Leptospirosis: Difference between revisions
ClueBot NG (talk | contribs) m Reverting possible vandalism by 49.145.177.18 to version by RDBrown. False positive? Report it. Thanks, ClueBot NG. (1956219) (Bot) |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Short description|Blood infection caused by bacteria}} |
|||
{{Infobox disease |
|||
{{redirect|Rat fever|the 2011 Brazilian film|Rat Fever}} |
|||
|Name = Leptospirosis |
|||
{{good article}} |
|||
|Image = Leptospirosis darkfield.jpg |
|||
{{Use dmy dates|date=December 2019}} |
|||
|Caption = ''Leptospira'' magnified 200 times with [[dark-field microscope]] |
|||
{{Use British English|date=March 2020}} |
|||
|DiseasesDB = 7403 |
|||
{{Infobox medical condition (new) |
|||
|ICD10 = {{ICD10|A|27| |a|20}} |
|||
| name = Leptospirosis |
|||
|ICD9 = {{ICD9|100}} |
|||
| synonyms = Rat fever,<ref>{{cite book|last1=Berger |first1= Stephen | name-list-style = vanc |title=Leptospirosis: Global Status |date=2018 |publisher=GIDEON Informatics Inc |isbn=978-1-4988-2031-8 |page=7 |url=https://books.google.com/books?id=ekBLDwAAQBAJ&pg=PA7 |language=en}}</ref> field fever,<ref name=Mos2013>{{cite book|title=Mosby's Medical Dictionary|year=2013|publisher=[[Elsevier Health Sciences]]|isbn=978-0-323-11258-1|page=697|url=https://books.google.com/books?id=aW0zkZl0JgQC&pg=PA697|edition=9|access-date=21 February 2016|archive-url=https://web.archive.org/web/20170908221631/https://books.google.com/books?id=aW0zkZl0JgQC&pg=PA697|archive-date=8 September 2017|url-status=live}}</ref> rat catcher's yellows,<ref name=Mckay2001>{{cite book|last=McKay|first=James E. | name-list-style = vanc |title=Comprehensive Health Care for Dogs|year=2001|publisher=[[The Quarto Group|Creative Pub. International]]|location=Minnetonka, MN.|isbn=978-1-55971-783-0|page=97}}</ref> pretibial fever<ref name="Andrews">{{cite book| first1 = William D | last1 = James | first2 = Dirk M | last2 = Elston | first3 = Timothy G | last3 = Berger | first4 = George Clinton | last4 = Andrews | name-list-style = vanc |title=Andrews' Diseases of the Skin: Clinical Dermatology |publisher=[[Saunders (imprint)|Saunders Elsevier]] |year=2006 |isbn=978-0-7216-2921-6 }}{{rp|290}}</ref> |
|||
|OMIM = 607948 |
|||
| image = Leptospirosis darkfield.jpg |
|||
|MedlinePlus = 001376 |
|||
| alt = |
|||
|eMedicineSubj = article |
|||
| caption = ''Leptospira'' magnified 200-fold with a [[dark-field microscope]]|<!-- altcaption = A magnified image of Leptospira --> |
|||
|eMedicineTopic = 220563 |
|||
| field = [[Infectious disease (medical specialty)|Infectious disease]] |
|||
|eMedicine_mult = {{eMedicine2|article|96569}} {{eMedicine2|article|788751}} |
|||
| symptoms = None, [[headache]]s, [[Myalgia|muscle pains]], [[fever]]s<ref name="Zoey2020"/> |
|||
|MeshName = Leptospirosis |
|||
| complications = [[pulmonary haemorrhage|Bleeding from the lungs]], [[meningitis]], [[kidney failure]]<ref name="Zoey2020"/><ref name=McB2005>{{cite journal | vauthors = McBride AJ, Athanazio DA, Reis MG, Ko AI | title = Leptospirosis | journal = Current Opinion in Infectious Diseases | volume = 18 | issue = 5 | pages = 376–86 | date = October 2005 | pmid = 16148523 | doi = 10.1097/01.qco.0000178824.05715.2c | s2cid = 220576544 }}</ref> |
|||
|MeshNumber = C01.252.400.511 |
|||
| onset = One to two weeks<ref name="Karpagm2020"/> |
|||
| |
|||
| duration = |
|||
| types = |
|||
| causes = ''[[Leptospira]]'' typically spread by [[rodents]]<ref name="Lane 2016"/> |
|||
| risks = Exposure to infected animals, especially their urine, or fresh water or damp soil contaminated with infectious urine<ref name="Lane 2016"/> |
|||
| diagnosis = Testing blood for [[antibodies]] against the bacterium or its [[DNA]]<ref name="Zoey2020"/> |
|||
| differential = [[Malaria]], [[enteric fever]], [[rickettsiosis]], [[dengue]]<ref>{{cite book|last1=Farrar|first1=Jeremy|last2=Hotez|first2=Peter|last3=Junghanss|first3=Thomas|last4=Kang|first4=Gagandeep|last5=Lalloo|first5=David|last6=White|first6=Nicholas J. | name-list-style = vanc |title=Manson's Tropical Diseases E-Book|date=2013|publisher=Elsevier Health Sciences|isbn=978-0-7020-5306-1|page=438|url=https://books.google.com/books?id=GTjRAQAAQBAJ&pg=PA438|language=en|access-date=2 September 2017|archive-url=https://web.archive.org/web/20170908221631/https://books.google.com/books?id=GTjRAQAAQBAJ&pg=PA438|archive-date=8 September 2017|url-status=live}}</ref> |
