/https://www.cdc.gov/vhf/ebola/clinicians/evd/clinicians.html |url-status=live }}</ref> possibly due to improved prevention of [[disseminated intravascular coagulation]].<ref name="Sharma2015" /> |
|||
In the bleeding phase internal and subcutaneous bleeding may present itself through [[red eyes (medicine)|reddening of the eyes]] and [[hematemesis|bloody vomit]].<ref name="Gatherer 2014"/> Bleeding into the skin may create [[petechia]]e, [[purpura]], [[Ecchymosis|ecchymoses]], and [[hematoma]]s (especially around needle injection sites). |
|||
===Recovery or death=== |
|||
Recovery may begin between seven and 14 days after first symptoms.<ref name=Hun2012/> Death, if it occurs, follows typically six to sixteen days from first symptoms and is often due to [[hypovolemic shock|shock from fluid loss]].<ref name=Ruz2014/> In general, bleeding often indicates a worse outcome, and blood loss may result in death.<ref name="Gatherer 2014" /> People are often in a [[coma]] near the end of life.<ref name=Hun2012/> |
|||
Those who survive often have ongoing muscular and joint pain, [[hepatitis|liver inflammation]], and decreased hearing, and may have continued tiredness, continued weakness, decreased appetite, and difficulty returning to pre-illness weight.<ref name="Hun2012" /><ref name="Tosh2014" /> Problems with vision may develop.<ref>{{Cite web |date=7 August 2015 |title=An emergency within an emergency: caring for Ebola survivors |url=https://www.afro.who.int/news/emergency-within-emergency-caring-ebola-survivors |url-status=live |archive-url=https://web.archive.org/web/20150813163313/https://www.afro.who.int/en/sierra-leone/press-materials/item/7908-an-emergency-within-an-emergency-caring-for-ebola-survivors.html |archive-date=13 August 2015 |access-date=12 August 2015 |publisher=[[World Health Organization]] (WHO)}}</ref> It is recommended that survivors of EVD wear condoms for at least twelve months after initial infection or until the semen of a male survivor tests negative for Ebola virus on two separate occasions.<ref>{{Cite web |title=Ebola Virus Disease |url=https://srhd.org/health-topics/diseases-conditions/ebola |access-date=15 September 2020 |website=SRHD |language=en-US |archive-date=15 September 2020 |archive-url=https://web.archive.org/web/20200915145404/https://srhd.org/health-topics/diseases-conditions/ebola |url-status=live }}</ref> |
|||
Survivors develop [[antibodies]] against Ebola that last at least 10 years, but it is unclear whether they are immune to additional infections.<ref name="CDC2014QAT" /> |
|||
==Cause== |
|||
EVD in humans is caused by four of six viruses of the genus ''[[Ebolavirus]]''. The four are [[Bundibugyo virus]] (BDBV), [[Sudan virus]] (SUDV), [[Taï Forest virus]] (TAFV) and one simply called [[Ebola virus]] (EBOV, formerly Zaire Ebola virus).<ref name="Hoenen2012" /> EBOV, species ''[[Zaire ebolavirus]]'', is the most dangerous of the known EVD-causing viruses, and is responsible for the largest number of outbreaks.<ref name="KuhnArch">{{Cite journal |display-authors=6 |vauthors=Kuhn JH, Becker S, Ebihara H, Geisbert TW, Johnson KM, Kawaoka Y, Lipkin WI, Negredo AI, Netesov SV, Nichol ST, Palacios G, Peters CJ, Tenorio A, Volchkov VE, Jahrling PB |date=December 2010 |title=Proposal for a revised taxonomy of the family Filoviridae: Classification, names of taxa and viruses, and virus abbreviations |journal=Archives of Virology |volume=155 |issue=12 |pages=2083–2103 |doi=10.1007/s00705-010-0814-x |pmc=3074192 |pmid=21046175}}</ref> The fifth and sixth viruses, [[Reston virus]] (RESTV) and [[Bombali ebolavirus|Bombali virus]] (BOMV),<ref>{{Cite web |vauthors=Branswell H |date=27 July 2018 |title=New Ebola species is reported for first time in a decade |url=https://www.statnews.com/2018/07/27/ebola-virus-discovery/ |access-date=8 July 2022 |website=[[Stat (website)|Stat]] |language=en-US |archive-date=27 July 2018 |archive-url=https://web.archive.org/web/20180727151617/https://www.statnews.com/2018/07/27/ebola-virus-discovery/ |url-status=live }}</ref> are not thought to cause disease in humans, but have caused disease in other primates.<ref name="Spickler">{{Cite web | vauthors = Spickler A |title=Ebolavirus and Marburgvirus Infections |url=http://www.cfsph.iastate.edu/Factsheets/pdfs/viral_hemorrhagic_fever_filovirus.pdf |url-status=live |archive-url=https://web.archive.org/web/20150430165458/http://www.cfsph.iastate.edu/Factsheets/pdfs/viral_hemorrhagic_fever_filovirus.pdf |archive-date=30 April 2015}}</ref><ref>{{Cite web |title=About Ebola Virus Disease |url=https://www.cdc.gov/vhf/ebola/about.html |url-status=live |archive-url=https://web.archive.org/web/20141016080233/https://www.cdc.gov/vhf/ebola/about.html |archive-date=16 October 2014 |access-date=18 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> All six viruses are closely related to [[marburgvirus]]es.<ref name="Hoenen2012" /> |
|||
===Virology=== |
|||
{{Main|Ebolavirus|l1=''Ebolavirus'' (taxonomic group)|Ebola virus|l2=Ebola virus (specific virus)}} |
|||
[[File:Ebola virus virion.jpg|thumb|[[Electron micrograph]] of an Ebola virus [[virion]]]] |
|||
Ebolaviruses contain single-stranded, non-infectious [[RNA]] [[genome]]s.<ref name="Fauquet2005">{{Cite book | vauthors = Pringle CR |title=Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses |publisher=Elsevier/Academic Press |year=2005 |isbn=978-0-12-370200-5 | veditors = Fauquet CM, Mayo MA, Maniloff J, Desselberger U, Ball LA |location=San Diego |pages=609–614 |chapter=Order Mononegavirales }}</ref> ''Ebolavirus'' genomes contain seven [[gene]]s including [[Three prime untranslated region|3'-UTR]]-''NP''-''VP35''-''VP40''-''GP''-''VP30''-''VP24''-''L''-[[Five prime untranslated region|5'-UTR]].<ref name="Feldmann2011" /><ref name="Stahelin2014">{{Cite journal |vauthors=Stahelin RV |date=June 2014 |title=Membrane binding and bending in Ebola VP40 assembly and egress |journal=Front Microbiol |volume=5 |page=300 |doi=10.3389/fmicb.2014.00300 |pmc=4061899 |pmid=24995005 |doi-access=free}}</ref> The genomes of the five different ebolaviruses (BDBV, EBOV, RESTV, SUDV and TAFV) differ in [[nucleic acid sequence|sequence]] and the number and location of gene overlaps. As with all [[filovirus]]es, ebolavirus virions are filamentous particles that may appear in the shape of a shepherd's crook, of a "U" or of a "6," and they may be coiled, toroid or branched.<ref name="Stahelin2014" /><ref>{{Cite journal |display-authors=6 |vauthors=Ascenzi P, Bocedi A, Heptonstall J, Capobianchi MR, Di Caro A, Mastrangelo E, Bolognesi M, Ippolito G |date=June 2008 |title=Ebolavirus and Marburgvirus: insight the Filoviridae family |url=https://air.unimi.it/retrieve/handle/2434/53604/1077822/Ebola_2008%29_Proofs.pdf |journal=Mol Aspects Med |volume=29 |issue=3 |pages=151–185 |doi=10.1016/j.mam.2007.09.005 |pmid=18063023 |hdl-access=free |hdl=2434/53604 |access-date=20 August 2019 |archive-date=8 March 2021 |archive-url=https://web.archive.org/web/20210308082442/https://air.unimi.it/retrieve/handle/2434/53604/1077822/Ebola_2008)_Proofs.pdf |url-status=live }}</ref> In general, ebolavirions are 80 nanometers (nm) in width and may be as long as 14,000 nm.<ref name="Chippaux2014">{{Cite journal |vauthors=Chippaux JP |date=October 2014 |title=Outbreaks of Ebola virus disease in Africa: the beginnings of a tragic saga |journal=J Venom Anim Toxins Incl Trop Dis |volume=20 |issue=1 |page=44 |doi=10.1186/1678-9199-20-44 |pmc=4197285 |pmid=25320574 |doi-access=free }}</ref> |
|||
All people infected show some symptoms of [[circulatory system]] involvement, including [[bleeding disorder| impaired blood clotting]].<ref name=Hoenen2006 /> Bleeding from puncture sites and [[mucous membrane]]s (e.g. [[human gastrointestinal tract|gastrointestinal tract]], [[nose]], [[vagina]] and [[gums]]) is reported in 40–50% of cases.<ref>{{cite web | title = Ebola Virus, Clinical Presentation | publisher = Medscape | url = http://emedicine.medscape.com/article/216288-clinical#a0217|accessdate=2012-07-30 }}</ref> Types of bleeding known to occur with Ebola virus disease include [[hematemesis|vomiting blood]], [[hemoptysis|coughing it up]] or [[Blood in stool|blood in the stool]]. Heavy bleeding is rare and is usually confined to the gastrointestinal tract.<ref name=Hoenen2006>{{cite journal | author = Hoenen T, Groseth A, Falzarano D, Feldmann H | title = Ebola virus: unravelling pathogenesis to combat a deadly disease | journal = Trends in Molecular Medicine | volume = 12 | issue = 5 | pages = 206–215 | date = May 2006 | pmid = 16616875 | doi = 10.1016/j.molmed.2006.03.006 }}</ref><ref>{{cite journal | author = Fisher-Hoch SP, Platt GS, Neild GH, Southee T, Baskerville A, Raymond RT, Lloyd G, Simpson DI | title = Pathophysiology of shock and hemorrhage in a fulminating viral infection (Ebola) | journal = J. Infect. Dis. | volume = 152 | issue = 5 | pages = 887–894 | year = 1985 | pmid = 4045253 | doi = 10.1093/infdis/152.5.887 }}</ref> In general, the development of bleeding symptoms often indicates a worse prognosis and this blood loss can result in death.<ref name=Gath2014>{{cite journal|last1=Gatherer|first1=D|title=The 2014 Ebola virus disease outbreak in West Africa.|journal=The Journal of general virology|date=2014 Aug|volume=95|issue=Pt 8|pages=1619-1624|pmid=24795448}}</ref> |
|||
Their [[Biological life cycle|life cycle]] is thought to begin with a virion attaching to specific [[Cell surface receptor|cell-surface receptors]] such as [[C-type lectin]]s, [[DC-SIGN]], or [[integrin]]s, which is followed by fusion of the [[Pinocytosis|viral envelope with cellular membranes]].<ref name="Misasi2014">{{Cite journal |vauthors=Misasi J, Sullivan NJ |date=October 2014 |title=Camouflage and Misdirection: The Full-On Assault of Ebola Virus Disease |journal=Cell |volume=159 |issue=3 |pages=477–486 |doi=10.1016/j.cell.2014.10.006 |pmc=4243531 |pmid=25417101}}</ref> The virions taken up by the cell then travel to acidic [[endosome]]s and [[lysosome]]s where the viral envelope glycoprotein GP is cleaved.<ref name="Misasi2014" /> This processing appears to allow the virus to bind to cellular proteins enabling it to fuse with internal cellular membranes and release the viral [[nucleocapsid]].<ref name="Misasi2014" /> The ''Ebolavirus'' structural glycoprotein (known as GP1,2) is responsible for the virus' ability to bind to and infect targeted cells.<ref name="Kuhl2012">{{Cite journal |vauthors=Kühl A, Pöhlmann S |date=September 2012 |title=How Ebola virus counters the interferon system |journal=Zoonoses Public Health |volume=59 |issue=Supplement 2 |pages=116–131 |doi=10.1111/j.1863-2378.2012.01454.x |pmc=7165950 |pmid=22958256}}</ref> The viral [[RNA-dependent RNA polymerase|RNA polymerase]], encoded by the ''L'' gene, partially uncoats the nucleocapsid and [[Transcription (genetics)|transcribes]] the genes into positive-strand [[mRNA]]s, which are then [[translation (biology)|translated]] into structural and nonstructural proteins. The most abundant protein produced is the nucleoprotein, whose concentration in the host cell determines when L switches from gene transcription to genome replication. Replication of the viral genome results in full-length, positive-strand antigenomes that are, in turn, transcribed into genome copies of negative-strand virus progeny.<ref name="Olejnik2011" /> Newly synthesised structural proteins and genomes self-assemble and accumulate near the inside of the [[cell membrane]]. Virions [[Budding|bud]] off from the cell, gaining their envelopes from the cellular membrane from which they bud. The mature progeny particles then infect other cells to repeat the cycle. The genetics of the Ebola virus are difficult to study because of EBOV's virulent characteristics.<ref name="Feldmann2005">{{Cite book | vauthors = Feldmann H, Geisbert TW, Jahrling PB, Klenk H, Netesov SV, Peters CJ, Sanchez A, Swanepoel R, Volchkov VE |title=Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses | publisher=Elsevier/Academic Press |year=2005 |isbn=978-0123702005 | veditors = Fauquet CM, Mayo MA, Maniloff J, Desselberger U, Ball LA }}</ref> |
|||
==Causes== |
|||
{{Main| Ebolavirus}} |
|||
[[File:EbolaCycle.png|thumb|Life cycles of the Ebolavirus]] |
|||
EVD is caused by four of five viruses classified in the genus ''[[Ebolavirus]]'', family ''[[Filoviridae]]'', order ''[[Mononegavirales]]''. These four viruses are [[Bundibugyo virus]] (BDBV), [[Ebola virus]] (EBOV), [[Sudan virus]] (SUDV), [[Taï Forest virus]] (TAFV). The fifth virus, [[Reston virus]] (RESTV), is not thought to be disease-causing in humans. During an outbreak those at highest risk are health care workers and close contacts of those with the infection.<ref>{{cite web|title=Ebola Hemorrhagic Fever Risk of Exposure|url=http://www.cdc.gov/vhf/ebola/exposure/index.html|website=CDC|accessdate=2 August 2014|date=August 1, 2014}}</ref> |
|||
===Transmission=== |
===Transmission=== |
||
[[File:EbolaCycle.png|thumb|upright=1.8|Life cycles of the ''[[Ebolavirus]]'']] |
|||
<!-- Main route --> |
|||
[[File:Ebola illustration- safe burial (15573264517).jpg|thumb|An illustration of safe burial practices]] |
|||
It is not entirely clear how Ebola is spread.<ref name=CDC2014P>{{cite web|title=Ebola Hemorrhagic Fever Prevention|url=http://www.cdc.gov/vhf/ebola/prevention/index.html|website=CDC|accessdate=2 August 2014|date=July 31, 2014}}</ref> EVD is believed to occur after an ebola virus is transmitted to an initial human by contact with an infected animal's bodily fluids. Human-to-human transmission can occur via direct contact with blood or bodily fluids from an infected person (including [[embalming]] of an infected dead person) or by contact with contaminated medical equipment, particularly needles and syringes.<ref name=CDCPress2014/> Semen is infectious in survivors for up to 50 days. Transmission through oral exposure and through [[conjunctiva]] exposure is likely<ref>{{cite journal | author = Jaax N, Jahrling P, Geisbert T, Geisbert J, Steele K, McKee K, Nagley D, Johnson E, Jaax G, Peters C | title = Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory | journal = Lancet | volume = 346 | issue = 8991–8992 | pages = 1669–1671 | date = Dec 1995 | pmid = 8551825 | doi = 10.1016/S0140-6736(95)92841-3 | issn = 0140-6736 }}</ref> and has been confirmed in non-human primates.<ref>{{cite journal | author = Jaax NK, Davis KJ, Geisbert TJ, Vogel P, Jaax GP, Topper M, Jahrling PB | title = Timed appearance of lymphocytic choriomeningitis virus after gastric inoculation of mice | journal = Archives of pathology & laboratory medicine | volume = 120 | issue = 2 | pages = 140–155 | date = Feb 1996 | pmid = 8712894 | first4 = P. | issn = 0003-9985 | first2 = K. J. | first5 = G. P. | first3 = T. J. | first6 = M. | first7 = P. B. }}</ref> The potential for widespread EVD infections is considered low as the disease is only spread by direct contact with the secretions from someone who is showing signs of infection.<ref name=CDCPress2014>{{cite web|title=CDC Telebriefing on Ebola outbreak in West Africa|url=http://www.cdc.gov/media/releases/2014/t0728-ebola.html|website=CDC|accessdate=3 August 2014|date=July 28, 2014}}</ref> The quick onset of symptoms makes it easier to identify sick individuals and limits a person's ability to spread the disease by traveling. Because dead bodies are still infectious, some doctors disposed of them in a safe manner, despite local traditional burial rituals.<ref name="nyt">{{Cite news|first=Blaine|last=Harden|title=Dr. Matthew's Passion|url=http://www.nytimes.com/library/magazine/home/20010218mag%2debola.html|work=[[New York Times]] Magazine|date=2001-02-18|accessdate=2008-02-25}}</ref> |
|||
<!-- Between people --> |
|||
It is believed that between people, Ebola disease spreads only by direct contact with the blood or other [[body fluid]]s of a person who has developed symptoms of the disease.<ref name="Funk2014" /><ref>{{Cite web |date=5 November 2014 |title=Ebola (Ebola Virus Disease) Transmission |url=https://www.cdc.gov/vhf/ebola/transmission/index.html |url-status=live |archive-url=https://web.archive.org/web/20141106022141/https://www.cdc.gov/vhf/ebola/transmission/index.html |archive-date=6 November 2014 |access-date=7 November 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref><ref name="Drazen2014">{{Cite journal |vauthors=Drazen JM, Kanapathipillai R, Campion EW, Rubin EJ, Hammer SM, Morrissey S, Baden LR |date=November 2014 |title=Ebola and quarantine |journal=N Engl J Med |volume=371 |issue=21 |pages=2029–2030 |doi=10.1056/NEJMe1413139 |pmid=25347231|doi-access=free }}</ref> Body fluids that may contain Ebola viruses include saliva, mucus, vomit, feces, sweat, tears, breast milk, urine and [[semen]].<ref name=cdc9months/><ref name=CDC2014QAT/> The WHO states that only people who are very sick are able to spread Ebola disease in [[saliva]], and the virus has not been reported to be transmitted through sweat. Most people spread the virus through blood, [[feces]] and vomit.<ref>{{Cite news | vauthors = McNeil Jr DG |author-link=Donald McNeil Jr. |name-list-style=vanc |date=3 October 2014 |title=Ask Well: How Does Ebola Spread? How Long Can the Virus Survive? |work=[[The New York Times]] |url=http://well.blogs.nytimes.com/2014/10/03/ebola-ask-well-spread-public-transit/ |url-status=live |access-date=24 October 2014 |archive-url=https://web.archive.org/web/20141024061521/http://well.blogs.nytimes.com/2014/10/03/ebola-ask-well-spread-public-transit/ |archive-date=24 October 2014 }}</ref> Entry points for the virus include the nose, mouth, eyes, open wounds, cuts and abrasions.<ref name="CDC2014QAT">{{Cite web |date=September 2014 |title=Q&A on Transmission, Ebola |url=https://www.cdc.gov/vhf/ebola/transmission/qas.html |url-status=live |archive-url=https://web.archive.org/web/20141002210702/https://www.cdc.gov/vhf/ebola/transmission/qas.html |archive-date=2 October 2014 |access-date=3 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> Ebola may be spread through large [[Transmission (medicine)#Droplet|droplets]]; however, this is believed to occur only when a person is very sick.<ref name="CDCNOV2014">{{Cite web |date=1 November 2014 |title=How Ebola Is Spread |url=https://www.cdc.gov/vhf/ebola/pdf/infections-spread-by-air-or-droplets.pdf |url-status=live |archive-url=https://web.archive.org/web/20170708092027/https://www.cdc.gov/vhf/ebola/pdf/infections-spread-by-air-or-droplets.pdf |archive-date=8 July 2017 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> This contamination can happen if a person is splashed with droplets.<ref name=CDCNOV2014/> Contact with surfaces or objects contaminated by the virus, particularly needles and syringes, may also transmit the infection.<ref name=CDC2014T/><ref name="Chowell2014" /> The virus is able to survive on objects for a few hours in a dried state, and can survive for a few days within body fluids outside of a person.<ref name=CDC2014QAT/><ref name=Ost2015/> |
|||
The Ebola virus may be able to persist for more than three months in the semen after recovery, which could lead to infections via [[sexual intercourse]].<ref name=cdc9months/><ref>{{Cite web |date=4 April 2015 |title=Sexual transmission of the Ebola Virus : evidence and knowledge gaps |url=https://www.who.int/reproductivehealth/topics/rtis/ebola-virus-semen/en/ |url-status=live |archive-url=https://web.archive.org/web/20150414084657/https://www.who.int/reproductivehealth/topics/rtis/ebola-virus-semen/en/ |archive-date=14 April 2015 |access-date=16 April 2015 |publisher=[[World Health Organization]] (WHO)}}</ref><ref>{{Cite news | vauthors = Wu B |date=2 May 2015 |title=Ebola Can Be Transmitted Through Sex |work=Science Times |url=http://www.sciencetimes.com/articles/6000/20150502/ebola-transmitted-through-sex.htm |url-status=live |access-date=3 May 2015 |archive-url=https://web.archive.org/web/20150502222419/http://www.sciencetimes.com/articles/6000/20150502/ebola-transmitted-through-sex.htm |archive-date=2 May 2015}}</ref> Virus persistence in semen for over a year has been recorded in a national screening programme.<ref>{{Cite journal |display-authors=6 |vauthors=Soka MJ, Choi MJ, Baller A, White S, Rogers E, Purpura LJ, Mahmoud N, Wasunna C, Massaquoi M, Abad N, Kollie J, Dweh S, Bemah PK, Christie A, Ladele V, Subah OC, Pillai S, Mugisha M, Kpaka J, Kowalewski S, German E, Stenger M, Nichol S, Ströher U, Vanderende KE, Zarecki SM, Green HH, Bailey JA, Rollin P, Marston B, Nyenswah TG, Gasasira A, Knust B, Williams D |year=2016 |title=Prevention of sexual transmission of Ebola in Liberia through a national semen testing and counselling programme for survivors: an analysis of Ebola virus RNA results and behavioural data |journal=Lancet Global Health |volume=4 |issue=10 |pages=e736–e743 |doi=10.1016/S2214-109X(16)30175-9 |pmid=27596037 |doi-access=free}}</ref> Ebola may also occur in the breast milk of women after recovery, and it is not known when it is safe to breastfeed again.<ref name=CDCBreast2014/> The virus was also found in the eye of [[Ian Crozier|one patient]], in 2014, two months after it was cleared from his blood.<ref>{{Cite journal |display-authors=6 |vauthors=Varkey JB, Shantha JG, Crozier I, Kraft CS, Lyon GM, Mehta AK, Kumar G, Smith JR, Kainulainen MH, Whitmer S, Ströher U, Uyeki TM, Ribner BS, Yeh S |date=7 May 2015 |title=Persistence of Ebola Virus in Ocular Fluid during Convalescence |journal=The New England Journal of Medicine |volume=372 |issue=25 |pages=2423–227 |doi=10.1056/NEJMoa1500306 |pmc=4547451 |pmid=25950269 |hdl=2328/35704}}</ref> Otherwise, people who have recovered are not infectious.<ref name=CDC2014T/> |
|||
The potential for [[pandemics|widespread infections]] in countries with medical systems capable of observing correct medical isolation procedures is considered low.<ref name="CDCPress2014">{{Cite web |date=28 July 2014 |title=CDC Telebriefing on Ebola outbreak in West Africa |url=https://www.cdc.gov/media/releases/2014/t0728-ebola.html |url-status=live |archive-url=https://web.archive.org/web/20140802025607/https://www.cdc.gov/media/releases/2014/t0728-ebola.html |archive-date=2 August 2014 |access-date=3 August 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> Usually when someone has symptoms of the disease, they are unable to travel without assistance.<ref name="WHO2014T">{{Cite web |date=14 August 2014 |title=Air travel is low-risk for Ebola transmission |url=https://www.who.int/mediacentre/news/notes/2014/ebola-travel/en/ |url-status=dead |archive-url=https://web.archive.org/web/20150119231747/https://www.who.int/mediacentre/news/notes/2014/ebola-travel/en/ |archive-date=19 January 2015 |publisher=[[World Health Organization]] (WHO)}}</ref> |
|||
<!-- Dead bodies --> |
|||
Dead bodies remain infectious; thus, people handling human remains in practices such as traditional burial rituals or more modern processes such as [[embalming]] are at risk.<ref name=CDCPress2014/> Of the cases of Ebola infections in Guinea during the 2014 outbreak, 69% are believed to have been contracted via unprotected (or unsuitably protected) contact with infected corpses during certain Guinean burial rituals.<ref name="Chan2014">{{Cite journal |vauthors=Chan M |date=September 2014 |title=Ebola virus disease in West Africa – no early end to the outbreak |journal=N Engl J Med |volume=371 |issue=13 |pages=1183–1185 |doi=10.1056/NEJMp1409859 |pmid=25140856|doi-access=free }}</ref><ref>{{Cite web |title=Sierra Leone: a traditional healer and a funeral |url=https://www.who.int/csr/disease/ebola/ebola-6-months/sierra-leone/en/ |url-status=dead |archive-url=https://web.archive.org/web/20141006082559/https://www.who.int/csr/disease/ebola/ebola-6-months/sierra-leone/en/ |archive-date=6 October 2014 |access-date=6 October 2014 |publisher=[[World Health Organization]] (WHO) }}</ref> |
|||
<!-- Hospitals --> |
<!-- Hospitals --> |
||
Health-care workers treating people with Ebola are at greatest risk of infection.<ref name="CDC2014T">{{Cite web |date=17 October 2014 |title=Transmission |url=https://www.cdc.gov/vhf/ebola/transmission/ |url-status=live |archive-url=https://web.archive.org/web/20141019024316/https://www.cdc.gov/vhf/ebola/transmission/ |archive-date=19 October 2014 |access-date=18 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> The risk increases when they do not have appropriate protective clothing such as masks, gowns, gloves and eye protection; do not wear it properly; or handle contaminated clothing incorrectly.<ref name=CDC2014T/> This risk is particularly common in parts of Africa where the disease mostly occurs and health systems function poorly.<ref>{{Cite web | vauthors = Salaam-Blyther T |date=26 August 2014 |title=The 2014 Ebola Outbreak: International and U.S. Responses |url=https://fas.org/sgp/crs/row/R43697.pdf |url-status=live |archive-url=https://web.archive.org/web/20140903122230/http://fas.org/sgp/crs/row/R43697.pdf |archive-date=3 September 2014 |access-date=9 September 2014}}</ref> There has been transmission [[nosocomial|in hospitals]] in some African countries that reuse hypodermic needles.<ref>{{Cite book |url=https://books.google.com/books?id=fsaWlKQ4OjcC&pg=PA141 |title=Emerging infectious diseases trends and issues |date=2007 |publisher=Springer |isbn=978-0826103505 | veditors = Lashley FR, Durham JD |edition=2nd |location=New York |page=141 |archive-url=https://web.archive.org/web/20160509224252/https://books.google.com/books?id=fsaWlKQ4OjcC&pg=PA141 |archive-date=9 May 2016 |url-status=live}}</ref><ref>{{Cite book |url=https://books.google.com/books?id=x15umovaD08C&pg=PA170 |title=Hunter's tropical medicine and emerging infectious disease |publisher=Elsevier |year=2013 |isbn=978-1455740437 | veditors = Magill AJ, Strickland GT, Maguire JH, Ryan ET, Solomon T |edition=9th |location=London; New York |pages=170–172 |oclc=822525408 |archive-url=https://web.archive.org/web/20160520120141/https://books.google.com/books?id=x15umovaD08C&pg=PA170 |archive-date=20 May 2016 |url-status=live}}</ref> Some health-care centres caring for people with the disease do not have running water.<ref name="CDCQA2014">{{Cite web |date=22 May 2018 |title=Questions and Answers on Ebola Hemorrhagic Fever |url=https://www.cdc.gov/vhf/ebola/outbreaks/guinea/qa.html |url-status=live |archive-url=https://web.archive.org/web/20170728032458/https://www.cdc.gov/vhf/ebola/outbreaks/guinea/qa.html |archive-date=28 July 2017 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> In the United States the spread to two medical workers treating infected patients prompted criticism of inadequate training and procedures.<ref name="NBC-ebolaTX">{{Cite web |date=15 October 2014 |title=Ebola in Texas: Second Health Care Worker Tests Positive |url=https://www.nbcnews.com/storyline/ebola-virus-outbreak/ebola-texas-second-health-care-worker-tests-positive-n226161 |url-status=live |archive-url=https://web.archive.org/web/20141015211852/http://www.nbcnews.com/storyline/ebola-virus-outbreak/ebola-texas-second-health-care-worker-tests-positive-n226161 |archive-date=15 October 2014 |website=NBC News}}</ref> |
|||
Medical workers who do not wear appropriate protective clothing may also contract the disease.<ref>{{Citation | title = Ebola virus and Marburg virus: Causes | publisher = Mayo Clinic | url = http://www.mayoclinic.org/diseases-conditions/ebola-virus/basics/causes/con-20031241 | author = Mayo Clinic Staff }}</ref> In the past, [[nosocomial|hospital-acquired]] transmission has occurred in African hospitals due to the reuse of needles and lack of [[universal precautions]].<ref>{{cite book|last1=Lashley|first1=edited by Felissa R.|last2=Durham|first2=Jerry D.|title=Emerging infectious diseases trends and issues|date=2007|publisher=Springer Pub. Co.|location=New York|isbn=9780826103505|page=141|edition=2nd ed.|url=http://books.google.ca/books?id=fsaWlKQ4OjcC&pg=PA141}}</ref> |
|||
<!-- |
<!-- Air, water, insects --> |
||
Human-to-human transmission of EBOV through the air has not been reported to occur during EVD outbreaks,<ref name=WHOAir2014/> and airborne transmission has only been demonstrated in very strict laboratory conditions, and then only from pigs to [[primates]], but not from primates to primates.<ref name="Funk2014" /><ref name="Chowell2014" /> Spread of EBOV by water, or food other than bushmeat, has not been observed.<ref name=CDC2014T/><ref name="Chowell2014" /> No spread by mosquitos or other insects has been reported.<ref name=CDC2014T/> Other possible methods of transmission are being studied.<ref name="Ost2015">{{Cite journal |display-authors=6 |vauthors=Osterholm MT, Moore KA, Kelley NS, Brosseau LM, Wong G, Murphy FA, Peters CJ, LeDuc JW, Russell PK, Van Herp M, Kapetshi J, Muyembe JJ, Ilunga BK, Strong JE, Grolla A, Wolz A, Kargbo B, Kargbo DK, Sanders DA, Kobinger GP |date=19 February 2015 |title=Transmission of Ebola viruses: what we know and what we do not know |journal=mBio |volume=6 |issue=2 |pages=e00137 |doi=10.1128/mBio.00137-15 |pmc=4358015 |pmid=25698835}}</ref> |
|||
EVD is not naturally transmitted through the air.<ref name=WHOAir2014/> They are, however, infectious as breathable 0.8–1.2 micrometre laboratory generated droplets;<ref>{{cite journal | author = Johnson E, Jaax N, White J, Jahrling P | title = Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus | journal = International journal of experimental pathology | volume = 76 | issue = 4 | pages = 227–236 | date = Aug 1995 | pmid = 7547435 | pmc = 1997182 | first4 = P. | issn = 0959-9673 | first2 = N. | first3 = J. }}</ref> because of this potential route of infection, these viruses have been classified as Category A biological weapons.<ref>{{cite journal | author = Leffel EK, Reed DS | title = Marburg and Ebola viruses as aerosol threats | journal = Biosecurity and bioterrorism : biodefense strategy, practice, and science | volume = 2 | issue = 3 | pages = 186–191 | year = 2004 | pmid = 15588056 | doi = 10.1089/bsp.2004.2.186 | issn = 1538-7135 | month = }}</ref> Recently the virus has been shown to travel without contact from pigs to non-human [[primate]]s.<ref name="pmid23155478">{{cite journal | author = Weingartl HM, Embury-Hyatt C, Nfon C, Leung A, Smith G, Kobinger G | title = Transmission of Ebola virus from pigs to non-human primates | journal = Sci Rep | volume = 2 | issue = | pages = 811 | year = 2012 | pmid = 23155478 | pmc = 3498927 | doi = 10.1038/srep00811 }}</ref> |
|||
Airborne transmission among humans is theoretically possible due to the presence of Ebola virus particles in saliva, which can be discharged into the air with a cough or sneeze, but observational data from previous epidemics suggests the actual risk of airborne transmission is low.<ref name="Jones2015">{{Cite journal |vauthors=Jones RM, Brosseau LM |date=May 2015 |title=Aerosol transmission of infectious disease |journal=Journal of Occupational and Environmental Medicine |type=Review |volume=57 |issue=5 |pages=501–508 |doi=10.1097/JOM.0000000000000448 |pmid=25816216 |s2cid=11166016}}</ref> A number of studies examining airborne transmission broadly concluded that transmission from pigs to primates could happen without direct contact because, unlike humans and primates, pigs with EVD get very high ebolavirus concentrations in their lungs, and not their bloodstream.<ref name="virology1">{{Cite web |date=27 September 2014 |title=Transmission of Ebola virus |url=http://www.virology.ws/2014/09/27/transmission-of-ebola-virus/ |url-status=live |archive-url=https://web.archive.org/web/20160129111738/http://www.virology.ws/2014/09/27/transmission-of-ebola-virus/ |archive-date=29 January 2016 |access-date=22 January 2016 |website=virology.ws}}</ref> Therefore, pigs with EVD can spread the disease through droplets in the air or on the ground when they sneeze or cough.<ref name="sb1">{{Cite journal |vauthors=Weingartl HM, Embury-Hyatt C, Nfon C, Leung A, Smith G, Kobinger G |date=2012 |title=Transmission of Ebola virus from pigs to non-human primates |journal=Scientific Reports |volume=2 |page=811 |bibcode=2012NatSR...2..811W |doi=10.1038/srep00811 |pmc=3498927 |pmid=23155478}}</ref> By contrast, humans and other primates accumulate the virus throughout their body and specifically in their blood, but not very much in their lungs.<ref name="sb1" /> It is believed that this is the reason researchers have observed pig to primate transmission without physical contact, but no evidence has been found of primates being infected without actual contact, even in experiments where infected and uninfected primates shared the same air.<ref name="virology1" /><ref name="sb1" /> |
|||
Bats drop partially eaten fruits and pulp, then land mammals such as gorillas and [[duiker]]s feed on these fallen fruits. This chain of events forms a possible indirect means of transmission from the natural host to animal populations, which have led to research towards viral shedding in the saliva of bats. Fruit production, animal behavior, and other factors vary at different times and places that may trigger outbreaks among animal populations.<ref>{{cite journal | author = Gonzalez JP, Pourrut X, Leroy E | title = Ebolavirus and other filoviruses | journal = Current topics in microbiology and immunology | volume = 315 | pages = 363–387 | year = 2007 | pmid = 17848072 | doi = 10.1007/978-3-540-70962-6_15 | isbn = 978-3-540-70961-9 | series = Current Topics in Microbiology and Immunology }}</ref> |
|||
=== |
===Initial case=== |
||
<!-- Animals to humans --> |
|||
[[File:Bushmeat - Buschfleisch Ghana.JPG|thumb|[[Bushmeat]] being prepared for cooking in [[Ghana]], 2013. Human consumption of equatorial animals in Africa in the form of bushmeat has been linked to the transmission of diseases to people, including Ebola.<ref name="urlAfrican monkey meat that could be behind the next HIV - Health News - Health & Families - The Independent">{{cite web | url = http://www.independent.co.uk/life-style/health-and-families/health-news/african-monkey-meat-that-could-be-behind-the-next-hiv-7786152.html | title = African monkey meat that could be behind the next HIV | publisher = The Independent | work = Health News - Health & Families | author = Williams E | quote = 25 people in Bakaklion, Cameroon killed due to eating of ape }}</ref>]] |
|||
[[File:Bushmeat - Buschfleisch Ghana.JPG|thumb|[[Bushmeat]] having been smoked in [[Ghana]]. In Africa, wild animals including fruit bats are hunted for food and are referred to as bushmeat.<ref name="CDC2014Bush">{{Cite web |date=12 October 2014 |title=Risk of Exposure |url=https://www.cdc.gov/vhf/ebola/exposure/index.html |url-status=live |archive-url=https://web.archive.org/web/20141016205158/https://www.cdc.gov/vhf/ebola/exposure/index.html |archive-date=16 October 2014 |access-date=18 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref><ref>{{Cite web |date=21 July 2014 |title=FAO warns of fruit bat risk in West African Ebola epidemic |url=http://www.fao.org/news/story/en/item/239123/icode/ |url-status=live |archive-url=https://web.archive.org/web/20141013151812/http://www.fao.org/news/story/en/item/239123/icode/ |archive-date=13 October 2014 |access-date=22 October 2014 |website=fao.org}}</ref> In equatorial Africa, human consumption of bushmeat has been linked to animal-to-human transmission of diseases, including Ebola.<ref name="urlAfrican monkey meat that could be behind the next HIV – Health News – Health & Families – The Independent">{{Cite news | vauthors = Williams E |title=African monkey meat that could be behind the next HIV |work=[[The Independent]] |url=https://www.independent.co.uk/life-style/health-and-families/health-news/african-monkey-meat-that-could-be-behind-the-next-hiv-7786152.html |url-status=live |archive-url=https://web.archive.org/web/20170622133307/http://www.independent.co.uk/life-style/health-and-families/health-news/african-monkey-meat-that-could-be-behind-the-next-hiv-7786152.html |archive-date=22 June 2017 |quote=25 people in Bakaklion, Cameroon killed due to eating of ape }}</ref>]] |
|||
Although it is not entirely clear how Ebola initially spreads from animals to humans, the spread is believed to involve direct contact with an infected wild animal or fruit bat.<ref name=CDC2014T/> Besides bats, other wild animals that are sometimes infected with EBOV include several species of monkeys such as [[baboon]]s, [[great apes]] ([[chimpanzee]]s and [[gorilla]]s), and [[duikers]] (a species of [[antelope]]).<ref name="urlEbolavirus – Pathogen Safety Data Sheets">{{Cite web |date=17 September 2001 |title=Ebolavirus – Pathogen Safety Data Sheets |url=http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/ebola-eng.php |url-status=live |archive-url=https://web.archive.org/web/20140820211755/http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/ebola-eng.php |archive-date=20 August 2014 |access-date=22 August 2014 |publisher=Public Health Agency of Canada }}</ref> |
|||
[[Bat]]s are considered the most likely [[natural reservoir]] of the Ebola virus (EBOV); plants, [[arthropod]]s, and birds have also been considered.<ref>{{Cite news|title=Fruit bats may carry Ebola virus |url=http://news.bbc.co.uk/2/hi/health/4484494.stm|work=BBC News|date=2005-12-11|accessdate=2008-02-25}}</ref> Bats were known to reside in the cotton factory in which the [[index case|first case]]s for the 1976 and 1979 outbreaks were employed, and they have also been implicated in [[Marburg virus]] infections in 1975 and 1980.<ref name="Pourrut2005" /> Of 24 plant species and 19 vertebrate species experimentally inoculated with EBOV, only bats became infected.<ref>{{cite journal | author = Swanepoel R, Leman PA, Burt FJ, Zachariades NA, Braack LE, Ksiazek TG, Rollin PE, Zaki SR, Peters CJ | title = Experimental inoculation of plants and animals with Ebola virus | journal = Emerging Infectious Diseases | volume = 2 | issue = 4 | pages = 321–325 | date = Oct 1996 | pmid = 8969248 | pmc = 2639914 | doi = 10.3201/eid0204.960407 | issn = 1080-6040 }}</ref> The absence of clinical signs in these bats is characteristic of a reservoir species. In a 2002–2003 survey of 1,030 animals including 679 bats from [[Gabon]] and the [[Republic of the Congo]], 13 fruit bats were found to contain EBOV RNA fragments.<ref>{{cite journal | author = Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, Yaba P, Délicat A, Paweska JT, Gonzalez JP, Swanepoel R | title = Fruit bats as reservoirs of Ebola virus | journal = Nature | volume = 438 | issue = 7068 | pages = 575–576 | year = 2005 | pmid = 16319873 | doi = 10.1038/438575a | bibcode = 2005Natur.438..575L }}</ref> As of 2005, three types of [[fruit bat]]s (''[[Hypsignathus monstrosus]]'', ''[[Epomops franqueti]]'', and ''[[Myonycteris torquata]]'') have been identified as being in contact with EBOV. They are now suspected to represent the EBOV reservoir hosts.<ref>{{cite journal | author = Pourrut X, Délicat A, Rollin PE, Ksiazek TG, Gonzalez JP, Leroy EM | title = Spatial and temporal patterns of Zaire ebolavirus antibody prevalence in the possible reservoir bat species | journal = The Journal of infectious diseases | volume = Suppl 2 | issue = s2 | pages = S176–S183 | year = 2007 | pmid = 17940947 | doi = 10.1086/520541 }}</ref><ref name = Times>Starkey, Jerome (5 April 2014) [http://www.thetimes.co.uk/tto/news/world/africa/article4054794.ece 90 killed as fruit bats spread Ebola virus across West Africa] The Times (subscription may be needed), Retrieved 5 April 2014</ref> Antibodies against Ebola Zaire and [[Reston virus]]es have been found in [[Megabat|fruit bats]] in [[Bangladesh]], thus identifying potential virus hosts and signs of the filoviruses in Asia.<ref name="pmid23343532">{{cite journal | author = Olival KJ, Islam A, Yu M, Anthony SJ, Epstein JH, Khan SA, Khan SU, Crameri G, Wang LF, Lipkin WI, Luby SP, Daszak P | title = Ebola virus antibodies in fruit bats, bangladesh | journal = Emerging Infect. Dis. | volume = 19 | issue = 2 | pages = 270–3 | year = 2013 | pmid = 23343532 | pmc = 3559038 | doi = 10.3201/eid1902.120524 }}</ref> |
|||
Animals may become infected when they eat fruit partially eaten by bats carrying the virus.<ref name=Gon2007/> Fruit production, animal behavior and other factors may trigger outbreaks among animal populations.<ref name="Gon2007">{{Cite book |title=Wildlife and Emerging Zoonotic Diseases: The Biology, Circumstances and Consequences of Cross-Species Transmission |vauthors=Gonzalez JP, Pourrut X, Leroy E |work=Current Topics in Microbiology and Immunology |year=2007 |isbn=978-3540709619 |series=Ebolavirus and other filoviruses |volume=315 |pages=363–387 |chapter=Ebolavirus and Other Filoviruses |doi=10.1007/978-3-540-70962-6_15 |pmc=7121322 |pmid=17848072}}</ref> |
|||
Between 1976 and 1998, in 30,000 mammals, birds, reptiles, amphibians, and [[arthropod]]s sampled from outbreak regions, no ''ebolavirus'' was detected apart from some genetic traces found in six rodents (''[[Mus setulosus]]'' and ''[[Praomys]]'') and one [[shrew]] (''[[Sylvisorex ollula]]'') collected from the [[Central African Republic]].<ref name="Pourrut2005">{{cite journal | author = Pourrut X, Kumulungui B, Wittmann T, Moussavou G, Délicat A, Yaba P, Nkoghe D, Gonzalez JP, Leroy EM | title = The natural history of Ebola virus in Africa | journal = Microbes and infection / Institut Pasteur | volume = 7 | issue = 7–8 | pages = 1005–1014 | year = 2005 | pmid = 16002313 | doi = 10.1016/j.micinf.2005.04.006 }}</ref><ref name="Morvan1999">{{cite journal | author = Morvan JM, Deubel V, Gounon P, Nakouné E, Barrière P, Murri S, Perpète O, Selekon B, Coudrier D, Gautier-Hion A, Colyn M, Volehkov V | title = Identification of Ebola virus sequences present as RNA or DNA in organs of terrestrial small mammals of the Central African Republic | journal = Microbes and Infection | volume = 1 | issue = 14 | pages = 1193–1201 | year = 1999 | pmid = 10580275 | doi = 10.1016/S1286-4579(99)00242-7 }}</ref> Traces of EBOV were detected in the carcasses of [[gorilla]]s and chimpanzees during outbreaks in 2001 and 2003, which later became the source of human infections. However, the high lethality from infection in these species makes them unlikely as a [[natural reservoir]].<ref name="Pourrut2005" /> |
|||
Evidence indicates that both domestic dogs and pigs can also be infected with EBOV.<ref name="Weingartl_2013">{{Cite book |title=Vaccines and Diagnostics for Transboundary Animal Diseases |vauthors=Weingartl HM, Nfon C, Kobinger G |chapter=Review of Ebola Virus Infections in Domestic Animals |date=May 2013 |work=Dev Biol |isbn=978-3318023657 |series=Developments in Biologicals |volume=135 |pages=211–218 |doi=10.1159/000178495 |pmid=23689899 |author-link3=Gary Kobinger}}</ref> Dogs do not appear to develop symptoms when they carry the virus, and pigs appear to be able to transmit the virus to at least some primates.<ref name="Weingartl_2013" /> Although some dogs in an area in which a human outbreak occurred had antibodies to EBOV, it is unclear whether they played a role in spreading the disease to people.<ref name="Weingartl_2013" /> |
|||
Transmission between natural reservoir and humans is rare, and outbreaks are usually traceable to a single case where an individual has handled the carcass of gorilla, chimpanzee, or duiker.<ref>{{cite journal | author = Peterson AT, Bauer JT, Mills JN | title = Ecologic and Geographic Distribution of Filovirus Disease | journal = Emerging Infectious Diseases | volume = 10 | issue = 1 | pages = 40–47 | year = 2004 | pmid = 15078595 | pmc = 3322747 | doi = 10.3201/eid1001.030125 }}</ref> Fruit bats are also eaten by people in parts of West Africa where they are smoked, grilled or made into a spicy soup.<ref name = Times/><ref>http://www.bbc.co.uk/news/world-africa-26735118</ref> |
|||
=== |
===Reservoir=== |
||
The [[natural reservoir]] for Ebola has yet to be confirmed; however, [[bat]]s are considered to be the most likely candidate.<ref name="Chowell2014">{{Cite journal |vauthors=Chowell G, Nishiura H |date=October 2014 |title=Transmission dynamics and control of Ebola virus disease (EVD): a review |journal=BMC Med |volume=12 |issue=1 |page=196 |doi=10.1186/s12916-014-0196-0 |pmc=4207625 |pmid=25300956 |doi-access=free }}</ref> Three types of fruit bats (''[[Hypsignathus monstrosus]]'', ''[[Epomops franqueti]]'' and ''[[Myonycteris torquata]]'') were found to possibly carry the virus without getting sick.<ref>{{Cite journal |vauthors=Laupland KB, Valiquette L |date=May 2014 |title=Ebola virus disease |journal=Can J Infect Dis Med Microbiol |volume=25 |issue=3 |pages=128–129 |doi=10.1155/2014/527378 |pmc=4173971 |pmid=25285105 |doi-access=free}}</ref> {{As of|2013}}, whether other animals are involved in its spread is not known.<ref name="Weingartl_2013" /> Plants, [[arthropod]]s, [[rodent]]s, and birds have also been considered possible viral reservoirs.<ref name=WHO2014/><ref name="Sharma2015" /> |
|||
{{Main| Ebola virus}} |
|||
====Genome==== |
|||
[[File:Ebola virus virion.jpg|thumb|Electron [[micrograph]] of an Ebola virus [[virion]]]] |
|||
Like all [[Mononegavirales|mononegaviruses]], ebolavirions contain linear nonsegmented, single-strand, non-infectious [[RNA]] [[genome]]s of negative polarity that possesses inverse-complementary 3' and 5' termini, do not possess a [[5' cap]], are not [[Polyadenylation|polyadenylated]], and are not [[Covalent bond|covalently]] linked to a [[protein]].<ref name=Fauquet2005>{{Cite book | last1 = Pringle | first1 = C. R. | chapter = Order Mononegavirales | year = 2005 | editor-last = Fauquet | editor-first = C. M. | editor2-last = Mayo | editor2-first = M. A. | editor3-last = Maniloff | editor3-first = J. | editor4-last = Desselberger | editor4-first = U. | editor5-last = Ball | editor5-first = L. A. | title = Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses | pages = 609–614 | publisher = Elsevier/Academic Press | location = San Diego, US | isbn = 0-12-370200-3 | ref = harv | postscript = <!-- Bot-inserted parameter. Either remove it or change its value to "." for the cite to end in a ".", as necessary. -->{{inconsistent citations}} }}</ref> Ebolavirus genomes are approximately 19 [[Base_pair#Length_measurements|kilobase pairs]] long and contain seven [[gene]]s in the order [[Three prime untranslated region|3'-UTR]]-''NP''-''VP35''-''VP40''-''GP''-''VP30''-''VP24''-''L''-[[Five prime untranslated region|5'-UTR]].<ref name = Kiley1982>{{cite journal | author = Kiley MP, Bowen ET, Eddy GA, Isaäcson M, Johnson KM, McCormick JB, Murphy FA, Pattyn SR, Peters D, Prozesky OW, Regnery RL, Simpson DI, Slenczka W, Sureau P, van der Groen G, Webb PA, Wulff H | title = Filoviridae: A taxonomic home for Marburg and Ebola viruses? | journal = Intervirology | volume = 18 | issue = 1–2 | pages = 24–32 | year = 1982 | pmid = 7118520 | doi = 10.1159/000149300 }}</ref> The genomes of the five different ebolaviruses (BDBV, EBOV, RESTV, SUDV, and TAFV) differ in [[nucleic acid sequence|sequence]] and the number and location of gene overlaps. |
|||
Bats were known to roost in the cotton factory in which the [[index case|first case]]s of the 1976 and 1979 outbreaks were observed, and they have also been implicated in Marburg virus infections in 1975 and 1980.<ref name="Pourrut2005" /> Of 24 plant and 19 vertebrate species experimentally inoculated with EBOV, only bats became infected.<ref>{{Cite journal |display-authors=6 |vauthors=Swanepoel R, Leman PA, Burt FJ, Zachariades NA, Braack LE, Ksiazek TG, Rollin PE, Zaki SR, Peters CJ |date=October 1996 |title=Experimental inoculation of plants and animals with Ebola virus |journal=Emerg. Infect. Dis. |volume=2 |issue=4 |pages=321–325 |doi=10.3201/eid0204.960407 |issn=1080-6040 |pmc=2639914 |pmid=8969248}}</ref> The bats displayed no clinical signs of disease, which is considered evidence that these bats are a reservoir species of EBOV. In a 2002–2003 survey of 1,030 animals including 679 bats from [[Gabon]] and the [[Republic of the Congo]], immunoglobulin G (IgG) immune defense molecules indicative of Ebola infection were found in three bat species; at various periods of study, between 2.2 and 22.6% of bats were found to contain both RNA sequences and IgG molecules indicating Ebola infection.<ref>{{Cite journal |display-authors=6 |vauthors=Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, Yaba P, Délicat A, Paweska JT, Gonzalez JP, Swanepoel R |date=December 2005 |title=Fruit bats as reservoirs of Ebola virus |journal=Nature |volume=438 |issue=7068 |pages=575–576 |bibcode=2005Natur.438..575L |doi=10.1038/438575a |pmid=16319873 |s2cid=4403209}}</ref> Antibodies against Zaire and Reston viruses have been found in fruit bats in [[Bangladesh]], suggesting that these bats are also potential hosts of the virus and that the filoviruses are present in Asia.<ref name="Olival2013">{{Cite journal |display-authors=6 |vauthors=Olival KJ, Islam A, Yu M, Anthony SJ, Epstein JH, Khan SA, Khan SU, Crameri G, Wang LF, Lipkin WI, Luby SP, Daszak P |date=February 2013 |title=Ebola virus antibodies in fruit bats, Bangladesh |journal=Emerg. Infect. Dis. |volume=19 |issue=2 |pages=270–273 |doi=10.3201/eid1902.120524 |pmc=3559038 |pmid=23343532}}</ref> |
|||
====Structure==== |
|||
Like all [[Filoviridae|filoviruses]], ebolavirions are filamentous particles that may appear in the shape of a shepherd's crook or in the shape of a "U" or a "6", and they may be coiled, toroid, or branched.<ref name = Kiley1982/> In general, ebolavirions are 80 nm in width, but vary somewhat in length. In general, the median particle length of ebolaviruses ranges from 974 to 1,086 nm (in contrast to marburgvirions, whose median particle length was measured at 795–828 nm), but particles as long as 14,000 nm have been detected in tissue culture.<ref name=Geisbert1995>{{cite journal | author = Geisbert TW, Jahrling PB | title = Differentiation of filoviruses by electron microscopy | journal = Virus research | volume = 39 | issue = 2–3 | pages = 129–150 | year = 1995 | pmid = 8837880 }}</ref> |
|||
Between 1976 and 1998, in 30,000 mammals, birds, reptiles, amphibians and [[arthropod]]s sampled from regions of EBOV outbreaks, no Ebola virus was detected apart from some genetic traces found in six rodents (belonging to the species ''[[Mus setulosus]]'' and ''[[Praomys]]'') and one [[shrew]] (''[[Sylvisorex ollula]]'') collected from the [[Central African Republic]].<ref name="Pourrut2005">{{Cite journal |display-authors=6 |vauthors=Pourrut X, Kumulungui B, Wittmann T, Moussavou G, Délicat A, Yaba P, Nkoghe D, Gonzalez JP, Leroy EM |date=June 2005 |title=The natural history of Ebola virus in Africa |journal=Microbes Infect |volume=7 |issue=7–8 |pages=1005–1014 |doi=10.1016/j.micinf.2005.04.006 |pmid=16002313|doi-access=free }}</ref><ref name="Morvan1999">{{Cite journal |display-authors=6 |vauthors=Morvan JM, Deubel V, Gounon P, Nakouné E, Barrière P, Murri S, Perpète O, Selekon B, Coudrier D, Gautier-Hion A, Colyn M, Volehkov V |date=December 1999 |title=Identification of Ebola virus sequences present as RNA or DNA in organs of terrestrial small mammals of the Central African Republic |journal=Microbes and Infection |volume=1 |issue=14 |pages=1193–1201 |doi=10.1016/S1286-4579(99)00242-7 |pmid=10580275}}</ref> However, further research efforts have not confirmed rodents as a reservoir.<ref name="Groseth2007">{{Cite journal |vauthors=Groseth A, Feldmann H, Strong JE |date=September 2007 |title=The ecology of Ebola virus |journal=Trends Microbiol |volume=15 |issue=9 |pages=408–416 |doi=10.1016/j.tim.2007.08.001 |pmid=17698361}}</ref> Traces of EBOV were detected in the carcasses of gorillas and chimpanzees during outbreaks in 2001 and 2003, which later became the source of human infections. However, the high rates of death in these species resulting from EBOV infection make it unlikely that these species represent a natural reservoir for the virus.<ref name="Pourrut2005" /> |
|||
====Replication==== |
|||
The ebolavirus [[Biological life cycle|life cycle]] begins with virion attachment to specific cell-surface [[Receptor (biochemistry)|receptors]], followed by [[Lipid bilayer fusion|fusion]] of the virion envelope with cellular membranes and the concomitant release of the virus [[nucleocapsid]] into the [[cytosol]]. The viral [[RNA-dependent RNA polymerase|RNA polymerase]], encoded by the L gene, partially uncoats the nucleocapsid and [[Transcription (genetics)|transcribes]] the genes into positive-strand [[mRNA]]s, which are then [[translation (biology)|translated]] into structural and nonstructural proteins. Ebolavirus RNA polymerase (L) binds to a single [[Promoter (biology)|promoter]] located at the 3' end of the genome. Transcription either terminates after a gene or continues to the next gene downstream. This means that genes close to the 3' end of the genome are transcribed in the greatest abundance, whereas those toward the 5' end are least likely to be transcribed. The gene order is, therefore, a simple but effective form of transcriptional regulation. The most abundant protein produced is the nucleoprotein, whose concentration in the cell determines when L switches from gene transcription to genome replication. Replication results in full-length, positive-strand antigenomes that are, in turn, transcribed into negative-strand virus progeny genome copy. Newly synthesized structural proteins and genomes self-assemble and accumulate near the inside of the [[cell membrane]]. Virions [[Budding|bud]] off from the cell, gaining their envelopes from the cellular membrane they bud from. The mature progeny particles then infect other cells to repeat the cycle.<ref name=Feldmann2005>{{Cite book | last1 = Feldmann | first1 = H. | last2 = Geisbert | first2 = T. W. | last3 = Jahrling | first3 = P. B. | last4 = Klenk | first4 = H.-D. | last5 = Netesov | first5 = S. V. | last6 = Peters | first6 = C. J. | last7 = Sanchez | first7 = A. | last8 = Swanepoel | first8 = R. | last9 = Volchkov | first9 = V. E. | chapter = Family Filoviridae | year = 2005 | editor-last = Fauquet | editor-first = C. M. | editor2-last = Mayo | editor2-first = M. A. | editor3-last = Maniloff | editor3-first = J. | editor4-last = Desselberger | editor4-first = U. | editor5-last = Ball | editor5-first = L. A. | title = Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses | pages = 645–653 | publisher = Elsevier/Academic Press | location = San Diego, US | isbn = 0-12-370200-3 | display-authors = 9 | ref = harv | postscript = <!-- Bot-inserted parameter. Either remove it or change its value to "." for the cite to end in a ".", as necessary. -->{{inconsistent citations}} }}</ref> |
|||
[[Deforestation in the Democratic Republic of the Congo|Deforestation]] has been mentioned as a possible contributor to recent outbreaks, including the [[West African Ebola virus epidemic]]. Index cases of EVD have often been close to recently deforested lands.<ref>{{Cite web |date=10 April 2018 |title=Did deforestation cause the Ebola outbreak? |url=https://newint.org/features/web-exclusive/2018/04/10/deforestation-ebola-outbreak |access-date=10 July 2018 |website=New Internationalist |archive-date=26 June 2018 |archive-url=https://web.archive.org/web/20180626001604/https://newint.org/features/web-exclusive/2018/04/10/deforestation-ebola-outbreak |url-status=live }}</ref><ref>{{Cite journal |display-authors=6 |vauthors=Olivero J, Fa JE, Real R, Márquez AL, Farfán MA, Vargas JM, Gaveau D, Salim MA, Park D, Suter J, King S, Leendertz SA, Sheil D, Nasi R |date=30 October 2017 |title=Recent loss of closed forests is associated with Ebola virus disease outbreaks |journal=Scientific Reports |volume=7 |issue=1 |pages=14291 |bibcode=2017NatSR...714291O |doi=10.1038/s41598-017-14727-9 |issn=2045-2322 |pmc=5662765 |pmid=29085050}}</ref> |
|||
==Pathophysiology== |
==Pathophysiology== |
||
[[File:Ebola Pathenogensis path.svg|thumb|Pathogenesis schematic]] |
[[File:Ebola Pathenogensis path.svg|thumb|[[Pathogenesis]] schematic]] |
||
[[Endothelium|Endothelial cells]], mononuclear [[phagocytes]], and [[hepatocytes]] are the main targets of infection. After infection, a secreted glycoprotein (sGP) known as the Ebola virus glycoprotein (GP) is synthesized. Ebola replication overwhelms protein synthesis of infected cells and host immune defenses. The GP forms a [[Trimer (biochemistry)|trimeric complex]], which binds the virus to the endothelial cells lining the interior surface of blood vessels. The sGP forms a [[protein dimer|dimeric protein]] that interferes with the signaling of [[neutrophils]], a type of [[white blood cell]], which allows the virus to evade the immune system by inhibiting early steps of neutrophil activation. These white blood cells also serve as carriers to transport the virus throughout the entire body to places such as the lymph nodes, liver, lungs, and spleen.<ref name="isbn0-7910-8505-8">{{cite book |author=Smith, Tara |title=Ebola (Deadly Diseases and Epidemics) |publisher=Chelsea House Publications |location= |year=2005 |pages= |isbn=0-7910-8505-8 |oclc= |doi= |accessdate=}}</ref> |
|||
Like other [[Filoviridae|filoviruses]], EBOV replicates very efficiently in many [[List of distinct cell types in the adult human body|cells]], producing large amounts of virus in [[monocyte]]s, [[macrophage]]s, [[dendritic cell]]s and other cells including [[hepatocyte|liver cells]], [[fibroblast]]s, and [[adrenal gland|adrenal gland cells]].<ref name="Ansari2014">{{Cite journal |vauthors=Ansari AA |date=September 2014 |title=Clinical features and pathobiology of Ebolavirus infection |journal=J Autoimmun |volume=55 |pages=1–9 |doi=10.1016/j.jaut.2014.09.001 |pmid=25260583}}</ref> Viral replication triggers [[cytokine storm|high levels of inflammatory chemical signals]] and leads to a [[Sepsis|septic state]].<ref name="Tosh2014">{{Cite journal |vauthors=Tosh PK, Sampathkumar P |date=December 2014 |title=What Clinicians Should Know About the 2014 Ebola Outbreak |journal=Mayo Clin Proc |volume=89 |issue=12 |pages=1710–17 |doi=10.1016/j.mayocp.2014.10.010 |pmid=25467644 |doi-access=free}}</ref> |
|||
The presence of viral particles and cell damage resulting from budding causes the release of [[cytokines]] (to be specific, [[Tumor necrosis factor-alpha|TNF-α]], [[Interleukin 6|IL-6]], [[Interleukin 8|IL-8]], etc.), which are the signaling molecules for fever and inflammation. The [[cytopathic effect]], from infection in the endothelial cells, results in a loss of vascular integrity. This loss in vascular integrity is furthered with synthesis of GP, which reduces specific integrins responsible for cell adhesion to the inter-cellular structure, and damage to the liver, which leads to coagulopathy.<ref name="doi10.1128/JVI.77.18.9733-9737.2003">{{cite journal | author = Sullivan N, Yang ZY, Nabel GJ | title = Ebola Virus Pathogenesis: Implications for Vaccines and Therapies | journal = Journal of Virology | volume = 77 | issue = 18 | pages = 9733–9737 | year = 2003 | pmid = 12941881 | pmc = 224575 | doi = 10.1128/JVI.77.18.9733-9737.2003 | url = http://jvi.asm.org/content/77/18/9733.full.pdf | format = Free full text }}</ref> |
|||
EBOV is thought to infect humans through contact with mucous membranes or skin breaks.<ref name="Funk2014">{{Cite journal |vauthors=Funk DJ, Kumar A |date=November 2014 |title=Ebola virus disease: an update for anesthesiologists and intensivists |journal=Can J Anaesth |volume=62 |issue=1 |pages=80–91 |doi=10.1007/s12630-014-0257-z |pmc=4286619 |pmid=25373801}}</ref> After infection, [[endothelial cells]] (cells lining the inside of blood vessels), liver cells, and several types of immune cells such as [[Mononuclear phagocyte system|macrophages, monocytes]], and dendritic cells are the main targets of attack.<ref name="Funk2014" /> Following infection, immune cells carry the virus to nearby [[lymph node]]s where further reproduction of the virus takes place.<ref name="Funk2014" /> From there the virus can enter the bloodstream and [[lymphatic system]] and spread throughout the body.<ref name="Funk2014" /> Macrophages are the first cells infected with the virus, and this infection results in [[Apoptosis|programmed cell death]].<ref name="Chippaux2014" /> Other types of [[white blood cell]]s, such as [[lymphocyte]]s, also undergo programmed cell death leading to an abnormally [[lymphocytopenia|low concentration of lymphocytes]] in the blood.<ref name="Funk2014" /> This contributes to the weakened immune response seen in those infected with EBOV.<ref name="Funk2014" /> |
|||
==Diagnosis== |
|||
The [[medical history]], especially travel and work history along with exposure to wildlife are important to suspect the diagnosis of EVD. The diagnosis is confirmed by isolating the virus, detecting its RNA or proteins, or detecting [[antibodies]] against the virus in a person's blood.<!-- <ref name=CDC2014Diag/> --> Isolating the virus by [[cell culture]], detecting the viral RNA by [[polymerase chain reaction]] (PCR) and detecting proteins by [[enzyme-linked immunosorbent assay]] (ELISA) is effective early and in those who have died from the disease.<!-- <ref name=CDC2014Diag/> --> Detecting antibodies against the virus is effective late in the disease and in those who recover.<ref name=CDC2014Diag>{{cite web|title=Ebola Hemorrhagic Fever Diagnosis|url=http://www.cdc.gov/vhf/ebola/diagnosis/index.html|website=CDC|accessdate=3 August 2014|date=January 28, 2014}}</ref> |
|||
Endothelial cells may be infected within three days after exposure to the virus.<ref name="Chippaux2014" /> The breakdown of endothelial cells leading to [[blood vessel]] injury can be attributed to EBOV [[glycoprotein]]s. This damage occurs due to the synthesis of Ebola virus [[glycoprotein]] (GP), which reduces the availability of specific [[integrin]]s responsible for cell adhesion to the intercellular structure and causes liver damage, leading to [[coagulopathy|improper clotting]]. The widespread [[bleeding]] that occurs in affected people causes [[oedema|swelling]] and [[Hypovolemic shock|shock due to loss of blood volume]].<ref name="isbn0-7910-8505-8" /> The [[Disseminated intravascular coagulation|dysfunctional bleeding and clotting]] commonly seen in EVD has been attributed to increased activation of the [[Tissue factor pathway|extrinsic pathway]] of the [[coagulation cascade]] due to excessive [[tissue factor]] production by macrophages and monocytes.<ref name="Goeijenbier2014" /> |
|||
During an outbreak, virus isolation is often not feasible. The most common diagnostic methods are therefore real time PCR and ELISA detection of proteins, which can be performed in field or mobile hospitals.<ref name="pmid16267962">{{cite journal | author = Grolla A, Lucht A, Dick D, Strong JE, Feldmann H | title = Laboratory diagnosis of Ebola and Marburg hemorrhagic fever | journal = Bull Soc Pathol Exot | volume = 98 | issue = 3 | pages = 205–9 | year = 2005 | pmid = 16267962 | doi = }}</ref> Filovirions can be seen and identified in cell culture by [[electron microscopy]] due to their unique filamentous shapes, but electron microscopy cannot tell the difference between the various filoviruses despite there being some length differences.<ref name=Geisbert1995 /> |
|||
After infection, a secreted [[glycoprotein]], small soluble glycoprotein (sGP or GP) is synthesised. EBOV replication overwhelms protein synthesis of infected cells and the host immune defences. The GP forms a [[Trimer (biochemistry)|trimeric complex]], which tethers the virus to the endothelial cells. The sGP forms a [[protein dimer|dimeric protein]] that interferes with the signalling of [[neutrophils]], another type of white blood cell. This enables the virus to evade the immune system by inhibiting early steps of neutrophil activation.{{medcn|date=August 2019}} Furthermore, the virus is capable of hijacking cellular metabolism. Studies have shown that Ebola virus-like particles can reprogram metabolism in both vascular and immune cells.<ref>{{cite journal | vauthors = Tang H, Abouleila Y, Saris A, Shimizu Y, Ottenhoff TH, Mashaghi A | title = Ebola virus-like particles reprogram cellular metabolism | journal = Journal of Molecular Medicine | volume = 101 | issue = 5 | pages = 557–568 | date = May 2023 | pmid = 36959259 | pmc = 10036248 | doi = 10.1007/s00109-023-02309-4 }}</ref> |
|||
===Immune system evasion=== |
|||
Filoviral infection also interferes with proper functioning of the [[innate immune system]].<ref name="Misasi2014" /><ref name="Olejnik2011">{{Cite journal |vauthors=Olejnik J, Ryabchikova E, Corley RB, Mühlberger E |date=August 2011 |title=Intracellular events and cell fate in filovirus infection |journal=Viruses |volume=3 |issue=8 |pages=1501–31 |doi=10.3390/v3081501 |pmc=3172725 |pmid=21927676 |doi-access=free}}</ref> EBOV proteins blunt the human immune system's response to viral infections by interfering with the cells' ability to produce and respond to interferon proteins such as [[interferon-alpha]], [[interferon-beta]], and [[interferon gamma]].<ref name="Kuhl2012" /><ref name="Ramanan2011">{{Cite journal |vauthors=Ramanan P, Shabman RS, Brown CS, Amarasinghe GK, Basler CF, Leung DW |date=September 2011 |title=Filoviral immune evasion mechanisms |journal=Viruses |volume=3 |issue=9 |pages=1634–49 |doi=10.3390/v3091634 |pmc=3187693 |pmid=21994800 |doi-access=free}}</ref> |
|||
The VP24 and VP35 structural proteins of EBOV play a key role in this interference. When a cell is infected with EBOV, receptors located in the cell's [[cytosol]] (such as [[RIG-I]] and [[MDA5]]) or outside of the cytosol (such as [[Toll-like receptor 3|Toll-like receptor 3 (TLR3)]], [[Toll-like receptor 7|TLR7]], [[Toll-like receptor 8|TLR8]] and [[Toll-like receptor 9|TLR9]]) recognise [[pathogen-associated molecular pattern|infectious molecules]] associated with the virus.<ref name="Kuhl2012" /> On TLR activation, proteins including [[Interferon Regulatory Factor 3|interferon regulatory factor 3]] and [[Interferon regulatory factor-7|interferon regulatory factor 7]] trigger a signalling cascade that leads to the expression of [[type 1 interferon]]s.<ref name="Kuhl2012" /> The type 1 interferons are then released and bind to the [[IFNAR1]] and [[IFNAR2]] receptors expressed on the surface of a neighbouring cell.<ref name="Kuhl2012" /> Once interferon has bound to its receptors on the neighbouring cell, the signalling proteins [[STAT1]] and [[STAT2]] are activated and move to the [[Cell nucleus|cell's nucleus]].<ref name="Kuhl2012" /> This triggers the expression of [[Interferome|interferon-stimulated genes]], which code for proteins with antiviral properties.<ref name="Kuhl2012" /> EBOV's V24 protein blocks the production of these antiviral proteins by preventing the STAT1 signalling protein in the neighbouring cell from entering the nucleus.<ref name="Kuhl2012" /> The VP35 protein directly inhibits the production of interferon-beta.<ref name="Ramanan2011" /> By inhibiting these immune responses, EBOV may quickly spread throughout the body.<ref name="Chippaux2014" /> |
|||
==Diagnosis== |
|||
When EVD is suspected, travel, work history, and exposure to wildlife are important factors with respect to further diagnostic efforts.<ref>{{Cite web |date=5 May 2021 |title=Screening Patients {{!}} For Clinicians {{!}} Ebola Virus Disease {{!}} CDC |url=https://www.cdc.gov/vhf/ebola/clinicians/evaluating-patients/index.html |access-date=20 September 2022 |website=www.cdc.gov |language=en-us |archive-date=20 September 2022 |archive-url=https://web.archive.org/web/20220920174419/https://www.cdc.gov/vhf/ebola/clinicians/evaluating-patients/index.html |url-status=live }}</ref> |
|||
=== |
===Laboratory testing=== |
||
Possible non-specific laboratory indicators of EVD include a [[thrombocytopenia|low platelet count]]; an initially [[leucopenia|decreased white blood cell count]] followed by an [[leucocytosis|increased white blood cell count]]; elevated levels of the liver enzymes [[alanine aminotransferase]] (ALT) and [[aspartate aminotransferase]] (AST); and abnormalities in blood clotting often consistent with [[disseminated intravascular coagulation]] (DIC) such as a prolonged [[prothrombin time]], [[partial thromboplastin time]], and [[bleeding time]].<ref name="Kortepeter2011">{{Cite journal |vauthors=Kortepeter MG, Bausch DG, Bray M |date=November 2011 |title=Basic clinical and laboratory features of filoviral hemorrhagic fever |journal=J Infect Dis |volume=204 |issue=Supplement 3 |pages=S810–16 |doi=10.1093/infdis/jir299 |pmid=21987756 |doi-access=free }}</ref> Filovirions such as EBOV may be identified by their unique filamentous shapes in cell cultures examined with [[electron microscopy]].<ref name="Goldsmith2009">{{Cite journal |vauthors=Goldsmith CS, Miller SE |date=October 2009 |title=Modern uses of electron microscopy for detection of viruses |journal=Clinical Microbiology Reviews |type=Review |volume=22 |issue=4 |pages=552–63 |doi=10.1128/CMR.00027-09 |pmc=2772359 |pmid=19822888}}</ref> |
|||
[[File:Filovirus phylogenetic tree.svg|300px|thumb|[[Phylogenetic tree]] comparing the Ebolavirus and Marburgvirus. Numbers indicate percent confidence of branches.]] |
|||
The genera ''Ebolavirus'' and ''[[Marburgvirus]]'' were originally classified as the species of the now-obsolete ''Filovirus'' genus. In March 1998, the Vertebrate Virus Subcommittee proposed in the [[International Committee on Taxonomy of Viruses]] (ICTV) to change the ''Filovirus'' genus to the ''Filoviridae'' family with two specific genera: ''Ebola-like viruses'' and ''Marburg-like viruses''. This proposal was implemented in Washington, DC on April 2001 and in Paris on July 2002. In 2000, another proposal was made in Washington, D.C., to change the "-like viruses" to "-virus" resulting in today's ''Ebolavirus'' and ''Marburgvirus''.<ref>{{cite web|url=http://www.ncbi.nlm.nih.gov/ICTVdb/ICTVdB/01.025.0.02.htm|title=ICTVdB Virus Description – 01.025.0.02. Ebolavirus|accessdate=2009-06-02|last=Büchen-Osmond|first=Cornelia|date=2006-04-25|publisher=International Committee on Taxonomy of Viruses}}</ref> |
|||
The specific diagnosis of EVD is confirmed by isolating the virus, detecting its [[RNA]] or proteins, or detecting [[antibodies]] against the virus in a person's blood.<ref name=CDC2014Diag/> Isolating the virus by [[cell culture]], detecting the viral RNA by [[polymerase chain reaction]] (PCR)<ref name="Bro2016" /><ref name="Goeijenbier2014" /> and detecting proteins by [[enzyme-linked immunosorbent assay]] (ELISA) are methods best used in the early stages of the disease and also for detecting the virus in human remains.<ref name="Bro2016" /><ref name=CDC2014Diag/> Detecting antibodies against the virus is most reliable in the later stages of the disease and in those who recover.<ref name="CDC2014Diag">{{Cite web |date=28 January 2014 |title=Ebola Hemorrhagic Fever Diagnosis |url=https://www.cdc.gov/vhf/ebola/diagnosis/index.html |url-status=live |archive-url=https://web.archive.org/web/20140924150049/https://www.cdc.gov/vhf/ebola/diagnosis/index.html |archive-date=24 September 2014 |access-date=3 August 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> [[Immunoglobulin M|IgM antibodies]] are detectable two days after symptom onset and [[Immunoglobulin G|IgG antibodies]] can be detected six to 18 days after symptom onset.<ref name="Goeijenbier2014" /> During an outbreak, isolation of the virus with cell culture methods is often not feasible. In field or mobile hospitals, the most common and sensitive diagnostic methods are [[real-time PCR]] and ELISA.<ref name="Grolla2005">{{Cite journal |vauthors=Grolla A, Lucht A, Dick D, Strong JE, Feldmann H |date=September 2005 |title=Laboratory diagnosis of Ebola and Marburg hemorrhagic fever |journal=Bull Soc Pathol Exot |volume=98 |issue=3 |pages=205–09 |pmid=16267962}}</ref> In 2014, with new mobile testing facilities deployed in parts of Liberia, test results were obtained 3–5 hours after sample submission.<ref>{{Cite web |date=October 2014 |title=Liberia: New Ebola mobile lab speeds up diagnosis and improves care |url=https://www.who.int/features/2014/liberia-mobile-ebola-lab/en/ |url-status=dead |archive-url=https://web.archive.org/web/20141024235048/http://who.int/features/2014/liberia-mobile-ebola-lab/en/ |archive-date=24 October 2014 |access-date=26 October 2014 |publisher=[[World Health Organization]] (WHO)}}</ref> In 2015, a rapid antigen test which gives results in 15 minutes was approved for use by WHO.<ref name=WHO2015Test/> It is able to confirm Ebola in 92% of those affected and rule it out in 85% of those not affected.<ref name="WHO2015Test">{{Cite web |title=First Antigen Rapid Test for Ebola through Emergency Assessment and Eligible for Procurement |url=https://www.who.int/medicines/ebola-treatment/1st_antigen_RT_Ebola/en/ |url-status=dead |archive-url=https://web.archive.org/web/20150220203131/https://www.who.int/medicines/ebola-treatment/1st_antigen_RT_Ebola/en/ |archive-date=20 February 2015 |access-date=20 February 2015 |publisher=[[World Health Organization]] (WHO)}}</ref> |
|||
Rates of genetic change are 100 times slower than [[influenza A]] in humans, but on the same magnitude as those of [[hepatitis B]]. [[Molecular clock|Extrapolating backwards]] using these rates indicates that Ebolavirus and Marburgvirus diverged several thousand years ago.<ref>{{cite journal | author = Suzuki Y, Gojobori T | title = The origin and evolution of Ebola and Marburg viruses | journal = Molecular Biology and Evolution | volume = 14 | issue = 8 | pages = 800–6 | year = 1997 | pmid = 9254917 }}</ref> However, [[paleovirus]]es (genomic fossils) of [[filovirus]]es (Filoviridae) found in mammals indicate that the family itself is at least tens of millions of years old.<ref name="Cite pmid| 20569424">{{cite journal | author = Taylor DJ, Leach RW, Bruenn J | title = Filoviruses are ancient and integrated into mammalian genomes | journal = BMC Evolutionary Biology | volume = 10 | pages = 193 | year = 2010 | pmid = 20569424 | pmc = 2906475 | doi = 10.1186/1471-2148-10-193 }}</ref> [[Endogenous viral element|Fossilized viruses]] that are closely related to ebolaviruses have been found in the genome of the [[Chinese hamster]].<ref>{{cite journal | author = Taylor DJ, Dittmar K, Ballinger MJ, Bruenn JA | title = Evolutionary maintenance of filovirus-like genes in bat genomes | journal = BMC Evolutionary Biology | volume = 11 | pages = 336 | year = 2011 | pmid = 22093762 | pmc = 3229293 | doi = 10.1186/1471-2148-11-336 }}</ref> |
|||
===Differential diagnosis=== |
===Differential diagnosis=== |
||
Early symptoms of EVD may be similar to those of other diseases common in Africa, including [[malaria]] and [[dengue fever]].<ref name="Gatherer 2014" /> The symptoms are also similar to those of other viral haemorrhagic fevers such as [[Marburg virus disease]], [[Crimean–Congo haemorrhagic fever]], and [[Lassa fever]].<ref name="Harrison">{{Cite book | veditors = Longo DL, Kasper DL, Jameson JL, Fauci AS, Hauser SL, Loscalzo J |title=Harrison's Principles of Internal Medicine |publisher=McGraw-Hill |year=2011 |isbn=978-0071748896 |edition=18th |chapter=Chapter 197 }}</ref><ref name="Beeching2014">{{Cite journal |vauthors=Beeching NJ, Fenech M, Houlihan CF |date=December 2014 |title=Ebola Virus Disease |journal=BMJ |type=Review |volume=10 |issue=349 |page=g7438 |doi=10.1136/bmj.g7348 |pmc=4707720 |pmid=25497512}}</ref> |
|||
The complete [[differential diagnosis]] is extensive and requires consideration of many other infectious diseases such as [[typhoid fever]], [[shigellosis]], [[rickettsia|rickettsial diseases]], [[cholera]], [[sepsis]], [[borreliosis]], [[Verotoxin-producing Escherichia coli|EHEC enteritis]], [[leptospirosis]], [[scrub typhus]], [[plague (disease)|plague]], [[Q fever]], [[candidiasis]], [[histoplasmosis]], [[trypanosomiasis]], [[visceral]] [[leishmaniasis]], [[measles]], and [[viral hepatitis]] among others.<ref>{{Cite web |date=July 2008 |title=Viral Hemorrhagic Fever |url=https://www.sfcdcp.org/document.html?id=316 |url-status=dead |archive-url=https://web.archive.org/web/20130420174306/http://www.sfcdcp.org/document.html?id=316 |archive-date=20 April 2013 |access-date=17 August 2014 |publisher=S.F. Dept Public Health – Infectious Disease Emergencies |format=PDF}}</ref> |
|||
The symptoms of EVD are similar to those of [[Marburg virus disease]].<ref name="Harrison">{{Cite book | title=Harrison's Principles of Internal Medicine | publisher=McGraw-Hill | editor-last=Longo | editor-first=DL | editor-last2=Kasper | editor-first2=DL | editor-last3=Jameson | editor-first3=JL | editor-last4=Fauci | editor-first4=AS | editor-last5=Hauser | editor-first5=SL | editor-last6=Loscalzo | editor-first6=J | year=2012 | chapter=Chapter 197 | edition=18th | isbn=0-07-174889-X }}</ref> It can also easily be confused with many other diseases common in [[Equatorial Africa]] such as other [[viral hemorrhagic fever]]s, [[malaria|falciparum malaria]], [[typhoid fever]], [[shigellosis]], [[rickettsia|rickettsial diseases]] such as [[typhus]], [[cholera]], [[Gram-negative bacteria|gram-negative]] [[sepsis|septicemia]], [[borreliosis]] such as [[relapsing fever]] or [[Verotoxin-producing Escherichia coli|EHEC enteritis]]. Other infectious diseases that should be included in the [[differential diagnosis]] include the following: [[leptospirosis]], [[scrub typhus]], [[plague (disease)|plague]], [[Q fever]], [[candidiasis]], [[histoplasmosis]], [[trypanosomiasis]], [[visceral]] [[leishmaniasis]], hemorrhagic [[smallpox]], [[measles]], and fulminant [[viral hepatitis]].{{citation needed|date=March 2014}} Non-infectious diseases that can be confused with EVD are [[acute promyelocytic leukemia]], [[hemolytic uremic syndrome]], [[snake]] [[envenomation]], [[coagulation|clotting factor]] deficiencies/platelet disorders, [[thrombotic thrombocytopenic purpura]], [[hereditary hemorrhagic telangiectasia]], [[Kawasaki disease]], and even [[warfarin]] poisoning.<ref name=Gear1989>{{cite journal | author = Gear JH | title = Clinical aspects of African viral hemorrhagic fevers | journal = Reviews of infectious diseases | volume = 11 Suppl 4 | pages = S777–S782 | year = 1989 | pmid = 2665013 }}</ref><ref name=Gear1978>{{cite journal | author = Gear JH, Ryan J, Rossouw E | title = A consideration of the diagnosis of dangerous infectious fevers in South Africa | journal = South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde | volume = 53 | issue = 7 | pages = 235–237 | year = 1978 | pmid = 565951 }}</ref><ref name=Grolla2005>{{cite journal | author = Grolla A, Lucht A, Dick D, Strong JE, Feldmann H | title = Laboratory diagnosis of Ebola and Marburg hemorrhagic fever | journal = Bulletin de la Societe de pathologie exotique (1990) | volume = 98 | issue = 3 | pages = 205–209 | year = 2005 | pmid = 16267962 }}</ref><ref name=Bogomolov1998>{{cite journal | author = Bogomolov BP | title = Differential diagnosis of infectious diseases with hemorrhagic syndrome | journal = Terapevticheskii arkhiv | volume = 70 | issue = 4 | pages = 63–68 | year = 1998 | pmid = 9612907 }}</ref> |
|||
Non-infectious diseases that may result in symptoms similar to those of EVD include [[acute promyelocytic leukaemia]], [[haemolytic uraemic syndrome]], [[snake envenomation]], [[coagulation|clotting factor]] deficiencies/platelet disorders, [[thrombotic thrombocytopenic purpura]], [[hereditary haemorrhagic telangiectasia]], [[Kawasaki disease]], and [[warfarin]] poisoning.<ref name="Grolla2005" /><ref name="Gear1989">{{Cite journal |vauthors=Gear JH |date=May–June 1989 |title=Clinical aspects of African viral hemorrhagic fevers |journal=Rev Infect Dis |volume=11 |issue=Supplement 4 |pages=S777–82 |doi=10.1093/clinids/11.supplement_4.s777 |pmid=2665013}}</ref><ref name="Gear1978">{{Cite journal |vauthors=Gear JH, Ryan J, Rossouw E |date=February 1978 |title=A consideration of the diagnosis of dangerous infectious fevers in South Africa |journal=South African Medical Journal |volume=53 |issue=7 |pages=235–37 |pmid=565951}}</ref><ref name="Bogomolov1998">{{Cite journal |vauthors=Bogomolov BP |year=1998 |title=Differential diagnosis of infectious diseases with hemorrhagic syndrome |journal=Terapevticheskii Arkhiv |volume=70 |issue=4 |pages=63–68 |pmid=9612907}}</ref> |
|||
==Prevention== |
==Prevention== |
||
{{Main|Prevention of viral hemorrhagic fever}} |
|||
[[File:Biosafety level 4 hazmat suit.jpg|thumb|A researcher working with the Ebola virus while wearing a [[positive pressure personnel suit|BSL-4 positive pressure suit]] to avoid infection]] |
|||
===Behavioral changes=== |
|||
Ebola viruses are [[Contagious disease|contagious]], with prevention predominantly involving behavior changes, proper full body [[personal protective equipment]], and [[disinfection]]. Techniques to avoid infection involve not contacting infected blood or secretions, including from those who are dead.<ref name=CDC2014P/> This involves suspecting and diagnosing the disease early and using [[standard precautions]] for all patients in the healthcare setting.<ref name=CDC1998>{{Cite book|last=Centers for Disease Control and Prevention and World Health Organization | title = Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting | url = http://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf | format = PDF | accessdate = 2013-02-08 | year = 1998 | publisher = Centers for Disease Control and Prevention | location = Atlanta, Georgia, US }}</ref> Recommended measures when caring for those who are infected include: wearing protective clothing including: masks, gloves, gowns and goggles, equipment sterilization and isolating them.<ref name=CDC2014P/> [[Hand washing]] is important but can be difficult in areas where there is not even enough water for drinking.<ref name=Gath2014/> |
|||
===Vaccines=== |
|||
Due to lack of proper equipment and hygienic practices, large-scale epidemics have occured mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Traditional [[burial]] rituals, especially those requiring [[embalming]] of bodies, should be discouraged or modified.<ref name=CDC1998/> Airline crews who fly to areas of these areas of the world are taught to identify Ebola and are to isolate anyone who has symptoms.<ref>[http://www.webmd.com/a-to-z-guides/ebola-fever-virus-infection Ebola Virus: Symptoms, Treatment, and Prevention<!-- Bot generated title -->]</ref> |
|||
{{Main|Ebola vaccine}} |
|||
An [[Ebola vaccine]], [[rVSV-ZEBOV]], was approved in the United States in December 2019.<ref name="FDA2019Vac" /> It appears to be fully effective ten days after being given.<ref name=FDA2019Vac/> It was studied in Guinea between 2014 and 2016.<ref name=FDA2019Vac/> More than 100,000 people have been vaccinated against Ebola {{as of |2019|lc=yes}}.<ref>{{Cite news |date=3 May 2019 |title=Congo Ebola deaths surpass 1,000 as attacks on treatment centers go on |work=Reuters |url=https://www.reuters.com/article/us-health-ebola-who/congo-ebola-death-toll-to-hit-1000-new-vaccine-planned-who-idUSKCN1S9161 |access-date=8 May 2019 |archive-date=8 May 2019 |archive-url=https://web.archive.org/web/20190508094044/https://www.reuters.com/article/us-health-ebola-who/congo-ebola-death-toll-to-hit-1000-new-vaccine-planned-who-idUSKCN1S9161 |url-status=live }}</ref> The WHO reported that approximately 345,000 people were given the vaccine during the [[Kivu Ebola epidemic]] from 2018 to 2020.<ref>{{Cite web |title=Ebola virus disease: Vaccines |url=https://www.who.int/news-room/questions-and-answers/item/ebola-vaccines |access-date=29 March 2023 |website=www.who.int |language=en |archive-date=29 March 2023 |archive-url=https://web.archive.org/web/20230329030714/https://www.who.int/news-room/questions-and-answers/item/ebola-vaccines |url-status=live }}</ref> |
|||
===Quarantine=== |
|||
[[Quarantine]], also known as enforced isolation, is usually effective in decreasing spread.<ref>{{cite book|last1=Sompayrac|first1=Lauren|title=How pathogenic viruses work|date=2002|publisher=Jones and Bartlett Publishers|location=Boston|isbn=9780763720827|page=87|edition=3. print.|url=http://books.google.ca/books?id=PrOHLe35qNEC&pg=PA87}}</ref><ref>{{cite journal|last1=Alazard-Dany|first1=N|last2=Ottmann Terrangle|first2=M|last3=Volchkov|first3=V|title=[Ebola and Marburg viruses: the humans strike back].|journal=Medecine sciences : M/S|date=2006 Apr|volume=22|issue=4|pages=405-10|pmid=16597410}}</ref> Governments often quarantine areas where the disease is occurring or those who may be infected.<ref name="KnownCasesCDC">{{cite web | url = http://www.cdc.gov/vhf/ebola/ | title = Known Cases and Outbreaks of Ebola Hemorrhagic Fever | accessdate = 2008-08-02 | author = Special Pathogens Branch CDC | date = 2008-01-14 | publisher = Center for Disease Control and Prevention }}</ref> In the United States the law allows quarantine of those infected with Ebola.<ref>{{cite book|last1=Schultz|first1=edited by Kristi Koenig, Carl|title=Koenig and Schultz's disaster medicine : comprehensive principles and practices|date=2009|publisher=Cambridge University Press|location=Cambridge|isbn=9780521873673|page=209|url=http://books.google.ca/books?id=IfpOtV-FAl4C&pg=PA209}}</ref> The lack of roads and transportation may help slow the disease in Africa. During the 2014 outbreak Liberia closed schools.<ref>{{cite news|last1=Lewis1|first1=David|title=Liberia shuts schools, considers quarantine to curb Ebola|url=http://www.reuters.com/article/2014/07/30/us-health-ebola-liberia-idUSKBN0FZ22H20140730|accessdate=3 August 2014|agency=Reuters|date=Jul 30, 2014}}</ref> |
|||
=== |
===Infection control=== |
||
<!-- Caring for the infected --> |
|||
No [[vaccine]] is currently available for humans.<ref name=WHO2014/><ref name=Hoenen-2012>{{cite journal |author=Hoenen T, Groseth A, Feldmann H |title=Current ebola vaccines |journal=Expert Opinion on Biological Therapy |volume=12 |issue=7 |pages=859–72 |year=2012 |month=July |pmid=22559078 |pmc=3422127 |doi=10.1517/14712598.2012.685152 |url=http://informahealthcare.com/doi/abs/10.1517/14712598.2012.685152}}</ref><ref name=Choi-2013>{{cite journal |author=Choi JH, Croyle MA |title=Emerging targets and novel approaches to Ebola virus prophylaxis and treatment |journal=BioDrugs |volume=27 |issue=6 |pages=565–83 |year=2013 |month=December |pmid=23813435 |doi=10.1007/s40259-013-0046-1 |url=http://link.springer.com/article/10.1007/s40259-013-0046-1#page-1}}</ref> The most promising candidates are [[DNA vaccination|DNA vaccines]]<ref name="Xu1998">{{cite journal | author = Xu L, Sanchez A, Yang Z, Zaki SR, Nabel EG, Nichol ST, Nabel GJ | title = Immunization for Ebola virus infection | journal = Nature Medicine | volume = 4 | issue = 1 | pages = 37–42 | year = 1998 | pmid = 9427604 | doi = 10.1038/nm0198-037 }}</ref> or vaccines derived from [[Adenoviridae|adenoviruses]],<ref name=Sullivan2003/> [[vesicular stomatitis virus|vesicular stomatitis Indiana virus (VSIV)]]<ref name=Geisbert1-2008>{{cite journal | author = Geisbert TW, Daddario-Dicaprio KM, Geisbert JB, Reed DS, Feldmann F, Grolla A, Ströher U, Fritz EA, Hensley LE, Jones SM, Feldmann H | title = Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses | journal = Vaccine | volume = 26 | issue = 52 | pages = 6894–6900 | year = 2008 | pmid = 18930776 | pmc = 3398796 | doi = 10.1016/j.vaccine.2008.09.082 }}</ref><ref name=Geisbert2-2008>{{cite journal | author = Geisbert TW, Daddario-Dicaprio KM, Lewis MG, Geisbert JB, Grolla A, Leung A, Paragas J, Matthias L, Smith MA, Jones SM, Hensley LE, Feldmann H, Jahrling PB | title = Vesicular Stomatitis Virus-Based Ebola Vaccine is Well-Tolerated and Protects Immunocompromised Nonhuman Primates | journal = PLoS Pathogens | volume = 4 | issue = 11 | pages = e1000225 | year = 2008 | pmid = 19043556 | pmc = 2582959 | doi = 10.1371/journal.ppat.1000225 | editor1-last = Kawaoka | editor1-first = Yoshihiro }}</ref><ref name=Geisbert2009>{{cite journal | author = Geisbert TW, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, Grolla A, Feldmann H | title = Single-Injection Vaccine Protects Nonhuman Primates against Infection with Marburg Virus and Three Species of Ebola Virus | journal = Journal of Virology | volume = 83 | issue = 14 | pages = 7296–7304 | year = 2009 | pmid = 19386702 | pmc = 2704787 | doi = 10.1128/JVI.00561-09 }}</ref> or [[virus-like particle|filovirus-like particles (VLPs)]]<ref name=Warfield2007>{{cite journal | author = Warfield KL, Swenson DL, Olinger GG, Kalina WV, Aman MJ, Bavari S | title = Ebola Virus‐Like Particle–Based Vaccine Protects Nonhuman Primates against Lethal Ebola Virus Challenge | journal = The Journal of Infectious Diseases | volume = 196 | pages = S430–S437 | year = 2007 | pmid = 17940980 | doi = 10.1086/520583 }}</ref> because these candidates could protect nonhuman primates from ebolavirus-induced disease. DNA vaccines, adenovirus-based vaccines, and VSIV-based vaccines have entered clinical trials.<ref name="Oplinger"/><ref name="NIAIDVaccineDevelopment"/><ref name=Martin2006>{{cite journal | author = Martin JE, Sullivan NJ, Enama ME, Gordon IJ, Roederer M, Koup RA, Bailer RT, Chakrabarti BK, Bailey MA, Gomez PL, Andrews CA, Moodie Z, Gu L, Stein JA, Nabel GJ, Graham BS | title = A DNA Vaccine for Ebola Virus is Safe and Immunogenic in a Phase I Clinical Trial | journal = Clinical and Vaccine Immunology | volume = 13 | issue = 11 | pages = 1267–1277 | year = 2006 | pmid = 16988008 | pmc = 1656552 | doi = 10.1128/CVI.00162-06 | author17 = the VRC 204 Study Team1‡ }}</ref><ref>{{Cite journal|last=Bush|first=L|year=2005|title=Crucell and NIH sign Ebola vaccine manufacturing contract|journal=Pharmaceutical Technology|volume=29|page=28|ref=harv|}}</ref> |
|||
[[File:VHFisolation.png|thumb|upright=1.5|VHF isolation precautions poster]] |
|||
Community awareness of the benefits on survival chances of admitting cases early is important for the infected and infection control <ref name="Guiliani 2022" /> |
|||
====Caregivers==== |
|||
Vaccines have protected nonhuman primates. Immunization takes six months, which impedes the counter-epidemic use of the vaccines. Searching for a quicker onset of effectiveness, in 2003 a vaccine using an [[Adenoviridae|adenoviral]] (ADV) vector carrying the Ebola spike protein was tested on [[Crab-eating_macaque|crab-eating macaques]]. Twenty-eight days later they were challenged with the virus and remained resistant.<ref name="Sullivan2003">{{cite journal | author = Sullivan NJ, Geisbert TW, Geisbert JB, Xu L, Yang ZY, Roederer M, Koup RA, Jahrling PB, Nabel GJ | title = Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates | journal = Nature | volume = 424 | issue = 6949 | pages = 681–684 | year = 2003 | pmid = 12904795 | doi = 10.1038/nature01876 }}</ref> A vaccine based on attenuated recombinant [[vesicular stomatitis virus]] (VSV) vector carrying either the Ebola glycoprotein or the Marburg glycoprotein in 2005 protected nonhuman primates,<ref name="Jones2005">{{cite journal | author = Jones SM, Feldmann H, Ströher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volchkov VE, Fritz EA, Daddario KM, Hensley LE, Jahrling PB, Geisbert TW | title = Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses | journal = Nature Medicine | volume = 11 | issue = 7 | pages = 786–790 | year = 2005 | pmid = 15937495 | doi = 10.1038/nm1258 }}</ref> opening clinical trials in humans.<ref name="Oplinger">{{Cite book|last=Oplinger|first=Anne A.|date=2003-11-18|title=NIAID Ebola vaccine enters human trial|url=http://news.bio-medicine.org/medicine-news-2/NIAID-Ebola-vaccine-enters-human-trial-4881-1/|publisher=Bio-Medicine}}</ref> The study by October completed the first human trial, over three months giving three vaccinations safely inducing an immune response. Individuals for a year were followed, and, in 2006, a study testing a faster-acting, single-shot vaccine began; this new study was completed in 2008.<ref name="NIAIDVaccineDevelopment">{{Cite press release|title=Ebola/Marburg Vaccine Development|publisher=National Institute of Allergy and Infectious Diseases|date=2008-09-15|url=http://www3.niaid.nih.gov/topics/ebolaMarburg/default.htm}}</ref> Trying the vaccine on a strain of Ebola that more resembles the one that infects humans is the next step.{{citation needed|date=June 2012}} |
|||
[[File:Donna Wood, Nurse and NHS Ebola volunteer (15652582937).jpg|thumb|right|British woman wearing protective gear]] |
|||
People who care for those infected with Ebola should wear protective clothing including masks, gloves, gowns and goggles.<ref name=CDC2014P/> The U.S. [[Centers for Disease Control]] (CDC) recommend that the protective gear leaves no skin exposed.<ref name=Oct2014CDC/> These measures are also recommended for those who may handle objects contaminated by an infected person's body fluids.<ref name=CDCBook1998/> In 2014, the CDC began recommending that medical personnel receive training on the proper suit-up and removal of [[personal protective equipment]] (PPE); in addition, a designated person, appropriately trained in biosafety, should be watching each step of these procedures to ensure they are done correctly.<ref name="Oct2014CDC">{{Cite web |date=20 October 2014 |title=Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus Disease in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing) |url=https://www.cdc.gov/vhf/ebola/hcp/procedures-for-ppe.html |url-status=live |archive-url=https://web.archive.org/web/20141022024557/https://www.cdc.gov/vhf/ebola/hcp/procedures-for-ppe.html |archive-date=22 October 2014 |access-date=22 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> In Sierra Leone, the typical training period for the use of such safety equipment lasts approximately 12 days.<ref>{{cite web | url = https://www.telegraph.co.uk/news/worldnews/ebola/11155840/Ebola-medics-better-trained-in-Sierra-Leone-than-Spain.html | title = Ebola medics 'better trained in Sierra Leone than Spain' | archive-url = https://web.archive.org/web/20200628201158/https://www.telegraph.co.uk/news/worldnews/ebola/11155840/Ebola-medics-better-trained-in-Sierra-Leone-than-Spain.html | archive-date=28 June 2020 | work = The Telegraph | vauthors = Govan F | date = 11 October 2014 }}</ref> |
|||
On 6 December 2011, the development of a successful [[vaccine]] against Ebola for mice was reported. Unlike the predecessors, it can be [[Freeze-drying|freeze-dried]] and thus stored for long periods in wait for an outbreak.<ref name="pmid22143779">{{cite journal | author = Phoolcharoen W, Dye JM, Kilbourne J, Piensook K, Pratt WD, Arntzen CJ, Chen Q, Mason HS, Herbst-Kralovetz MM | title = A nonreplicating subunit vaccine protects mice against lethal Ebola virus challenge | journal = Proc. Natl. Acad. Sci. U.S.A. | volume = 108 | issue = 51 | pages = 20695–700 | year = 2011 | pmid = 22143779 | pmc = 3251076 | doi = 10.1073/pnas.1117715108 | bibcode = 2011PNAS..10820695P | laysummary = http://www.bbc.co.uk/news/science-environment-16011748 | laysource = BBC News }}</ref> An experimental vaccine made by researchers at Canada's national laboratory in Winnipeg was used in 2009 to pre-emptively treat a German scientist who might have been infected during a lab accident.<ref>{{cite news|title=Canadian Press|url=http://www.cbc.ca/news/technology/canadian-made-ebola-vaccine-used-after-german-lab-accident-1.827949|accessdate=2 August 2014|work=CBCNews|publisher=Canadian Broadcasting Corporation (CBC)|date=20 March 2009}}</ref> However, actual EBOV infection could never be demonstrated without a doubt.<ref>{{cite journal | author = Tuffs A | title = Experimental vaccine may have saved Hamburg scientist from Ebola fever | journal = BMJ | volume = 338 | pages = b1223 | year = 2009 | pmid = 19307268 | doi = 10.1136/bmj.b1223 }}</ref> Experimentally, recombinant [[Vesicular stomatitis virus|vesicular stomatitis Indiana virus]] (VSIV) expressing the glycoprotein of EBOV or SUDV has been used successfully in nonhuman primate models as [[post-exposure prophylaxis]].<ref>{{cite journal | author = Feldmann H, Jones SM, Daddario-DiCaprio KM, Geisbert JB, Ströher U, Grolla A, Bray M, Fritz EA, Fernando L, Feldmann F, Hensley LE, Geisbert TW | title = Effective Post-Exposure Treatment of Ebola Infection | journal = PLoS Pathogens | volume = 3 | issue = 1 | pages = e2 | year = 2007 | pmid = 17238284 | pmc = 1779298 | doi = 10.1371/journal.ppat.0030002 }}</ref><ref>{{cite journal | author = Geisbert TW, Daddario-DiCaprio KM, Williams KJ, Geisbert JB, Leung A, Feldmann F, Hensley LE, Feldmann H, Jones SM | title = Recombinant Vesicular Stomatitis Virus Vector Mediates Postexposure Protection against Sudan Ebola Hemorrhagic Fever in Nonhuman Primates | journal = Journal of Virology | volume = 82 | issue = 11 | pages = 5664–5668 | year = 2008 | pmid = 18385248 | pmc = 2395203 | doi = 10.1128/JVI.00456-08 }}</ref>{{Clarify|date=July 2014}} |
|||
In 2022 in Uganda, lighter personal protection equipment has become available as well as possibilities to monitor and communicate with patients from windows in the treatment tents until it is necessary to enter if e.g. a patient's oxygen levels drop. <ref name="Guiliani 2022" /> |
|||
====Patients and household members==== |
|||
===Laboratory=== |
|||
The infected person should be in [[Isolation (health care)|barrier-isolation]] from other people.<ref name=CDC2014P/> All equipment, medical waste, patient waste and surfaces that may have come into contact with body fluids need to be [[disinfection|disinfected]].<ref name="CDCBook1998">{{Cite book | vauthors = Peters CJ |url= https://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf |title=Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting |date=December 1998 |publisher=[[Centers for Disease Control and Prevention]] (CDC) |archive-url=https://web.archive.org/web/20170708093022/https://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf |archive-date=8 July 2017 |url-status=live}}</ref> During the 2014 outbreak, kits were put together to help families treat Ebola disease in their homes, which included protective clothing as well as [[chlorine powder]] and other cleaning supplies.<ref>{{cite web | url = https://time.com/3481394/equipping-homes-to-treat-ebola-patients/ | title = This Is How Ebola Patients Are Equipping Their Homes | archive-url = https://web.archive.org/web/20150305172616/http://time.com/3481394/equipping-homes-to-treat-ebola-patients/ | archive-date=5 March 2015 | work = Time Magazine | vauthors = Sifferlin A | url-status = live | date = 9 October 2014 }}</ref> Education of caregivers in these techniques, and providing such barrier-separation supplies has been a priority of [[Doctors Without Borders]].<ref>{{Cite news | vauthors = Sheri F, Nossiter A, Kanter J |date=10 October 2014 |title=Doctors Without Borders Evolves as It Forms the Vanguard in Ebola Fight |work=[[The New York Times]] |url=https://www.nytimes.com/2014/10/11/world/africa/doctors-without-borders-evolves-as-it-forms-the-vanguard-in-ebola-fight-.html |url-status=live |access-date=12 October 2014 |archive-url=https://web.archive.org/web/20141014172320/http://www.nytimes.com/2014/10/11/world/africa/doctors-without-borders-evolves-as-it-forms-the-vanguard-in-ebola-fight-.html |archive-date=14 October 2014}}</ref> |
|||
Ebola viruses are [[World Health Organization]] Risk Group 4 pathogens, requiring [[Biosafety level|biosafety level 4-equivalent containment]]. Laboratory researchers must be properly trained in BSL-4 practices and wear proper personal protective equipment. |
|||
====Disinfection==== |
|||
==Treatment== |
|||
<!-- Disinfecting surfaces --> |
|||
[[File:Ebola outbreak in Gulu Municipal Hospital.jpg|thumb|A hospital isolation ward in [[Gulu]], [[Uganda]], during the October 2000 outbreak]] |
|||
Ebolaviruses can be [[Sterilization (microbiology)|eliminated]] with heat (heating for 30 to 60 minutes at 60 °C or boiling for five minutes). To [[disinfectants|disinfect]] surfaces, some lipid solvents such as some alcohol-based products, detergents, sodium hypochlorite (bleach) or [[calcium hypochlorite]] (bleaching powder), and other suitable disinfectants may be used at appropriate concentrations.<ref name="urlEbolavirus – Pathogen Safety Data Sheets" /><ref name="Infection Guidance">{{Cite journal |date=August 2014 |title=Interim infection prevention and control guidance for care of patients with suspected or confirmed filovirus haemorrhagic fever in health-care settings, with focus on Ebola |publisher=[[World Health Organization]] (WHO) |id=WHO/HIS/SDS/2014.4 Rev. 1 |hdl-access=free |hdl=10665/130596 |periodical=WHO Technical Documents |last1=Organization |first1=World Health }}</ref> |
|||
No ebolavirus-specific treatment exists.<ref name=Choi-2013/> Treatment is primarily supportive in nature and includes minimizing invasive procedures, balancing fluids and [[electrolyte]]s to counter [[dehydration]], administration of [[anticoagulants]] early in infection to prevent or control [[disseminated intravascular coagulation]], administration of [[coagulation|procoagulants]] late in infection to control [[bleeding]], maintaining [[oxygen]] levels, [[pain management]], and the use of medications to treat bacterial or fungal secondary infections.<ref>{{cite journal | author = Bausch DG, Feldmann H, Geisbert TW, Bray M, Sprecher AG, Boumandouki P, Rollin PE, Roth C | title = Outbreaks of Filovirus Hemorrhagic Fever: Time to Refocus on the Patient | journal = The Journal of Infectious Diseases | volume = 196 | pages = S136–S141 | year = 2007 | pmid = 17940941 | doi = 10.1086/520542 | author9 = Winnipeg Filovirus Clinical Working Group }}</ref><ref>{{cite journal | author = Jeffs B | title = A clinical guide to viral haemorrhagic fevers: Ebola, Marburg and Lassa | journal = Tropical Doctor | volume = 36 | issue = 1 | pages = 1–4 | year = 2006 | pmid = 16483416 | doi = 10.1258/004947506775598914 }}</ref><ref>{{cite journal | author = Nkoghé D, Formenty P, Nnégué S, Mvé MT, Hypolite I, Léonard P, Leroy E | title = Practical guidelines for the management of Ebola infected patients in the field | journal = Medecine tropicale : revue du Corps de sante colonial | volume = 64 | issue = 2 | pages = 199–204 | year = 2004 | pmid = 15460155 | author8 = Comité International de Coordination Technique et Scientifique }}</ref> Early treatment may increase the chance of survival.<ref>{{cite web|url=http://www.businessweek.com/news/2014-07-29/sierra-leone-is-epicenter-of-ebola-as-guinea-clinic-shut|title=Sierra Leone Is Epicenter of Ebola as Guinea Clinic Shut|date=2014-06-08 |accessdate=2014-07-30}}</ref> A number of experimental treatment are being studied. |
|||
====General population==== |
|||
<!-- General population --> |
|||
Education of the general public about the risk factors for Ebola infection and of the protective measures individuals may take to prevent infection is recommended by the [[World Health Organization]].<ref name=WHO2014/> These measures include avoiding direct contact with infected people and regular [[hand washing]] using soap and water.<ref>{{Cite web |date=6 September 2014 |title=Ebola – 5 tips to avoid the deadly disease |url=https://plan-international.org/about-plan/resources/news/ebola-outbreak-5-tips-to-avoid-the-deadly-disease/ |url-status=live |archive-url=https://web.archive.org/web/20150324061050/http://plan-international.org/about-plan/resources/news/ebola-outbreak-5-tips-to-avoid-the-deadly-disease/ |archive-date=24 March 2015 |publisher=Plan International }}</ref> |
|||
====Bushmeat==== |
|||
<!-- Bush meat --> |
|||
[[Bushmeat]], an important source of protein in the diet of some Africans, should be handled and prepared with appropriate protective clothing and thoroughly cooked before consumption.<ref name=WHO2014/> Some research suggests that an outbreak of Ebola disease in the wild animals used for consumption may result in a corresponding human outbreak. Since 2003, such animal outbreaks have been monitored to predict and prevent Ebola outbreaks in humans.<ref name="Rouquet_2005">{{Cite journal |display-authors=6 |vauthors=Rouquet P, Froment JM, Bermejo M, Kilbourn A, Karesh W, Reed P, Kumulungui B, Yaba P, Délicat A, Rollin PE, Leroy EM |date=February 2005 |title=Wild animal mortality monitoring and human Ebola outbreaks, Gabon and Republic of Congo, 2001–2003 |journal=Emerg. Infect. Dis. |volume=11 |issue=2 |pages=283–90 |doi=10.3201/eid1102.040533 |issn=1080-6040 |pmc=3320460 |pmid=15752448 }}</ref> |
|||
====Corpses, burial==== |
|||
<!-- Dead bodies --> |
|||
If a person with Ebola disease dies, direct contact with the body should be avoided.<ref name="CDC2014P">{{Cite web |date=31 July 2014 |title=Ebola Hemorrhagic Fever Prevention |url=https://www.cdc.gov/vhf/ebola/prevention/index.html |url-status=live |archive-url=https://web.archive.org/web/20140904125431/https://www.cdc.gov/vhf/ebola/prevention/index.html |archive-date=4 September 2014 |access-date=2 August 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> Certain [[burial ritual]]s, which may have included making various direct contacts with a dead body, require reformulation so that they consistently maintain a proper protective barrier between the dead body and the living.<ref name="CDC1998">{{Cite book |last=Centers for Disease Control and Prevention and World Health Organization |url=https://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf |title=Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting |publisher=[[Centers for Disease Control and Prevention]] (CDC) |year=1998 |access-date=8 February 2013 |archive-url=https://web.archive.org/web/20140411222536/https://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf |archive-date=11 April 2014 |url-status=live }}</ref><ref name="url_www.who.int_ burial">{{Cite web |date=1 June 2014 |title=Section 7: Use Safe Burial Practices |url=https://www.who.int/csr/resources/publications/ebola/whoemcesr982sec7-9.pdf |url-status=live |archive-url=https://web.archive.org/web/20150226091100/https://www.who.int/csr/resources/publications/ebola/whoemcesr982sec7-9.pdf |archive-date=26 February 2015 |website=Information resources on Ebola virus disease |publisher=[[World Health Organization]] (WHO) }}</ref><ref>{{Cite news | vauthors = Harden B |date=24 December 2000 |title=Ebola's Shadow |work=[[The New York Times]] |url=https://archive.nytimes.com/www.nytimes.com/library/magazine/home/20001224mag-ebola.html |url-status=live |access-date=12 October 2014 |archive-url=https://web.archive.org/web/20141020200433/http://partners.nytimes.com/library/magazine/home/20001224mag-ebola.html |archive-date=20 October 2014}}</ref> Social anthropologists may help find alternatives to traditional rules for burials.<ref>{{Cite web | vauthors = Fassassi A |date=September 2014 |title=How anthropologists help medics fight Ebola in Guinea |url=http://www.scidev.net/global/cooperation/feature/anthropologists-medics-ebola-guinea.html |url-status=live |archive-url=https://web.archive.org/web/20141006112752/http://www.scidev.net/global/cooperation/feature/anthropologists-medics-ebola-guinea.html |archive-date=6 October 2014 |access-date=3 October 2014 |publisher=SciDev.Net }}</ref> |
|||
====Transport, travel, contact==== |
|||
<!-- Transportation --> |
|||
Transportation crews are instructed to follow a certain isolation procedure, should anyone exhibit symptoms resembling EVD.<ref name="urlWHO – West Africa – Ebola virus disease">{{Cite web |title=West Africa – Ebola virus disease Update: Travel and transport |url=https://www.who.int/ith/updates/20140421/en/ |url-status=dead |archive-url=https://web.archive.org/web/20140729034008/https://www.who.int/ith/updates/20140421/en/ |archive-date=29 July 2014 |website=International travel and health |publisher=[[World Health Organization]] (WHO) }}</ref> {{As of|August 2014}}, the WHO does not consider travel bans to be useful in decreasing spread of the disease.<ref name=WHO2014T/> In October 2014, the CDC defined four risk levels used to determine the level of 21-day monitoring for symptoms and restrictions on public activities.<ref name="CDC_monitor_movement">{{Cite web |date=27 October 2014 |title=Monitoring Symptoms and Controlling Movement to Stop Spread of Ebola |url=https://www.cdc.gov/media/releases/2014/fs1027-monitoring-symptoms-controlling-movement.html |url-status=live |archive-url=https://web.archive.org/web/20170708091445/https://www.cdc.gov/media/releases/2014/fs1027-monitoring-symptoms-controlling-movement.html |archive-date=8 July 2017 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> In the United States, the CDC recommends that restrictions on public activity, including travel restrictions, are not required for the following defined risk levels:<ref name=CDC_monitor_movement/> |
|||
* having been in a country with widespread Ebola disease transmission and having no known exposure (low risk); or having been in that country more than 21 days ago (no risk) |
|||
* encounter with a person showing symptoms; but not within three feet of the person with Ebola without wearing PPE; and no direct contact with body fluids |
|||
* having had brief skin contact with a person showing symptoms of Ebola disease when the person was believed to be not very contagious (low risk) |
|||
* in countries without widespread Ebola disease transmission: direct contact with a person showing symptoms of the disease while wearing PPE (low risk) |
|||
* contact with a person with Ebola disease before the person was showing symptoms (no risk). |
|||
The CDC recommends monitoring for the symptoms of Ebola disease for those both at "low risk" and at higher risk.<ref name=CDC_monitor_movement/> |
|||
====Laboratory==== |
|||
<!-- Laboratory --> |
|||
In laboratories where diagnostic testing is carried out, [[Biosafety level|biosafety level 4-equivalent containment]] is required.<ref name="OSHA">{{Cite web |title=Ebola: Control and Prevention |url=https://www.osha.gov/SLTC/ebola/control_prevention.html |url-status=live |archive-url=https://web.archive.org/web/20141109145135/https://www.osha.gov/SLTC/ebola/control_prevention.html |archive-date=9 November 2014 |access-date=9 November 2014 |publisher=[[Occupational Safety and Health Administration]] (OSHA) }}</ref> Laboratory researchers must be properly trained in BSL-4 practices and wear proper PPE.<ref name=OSHA/> |
|||
===Isolation=== |
|||
Isolation refers to separating those who are sick from those who are not. [[Quarantine]] refers to separating those who may have been exposed to a disease until they either show signs of the disease or are no longer at risk.<ref>{{Cite web |date=28 August 2014 |title=About Quarantine and Isolation |url=https://www.cdc.gov/quarantine/quarantineisolation.html |url-status=live |archive-url=https://web.archive.org/web/20141020041517/https://www.cdc.gov/quarantine/quarantineisolation.html |archive-date=20 October 2014 |access-date=26 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> Quarantine, also known as enforced isolation, is usually effective in decreasing spread.<ref>{{Cite book | vauthors = Sompayrac L |url=https://archive.org/details/howpathogenicvir0000somp |title=How pathogenic viruses work |date=2002 |publisher=Jones and Bartlett Publishers |isbn=978-0763720827 |edition=3rd |location=Boston |page=[https://archive.org/details/howpathogenicvir0000somp/page/87 87] |url-access=registration}}</ref><ref name="pmid16597410">{{Cite journal |vauthors=Alazard-Dany N, Ottmann Terrangle M, Volchkov V |date=April 2006 |title=[Ebola and Marburg viruses: the humans strike back] |url=https://www.medecinesciences.org/articles/medsci/pdf/2006/05/medsci2006224p405.pdf |journal=Med Sci (Paris) |language=fr |volume=22 |issue=4 |pages=405–10 |doi=10.1051/medsci/2006224405 |pmid=16597410 |doi-access=free |access-date=20 August 2019 |archive-date=22 February 2020 |archive-url=https://web.archive.org/web/20200222201753/https://www.medecinesciences.org/articles/medsci/pdf/2006/05/medsci2006224p405.pdf |url-status=live }}</ref> Governments often quarantine areas where the disease is occurring or individuals who may transmit the disease outside of an initial area.<ref>{{Cite web |date=19 August 2014 |title=Ebola virus disease update – west Africa |url=https://www.who.int/csr/don/2014_08_19_ebola/en/ |url-status=dead |archive-url=https://web.archive.org/web/20141022110953/https://www.who.int/csr/don/2014_08_19_ebola/en/ |archive-date=22 October 2014 |access-date=26 October 2014 |publisher=[[World Health Organization]] (WHO)}}</ref> In the United States, the law allows quarantine of those infected with ebolaviruses.<ref>{{Cite book |url=https://books.google.com/books?id=IfpOtV-FAl4C&pg=PA209 |title=Koenig and Schultz's disaster medicine : comprehensive principles and practices |date=2009 |publisher=Cambridge University Press |isbn=978-0521873673 | veditors = Koenig K, Schultz C |location=Cambridge |page=209 |archive-url=https://web.archive.org/web/20160515175653/https://books.google.com/books?id=IfpOtV-FAl4C&pg=PA209 |archive-date=15 May 2016 |url-status=live}}</ref><ref>{{Cite web |date=19 January 2017 |title=Control of Communicable Diseases |url=https://www.federalregister.gov/documents/2017/01/19/2017-00615/control-of-communicable-diseases |access-date=13 August 2019 |website=[[Federal Register]] |archive-date=6 August 2019 |archive-url=https://web.archive.org/web/20190806212142/https://www.federalregister.gov/documents/2017/01/19/2017-00615/control-of-communicable-diseases |url-status=live }}</ref> |
|||
===Contact tracing=== |
|||
[[Contact tracing]] is considered important to contain an outbreak. It involves finding everyone who had close contact with infected individuals and monitoring them for signs of illness for 21 days. If any of these contacts comes down with the disease, they should be isolated, tested and treated. Then the process is repeated, tracing the contacts' contacts.<ref>{{Cite journal |vauthors=Frieden TR, Damon I, Bell BP, Kenyon T, Nichol S |date=25 September 2014 |title=Ebola 2014 – New Challenges, New Global Response and Responsibility |journal=New England Journal of Medicine |volume=371 |issue=13 |pages=1177–1180 |doi=10.1056/NEJMp1409903 |pmid=25140858|doi-access=free }}</ref><ref>{{Cite web |title=What is Contact Tracing? |url=https://www.cdc.gov/vhf/ebola/pdf/contact-tracing.pdf |url-status=live |archive-url=https://web.archive.org/web/20140912114723/https://www.cdc.gov/vhf/ebola/pdf/contact-tracing.pdf |archive-date=12 September 2014 |access-date=15 September 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> |
|||
{{anchor|Treatment}} |
|||
==Management== |
|||
{{as of |2019}} two treatments ([[atoltivimab/maftivimab/odesivimab]] and [[ansuvimab]]) are associated with improved outcomes.<ref name="NIH2019" /><ref name=NIH2019Tx/> The U.S. [[Food and Drug Administration]] (FDA) advises people to be careful of advertisements making unverified or fraudulent claims of benefits supposedly gained from various anti-Ebola products.<ref name="FDA2014R">{{Cite press release |title=FDA warns consumers about fraudulent Ebola treatment products |url=https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm410086.htm |access-date=20 August 2014 |url-status=dead |archive-url=https://wayback.archive-it.org/7993/20170111194035/https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm410086.htm |archive-date=11 January 2017}}</ref><ref>{{Cite web |date=22 September 2014 |title=Natural Solutions Foundation Warning Letter |url=https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/warning-letters/natural-solutions-foundation-09222014 |url-status=live |archive-url=https://web.archive.org/web/20141008213137/https://www.fda.gov/ICECI/EnforcementActions/WarningLetters/2014/ucm416051.htm |archive-date=8 October 2014 |access-date=9 October 2014 |publisher=U.S. [[Food and Drug Administration]] (FDA)}}</ref> |
|||
In October 2020, the U.S. [[Food and Drug Administration]] (FDA) approved atoltivimab/maftivimab/odesivimab with an [[Indication (medicine)|indication]] for the treatment of infection caused by ''Zaire ebolavirus''.<ref name="FDA PR">{{Cite press release |title=FDA Approves First Treatment for Ebola Virus |date=14 October 2020 |url=https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-ebola-virus |access-date=14 October 2020 |website=U.S. [[Food and Drug Administration]] (FDA) |archive-date=15 October 2020 |archive-url=https://web.archive.org/web/20201015021206/https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-ebola-virus |url-status=live }} {{PD-notice}}</ref> |
|||
===Standard support=== |
|||
[[File:Ebola outbreak in Gulu Municipal Hospital.jpg|thumb|A hospital isolation ward in [[Gulu|Gulu, Uganda]], during the October 2000 outbreak]] |
|||
Treatment is primarily [[Palliative care|supportive]] in nature.<ref name="Clark_2012">{{Cite journal |vauthors=Clark DV, Jahrling PB, Lawler JV |date=September 2012 |title=Clinical management of filovirus-infected patients |journal=Viruses |volume=4 |issue=9 |pages=1668–86 |doi=10.3390/v4091668 |pmc=3499825 |pmid=23170178 |doi-access=free}}</ref> Early supportive care with rehydration and symptomatic treatment improves survival.<ref name=WHO2014/> Rehydration may be via the [[Oral rehydration therapy|oral]] or [[Intravenous therapy|intravenous]] route.<ref name=Clark_2012/> These measures may include [[pain management]], and treatment for [[antiemetic|nausea]], [[antipyretic|fever]], and [[anxiolytic|anxiety]].<ref name=Clark_2012/> The [[World Health Organization]] (WHO) recommends avoiding [[aspirin]] or [[ibuprofen]] for pain management, due to the risk of bleeding associated with these medications.<ref>{{Cite web |title=Ebola messages for the general public |url=https://www.who.int/csr/disease/ebola/messages/en/ |url-status=dead |archive-url=https://web.archive.org/web/20141025120028/https://www.who.int/csr/disease/ebola/messages/en/ |archive-date=25 October 2014 |access-date=26 October 2014 |publisher=[[World Health Organization]] (WHO)}}</ref> |
|||
Blood products such as [[packed red blood cells]], [[platelet]]s, or [[fresh frozen plasma]] may also be used.<ref name=Clark_2012/> Other regulators of coagulation have also been tried including [[heparin]] in an effort to prevent [[disseminated intravascular coagulation]] and [[Coagulation factors|clotting factors]] to decrease bleeding.<ref name=Clark_2012/> [[Antimalarial medication]]s and [[antibiotics]] are often used before the diagnosis is confirmed,<ref name=Clark_2012/> though there is no evidence to suggest such treatment helps. Several [[Ebola virus disease treatment research|experimental treatments are being studied]].<ref name=":4">{{Cite web |title=Ebola virus disease |url=https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease |access-date=28 May 2020 |website=www.who.int |language=en |archive-date=16 February 2021 |archive-url=https://web.archive.org/web/20210216200615/https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease |url-status=live }}</ref> |
|||
Where hospital care is not possible, the WHO's guidelines for home care have been relatively successful. Recommendations include using towels soaked in a bleach solution when moving infected people or bodies and also applying bleach on stains. It is also recommended that the caregivers wash hands with bleach solutions and cover their mouth and nose with a cloth.<ref>{{Cite web |title=Annex 18. Transmission risk reduction of filoviruses in home-care settings |url=https://www.who.int/csr/disease/ebola/Annex_18_risk_reduction_home_care.pdf?ua=1 |url-status=live |archive-url=https://web.archive.org/web/20141026092619/https://www.who.int/csr/disease/ebola/Annex_18_risk_reduction_home_care.pdf?ua=1 |archive-date=26 October 2014 |access-date=26 October 2014 |publisher=[[World Health Organization]] (WHO)}}</ref> |
|||
===Intensive care=== |
|||
[[Intensive care]] is often used in the developed world.<ref name="Feldmann2011" /> This may include maintaining blood volume and electrolytes (salts) balance as well as treating any bacterial infections that may develop.<ref name="Feldmann2011">{{Cite journal |vauthors=Feldmann H, Geisbert TW |date=March 2011 |title=Ebola haemorrhagic fever |journal=Lancet |volume=377 |issue=9768 |pages=849–62 |doi=10.1016/S0140-6736(10)60667-8 |pmc=3406178 |pmid=21084112}}</ref> [[Haemodialysis|Dialysis]] may be needed for [[kidney failure]], and [[extracorporeal membrane oxygenation]] may be used for lung dysfunction.<ref name="Feldmann2011" /> |
|||
==Prognosis== |
==Prognosis== |
||
EVD has a [[case fatality rate|risk of death in those infected]] of between 25% and 90%.<ref name=WHO2014/><ref name="Elsevier/Academic Press">{{Cite book | vauthors = Fauquet CM |url=https://books.google.com/books?id=9Wy7Jgy5RWYC&pg=PA648 |title=Virus taxonomy classification and nomenclature of viruses; 8th report of the International Committee on Taxonomy of Viruses |date=2005 |publisher=Elsevier/Academic Press |isbn=978-0080575483 |location=Oxford |page=648 |archive-url=https://web.archive.org/web/20160604013646/https://books.google.com/books?id=9Wy7Jgy5RWYC&pg=PA648 |archive-date=4 June 2016 |url-status=live}}</ref> {{As of|September 2014}}, the average risk of death among those infected is 50%.<ref name="WHO2014" /> The highest risk of death was 90% in the 2002–2003 [[Republic of the Congo]] outbreak.<ref>{{Cite web |title=More or Less behind the stats Ebola |url=http://www.bbc.co.uk/programmes/p0244jdt |url-status=live |archive-url=https://web.archive.org/web/20140903044359/http://www.bbc.co.uk/programmes/p0244jdt |archive-date=3 September 2014 |access-date=8 October 2014 |publisher=BBC World Service}}</ref> |
|||
The disease has a high mortality rate: often between 50 percent and 90 percent.<ref name=WHO2014/><ref name="Elsevier/Academic Press"/> If an infected person survives, recovery may be quick and complete. Prolonged cases are often complicated by the occurrence of long term problems, such as [[orchitis|inflammation of the testicles]], [[arthralgia|joint pains]], [[myalgia|muscle pains]], [[desquamation|skin peeling]], or [[alopecia|hair loss]]. Eye symptoms, such as [[photophobia|light sensitivity]], [[hyperlacrimation|excess tearing]], [[iritis]], [[iridocyclitis]], [[choroiditis]] and [[blindness]] have also been described. EBOV and SUDV may be able to persist in the [[semen]] of some survivors for up to seven weeks, which could give rise to infections and disease via [[sexual intercourse]].<ref name=WHO2014/> |
|||
Early admission significantly increases survival rates <ref name="Guiliani 2022" /> |
|||
Death, if it occurs, follows typically six to sixteen days after symptoms appear and is often due to [[hypovolemic shock|low blood pressure from fluid loss]].<ref name=Ruz2014/> Early supportive care to prevent dehydration may reduce the risk of death.<ref name=":4" /> |
|||
=== Post-Ebola virus syndrome === |
|||
If an infected person survives, recovery may be quick and complete.<ref name="Goeijenbier2014" /><ref name="Shantha2017" /> However, a large portion of survivors develop [[post-Ebola virus syndrome]] after the acute phase of the infection.<ref name="pmid31806422">{{cite journal |vauthors=Rojas M, Monsalve DM, Pacheco Y, Acosta-Ampudia Y, Ramírez-Santana C, Ansari AA, Gershwin ME, Anaya JM |date=January 2020 |title=Ebola virus disease: An emerging and re-emerging viral threat |url= |journal=Journal of Autoimmunity |volume=106 |issue= |pages=102375 |doi=10.1016/j.jaut.2019.102375 |pmid=31806422|doi-access=free }}</ref> |
|||
Prolonged cases are often complicated by the occurrence of long-term problems, such as [[orchitis|inflammation of the testicles]], [[arthralgia|joint pains]], fatigue, hearing loss, mood and sleep disturbances, [[myalgia|muscular pain]], abdominal pain, [[menstrual period|menstrual abnormalities]], [[miscarriage]]s, [[desquamation|skin peeling]], or [[alopecia|hair loss]].<ref name="Goeijenbier2014" /><ref name="Shantha2017">{{Cite journal |vauthors=Shantha JG, Crozier I, Yeh S |date=November 2017 |title=An update on ocular complications of Ebola virus disease |journal=Current Opinion in Ophthalmology |volume=28 |issue=6 |pages=600–606 |doi=10.1097/ICU.0000000000000426 |pmc=5988239 |pmid=28872492}}</ref> [[Uveitis|Inflammation and swelling of the uveal layer of the eye]] is the most common eye complication in survivors of Ebola virus disease.<ref name="Shantha2017" /> Eye symptoms, such as [[photophobia|light sensitivity]], [[hyperlacrimation|excess tearing]], and [[vision loss]] have been described.<ref>{{Cite journal |vauthors=Wiwanitkit S, Wiwanitkit V |date=2015 |title=Ocular problem in Ebola virus infection: A short review |journal=Saudi Journal of Ophthalmology |volume=29 |issue=3 |pages=225–226 |doi=10.1016/j.sjopt.2015.02.006 |pmc=4487942 |pmid=26155084}}</ref> |
|||
Ebola can stay in some body parts like the eyes,<ref name="VarkeyShantha2015">{{Cite journal |display-authors=6 |vauthors=Varkey JB, Shantha JG, Crozier I, Kraft CS, Lyon GM, Mehta AK, Kumar G, Smith JR, Kainulainen MH, Whitmer S, Ströher U, Uyeki TM, Ribner BS, Yeh S |year=2015 |title=Persistence of Ebola Virus in Ocular Fluid during Convalescence |journal=New England Journal of Medicine |volume=372 |issue=25 |pages=2423–2427 |doi=10.1056/NEJMoa1500306 |issn=0028-4793 |pmc=4547451 |pmid=25950269 |hdl=2328/35704}}</ref> breasts, and testicles after infection.<ref name=cdc9months/><ref name="MackayArden2015">{{Cite journal |vauthors=Mackay IM, Arden KE |year=2015 |title=Ebola virus in the semen of convalescent men |journal=The Lancet Infectious Diseases |volume=15 |issue=2 |pages=149–150 |doi=10.1016/S1473-3099(14)71033-3 |issn=1473-3099 |pmid=25467652}}</ref> Sexual transmission after recovery has been suspected.<ref>{{Cite journal |vauthors=Rogstad KE, Tunbridge A |date=February 2015 |title=Ebola virus as a sexually transmitted infection |journal=Current Opinion in Infectious Diseases |volume=28 |issue=1 |pages=83–85 |doi=10.1097/qco.0000000000000135 |pmid=25501666 |s2cid=7538665}}</ref><ref>{{Cite journal |display-authors=6 |vauthors=Christie A, Davies-Wayne GJ, Cordier-Lassalle T, Blackley DJ, Laney AS, Williams DE, Shinde SA, Badio M, Lo T, Mate SE, Ladner JT, Wiley MR, Kugelman JR, Palacios G, Holbrook MR, Janosko KB, de Wit E, van Doremalen N, Munster VJ, Pettitt J, Schoepp RJ, Verhenne L, Evlampidou I, Kollie KK, Sieh SB, Gasasira A, Bolay F, Kateh FN, Nyenswah TG, De Cock KM, ((Centers for Disease Control and Prevention (CDC))) |date=8 May 2015 |title=Possible sexual transmission of Ebola virus – Liberia, 2015 |journal=MMWR. Morbidity and Mortality Weekly Report |volume=64 |issue=17 |pages=479–481 |pmc=4584553 |pmid=25950255}}</ref> If sexual transmission occurs following recovery it is believed to be a rare event.<ref>{{Cite journal |vauthors=Sprecher, A |date=14 October 2015 |title=Handle Survivors with Care |journal=The New England Journal of Medicine |volume=377 |issue=15 |pages=1480–1482 |doi=10.1056/NEJMe1512928 |pmid=26465064 |doi-access=free}}</ref> One case of a condition similar to [[meningitis]] has been reported many months after recovery, {{as of|October 2015|lc=yes}}.<ref>{{Cite web |title=Neuro complications cited in UK nurse's Ebola case |date=15 October 2015 |url=http://www.cidrap.umn.edu/news-perspective/2015/10/neuro-complications-cited-uk-nurses-ebola-case |url-status=live |archive-url=https://web.archive.org/web/20151017211314/http://www.cidrap.umn.edu/news-perspective/2015/10/neuro-complications-cited-uk-nurses-ebola-case |archive-date=17 October 2015 |access-date=19 October 2015}}</ref> |
|||
==Epidemiology== |
==Epidemiology== |
||
{{For|more about specific outbreaks |
{{For|more about specific outbreaks|List of Ebola outbreaks}} |
||
[[File:CDC worker incinerates med-waste from Ebola patients in Zaire.jpg|thumb|CDC worker incinerates medical waste from Ebola patients in Zaire in 1976]] |
|||
The disease typically occurs in outbreaks in tropical regions of [[Sub-Saharan Africa]].<ref name=WHO2014/> Between 1976, when it was first identified, through 2013, fewer than 1,000 people per year have been infected.<ref name=WHO2014/><ref name=MMWRJune2014>{{cite web|title=Ebola Viral Disease Outbreak — West Africa, 2014|url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6325a4.htm?s_cid=mm6325a4_w|website=CDC|accessdate=26 June 2014|date=June 27, 2014}}</ref> The largest outbreak to date is the ongoing [[2014 West Africa Ebola outbreak]], which is affecting [[Guinea]], [[Sierra Leone]], and [[Liberia]].<ref name=CDC2014/> As of August 2014 it likely also affecting [[Nigeria]].<ref name=CDCAug2014N/> As of July 2014 more than 1320 cases have been identified.<ref name=CDC2014>{{cite web|title=CDC urges all US residents to avoid nonessential travel to Liberia, Guinea, and Sierra Leone because of an unprecedented outbreak of Ebola.|url=http://wwwnc.cdc.gov/travel/notices/warning/ebola-liberia|website=CDC|accessdate=2 August 2014|date=July 31, 2014}}</ref> |
|||
The disease typically occurs in outbreaks in tropical regions of [[Sub-Saharan Africa]].<ref name="WHO2014" /> From 1976 (when it was first identified) through 2013, the WHO reported 2,387 confirmed cases with 1,590 overall fatalities.<ref name="WHO2014" /><ref name="MMWRJune2014" /> The largest outbreak to date was the [[Ebola virus epidemic in West Africa]], which caused a large number of deaths in [[Guinea]], [[Sierra Leone]], and [[Liberia]].<ref name="CDC2014" /><ref name="CDCAug2014N" /> |
|||
===2007 to 2011=== |
|||
As of 30 August 2007, 103 people (100 adults and three children) were infected by a suspected hemorrhagic fever outbreak in the village of [[Kampungu]], Democratic Republic of the Congo. The outbreak started after the funerals of two village chiefs, and 217 people in four villages fell ill. The World Health Organization sent a team to take blood samples for analysis and confirmed that many of the cases were the result of ''Ebolavirus''.<ref>{{Cite news|title=Ebola Outbreak Confirmed in Congo|url=http://www.newscientist.com/article/dn12624-ebola-outbreak-confirmed-in-congo.html|work=NewScientist.com|date=2007-09-11|accessdate=2008-02-25}}</ref><ref>{{Cite book|title=Ebola outbreak in Congo|url=http://www.cbc.ca/health/story/2007/09/12/ebola-outbreak.html|accessdate=2009-05-31|date=2007-09-12|publisher=CDC news}}</ref> The Congo's last major Ebola epidemic killed 245 people in 1995 in [[Kikwit]], about {{convert|200|mi|km}} from the source of the August 2007 outbreak.<ref>{{Cite news|title=Mystery DR Congo fever kills 100|url=http://news.bbc.co.uk/2/hi/africa/6973013.stm|work=BBC News|date=2007-08-31|accessdate=2008-02-25}}</ref> |
|||
===1976=== |
|||
On 30 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the Bundibugyo District. After confirmation of samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization confirmed the presence of a new species of ''Ebolavirus'', which was tentatively named Bundibugyo.<ref>{{Cite news|title=Uganda: Deadly Ebola Outbreak Confirmed – UN|url=http://allafrica.com/stories/200711301070.html|work=UN News Service|date=2007-11-30|accessdate=2008-02-25}}</ref> The epidemic came to an official end on 20 February 2008. While it lasted, 149 cases of this new strain were reported, and 37 of those led to deaths. |
|||
====Sudan==== |
|||
[[File:Cotton Factory in Nzara, South Sudan.jpg|thumb|Cotton factory in Nzara, South Sudan, where the first outbreak occurred]] |
|||
The first known outbreak of EVD was identified only after the fact. It occurred between June and November 1976, in [[Nzara, South Sudan]]<ref name="Hoenen2012">{{Cite journal |vauthors=Hoenen T, Groseth A, Feldmann H |date=July 2012 |title=Current Ebola vaccines |journal=Expert Opin Biol Ther |volume=12 |issue=7 |pages=859–872 |doi=10.1517/14712598.2012.685152 |pmc=3422127 |pmid=22559078}}</ref><ref name="Peterson AT, Bauer JT, Mills JN 2004 40–47">{{Cite journal |vauthors=Peterson AT, Bauer JT, Mills JN |year=2004 |title=Ecologic and Geographic Distribution of Filovirus Disease |journal=Emerg. Infect. Dis. |volume=10 |issue=1 |pages=40–47 |doi=10.3201/eid1001.030125 |pmc=3322747 |pmid=15078595}}</ref> (then part of [[Sudan]]), and was caused by [[Sudan virus]] (SUDV). The Sudan outbreak infected 284 people and killed 151. The first identifiable case in Sudan occurred on 27 June in a storekeeper in a cotton factory in [[Nzara]], who was hospitalised on 30 June and died on 6 July.<ref name="Feldmann2011" /><ref name="who's first encounter">{{Cite web |title=Ebola haemorrhagic fever in Sudan, 1976 |url=http://whqlibdoc.who.int/bulletin/1978/Vol56-No2/bulletin_1978_56(2)_247-270.pdf |url-status=dead |archive-url=https://web.archive.org/web/20141013194802/http://whqlibdoc.who.int/bulletin/1978/Vol56-No2/bulletin_1978_56(2)_247-270.pdf |archive-date=13 October 2014 |access-date=8 October 2014}}</ref> Although the WHO medical staff involved in the Sudan outbreak knew that they were dealing with a heretofore unknown disease, the actual "positive identification" process and the naming of the virus did not occur until some months later in [[Zaire]].<ref name="who's first encounter" /> |
|||
An International Symposium to explore the environment and filovirus, cell system and filovirus interaction, and filovirus treatment and prevention was held at Centre Culturel Français, [[Libreville]], Gabon, during March 2008.<ref>{{Cite book|title=The IV International Symposium on Filoviruses|url=http://www.ird.fr/filomeeting2008/venue.php|accessdate=2009-0-31|publisher=l'Institut de recherche pour le développement (IRD)}}</ref> The virus appeared in southern [[Kasai Occidental]] on 27 November 2008,<ref>{{Cite book|last=World Health Organization|title=RD Congo: Fièvre hémorragique à virus Ebola au Kasaï Occidental, Rapport de situation No 1 des 26 & 27 décembre 2008|url=http://www.reliefweb.int/rw/rwb.nsf/db900sid/ASAZ-7MSCBQ?OpenDocument|accessdate=2009-06-02|date=2008-12-27|publisher=Relief Web|language=French}}</ref> and blood and stool samples were sent to laboratories in Gabon and South Africa for identification. |
|||
====Zaire==== |
|||
On 25 December 2008, it was reported that the Ebola virus had killed 9 and infected 21 people in the Western Kasai province of the Democratic Republic of Congo.<ref name="FluTrackers">{{cite web | url=http://www.flutrackers.com/forum/printthread.php?t=89268 | title=DR Congo: Ebola Outbreak Confirmed, 9 Deaths | date=December 25, 2008 | accessdate=3 August 2014}}</ref> On 29 December, Doctors Without Borders reported 11 deaths in the same area, stating that a further 24 cases were being treated. In January 2009, Angola closed down part of its border with the Democratic Republic of Congo to prevent the spread of the outbreak.<ref>{{Cite book|title=Ebola alert shuts Angolan border|url=http://news.bbc.co.uk/2/hi/africa/7812868.stm|accessdate=2009-05-31|date=2009-01-06|publisher=BBC}}</ref> |
|||
{{main|1976 Zaire Ebola virus outbreak}} |
|||
[[File:CDC worker incinerates med-waste from Ebola patients in Zaire.jpg|thumb|upright|A CDC worker incinerates medical waste from Ebola patients in Zaire in 1976.]] |
|||
On 26 August 1976, the second outbreak of EVD began in [[Yambuku]], a small rural village in [[Mongala District]] in northern [[Zaire]] (now known as the [[Democratic Republic of the Congo]]).<ref>{{Cite book |vauthors=Hewlett B, Hewlett B |url=https://books.google.com/books?id=aboFAAAAQBAJ&pg=PA103 |title=Ebola, Culture and Politics: The Anthropology of an Emerging Disease |date=2007 |publisher=Cengage Learning |isbn=978-1111797317 |page=103 |access-date=31 July 2014 |archive-date=21 May 2024 |archive-url=https://web.archive.org/web/20240521144049/https://books.google.com/books?id=aboFAAAAQBAJ&pg=PA103 |url-status=live }}</ref><ref name="Feldmann2003">{{Cite journal |vauthors=Feldmann H, Jones S, Klenk HD, Schnittler HJ |date=August 2003 |title=Ebola virus: from discovery to vaccine |journal=Nature Reviews Immunology |volume=3 |issue=8 |pages=677–685 |doi=10.1038/nri1154 |pmid=12974482 |s2cid=27486878|doi-access=free }}</ref> This outbreak was caused by EBOV, formerly designated ''Zaire ebolavirus'', a different member of the [[genus]] ''Ebolavirus'' than in the first Sudan outbreak. The [[index case|first person infected with the disease]] was the village school's headmaster [[Mabalo Lokela]], who began displaying symptoms on 26 August 1976.<ref name="whqlibdoc.who.int">{{Cite journal |last=Report of an International Commission |year=1978 |title=Ebola haemorrhagic fever in Zaire, 1976 |url=http://whqlibdoc.who.int/bulletin/1978/Vol56-No2/bulletin_1978_56(2)_271-293.pdf |url-status=dead |journal=Bull. World Health Organ. |volume=56 |issue=2 |pages=271–293 |pmc=2395567 |pmid=307456 |archive-url=https://web.archive.org/web/20140808213715/http://whqlibdoc.who.int/bulletin/1978/Vol56-No2/bulletin_1978_56%282%29_271-293.pdf |archive-date=8 August 2014 |access-date=14 August 2014 }}</ref> Lokela had returned from a trip to Northern Zaire near the border of the [[Central African Republic]], after visiting the [[Ebola River]] between 12 and 22 August. He was originally believed to have [[malaria]] and was given [[quinine]]. However, his symptoms continued to worsen, and he was admitted to Yambuku Mission Hospital on 5 September. Lokela died on 8 September 14 days after he began displaying symptoms.<ref name="urlOutbreak of Ebola Viral Hemorrhagic Fever – Zaire, 1995">{{Cite journal |last=Centers for Disease Control Prevention (CDC) |year=1995 |title=Outbreak of Ebola Viral Hemorrhagic Fever – Zaire, 1995 |url=https://www.cdc.gov/mmwr/preview/mmwrhtml/00037078.htm |url-status=live |journal=Morbidity and Mortality Weekly Report |volume=44 |issue=19 |pages=381–382 |pmid=7739512 |archive-url=https://web.archive.org/web/20170625191457/https://www.cdc.gov/mmwr/preview/mmwrhtml/00037078.htm |archive-date=25 June 2017 }}</ref><ref name="urlMabalo Lokela Archives – Political Moll">{{Cite web | vauthors = Elezra M |title=Ebola: The Truth Behind The Outbreak (Video) l |url=http://politicalmoll.com/tag/mabalo-lokela/ |url-status=dead |archive-url=https://web.archive.org/web/20150712140500/http://politicalmoll.com/tag/mabalo-lokela/ |archive-date=12 July 2015 |access-date=18 October 2014 |website=Mabalo Lokela Archives – Political Mol}}</ref> |
|||
On 12 March 2009, an unidentified 45-year-old scientist from Germany accidentally pricked her finger with a needle used to inject Ebola into lab mice. She was given an experimental vaccine never before used on humans. Since the peak period for an outbreak during the 21-day Ebola incubation period had passed as of 2 April 2009, she had been declared healthy and safe. It remains unclear whether or not she was ever actually infected with the virus.<ref>{{cite news|last=Eddyn|first=Melissan|title=Scientist Injects Self With Ebola|url=http://www.gouverneurtimes.com/index.php?option=com_content&view=article&id=2202:scientist-injects-self-with-ebola&catid=54:worldnational-news&Itemid=153|accessdate=2009-05-02|date=2009-03-27|agency=Associated Press}}</ref> |
|||
Soon after Lokela's death, others who had been in contact with him also died, and people in Yambuku began to panic. The country's Minister of Health and Zaire President [[Mobutu Sese Seko]] declared the entire region, including Yambuku and the country's capital, [[Kinshasa]], a quarantine zone. No-one was permitted to enter or leave the area, and roads, waterways, and airfields were placed under [[martial law]]. Schools, businesses and social organisations were closed.<ref name="Stimola">{{Cite book | vauthors = Stimola A |url=https://archive.org/details/ebola0000stim/page/31 |title=Ebola |publisher=Rosen Pub. |year=2011 |isbn=978-1435894334 |edition=1st |location=New York |pages=[https://archive.org/details/ebola0000stim/page/31 31, 52] |url-access=registration}}</ref> The initial response was led by Congolese doctors, including [[Jean-Jacques Muyembe-Tamfum]], one of the discoverers of Ebola. Muyembe took a blood sample from a Belgian nun; this sample would eventually be used by [[Peter Piot]] to identify the previously unknown Ebola virus.<ref>{{Cite news |title=This Congolese Doctor Discovered Ebola But Never Got Credit For It – Until Now |work=NPR.org |url=https://www.npr.org/sections/goatsandsoda/2019/11/04/774863495/this-congolese-doctor-discovered-ebola-but-never-got-credit-for-it-until-now |access-date=5 November 2019 |archive-date=5 November 2019 |archive-url=https://web.archive.org/web/20191105012037/https://www.npr.org/sections/goatsandsoda/2019/11/04/774863495/this-congolese-doctor-discovered-ebola-but-never-got-credit-for-it-until-now |url-status=live }}</ref> Muyembe was also the first scientist to come into direct contact with the disease and survive.<ref>{{Cite web |vauthors=McNeish H |date=24 March 2017 |title=He Treated The Very First Ebola Cases 40 Years Ago. Then He Watched The World Forget. |url=https://www.huffpost.com/entry/ebola-neglected-tropical-diseases_n_58d2ac02e4b0f838c62e9e0d |access-date=5 November 2019 |website=HuffPost |archive-date=25 July 2019 |archive-url=https://web.archive.org/web/20190725203823/https://www.huffpost.com/entry/ebola-neglected-tropical-diseases_n_58d2ac02e4b0f838c62e9e0d |url-status=live }}</ref> Researchers from the [[Centers for Disease Control and Prevention]] (CDC), including Piot, co-discoverer of Ebola, later arrived to assess the effects of the outbreak, observing that "the whole region was in panic."<ref name="Piot_2012">{{Cite book |title=No time to lose: a life in pursuit of deadly viruses |vauthors=Piot P, Marshall R |publisher=W.W. Norton & Co. |year=2012 |isbn=978-0393063165 |edition=1st |location=New York |pages=30, 90}}</ref><ref name="Piot-one">{{Cite news | vauthors = Piot P |date=11 August 2014 |title=Part one: A virologist's tale of Africa's first encounter with Ebola |work=ScienceInsider |url=https://www.science.org/content/article/part-one-virologists-tale-africas-first-encounter-ebola |url-status=live |archive-url=https://web.archive.org/web/20141009050901/http://news.sciencemag.org/africa/2014/08/part-one-virologists-tale-africas-first-encounter-ebola |archive-date=9 October 2014 }}</ref><ref name="Piot-two">{{Cite news | vauthors = Piot P |date=13 August 2014 |title=Part two: A virologist's tale of Africa's first encounter with Ebola |work=ScienceInsider |url=https://www.science.org/content/article/part-two-virologists-tale-africas-first-encounter-ebola |url-status=live |archive-url=https://web.archive.org/web/20141116233325/http://news.sciencemag.org/africa/2014/08/part-two-virologists-tale-africas-first-encounter-ebola |archive-date=16 November 2014 }}</ref> |
|||
In May 2011, a 12-year-old girl in Uganda died from Ebola (Sudan subspecies). No further cases were recorded.<ref>{{Cite news|last=Malone|first=Barry|title=Uganda says Ebola outbreak is over|url=http://www.reuters.com/article/2011/06/17/us-uganda-ebola-idUSTRE75G24E20110617|accessdate=2011-07-06|date=2011-06-17|publisher=Reuters}}</ref> |
|||
Piot concluded that Belgian nuns had inadvertently started the epidemic by giving unnecessary vitamin injections to pregnant women without sterilizing the syringes and needles. The outbreak lasted 26 days and the quarantine lasted two weeks. Researchers speculated that the disease disappeared due to the precautions taken by locals, the quarantine of the area, and discontinuing of the injections.<ref name=Stimola/> |
|||
===2012 outbreaks=== |
|||
In July 2012, the Ugandan Health Ministry confirmed 13 deaths due to an outbreak of the Ebola-Sudan variant<ref>{{cite web | publisher = Norwegian Council for Africa | url = http://www.afrika.no/Detailed/22121.html |title=Congo (DRC): Bushmeat blamed for Ebola outbreak | date = 2012-08-24 | accessdate = 2013-04-15}}</ref> in the [[Kibaale]] District.<ref>{{Cite news |url=http://www.bbc.co.uk/news/world-africa-19031860 |title=Outbreak of Ebola in Uganda kills 13 |work=BBC News |date=July 28, 2012 }}</ref> On 28 July, it was reported that 14 out of 20 (70% mortality rate) had died in Kibaale.<ref>{{cite web|url=http://www.msnbc.msn.com/id/48372851/ns/health/ |title=Officials: Uganda Ebola outbreak kills 14 | work = Health | publisher = MSNBC | date = 2012-07-28 | accessdate = 2013-04-15 | author = Muhumuza R }}</ref> On 30 July, Stephen Byaruhanga, a health official in Kibaale District, said the Ebola outbreak had spread from one remote village to several villages.<ref>{{cite news|title=Ebola Outbreak Spreads|accessdate=2012-07-31|newspaper=Associated Press – The Express|date=July 31, 2012}}</ref> |
|||
During this outbreak, Ngoy Mushola recorded the first clinical description of EVD in [[Yambuku]], where he wrote the following in his daily log: "The illness is characterised with a high temperature of about {{convert|39|°C|0}}, [[haematemesis]], diarrhoea with blood, retrosternal abdominal pain, prostration with 'heavy' articulations, and rapid evolution death after a mean of three days."<ref>{{Cite web | vauthors = Bardi JS |title=Death Called a River |url=http://www.scripps.edu/newsandviews/e_20020114/ebola1.html |url-status=live |archive-url=https://web.archive.org/web/20140802170848/http://www.scripps.edu/newsandviews/e_20020114/ebola1.html |archive-date=2 August 2014 |access-date=9 October 2014 |website=The Scripps Research Institute}}</ref> |
|||
The [[World Health Organization]]'s (WHO) global and alert response network reported on August 3 that the suspected case count had risen to 53, including 16 deaths. Of these cases, five were confirmed by [[UVRI]] as Ebola cases. There were no confirmed cases outside of [[Kibaale]] District except for a patient who was medically evacuated to [[Kampala]] District and then died. [[WHO]] and [[Centers for Disease Control and Prevention|CDC]] support was on the ground in Uganda supporting the government response. There were no confirmed cases outside of [[Uganda]].<ref>{{cite web|url=http://www.who.int/csr/don/2012_08_03/en/index.html |title=WHO | Ebola in Uganda – update |publisher=Who.int |date=2012-08-03 |accessdate=2013-04-15}}</ref> Included among populations confirmed to be affected were prisoners in Kabbale prison. <ref name="urlPrisoner with suspected case of Ebola escapes from hospital in Uganda - CNN.com">{{cite web | url = http://www.cnn.com/2012/08/03/health/uganda-ebola-virus/index.html | title = Prisoner with suspected case of Ebola escapes from hospital in Uganda | publisher = CNN.com | date =6 August 2012 | author = McKenzie D }}</ref> Dr. Joaquim Saweka, the [[WHO]] representative to Uganda, reported that the outbreak was under control and that everyone known to have had contact with a known Ebola patient was in isolation.<ref>{{cite web|url=http://www.medicaldaily.com/news/20120803/11282/un-world-health-organization-ebola-uganda.htm |title=WHO: Ebola Outbreak in Uganda is Under Control | work = US/World | publisher = Medical Daily | date = 2012-08-03 | accessdate = 2013-04-15 | author = Hsu C }}</ref> |
|||
The virus responsible for the initial outbreak, first thought to be the [[Marburg virus]], was later identified as a new type of virus related to the genus ''[[Marburgvirus]]''. Virus strain samples isolated from both outbreaks were named "Ebola virus" after the [[Ebola River]], near the first-identified viral outbreak site in Zaire.<ref name=Feldmann2011/> Reports conflict about who initially coined the name: either Karl Johnson of the American CDC team<ref name="hz">{{Cite book | vauthors = Preston R |title=The Hot Zone |title-link=The Hot Zone |date=20 July 1995 |publisher=Anchor Books ([[Random House]]) |page=[https://archive.org/details/hotzone1995pres/page/n144 117] |quote=Karl Johnson named it Ebola |author-link=Richard Preston}}</ref> or Belgian researchers.<ref name="observer">{{Cite web | vauthors = von Bredow R, Hackenbroch V |date=4 October 2014 |title=In 1976 I Discovered Ebola – Now I Fear an Unimaginable Tragedy |url=https://www.theguardian.com/world/2014/oct/04/ebola-zaire-peter-piot-outbreak |url-status=live |archive-url=https://web.archive.org/web/20170103105318/https://www.theguardian.com/world/2014/oct/04/ebola-zaire-peter-piot-outbreak |archive-date=3 January 2017 |website=[[The Guardian]]}}</ref> Subsequently, a number of other cases were reported, almost all centred on the Yambuku mission hospital or close contacts of another case.<ref name="whqlibdoc.who.int" /> In all, 318 cases and 280 deaths (an 88% fatality rate) occurred in Zaire.<ref name="emedicine.com">{{Cite web | vauthors = King JW |date=2 April 2008 |title=Ebola Virus |url=http://www.emedicine.com/MED/topic626.htm |url-status=live |archive-url=https://web.archive.org/web/20080928063653/http://www.emedicine.com/med/TOPIC626.HTM |archive-date=28 September 2008 |access-date=6 October 2008 |website=eMedicine |publisher=WebMD }}</ref> Although the two outbreaks were at first believed connected, scientists later realised that they were caused by two distinct ebolaviruses, SUDV and EBOV.<ref name=Feldmann2003/> |
|||
On 8 August, the Ugandan Ministry of Health recorded 23 probable and confirmed cases, including 16 deaths. Ten cases were confirmed by the [[UVRI|Uganda Virus Research Institute]] as Ebola. 185 people who came into contact with probable and confirmed Ebola cases were followed during the incubation period of 21 days.<ref>{{cite web | url=http://www.who.int/csr/don/2012_08_10/en/index.html | title = Ebola in Uganda – update | publisher = WHO | accessdate = 2012-08-10}}</ref> |
|||
===1995–2014=== |
|||
On 17 August, the Ministry of Health of the [[Democratic Republic of the Congo]] reported an outbreak of the Ebola-Bundibugyo variant<ref>{{cite web|url=http://www.voanews.com/content/Ebola-drc-outbreak/1492233.html |title=DRC Confirms Ebola Outbreak |publisher=Voanews.com |accessdate=2013-04-15}}</ref> in the eastern region.<ref>{{cite web|url=http://www.who.int/csr/don/2012_08_18/en/index.html |title=WHO | Ebola outbreak in Democratic Republic of Congo |publisher=Who.int |date=2012-08-17 |accessdate=2013-04-15}}</ref> By 21 August, the [[WHO]] reported a total of 15 cases and 10 fatalities.<ref>{{cite web|url=http://www.who.int/csr/don/2012_08_21/en/index.html |title=WHO | Ebola outbreak in Democratic Republic of Congo – update |publisher=Who.int |date=2012-08-21 |accessdate=2013-04-15}}</ref> No evidence suggested that this outbreak was connected to the Ugandan outbreak.<ref>{{cite web|url=http://www.disasternews.net/news/article.php?articleid=5009 |title=Ebola outbreak in DRC – Disaster News Network |publisher=Disasternews.net |date=2012-08-22 |accessdate=2013-04-15}}</ref> By 13 September 2012, the WHO revealed that the virus had claimed 32 lives and that the probable cause of the outbreak was tainted [[bush meat]] hunted by local villagers around the towns of [[Isiro]] and Viadana.<ref>{{Cite journal | url = http://www.cbsnews.com/8301-504763_162-57512216-10391704/ebola-virus-claims-31-lives-in-democratic-republic-of-the-congo/ | title = Ebola virus claims 31 lives in Democratic Republic of the Congo | year = 2012 | publisher = [[CBS News]] | publication-place = [[United States]] | accessdate = 14 September 2012 | ref = harv | author = Castillo M }}</ref> |
|||
[[File:Ebolafälle bis einschließlich 2020 english.png|thumb|upright=1.3|Cases of Ebola fever in Africa since 1976]] |
|||
The second major outbreak occurred in Zaire (now the [[Democratic Republic of the Congo]], DRC), in 1995, affecting 315 and killing 254.<ref name="WHO2014" /> |
|||
In 2000, [[Uganda]] had an outbreak infecting 425 and killing 224; in this case, the Sudan virus was found to be the Ebola species responsible for the outbreak.<ref name="WHO2014" /> |
|||
===2014 outbreak=== |
|||
{{main|2014 West Africa Ebola outbreak}} |
|||
[[File:Diseased Ebola 2014.png|thumb|Increase over time in the cases and deaths during the 2014 outbreak.]] |
|||
In March 2014, an outbreak of the Ebola virus occurred in the Western African nation of [[Guinea]].<ref name=CDC2014Out>{{cite web|title=Guidelines for Evaluation of US Patients Suspected of Having Ebola Virus Disease|url=http://emergency.cdc.gov/han/han00364.asp|website=CDC|accessdate=5 August 2014|date=August 1, 2014}}</ref> This is the first Ebola virus outbreak registered in the region.<ref name=CDC2014Out/> As of April 10, 157 suspected and confirmed cases and 101 deaths had been reported in Guinea, 22 suspected cases in [[Liberia]] including 14 deaths, 8 suspected cases in [[Sierra Leone]] including 6 deaths, and 1 suspected case in [[Mali]].<ref>{{cite web | title = Outbreak of Ebola in Guinea and Liberia | url = http://www.cdc.gov/vhf/ebola/outbreaks/guinea/ | publisher = Centers for Disease Control and Prevention | accessdate = 13 April 2014 }}</ref><ref name="urlEbola virus disease, West Africa (Situation as of 7 April 2014) - Guinea | ReliefWeb">{{cite web | url = http://reliefweb.int/report/guinea/ebola-virus-disease-west-africa-situation-7-april-2014 | title = Ebola virus disease, West Africa (Situation as of 7 April 2014) - Guinea | author = World Health Organization | publisher = ReliefWeb | date = 2014-04-07 }}</ref> By late June 2014 the death toll had reached 390 with over 600 cases reported.<ref>[http://www.bignewsnetwork.com/index.php/sid/223347161/scat/c08dd24cec417021/ht/WHO-warns-drastic-action-needed-to-combat-Ebola-outbreak WHO warns drastic action needed to combat Ebola outbreak | Big News Network.com]</ref> By 23 July 2014, the [[World Health Organization]] had reported 1201 confirmed cases including 672 deaths since the epidemic began in March.<ref name=WHO_25_July_2014>{{cite web |url=http://www.afro.who.int/en/clusters-a-programmes/dpc/epidemic-a-pandemic-alert-and-response/outbreak-news/4233-ebola-virus-disease-west-africa-25-july-2014.html |title=Ebola virus disease, West Africa – update 25 July 2014 | publisher = World Health Organization | work = WHO: Outbreak news | date = 2014-07-25 |accessdate = 2014-07-30 }}</ref> On 31 July 2014, WHO reports the death toll has reached 826 from 1440 cases.<ref>http://www.afro.who.int/en/clusters-a-programmes/dpc/epidemic-a-pandemic-alert-and-response/outbreak-news/4238-ebola-virus-disease-west-africa-31-july-2014.html WHO - Ebola virus disease, West Africa – update 31 July 2014</ref> |
|||
In 2003, an outbreak in the DRC infected 143 and killed 128, a 90% death rate, the highest of a [[genus]] ''Ebolavirus'' outbreak to date.<ref name="pmid14579469">{{Cite journal |display-authors=6 |vauthors=Formenty P, Libama F, Epelboin A, Allarangar Y, Leroy E, Moudzeo H, Tarangonia P, Molamou A, Lenzi M, Ait-Ikhlef K, Hewlett B, Roth C, Grein T |year=2003 |title=[Outbreak of Ebola hemorrhagic fever in the Republic of the Congo, 2003: a new strategy?] |journal=Med Trop (Mars) |language=fr |volume=63 |issue=3 |pages=291–295 |pmid=14579469}}</ref> |
|||
[[Emory University Hospital]] was the first US hospital to care for people exposed to Ebola.<ref name="urlEmory Healthcare statement and letter to the Emory Community | Emory University | Atlanta, GA">{{cite web | url = http://news.emory.edu/stories/2014/07/euh_ebola_patient/campus.html+ | title = Emory Healthcare statement and letter to the Emory Community | publisher = Emory University | date = 2014-08-01 | work = Emory Healthcare Statement }}</ref> Two American medical providers, Kent Brantly and [[Nancy Writebol]], were exposed while treating infected patients in Liberia. Arrangements were made for them to be transported to Emory via speciality aircraft. Emory Hospital has a specially built isolation unit set up in collaboration with the [[Centers for Disease Control and Prevention|CDC]] to treat people exposed to certain serious infectious diseases.<ref name="url2 American Ebola patients head to USA">{{cite web | url = http://www.usatoday.com/story/news/nation/2014/08/01/ebola-liberia-american-patient-emory/13453997 | title = 2 American Ebola patients head to USA | author = Stanglin D | publisher = USA Today | date = 2014-08-01 }}</ref><ref name="urlEbola coming to U.S, as Atlanta hospital prepares - CNN.com">{{cite web | url = http://www.cnn.com/2014/08/01/health/ebola-outbreak/index.html?hpt=hp_c2 | title = Ebola coming to U.S, as Atlanta hospital prepares | publisher = CNN.com | author = Botelho G, Brumfield B, Carter CJ | date = 2014-08-02 }}</ref><ref name="urlMedical Evacuations of Two U.S. Citizens From West Africa">{{cite web | url = http://www.state.gov/r/pa/prs/ps/2014/230120.htm | title = Medical Evacuations of Two U.S. Citizens From West Africa | publisher = U.S. Department of State | author = Harf M | work = Press Statement | date = 2014-08-01 }}</ref> On 2 August 2014 Brantly was flown in to [[Dobbins Air Force Base]] in [[Marietta, Georgia]] and transferred to Emory Hospital.<ref name="EbolaVictims">{{cite news|title=US allays Ebola fears as doctors flown home for treatment|url=http://www.atlantanews.net/index.php/sid/224382413/scat/ffe56b8f30c50146/ht/US-allays-Ebola-fears-as-doctors-flown-home-for-treatmentom|accessdate=2 August 2014|publisher=''Atlanta News.Net''}}</ref> |
|||
In 2004, a Russian scientist died from Ebola after [[Needlestick injury|sticking]] herself with an infected needle.<ref>{{Cite news | vauthors = Miller J |date=25 May 2004 |title=Russian Scientist Dies in Ebola Accident at Former Weapons Lab |work=[[The New York Times]] |url=https://www.nytimes.com/2004/05/25/world/russian-scientist-dies-in-ebola-accident-at-former-weapons-lab.html |url-status=live |access-date=12 October 2014 |archive-url=https://web.archive.org/web/20141017035417/http://www.nytimes.com/2004/05/25/world/russian-scientist-dies-in-ebola-accident-at-former-weapons-lab.html |archive-date=17 October 2014}}</ref> |
|||
==History== |
|||
{{For|more about the outbreak in Virginia, US|Reston virus}} |
|||
[[File:EbolaSubmit2.png|thumb|350px|Cases of ebola fever in Africa from 1979 to 2008.]] |
|||
Ebola virus was first isolated in 1976 during outbreaks of Ebola hemorrhagic fever in [[Zaire]]<ref name = Piot>{{cite web | url = http://www.bbc.co.uk/news/magazine-28262541 | title = The virus detective who discovered Ebola in 1976 | publisher = BBC News | author = Brown R | date = 2014-07-17 | work = News Magazine }}</ref> and [[Sudan]].<ref>{{cite journal | author = Bennett D, Brown D | title = Ebola virus | journal = BMJ (Clinical research ed.) | volume = 310 | issue = 6991 | pages = 1344–1345 | date = May 1995 | pmid = 7787519 | pmc = 2549737 | doi = 10.1136/bmj.310.6991.1344 }}</ref> The strain of Ebola that broke out in Zaire has one of the highest [[case fatality rate]]s of any human virus, roughly 90%.<ref name="emedicine.com">{{cite web | url = http://www.emedicine.com/MED/topic626.htm | accessdate = 2008-10-06 | author = King JW | title = Ebola Virus | date = 2008-04-02 | work = eMedicine | publisher = WebMd }}</ref> |
|||
Between April and August 2007, a fever epidemic<ref name="CBCRadioSept2007">{{Cite news |date=12 September 2007 |title=Ebola outbreak in Congo |publisher=[[CBC News]] |url=http://www.cbc.ca/news/world/ebola-outbreak-in-congo-1.648593 |url-status=live |archive-url=https://web.archive.org/web/20141119105248/http://www.cbc.ca/news/world/ebola-outbreak-in-congo-1.648593 |archive-date=19 November 2014}}</ref> in a four-village region<ref name="Mystery DR Congo fever kills 100">{{Cite news |date=31 August 2007 |title=Mystery DR Congo fever kills 100 |work=BBC News Online |url=http://news.bbc.co.uk/2/hi/africa/6973013.stm |url-status=live |archive-url=https://web.archive.org/web/20071111024636/http://news.bbc.co.uk/2/hi/africa/6973013.stm |archive-date=11 November 2007}}</ref> of the DRC was confirmed in September to have been cases of Ebola.<ref>{{Cite news |date=11 September 2007 |title=Ebola Outbreak Confirmed in Congo |work=NewScientist.com |url=https://www.newscientist.com/article/dn12624-ebola-outbreak-confirmed-in-congo.html |url-status=live |archive-url=https://web.archive.org/web/20150618230241/http://www.newscientist.com/article/dn12624-ebola-outbreak-confirmed-in-congo.html |archive-date=18 June 2015}}</ref> Many people who attended the recent funeral of a local village chief died.<ref name="Mystery DR Congo fever kills 100" /> The 2007 outbreak eventually infected 264 individuals and killed 187.<ref name="WHO2014" /> |
|||
The name of the disease originates from one of those first recorded outbreaks in 1976 in [[Yambuku]], Democratic Republic of the Congo (then Zaire), which lies on the [[Ebola River]].<ref name = Piot/> |
|||
On 30 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the [[Bundibugyo District]] in Western Uganda. After confirming samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization (WHO) confirmed the presence of a new species of [[genus]] ''Ebolavirus'', which was tentatively named Bundibugyo.<ref>{{Cite news |date=30 November 2007 |title=Uganda: Deadly Ebola Outbreak Confirmed – UN |publisher=UN News Service |url=http://allafrica.com/stories/200711301070.html |url-status=live |access-date=25 February 2008 |archive-url=https://web.archive.org/web/20080303200540/http://allafrica.com/stories/200711301070.html |archive-date=3 March 2008}}</ref> The WHO reported 149 cases of this new strain and 37 of those led to deaths.<ref name="WHO2014" /> |
|||
While investigating an outbreak of [[Simian hemorrhagic fever virus]] (SHFV) in November 1989, an electron microscopist from [[USAMRIID]] discovered [[filoviruses]] similar in appearance to Ebola in tissue samples taken from [[crab-eating macaque]] imported from the [[Philippines]] to Hazleton Laboratories Reston, Virginia.<ref name="McCormick 1999 277–279">{{harvnb|McCormick|Fisher-Hoch|1999|pp=277–279}}</ref> Blood samples were taken from 178 animal handlers during the incident.<ref name="Waterman 1999">{{Cite book|last=Waterman|first=Tara|url=http://www.stanford.edu/group/virus/filo/ebor.html|title=Ebola Reston Outbreaks|accessdate=2008-08-02|year=1999|publisher=Stanford University}}</ref> Of those, six animal handlers eventually [[seroconverted]]. When the handlers did not become ill, the CDC concluded that the virus had a very low pathogenicity to humans.<ref name="McCormick 1999 298–299">{{harvnb|McCormick|Fisher-Hoch|1999|pp=298–299}}</ref> |
|||
The WHO confirmed two small outbreaks in Uganda in 2012, both caused by the Sudan variant. The first outbreak affected seven people, killing four, and the second affected 24, killing 17.<ref name="WHO2014" /> |
|||
In 1990, Hazelton Research Products' Reston Quarantine Unit in [[Reston, Virginia]] suffered a mysterious outbreak of fatal illness among a shipment of [[crab-eating macaque]] monkeys imported from the Philippines. The company's veterinary pathologist sent tissue samples from dead animals to the [[United States Army Medical Research Institute of Infectious Diseases]] (USAMRIID) at [[Fort Detrick, Maryland]], where a laboratory test known as an [[ELISA]] assay showed antibodies to Ebola virus. |
|||
On 17 August 2012, the Ministry of Health of the DRC reported an outbreak of the Ebola-Bundibugyo variant<ref>{{Cite web |title=DRC Confirms Ebola Outbreak |date=21 August 2012 |url=http://www.voanews.com/content/Ebola-drc-outbreak/1492233.html |url-status=live |archive-url=https://web.archive.org/web/20120915235056/http://www.voanews.com/content/Ebola-drc-outbreak/1492233.html |archive-date=15 September 2012 |access-date=15 April 2013 |publisher=Voanews.com}}</ref> in the eastern region.<ref>{{Cite web |date=17 August 2012 |title=WHO – Ebola outbreak in Democratic Republic of Congo |url=https://www.who.int/csr/don/2012_08_18/en/index.html |url-status=dead |archive-url=https://web.archive.org/web/20131027035536/https://www.who.int/csr/don/2012_08_18/en/index.html |archive-date=27 October 2013 |access-date=15 April 2013 |publisher=[[World Health Organization]] (WHO)}}</ref><ref>{{Cite web |date=21 August 2012 |title=WHO – Ebola outbreak in Democratic Republic of Congo – update |url=https://www.who.int/csr/don/2012_08_21/en/index.html |url-status=dead |archive-url=https://web.archive.org/web/20121216144914/https://www.who.int/csr/don/2012_08_21/en/index.html |archive-date=16 December 2012 |access-date=15 April 2013 |publisher=[[World Health Organization]] (WHO)}}</ref> Other than its discovery in 2007, this was the only time that this variant has been identified as responsible for an outbreak. The WHO revealed that the virus had sickened 57 people and killed 29. The probable cause of the outbreak was tainted [[bush meat]] hunted by local villagers around the towns of [[Isiro]] and Viadana.<ref name="WHO2014" /><ref>{{Cite news | vauthors = Castillo M |year=2012 |title=Ebola virus claims 31 lives in Democratic Republic of the Congo |work=[[CBS News]] |location=United States |url=https://www.cbsnews.com/news/ebola-virus-claims-31-lives-in-democratic-republic-of-the-congo/ |url-status=live |access-date=14 September 2012 |archive-url=https://web.archive.org/web/20120914015301/http://www.cbsnews.com/8301-504763_162-57512216-10391704/ebola-virus-claims-31-lives-in-democratic-republic-of-the-congo/ |archive-date=14 September 2012 }}</ref> |
|||
Shortly afterward, a [[US Army]] team headquartered at USAMRIID went into action to [[Euthanisia|euthanize]] the monkeys which had not yet died, bringing those monkeys and those which had already died of the disease to [[Ft. Detrick]] for study by the Army's veterinary pathologists and virologists, and eventual disposal under safe conditions. |
|||
The Philippines and the United States had no previous cases of Ebola infection, and upon further isolation researchers concluded it was another strain of Ebola, or a new filovirus of Asian origin, which they named ''[[Reston ebolavirus]]'' (REBOV) after the location of the incident.<ref name="Preston">{{cite book | title=The Hot Zone | publisher=Random House | author=Preston, Richard | year=1994 | location=New York | pages=300 | isbn=978-0679437840}}</ref> |
|||
In 2014, an outbreak occurred in the DRC. [[Whole genome sequencing|Genome-sequencing]] showed that this outbreak was not related to the [[West Africa Ebola virus outbreak|2014–15 West Africa Ebola virus outbreak]], but was the same [[EBOV]] species, the Zaire species.<ref name="2014 DRC Who Strain">{{Cite web |date=2 September 2014 |title=Virological Analysis: no link between Ebola outbreaks in west Africa and Democratic Republic of Congo |url=https://www.who.int/mediacentre/news/ebola/2-september-2014/en/ |url-status=dead |archive-url=https://web.archive.org/web/20141121121328/https://www.who.int/mediacentre/news/ebola/2-september-2014/en/ |archive-date=21 November 2014 |publisher=[[World Health Organization]] (WHO) }}</ref> It began in August 2014, and was declared over in November with 66 cases and 49 deaths.<ref name="reuters1511">{{Cite news |date=15 November 2014 |title=Congo declares its Ebola outbreak over |work=Reuters |url=http://uk.reuters.com/article/health-ebola-congodemocratic-idUKL6N0T50F720141115 |url-status=dead |access-date=15 November 2014 |archive-url=https://web.archive.org/web/20141129065140/http://uk.reuters.com/article/2014/11/15/health-ebola-congodemocratic-idUKL6N0T50F720141115 |archive-date=29 November 2014}}</ref> This was the 7th outbreak in the DRC, three of which occurred during the period when the country was known as [[Zaire]].<ref>{{Cite web |date=December 2014 |title=Democratic Republic of the Congo: The country that knows how to beat Ebola |url=https://www.who.int/features/2014/drc-beats-ebola/en/ |url-status=dead |archive-url=https://web.archive.org/web/20150226005300/https://www.who.int/features/2014/drc-beats-ebola/en/ |archive-date=26 February 2015 |access-date=26 February 2015 |publisher=[[World Health Organization]] (WHO)}}</ref> |
|||
Some scientists also believe that the [[Plague of Athens]], which wiped out about a third of its inhabitants during the [[Peloponnesian War]], may have been caused by Ebola. However, these studies are conflicting, and point to other possible diseases such as typhoid.<ref>{{cite web|url=http://en.wikipedia.org/wiki/Plague_of_Athens#Viral_Hemorrhagic_Fever|title=Plague of Athens}}</ref> |
|||
===2013–2016 West Africa=== |
|||
{{main|West African Ebola virus epidemic}} |
|||
[[File:Diseased Ebola 2014.png|thumb|upright=1.3|Cases and deaths from April 2014 to July 2015 during the [[Ebola virus epidemic in West Africa|2013–2015 outbreak]]]] |
|||
In March 2014, the [[World Health Organization]] (WHO) reported a major Ebola outbreak in [[Guinea]], a West African nation.<ref name="CDC2014Out">{{Cite web |date=1 August 2014 |title=Guidelines for Evaluation of US Patients Suspected of Having Ebola Virus Disease |url=https://stacks.cdc.gov/view/cdc/24830 |url-status=live |archive-url=https://web.archive.org/web/20140808075214/http://emergency.cdc.gov/han/han00364.asp |archive-date=8 August 2014 |access-date=5 August 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC)}}</ref> Researchers traced the outbreak to a one-year-old child who died in December 2013.<ref name="Baize2014">{{Cite journal |display-authors=6 |vauthors=Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba N, Soropogui B, Sow MS, Keïta S, De Clerck H, Tiffany A, Dominguez G, Loua M, Traoré A, Kolié M, Malano ER, Heleze E, Bocquin A, Mély S, Raoul H, Caro V, Cadar D, Gabriel M, Pahlmann M, Tappe D, Schmidt-Chanasit J, Impouma B, Diallo AK, Formenty P, Van Herp M, Günther S |date=October 2014 |title=Emergence of Zaire Ebola Virus Disease in Guinea |url=http://pdfs.semanticscholar.org/2fac/85d09a91e4b0f670afda192af30d9620498b.pdf |url-status=dead |journal=New England Journal of Medicine |volume=371 |issue=15 |pages=1418–1425 |doi=10.1056/NEJMoa1404505 |pmid=24738640 |archive-url=https://web.archive.org/web/20190221224737/http://pdfs.semanticscholar.org/2fac/85d09a91e4b0f670afda192af30d9620498b.pdf |archive-date=21 February 2019 |s2cid=34198809}}</ref><ref name="1st Chain">{{Cite web |name-list-style=vanc |year=2014 |title=The first cases of this Ebola outbreak traced by WHO |url=http://who.int/csr/disease/ebola/ebola-6-months/guinea-chart-big.png?ua=1 |url-status=live |archive-url=https://web.archive.org/web/20141006092047/http://who.int/csr/disease/ebola/ebola-6-months/guinea-chart-big.png?ua=1 |archive-date=6 October 2014 |publisher=[[World Health Organization]] (WHO) |format=png |ref=1st-chain}}</ref> The disease rapidly spread to the neighbouring countries of [[Liberia]] and [[Sierra Leone]]. It was the largest Ebola outbreak ever documented, and the first recorded in the region.<ref name="CDC2014Out" /> On 8 August 2014, the WHO declared the epidemic an international public health emergency. Urging the world to offer aid to the affected regions, its Director-General said, "Countries affected to date simply do not have the capacity to manage an outbreak of this size and complexity on their own. I urge the international community to provide this support on the most urgent basis possible."<ref>{{Cite news |title=WHO raises global alarm over Ebola outbreak |work=CBS News |url=https://www.cbsnews.com/news/ebola-outbreak-international-public-health-emergency-who/ |url-status=live |access-date=2 August 2014 |archive-url=https://web.archive.org/web/20140808095616/http://www.cbsnews.com/news/ebola-outbreak-international-public-health-emergency-who/ |archive-date=8 August 2014 }}</ref> By mid-August 2014, [[Doctors Without Borders]] reported the situation in Liberia's capital, [[Monrovia]], was "catastrophic" and "deteriorating daily". They reported that fears of Ebola among staff members and patients had shut down much of the city's health system, leaving many people without medical treatment for other conditions.<ref name="Common Dreams">{{Cite web | vauthors = Fulton D |date=18 August 2014 |title=In Liberia's Ebola-Stricken Villages, Residents Face 'Stark' Choices |url=http://www.commondreams.org/news/2014/08/18/liberias-ebola-stricken-villages-residents-face-stark-choices |url-status=live |archive-url=https://web.archive.org/web/20140820041111/http://www.commondreams.org/news/2014/08/18/liberias-ebola-stricken-villages-residents-face-stark-choices |archive-date=20 August 2014 |access-date=20 August 2014 |publisher=Common Dreams }}</ref> In a 26 September statement, WHO said, "The Ebola epidemic ravaging parts of West Africa is the most severe acute public health emergency seen in modern times. Never before in recorded history has a [[biosafety level]] four pathogen infected so many people so quickly, over such a broad geographical area, for so long."<ref name="Ebola situation assessment ">{{Cite press release |title=Experimental therapies: growing interest in the use of whole blood or plasma from recovered Ebola patients (convalescent therapies) |date=26 September 2014 |publisher=World Health Organization (WHO) |url=https://www.who.int/mediacentre/news/ebola/26-september-2014/en/ |access-date=28 September 2014 |url-status=dead |archive-url=https://web.archive.org/web/20140928143036/https://www.who.int/mediacentre/news/ebola/26-september-2014/en/ |archive-date=28 September 2014 }}</ref> |
|||
Intense contact tracing and strict isolation largely prevented further spread of the disease in the countries that had imported cases. {{#section:Ebola virus epidemic in West Africa|casesasof}}, {{#section:Ebola virus epidemic in West Africa|cases}} suspected cases and {{#section:Ebola virus epidemic in West Africa|deaths}} deaths were reported;{{#section:Ebola virus epidemic in West Africa|caserefs}}<ref name=":0">{{Cite web |date=2014 |title=2014 Ebola Outbreak in West Africa – Case Counts |url=https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/index.html |url-status=live |archive-url=https://web.archive.org/web/20170806135144/https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/index.html |archive-date=6 August 2017 |publisher=[[Centers for Disease Control and Prevention]] (CDC) }}</ref> however, the WHO said that these numbers may be underestimated.<ref name="Ebola_Outbreak_total_WHO_28_Sept">{{Cite web |date=1 October 2014 |title=Ebola Response Roadmap Situation Report |url=http://apps.who.int/iris/bitstream/10665/135600/1/roadmapsitrep_1Oct2014_eng.pdf?ua=1 |url-status=live |archive-url=https://web.archive.org/web/20141002142707/http://apps.who.int/iris/bitstream/10665/135600/1/roadmapsitrep_1Oct2014_eng.pdf?ua=1 |archive-date=2 October 2014 |publisher=[[World Health Organization]] (WHO) }}</ref> Because they work closely with the body fluids of infected patients, healthcare workers were especially vulnerable to infection; in August 2014, the WHO reported that 10% of the dead were healthcare workers.<ref>{{Cite web |date=25 August 2014 |title=Unprecedented number of medical staff infected with Ebola |url=https://www.who.int/mediacentre/news/ebola/25-august-2014/en/ |url-status=dead |archive-url=https://web.archive.org/web/20140828123825/https://www.who.int/mediacentre/news/ebola/25-august-2014/en/ |archive-date=28 August 2014 |access-date=29 August 2014 |publisher=[[World Health Organization]] (WHO)}}</ref> |
|||
[[File:2014 ebola virus epidemic in West Africa.svg|thumb|upright=1.3|2014 Ebola virus epidemic in West Africa]] |
|||
In September 2014, it was estimated that the countries' capacity for treating Ebola patients was insufficient by the equivalent of 2,122 beds; by December there were a sufficient number of beds to treat and isolate all reported Ebola cases, although the uneven distribution of cases was causing serious shortfalls in some areas.<ref name="WHO2014_12_10">{{Cite web |date=10 December 2014 |title=Ebola response roadmap – Situation report |url=http://apps.who.int/iris/bitstream/10665/145198/1/roadmapsitrep_10Dec2014_eng.pdf?ua=1 |url-status=live |archive-url=https://web.archive.org/web/20141210214551/http://apps.who.int/iris/bitstream/10665/145198/1/roadmapsitrep_10Dec2014_eng.pdf?ua=1 |archive-date=10 December 2014 |access-date=11 December 2014 |publisher=[[World Health Organization]] (WHO) |format=PDF}}</ref> On 28 January 2015, the WHO reported that for the first time since the week ending 29 June 2014, there had been fewer than 100 new confirmed cases reported in a week in the three most-affected countries. The response to the epidemic then moved to a second phase, as the focus shifted from slowing transmission to ending the epidemic.<ref name="World Health Organization">{{Cite web |date=28 January 2015 |title=Ebola Situation Report |url=http://apps.who.int/ebola/en/ebola-situation-report/situation-reports/ebola-situation-report-28-january-2015 |url-status=dead |archive-url=https://web.archive.org/web/20150203214717/http://apps.who.int/ebola/en/ebola-situation-report/situation-reports/ebola-situation-report-28-january-2015 |archive-date=3 February 2015 |access-date=5 February 2015 |publisher=[[World Health Organization]] (WHO) }}</ref> On 8 April 2015, the WHO reported only 30 confirmed cases, the lowest weekly total since the third week of May 2014.<ref name="WHO">{{Cite web |date=8 April 2015 |title=Ebola Situation Report |url=http://apps.who.int/iris/bitstream/10665/161244/1/roadmapsitrep_8Apr2015_eng.pdf?ua=1&ua=1 |url-status=live |archive-url=https://web.archive.org/web/20150414170339/http://apps.who.int/iris/bitstream/10665/161244/1/roadmapsitrep_8Apr2015_eng.pdf?ua=1&ua=1 |archive-date=14 April 2015 |access-date=14 April 2015 |publisher=[[World Health Organization]] (WHO) }}</ref> |
|||
On 29 December 2015, 42 days after the last person tested negative for a second time, Guinea was declared free of Ebola transmission.<ref>{{Cite news |date=29 December 2015 |title=Ebola gone from Guinea |publisher=[[CBC News]] |agency=Thomson Reuters |url=http://www.cbc.ca/news/health/ebola-guinea-1.3382945 |url-status=live |access-date=30 December 2015 |archive-url=https://web.archive.org/web/20151230001240/http://www.cbc.ca/news/health/ebola-guinea-1.3382945 |archive-date=30 December 2015}}</ref> At that time, a 90-day period of heightened surveillance was announced by that agency. "This is the first time that all three countries – Guinea, Liberia and Sierra Leone – have stopped the original chains of transmission ...", the organisation stated in a news release.<ref>{{Cite press release |title=UN declares end to Ebola virus transmission in Guinea; first time all three host countries free |publisher=United Nations |url=https://www.un.org/apps/news/story.asp?NewsID=52913 |access-date=30 December 2015 |url-status=live |archive-url=https://web.archive.org/web/20160101115517/http://www.un.org/apps/news/story.asp?NewsID=52913 |archive-date=1 January 2016 |author=<!-- no by-line. --> |name-list-style=vanc}}</ref> A new case was detected in Sierra Leone on 14 January 2016.<ref>{{Cite web |date=15 January 2016 |title=New Ebola case in Sierra Leone. WHO continues to stress risk of more flare-ups |url=https://www.who.int/mediacentre/news/statements/2016/new-ebola-case/en/ |url-status=live |archive-url=https://web.archive.org/web/20160127143222/https://www.who.int/mediacentre/news/statements/2016/new-ebola-case/en/ |archive-date=27 January 2016 |access-date=25 January 2016 |publisher=[[World Health Organization]] (WHO)}}</ref> However, the outbreak was declared no longer an emergency on 29 March 2016.<ref name="who.int" /> |
|||
====2014 spread outside West Africa==== |
|||
{{main|Ebola virus cases in the United States|Ebola virus disease in Spain|Ebola virus disease in the United Kingdom}} |
|||
On 19 September, Eric Duncan flew from his native Liberia to Texas; five days later he began showing symptoms and visited a hospital but was sent home. His condition worsened and he returned to the hospital on 28 September, where he died on 8 October. Health officials confirmed a diagnosis of Ebola on 30 September – the first case in the United States.<ref>{{Cite news | vauthors = Botelho G, Wilson J |date=8 October 2014 |title=Thomas Eric Duncan: First Ebola death in U.S. |publisher=CNN |url=http://edition.cnn.com/2014/10/08/health/thomas-eric-duncan-ebola/index.html |url-status=live |access-date=8 August 2017 |archive-url=https://web.archive.org/web/20160529040652/http://edition.cnn.com/2014/10/08/health/thomas-eric-duncan-ebola/index.html |archive-date=29 May 2016}}</ref> |
|||
In early October, Teresa Romero, a 44-year-old Spanish nurse, contracted Ebola after caring for a priest who had been repatriated from West Africa. This was the first transmission of the virus to occur outside Africa.<ref>{{Cite web |title=Second US Ebola diagnosis 'deeply concerning', admits CDC chief |url=https://www.msn.com/en-us/news/us/second-us-ebola-diagnosis-deeply-concerning-admits-cdc-chief/ar-BB8UFz0 |url-status=dead |archive-url=https://web.archive.org/web/20141014175544/http://www.msn.com/en-us/news/us/second-us-ebola-diagnosis-deeply-concerning-admits-cdc-chief/ar-BB8UFz0 |archive-date=14 October 2014 |access-date=20 February 2020 |website=[[MSN]]}}archive-url= October 2013</ref> Romero tested negative for the disease on 20 October, suggesting that she may have recovered from Ebola infection.<ref>{{Cite news |date=20 October 2014 |title=Ebola crisis: Tests show Spanish nurse Teresa Romero no longer has the virus |work=ABC News |url=http://www.abc.net.au/news/2014-10-20/spanish-nurse-infected-with-ebola-no-longer-has-virus/5825720 |url-status=live |archive-url=https://web.archive.org/web/20141029201132/http://www.abc.net.au/news/2014-10-20/spanish-nurse-infected-with-ebola-no-longer-has-virus/5825720 |archive-date=29 October 2014 }}</ref> |
|||
On 12 October, the [[Centers for Disease Control and Prevention]] (CDC) confirmed that a nurse in Texas, [[Nina Pham]], who had treated Duncan tested positive for the Ebola virus, the first known case of transmission in the United States.<ref name="NYT-20141012-MF">{{Cite news | vauthors = Fernandez M |date=12 October 2014 |title=Texas Health Worker Tests Positive for Ebola |work=[[The New York Times]] |url=https://www.nytimes.com/2014/10/13/us/texas-health-worker-tests-positive-for-ebola.html |url-status=live |access-date=12 October 2014 |archive-url=https://web.archive.org/web/20141012162113/http://www.nytimes.com/2014/10/13/us/texas-health-worker-tests-positive-for-ebola.html |archive-date=12 October 2014}}</ref> On 15 October, a second Texas health-care worker who had treated Duncan was confirmed to have the virus.<ref name="NBC-ebolaTX" /><ref>{{Cite news |title=Ebola in Texas: Second Health Care Worker Tests Positive |url=https://www.nbcnews.com/storyline/ebola-virus-outbreak/ebola-texas-second-health-care-worker-tests-positive-n226161 |url-status=live |archive-url=https://web.archive.org/web/20141015211852/http://www.nbcnews.com/storyline/ebola-virus-outbreak/ebola-texas-second-health-care-worker-tests-positive-n226161 |archive-date=15 October 2014}}</ref> Both of these people recovered.<ref name="CDC-20142411">{{Cite web |date=22 May 2018 |title=Cases of Ebola Diagnosed in the United States |url=https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/united-states-imported-case.html |url-status=live |archive-url=https://web.archive.org/web/20170226055827/https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/united-states-imported-case.html |archive-date=26 February 2017 }}</ref> An unrelated case involved a doctor in New York City, who returned to the United States from Guinea after working with [[Médecins Sans Frontières]] and tested positive for Ebola on 23 October.<ref>{{Cite news | vauthors = Sanchez R, Prokupecz S |date=23 October 2014 |title=N.Y. doctor positive for Ebola had no symptoms until Thursday, officials say |publisher=CNN |url=http://www.cnn.com/2014/10/23/health/new-york-possible-ebola-case/index.html |url-status=live |access-date=23 October 2014 |archive-url=https://web.archive.org/web/20141024022702/http://www.cnn.com/2014/10/23/health/new-york-possible-ebola-case/index.html?hpt=hp_t1 |archive-date=24 October 2014 }}</ref> The person recovered and was discharged from [[Bellevue Hospital]] on 11 November.<ref name="CDC-20142411" /> On 24 December 2014, a laboratory in [[Atlanta]], Georgia reported that a technician had been exposed to Ebola.<ref>{{Cite news | vauthors = Sun LH, Achenbach J |date=24 December 2014 |title=CDC reports potential Ebola exposure in Atlanta lab |newspaper=[[The Washington Post]] |url=https://www.washingtonpost.com/national/health-science/cdc-reports-potential-ebola-exposure-in-atlanta-lab/2014/12/24/f1a9f26c-8b8e-11e4-8ff4-fb93129c9c8b_story.html |url-status=live |access-date=25 December 2014 |archive-url=https://web.archive.org/web/20141225002131/http://www.washingtonpost.com/national/health-science/cdc-reports-potential-ebola-exposure-in-atlanta-lab/2014/12/24/f1a9f26c-8b8e-11e4-8ff4-fb93129c9c8b_story.html |archive-date=25 December 2014}}</ref> |
|||
On 29 December 2014, [[Pauline Cafferkey]], a British nurse who had just returned to [[Glasgow]] from Sierra Leone, was diagnosed with Ebola at Glasgow's [[Gartnavel General Hospital]].<ref name="BBC-30628349">{{Cite news |date=29 December 2014 |title=Ebola case confirmed in Glasgow hospital |work=BBC News Online |url=https://www.bbc.co.uk/news/uk-scotland-30628349 |url-status=live |archive-url=https://web.archive.org/web/20141229191607/http://www.bbc.co.uk/news/uk-scotland-30628349 |archive-date=29 December 2014}}</ref> After initial treatment in Glasgow, she was transferred by air to [[RAF Northolt]], then to the specialist [[high-level isolation unit]] at the [[Royal Free Hospital]] in [[London]] for longer-term treatment.<ref name="BBC-30629397">{{Cite news |date=30 December 2014 |title=Ebola nurse Pauline Cafferkey transferred to London unit |work=BBC News Online |url=https://www.bbc.com/news/uk-scotland-30629397 |url-status=live |archive-url=https://web.archive.org/web/20141230120858/http://www.bbc.com/news/uk-scotland-30629397 |archive-date=30 December 2014}}</ref> |
|||
=== 2017 Democratic Republic of the Congo === |
|||
{{Main|2017 Democratic Republic of the Congo Ebola virus outbreak}} |
|||
On 11 May 2017, the DRC Ministry of Public Health notified the WHO about an outbreak of Ebola. Four people died, and four people survived; five of these eight cases were laboratory-confirmed. A total of 583 contacts were monitored. On 2 July 2017, the WHO declared the end of the outbreak.<ref>{{Cite web |title=Ebola Epidemiology |url=http://www.ebolavirusnet.com/epidemiology.html |access-date=26 May 2020 |website=www.ebolavirusnet.com |language=en-gb |archive-date=31 May 2020 |archive-url=https://web.archive.org/web/20200531182238/http://ebolavirusnet.com/epidemiology.html |url-status=dead }}</ref> |
|||
=== 2018 Équateur province === |
|||
{{Main|2018 Équateur province Ebola outbreak}} |
|||
On 14 May 2018, the World Health Organization reported that "the Democratic Republic of Congo reported 39 suspected, probable or confirmed cases of Ebola between 4 April and 13 May, including 19 deaths."<ref name="first 2018 DRC outbreak report">{{Cite web |title=WHO says 19 dead, 39 infected so far in Congo Ebola outbreak |url=https://www.msn.com/en-us/health/medical/who-says-19-dead-39-infected-so-far-in-congo-ebola-outbreak/ar-AAxfhX9?ocid=ientp |access-date=14 May 2018 |publisher=MSN |archive-date=15 May 2018 |archive-url=https://web.archive.org/web/20180515043721/http://www.msn.com/en-us/health/medical/who-says-19-dead-39-infected-so-far-in-congo-ebola-outbreak/ar-AAxfhX9?ocid=ientp |url-status=live }}</ref> Some 393 people identified as contacts of Ebola patients were being followed up. The outbreak centred on the [[Bikoro]], Iboko, and [[Wangata]] areas in [[Equateur]] province,<ref name="first 2018 DRC outbreak report" /> including in the large city of [[Mbandaka]]. The DRC Ministry of Public Health approved the use of an experimental vaccine.<ref>{{Cite web |title=WHO planning for 'worst case scenario' over DRC Ebola outbreak |url=https://www.aljazeera.com/news/2018/05/planning-worst-case-scenario-drc-ebola-outbreak-180511153458973.html |access-date=14 May 2018 |publisher=[[Al Jazeera English|Al Jazeera]] |archive-date=13 May 2018 |archive-url=https://web.archive.org/web/20180513214320/https://www.aljazeera.com/news/2018/05/planning-worst-case-scenario-drc-ebola-outbreak-180511153458973.html |url-status=live }}</ref><ref>{{Cite web |title=19 dead in latest Congo Ebola outbreak: WHO |url=https://www.reuters.com/video/2018/05/14/19-dead-in-latest-congo-ebola-outbreak-w?videoId=426863714&videoChannel=118261 |access-date=14 May 2018 |website=[[Reuters]] |archive-date=15 May 2018 |archive-url=https://web.archive.org/web/20180515112141/https://www.reuters.com/video/2018/05/14/19-dead-in-latest-congo-ebola-outbreak-w?videoId=426863714&videoChannel=118261 |url-status=live }}</ref><ref>{{Cite news |date=14 May 2018 |title=Update 1 – WHO gets approval to use Ebola vaccine in Democratic… |work=Reuters |url=https://www.reuters.com/article/health-ebola-who/update-1-who-gets-approval-to-use-ebola-vaccine-in-democratic-republic-of-congo-idUSL5N1SL554 |access-date=5 August 2018 |archive-date=5 August 2018 |archive-url=https://web.archive.org/web/20180805082726/https://www.reuters.com/article/health-ebola-who/update-1-who-gets-approval-to-use-ebola-vaccine-in-democratic-republic-of-congo-idUSL5N1SL554 |url-status=live }}</ref> On 13 May 2018, WHO Director-General [[Tedros Adhanom Ghebreyesus]] visited Bikoro.<ref>{{Cite web |title=WHO Director General visits Ebola-affected areas in DR Congo |url=https://www.who.int/news-room/detail/13-05-2018-who-director-general-visits-ebola-affected-areas-in-dr-congo |access-date=14 May 2018 |publisher=[[World Health Organization]] (WHO) |archive-date=10 September 2020 |archive-url=https://web.archive.org/web/20200910190735/https://www.who.int/news-room/detail/13-05-2018-who-director-general-visits-ebola-affected-areas-in-dr-congo |url-status=live }}</ref> Reports emerged that maps of the area were inaccurate, not so much hampering medical providers as [[epidemiologist]]s and officials trying to assess the outbreak and containment efforts.<ref>{{Cite web |vauthors=Yong E |date=21 May 2018 |title=Most Maps of the New Ebola Outbreak Are Wrong: Villages, and sometimes whole regions of the Congo, are misplaced – but the ministry of health and a team of cartographers are racing to get better data |url=https://www.theatlantic.com/health/archive/2018/05/most-maps-of-the-new-ebola-outbreak-are-wrong/560777/ |website=[[The Atlantic]] |access-date=26 May 2018 |archive-date=30 July 2020 |archive-url=https://web.archive.org/web/20200730225018/https://www.theatlantic.com/health/archive/2018/05/most-maps-of-the-new-ebola-outbreak-are-wrong/560777/ |url-status=live }}</ref> The 2018 outbreak in the DRC was declared over on 24 July 2018.<ref name=WHO2018DRCOver/> |
|||
=== 2018–2020 Kivu === |
|||
{{Main|Kivu Ebola epidemic}} |
|||
On 1 August 2018, the world's 10th Ebola outbreak was declared in [[North Kivu]] province of the Democratic Republic of the Congo. It was the first Ebola outbreak in a military conflict zone, with thousands of refugees in the area.<ref>{{Cite news |vauthors=Beaubien J |date=2 August 2018 |title=Ebola In A Conflict Zone |work=NPR |publisher=[[National Public Radio]] (NPR) |url=https://www.npr.org/sections/goatsandsoda/2018/08/02/635016034/ebola-in-a-conflict-zone |access-date=5 August 2018 |archive-date=5 August 2018 |archive-url=https://web.archive.org/web/20180805074044/https://www.npr.org/sections/goatsandsoda/2018/08/02/635016034/ebola-in-a-conflict-zone |url-status=live }}</ref><ref>{{Cite news |vauthors=Specia M |date=2 August 2018 |title=The Latest Ebola Outbreak Is Centered in a War Zone |work=The New York Times |url=https://www.nytimes.com/2018/08/02/world/africa/ebola-outbreak-congo-war-zone.html |access-date=5 August 2018 |archive-date=4 August 2018 |archive-url=https://web.archive.org/web/20180804143145/https://www.nytimes.com/2018/08/02/world/africa/ebola-outbreak-congo-war-zone.html |url-status=live }}</ref> By November 2018, nearly 200 Congolese had died of Ebola, about half of them from the city of [[Beni, Democratic Republic of the Congo|Beni]], where armed groups are fighting over the region's mineral wealth, impeding medical relief efforts.<ref>{{Cite web |date=13 November 2018 |title=DRC: Ebola Outbreak Worst in Country's History, Kills Almost 200 |url=https://www.democracynow.org/2018/11/13/headlines/drc_ebola_outbreak_worst_in_countrys_history_kills_almost_200 |access-date=14 November 2018 |publisher=Democracy Now |archive-date=13 November 2018 |archive-url=https://web.archive.org/web/20181113195520/https://www.democracynow.org/2018/11/13/headlines/drc_ebola_outbreak_worst_in_countrys_history_kills_almost_200 |url-status=live }}</ref> |
|||
By March 2019, this became the second largest Ebola outbreak ever recorded, with more than 1,000 cases and insecurity continuing to be the major resistance to providing an adequate response.<ref name="CDC24March2019">{{Cite press release |title=Ebola outbreak in eastern Democratic Republic of Congo tops 1,000 cases |date=29 March 2019 |publisher=[[Centers for Disease Control and Prevention]] (CDC) |url=https://www.cdc.gov/media/releases/2019/s0322-ebola-congo.html |access-date=12 May 2019 |archive-date=15 June 2019 |archive-url=https://web.archive.org/web/20190615140028/https://www.cdc.gov/media/releases/2019/s0322-ebola-congo.html |url-status=live }}</ref><ref name="WHOMay2019">{{Cite web |title=Ebola virus disease – Democratic Republic of the Congo |url=https://www.who.int/csr/don/02-may-2019-ebola-drc/en/ |url-status=dead |archive-url=https://web.archive.org/web/20190505054446/https://www.who.int/csr/don/02-may-2019-ebola-drc/en/ |archive-date=5 May 2019 |access-date=12 May 2019 |publisher=[[World Health Organization]] (WHO)}}</ref> {{As of|2019|6|4}}, the WHO reported 2025 confirmed and probable cases with 1357 deaths.<ref>{{Cite web |date=6 June 2019 |title=Ebola virus disease – Democratic Republic of the Congo – Disease outbreak news: Update 6 June 2019 |url=https://www.who.int/csr/don/06-june-2019-ebola-drc/en/ |archive-url=https://web.archive.org/web/20190607113738/https://www.who.int/csr/don/06-june-2019-ebola-drc/en/ |archive-date=7 June 2019 |access-date=7 June 2019 |publisher=[[World Health Organization]] (WHO)}}</ref> In June 2019, two people died of Ebola in neighbouring [[Uganda]].<ref>{{Cite news |date=13 June 2019 |title=Ebola outbreak: Grandmother dies in Uganda |work=[[BBC News Online]] |url=https://www.bbc.co.uk/news/world-africa-48622635 |access-date=15 June 2019 |archive-date=14 June 2019 |archive-url=https://web.archive.org/web/20190614131151/https://www.bbc.co.uk/news/world-africa-48622635 |url-status=live }}</ref> |
|||
In July 2019, an infected man travelled to [[Goma]], home to more than two million people.<ref>{{Cite web |vauthors=Larson K |date=15 July 2019 |title=Congo tracing contacts of first Ebola case in eastern city |url=https://apnews.com/7ae99b8b4e414467b9139abde98684ee |access-date=17 July 2019 |website=AP News |archive-date=16 July 2019 |archive-url=https://web.archive.org/web/20190716160349/https://apnews.com/7ae99b8b4e414467b9139abde98684ee |url-status=live }}</ref> One week later, on 17 July 2019, the WHO declared the Ebola outbreak a [[Public Health Emergency of International Concern|global health emergency]], the fifth time such a declaration has been made by the organisation.<ref>{{Cite web |vauthors=Cheng M, Keaten J |date=17 July 2019 |title=Ebola outbreak in Congo declared a global health emergency |url=https://apnews.com/204fc739fc5846cdba4093ee65c4f7db |access-date=17 July 2019 |website=AP News |archive-date=17 July 2019 |archive-url=https://web.archive.org/web/20190717200951/https://apnews.com/204fc739fc5846cdba4093ee65c4f7db |url-status=live }}</ref> A government spokesman said that half of the Ebola cases are unidentified, and he added that the current outbreak could last up to three years.<ref>{{Cite news |date=2 August 2019 |title=Half of Ebola cases in DR Congo 'unidentified' |work=BBC News Online |url=https://www.bbc.com/news/world-africa-49212116 |access-date=3 August 2019 |archive-date=3 August 2019 |archive-url=https://web.archive.org/web/20190803001148/https://www.bbc.com/news/world-africa-49212116 |url-status=live }}</ref> |
|||
On 25 June 2020, the second biggest EVD outbreak ever was declared over.<ref name="finish">{{Cite web |date=25 June 2020 |title=DR Congo's deadliest Ebola outbreak declared over |url=https://www.bbc.com/news/world-africa-53179323 |access-date=25 June 2020 |website=BBC News |archive-date=31 December 2020 |archive-url=https://web.archive.org/web/20201231180943/https://www.bbc.com/news/world-africa-53179323 |url-status=live }}</ref> |
|||
=== 2020 Équateur province === |
|||
On 1 June 2020, the Congolese health ministry announced a new DRC outbreak of Ebola in [[Mbandaka]], [[Équateur Province]], a region along the Congo River. Genome sequencing suggests that this outbreak, the 11th outbreak since the virus was first discovered in the country in 1976, is unrelated to the one in North Kivu Province or the previous outbreak in the same area in 2018. It was reported that six cases had been identified; four of the people had died. It is expected that more people will be identified as surveillance activities increase.<ref>{{Cite web |date=5 June 2020 |title=Ebola virus disease case in Equateur Province, DRC is a new spillover |url=https://virological.org/t/ebola-virus-disease-case-in-equateur-province-drc-is-a-new-spillover/504 |access-date=8 June 2020 |website=Virological.org |archive-date=8 June 2020 |archive-url=https://web.archive.org/web/20200608145842/https://virological.org/t/ebola-virus-disease-case-in-equateur-province-drc-is-a-new-spillover/504 |url-status=live }}</ref> By 15 June the case count had increased to 17 with 11 deaths, with more than 2,500 people having been vaccinated.<ref>{{Cite web |title=17 infected, 11 dead in new Ebola outbreak in DR Congo |url=https://www.aljazeera.com/news/2020/06/17-infected-11-dead-ebola-outbreak-dr-congo-200615112609457.html |access-date=15 June 2020 |website=www.aljazeera.com |archive-date=15 June 2020 |archive-url=https://web.archive.org/web/20200615123300/https://www.aljazeera.com/news/2020/06/17-infected-11-dead-ebola-outbreak-dr-congo-200615112609457.html |url-status=live }}</ref> The 11th EVD outbreak was officially declared over on 19 November 2020.<ref>{{Cite web |date=19 November 2020 |title=Democratic Republic of the Congo declares the end to its 11th Ebola outbreak |url=https://edition.cnn.com/2020/11/18/health/drc-ebola-outbreak-over-intl-hnk/index.html |access-date=19 November 2020 |website=www.cnn.com |archive-date=19 November 2020 |archive-url=https://web.archive.org/web/20201119032337/https://edition.cnn.com/2020/11/18/health/drc-ebola-outbreak-over-intl-hnk/index.html |url-status=live }}</ref> By the time the Équateur outbreak ended, it had 130 confirmed cases with 75 recoveries and 55 deaths. |
|||
=== 2021 === |
|||
==== North Kivu ==== |
|||
On 7 February 2021, the Congolese health ministry announced a new case of Ebola near Butembo, North Kivu detected a day before. The case was a 42-year-old woman who had symptoms of Ebola in Biena on 1 February 2021. A few days after, she died in a hospital in Butembo. The WHO said that more than 70 people with contact with the woman had been tracked.<ref>{{Cite web |title=New Ebola case detected in eastern DRC |url=https://www.aljazeera.com/news/2021/2/7/new-ebola-case-detected-in-eastern-dr-congo-health-ministry |access-date=17 February 2021 |website=www.aljazeera.com |language=en |archive-date=16 February 2021 |archive-url=https://web.archive.org/web/20210216115744/https://www.aljazeera.com/news/2021/2/7/new-ebola-case-detected-in-eastern-dr-congo-health-ministry |url-status=live }}</ref><ref name=":2">{{Cite web |date=15 February 2021 |title=Outbreak of Ebola virus disease in North Kivu – Democratic Republic of the Congo – 2021 |url=https://www.ecdc.europa.eu/en/news-events/outbreak-ebola-virus-disease-north-kivu-democratic-republic-congo-2021 |access-date=17 February 2021 |website=European Centre for Disease Prevention and Control |language=en |archive-date=17 February 2021 |archive-url=https://web.archive.org/web/20210217000744/https://www.ecdc.europa.eu/en/news-events/outbreak-ebola-virus-disease-north-kivu-democratic-republic-congo-2021 |url-status=live }}</ref> |
|||
On 11 February 2021, another woman who had contact with the previous woman died in the same town, and the number of traced contacts increased to 100.<ref>{{Cite web |title=DRC confirms two Ebola deaths in resurgence of outbreak |url=https://www.aljazeera.com/news/2021/2/11/drc-confirms-two-ebola-deaths-in-resurgence-of-outbreak |access-date=17 February 2021 |website=www.aljazeera.com |language=en |archive-date=17 February 2021 |archive-url=https://web.archive.org/web/20210217020551/https://www.aljazeera.com/news/2021/2/11/drc-confirms-two-ebola-deaths-in-resurgence-of-outbreak |url-status=live }}</ref> A day after, a third case was detected in Butembo.<ref>{{Cite web |title=DRC confirms third Ebola case in North Kivu province |url=https://www.aljazeera.com/news/2021/2/12/drc-confirms-third-ebola-case-in-north-kivu-province |access-date=17 February 2021 |website=www.aljazeera.com |language=en |archive-date=17 February 2021 |archive-url=https://web.archive.org/web/20210217135406/https://www.aljazeera.com/news/2021/2/12/drc-confirms-third-ebola-case-in-north-kivu-province |url-status=live }}</ref> |
|||
On 3 May 2021, the 12th EVD outbreak was declared over, resulting in 12 cases and six deaths.<ref name=":3">{{Cite web |date=7 May 2021 |title=Communicable Disease Threats Report |url=https://www.ecdc.europa.eu/sites/default/files/documents/Communicable-disease-threats-report-8-may-2021.pdf |access-date=10 May 2021 |website=[[European Centre for Disease Prevention and Control]] |archive-date=7 May 2021 |archive-url=https://web.archive.org/web/20210507225232/https://www.ecdc.europa.eu/sites/default/files/documents/Communicable-disease-threats-report-8-may-2021.pdf |url-status=live }}</ref><ref>{{Cite web |date=3 May 2021 |title=Latest deadly Ebola virus outbreak in DR Congo declared over |url=https://news.un.org/en/story/2021/05/1091162 |access-date=10 May 2021 |website=UN News |language=en |archive-date=10 May 2021 |archive-url=https://web.archive.org/web/20210510014805/https://news.un.org/en/story/2021/05/1091162 |url-status=live }}</ref> Heightened surveillance will continue for 90 days after the declaration, in case of resurgence.<ref name=":3" /> |
|||
==== Guinea ==== |
|||
In February 2021, Sakoba Keita, head of Guinea's national health agency confirmed that three people had died of Ebola in the south-eastern region near the city of Nzérékoré. A further five people also tested positive. Keita also confirmed more testing was underway, and attempts to trace and isolate further cases had begun.<ref>{{Cite web |date=14 February 2021 |title=Guinea records first Ebola deaths since 2016 |url=https://www.bbc.co.uk/news/world-africa-56060728 |access-date=14 February 2021 |website=BBC News |archive-date=14 February 2021 |archive-url=https://web.archive.org/web/20210214104857/https://www.bbc.co.uk/news/world-africa-56060728 |url-status=live }}</ref> On 14 February, the Guinean government declared an Ebola epidemic.<ref>{{Cite web |title=Guinea declares Ebola epidemic after three deaths |url=https://www.aljazeera.com/news/2021/2/14/guinea-sees-first-ebola-deaths-since-2016 |access-date=15 February 2021 |website=www.aljazeera.com |language=en |archive-date=14 February 2021 |archive-url=https://web.archive.org/web/20210214201904/https://www.aljazeera.com/news/2021/2/14/guinea-sees-first-ebola-deaths-since-2016 |url-status=live }}</ref> The outbreak may have started following reactivation of a [[viral latency|latent case]] in a survivor of an earlier outbreak.<ref name="KuperschmidtReactivation">{{Cite journal |vauthors=Kupferschmidt, K |date=March 2021 |title=Ebola virus may lurk in survivors for many years |journal=Science |volume=371 |issue=6535 |pages=1188 |bibcode=2021Sci...371.1188K |doi=10.1126/science.371.6535.1188 |issn=0036-8075 |pmid=33737465 |s2cid=232303082}}</ref><ref name="VirologicalKeitaGuinea21">{{Cite web |vauthors=Keita AK, Düx A, Diallo H, Calvignac-Spencer S, Sow MS, Keita MB, Sidibe Y, Ayouba A, Lemarcis F, Marí Saéz A |display-authors=6 |date=12 March 2021 |title=Resurgence of Ebola virus in Guinea after 5 years calls for careful attention to survivors without creating further stigmatization |url=https://virological.org/t/guinea-2021-ebov-genomes/651 |access-date=23 March 2021 |website=virological.org |language=en |archive-date=25 March 2021 |archive-url=https://web.archive.org/web/20210325051915/https://virological.org/t/guinea-2021-ebov-genomes/651 |url-status=live }}</ref> As of 4 May 2021, 23 cases were reported, with no new cases or deaths since 3 April 2021.<ref name=":3" /> A 42-day countdown period was started on 8 May 2021, and on 19 June, the outbreak was declared over.<ref name=":3" /><ref>{{Cite tweet |number=1406227793281757189 |user=WHOAFRO |title=The #Ebola outbreak in #Guinea was declared over today! Here is a look back at the hard work of communities, health workers, partners & Guinea's health authorities to bring this outbreak to an end while also fighting #COVID19.}}</ref> |
|||
==== Ivory Coast ==== |
|||
On 14 August 2021, The Ministry of Health of [[Cote d’Ivoire]] confirmed the country's first case of Ebola since 1994. This came after the Institut Pasteur in Cote d'Ivoire confirmed the Ebola Virus Disease in samples collected from a patient, who was hospitalized in the commercial capital of [[Abidjan]], after arriving from Guinea.<ref>{{Cite web |date=14 August 2021 |title=Cote d'Ivoire declares first Ebola outbreak in more than 25 years |url=https://www.afro.who.int/news/cote-divoire-declares-first-ebola-outbreak-more-25-years |access-date=15 August 2021 |website=afro.who.int |archive-date=15 August 2021 |archive-url=https://web.archive.org/web/20210815012621/https://www.afro.who.int/news/cote-divoire-declares-first-ebola-outbreak-more-25-years |url-status=live }}</ref> |
|||
However, on 31 August 2021, the WHO found that, after further tests in a laboratory in [[Lyon]], the patient did not have Ebola. The cause of her disease is still being analyzed.<ref>{{Cite web |title=New test finds no evidence of Ebola virus in Cote d'Ivoire case |url=https://www.afro.who.int/news/new-test-finds-no-evidence-ebola-virus-cote-divoire-case |access-date=3 October 2021 |website=WHO {{!}} Regional Office for Africa |language=en |archive-date=3 October 2021 |archive-url=https://web.archive.org/web/20211003083053/https://www.afro.who.int/news/new-test-finds-no-evidence-ebola-virus-cote-divoire-case |url-status=live }}</ref> |
|||
=== 2022 === |
|||
On 23 April 2022, a case of Ebola was confirmed in the DRC in the Equateur province. The case was a 31-year-old man whose symptoms began on 5 April, but did not seek treatment for over a week. On 21 April, he was admitted to an Ebola treatment centre and died later that day.<ref>{{Cite web |date=23 April 2022 |title=New case of Ebola hemorrhagic fever found in DR Congo |url=https://www.aljazeera.com/news/2022/4/23/new-case-of-ebola-hemorrhagic-fever-found-in-dr-congo |access-date=24 April 2022 |website=[[Al Jazeera English|Al Jazeera]] |language=en |archive-date=24 April 2022 |archive-url=https://web.archive.org/web/20220424024753/https://www.aljazeera.com/news/2022/4/23/new-case-of-ebola-hemorrhagic-fever-found-in-dr-congo |url-status=live }}</ref> By 24 May 2022, there were 5 recorded deaths in the DRC.<ref>{{Cite web |date=24 May 2022 |title=All reported DR Congo Ebola patients dead: WHO |url=https://gazettengr.com/all-reported-dr-congo-ebola-patients-dead-who/ |access-date=25 May 2022 |website=[[Peoples Gazette]] |archive-date=25 May 2022 |archive-url=https://web.archive.org/web/20220525095616/https://gazettengr.com/all-reported-dr-congo-ebola-patients-dead-who/ |url-status=live }}</ref> On 15 August, the fifth case was buried, and the outbreak was declared over, 42 days after, on 4 July 2022.<ref>{{Citation |title=Ebola virus disease – Democratic Republic of the Congo |date=4 July 2022 |url=https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON398 |work=[[World Health Organization]] |language=en |access-date=15 September 2022 |archive-date=22 September 2022 |archive-url=https://web.archive.org/web/20220922205524/https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON398 |url-status=live }}</ref> |
|||
In September 2022, [[2022 Uganda Ebola outbreak|Uganda reported 7 cases infected with the Ebola Sudan strain]],<ref>{{Cite news |vauthors=Biryabarema E |date=22 September 2022 |title=Uganda has confirmed seven Ebola cases so far, one death |language=en |work=Reuters |url=https://www.reuters.com/world/africa/uganda-ebola-cases-stand-seven-so-far-2022-09-22/ |access-date=23 September 2022 |archive-date=27 September 2022 |archive-url=https://web.archive.org/web/20220927171151/https://www.reuters.com/world/africa/uganda-ebola-cases-stand-seven-so-far-2022-09-22/ |url-status=live }}</ref> but by mid-October the count had increased to 63.<ref>{{Cite web |date=10 October 2022 |title=Uganda is battling Ebola again – and the world doesn't have a vaccine {{!}} Devi Sridhar |url=https://www.theguardian.com/commentisfree/2022/oct/10/uganda-ebola-vaccine |access-date=12 October 2022 |website=the Guardian |language=en |archive-date=10 October 2022 |archive-url=https://web.archive.org/web/20221010155732/https://www.theguardian.com/commentisfree/2022/oct/10/uganda-ebola-vaccine |url-status=live }}</ref> |
|||
In November 2022, the outbreak in Uganda continued - still without a vaccine.<ref name="Guiliani 2022" /> On 10 January 2023, the outbreak was considered over after no new cases had been reported for 42 days; the outbreak killed nearly 80 people.<ref>{{Cite web |date=10 January 2023 |title=Ebola outbreak in Uganda declared over |url=https://bnonews.com/index.php/2023/01/ebola-outbreak-in-uganda-declared-over/ |access-date=12 January 2023 |website=BNO News |language=en-US |archive-date=26 March 2023 |archive-url=https://web.archive.org/web/20230326170025/https://bnonews.com/index.php/2023/01/ebola-outbreak-in-uganda-declared-over/ |url-status=live }}</ref> |
|||
==Society and culture== |
==Society and culture== |
||
{{see also|Cultural effects of the Ebola crisis}} |
|||
Given the lethal nature of Ebola, and since no approved [[vaccine]] or treatment is available, it is classified as a [[Biosafety level#Levels|biosafety level 4]] agent, as well as a [[Bioterrorism#Category A agents|Category A bioterrorism]] agent by the Centers for Disease Control and Prevention. It has the potential to be weaponized for use in [[biological warfare]].<ref name="pmid11988060">{{cite journal | author = Borio L, Inglesby T, Peters CJ, Schmaljohn AL, Hughes JM, Jahrling PB, Ksiazek T, Johnson KM, Meyerhoff A, O'Toole T, Ascher MS, Bartlett J, Breman JG, Eitzen EM, Hamburg M, Hauer J, Henderson DA, Johnson RT, Kwik G, Layton M, Lillibridge S, Nabel GJ, Osterholm MT, Perl TM, Russell P, Tonat K | title = Hemorrhagic fever viruses as biological weapons: medical and public health management | journal = Journal of the American Medical Association | volume = 287 | issue = 18 | pages = 2391–405 | year = 2002 | pmid = 11988060 | doi = 10.1001/jama.287.18.2391 }}</ref><ref>{{cite journal | author = Salvaggio MR, Baddley JW | title = Other viral bioweapons: Ebola and Marburg hemorrhagic fever | journal = Dermatologic clinics | volume = 22 | issue = 3 | pages = 291–302, vi | year = 2004 | pmid = 15207310 | doi = 10.1016/j.det.2004.03.003 }}</ref> |
|||
===Weaponisation=== |
|||
''Ebolavirus'' is classified as a [[Biosafety level#Levels|biosafety level 4]] agent, as well as a [[Bioterrorism#Category A|Category A bioterrorism]] agent by the Centers for Disease Control and Prevention.<ref name="Ansari2014" /><ref name="MacNeil2012">{{Cite journal |vauthors=MacNeil A, Rollin PE |date=June 2012 |title=Ebola and Marburg hemorrhagic fevers: neglected tropical diseases? |journal=PLOS Negl Trop Dis |volume=6 |issue=6 |pages=e1546 |doi=10.1371/journal.pntd.0001546 |pmc=3385614 |pmid=22761967 |doi-access=free }}</ref> It has the potential to be weaponised for use in [[biological warfare]],<ref name="pmid11988060">{{Cite journal |display-authors=6 |vauthors=Borio L, Inglesby T, Peters CJ, Schmaljohn AL, Hughes JM, Jahrling PB, Ksiazek T, Johnson KM, Meyerhoff A, O'Toole T, Ascher MS, Bartlett J, Breman JG, Eitzen EM, Hamburg M, Hauer J, Henderson DA, Johnson RT, Kwik G, Layton M, Lillibridge S, Nabel GJ, Osterholm MT, Perl TM, Russell P, Tonat K |date=May 2002 |title=Hemorrhagic fever viruses as biological weapons: medical and public health management |journal=Journal of the American Medical Association |volume=287 |issue=18 |pages=2391–405 |doi=10.1001/jama.287.18.2391 |pmid=11988060}}</ref><ref>{{Cite journal |vauthors=Salvaggio MR, Baddley JW |date=July 2004 |title=Other viral bioweapons: Ebola and Marburg hemorrhagic fever |journal=Dermatologic Clinics |volume=22 |issue=3 |pages=291–302, vi |doi=10.1016/j.det.2004.03.003 |pmid=15207310}}</ref> and was investigated by [[Biopreparat]] for such use, but might be difficult to prepare as a [[weapon of mass destruction]] because the virus becomes ineffective quickly in open air.<ref name="Zubray">{{Cite book | vauthors = Zubray G |url=https://books.google.com/books?id=AwkVgNPRnKoC&pg=PA73 |title=Agents of Bioterrorism: Pathogens and Their Weaponization |publisher=Columbia University Press |year=2013 |isbn=978-0231518130 |location=New York |pages=73–74 |archive-url=https://web.archive.org/web/20160504004715/https://books.google.com/books?id=AwkVgNPRnKoC&pg=PA73 |archive-date=4 May 2016 |url-status=live |name-list-style=vanc }}</ref> Fake emails pretending to be Ebola information from the WHO or the Mexican government have, in 2014, been misused to spread computer malware.<ref>{{Cite web |date=24 October 2014 |title=Malicious Ebola-Themed Emails Are on the Rise |url=http://bits.blogs.nytimes.com/2014/10/24/malicious-ebola-themed-emails-are-on-the-rise/ |url-status=live |archive-url=https://web.archive.org/web/20170707125209/https://bits.blogs.nytimes.com/2014/10/24/malicious-ebola-themed-emails-are-on-the-rise/?action=click&contentCollection=US%20Open®ion=Article&module=Promotron |archive-date=7 July 2017 |access-date=26 October 2014 |website=The New York Times }}</ref> The BBC reported in 2015 that "North Korean state media has suggested the disease was created by the U.S. military as a biological weapon."<ref>{{Cite news |date=23 February 2015 |title=North Korea bans foreigners from Pyongyang marathon over Ebola |work=BBC News Online |url=https://www.bbc.com/news/world-asia-31581935 |url-status=live |access-date=23 February 2015 |archive-url=https://web.archive.org/web/20150224061401/http://www.bbc.com/news/world-asia-31581935 |archive-date=24 February 2015}}</ref> |
|||
===Literature=== |
|||
[[Richard Preston]]'s 1995 [[best-selling]] book, ''[[The Hot Zone]]'', dramatised the Ebola outbreak in Reston, Virginia.<ref>{{Cite book | vauthors = Preston R |url=https://books.google.com/books?id=E6BKpf2tSkoC |title=The Hot Zone, A Terrifying True Story |publisher=Anchor Books |year=1995 |isbn=978-0385479561 |oclc=32052009 |author-link=Richard Preston |archive-url=https://web.archive.org/web/20160513222825/https://books.google.com/books?id=E6BKpf2tSkoC |archive-date=13 May 2016 |url-status=live }}</ref><ref>{{Cite news |date=4 June 1995 |title=Best Sellers: 4 June 1995 |work=[[The New York Times Book Review]] |url=https://www.nytimes.com/1995/06/04/books/best-sellers-june-4-1995.html |access-date=10 September 2014 |archive-date=8 October 2014 |archive-url=https://web.archive.org/web/20141008122652/http://www.nytimes.com/1995/06/04/books/best-sellers-june-4-1995.html |url-status=live }}</ref><ref>{{Cite web |title=About The Hot Zone |url= http://www.randomhouse.com/features/richardpreston/bookshelf/hz.html |url-status=dead |archive-url= https://web.archive.org/web/20141007011934/http://www.randomhouse.com/features/richardpreston/bookshelf/hz.html |archive-date=7 October 2014 |access-date=10 September 2014 |publisher=Random House}}</ref> |
|||
[[William Close]]'s 1995 ''Ebola: A Documentary Novel of Its First Explosion''<ref>{{Cite book | vauthors = Close WT |url=https://archive.org/details/eboladocumentary00clos |title=Ebola: A Documentary Novel of Its First Explosion |publisher=[[Ivy Books]] |year=1995 |isbn=978-0804114325 |location=New York |oclc=32753758 |author-link=William Close |url-access=registration}}</ref><ref>{{Cite web | vauthors = Grove R |date=2 June 2006 |title=More about the people than the virus |url=https://www.amazon.com/Ebola-documentary-novel-first-explosion/dp/B007HEJSE6 |url-status=live |archive-url=https://web.archive.org/web/20141021075254/http://www.amazon.com/Ebola-documentary-novel-first-explosion/dp/B007HEJSE6 |archive-date=21 October 2014 |access-date=17 September 2014 |website=Review of Close, William T., Ebola: A Documentary Novel of Its First Explosion}}</ref> and 2002 ''Ebola: Through the Eyes of the People'' focused on individuals' reactions to the 1976 Ebola outbreak in Zaire.<ref>{{Cite book | vauthors = Close WT |url=https://books.google.com/books?id=BX0gAQAAIAAJ |title=Ebola: Through the Eyes of the People |publisher=Meadowlark Springs Productions |year=2002 |isbn=978-0970337115 |location=Marbleton, Wyoming |oclc=49193962 |author-link=William Close |archive-url=https://web.archive.org/web/20160617210838/https://books.google.com/books?id=BX0gAQAAIAAJ |archive-date=17 June 2016 |url-status=live}}</ref><ref>{{Cite web | vauthors = Pink B |date=24 June 2008 |title=A fascinating perspective |url=https://www.amazon.com/Ebola-Through-William-T-Close/product-reviews/0970337116 |url-status=live |archive-url=https://web.archive.org/web/20141021075312/http://www.amazon.com/Ebola-Through-William-T-Close/product-reviews/0970337116 |archive-date=21 October 2014 |access-date=17 September 2014 |website=Review of Close, William T., Ebola: Through the Eyes of the People}}</ref> |
|||
[[Tom Clancy]]'s 1996 novel, ''[[Executive Orders]]'', involves a [[Middle East]]ern terrorist attack on the United States using an airborne form of a deadly Ebola virus strain named "Ebola Mayinga" (see [[Mayinga N'Seka]]).<ref>{{Cite book | vauthors = Clancy T |url=https://archive.org/details/executiveorders00clan |title=Executive Orders |publisher=Putnam |year=1996 |isbn=978-0399142185 |location=New York |oclc=34878804 |author-link=Tom Clancy |url-access=registration}}</ref><ref>{{Cite news | vauthors = Stone O |author-link=Oliver Stone |date=2 September 1996 |title=Who's That in the Oval Office? |work=The New York Times |url=https://www.nytimes.com/books/97/08/17/bsp/20141.html |access-date=10 September 2014 |archive-url=https://web.archive.org/web/20090410091107/http://www.nytimes.com/books/97/08/17/bsp/20141.html |archive-date=10 April 2009}}</ref> |
|||
As the Ebola virus epidemic in West Africa developed in 2014, a number of popular self-published and well-reviewed books containing sensational and misleading information about the disease appeared in electronic and printed formats. The authors of some such books admitted that they lacked medical credentials and were not technically qualified to give medical advice. The World Health Organization and the United Nations stated that such misinformation had contributed to the spread of the disease.<ref>{{Cite news | vauthors = Dewey C |date=2 October 2014 |title=Popular on Amazon: Wildly misleading self-published books about Ebola, by random people without medical degrees |newspaper=[[The Washington Post]] |url=https://www.washingtonpost.com/news/the-intersect/wp/2014/10/02/popular-on-amazon-wildly-misleading-self-published-books-about-ebola-by-random-people-without-medical-degrees/ |url-status=live |access-date=27 October 2014 |archive-url=https://web.archive.org/web/20141022174054/http://www.washingtonpost.com/news/the-intersect/wp/2014/10/02/popular-on-amazon-wildly-misleading-self-published-books-about-ebola-by-random-people-without-medical-degrees/ |archive-date=22 October 2014}}</ref> |
|||
==Other animals== |
==Other animals== |
||
===Wild animals=== |
|||
In general, outbreaks of EVD among human populations result from handling infected wild animal carcasses. In general, declines in animal populations precede outbreaks among human populations. Since 2003, such declines have been monitored through surveillance of animal populations with the aim of predicting and preventing EVD outbreaks in humans.<ref name="Cite pmid|15752448">{{cite journal | author = Rouquet P, Froment JM, Bermejo M, Kilbourn A, Karesh W, Reed P, Kumulungui B, Yaba P, Délicat A, Rollin PE, Leroy EM | title = Wild animal mortality monitoring and human Ebola outbreaks, Gabon and Republic of Congo, 2001–2003 | journal = Emerging Infectious Diseases | volume = 11 | issue = 2 | pages = 283–290 | date = Feb 2005 | pmid = 15752448 | pmc = 3320460 | doi = 10.3201/eid1102.040533 | url = http://www.cdc.gov/ncidod/EID/vol11no02/04-0533.htm | issn = 1080-6040 | format = Free full text }}</ref> |
|||
Ebola has a high mortality rate among primates.<ref name="Choi2013">{{Cite journal |vauthors=Choi JH, Croyle MA |date=December 2013 |title=Emerging targets and novel approaches to Ebola virus prophylaxis and treatment |journal=BioDrugs |volume=27 |issue=6 |pages=565–583 |doi=10.1007/s40259-013-0046-1 |pmc=3833964 |pmid=23813435}}</ref> Frequent outbreaks of Ebola may have resulted in the deaths of 5,000 gorillas.<ref>{{Cite news |date=8 December 2006 |title=Ebola 'kills over 5,000 gorillas' |work=BBC News Online |url=http://news.bbc.co.uk/2/hi/science/nature/6220122.stm |url-status=live |access-date=31 May 2009 |archive-url=https://web.archive.org/web/20090329013552/http://news.bbc.co.uk/2/hi/science/nature/6220122.stm |archive-date=29 March 2009}}</ref> Outbreaks of Ebola may have been responsible for an 88% decline in tracking indices of observed chimpanzee populations in the 420 km<sup>2</sup> Lossi Sanctuary between 2002 and 2003.<ref name="doi10.1126/science.1092528" /> Transmission among chimpanzees through meat consumption constitutes a significant risk factor, whereas contact between the animals, such as touching dead bodies and grooming, is not.<ref>{{Cite journal |display-authors=6 |vauthors=Formenty P, Boesch C, Wyers M, Steiner C, Donati F, Dind F, Walker F, Le Guenno B |date=February 1999 |title=Ebola virus outbreak among wild chimpanzees living in a rain forest of Côte d'Ivoire |journal=The Journal of Infectious Diseases | volume = 179 |issue= Suppl 1 |pages=S120–S126 |citeseerx=10.1.1.484.5782 |doi=10.1086/514296 |pmid=9988175 |s2cid=18658117}}</ref> |
|||
Recovered carcasses from gorillas contain multiple Ebola virus strains, which suggest multiple introductions of the virus. Bodies decompose quickly and carcasses are not infectious after three to four days. Contact between gorilla groups is rare, suggesting transmission among gorilla groups is unlikely, and that outbreaks result from transmission between viral reservoir and animal populations.<ref name="doi10.1126/science.1092528">{{cite journal | author = Leroy EM, Rouquet P, Formenty P, Souquière S, Kilbourne A, Froment JM, Bermejo M, Smit S, Karesh W, Swanepoel R, Zaki SR, Rollin PE | title = Multiple Ebola virus transmission events and rapid decline of central African wildlife | journal = Science | volume = 303 | issue = 5656 | pages = 387–390 | year = 2004 | pmid = 14726594 | doi = 10.1126/science.1092528 | bibcode = 2004Sci...303..387L }}</ref> |
|||
Recovered gorilla carcasses have contained multiple Ebola virus strains, suggesting multiple introductions of the virus. Bodies decompose quickly and carcasses are not infectious after three to four days. Contact between gorilla groups is rare, suggesting that transmission among gorilla groups is unlikely, and that outbreaks result from transmission between viral reservoirs and animal populations.<ref name="doi10.1126/science.1092528">{{Cite journal |display-authors=6 |vauthors=Leroy EM, Rouquet P, Formenty P, Souquière S, Kilbourne A, Froment JM, Bermejo M, Smit S, Karesh W, Swanepoel R, Zaki SR, Rollin PE |date=January 2004 |title=Multiple Ebola virus transmission events and rapid decline of central African wildlife |journal=Science |volume=303 |issue=5656 |pages=387–390 |bibcode=2004Sci...303..387L |doi=10.1126/science.1092528 |pmid=14726594 |s2cid=43305484}}</ref> |
|||
Ebola has a high mortality among primates.<ref>{{cite journal|last1=Choi|first1=JH|last2=Croyle|first2=MA|title=Emerging targets and novel approaches to Ebola virus prophylaxis and treatment.|journal=BioDrugs : clinical immunotherapeutics, biopharmaceuticals and gene therapy|date=2013 Dec|volume=27|issue=6|pages=565-83|pmid=23813435}}</ref> Frequent outbreaks of Ebola may have resulted in the deaths of 5,000 gorillas.<ref>{{Cite book|title=Ebola 'kills over 5,000 gorillas'|url=http://news.bbc.co.uk/2/hi/science/nature/6220122.stm|accessdate=2009-05-31|date=2006-12-08|publisher=BBC}}</ref> Outbreaks of EVD may have been responsible for an 88% decline in tracking indices of observed chimpanzee populations in 420 square kilometer Lossi Sanctuary between 2002 and 2003.<ref name="doi10.1126/science.1092528" /> Transmission among chimpanzees through meat consumption constitutes a significant risk factor, while contact between individuals, such as touching dead bodies and grooming is not.<ref>{{cite journal | author = Formenty P, Boesch C, Wyers M, Steiner C, Donati F, Dind F, Walker F, Le Guenno B | title = Ebola virus outbreak among wild chimpanzees living in a rain forest of Côte d'Ivoire | journal = The Journal of infectious diseases | volume = Suppl 1 | issue = s1 | pages = S120–S126 | year = 1999 | pmid = 9988175 | doi = 10.1086/514296 | series = 179 }}</ref> |
|||
===Domestic animals=== |
===Domestic animals=== |
||
In 2012, it was demonstrated that the virus can travel without contact from pigs to nonhuman primates, although the same study failed to achieve transmission in that manner between primates.<ref name="Weingartl_2013" /><ref name="Weingartl2012">{{Cite journal |vauthors=Weingartl HM, Embury-Hyatt C, Nfon C, Leung A, Smith G, Kobinger G |date=November 2012 |title=Transmission of Ebola virus from pigs to non-human primates |journal=Sci Rep |volume=2 |page=811 |bibcode=2012NatSR...2..811W |doi=10.1038/srep00811 |pmc=3498927 |pmid=23155478}}</ref> |
|||
Dogs may become infected with EBOV but not develop symptoms. Dogs in some parts of Africa [[scavenge]] for food, and they sometimes eat EBOV-infected animals and also the corpses of humans. A 2005 survey of dogs during an EBOV outbreak found that although they remain asymptomatic, about 32 percent of dogs closest to an outbreak showed a [[seroprevalence]] for EBOV versus nine percent of those farther away.<ref name="pmid15757552">{{Cite journal |display-authors=6 |vauthors=Allela L, Boury O, Pouillot R, Délicat A, Yaba P, Kumulungui B, Rouquet P, Gonzalez JP, Leroy EM |date=March 2005 |title=Ebola virus antibody prevalence in dogs and human risk |journal=Emerg. Infect. Dis. |volume=11 |issue=3 |pages=385–390 |doi=10.3201/eid1103.040981 |pmc=3298261 |pmid=15757552}}</ref> The authors concluded that there were "potential implications for preventing and controlling human outbreaks." |
|||
Ebola virus can be transmitted to [[dog]]s and [[pig]]s.<ref name="pmid23689899">{{cite journal | author = Weingartl HM, Nfon C, Kobinger G | title = Review of Ebola virus infections in domestic animals | journal = Dev Biol (Basel) | volume = 135 | issue = | pages = 211–8 | year = 2013 | pmid = 23689899 | doi = 10.1159/000178495 }}</ref> While dogs may be asymptomatic, pigs tend to develop symptomatic disease. |
|||
===Reston virus=== |
|||
{{For|more about the outbreak in Virginia, US|Reston virus}} |
|||
In late 1989, Hazelton Research Products' Reston Quarantine Unit in [[Reston, Virginia]], had an outbreak of fatal illness amongst certain lab monkeys. This lab outbreak was initially diagnosed as [[simian haemorrhagic fever virus]] (SHFV) and occurred amongst a shipment of [[crab-eating macaque]] monkeys imported from the Philippines. Hazelton's veterinary pathologist in Reston sent tissue samples from dead animals to the [[United States Army Medical Research Institute of Infectious Diseases]] (USAMRIID) at [[Fort Detrick, Maryland]], where an [[ELISA]] test indicated the antibodies present in the tissue were a response to Ebola virus and not SHFV.<ref name="Preston">{{Cite book | vauthors = Preston R |url=https://archive.org/details/hotzone00pres |title=The Hot Zone |publisher=Random House |year=1994 |isbn=978-0679437840 |location=New York |page=[https://archive.org/details/hotzone00pres/page/300 300] |url-access=registration}}</ref> An electron microscopist from USAMRIID discovered [[filoviruses]] similar in appearance, in crystalloid aggregates and as single filaments with a shepherd's hook, to Ebola in the tissue samples sent from Hazelton Research Products' Reston Quarantine Unit.<ref name="McCormick 1999 277–279">{{harvnb|McCormick|Fisher-Hoch|Horvitz|1999|pp=277–279}}</ref> |
|||
A [[US Army]] team headquartered at USAMRIID [[Euthanisia|euthanised]] the surviving monkeys, and brought all the dead monkeys to Fort Detrick for study by the Army's veterinary pathologists and virologists, and eventual disposal under safe conditions.<ref name="Preston" /> Blood samples were taken from 178 animal handlers during the incident.<ref name="Waterman 1999">{{Cite book | vauthors = Waterman T |url=http://www.stanford.edu/group/virus/filo/ebor.html |title=Ebola Reston Outbreaks |publisher=Stanford University |year=1999 |access-date=2 August 2008 |archive-url=https://web.archive.org/web/20080616192533/http://www.stanford.edu/group/virus/filo/ebor.html |archive-date=16 June 2008 |url-status=live}}</ref> Of those, six animal handlers eventually [[seroconversion|seroconverted]], including one who had cut himself with a bloody scalpel.<ref name="isbn0-7910-8505-8">{{Cite book | vauthors = Smith T |url=https://archive.org/details/ebola0000smit |title=Ebola (Deadly Diseases and Epidemics) |publisher=Chelsea House Publications |year=2005 |isbn=978-0791085059 |url-access=registration}}</ref><ref name="McCormick 1999 298–299">{{harvnb|McCormick|Fisher-Hoch|Horvitz|1999|pp=298–299}}</ref> Despite its status as a [[Biosafety level 4|Level‑4]] organism and its apparent [[pathogen]]icity in monkeys, when the handlers did not become ill, the CDC concluded that the virus had a very low pathogenicity to humans.<ref name="McCormick 1999 298–299" /><ref>{{harvnb|McCormick|Fisher-Hoch|Horvitz|1999|p=300}}</ref> |
|||
The Philippines and the United States had no previous cases of Ebola infection, and upon further isolation, researchers concluded it was another strain of Ebola, or a new filovirus of Asian origin, which they named ''[[Reston ebolavirus]]'' (RESTV) after the location of the incident.<ref name="Preston" /> Reston virus (RESTV) can be transmitted to pigs.<ref name="Weingartl_2013" /> Since the initial outbreak it has since been found in nonhuman [[primate]]s in Pennsylvania, Texas, and Italy,<ref name="KnownCasesCDC">{{Cite web |title=Outbreaks Chronology: Ebola Virus Disease |url=http://origin.glb.cdc.gov/vhf/ebola/outbreaks/history/chronology.html |url-status=dead |archive-url=https://web.archive.org/web/20141026230925/http://origin.glb.cdc.gov/vhf/ebola/outbreaks/history/chronology.html |archive-date=26 October 2014 |access-date=26 October 2014 |publisher=[[Centers for Disease Control and Prevention]] (CDC).gov}}</ref> where the virus had infected pigs.<ref>{{Cite news | vauthors = McNeil Jr DG |date=24 January 2009 |title=Pig-to-Human Ebola Case Suspected in Philippines |work=The New York Times |url=https://www.nytimes.com/2009/01/24/health/24ebola.html |url-status=live |access-date=26 January 2009 |archive-url=https://web.archive.org/web/20090310113731/http://www.nytimes.com/2009/01/24/health/24ebola.html |archive-date=10 March 2009}}</ref> According to the WHO, routine cleaning and disinfection of pig (or monkey) farms with [[sodium hypochlorite]] or [[detergents]] should be effective in inactivating the ''Reston ebolavirus''. Pigs that have been infected with RESTV tend to show [[symptoms]] of the disease.<ref>{{Cite journal | vauthors = Lee J |date=2009 |title=Ebola-Reston virus in pigs |journal=Microbiology Australia |volume=30 |issue=4 |pages=140 |doi=10.1071/ma09140 |issn=1324-4272 |doi-access=free}}</ref> |
|||
==Research== |
==Research== |
||
=== |
===Treatments=== |
||
{{Main|Ebola virus disease treatment research}} |
|||
[[Favipiravir]] looks like it may be useful in a mouse model of the disease.<ref name=Gath2014/> Estrogen receptor drugs used to treat infertility and breast cancer ([[clomiphene]] and [[toremifene]]) inhibit the progress of Ebola virus in infected mice.<ref name="Johansen_2013">{{cite journal | author = Johansen LM, Brannan JM, Delos SE, Shoemaker CJ, Stossel A, Lear C, Hoffstrom BG, Dewald LE, Schornberg KL, Scully C, Lehár J, Hensley LE, White JM, Olinger GG | title = FDA-approved selective estrogen receptor modulators inhibit Ebola virus infection | journal = Sci Transl Med | volume = 5 | issue = 190 | pages = 190ra79 | year = 2013 | pmid = 23785035 | pmc = 3955358 | doi = 10.1126/scitranslmed.3005471 | laysummary = http://www.healthline.com/health-news/tech-breast-cancer-drugs-fight-ebola-virus-infection-062013 | laysource = Healthline Networks, Inc. }}</ref> Ninety percent of the mice treated with clomiphene and fifty percent of those treated with toremifene survived the tests.<ref name="Johansen_2013"/> Given their oral availability and history of human use, these drugs would be candidates for treating Ebola virus infection in remote geographical locations, either on their own or together with other antiviral drugs. |
|||
[[File:monoclonal antibodies3.jpg|thumb|Researchers looking at slides of cultures of cells that make [[monoclonal antibodies]]. These are grown in a lab and the researchers are analyzing the products to select the most promising.]] |
|||
{{As of|2015|7}}, no medication has been proven safe and effective for treating Ebola. By the time the [[Ebola virus epidemic in West Africa]] began in 2013, there were at least nine different candidate treatments. Several trials were conducted in late 2014, and early 2015, but some were abandoned due to lack of efficacy or lack of people to study.<ref>{{Cite web |title=Final trial results confirm Ebola vaccine provides high protection against disease |url=https://www.who.int/mediacentre/news/releases/2016/ebola-vaccine-results/en/ |url-status=live |archive-url=https://web.archive.org/web/20170401042946/http://who.int/mediacentre/news/releases/2016/ebola-vaccine-results/en/ |archive-date=1 April 2017 |access-date=29 March 2017 |publisher=[[World Health Organization]] (WHO)}}</ref> |
|||
=== Antibodies === |
|||
{{Main|2014 West Africa Ebola outbreak#Treatment}} |
|||
[[Image:monoclonal antibodies3.jpg|200px|thumb|right|Researchers looking at slides of cultures of cells that make monoclonal antibodies. These are grown in a lab and the researchers are analyzing the products to select the most promising of them.]] |
|||
During an outbreak 1999 in the Democratic Republic of the Congo, seven of eight people who received blood transfusions from individuals who had previously survived the infection survived themselves.<ref>{{cite journal | author = Mupapa K, Massamba M, Kibadi K, Kuvula K, Bwaka A, Kipasa M, Colebunders R, Muyembe-Tamfum JJ | title = Treatment of Ebola Hemorrhagic Fever with Blood Transfusions from Convalescent Patients | journal = The Journal of Infectious Diseases | volume = 179 | pages = S18–S23 | year = 1999 | pmid = 9988160 | pmc = | doi = 10.1086/514298 }}</ref> However, this potential treatment is considered controversial.<ref name=Lancet2011>{{cite journal | author = Feldmann H, Geisbert TW | title = Ebola haemorrhagic fever | journal = The Lancet | volume = 377 | issue = 9768 | pages = 849–862 | year = 2011 | pmid = 21084112 | doi = 10.1016/S0140-6736(10)60667-8 }}</ref> Intravenous antibodies appear to be protective in non-human primates who have been exposed to large doses of ebola.<ref>{{cite journal|last1=Saphire|first1=EO|title=An update on the use of antibodies against the filoviruses.|journal=Immunotherapy|date=2013 Nov|volume=5|issue=11|pages=1221-33|pmid=24188676}}</ref> |
|||
{{As of|2019|8}}, two experimental treatments known as [[atoltivimab/maftivimab/odesivimab]] and [[ansuvimab]] were found to be 90% effective.<ref>{{Cite journal |vauthors=Maxmen A |date=12 August 2019 |title=Two Ebola drugs show promise amid ongoing outbreak |journal=Nature |doi=10.1038/d41586-019-02442-6 |issn=0028-0836 |pmid=32778704 |s2cid=201975390}}</ref><ref>{{Cite journal |vauthors=Hoenen T, Groseth A, Feldmann H |date=24 July 2019 |title=Therapeutic strategies to target the Ebola virus life cycle |journal=Nature Reviews. Microbiology |volume=17 |issue=10 |pages=593–606 |doi=10.1038/s41579-019-0233-2 |issn=1740-1526 |pmid=31341272 |doi-access=free}}</ref><ref>{{Cite press release |title=Investigational Monoclonal Antibody to Treat Ebola Is Safe in Adults |date=24 January 2019 |publisher=[[National Institute of Allergy and Infectious Diseases]] (NIAID) |url=https://www.niaid.nih.gov/news-events/investigational-monoclonal-antibody-treat-ebola-safe-adults |access-date=12 August 2019 |archive-date=13 August 2019 |archive-url=https://web.archive.org/web/20190813064914/https://www.niaid.nih.gov/news-events/investigational-monoclonal-antibody-treat-ebola-safe-adults |url-status=live }}</ref> |
|||
On 4 August 2014 an experimental drug, [[ZMapp]], was first tested on humans. It was administered to two Americans who had been infected with Ebola. Both people appeared to have had positive results.<ref>{{cite web|url=http://edition.cnn.com/2014/08/04/health/experimental-ebola-serum|title=Experimental drug likely saved Ebola patients|date=August 4, 2014|publisher=CNN}}</ref><ref>{{cite web|url=http://www.latimes.com/science/sciencenow/la-sci-sn-ebola-serum-20140804-story.html|title=Mystery Ebola virus serum manufactured by San Diego firm|date=August 4, 2014|publisher=Los Angeles Times}}</ref> |
|||
=== |
===Diagnostic tests=== |
||
The diagnostic tests currently available require specialised equipment and highly trained personnel. Since there are few suitable testing centres in West Africa, this leads to delay in diagnosis.<ref>{{Cite magazine | vauthors = Butler D |title=Ebola Experts Seek to Expand Testing |url=http://www.scientificamerican.com/article/ebola-experts-seek-to-expand-testing/ |url-status=live |magazine=[[Scientific American]] |archive-url=https://web.archive.org/web/20141213012943/http://www.scientificamerican.com/article/ebola-experts-seek-to-expand-testing/ |archive-date=13 December 2014 |access-date=11 December 2014}}</ref> |
|||
Other promising treatments rely on [[antisense therapy|antisense technology]]. Both [[small interfering RNA]]s (siRNAs) and [[Morpholino|phosphorodiamidate morpholino oligomers]] (PMOs) targeting the Zaire Ebola virus (ZEBOV) RNA polymerase L protein could prevent disease in nonhuman primates.<ref>{{cite journal | author = Geisbert TW, Lee AC, Robbins M, Geisbert JB, Honko AN, Sood V, Johnson JC, de Jong S, Tavakoli I, Judge A, Hensley LE, Maclachlan I | title = Postexposure protection of non-human primates against a lethal Ebola virus challenge with RNA interference: A proof-of-concept study | journal = The Lancet | volume = 375 | issue = 9729 | pages = 1896–1905 | year = 2010 | pmid = 20511019 | doi = 10.1016/S0140-6736(10)60357-1 }}</ref><ref>{{cite journal | author = Warren TK, Warfield KL, Wells J, Swenson DL, Donner KS, Van Tongeren SA, Garza NL, Dong L, Mourich DV, Crumley S, Nichols DK, Iversen PL, Bavari S | title = Advanced antisense therapies for postexposure protection against lethal filovirus infections | journal = Nature Medicine | volume = 16 | issue = 9 | pages = 991–994 | year = 2010 | pmid = 20729866 | doi = 10.1038/nm.2202 }}</ref> |
|||
{{-}} |
|||
On 29 November 2014, a new 15-minute Ebola test was reported that if successful, "not only gives patients a better chance of survival, but it prevents transmission of the virus to other people." The new equipment, about the size of a laptop and solar-powered, allows testing to be done in remote areas.<ref>{{Cite news | vauthors = Buchanan RT |date=29 November 2014 |title=Ebola outbreak: New 15-minute test offers hope for thousands |work=The Independent |url=https://www.independent.co.uk/news/world/africa/ebola-outbreak-new-15minute-test-trialled-in-guinea-offers-hope-for-thousands-9892543.html |url-status=live |access-date=1 December 2014 |archive-url=https://web.archive.org/web/20141201003020/http://www.independent.co.uk/news/world/africa/ebola-outbreak-new-15minute-test-trialled-in-guinea-offers-hope-for-thousands-9892543.html |archive-date=1 December 2014}}</ref> |
|||
On 29 December 2014, the U.S. [[Food and Drug Administration]] (FDA) approved the LightMix Ebola Zaire [[Reverse transcription polymerase chain reaction|rRT-PCR]] test for patients with symptoms of Ebola.<ref>{{Cite news | vauthors = Falconi M |date=29 December 2014 |title=Roche Secures Emergency Approval by U.S. Regulators for Ebola Test |work=[[The Wall Street Journal]] |url=https://www.wsj.com/articles/roche-secures-emergency-approval-by-u-s-regulators-for-ebola-test-1419840858 |url-status=live |url-access=subscription |access-date=29 December 2014 |archive-url=https://web.archive.org/web/20141229163045/http://www.wsj.com/articles/roche-secures-emergency-approval-by-u-s-regulators-for-ebola-test-1419840858 |archive-date=29 December 2014}}</ref> |
|||
===Disease models=== |
|||
Animal models and in particular non-human primates are being used to study different aspects of Ebola virus disease. Developments in [[organ-on-a-chip]] technology have led to a chip-based model for Ebola haemorrhagic syndrome.<ref>{{cite journal | vauthors = Junaid A, Tang H, van Reeuwijk A, Abouleila Y, Wuelfroth P, van Duinen V, Stam W, van Zonneveld AJ, Hankemeier T, Mashaghi A | display-authors = 6 | title = Ebola Hemorrhagic Shock Syndrome-on-a-Chip | journal = iScience | volume = 23 | issue = 1 | pages = 100765 | date = January 2020 | pmid = 31887664 | pmc = 6941864 | doi = 10.1016/j.isci.2019.100765 | bibcode = 2020iSci...23j0765J }}</ref> |
|||
==See also== |
|||
* [[Bibliography of Ebola]] |
|||
==Notes== |
|||
{{reflist|group=note}} |
|||
==References== |
==References== |
||
{{Reflist| |
{{Reflist|refs= |
||
<ref name="WHO2014_12_28">{{Cite report |url=http://apps.who.int/ebolaweb/sitreps/20141231/20141231.pdf |title=Ebola response roadmap situation report |date=31 December 2014 |publisher=WHO |quote=The reported case fatality rate in the three intense-transmission countries among all cases for whom a definitive outcome is known is 71%. |access-date=1 January 2015 |archive-url=https://web.archive.org/web/20141231222250/http://apps.who.int/ebolaweb/sitreps/20141231/20141231.pdf |archive-date=31 December 2014 |url-status=dead}}</ref> |
|||
}} |
|||
* ''The article uses public domain text from the CDC as cited.'' |
|||
=== Bibliography === |
|||
{{Refbegin}} |
{{Refbegin}} |
||
* {{Cite book |vauthors=McCormick J, Fisher-Hoch S, Horvitz LA |url=https://books.google.com/books?id=QEvR3aJX2m0C |title=Level 4: Virus Hunters of the CDC |date=1999 |publisher=Barnes & Noble |isbn=978-0760712085 |edition=Updated [3rd] |format=Limited preview |orig-year=1996 |access-date=3 September 2020 |archive-date=21 May 2024 |archive-url=https://web.archive.org/web/20240521143950/https://books.google.com/books?id=QEvR3aJX2m0C |url-status=live }} |
|||
* {{Cite book |last=Klenk |first=Hans-Dieter |title=Marburg and Ebola Viruses (Current Topics in Microbiology and Immunology) |date=January 1999 |publisher=Springer-Verlag Telos |location=Berlin |isbn=978-3-540-64729-4 |ref=CITEREFKlenk1999}} |
|||
* {{Cite book |first1=Hans-Dieter |last1=Klenk |first2=Heinz |last2=Feldmann |title=Ebola and Marburg viruses: molecular and cellular biology |url=http://books.google.com/?id=EV_mFgnyPoMC |format=Limited preview |year=2004 |publisher=Horizon Bioscience |location=Wymondham, Norfolk, UK |isbn=978-0-9545232-3-7 |ref=CITEREFKlenkFeldmann2004}} |
|||
* {{Cite book |last=Kuhn |first=Jens H. |title=Filoviruses: A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies. Archives of Virology Supplement, vol. 20 |url=http://books.google.com/?id=LaOue0F9Ns4C |format=Limited preview |year=2008 |publisher=SpringerWienNewYork |location=Vienna |isbn=978-3-211-20670-6 |ref=CITEREFKuhn2008}} |
|||
* {{Cite book |last1=McCormick |first1=Joseph |last2=Fisher-Hoch |first2=Susan |others=Horvitz, Leslie Alan |title=Level 4: Virus Hunters of the CDC |url=http://books.google.com/?id=QEvR3aJX2m0C |format=Limited preview |origyear=1996 |edition=Updated [3rd] |year=1999 |publisher=Barnes & Noble |isbn=978-0-7607-1208-5 |ref=CITEREFMcCormickFisher-Hoch1999 |month=June}} |
|||
* {{Cite book |last=Pattyn |first=S. R. |title=Ebola Virus Haemorrhagic Fever |year=1978 |url=http://www.itg.be/ebola/ |format=Full free text |edition=1st |publisher=Elsevier/North-Holland Biomedical Press |location=Amsterdam |isbn=0-444-80060-3 |ref=CITEREFPattyn1978}} |
|||
* {{Cite book | last1 = Ryabchikova | first1 = Elena I. | last2 = Price | first2 = Barbara B. | title = Ebola and Marburg Viruses: A View of Infection Using Electron Microscopy | year = 2004 | publisher = Battelle Press | location = Columbus, Ohio | isbn = 978-1-57477-131-2 | ref = CITEREFRyabchikovaPrice2004 }} |
|||
{{Refend}} |
{{Refend}} |
||
== Further reading == |
|||
==External links== |
|||
{{Portal bar|Medicine|Viruses}} |
|||
{{Sister project links|Ebola}} |
|||
{{Refbegin}} |
{{Refbegin}} |
||
* {{Cite book |vauthors=Wilson F |url=https://books.google.com/books?id=yMQNBQAAQBAJ&pg=PP1 |title=CDC Guidance on Ebola Virus (EVD) |publisher=International Publications Media Group |year=2014 |isbn=978-1632670113 }} |
|||
* [http://viralzone.expasy.org/all_by_species/207.html ViralZone: Ebola-like viruses] – Virological repository from the [[Swiss Institute of Bioinformatics]] |
|||
* {{Cite book |url=https://books.google.com/books?id=nLA4W5IjJpwC&pg=PP1 |title=Ebola Virus: New Insights for the Healthcare Professional: 2011 Edition: ScholarlyPaper |publisher=Scholarly Editions |year=2012 |isbn=978-1464914935 }} |
|||
* [http://www.cdc.gov/vhf/ebola/ CDC: Ebola hemorrhagic fever] – Centers for Disease Control and Prevention, Special Pathogens Branch |
|||
* {{Cite book | vauthors = Klenk HD |title=Marburg and Ebola Viruses |date=January 1999 |publisher=Springer-Verlag Telos |isbn=978-3540647294 |series=Current Topics in Microbiology and Immunology 235 |location=Berlin}} |
|||
* [http://www.who.int/csr/disease/ebola/en/ WHO: Ebola haemorrhagic fever] – World Health Organization, Global Alert and Response |
|||
* {{Cite book |vauthors=Klenk HD, Feldmann H |url=https://books.google.com/books?id=EV_mFgnyPoMC |title=Ebola and Marburg viruses: molecular and cellular biology |publisher=Horizon Bioscience |year=2004 |isbn=978-0954523237 |location=Wymondham, Norfolk |format=Limited preview |access-date=3 September 2020 |archive-date=21 May 2024 |archive-url=https://web.archive.org/web/20240521143950/https://books.google.com/books?id=EV_mFgnyPoMC |url-status=live }} |
|||
* [http://www.viprbrc.org/brc/home.do?decorator=filo Virus Pathogen Database and Analysis Resource (ViPR): Filoviridae] |
|||
* {{Cite book |vauthors=Kuhn JH |url=https://books.google.com/books?id=LaOue0F9Ns4C |title=Filoviruses: A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies. Archives of Virology Supplement |volume=20 |publisher=SpringerWienNewYork |year=2008 |isbn=978-3211206706 |location=Vienna |format=Limited preview |access-date=3 September 2020 |archive-date=21 May 2024 |archive-url=https://web.archive.org/web/20240521144049/https://books.google.com/books?id=LaOue0F9Ns4C |url-status=live }} |
|||
* [http://www.ebi.ac.uk/pdbe/emdb/searchResults.html/?q=ebola 3D macromolecular structures of the Ebola virus archived in the EM Data Bank(EMDB)] |
|||
* {{Cite book |vauthors=Pattyn SR |url=http://www.itg.be/ebola/ |title=Ebola Virus Haemorrhagic Fever |publisher=Elsevier/North-Holland Biomedical Press |year=1978 |isbn=978-0444800602 |edition=1st |location=Amsterdam |format=Full free text |archive-url=https://web.archive.org/web/20101211083855/http://www.itg.be/ebola/ |archive-date=11 December 2010 |url-status=dead }} |
|||
* [https://maps.google.com/maps/ms?msa=0&msid=202977755949863934429.0004c658eb30f9c4fb1c0&ie=UTF8&t=h&ll=27.371767,5.273438&spn=110.017392,184.21875&z=2&source=embed&dg=feature Google Map of Ebola Outbreaks] |
|||
* {{Cite book | vauthors = Ryabchikova EI, Price BB |title=Ebola and Marburg Viruses: A View of Infection Using Electron Microscopy |publisher=Battelle Press |year=2004 |isbn=978-1574771312 |location=Columbus, Ohio}} |
|||
* [http://www.who.int/csr/bioriskreduction/filovirus_infection_control/en/ WHO recommended infection control measures] |
|||
{{Refend}} |
{{Refend}} |
||
==External links== |
|||
{{incubator|vai/ꔤꕷꕞ}} |
|||
* [https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease WHO fact sheet on Ebola] |
|||
* [https://www.cdc.gov/vhf/ebola/ Ebola (Ebola Virus Disease)] – Centers for Disease Control and Prevention, Viral Special Pathogens Branch. |
|||
* [https://web.archive.org/web/20140823072115/http://www.who.int/csr/disease/ebola/videos/en/ Videos: Ebola outbreak response] – World Health Organization. |
|||
* {{Cite web |date=13 January 2021 |title=Ebola Preparedness and Response |url=https://www.fda.gov/emergency-preparedness-and-response/mcm-issues/ebola-preparedness-and-response-updates-fda |website=U.S. [[Food and Drug Administration]] (FDA)}} |
|||
* [https://www.scientificamerican.com/report/ebola-what-you-need-to-know1/ Ebola: What You Need to Know] – ''[[Scientific American]]'' articles related to Ebola; note these are general reading articles, they are not scientific peer-reviewed research articles. |
|||
{{Medical condition classification and resources |
|||
| DiseasesDB = 18043 |
|||
| ICD11 = {{ICD10|1D60.0}} |
|||
| ICD10 = {{ICD10|A|98|4|a|90}} |
|||
| ICD9 = {{ICD9|078.89}} |
|||
| MedlinePlus = 001339 |
|||
| eMedicineSubj = med |
|||
| eMedicineTopic = 626 |
|||
| MeshID = D019142 |
|||
}} |
|||
{{Ebola|state=autocollapse}} |
|||
{{Zoonotic viral diseases}} |
{{Zoonotic viral diseases}} |
||
{{Subject bar | Medicine | Viruses |commons=y |commons-search=Ebola |wikt=y |wikt-search=Ebola |q=y |v=y |v-search=Ebola |n=y |n-search=Category:Ebola virus |d=y |d-search=Q51993 }} |
|||
{{Authority control}} |
|||
[[Category:Ebola| ]] |
[[Category:Ebola| ]] |
||
[[Category: |
[[Category:Animal viral diseases]] |
||
[[Category:Articles containing video clips]] |
|||
[[Category:Bat virome]] |
|||
[[Category:Biological agents]] |
|||
[[Category:Health in Africa]] |
[[Category:Health in Africa]] |
||
[[Category:Hemorrhagic fevers]] |
[[Category:Hemorrhagic fevers]] |
||
[[Category:Wikipedia medicine articles ready to translate]] |
|||
[[Category:Wikipedia infectious disease articles ready to translate]] |
|||
[[Category:Sexually transmitted diseases and infections]] |
|||
[[Category:Tropical diseases]] |
[[Category:Tropical diseases]] |
||
[[Category:Virus-related cutaneous conditions]] |
|||
[[Category:West African Ebola virus epidemic]] |
|||
[[Category:Wikipedia pages referenced by the press]] |
|||
[[Category:Zoonoses]] |
[[Category:Zoonoses]] |
||
[[Category:Vaccine-preventable diseases]] |
|||
[[so:Ebola virus disease]] |
|||
Latest revision as of 08:01, 15 December 2024
| Ebola | |
|---|---|
| Other names | Ebola haemorrhagic fever (EHF), Ebola virus disease |
 | |
| Two nurses standing near Mayinga N'Seka, a nurse with Ebola virus disease in the 1976 outbreak in Zaire. N'Seka died a few days later. The nurses are not wearing proper protective equipment. | |
| Specialty | Infectious disease |
| Symptoms | Fever, sore throat, muscular pain, headaches, diarrhoea, bleeding[1] |
| Complications | shock from fluid loss[2] |
| Usual onset | Two days to three weeks post exposure[1] |
| Causes | Ebolaviruses spread by direct contact[1] |
| Diagnostic method | Finding the virus, viral RNA, or antibodies in blood[1] |
| Differential diagnosis | Malaria, cholera, typhoid fever, meningitis, other viral haemorrhagic fevers[1] |
| Prevention | Coordinated medical services, careful handling of bushmeat[1] |
| Treatment | Supportive care[1] |
| Medication | Atoltivimab/maftivimab/odesivimab (Inmazeb) |
| Prognosis | 25–90% mortality[1] |
Ebola, also known as Ebola virus disease (EVD) and Ebola hemorrhagic fever (EHF), is a viral hemorrhagic fever in humans and other primates, caused by ebolaviruses.[1] Symptoms typically start anywhere between two days and three weeks after infection.[3] The first symptoms are usually fever, sore throat, muscle pain, and headaches.[1] These are usually followed by vomiting, diarrhoea, rash and decreased liver and kidney function,[1] at which point some people begin to bleed both internally and externally.[1] It kills between 25% and 90% of those infected – about 50% on average.[1] Death is often due to shock from fluid loss, and typically occurs between six and 16 days after the first symptoms appear.[2] Early treatment of symptoms increases the survival rate considerably compared to late start.[4] An Ebola vaccine was approved by the US FDA in December 2019.
The virus spreads through direct contact with body fluids, such as blood from infected humans or other animals,[1] or from contact with items that have recently been contaminated with infected body fluids.[1] There have been no documented cases, either in nature or under laboratory conditions, of spread through the air between humans or other primates.[5] After recovering from Ebola, semen or breast milk may continue to carry the virus for anywhere between several weeks to several months.[1][6][7] Fruit bats are believed to be the normal carrier in nature; they are able to spread the virus without being affected by it.[1] The symptoms of Ebola may resemble those of several other diseases, including malaria, cholera, typhoid fever, meningitis and other viral hemorrhagic fevers.[1] Diagnosis is confirmed by testing blood samples for the presence of viral RNA, viral antibodies or the virus itself.[1][8]
Control of outbreaks requires coordinated medical services and community engagement,[1] including rapid detection, contact tracing of those exposed, quick access to laboratory services, care for those infected, and proper disposal of the dead through cremation or burial.[1][9] Prevention measures involve wearing proper protective clothing and washing hands when in close proximity to patients and while handling potentially infected bushmeat, as well as thoroughly cooking bushmeat.[1] An Ebola vaccine was approved by the US FDA in December 2019.[10] While there is no approved treatment for Ebola as of 2019[update],[11] two treatments (atoltivimab/maftivimab/odesivimab and ansuvimab) are associated with improved outcomes.[12] Supportive efforts also improve outcomes.[1] These include oral rehydration therapy (drinking slightly sweetened and salty water) or giving intravenous fluids, and treating symptoms.[1] In October 2020, atoltivimab/maftivimab/odesivimab (Inmazeb) was approved for medical use in the United States to treat the disease caused by Zaire ebolavirus.[13]
History and name
Ebola was first identified in 1976, in two simultaneous outbreaks, one in Nzara (a town in South Sudan) and the other in Yambuku (the Democratic Republic of the Congo), a village near the Ebola River, for which the disease was named.[1] Ebola outbreaks occur intermittently in tropical regions of sub-Saharan Africa.[1] Between 1976 and 2012, according to the World Health Organization, there were 24 outbreaks of Ebola resulting in a total of 2,387 cases, and 1,590 deaths.[1][14] The largest Ebola outbreak to date was an epidemic in West Africa from December 2013 to January 2016, with 28,646 cases and 11,323 deaths.[15][16][17] On 29 March 2016, it was declared to no longer be an emergency.[18] Other outbreaks in Africa began in the Democratic Republic of the Congo in May 2017,[19][20] and 2018.[21][22] In July 2019, the World Health Organization declared the Congo Ebola outbreak a world health emergency.[23]
Signs and symptoms

Onset
The length of time between exposure to the virus and the development of symptoms (incubation period) is between 2 and 21 days,[1][24] and usually between 4 and 10 days.[25] However, recent estimates based on mathematical models predict that around 5% of cases may take longer than 21 days to develop.[26]
Symptoms usually begin with a sudden influenza-like stage characterised by fatigue, fever, weakness, decreased appetite, muscular pain, joint pain, headache, and sore throat.[1][25][27][28] The fever is usually higher than 38.3 °C (101 °F).[29] This is often followed by nausea, vomiting, diarrhoea, abdominal pain, and sometimes hiccups.[28][30] The combination of severe vomiting and diarrhoea often leads to severe dehydration.[31] Next, shortness of breath and chest pain may occur, along with swelling, headaches, and confusion.[28] In about half of the cases, the skin may develop a maculopapular rash, a flat red area covered with small bumps, five to seven days after symptoms begin.[25][29]
Bleeding
In some cases, internal and external bleeding may occur.[1] This typically begins five to seven days after the first symptoms.[32] All infected people show some decreased blood clotting.[29] Bleeding from mucous membranes or from sites of needle punctures has been reported in 40–50% of cases.[33] This may cause vomiting blood, coughing up of blood, or blood in stool.[34] Bleeding into the skin may create petechiae, purpura, ecchymoses or haematomas (especially around needle injection sites).[35] Bleeding into the whites of the eyes may also occur.[36] Heavy bleeding is uncommon; if it occurs, it is usually in the gastrointestinal tract.[37] The incidence of bleeding into the gastrointestinal tract was reported to be ~58% in the 2001 outbreak in Gabon,[38] but in the 2014–15 outbreak in the US it was ~18%,[39] possibly due to improved prevention of disseminated intravascular coagulation.[31]
Recovery or death
Recovery may begin between seven and 14 days after first symptoms.[28] Death, if it occurs, follows typically six to sixteen days from first symptoms and is often due to shock from fluid loss.[2] In general, bleeding often indicates a worse outcome, and blood loss may result in death.[27] People are often in a coma near the end of life.[28]
Those who survive often have ongoing muscular and joint pain, liver inflammation, and decreased hearing, and may have continued tiredness, continued weakness, decreased appetite, and difficulty returning to pre-illness weight.[28][40] Problems with vision may develop.[41] It is recommended that survivors of EVD wear condoms for at least twelve months after initial infection or until the semen of a male survivor tests negative for Ebola virus on two separate occasions.[42]
Survivors develop antibodies against Ebola that last at least 10 years, but it is unclear whether they are immune to additional infections.[43]
Cause
EVD in humans is caused by four of six viruses of the genus Ebolavirus. The four are Bundibugyo virus (BDBV), Sudan virus (SUDV), Taï Forest virus (TAFV) and one simply called Ebola virus (EBOV, formerly Zaire Ebola virus).[44] EBOV, species Zaire ebolavirus, is the most dangerous of the known EVD-causing viruses, and is responsible for the largest number of outbreaks.[45] The fifth and sixth viruses, Reston virus (RESTV) and Bombali virus (BOMV),[46] are not thought to cause disease in humans, but have caused disease in other primates.[47][48] All six viruses are closely related to marburgviruses.[44]
Virology

Ebolaviruses contain single-stranded, non-infectious RNA genomes.[49] Ebolavirus genomes contain seven genes including 3'-UTR-NP-VP35-VP40-GP-VP30-VP24-L-5'-UTR.[35][50] The genomes of the five different ebolaviruses (BDBV, EBOV, RESTV, SUDV and TAFV) differ in sequence and the number and location of gene overlaps. As with all filoviruses, ebolavirus virions are filamentous particles that may appear in the shape of a shepherd's crook, of a "U" or of a "6," and they may be coiled, toroid or branched.[50][51] In general, ebolavirions are 80 nanometers (nm) in width and may be as long as 14,000 nm.[52]
Their life cycle is thought to begin with a virion attaching to specific cell-surface receptors such as C-type lectins, DC-SIGN, or integrins, which is followed by fusion of the viral envelope with cellular membranes.[53] The virions taken up by the cell then travel to acidic endosomes and lysosomes where the viral envelope glycoprotein GP is cleaved.[53] This processing appears to allow the virus to bind to cellular proteins enabling it to fuse with internal cellular membranes and release the viral nucleocapsid.[53] The Ebolavirus structural glycoprotein (known as GP1,2) is responsible for the virus' ability to bind to and infect targeted cells.[54] The viral RNA polymerase, encoded by the L gene, partially uncoats the nucleocapsid and transcribes the genes into positive-strand mRNAs, which are then translated into structural and nonstructural proteins. The most abundant protein produced is the nucleoprotein, whose concentration in the host cell determines when L switches from gene transcription to genome replication. Replication of the viral genome results in full-length, positive-strand antigenomes that are, in turn, transcribed into genome copies of negative-strand virus progeny.[55] Newly synthesised structural proteins and genomes self-assemble and accumulate near the inside of the cell membrane. Virions bud off from the cell, gaining their envelopes from the cellular membrane from which they bud. The mature progeny particles then infect other cells to repeat the cycle. The genetics of the Ebola virus are difficult to study because of EBOV's virulent characteristics.[56]
Transmission
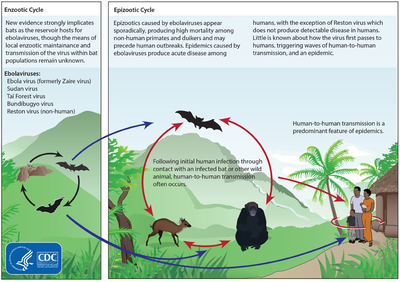

It is believed that between people, Ebola disease spreads only by direct contact with the blood or other body fluids of a person who has developed symptoms of the disease.[57][58][59] Body fluids that may contain Ebola viruses include saliva, mucus, vomit, feces, sweat, tears, breast milk, urine and semen.[6][43] The WHO states that only people who are very sick are able to spread Ebola disease in saliva, and the virus has not been reported to be transmitted through sweat. Most people spread the virus through blood, feces and vomit.[60] Entry points for the virus include the nose, mouth, eyes, open wounds, cuts and abrasions.[43] Ebola may be spread through large droplets; however, this is believed to occur only when a person is very sick.[61] This contamination can happen if a person is splashed with droplets.[61] Contact with surfaces or objects contaminated by the virus, particularly needles and syringes, may also transmit the infection.[62][63] The virus is able to survive on objects for a few hours in a dried state, and can survive for a few days within body fluids outside of a person.[43][64]
The Ebola virus may be able to persist for more than three months in the semen after recovery, which could lead to infections via sexual intercourse.[6][65][66] Virus persistence in semen for over a year has been recorded in a national screening programme.[67] Ebola may also occur in the breast milk of women after recovery, and it is not known when it is safe to breastfeed again.[7] The virus was also found in the eye of one patient, in 2014, two months after it was cleared from his blood.[68] Otherwise, people who have recovered are not infectious.[62]
The potential for widespread infections in countries with medical systems capable of observing correct medical isolation procedures is considered low.[69] Usually when someone has symptoms of the disease, they are unable to travel without assistance.[70]
Dead bodies remain infectious; thus, people handling human remains in practices such as traditional burial rituals or more modern processes such as embalming are at risk.[69] Of the cases of Ebola infections in Guinea during the 2014 outbreak, 69% are believed to have been contracted via unprotected (or unsuitably protected) contact with infected corpses during certain Guinean burial rituals.[71][72]
Health-care workers treating people with Ebola are at greatest risk of infection.[62] The risk increases when they do not have appropriate protective clothing such as masks, gowns, gloves and eye protection; do not wear it properly; or handle contaminated clothing incorrectly.[62] This risk is particularly common in parts of Africa where the disease mostly occurs and health systems function poorly.[73] There has been transmission in hospitals in some African countries that reuse hypodermic needles.[74][75] Some health-care centres caring for people with the disease do not have running water.[76] In the United States the spread to two medical workers treating infected patients prompted criticism of inadequate training and procedures.[77]
Human-to-human transmission of EBOV through the air has not been reported to occur during EVD outbreaks,[5] and airborne transmission has only been demonstrated in very strict laboratory conditions, and then only from pigs to primates, but not from primates to primates.[57][63] Spread of EBOV by water, or food other than bushmeat, has not been observed.[62][63] No spread by mosquitos or other insects has been reported.[62] Other possible methods of transmission are being studied.[64]
Airborne transmission among humans is theoretically possible due to the presence of Ebola virus particles in saliva, which can be discharged into the air with a cough or sneeze, but observational data from previous epidemics suggests the actual risk of airborne transmission is low.[78] A number of studies examining airborne transmission broadly concluded that transmission from pigs to primates could happen without direct contact because, unlike humans and primates, pigs with EVD get very high ebolavirus concentrations in their lungs, and not their bloodstream.[79] Therefore, pigs with EVD can spread the disease through droplets in the air or on the ground when they sneeze or cough.[80] By contrast, humans and other primates accumulate the virus throughout their body and specifically in their blood, but not very much in their lungs.[80] It is believed that this is the reason researchers have observed pig to primate transmission without physical contact, but no evidence has been found of primates being infected without actual contact, even in experiments where infected and uninfected primates shared the same air.[79][80]
Initial case

Although it is not entirely clear how Ebola initially spreads from animals to humans, the spread is believed to involve direct contact with an infected wild animal or fruit bat.[62] Besides bats, other wild animals that are sometimes infected with EBOV include several species of monkeys such as baboons, great apes (chimpanzees and gorillas), and duikers (a species of antelope).[84]
Animals may become infected when they eat fruit partially eaten by bats carrying the virus.[85] Fruit production, animal behavior and other factors may trigger outbreaks among animal populations.[85]
Evidence indicates that both domestic dogs and pigs can also be infected with EBOV.[86] Dogs do not appear to develop symptoms when they carry the virus, and pigs appear to be able to transmit the virus to at least some primates.[86] Although some dogs in an area in which a human outbreak occurred had antibodies to EBOV, it is unclear whether they played a role in spreading the disease to people.[86]
Reservoir
The natural reservoir for Ebola has yet to be confirmed; however, bats are considered to be the most likely candidate.[63] Three types of fruit bats (Hypsignathus monstrosus, Epomops franqueti and Myonycteris torquata) were found to possibly carry the virus without getting sick.[87] As of 2013[update], whether other animals are involved in its spread is not known.[86] Plants, arthropods, rodents, and birds have also been considered possible viral reservoirs.[1][31]
Bats were known to roost in the cotton factory in which the first cases of the 1976 and 1979 outbreaks were observed, and they have also been implicated in Marburg virus infections in 1975 and 1980.[88] Of 24 plant and 19 vertebrate species experimentally inoculated with EBOV, only bats became infected.[89] The bats displayed no clinical signs of disease, which is considered evidence that these bats are a reservoir species of EBOV. In a 2002–2003 survey of 1,030 animals including 679 bats from Gabon and the Republic of the Congo, immunoglobulin G (IgG) immune defense molecules indicative of Ebola infection were found in three bat species; at various periods of study, between 2.2 and 22.6% of bats were found to contain both RNA sequences and IgG molecules indicating Ebola infection.[90] Antibodies against Zaire and Reston viruses have been found in fruit bats in Bangladesh, suggesting that these bats are also potential hosts of the virus and that the filoviruses are present in Asia.[91]
Between 1976 and 1998, in 30,000 mammals, birds, reptiles, amphibians and arthropods sampled from regions of EBOV outbreaks, no Ebola virus was detected apart from some genetic traces found in six rodents (belonging to the species Mus setulosus and Praomys) and one shrew (Sylvisorex ollula) collected from the Central African Republic.[88][92] However, further research efforts have not confirmed rodents as a reservoir.[93] Traces of EBOV were detected in the carcasses of gorillas and chimpanzees during outbreaks in 2001 and 2003, which later became the source of human infections. However, the high rates of death in these species resulting from EBOV infection make it unlikely that these species represent a natural reservoir for the virus.[88]
Deforestation has been mentioned as a possible contributor to recent outbreaks, including the West African Ebola virus epidemic. Index cases of EVD have often been close to recently deforested lands.[94][95]
Pathophysiology

Like other filoviruses, EBOV replicates very efficiently in many cells, producing large amounts of virus in monocytes, macrophages, dendritic cells and other cells including liver cells, fibroblasts, and adrenal gland cells.[96] Viral replication triggers high levels of inflammatory chemical signals and leads to a septic state.[40]
EBOV is thought to infect humans through contact with mucous membranes or skin breaks.[57] After infection, endothelial cells (cells lining the inside of blood vessels), liver cells, and several types of immune cells such as macrophages, monocytes, and dendritic cells are the main targets of attack.[57] Following infection, immune cells carry the virus to nearby lymph nodes where further reproduction of the virus takes place.[57] From there the virus can enter the bloodstream and lymphatic system and spread throughout the body.[57] Macrophages are the first cells infected with the virus, and this infection results in programmed cell death.[52] Other types of white blood cells, such as lymphocytes, also undergo programmed cell death leading to an abnormally low concentration of lymphocytes in the blood.[57] This contributes to the weakened immune response seen in those infected with EBOV.[57]
Endothelial cells may be infected within three days after exposure to the virus.[52] The breakdown of endothelial cells leading to blood vessel injury can be attributed to EBOV glycoproteins. This damage occurs due to the synthesis of Ebola virus glycoprotein (GP), which reduces the availability of specific integrins responsible for cell adhesion to the intercellular structure and causes liver damage, leading to improper clotting. The widespread bleeding that occurs in affected people causes swelling and shock due to loss of blood volume.[97] The dysfunctional bleeding and clotting commonly seen in EVD has been attributed to increased activation of the extrinsic pathway of the coagulation cascade due to excessive tissue factor production by macrophages and monocytes.[25]
After infection, a secreted glycoprotein, small soluble glycoprotein (sGP or GP) is synthesised. EBOV replication overwhelms protein synthesis of infected cells and the host immune defences. The GP forms a trimeric complex, which tethers the virus to the endothelial cells. The sGP forms a dimeric protein that interferes with the signalling of neutrophils, another type of white blood cell. This enables the virus to evade the immune system by inhibiting early steps of neutrophil activation.[medical citation needed] Furthermore, the virus is capable of hijacking cellular metabolism. Studies have shown that Ebola virus-like particles can reprogram metabolism in both vascular and immune cells.[98]
Immune system evasion
Filoviral infection also interferes with proper functioning of the innate immune system.[53][55] EBOV proteins blunt the human immune system's response to viral infections by interfering with the cells' ability to produce and respond to interferon proteins such as interferon-alpha, interferon-beta, and interferon gamma.[54][99]
The VP24 and VP35 structural proteins of EBOV play a key role in this interference. When a cell is infected with EBOV, receptors located in the cell's cytosol (such as RIG-I and MDA5) or outside of the cytosol (such as Toll-like receptor 3 (TLR3), TLR7, TLR8 and TLR9) recognise infectious molecules associated with the virus.[54] On TLR activation, proteins including interferon regulatory factor 3 and interferon regulatory factor 7 trigger a signalling cascade that leads to the expression of type 1 interferons.[54] The type 1 interferons are then released and bind to the IFNAR1 and IFNAR2 receptors expressed on the surface of a neighbouring cell.[54] Once interferon has bound to its receptors on the neighbouring cell, the signalling proteins STAT1 and STAT2 are activated and move to the cell's nucleus.[54] This triggers the expression of interferon-stimulated genes, which code for proteins with antiviral properties.[54] EBOV's V24 protein blocks the production of these antiviral proteins by preventing the STAT1 signalling protein in the neighbouring cell from entering the nucleus.[54] The VP35 protein directly inhibits the production of interferon-beta.[99] By inhibiting these immune responses, EBOV may quickly spread throughout the body.[52]
Diagnosis
When EVD is suspected, travel, work history, and exposure to wildlife are important factors with respect to further diagnostic efforts.[100]
Laboratory testing
Possible non-specific laboratory indicators of EVD include a low platelet count; an initially decreased white blood cell count followed by an increased white blood cell count; elevated levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST); and abnormalities in blood clotting often consistent with disseminated intravascular coagulation (DIC) such as a prolonged prothrombin time, partial thromboplastin time, and bleeding time.[101] Filovirions such as EBOV may be identified by their unique filamentous shapes in cell cultures examined with electron microscopy.[102]
The specific diagnosis of EVD is confirmed by isolating the virus, detecting its RNA or proteins, or detecting antibodies against the virus in a person's blood.[103] Isolating the virus by cell culture, detecting the viral RNA by polymerase chain reaction (PCR)[8][25] and detecting proteins by enzyme-linked immunosorbent assay (ELISA) are methods best used in the early stages of the disease and also for detecting the virus in human remains.[8][103] Detecting antibodies against the virus is most reliable in the later stages of the disease and in those who recover.[103] IgM antibodies are detectable two days after symptom onset and IgG antibodies can be detected six to 18 days after symptom onset.[25] During an outbreak, isolation of the virus with cell culture methods is often not feasible. In field or mobile hospitals, the most common and sensitive diagnostic methods are real-time PCR and ELISA.[104] In 2014, with new mobile testing facilities deployed in parts of Liberia, test results were obtained 3–5 hours after sample submission.[105] In 2015, a rapid antigen test which gives results in 15 minutes was approved for use by WHO.[106] It is able to confirm Ebola in 92% of those affected and rule it out in 85% of those not affected.[106]
Differential diagnosis
Early symptoms of EVD may be similar to those of other diseases common in Africa, including malaria and dengue fever.[27] The symptoms are also similar to those of other viral haemorrhagic fevers such as Marburg virus disease, Crimean–Congo haemorrhagic fever, and Lassa fever.[107][108]
The complete differential diagnosis is extensive and requires consideration of many other infectious diseases such as typhoid fever, shigellosis, rickettsial diseases, cholera, sepsis, borreliosis, EHEC enteritis, leptospirosis, scrub typhus, plague, Q fever, candidiasis, histoplasmosis, trypanosomiasis, visceral leishmaniasis, measles, and viral hepatitis among others.[109]
Non-infectious diseases that may result in symptoms similar to those of EVD include acute promyelocytic leukaemia, haemolytic uraemic syndrome, snake envenomation, clotting factor deficiencies/platelet disorders, thrombotic thrombocytopenic purpura, hereditary haemorrhagic telangiectasia, Kawasaki disease, and warfarin poisoning.[104][110][111][112]
Prevention
Vaccines
An Ebola vaccine, rVSV-ZEBOV, was approved in the United States in December 2019.[10] It appears to be fully effective ten days after being given.[10] It was studied in Guinea between 2014 and 2016.[10] More than 100,000 people have been vaccinated against Ebola as of 2019[update].[113] The WHO reported that approximately 345,000 people were given the vaccine during the Kivu Ebola epidemic from 2018 to 2020.[114]
Infection control

Community awareness of the benefits on survival chances of admitting cases early is important for the infected and infection control [4]
Caregivers

People who care for those infected with Ebola should wear protective clothing including masks, gloves, gowns and goggles.[115] The U.S. Centers for Disease Control (CDC) recommend that the protective gear leaves no skin exposed.[116] These measures are also recommended for those who may handle objects contaminated by an infected person's body fluids.[117] In 2014, the CDC began recommending that medical personnel receive training on the proper suit-up and removal of personal protective equipment (PPE); in addition, a designated person, appropriately trained in biosafety, should be watching each step of these procedures to ensure they are done correctly.[116] In Sierra Leone, the typical training period for the use of such safety equipment lasts approximately 12 days.[118] In 2022 in Uganda, lighter personal protection equipment has become available as well as possibilities to monitor and communicate with patients from windows in the treatment tents until it is necessary to enter if e.g. a patient's oxygen levels drop. [4]
Patients and household members
The infected person should be in barrier-isolation from other people.[115] All equipment, medical waste, patient waste and surfaces that may have come into contact with body fluids need to be disinfected.[117] During the 2014 outbreak, kits were put together to help families treat Ebola disease in their homes, which included protective clothing as well as chlorine powder and other cleaning supplies.[119] Education of caregivers in these techniques, and providing such barrier-separation supplies has been a priority of Doctors Without Borders.[120]
Disinfection
Ebolaviruses can be eliminated with heat (heating for 30 to 60 minutes at 60 °C or boiling for five minutes). To disinfect surfaces, some lipid solvents such as some alcohol-based products, detergents, sodium hypochlorite (bleach) or calcium hypochlorite (bleaching powder), and other suitable disinfectants may be used at appropriate concentrations.[84][121]
General population
Education of the general public about the risk factors for Ebola infection and of the protective measures individuals may take to prevent infection is recommended by the World Health Organization.[1] These measures include avoiding direct contact with infected people and regular hand washing using soap and water.[122]
Bushmeat
Bushmeat, an important source of protein in the diet of some Africans, should be handled and prepared with appropriate protective clothing and thoroughly cooked before consumption.[1] Some research suggests that an outbreak of Ebola disease in the wild animals used for consumption may result in a corresponding human outbreak. Since 2003, such animal outbreaks have been monitored to predict and prevent Ebola outbreaks in humans.[123]
Corpses, burial
If a person with Ebola disease dies, direct contact with the body should be avoided.[115] Certain burial rituals, which may have included making various direct contacts with a dead body, require reformulation so that they consistently maintain a proper protective barrier between the dead body and the living.[124][125][126] Social anthropologists may help find alternatives to traditional rules for burials.[127]
Transport, travel, contact
Transportation crews are instructed to follow a certain isolation procedure, should anyone exhibit symptoms resembling EVD.[128] As of August 2014[update], the WHO does not consider travel bans to be useful in decreasing spread of the disease.[70] In October 2014, the CDC defined four risk levels used to determine the level of 21-day monitoring for symptoms and restrictions on public activities.[129] In the United States, the CDC recommends that restrictions on public activity, including travel restrictions, are not required for the following defined risk levels:[129]
- having been in a country with widespread Ebola disease transmission and having no known exposure (low risk); or having been in that country more than 21 days ago (no risk)
- encounter with a person showing symptoms; but not within three feet of the person with Ebola without wearing PPE; and no direct contact with body fluids
- having had brief skin contact with a person showing symptoms of Ebola disease when the person was believed to be not very contagious (low risk)
- in countries without widespread Ebola disease transmission: direct contact with a person showing symptoms of the disease while wearing PPE (low risk)
- contact with a person with Ebola disease before the person was showing symptoms (no risk).
The CDC recommends monitoring for the symptoms of Ebola disease for those both at "low risk" and at higher risk.[129]
Laboratory
In laboratories where diagnostic testing is carried out, biosafety level 4-equivalent containment is required.[130] Laboratory researchers must be properly trained in BSL-4 practices and wear proper PPE.[130]
Isolation
Isolation refers to separating those who are sick from those who are not. Quarantine refers to separating those who may have been exposed to a disease until they either show signs of the disease or are no longer at risk.[131] Quarantine, also known as enforced isolation, is usually effective in decreasing spread.[132][133] Governments often quarantine areas where the disease is occurring or individuals who may transmit the disease outside of an initial area.[134] In the United States, the law allows quarantine of those infected with ebolaviruses.[135][136]
Contact tracing
Contact tracing is considered important to contain an outbreak. It involves finding everyone who had close contact with infected individuals and monitoring them for signs of illness for 21 days. If any of these contacts comes down with the disease, they should be isolated, tested and treated. Then the process is repeated, tracing the contacts' contacts.[137][138]
Management
As of 2019[update] two treatments (atoltivimab/maftivimab/odesivimab and ansuvimab) are associated with improved outcomes.[11][12] The U.S. Food and Drug Administration (FDA) advises people to be careful of advertisements making unverified or fraudulent claims of benefits supposedly gained from various anti-Ebola products.[139][140]
In October 2020, the U.S. Food and Drug Administration (FDA) approved atoltivimab/maftivimab/odesivimab with an indication for the treatment of infection caused by Zaire ebolavirus.[13]
Standard support

Treatment is primarily supportive in nature.[141] Early supportive care with rehydration and symptomatic treatment improves survival.[1] Rehydration may be via the oral or intravenous route.[141] These measures may include pain management, and treatment for nausea, fever, and anxiety.[141] The World Health Organization (WHO) recommends avoiding aspirin or ibuprofen for pain management, due to the risk of bleeding associated with these medications.[142]
Blood products such as packed red blood cells, platelets, or fresh frozen plasma may also be used.[141] Other regulators of coagulation have also been tried including heparin in an effort to prevent disseminated intravascular coagulation and clotting factors to decrease bleeding.[141] Antimalarial medications and antibiotics are often used before the diagnosis is confirmed,[141] though there is no evidence to suggest such treatment helps. Several experimental treatments are being studied.[143]
Where hospital care is not possible, the WHO's guidelines for home care have been relatively successful. Recommendations include using towels soaked in a bleach solution when moving infected people or bodies and also applying bleach on stains. It is also recommended that the caregivers wash hands with bleach solutions and cover their mouth and nose with a cloth.[144]
Intensive care
Intensive care is often used in the developed world.[35] This may include maintaining blood volume and electrolytes (salts) balance as well as treating any bacterial infections that may develop.[35] Dialysis may be needed for kidney failure, and extracorporeal membrane oxygenation may be used for lung dysfunction.[35]
Prognosis
EVD has a risk of death in those infected of between 25% and 90%.[1][145] As of September 2014[update], the average risk of death among those infected is 50%.[1] The highest risk of death was 90% in the 2002–2003 Republic of the Congo outbreak.[146] Early admission significantly increases survival rates [4]
Death, if it occurs, follows typically six to sixteen days after symptoms appear and is often due to low blood pressure from fluid loss.[2] Early supportive care to prevent dehydration may reduce the risk of death.[143]
Post-Ebola virus syndrome
If an infected person survives, recovery may be quick and complete.[25][147] However, a large portion of survivors develop post-Ebola virus syndrome after the acute phase of the infection.[148]
Prolonged cases are often complicated by the occurrence of long-term problems, such as inflammation of the testicles, joint pains, fatigue, hearing loss, mood and sleep disturbances, muscular pain, abdominal pain, menstrual abnormalities, miscarriages, skin peeling, or hair loss.[25][147] Inflammation and swelling of the uveal layer of the eye is the most common eye complication in survivors of Ebola virus disease.[147] Eye symptoms, such as light sensitivity, excess tearing, and vision loss have been described.[149]
Ebola can stay in some body parts like the eyes,[150] breasts, and testicles after infection.[6][151] Sexual transmission after recovery has been suspected.[152][153] If sexual transmission occurs following recovery it is believed to be a rare event.[154] One case of a condition similar to meningitis has been reported many months after recovery, as of October 2015[update].[155]
Epidemiology
The disease typically occurs in outbreaks in tropical regions of Sub-Saharan Africa.[1] From 1976 (when it was first identified) through 2013, the WHO reported 2,387 confirmed cases with 1,590 overall fatalities.[1][14] The largest outbreak to date was the Ebola virus epidemic in West Africa, which caused a large number of deaths in Guinea, Sierra Leone, and Liberia.[16][17]
1976
Sudan

The first known outbreak of EVD was identified only after the fact. It occurred between June and November 1976, in Nzara, South Sudan[44][156] (then part of Sudan), and was caused by Sudan virus (SUDV). The Sudan outbreak infected 284 people and killed 151. The first identifiable case in Sudan occurred on 27 June in a storekeeper in a cotton factory in Nzara, who was hospitalised on 30 June and died on 6 July.[35][157] Although the WHO medical staff involved in the Sudan outbreak knew that they were dealing with a heretofore unknown disease, the actual "positive identification" process and the naming of the virus did not occur until some months later in Zaire.[157]
Zaire

On 26 August 1976, the second outbreak of EVD began in Yambuku, a small rural village in Mongala District in northern Zaire (now known as the Democratic Republic of the Congo).[158][159] This outbreak was caused by EBOV, formerly designated Zaire ebolavirus, a different member of the genus Ebolavirus than in the first Sudan outbreak. The first person infected with the disease was the village school's headmaster Mabalo Lokela, who began displaying symptoms on 26 August 1976.[160] Lokela had returned from a trip to Northern Zaire near the border of the Central African Republic, after visiting the Ebola River between 12 and 22 August. He was originally believed to have malaria and was given quinine. However, his symptoms continued to worsen, and he was admitted to Yambuku Mission Hospital on 5 September. Lokela died on 8 September 14 days after he began displaying symptoms.[161][162]
Soon after Lokela's death, others who had been in contact with him also died, and people in Yambuku began to panic. The country's Minister of Health and Zaire President Mobutu Sese Seko declared the entire region, including Yambuku and the country's capital, Kinshasa, a quarantine zone. No-one was permitted to enter or leave the area, and roads, waterways, and airfields were placed under martial law. Schools, businesses and social organisations were closed.[163] The initial response was led by Congolese doctors, including Jean-Jacques Muyembe-Tamfum, one of the discoverers of Ebola. Muyembe took a blood sample from a Belgian nun; this sample would eventually be used by Peter Piot to identify the previously unknown Ebola virus.[164] Muyembe was also the first scientist to come into direct contact with the disease and survive.[165] Researchers from the Centers for Disease Control and Prevention (CDC), including Piot, co-discoverer of Ebola, later arrived to assess the effects of the outbreak, observing that "the whole region was in panic."[166][167][168]
Piot concluded that Belgian nuns had inadvertently started the epidemic by giving unnecessary vitamin injections to pregnant women without sterilizing the syringes and needles. The outbreak lasted 26 days and the quarantine lasted two weeks. Researchers speculated that the disease disappeared due to the precautions taken by locals, the quarantine of the area, and discontinuing of the injections.[163]
During this outbreak, Ngoy Mushola recorded the first clinical description of EVD in Yambuku, where he wrote the following in his daily log: "The illness is characterised with a high temperature of about 39 °C (102 °F), haematemesis, diarrhoea with blood, retrosternal abdominal pain, prostration with 'heavy' articulations, and rapid evolution death after a mean of three days."[169]
The virus responsible for the initial outbreak, first thought to be the Marburg virus, was later identified as a new type of virus related to the genus Marburgvirus. Virus strain samples isolated from both outbreaks were named "Ebola virus" after the Ebola River, near the first-identified viral outbreak site in Zaire.[35] Reports conflict about who initially coined the name: either Karl Johnson of the American CDC team[170] or Belgian researchers.[171] Subsequently, a number of other cases were reported, almost all centred on the Yambuku mission hospital or close contacts of another case.[160] In all, 318 cases and 280 deaths (an 88% fatality rate) occurred in Zaire.[172] Although the two outbreaks were at first believed connected, scientists later realised that they were caused by two distinct ebolaviruses, SUDV and EBOV.[159]
1995–2014

The second major outbreak occurred in Zaire (now the Democratic Republic of the Congo, DRC), in 1995, affecting 315 and killing 254.[1]
In 2000, Uganda had an outbreak infecting 425 and killing 224; in this case, the Sudan virus was found to be the Ebola species responsible for the outbreak.[1]
In 2003, an outbreak in the DRC infected 143 and killed 128, a 90% death rate, the highest of a genus Ebolavirus outbreak to date.[173]
In 2004, a Russian scientist died from Ebola after sticking herself with an infected needle.[174]
Between April and August 2007, a fever epidemic[175] in a four-village region[176] of the DRC was confirmed in September to have been cases of Ebola.[177] Many people who attended the recent funeral of a local village chief died.[176] The 2007 outbreak eventually infected 264 individuals and killed 187.[1]
On 30 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the Bundibugyo District in Western Uganda. After confirming samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization (WHO) confirmed the presence of a new species of genus Ebolavirus, which was tentatively named Bundibugyo.[178] The WHO reported 149 cases of this new strain and 37 of those led to deaths.[1]
The WHO confirmed two small outbreaks in Uganda in 2012, both caused by the Sudan variant. The first outbreak affected seven people, killing four, and the second affected 24, killing 17.[1]
On 17 August 2012, the Ministry of Health of the DRC reported an outbreak of the Ebola-Bundibugyo variant[179] in the eastern region.[180][181] Other than its discovery in 2007, this was the only time that this variant has been identified as responsible for an outbreak. The WHO revealed that the virus had sickened 57 people and killed 29. The probable cause of the outbreak was tainted bush meat hunted by local villagers around the towns of Isiro and Viadana.[1][182]
In 2014, an outbreak occurred in the DRC. Genome-sequencing showed that this outbreak was not related to the 2014–15 West Africa Ebola virus outbreak, but was the same EBOV species, the Zaire species.[183] It began in August 2014, and was declared over in November with 66 cases and 49 deaths.[184] This was the 7th outbreak in the DRC, three of which occurred during the period when the country was known as Zaire.[185]
2013–2016 West Africa
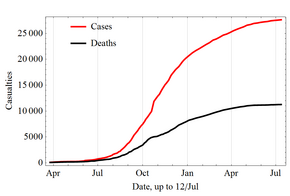
In March 2014, the World Health Organization (WHO) reported a major Ebola outbreak in Guinea, a West African nation.[186] Researchers traced the outbreak to a one-year-old child who died in December 2013.[187][188] The disease rapidly spread to the neighbouring countries of Liberia and Sierra Leone. It was the largest Ebola outbreak ever documented, and the first recorded in the region.[186] On 8 August 2014, the WHO declared the epidemic an international public health emergency. Urging the world to offer aid to the affected regions, its Director-General said, "Countries affected to date simply do not have the capacity to manage an outbreak of this size and complexity on their own. I urge the international community to provide this support on the most urgent basis possible."[189] By mid-August 2014, Doctors Without Borders reported the situation in Liberia's capital, Monrovia, was "catastrophic" and "deteriorating daily". They reported that fears of Ebola among staff members and patients had shut down much of the city's health system, leaving many people without medical treatment for other conditions.[190] In a 26 September statement, WHO said, "The Ebola epidemic ravaging parts of West Africa is the most severe acute public health emergency seen in modern times. Never before in recorded history has a biosafety level four pathogen infected so many people so quickly, over such a broad geographical area, for so long."[191]
Intense contact tracing and strict isolation largely prevented further spread of the disease in the countries that had imported cases.
It caused significant mortality, with a considerable case fatality rate.[192][193][194][note 1] By the end of the epidemic, 28,616 people had been infected; of these, 11,310 had died, for a case-fatality rate of 40%.[195] As of 8 May 2016[update], 28,646 suspected cases and 11,323 deaths were reported;[15][196] however, the WHO said that these numbers may be underestimated.[197] Because they work closely with the body fluids of infected patients, healthcare workers were especially vulnerable to infection; in August 2014, the WHO reported that 10% of the dead were healthcare workers.[198]

In September 2014, it was estimated that the countries' capacity for treating Ebola patients was insufficient by the equivalent of 2,122 beds; by December there were a sufficient number of beds to treat and isolate all reported Ebola cases, although the uneven distribution of cases was causing serious shortfalls in some areas.[199] On 28 January 2015, the WHO reported that for the first time since the week ending 29 June 2014, there had been fewer than 100 new confirmed cases reported in a week in the three most-affected countries. The response to the epidemic then moved to a second phase, as the focus shifted from slowing transmission to ending the epidemic.[200] On 8 April 2015, the WHO reported only 30 confirmed cases, the lowest weekly total since the third week of May 2014.[201]
On 29 December 2015, 42 days after the last person tested negative for a second time, Guinea was declared free of Ebola transmission.[202] At that time, a 90-day period of heightened surveillance was announced by that agency. "This is the first time that all three countries – Guinea, Liberia and Sierra Leone – have stopped the original chains of transmission ...", the organisation stated in a news release.[203] A new case was detected in Sierra Leone on 14 January 2016.[204] However, the outbreak was declared no longer an emergency on 29 March 2016.[18]
2014 spread outside West Africa
On 19 September, Eric Duncan flew from his native Liberia to Texas; five days later he began showing symptoms and visited a hospital but was sent home. His condition worsened and he returned to the hospital on 28 September, where he died on 8 October. Health officials confirmed a diagnosis of Ebola on 30 September – the first case in the United States.[205]
In early October, Teresa Romero, a 44-year-old Spanish nurse, contracted Ebola after caring for a priest who had been repatriated from West Africa. This was the first transmission of the virus to occur outside Africa.[206] Romero tested negative for the disease on 20 October, suggesting that she may have recovered from Ebola infection.[207]
On 12 October, the Centers for Disease Control and Prevention (CDC) confirmed that a nurse in Texas, Nina Pham, who had treated Duncan tested positive for the Ebola virus, the first known case of transmission in the United States.[208] On 15 October, a second Texas health-care worker who had treated Duncan was confirmed to have the virus.[77][209] Both of these people recovered.[210] An unrelated case involved a doctor in New York City, who returned to the United States from Guinea after working with Médecins Sans Frontières and tested positive for Ebola on 23 October.[211] The person recovered and was discharged from Bellevue Hospital on 11 November.[210] On 24 December 2014, a laboratory in Atlanta, Georgia reported that a technician had been exposed to Ebola.[212]
On 29 December 2014, Pauline Cafferkey, a British nurse who had just returned to Glasgow from Sierra Leone, was diagnosed with Ebola at Glasgow's Gartnavel General Hospital.[213] After initial treatment in Glasgow, she was transferred by air to RAF Northolt, then to the specialist high-level isolation unit at the Royal Free Hospital in London for longer-term treatment.[214]
2017 Democratic Republic of the Congo
On 11 May 2017, the DRC Ministry of Public Health notified the WHO about an outbreak of Ebola. Four people died, and four people survived; five of these eight cases were laboratory-confirmed. A total of 583 contacts were monitored. On 2 July 2017, the WHO declared the end of the outbreak.[215]
2018 Équateur province
On 14 May 2018, the World Health Organization reported that "the Democratic Republic of Congo reported 39 suspected, probable or confirmed cases of Ebola between 4 April and 13 May, including 19 deaths."[216] Some 393 people identified as contacts of Ebola patients were being followed up. The outbreak centred on the Bikoro, Iboko, and Wangata areas in Equateur province,[216] including in the large city of Mbandaka. The DRC Ministry of Public Health approved the use of an experimental vaccine.[217][218][219] On 13 May 2018, WHO Director-General Tedros Adhanom Ghebreyesus visited Bikoro.[220] Reports emerged that maps of the area were inaccurate, not so much hampering medical providers as epidemiologists and officials trying to assess the outbreak and containment efforts.[221] The 2018 outbreak in the DRC was declared over on 24 July 2018.[22]
2018–2020 Kivu
On 1 August 2018, the world's 10th Ebola outbreak was declared in North Kivu province of the Democratic Republic of the Congo. It was the first Ebola outbreak in a military conflict zone, with thousands of refugees in the area.[222][223] By November 2018, nearly 200 Congolese had died of Ebola, about half of them from the city of Beni, where armed groups are fighting over the region's mineral wealth, impeding medical relief efforts.[224]
By March 2019, this became the second largest Ebola outbreak ever recorded, with more than 1,000 cases and insecurity continuing to be the major resistance to providing an adequate response.[225][226] As of 4 June 2019[update], the WHO reported 2025 confirmed and probable cases with 1357 deaths.[227] In June 2019, two people died of Ebola in neighbouring Uganda.[228]
In July 2019, an infected man travelled to Goma, home to more than two million people.[229] One week later, on 17 July 2019, the WHO declared the Ebola outbreak a global health emergency, the fifth time such a declaration has been made by the organisation.[230] A government spokesman said that half of the Ebola cases are unidentified, and he added that the current outbreak could last up to three years.[231]
On 25 June 2020, the second biggest EVD outbreak ever was declared over.[232]
2020 Équateur province
On 1 June 2020, the Congolese health ministry announced a new DRC outbreak of Ebola in Mbandaka, Équateur Province, a region along the Congo River. Genome sequencing suggests that this outbreak, the 11th outbreak since the virus was first discovered in the country in 1976, is unrelated to the one in North Kivu Province or the previous outbreak in the same area in 2018. It was reported that six cases had been identified; four of the people had died. It is expected that more people will be identified as surveillance activities increase.[233] By 15 June the case count had increased to 17 with 11 deaths, with more than 2,500 people having been vaccinated.[234] The 11th EVD outbreak was officially declared over on 19 November 2020.[235] By the time the Équateur outbreak ended, it had 130 confirmed cases with 75 recoveries and 55 deaths.
2021
North Kivu
On 7 February 2021, the Congolese health ministry announced a new case of Ebola near Butembo, North Kivu detected a day before. The case was a 42-year-old woman who had symptoms of Ebola in Biena on 1 February 2021. A few days after, she died in a hospital in Butembo. The WHO said that more than 70 people with contact with the woman had been tracked.[236][237]
On 11 February 2021, another woman who had contact with the previous woman died in the same town, and the number of traced contacts increased to 100.[238] A day after, a third case was detected in Butembo.[239]
On 3 May 2021, the 12th EVD outbreak was declared over, resulting in 12 cases and six deaths.[240][241] Heightened surveillance will continue for 90 days after the declaration, in case of resurgence.[240]
Guinea
In February 2021, Sakoba Keita, head of Guinea's national health agency confirmed that three people had died of Ebola in the south-eastern region near the city of Nzérékoré. A further five people also tested positive. Keita also confirmed more testing was underway, and attempts to trace and isolate further cases had begun.[242] On 14 February, the Guinean government declared an Ebola epidemic.[243] The outbreak may have started following reactivation of a latent case in a survivor of an earlier outbreak.[244][245] As of 4 May 2021, 23 cases were reported, with no new cases or deaths since 3 April 2021.[240] A 42-day countdown period was started on 8 May 2021, and on 19 June, the outbreak was declared over.[240][246]
Ivory Coast
On 14 August 2021, The Ministry of Health of Cote d’Ivoire confirmed the country's first case of Ebola since 1994. This came after the Institut Pasteur in Cote d'Ivoire confirmed the Ebola Virus Disease in samples collected from a patient, who was hospitalized in the commercial capital of Abidjan, after arriving from Guinea.[247]
However, on 31 August 2021, the WHO found that, after further tests in a laboratory in Lyon, the patient did not have Ebola. The cause of her disease is still being analyzed.[248]
2022
On 23 April 2022, a case of Ebola was confirmed in the DRC in the Equateur province. The case was a 31-year-old man whose symptoms began on 5 April, but did not seek treatment for over a week. On 21 April, he was admitted to an Ebola treatment centre and died later that day.[249] By 24 May 2022, there were 5 recorded deaths in the DRC.[250] On 15 August, the fifth case was buried, and the outbreak was declared over, 42 days after, on 4 July 2022.[251]
In September 2022, Uganda reported 7 cases infected with the Ebola Sudan strain,[252] but by mid-October the count had increased to 63.[253] In November 2022, the outbreak in Uganda continued - still without a vaccine.[4] On 10 January 2023, the outbreak was considered over after no new cases had been reported for 42 days; the outbreak killed nearly 80 people.[254]
Society and culture
Weaponisation
Ebolavirus is classified as a biosafety level 4 agent, as well as a Category A bioterrorism agent by the Centers for Disease Control and Prevention.[96][255] It has the potential to be weaponised for use in biological warfare,[256][257] and was investigated by Biopreparat for such use, but might be difficult to prepare as a weapon of mass destruction because the virus becomes ineffective quickly in open air.[258] Fake emails pretending to be Ebola information from the WHO or the Mexican government have, in 2014, been misused to spread computer malware.[259] The BBC reported in 2015 that "North Korean state media has suggested the disease was created by the U.S. military as a biological weapon."[260]
Literature
Richard Preston's 1995 best-selling book, The Hot Zone, dramatised the Ebola outbreak in Reston, Virginia.[261][262][263]
William Close's 1995 Ebola: A Documentary Novel of Its First Explosion[264][265] and 2002 Ebola: Through the Eyes of the People focused on individuals' reactions to the 1976 Ebola outbreak in Zaire.[266][267]
Tom Clancy's 1996 novel, Executive Orders, involves a Middle Eastern terrorist attack on the United States using an airborne form of a deadly Ebola virus strain named "Ebola Mayinga" (see Mayinga N'Seka).[268][269]
As the Ebola virus epidemic in West Africa developed in 2014, a number of popular self-published and well-reviewed books containing sensational and misleading information about the disease appeared in electronic and printed formats. The authors of some such books admitted that they lacked medical credentials and were not technically qualified to give medical advice. The World Health Organization and the United Nations stated that such misinformation had contributed to the spread of the disease.[270]
Other animals
Wild animals
Ebola has a high mortality rate among primates.[271] Frequent outbreaks of Ebola may have resulted in the deaths of 5,000 gorillas.[272] Outbreaks of Ebola may have been responsible for an 88% decline in tracking indices of observed chimpanzee populations in the 420 km2 Lossi Sanctuary between 2002 and 2003.[273] Transmission among chimpanzees through meat consumption constitutes a significant risk factor, whereas contact between the animals, such as touching dead bodies and grooming, is not.[274]
Recovered gorilla carcasses have contained multiple Ebola virus strains, suggesting multiple introductions of the virus. Bodies decompose quickly and carcasses are not infectious after three to four days. Contact between gorilla groups is rare, suggesting that transmission among gorilla groups is unlikely, and that outbreaks result from transmission between viral reservoirs and animal populations.[273]
Domestic animals
In 2012, it was demonstrated that the virus can travel without contact from pigs to nonhuman primates, although the same study failed to achieve transmission in that manner between primates.[86][275]
Dogs may become infected with EBOV but not develop symptoms. Dogs in some parts of Africa scavenge for food, and they sometimes eat EBOV-infected animals and also the corpses of humans. A 2005 survey of dogs during an EBOV outbreak found that although they remain asymptomatic, about 32 percent of dogs closest to an outbreak showed a seroprevalence for EBOV versus nine percent of those farther away.[276] The authors concluded that there were "potential implications for preventing and controlling human outbreaks."
Reston virus
In late 1989, Hazelton Research Products' Reston Quarantine Unit in Reston, Virginia, had an outbreak of fatal illness amongst certain lab monkeys. This lab outbreak was initially diagnosed as simian haemorrhagic fever virus (SHFV) and occurred amongst a shipment of crab-eating macaque monkeys imported from the Philippines. Hazelton's veterinary pathologist in Reston sent tissue samples from dead animals to the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) at Fort Detrick, Maryland, where an ELISA test indicated the antibodies present in the tissue were a response to Ebola virus and not SHFV.[277] An electron microscopist from USAMRIID discovered filoviruses similar in appearance, in crystalloid aggregates and as single filaments with a shepherd's hook, to Ebola in the tissue samples sent from Hazelton Research Products' Reston Quarantine Unit.[278]
A US Army team headquartered at USAMRIID euthanised the surviving monkeys, and brought all the dead monkeys to Fort Detrick for study by the Army's veterinary pathologists and virologists, and eventual disposal under safe conditions.[277] Blood samples were taken from 178 animal handlers during the incident.[279] Of those, six animal handlers eventually seroconverted, including one who had cut himself with a bloody scalpel.[97][280] Despite its status as a Level‑4 organism and its apparent pathogenicity in monkeys, when the handlers did not become ill, the CDC concluded that the virus had a very low pathogenicity to humans.[280][281]
The Philippines and the United States had no previous cases of Ebola infection, and upon further isolation, researchers concluded it was another strain of Ebola, or a new filovirus of Asian origin, which they named Reston ebolavirus (RESTV) after the location of the incident.[277] Reston virus (RESTV) can be transmitted to pigs.[86] Since the initial outbreak it has since been found in nonhuman primates in Pennsylvania, Texas, and Italy,[282] where the virus had infected pigs.[283] According to the WHO, routine cleaning and disinfection of pig (or monkey) farms with sodium hypochlorite or detergents should be effective in inactivating the Reston ebolavirus. Pigs that have been infected with RESTV tend to show symptoms of the disease.[284]
Research
Treatments

As of July 2015[update], no medication has been proven safe and effective for treating Ebola. By the time the Ebola virus epidemic in West Africa began in 2013, there were at least nine different candidate treatments. Several trials were conducted in late 2014, and early 2015, but some were abandoned due to lack of efficacy or lack of people to study.[285]
As of August 2019[update], two experimental treatments known as atoltivimab/maftivimab/odesivimab and ansuvimab were found to be 90% effective.[286][287][288]
Diagnostic tests
The diagnostic tests currently available require specialised equipment and highly trained personnel. Since there are few suitable testing centres in West Africa, this leads to delay in diagnosis.[289]
On 29 November 2014, a new 15-minute Ebola test was reported that if successful, "not only gives patients a better chance of survival, but it prevents transmission of the virus to other people." The new equipment, about the size of a laptop and solar-powered, allows testing to be done in remote areas.[290]
On 29 December 2014, the U.S. Food and Drug Administration (FDA) approved the LightMix Ebola Zaire rRT-PCR test for patients with symptoms of Ebola.[291]
Disease models
Animal models and in particular non-human primates are being used to study different aspects of Ebola virus disease. Developments in organ-on-a-chip technology have led to a chip-based model for Ebola haemorrhagic syndrome.[292]
See also
Notes
- ^ The mortality (number of dead per number of healthy per time frame) recorded in Liberia up to 26 August 2014 was 70%.[194] However, due to the estimation method used, the estimated case fatality rate (70.8%) for this particular epidemic differs from the actual ratio between the number of deaths and the number of cases.
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar "Ebola virus disease, Fact sheet N°103, Updated September 2014". World Health Organization (WHO). September 2014. Archived from the original on 14 December 2014. Retrieved 15 December 2014.
- ^ a b c d Singh SK, Ruzek D, eds. (2014). Viral hemorrhagic fevers. Boca Raton: CRC Press, Taylor & Francis Group. p. 444. ISBN 978-1439884294. Archived from the original on 29 April 2016.
- ^ Modrow S, Falke D, Truyen U, Schätzl H (2013). "Viruses: Definition, Structure, Classification". In Modrow S, Falke D, Truyen U, Schätzl H (eds.). Molecular Virology. Berlin, Heidelberg: Springer. pp. 17–30. doi:10.1007/978-3-642-20718-1_2. ISBN 978-3-642-20718-1. S2CID 83235976.
- ^ a b c d e Ebola in Uganda: Guiliani R. "Our game-changing treatment centres will save more lives". msf.org.urk. Archived from the original on 15 November 2022. Retrieved 15 November 2022.
- ^ a b "2014 Ebola Virus Disease (EVD) outbreak in West Africa". World Health Organization (WHO). 21 April 2014. Archived from the original on 29 July 2014. Retrieved 3 August 2014.
- ^ a b c d "Preliminary study finds that Ebola virus fragments can persist in the semen of some survivors for at least nine months". Centers for Disease Control and Prevention (CDC). 14 October 2015. Archived from the original on 24 August 2017.
- ^ a b "Recommendations for Breastfeeding/Infant Feeding in the Context of Ebola". Centers for Disease Control and Prevention (CDC). 19 September 2014. Archived from the original on 24 October 2014. Retrieved 26 October 2014.
- ^ a b c Broadhurst MJ, Brooks TJ, Pollock NR (13 July 2016). "Diagnosis of Ebola Virus Disease: Past, Present, and Future". Clinical Microbiology Reviews. 29 (4). American Society for Microbiology: 773–793. doi:10.1128/cmr.00003-16. ISSN 0893-8512. LCCN 88647279. OCLC 38839512. PMC 5010747. PMID 27413095.
- ^ "Guidance for Safe Handling of Human Remains of Ebola Patients in U.S. Hospitals and Mortuaries". Centers for Disease Control and Prevention (CDC). Archived from the original on 9 October 2014. Retrieved 10 October 2014.
- ^ a b c d "First FDA-approved vaccine for the prevention of Ebola virus disease, marking a critical milestone in public health preparedness and response" (Press release). U.S. Food and Drug Administration (FDA). 20 December 2019. Archived from the original on 20 December 2019. Retrieved 22 December 2019.
- ^ a b "Ebola Treatment Research". NIH: National Institute of Allergy and Infectious Diseases. Archived from the original on 20 August 2019. Retrieved 20 August 2019.
- ^ a b "Independent Monitoring Board Recommends Early Termination of Ebola Therapeutics Trial in DRC Because of Favorable Results with Two of Four Candidates". NIH: National Institute of Allergy and Infectious Diseases. 12 August 2019. Archived from the original on 19 August 2019. Retrieved 20 August 2019.
- ^ a b "FDA Approves First Treatment for Ebola Virus". U.S. Food and Drug Administration (FDA) (Press release). 14 October 2020. Archived from the original on 15 October 2020. Retrieved 14 October 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ a b Dixon MG, Schafer IJ (June 2014). "Ebola viral disease outbreak – West Africa, 2014" (PDF). MMWR Morb. Mortal. Wkly. Rep. 63 (25): 548–551. PMC 5779383. PMID 24964881. Archived (PDF) from the original on 23 October 2020. Retrieved 7 April 2020.
- ^ a b Ebola virus disease (Report). World Health Organization. Retrieved 6 June 2019.
- ^ a b "CDC urges all US residents to avoid nonessential travel to Liberia, Guinea and Sierra Leone because of an unprecedented outbreak of Ebola". Centers for Disease Control and Prevention (CDC). 31 July 2014. Archived from the original on 9 August 2014. Retrieved 2 August 2014.
- ^ a b "2014 Ebola Outbreak in West Africa". Centers for Disease Control and Prevention (CDC). 4 August 2014. Archived from the original on 2 October 2014. Retrieved 5 August 2014.
- ^ a b "Statement on the 9th meeting of the IHR Emergency Committee regarding the Ebola outbreak in West Africa". World Health Organization (WHO). 29 March 2016. Archived from the original on 31 March 2016. Retrieved 30 March 2016.
- ^ "Statement on Ebola in the Democratic Republic of the Congo". World Health Organization (WHO). Archived from the original on 12 May 2017. Retrieved 12 May 2017.
- ^ Hodal K (12 May 2017). "Ebola outbreak declared in Democratic Republic of the Congo after three die". The Guardian. United Kingdom. ISSN 1756-3224. OCLC 60623878. Archived from the original on 12 May 2017. Retrieved 12 May 2017.
- ^ Scutti S, Goldschmidt D. "Ebola outbreak declared in Democratic Republic of Congo". CNN. Archived from the original on 8 May 2018. Retrieved 9 May 2018.
- ^ a b "Ebola outbreak in DRC ends: WHO calls for international efforts to stop other deadly outbreaks in the country". World Health Organization (WHO). Archived from the original on 25 July 2018. Retrieved 26 July 2018.
- ^ Grady D (17 July 2019). "Congo's Ebola Outbreak Is Declared a Global Health Emergency". The New York Times. ISSN 1553-8095. OCLC 1645522. Archived from the original on 17 July 2019. Retrieved 17 July 2019.
- ^ a b "Ebola Hemorrhagic Fever Signs and Symptoms". Centers for Disease Control and Prevention (CDC). 28 January 2014. Archived from the original on 1 August 2014. Retrieved 2 August 2014.
- ^ a b c d e f g h Goeijenbier M, van Kampen JJ, Reusken CB, Koopmans MP, van Gorp EC (November 2014). "Ebola virus disease: a review on epidemiology, symptoms, treatment and pathogenesis". Neth J Med. 72 (9): 442–448. PMID 25387613. Archived from the original on 29 November 2014.
- ^ Haas CN (14 October 2014). "On the Quarantine Period for Ebola Virus". PLOS Currents Outbreaks. 6. doi:10.1371/currents.outbreaks.2ab4b76ba7263ff0f084766e43abbd89. ISSN 2157-3999. PMC 4205154. PMID 25642371.
- ^ a b c Gatherer D (August 2014). "The 2014 Ebola virus disease outbreak in West Africa". J Gen Virol. 95 (Pt 8): 1619–1624. doi:10.1099/vir.0.067199-0. PMID 24795448.
- ^ a b c d e f Magill A (2013). Hunter's tropical medicine and emerging infectious diseases (9th ed.). New York: Saunders. p. 332. ISBN 978-1416043904. Archived from the original on 20 March 2016.
- ^ a b c Hoenen T, Groseth A, Falzarano D, Feldmann H (May 2006). "Ebola virus: unravelling pathogenesis to combat a deadly disease". Trends in Molecular Medicine. 12 (5): 206–215. doi:10.1016/j.molmed.2006.03.006. PMID 16616875.
- ^ Brown CS, Mepham S, Shorten RJ (June 2017). "Ebola Virus Disease: An Update on Epidemiology, Symptoms, Laboratory Findings, Diagnostic Issues, and Infection Prevention and Control Issues for Laboratory Professionals". Clinical Laboratory Medicine (Review). 37 (2): 269–284. doi:10.1016/j.cll.2017.01.003. PMID 28457350.
- ^ a b c Sharma N, Cappell MS (September 2015). "Gastrointestinal and Hepatic Manifestations of Ebola Virus Infection". Digestive Diseases and Sciences (Review). 60 (9): 2590–2603. doi:10.1007/s10620-015-3691-z. PMID 25972150. S2CID 5674317.
- ^ Simpson DI (1977). Marburg and Ebola virus infections: a guide for their diagnosis, management, and control. World Health Organization. p. 10f. hdl:10665/37138. ISBN 924170036X. WHO offset publication; no. 36.
- ^ King JW, Rafeek H (14 January 2021). Chandrasekar PH (ed.). "Ebola Virus, Clinical Presentation". Medscape. Archived from the original on 1 January 2012. Retrieved 30 July 2012.
- ^ "Appendix A: Disease-Specific Chapters – Chapter: Hemorrhagic fevers caused by: i) Ebola virus and ii) Marburg virus and iii) Other viral causes including bunyaviruses, arenaviruses, and flaviviruses" (PDF). Ministry of Health and Long-Term Care. Archived (PDF) from the original on 15 October 2014. Retrieved 9 October 2014.
- ^ a b c d e f g Feldmann H, Geisbert TW (March 2011). "Ebola haemorrhagic fever". Lancet. 377 (9768): 849–62. doi:10.1016/S0140-6736(10)60667-8. PMC 3406178. PMID 21084112.
- ^ Shantha JG, Yeh S, Nguyen QD (November 2016). "Ebola virus disease and the eye". Current Opinion in Ophthalmology (Review). 27 (6): 538–544. doi:10.1097/ICU.0000000000000313. PMID 27585217. S2CID 34367099.
- ^ West TE, von Saint André-von Arnim A (November 2014). "Clinical presentation and management of severe Ebola virus disease". Annals of the American Thoracic Society (Review). 11 (9): 1341–1350. doi:10.1513/AnnalsATS.201410-481PS. PMID 25369317.
- ^ Sharma N, Cappell MS (September 2015). "Gastrointestinal and Hepatic Manifestations of Ebola Virus Infection". Digestive Diseases and Sciences. 60 (9): 2590–2603. doi:10.1007/s10620-015-3691-z. PMID 25972150. S2CID 5674317.
- ^ "Ebola virus disease Information for Clinicians in U.S. Healthcare Settings | For Clinicians | Ebola (Ebola Virus Disease) | Ebola Hemorrhagic Fever | CDC". www.cdc.gov. 6 January 2020. Archived from the original on 1 April 2020. Retrieved 22 March 2020.
- ^ a b Tosh PK, Sampathkumar P (December 2014). "What Clinicians Should Know About the 2014 Ebola Outbreak". Mayo Clin Proc. 89 (12): 1710–17. doi:10.1016/j.mayocp.2014.10.010. PMID 25467644.
- ^ "An emergency within an emergency: caring for Ebola survivors". World Health Organization (WHO). 7 August 2015. Archived from the original on 13 August 2015. Retrieved 12 August 2015.
- ^ "Ebola Virus Disease". SRHD. Archived from the original on 15 September 2020. Retrieved 15 September 2020.
- ^ a b c d "Q&A on Transmission, Ebola". Centers for Disease Control and Prevention (CDC). September 2014. Archived from the original on 2 October 2014. Retrieved 3 October 2014.
- ^ a b c Hoenen T, Groseth A, Feldmann H (July 2012). "Current Ebola vaccines". Expert Opin Biol Ther. 12 (7): 859–872. doi:10.1517/14712598.2012.685152. PMC 3422127. PMID 22559078.
- ^ Kuhn JH, Becker S, Ebihara H, Geisbert TW, Johnson KM, Kawaoka Y, et al. (December 2010). "Proposal for a revised taxonomy of the family Filoviridae: Classification, names of taxa and viruses, and virus abbreviations". Archives of Virology. 155 (12): 2083–2103. doi:10.1007/s00705-010-0814-x. PMC 3074192. PMID 21046175.
- ^ Branswell H (27 July 2018). "New Ebola species is reported for first time in a decade". Stat. Archived from the original on 27 July 2018. Retrieved 8 July 2022.
- ^ Spickler A. "Ebolavirus and Marburgvirus Infections" (PDF). Archived (PDF) from the original on 30 April 2015.
- ^ "About Ebola Virus Disease". Centers for Disease Control and Prevention (CDC). Archived from the original on 16 October 2014. Retrieved 18 October 2014.
- ^ Pringle CR (2005). "Order Mononegavirales". In Fauquet CM, Mayo MA, Maniloff J, Desselberger U, Ball LA (eds.). Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses. San Diego: Elsevier/Academic Press. pp. 609–614. ISBN 978-0-12-370200-5.
- ^ a b Stahelin RV (June 2014). "Membrane binding and bending in Ebola VP40 assembly and egress". Front Microbiol. 5: 300. doi:10.3389/fmicb.2014.00300. PMC 4061899. PMID 24995005.
- ^ Ascenzi P, Bocedi A, Heptonstall J, Capobianchi MR, Di Caro A, Mastrangelo E, et al. (June 2008). "Ebolavirus and Marburgvirus: insight the Filoviridae family" (PDF). Mol Aspects Med. 29 (3): 151–185. doi:10.1016/j.mam.2007.09.005. hdl:2434/53604. PMID 18063023. Archived (PDF) from the original on 8 March 2021. Retrieved 20 August 2019.
- ^ a b c d Chippaux JP (October 2014). "Outbreaks of Ebola virus disease in Africa: the beginnings of a tragic saga". J Venom Anim Toxins Incl Trop Dis. 20 (1): 44. doi:10.1186/1678-9199-20-44. PMC 4197285. PMID 25320574.
- ^ a b c d Misasi J, Sullivan NJ (October 2014). "Camouflage and Misdirection: The Full-On Assault of Ebola Virus Disease". Cell. 159 (3): 477–486. doi:10.1016/j.cell.2014.10.006. PMC 4243531. PMID 25417101.
- ^ a b c d e f g h Kühl A, Pöhlmann S (September 2012). "How Ebola virus counters the interferon system". Zoonoses Public Health. 59 (Supplement 2): 116–131. doi:10.1111/j.1863-2378.2012.01454.x. PMC 7165950. PMID 22958256.
- ^ a b Olejnik J, Ryabchikova E, Corley RB, Mühlberger E (August 2011). "Intracellular events and cell fate in filovirus infection". Viruses. 3 (8): 1501–31. doi:10.3390/v3081501. PMC 3172725. PMID 21927676.
- ^ Feldmann H, Geisbert TW, Jahrling PB, Klenk H, Netesov SV, Peters CJ, Sanchez A, Swanepoel R, Volchkov VE (2005). Fauquet CM, Mayo MA, Maniloff J, Desselberger U, Ball LA (eds.). Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses. Elsevier/Academic Press. ISBN 978-0123702005.
- ^ a b c d e f g h Funk DJ, Kumar A (November 2014). "Ebola virus disease: an update for anesthesiologists and intensivists". Can J Anaesth. 62 (1): 80–91. doi:10.1007/s12630-014-0257-z. PMC 4286619. PMID 25373801.
- ^ "Ebola (Ebola Virus Disease) Transmission". Centers for Disease Control and Prevention (CDC). 5 November 2014. Archived from the original on 6 November 2014. Retrieved 7 November 2014.
- ^ Drazen JM, Kanapathipillai R, Campion EW, Rubin EJ, Hammer SM, Morrissey S, Baden LR (November 2014). "Ebola and quarantine". N Engl J Med. 371 (21): 2029–2030. doi:10.1056/NEJMe1413139. PMID 25347231.
- ^ McNeil Jr DG (3 October 2014). "Ask Well: How Does Ebola Spread? How Long Can the Virus Survive?". The New York Times. Archived from the original on 24 October 2014. Retrieved 24 October 2014.
- ^ a b "How Ebola Is Spread" (PDF). Centers for Disease Control and Prevention (CDC). 1 November 2014. Archived (PDF) from the original on 8 July 2017.
- ^ a b c d e f g "Transmission". Centers for Disease Control and Prevention (CDC). 17 October 2014. Archived from the original on 19 October 2014. Retrieved 18 October 2014.
- ^ a b c d Chowell G, Nishiura H (October 2014). "Transmission dynamics and control of Ebola virus disease (EVD): a review". BMC Med. 12 (1): 196. doi:10.1186/s12916-014-0196-0. PMC 4207625. PMID 25300956.
- ^ a b Osterholm MT, Moore KA, Kelley NS, Brosseau LM, Wong G, Murphy FA, et al. (19 February 2015). "Transmission of Ebola viruses: what we know and what we do not know". mBio. 6 (2): e00137. doi:10.1128/mBio.00137-15. PMC 4358015. PMID 25698835.
- ^ "Sexual transmission of the Ebola Virus : evidence and knowledge gaps". World Health Organization (WHO). 4 April 2015. Archived from the original on 14 April 2015. Retrieved 16 April 2015.
- ^ Wu B (2 May 2015). "Ebola Can Be Transmitted Through Sex". Science Times. Archived from the original on 2 May 2015. Retrieved 3 May 2015.
- ^ Soka MJ, Choi MJ, Baller A, White S, Rogers E, Purpura LJ, et al. (2016). "Prevention of sexual transmission of Ebola in Liberia through a national semen testing and counselling programme for survivors: an analysis of Ebola virus RNA results and behavioural data". Lancet Global Health. 4 (10): e736–e743. doi:10.1016/S2214-109X(16)30175-9. PMID 27596037.
- ^ Varkey JB, Shantha JG, Crozier I, Kraft CS, Lyon GM, Mehta AK, et al. (7 May 2015). "Persistence of Ebola Virus in Ocular Fluid during Convalescence". The New England Journal of Medicine. 372 (25): 2423–227. doi:10.1056/NEJMoa1500306. hdl:2328/35704. PMC 4547451. PMID 25950269.
- ^ a b "CDC Telebriefing on Ebola outbreak in West Africa". Centers for Disease Control and Prevention (CDC). 28 July 2014. Archived from the original on 2 August 2014. Retrieved 3 August 2014.
- ^ a b "Air travel is low-risk for Ebola transmission". World Health Organization (WHO). 14 August 2014. Archived from the original on 19 January 2015.
- ^ Chan M (September 2014). "Ebola virus disease in West Africa – no early end to the outbreak". N Engl J Med. 371 (13): 1183–1185. doi:10.1056/NEJMp1409859. PMID 25140856.
- ^ "Sierra Leone: a traditional healer and a funeral". World Health Organization (WHO). Archived from the original on 6 October 2014. Retrieved 6 October 2014.
- ^ Salaam-Blyther T (26 August 2014). "The 2014 Ebola Outbreak: International and U.S. Responses" (PDF). Archived (PDF) from the original on 3 September 2014. Retrieved 9 September 2014.
- ^ Lashley FR, Durham JD, eds. (2007). Emerging infectious diseases trends and issues (2nd ed.). New York: Springer. p. 141. ISBN 978-0826103505. Archived from the original on 9 May 2016.
- ^ Magill AJ, Strickland GT, Maguire JH, Ryan ET, Solomon T, eds. (2013). Hunter's tropical medicine and emerging infectious disease (9th ed.). London; New York: Elsevier. pp. 170–172. ISBN 978-1455740437. OCLC 822525408. Archived from the original on 20 May 2016.
- ^ "Questions and Answers on Ebola Hemorrhagic Fever". Centers for Disease Control and Prevention (CDC). 22 May 2018. Archived from the original on 28 July 2017.
- ^ a b "Ebola in Texas: Second Health Care Worker Tests Positive". NBC News. 15 October 2014. Archived from the original on 15 October 2014.
- ^ Jones RM, Brosseau LM (May 2015). "Aerosol transmission of infectious disease". Journal of Occupational and Environmental Medicine (Review). 57 (5): 501–508. doi:10.1097/JOM.0000000000000448. PMID 25816216. S2CID 11166016.
- ^ a b "Transmission of Ebola virus". virology.ws. 27 September 2014. Archived from the original on 29 January 2016. Retrieved 22 January 2016.
- ^ a b c Weingartl HM, Embury-Hyatt C, Nfon C, Leung A, Smith G, Kobinger G (2012). "Transmission of Ebola virus from pigs to non-human primates". Scientific Reports. 2: 811. Bibcode:2012NatSR...2..811W. doi:10.1038/srep00811. PMC 3498927. PMID 23155478.
- ^ "Risk of Exposure". Centers for Disease Control and Prevention (CDC). 12 October 2014. Archived from the original on 16 October 2014. Retrieved 18 October 2014.
- ^ "FAO warns of fruit bat risk in West African Ebola epidemic". fao.org. 21 July 2014. Archived from the original on 13 October 2014. Retrieved 22 October 2014.
- ^ Williams E. "African monkey meat that could be behind the next HIV". The Independent. Archived from the original on 22 June 2017.
25 people in Bakaklion, Cameroon killed due to eating of ape
- ^ a b "Ebolavirus – Pathogen Safety Data Sheets". Public Health Agency of Canada. 17 September 2001. Archived from the original on 20 August 2014. Retrieved 22 August 2014.
- ^ a b Gonzalez JP, Pourrut X, Leroy E (2007). "Ebolavirus and Other Filoviruses". Wildlife and Emerging Zoonotic Diseases: The Biology, Circumstances and Consequences of Cross-Species Transmission. Ebolavirus and other filoviruses. Vol. 315. pp. 363–387. doi:10.1007/978-3-540-70962-6_15. ISBN 978-3540709619. PMC 7121322. PMID 17848072.
{{cite book}}:|work=ignored (help) - ^ a b c d e f Weingartl HM, Nfon C, Kobinger G (May 2013). "Review of Ebola Virus Infections in Domestic Animals". Vaccines and Diagnostics for Transboundary Animal Diseases. Developments in Biologicals. Vol. 135. pp. 211–218. doi:10.1159/000178495. ISBN 978-3318023657. PMID 23689899.
{{cite book}}:|work=ignored (help) - ^ Laupland KB, Valiquette L (May 2014). "Ebola virus disease". Can J Infect Dis Med Microbiol. 25 (3): 128–129. doi:10.1155/2014/527378. PMC 4173971. PMID 25285105.
- ^ a b c Pourrut X, Kumulungui B, Wittmann T, Moussavou G, Délicat A, Yaba P, et al. (June 2005). "The natural history of Ebola virus in Africa". Microbes Infect. 7 (7–8): 1005–1014. doi:10.1016/j.micinf.2005.04.006. PMID 16002313.
- ^ Swanepoel R, Leman PA, Burt FJ, Zachariades NA, Braack LE, Ksiazek TG, et al. (October 1996). "Experimental inoculation of plants and animals with Ebola virus". Emerg. Infect. Dis. 2 (4): 321–325. doi:10.3201/eid0204.960407. ISSN 1080-6040. PMC 2639914. PMID 8969248.
- ^ Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, Yaba P, et al. (December 2005). "Fruit bats as reservoirs of Ebola virus". Nature. 438 (7068): 575–576. Bibcode:2005Natur.438..575L. doi:10.1038/438575a. PMID 16319873. S2CID 4403209.
- ^ Olival KJ, Islam A, Yu M, Anthony SJ, Epstein JH, Khan SA, et al. (February 2013). "Ebola virus antibodies in fruit bats, Bangladesh". Emerg. Infect. Dis. 19 (2): 270–273. doi:10.3201/eid1902.120524. PMC 3559038. PMID 23343532.
- ^ Morvan JM, Deubel V, Gounon P, Nakouné E, Barrière P, Murri S, et al. (December 1999). "Identification of Ebola virus sequences present as RNA or DNA in organs of terrestrial small mammals of the Central African Republic". Microbes and Infection. 1 (14): 1193–1201. doi:10.1016/S1286-4579(99)00242-7. PMID 10580275.
- ^ Groseth A, Feldmann H, Strong JE (September 2007). "The ecology of Ebola virus". Trends Microbiol. 15 (9): 408–416. doi:10.1016/j.tim.2007.08.001. PMID 17698361.
- ^ "Did deforestation cause the Ebola outbreak?". New Internationalist. 10 April 2018. Archived from the original on 26 June 2018. Retrieved 10 July 2018.
- ^ Olivero J, Fa JE, Real R, Márquez AL, Farfán MA, Vargas JM, et al. (30 October 2017). "Recent loss of closed forests is associated with Ebola virus disease outbreaks". Scientific Reports. 7 (1): 14291. Bibcode:2017NatSR...714291O. doi:10.1038/s41598-017-14727-9. ISSN 2045-2322. PMC 5662765. PMID 29085050.
- ^ a b Ansari AA (September 2014). "Clinical features and pathobiology of Ebolavirus infection". J Autoimmun. 55: 1–9. doi:10.1016/j.jaut.2014.09.001. PMID 25260583.
- ^ a b Smith T (2005). Ebola (Deadly Diseases and Epidemics). Chelsea House Publications. ISBN 978-0791085059.
- ^ Tang H, Abouleila Y, Saris A, Shimizu Y, Ottenhoff TH, Mashaghi A (May 2023). "Ebola virus-like particles reprogram cellular metabolism". Journal of Molecular Medicine. 101 (5): 557–568. doi:10.1007/s00109-023-02309-4. PMC 10036248. PMID 36959259.
- ^ a b Ramanan P, Shabman RS, Brown CS, Amarasinghe GK, Basler CF, Leung DW (September 2011). "Filoviral immune evasion mechanisms". Viruses. 3 (9): 1634–49. doi:10.3390/v3091634. PMC 3187693. PMID 21994800.
- ^ "Screening Patients | For Clinicians | Ebola Virus Disease | CDC". www.cdc.gov. 5 May 2021. Archived from the original on 20 September 2022. Retrieved 20 September 2022.
- ^ Kortepeter MG, Bausch DG, Bray M (November 2011). "Basic clinical and laboratory features of filoviral hemorrhagic fever". J Infect Dis. 204 (Supplement 3): S810–16. doi:10.1093/infdis/jir299. PMID 21987756.
- ^ Goldsmith CS, Miller SE (October 2009). "Modern uses of electron microscopy for detection of viruses". Clinical Microbiology Reviews (Review). 22 (4): 552–63. doi:10.1128/CMR.00027-09. PMC 2772359. PMID 19822888.
- ^ a b c "Ebola Hemorrhagic Fever Diagnosis". Centers for Disease Control and Prevention (CDC). 28 January 2014. Archived from the original on 24 September 2014. Retrieved 3 August 2014.
- ^ a b Grolla A, Lucht A, Dick D, Strong JE, Feldmann H (September 2005). "Laboratory diagnosis of Ebola and Marburg hemorrhagic fever". Bull Soc Pathol Exot. 98 (3): 205–09. PMID 16267962.
- ^ "Liberia: New Ebola mobile lab speeds up diagnosis and improves care". World Health Organization (WHO). October 2014. Archived from the original on 24 October 2014. Retrieved 26 October 2014.
- ^ a b "First Antigen Rapid Test for Ebola through Emergency Assessment and Eligible for Procurement". World Health Organization (WHO). Archived from the original on 20 February 2015. Retrieved 20 February 2015.
- ^ Longo DL, Kasper DL, Jameson JL, Fauci AS, Hauser SL, Loscalzo J, eds. (2011). "Chapter 197". Harrison's Principles of Internal Medicine (18th ed.). McGraw-Hill. ISBN 978-0071748896.
- ^ Beeching NJ, Fenech M, Houlihan CF (December 2014). "Ebola Virus Disease". BMJ (Review). 10 (349): g7438. doi:10.1136/bmj.g7348. PMC 4707720. PMID 25497512.
- ^ "Viral Hemorrhagic Fever". S.F. Dept Public Health – Infectious Disease Emergencies. July 2008. Archived from the original (PDF) on 20 April 2013. Retrieved 17 August 2014.
- ^ Gear JH (May–June 1989). "Clinical aspects of African viral hemorrhagic fevers". Rev Infect Dis. 11 (Supplement 4): S777–82. doi:10.1093/clinids/11.supplement_4.s777. PMID 2665013.
- ^ Gear JH, Ryan J, Rossouw E (February 1978). "A consideration of the diagnosis of dangerous infectious fevers in South Africa". South African Medical Journal. 53 (7): 235–37. PMID 565951.
- ^ Bogomolov BP (1998). "Differential diagnosis of infectious diseases with hemorrhagic syndrome". Terapevticheskii Arkhiv. 70 (4): 63–68. PMID 9612907.
- ^ "Congo Ebola deaths surpass 1,000 as attacks on treatment centers go on". Reuters. 3 May 2019. Archived from the original on 8 May 2019. Retrieved 8 May 2019.
- ^ "Ebola virus disease: Vaccines". www.who.int. Archived from the original on 29 March 2023. Retrieved 29 March 2023.
- ^ a b c "Ebola Hemorrhagic Fever Prevention". Centers for Disease Control and Prevention (CDC). 31 July 2014. Archived from the original on 4 September 2014. Retrieved 2 August 2014.
- ^ a b "Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus Disease in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing)". Centers for Disease Control and Prevention (CDC). 20 October 2014. Archived from the original on 22 October 2014. Retrieved 22 October 2014.
- ^ a b Peters CJ (December 1998). Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting (PDF). Centers for Disease Control and Prevention (CDC). Archived (PDF) from the original on 8 July 2017.
- ^ Govan F (11 October 2014). "Ebola medics 'better trained in Sierra Leone than Spain'". The Telegraph. Archived from the original on 28 June 2020.
- ^ Sifferlin A (9 October 2014). "This Is How Ebola Patients Are Equipping Their Homes". Time Magazine. Archived from the original on 5 March 2015.
- ^ Sheri F, Nossiter A, Kanter J (10 October 2014). "Doctors Without Borders Evolves as It Forms the Vanguard in Ebola Fight". The New York Times. Archived from the original on 14 October 2014. Retrieved 12 October 2014.
- ^ Organization, World Health (August 2014). "Interim infection prevention and control guidance for care of patients with suspected or confirmed filovirus haemorrhagic fever in health-care settings, with focus on Ebola". WHO Technical Documents. World Health Organization (WHO). hdl:10665/130596. WHO/HIS/SDS/2014.4 Rev. 1.
- ^ "Ebola – 5 tips to avoid the deadly disease". Plan International. 6 September 2014. Archived from the original on 24 March 2015.
- ^ Rouquet P, Froment JM, Bermejo M, Kilbourn A, Karesh W, Reed P, et al. (February 2005). "Wild animal mortality monitoring and human Ebola outbreaks, Gabon and Republic of Congo, 2001–2003". Emerg. Infect. Dis. 11 (2): 283–90. doi:10.3201/eid1102.040533. ISSN 1080-6040. PMC 3320460. PMID 15752448.
- ^ Centers for Disease Control and Prevention and World Health Organization (1998). Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting (PDF). Centers for Disease Control and Prevention (CDC). Archived (PDF) from the original on 11 April 2014. Retrieved 8 February 2013.
- ^ "Section 7: Use Safe Burial Practices" (PDF). Information resources on Ebola virus disease. World Health Organization (WHO). 1 June 2014. Archived (PDF) from the original on 26 February 2015.
- ^ Harden B (24 December 2000). "Ebola's Shadow". The New York Times. Archived from the original on 20 October 2014. Retrieved 12 October 2014.
- ^ Fassassi A (September 2014). "How anthropologists help medics fight Ebola in Guinea". SciDev.Net. Archived from the original on 6 October 2014. Retrieved 3 October 2014.
- ^ "West Africa – Ebola virus disease Update: Travel and transport". International travel and health. World Health Organization (WHO). Archived from the original on 29 July 2014.
- ^ a b c "Monitoring Symptoms and Controlling Movement to Stop Spread of Ebola". Centers for Disease Control and Prevention (CDC). 27 October 2014. Archived from the original on 8 July 2017.
- ^ a b "Ebola: Control and Prevention". Occupational Safety and Health Administration (OSHA). Archived from the original on 9 November 2014. Retrieved 9 November 2014.
- ^ "About Quarantine and Isolation". Centers for Disease Control and Prevention (CDC). 28 August 2014. Archived from the original on 20 October 2014. Retrieved 26 October 2014.
- ^ Sompayrac L (2002). How pathogenic viruses work (3rd ed.). Boston: Jones and Bartlett Publishers. p. 87. ISBN 978-0763720827.
- ^ Alazard-Dany N, Ottmann Terrangle M, Volchkov V (April 2006). "[Ebola and Marburg viruses: the humans strike back]" (PDF). Med Sci (Paris) (in French). 22 (4): 405–10. doi:10.1051/medsci/2006224405. PMID 16597410. Archived (PDF) from the original on 22 February 2020. Retrieved 20 August 2019.
- ^ "Ebola virus disease update – west Africa". World Health Organization (WHO). 19 August 2014. Archived from the original on 22 October 2014. Retrieved 26 October 2014.
- ^ Koenig K, Schultz C, eds. (2009). Koenig and Schultz's disaster medicine : comprehensive principles and practices. Cambridge: Cambridge University Press. p. 209. ISBN 978-0521873673. Archived from the original on 15 May 2016.
- ^ "Control of Communicable Diseases". Federal Register. 19 January 2017. Archived from the original on 6 August 2019. Retrieved 13 August 2019.
- ^ Frieden TR, Damon I, Bell BP, Kenyon T, Nichol S (25 September 2014). "Ebola 2014 – New Challenges, New Global Response and Responsibility". New England Journal of Medicine. 371 (13): 1177–1180. doi:10.1056/NEJMp1409903. PMID 25140858.
- ^ "What is Contact Tracing?" (PDF). Centers for Disease Control and Prevention (CDC). Archived (PDF) from the original on 12 September 2014. Retrieved 15 September 2014.
- ^ "FDA warns consumers about fraudulent Ebola treatment products" (Press release). Archived from the original on 11 January 2017. Retrieved 20 August 2014.
- ^ "Natural Solutions Foundation Warning Letter". U.S. Food and Drug Administration (FDA). 22 September 2014. Archived from the original on 8 October 2014. Retrieved 9 October 2014.
- ^ a b c d e f Clark DV, Jahrling PB, Lawler JV (September 2012). "Clinical management of filovirus-infected patients". Viruses. 4 (9): 1668–86. doi:10.3390/v4091668. PMC 3499825. PMID 23170178.
- ^ "Ebola messages for the general public". World Health Organization (WHO). Archived from the original on 25 October 2014. Retrieved 26 October 2014.
- ^ a b "Ebola virus disease". www.who.int. Archived from the original on 16 February 2021. Retrieved 28 May 2020.
- ^ "Annex 18. Transmission risk reduction of filoviruses in home-care settings" (PDF). World Health Organization (WHO). Archived (PDF) from the original on 26 October 2014. Retrieved 26 October 2014.
- ^ Fauquet CM (2005). Virus taxonomy classification and nomenclature of viruses; 8th report of the International Committee on Taxonomy of Viruses. Oxford: Elsevier/Academic Press. p. 648. ISBN 978-0080575483. Archived from the original on 4 June 2016.
- ^ "More or Less behind the stats Ebola". BBC World Service. Archived from the original on 3 September 2014. Retrieved 8 October 2014.
- ^ a b c Shantha JG, Crozier I, Yeh S (November 2017). "An update on ocular complications of Ebola virus disease". Current Opinion in Ophthalmology. 28 (6): 600–606. doi:10.1097/ICU.0000000000000426. PMC 5988239. PMID 28872492.
- ^ Rojas M, Monsalve DM, Pacheco Y, Acosta-Ampudia Y, Ramírez-Santana C, Ansari AA, Gershwin ME, Anaya JM (January 2020). "Ebola virus disease: An emerging and re-emerging viral threat". Journal of Autoimmunity. 106: 102375. doi:10.1016/j.jaut.2019.102375. PMID 31806422.
- ^ Wiwanitkit S, Wiwanitkit V (2015). "Ocular problem in Ebola virus infection: A short review". Saudi Journal of Ophthalmology. 29 (3): 225–226. doi:10.1016/j.sjopt.2015.02.006. PMC 4487942. PMID 26155084.
- ^ Varkey JB, Shantha JG, Crozier I, Kraft CS, Lyon GM, Mehta AK, et al. (2015). "Persistence of Ebola Virus in Ocular Fluid during Convalescence". New England Journal of Medicine. 372 (25): 2423–2427. doi:10.1056/NEJMoa1500306. hdl:2328/35704. ISSN 0028-4793. PMC 4547451. PMID 25950269.
- ^ Mackay IM, Arden KE (2015). "Ebola virus in the semen of convalescent men". The Lancet Infectious Diseases. 15 (2): 149–150. doi:10.1016/S1473-3099(14)71033-3. ISSN 1473-3099. PMID 25467652.
- ^ Rogstad KE, Tunbridge A (February 2015). "Ebola virus as a sexually transmitted infection". Current Opinion in Infectious Diseases. 28 (1): 83–85. doi:10.1097/qco.0000000000000135. PMID 25501666. S2CID 7538665.
- ^ Christie A, Davies-Wayne GJ, Cordier-Lassalle T, Blackley DJ, Laney AS, Williams DE, et al. (8 May 2015). "Possible sexual transmission of Ebola virus – Liberia, 2015". MMWR. Morbidity and Mortality Weekly Report. 64 (17): 479–481. PMC 4584553. PMID 25950255.
- ^ Sprecher, A (14 October 2015). "Handle Survivors with Care". The New England Journal of Medicine. 377 (15): 1480–1482. doi:10.1056/NEJMe1512928. PMID 26465064.
- ^ "Neuro complications cited in UK nurse's Ebola case". 15 October 2015. Archived from the original on 17 October 2015. Retrieved 19 October 2015.
- ^ Peterson AT, Bauer JT, Mills JN (2004). "Ecologic and Geographic Distribution of Filovirus Disease". Emerg. Infect. Dis. 10 (1): 40–47. doi:10.3201/eid1001.030125. PMC 3322747. PMID 15078595.
- ^ a b "Ebola haemorrhagic fever in Sudan, 1976" (PDF). Archived from the original (PDF) on 13 October 2014. Retrieved 8 October 2014.
- ^ Hewlett B, Hewlett B (2007). Ebola, Culture and Politics: The Anthropology of an Emerging Disease. Cengage Learning. p. 103. ISBN 978-1111797317. Archived from the original on 21 May 2024. Retrieved 31 July 2014.
- ^ a b Feldmann H, Jones S, Klenk HD, Schnittler HJ (August 2003). "Ebola virus: from discovery to vaccine". Nature Reviews Immunology. 3 (8): 677–685. doi:10.1038/nri1154. PMID 12974482. S2CID 27486878.
- ^ a b Report of an International Commission (1978). "Ebola haemorrhagic fever in Zaire, 1976" (PDF). Bull. World Health Organ. 56 (2): 271–293. PMC 2395567. PMID 307456. Archived from the original (PDF) on 8 August 2014. Retrieved 14 August 2014.
- ^ Centers for Disease Control Prevention (CDC) (1995). "Outbreak of Ebola Viral Hemorrhagic Fever – Zaire, 1995". Morbidity and Mortality Weekly Report. 44 (19): 381–382. PMID 7739512. Archived from the original on 25 June 2017.
- ^ Elezra M. "Ebola: The Truth Behind The Outbreak (Video) l". Mabalo Lokela Archives – Political Mol. Archived from the original on 12 July 2015. Retrieved 18 October 2014.
- ^ a b Stimola A (2011). Ebola (1st ed.). New York: Rosen Pub. pp. 31, 52. ISBN 978-1435894334.
- ^ "This Congolese Doctor Discovered Ebola But Never Got Credit For It – Until Now". NPR.org. Archived from the original on 5 November 2019. Retrieved 5 November 2019.
- ^ McNeish H (24 March 2017). "He Treated The Very First Ebola Cases 40 Years Ago. Then He Watched The World Forget". HuffPost. Archived from the original on 25 July 2019. Retrieved 5 November 2019.
- ^ Piot P, Marshall R (2012). No time to lose: a life in pursuit of deadly viruses (1st ed.). New York: W.W. Norton & Co. pp. 30, 90. ISBN 978-0393063165.
- ^ Piot P (11 August 2014). "Part one: A virologist's tale of Africa's first encounter with Ebola". ScienceInsider. Archived from the original on 9 October 2014.
- ^ Piot P (13 August 2014). "Part two: A virologist's tale of Africa's first encounter with Ebola". ScienceInsider. Archived from the original on 16 November 2014.
- ^ Bardi JS. "Death Called a River". The Scripps Research Institute. Archived from the original on 2 August 2014. Retrieved 9 October 2014.
- ^ Preston R (20 July 1995). The Hot Zone. Anchor Books (Random House). p. 117.
Karl Johnson named it Ebola
- ^ von Bredow R, Hackenbroch V (4 October 2014). "In 1976 I Discovered Ebola – Now I Fear an Unimaginable Tragedy". The Guardian. Archived from the original on 3 January 2017.
- ^ King JW (2 April 2008). "Ebola Virus". eMedicine. WebMD. Archived from the original on 28 September 2008. Retrieved 6 October 2008.
- ^ Formenty P, Libama F, Epelboin A, Allarangar Y, Leroy E, Moudzeo H, et al. (2003). "[Outbreak of Ebola hemorrhagic fever in the Republic of the Congo, 2003: a new strategy?]". Med Trop (Mars) (in French). 63 (3): 291–295. PMID 14579469.
- ^ Miller J (25 May 2004). "Russian Scientist Dies in Ebola Accident at Former Weapons Lab". The New York Times. Archived from the original on 17 October 2014. Retrieved 12 October 2014.
- ^ "Ebola outbreak in Congo". CBC News. 12 September 2007. Archived from the original on 19 November 2014.
- ^ a b "Mystery DR Congo fever kills 100". BBC News Online. 31 August 2007. Archived from the original on 11 November 2007.
- ^ "Ebola Outbreak Confirmed in Congo". NewScientist.com. 11 September 2007. Archived from the original on 18 June 2015.
- ^ "Uganda: Deadly Ebola Outbreak Confirmed – UN". UN News Service. 30 November 2007. Archived from the original on 3 March 2008. Retrieved 25 February 2008.
- ^ "DRC Confirms Ebola Outbreak". Voanews.com. 21 August 2012. Archived from the original on 15 September 2012. Retrieved 15 April 2013.
- ^ "WHO – Ebola outbreak in Democratic Republic of Congo". World Health Organization (WHO). 17 August 2012. Archived from the original on 27 October 2013. Retrieved 15 April 2013.
- ^ "WHO – Ebola outbreak in Democratic Republic of Congo – update". World Health Organization (WHO). 21 August 2012. Archived from the original on 16 December 2012. Retrieved 15 April 2013.
- ^ Castillo M (2012). "Ebola virus claims 31 lives in Democratic Republic of the Congo". CBS News. United States. Archived from the original on 14 September 2012. Retrieved 14 September 2012.
- ^ "Virological Analysis: no link between Ebola outbreaks in west Africa and Democratic Republic of Congo". World Health Organization (WHO). 2 September 2014. Archived from the original on 21 November 2014.
- ^ "Congo declares its Ebola outbreak over". Reuters. 15 November 2014. Archived from the original on 29 November 2014. Retrieved 15 November 2014.
- ^ "Democratic Republic of the Congo: The country that knows how to beat Ebola". World Health Organization (WHO). December 2014. Archived from the original on 26 February 2015. Retrieved 26 February 2015.
- ^ a b "Guidelines for Evaluation of US Patients Suspected of Having Ebola Virus Disease". Centers for Disease Control and Prevention (CDC). 1 August 2014. Archived from the original on 8 August 2014. Retrieved 5 August 2014.
- ^ Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba N, et al. (October 2014). "Emergence of Zaire Ebola Virus Disease in Guinea" (PDF). New England Journal of Medicine. 371 (15): 1418–1425. doi:10.1056/NEJMoa1404505. PMID 24738640. S2CID 34198809. Archived from the original (PDF) on 21 February 2019.
- ^ "The first cases of this Ebola outbreak traced by WHO" (png). World Health Organization (WHO). 2014. Archived from the original on 6 October 2014.
- ^ "WHO raises global alarm over Ebola outbreak". CBS News. Archived from the original on 8 August 2014. Retrieved 2 August 2014.
- ^ Fulton D (18 August 2014). "In Liberia's Ebola-Stricken Villages, Residents Face 'Stark' Choices". Common Dreams. Archived from the original on 20 August 2014. Retrieved 20 August 2014.
- ^ "Experimental therapies: growing interest in the use of whole blood or plasma from recovered Ebola patients (convalescent therapies)" (Press release). World Health Organization (WHO). 26 September 2014. Archived from the original on 28 September 2014. Retrieved 28 September 2014.
- ^ WHO Ebola Response Team (23 September 2014). "Ebola virus disease in West Africa – the first 9 months of the epidemic and forward projections". The New England Journal of Medicine. 371 (16): 1481–1495. doi:10.1056/NEJMoa1411100. PMC 4235004. PMID 25244186.
... we estimate that the case fatality rate is 70.8% (95% confidence interval [CI], 69 to 73) among persons with known clinical outcome of infection.
- ^ Ebola response roadmap situation report (PDF) (Report). WHO. 31 December 2014. Archived from the original (PDF) on 31 December 2014. Retrieved 1 January 2015.
The reported case fatality rate in the three intense-transmission countries among all cases for whom a definitive outcome is known is 71%.
- ^ a b "Case Fatality Rate for ebolavirus". University of Edinburgh. 2015. Archived from the original on 29 August 2014. Retrieved 28 January 2015.
- ^ Wappes J. "US health worker monitored as DRC Ebola nears 600 cases". CIDRAP. Retrieved 23 January 2019.
- ^ "2014 Ebola Outbreak in West Africa – Case Counts". Centers for Disease Control and Prevention (CDC). 2014. Archived from the original on 6 August 2017.
- ^ "Ebola Response Roadmap Situation Report" (PDF). World Health Organization (WHO). 1 October 2014. Archived (PDF) from the original on 2 October 2014.
- ^ "Unprecedented number of medical staff infected with Ebola". World Health Organization (WHO). 25 August 2014. Archived from the original on 28 August 2014. Retrieved 29 August 2014.
- ^ "Ebola response roadmap – Situation report" (PDF). World Health Organization (WHO). 10 December 2014. Archived (PDF) from the original on 10 December 2014. Retrieved 11 December 2014.
- ^ "Ebola Situation Report". World Health Organization (WHO). 28 January 2015. Archived from the original on 3 February 2015. Retrieved 5 February 2015.
- ^ "Ebola Situation Report" (PDF). World Health Organization (WHO). 8 April 2015. Archived (PDF) from the original on 14 April 2015. Retrieved 14 April 2015.
- ^ "Ebola gone from Guinea". CBC News. Thomson Reuters. 29 December 2015. Archived from the original on 30 December 2015. Retrieved 30 December 2015.
- ^ "UN declares end to Ebola virus transmission in Guinea; first time all three host countries free" (Press release). United Nations. Archived from the original on 1 January 2016. Retrieved 30 December 2015.
- ^ "New Ebola case in Sierra Leone. WHO continues to stress risk of more flare-ups". World Health Organization (WHO). 15 January 2016. Archived from the original on 27 January 2016. Retrieved 25 January 2016.
- ^ Botelho G, Wilson J (8 October 2014). "Thomas Eric Duncan: First Ebola death in U.S." CNN. Archived from the original on 29 May 2016. Retrieved 8 August 2017.
- ^ "Second US Ebola diagnosis 'deeply concerning', admits CDC chief". MSN. Archived from the original on 14 October 2014. Retrieved 20 February 2020.archive-url= October 2013
- ^ "Ebola crisis: Tests show Spanish nurse Teresa Romero no longer has the virus". ABC News. 20 October 2014. Archived from the original on 29 October 2014.
- ^ Fernandez M (12 October 2014). "Texas Health Worker Tests Positive for Ebola". The New York Times. Archived from the original on 12 October 2014. Retrieved 12 October 2014.
- ^ "Ebola in Texas: Second Health Care Worker Tests Positive". Archived from the original on 15 October 2014.
- ^ a b "Cases of Ebola Diagnosed in the United States". 22 May 2018. Archived from the original on 26 February 2017.
- ^ Sanchez R, Prokupecz S (23 October 2014). "N.Y. doctor positive for Ebola had no symptoms until Thursday, officials say". CNN. Archived from the original on 24 October 2014. Retrieved 23 October 2014.
- ^ Sun LH, Achenbach J (24 December 2014). "CDC reports potential Ebola exposure in Atlanta lab". The Washington Post. Archived from the original on 25 December 2014. Retrieved 25 December 2014.
- ^ "Ebola case confirmed in Glasgow hospital". BBC News Online. 29 December 2014. Archived from the original on 29 December 2014.
- ^ "Ebola nurse Pauline Cafferkey transferred to London unit". BBC News Online. 30 December 2014. Archived from the original on 30 December 2014.
- ^ "Ebola Epidemiology". www.ebolavirusnet.com. Archived from the original on 31 May 2020. Retrieved 26 May 2020.
- ^ a b "WHO says 19 dead, 39 infected so far in Congo Ebola outbreak". MSN. Archived from the original on 15 May 2018. Retrieved 14 May 2018.
- ^ "WHO planning for 'worst case scenario' over DRC Ebola outbreak". Al Jazeera. Archived from the original on 13 May 2018. Retrieved 14 May 2018.
- ^ "19 dead in latest Congo Ebola outbreak: WHO". Reuters. Archived from the original on 15 May 2018. Retrieved 14 May 2018.
- ^ "Update 1 – WHO gets approval to use Ebola vaccine in Democratic…". Reuters. 14 May 2018. Archived from the original on 5 August 2018. Retrieved 5 August 2018.
- ^ "WHO Director General visits Ebola-affected areas in DR Congo". World Health Organization (WHO). Archived from the original on 10 September 2020. Retrieved 14 May 2018.
- ^ Yong E (21 May 2018). "Most Maps of the New Ebola Outbreak Are Wrong: Villages, and sometimes whole regions of the Congo, are misplaced – but the ministry of health and a team of cartographers are racing to get better data". The Atlantic. Archived from the original on 30 July 2020. Retrieved 26 May 2018.
- ^ Beaubien J (2 August 2018). "Ebola In A Conflict Zone". NPR. National Public Radio (NPR). Archived from the original on 5 August 2018. Retrieved 5 August 2018.
- ^ Specia M (2 August 2018). "The Latest Ebola Outbreak Is Centered in a War Zone". The New York Times. Archived from the original on 4 August 2018. Retrieved 5 August 2018.
- ^ "DRC: Ebola Outbreak Worst in Country's History, Kills Almost 200". Democracy Now. 13 November 2018. Archived from the original on 13 November 2018. Retrieved 14 November 2018.
- ^ "Ebola outbreak in eastern Democratic Republic of Congo tops 1,000 cases" (Press release). Centers for Disease Control and Prevention (CDC). 29 March 2019. Archived from the original on 15 June 2019. Retrieved 12 May 2019.
- ^ "Ebola virus disease – Democratic Republic of the Congo". World Health Organization (WHO). Archived from the original on 5 May 2019. Retrieved 12 May 2019.
- ^ "Ebola virus disease – Democratic Republic of the Congo – Disease outbreak news: Update 6 June 2019". World Health Organization (WHO). 6 June 2019. Archived from the original on 7 June 2019. Retrieved 7 June 2019.
- ^ "Ebola outbreak: Grandmother dies in Uganda". BBC News Online. 13 June 2019. Archived from the original on 14 June 2019. Retrieved 15 June 2019.
- ^ Larson K (15 July 2019). "Congo tracing contacts of first Ebola case in eastern city". AP News. Archived from the original on 16 July 2019. Retrieved 17 July 2019.
- ^ Cheng M, Keaten J (17 July 2019). "Ebola outbreak in Congo declared a global health emergency". AP News. Archived from the original on 17 July 2019. Retrieved 17 July 2019.
- ^ "Half of Ebola cases in DR Congo 'unidentified'". BBC News Online. 2 August 2019. Archived from the original on 3 August 2019. Retrieved 3 August 2019.
- ^ "DR Congo's deadliest Ebola outbreak declared over". BBC News. 25 June 2020. Archived from the original on 31 December 2020. Retrieved 25 June 2020.
- ^ "Ebola virus disease case in Equateur Province, DRC is a new spillover". Virological.org. 5 June 2020. Archived from the original on 8 June 2020. Retrieved 8 June 2020.
- ^ "17 infected, 11 dead in new Ebola outbreak in DR Congo". www.aljazeera.com. Archived from the original on 15 June 2020. Retrieved 15 June 2020.
- ^ "Democratic Republic of the Congo declares the end to its 11th Ebola outbreak". www.cnn.com. 19 November 2020. Archived from the original on 19 November 2020. Retrieved 19 November 2020.
- ^ "New Ebola case detected in eastern DRC". www.aljazeera.com. Archived from the original on 16 February 2021. Retrieved 17 February 2021.
- ^ "Outbreak of Ebola virus disease in North Kivu – Democratic Republic of the Congo – 2021". European Centre for Disease Prevention and Control. 15 February 2021. Archived from the original on 17 February 2021. Retrieved 17 February 2021.
- ^ "DRC confirms two Ebola deaths in resurgence of outbreak". www.aljazeera.com. Archived from the original on 17 February 2021. Retrieved 17 February 2021.
- ^ "DRC confirms third Ebola case in North Kivu province". www.aljazeera.com. Archived from the original on 17 February 2021. Retrieved 17 February 2021.
- ^ a b c d "Communicable Disease Threats Report" (PDF). European Centre for Disease Prevention and Control. 7 May 2021. Archived (PDF) from the original on 7 May 2021. Retrieved 10 May 2021.
- ^ "Latest deadly Ebola virus outbreak in DR Congo declared over". UN News. 3 May 2021. Archived from the original on 10 May 2021. Retrieved 10 May 2021.
- ^ "Guinea records first Ebola deaths since 2016". BBC News. 14 February 2021. Archived from the original on 14 February 2021. Retrieved 14 February 2021.
- ^ "Guinea declares Ebola epidemic after three deaths". www.aljazeera.com. Archived from the original on 14 February 2021. Retrieved 15 February 2021.
- ^ Kupferschmidt, K (March 2021). "Ebola virus may lurk in survivors for many years". Science. 371 (6535): 1188. Bibcode:2021Sci...371.1188K. doi:10.1126/science.371.6535.1188. ISSN 0036-8075. PMID 33737465. S2CID 232303082.
- ^ Keita AK, Düx A, Diallo H, Calvignac-Spencer S, Sow MS, Keita MB, et al. (12 March 2021). "Resurgence of Ebola virus in Guinea after 5 years calls for careful attention to survivors without creating further stigmatization". virological.org. Archived from the original on 25 March 2021. Retrieved 23 March 2021.
- ^ @WHOAFRO (19 June 2021). "The #Ebola outbreak in #Guinea was declared over today! Here is a look back at the hard work of communities, health workers, partners & Guinea's health authorities to bring this outbreak to an end while also fighting #COVID19" (Tweet) – via Twitter.
- ^ "Cote d'Ivoire declares first Ebola outbreak in more than 25 years". afro.who.int. 14 August 2021. Archived from the original on 15 August 2021. Retrieved 15 August 2021.
- ^ "New test finds no evidence of Ebola virus in Cote d'Ivoire case". WHO | Regional Office for Africa. Archived from the original on 3 October 2021. Retrieved 3 October 2021.
- ^ "New case of Ebola hemorrhagic fever found in DR Congo". Al Jazeera. 23 April 2022. Archived from the original on 24 April 2022. Retrieved 24 April 2022.
- ^ "All reported DR Congo Ebola patients dead: WHO". Peoples Gazette. 24 May 2022. Archived from the original on 25 May 2022. Retrieved 25 May 2022.
- ^ "Ebola virus disease – Democratic Republic of the Congo", World Health Organization, 4 July 2022, archived from the original on 22 September 2022, retrieved 15 September 2022
- ^ Biryabarema E (22 September 2022). "Uganda has confirmed seven Ebola cases so far, one death". Reuters. Archived from the original on 27 September 2022. Retrieved 23 September 2022.
- ^ "Uganda is battling Ebola again – and the world doesn't have a vaccine | Devi Sridhar". the Guardian. 10 October 2022. Archived from the original on 10 October 2022. Retrieved 12 October 2022.
- ^ "Ebola outbreak in Uganda declared over". BNO News. 10 January 2023. Archived from the original on 26 March 2023. Retrieved 12 January 2023.
- ^ MacNeil A, Rollin PE (June 2012). "Ebola and Marburg hemorrhagic fevers: neglected tropical diseases?". PLOS Negl Trop Dis. 6 (6): e1546. doi:10.1371/journal.pntd.0001546. PMC 3385614. PMID 22761967.
- ^ Borio L, Inglesby T, Peters CJ, Schmaljohn AL, Hughes JM, Jahrling PB, et al. (May 2002). "Hemorrhagic fever viruses as biological weapons: medical and public health management". Journal of the American Medical Association. 287 (18): 2391–405. doi:10.1001/jama.287.18.2391. PMID 11988060.
- ^ Salvaggio MR, Baddley JW (July 2004). "Other viral bioweapons: Ebola and Marburg hemorrhagic fever". Dermatologic Clinics. 22 (3): 291–302, vi. doi:10.1016/j.det.2004.03.003. PMID 15207310.
- ^ Zubray G (2013). Agents of Bioterrorism: Pathogens and Their Weaponization. New York: Columbia University Press. pp. 73–74. ISBN 978-0231518130. Archived from the original on 4 May 2016.
- ^ "Malicious Ebola-Themed Emails Are on the Rise". The New York Times. 24 October 2014. Archived from the original on 7 July 2017. Retrieved 26 October 2014.
- ^ "North Korea bans foreigners from Pyongyang marathon over Ebola". BBC News Online. 23 February 2015. Archived from the original on 24 February 2015. Retrieved 23 February 2015.
- ^ Preston R (1995). The Hot Zone, A Terrifying True Story. Anchor Books. ISBN 978-0385479561. OCLC 32052009. Archived from the original on 13 May 2016.
- ^ "Best Sellers: 4 June 1995". The New York Times Book Review. 4 June 1995. Archived from the original on 8 October 2014. Retrieved 10 September 2014.
- ^ "About The Hot Zone". Random House. Archived from the original on 7 October 2014. Retrieved 10 September 2014.
- ^ Close WT (1995). Ebola: A Documentary Novel of Its First Explosion. New York: Ivy Books. ISBN 978-0804114325. OCLC 32753758.
- ^ Grove R (2 June 2006). "More about the people than the virus". Review of Close, William T., Ebola: A Documentary Novel of Its First Explosion. Archived from the original on 21 October 2014. Retrieved 17 September 2014.
- ^ Close WT (2002). Ebola: Through the Eyes of the People. Marbleton, Wyoming: Meadowlark Springs Productions. ISBN 978-0970337115. OCLC 49193962. Archived from the original on 17 June 2016.
- ^ Pink B (24 June 2008). "A fascinating perspective". Review of Close, William T., Ebola: Through the Eyes of the People. Archived from the original on 21 October 2014. Retrieved 17 September 2014.
- ^ Clancy T (1996). Executive Orders. New York: Putnam. ISBN 978-0399142185. OCLC 34878804.
- ^ Stone O (2 September 1996). "Who's That in the Oval Office?". The New York Times. Archived from the original on 10 April 2009. Retrieved 10 September 2014.
- ^ Dewey C (2 October 2014). "Popular on Amazon: Wildly misleading self-published books about Ebola, by random people without medical degrees". The Washington Post. Archived from the original on 22 October 2014. Retrieved 27 October 2014.
- ^ Choi JH, Croyle MA (December 2013). "Emerging targets and novel approaches to Ebola virus prophylaxis and treatment". BioDrugs. 27 (6): 565–583. doi:10.1007/s40259-013-0046-1. PMC 3833964. PMID 23813435.
- ^ "Ebola 'kills over 5,000 gorillas'". BBC News Online. 8 December 2006. Archived from the original on 29 March 2009. Retrieved 31 May 2009.
- ^ a b Leroy EM, Rouquet P, Formenty P, Souquière S, Kilbourne A, Froment JM, et al. (January 2004). "Multiple Ebola virus transmission events and rapid decline of central African wildlife". Science. 303 (5656): 387–390. Bibcode:2004Sci...303..387L. doi:10.1126/science.1092528. PMID 14726594. S2CID 43305484.
- ^ Formenty P, Boesch C, Wyers M, Steiner C, Donati F, Dind F, et al. (February 1999). "Ebola virus outbreak among wild chimpanzees living in a rain forest of Côte d'Ivoire". The Journal of Infectious Diseases. 179 (Suppl 1): S120–S126. CiteSeerX 10.1.1.484.5782. doi:10.1086/514296. PMID 9988175. S2CID 18658117.
- ^ Weingartl HM, Embury-Hyatt C, Nfon C, Leung A, Smith G, Kobinger G (November 2012). "Transmission of Ebola virus from pigs to non-human primates". Sci Rep. 2: 811. Bibcode:2012NatSR...2..811W. doi:10.1038/srep00811. PMC 3498927. PMID 23155478.
- ^ Allela L, Boury O, Pouillot R, Délicat A, Yaba P, Kumulungui B, et al. (March 2005). "Ebola virus antibody prevalence in dogs and human risk". Emerg. Infect. Dis. 11 (3): 385–390. doi:10.3201/eid1103.040981. PMC 3298261. PMID 15757552.
- ^ a b c Preston R (1994). The Hot Zone. New York: Random House. p. 300. ISBN 978-0679437840.
- ^ McCormick, Fisher-Hoch & Horvitz 1999, pp. 277–279
- ^ Waterman T (1999). Ebola Reston Outbreaks. Stanford University. Archived from the original on 16 June 2008. Retrieved 2 August 2008.
- ^ a b McCormick, Fisher-Hoch & Horvitz 1999, pp. 298–299
- ^ McCormick, Fisher-Hoch & Horvitz 1999, p. 300
- ^ "Outbreaks Chronology: Ebola Virus Disease". Centers for Disease Control and Prevention (CDC).gov. Archived from the original on 26 October 2014. Retrieved 26 October 2014.
- ^ McNeil Jr DG (24 January 2009). "Pig-to-Human Ebola Case Suspected in Philippines". The New York Times. Archived from the original on 10 March 2009. Retrieved 26 January 2009.
- ^ Lee J (2009). "Ebola-Reston virus in pigs". Microbiology Australia. 30 (4): 140. doi:10.1071/ma09140. ISSN 1324-4272.
- ^ "Final trial results confirm Ebola vaccine provides high protection against disease". World Health Organization (WHO). Archived from the original on 1 April 2017. Retrieved 29 March 2017.
- ^ Maxmen A (12 August 2019). "Two Ebola drugs show promise amid ongoing outbreak". Nature. doi:10.1038/d41586-019-02442-6. ISSN 0028-0836. PMID 32778704. S2CID 201975390.
- ^ Hoenen T, Groseth A, Feldmann H (24 July 2019). "Therapeutic strategies to target the Ebola virus life cycle". Nature Reviews. Microbiology. 17 (10): 593–606. doi:10.1038/s41579-019-0233-2. ISSN 1740-1526. PMID 31341272.
- ^ "Investigational Monoclonal Antibody to Treat Ebola Is Safe in Adults" (Press release). National Institute of Allergy and Infectious Diseases (NIAID). 24 January 2019. Archived from the original on 13 August 2019. Retrieved 12 August 2019.
- ^ Butler D. "Ebola Experts Seek to Expand Testing". Scientific American. Archived from the original on 13 December 2014. Retrieved 11 December 2014.
- ^ Buchanan RT (29 November 2014). "Ebola outbreak: New 15-minute test offers hope for thousands". The Independent. Archived from the original on 1 December 2014. Retrieved 1 December 2014.
- ^ Falconi M (29 December 2014). "Roche Secures Emergency Approval by U.S. Regulators for Ebola Test". The Wall Street Journal. Archived from the original on 29 December 2014. Retrieved 29 December 2014.
- ^ Junaid A, Tang H, van Reeuwijk A, Abouleila Y, Wuelfroth P, van Duinen V, et al. (January 2020). "Ebola Hemorrhagic Shock Syndrome-on-a-Chip". iScience. 23 (1): 100765. Bibcode:2020iSci...23j0765J. doi:10.1016/j.isci.2019.100765. PMC 6941864. PMID 31887664.
- The article uses public domain text from the CDC as cited.
Bibliography
- McCormick J, Fisher-Hoch S, Horvitz LA (1999) [1996]. Level 4: Virus Hunters of the CDC (Limited preview) (Updated [3rd] ed.). Barnes & Noble. ISBN 978-0760712085. Archived from the original on 21 May 2024. Retrieved 3 September 2020.
Further reading
- Wilson F (2014). CDC Guidance on Ebola Virus (EVD). International Publications Media Group. ISBN 978-1632670113.
- Ebola Virus: New Insights for the Healthcare Professional: 2011 Edition: ScholarlyPaper. Scholarly Editions. 2012. ISBN 978-1464914935.
- Klenk HD (January 1999). Marburg and Ebola Viruses. Current Topics in Microbiology and Immunology 235. Berlin: Springer-Verlag Telos. ISBN 978-3540647294.
- Klenk HD, Feldmann H (2004). Ebola and Marburg viruses: molecular and cellular biology (Limited preview). Wymondham, Norfolk: Horizon Bioscience. ISBN 978-0954523237. Archived from the original on 21 May 2024. Retrieved 3 September 2020.
- Kuhn JH (2008). Filoviruses: A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies. Archives of Virology Supplement (Limited preview). Vol. 20. Vienna: SpringerWienNewYork. ISBN 978-3211206706. Archived from the original on 21 May 2024. Retrieved 3 September 2020.
- Pattyn SR (1978). Ebola Virus Haemorrhagic Fever (1st ed.). Amsterdam: Elsevier/North-Holland Biomedical Press. ISBN 978-0444800602. Archived from the original (Full free text) on 11 December 2010.
- Ryabchikova EI, Price BB (2004). Ebola and Marburg Viruses: A View of Infection Using Electron Microscopy. Columbus, Ohio: Battelle Press. ISBN 978-1574771312.
External links
- WHO fact sheet on Ebola
- Ebola (Ebola Virus Disease) – Centers for Disease Control and Prevention, Viral Special Pathogens Branch.
- Videos: Ebola outbreak response – World Health Organization.
- "Ebola Preparedness and Response". U.S. Food and Drug Administration (FDA). 13 January 2021.
- Ebola: What You Need to Know – Scientific American articles related to Ebola; note these are general reading articles, they are not scientific peer-reviewed research articles.