|||
| prevention = [[Personal protective equipment]], hygiene measures, [[doxycycline]]<ref name="Karpagm2020"/> |
|||
| treatment = [[Doxycycline]], [[penicillin]], [[ceftriaxone]]<ref name="Lane 2016"/> |
|||
| medication = |
|||
| prognosis = Risk of death ~7.5%<ref name="Evangelista2010" /> |
|||
| frequency = One million people per year<ref name=Karpagm2020/><ref name=Costa2015/> |
|||
| deaths = 58,900 per year<ref name=Costa2015/> |
|||
}} |
}} |
||
<!-- Definition and symptoms --> |
|||
'''Leptospirosis''' (also known as '''field fever''',<ref name=Mos2013>{{cite book|title=Mosby's Medical Dictionary|year=2013|publisher=Elsevier Health Sciences|isbn=9780323112581|page=697|url=http://books.google.ca/books?id=aW0zkZl0JgQC&pg=PA697|edition=9}}</ref> '''rat catcher's yellows''',<ref name=Mckay2001>{{cite book|last=McKay|first=James E.|title=Comprehensive health care for dogs|year=2001|publisher=Creative Pub. International|location=Minnetonka, MN.|isbn=9781559717830|page=97}}</ref> and '''pretibial fever'''<ref name="Andrews">{{Cite book|author=James, William D.; Berger, Timothy G.; et al. |title=Andrews' Diseases of the Skin: clinical Dermatology |publisher=Saunders Elsevier |year=2006 |isbn=0-7216-2921-0 }}{{rp|290}}</ref> among others names) is an [[infection]] caused by [[bacteria]] of the ''[[Leptospira]]'' type. Symptoms can range from none to mild such as [[headache]]s, muscle pains, and [[fever]]s; to severe with [[pulmonary hemorrhage|bleeding from the lungs]] or [[meningitis]].<ref name=AFP2010>{{cite journal|last=Slack|first=A|title=Leptospirosis.|journal=Australian family physician|date=Jul 2010|volume=39|issue=7|pages=495–8|pmid=20628664}}</ref><ref name=McB2005/> If the infection causes the person to turn [[jaundice|yellow]], have [[kidney failure]] and bleeding it is then known as ''' Weil's disease'''.<ref name=McB2005>{{cite journal|last=McBride|first=AJ|author2=Athanazio, DA |author3=Reis, MG |author4= Ko, AI |title=Leptospirosis |journal=Current opinion in infectious diseases|date=Oct 2005|volume=18|issue=5|pages=376–86|pmid=16148523 |doi=10.1097/01.qco.0000178824.05715.2c}}</ref> If it causes lots of bleeding from the lungs it is known as '''severe pulmonary haemorrhage syndrome'''.<ref name=McB2005/> |
|||
'''Leptospirosis''' is a [[blood infection]] caused by the [[bacterium]] ''[[Leptospira]]''<ref name="Lane 2016"/> that can infect humans, dogs, [[rodent]]s and many other wild and domesticated animals.<ref name="Lane 2016"/> Signs and symptoms can range from none to mild ([[headache]]s, [[Myalgia|muscle pains]], and [[fever]]s) to severe ([[pulmonary hemorrhage|bleeding in the lungs]] or [[meningitis]]).<ref name="Zoey2020">{{cite journal | vauthors = Soo ZM, Khan NA, Siddiqui R | title = Leptospirosis: Increasing importance in developing countries | journal = Acta Tropica | volume = 201 | pages = 105183 | date = January 2020 | pmid = 31542372 | doi = 10.1016/j.actatropica.2019.105183 | doi-access = free }}</ref> '''Weil's disease''' ({{IPAc-en|'|v|ai|l|z}} {{respell|VILES}}),<ref>{{Cite web|url=https://www.rhs.org.uk/biodiversity/rats|title=Rats / RHS Gardening|website=www.rhs.org.uk}}</ref> the acute, severe form of leptospirosis, causes the infected individual to become [[jaundice]]d (skin and eyes become yellow), develop [[kidney failure]], and bleed.<ref name=McB2005/> Bleeding from the lungs associated with leptospirosis is known as '''severe pulmonary haemorrhage syndrome'''.<ref name="Zoey2020"/> |
|||
<!-- Cause and Diagnosis--> |
<!-- Cause and Diagnosis --> |
||
More than ten genetic types of ''Leptospira'' cause disease in humans.<ref name=Picardeau2017>{{cite journal | vauthors = Picardeau M | title = Virulence of the zoonotic agent of leptospirosis: still terra incognita? | journal = [[Nature Reviews Microbiology|Nature Reviews. Microbiology]] | volume = 15 | issue = 5 | pages = 297–307 | date = May 2017 | pmid = 28260786 | doi = 10.1038/nrmicro.2017.5 | s2cid = 11626842 }}</ref> Both wild and domestic animals can spread the disease, most commonly rodents.<ref name="Lane 2016"/> The bacteria are spread to humans through [[animal urine]] or [[manure|feces]], or water or soil contaminated with animal urine and feces, coming into contact with the eyes, mouth, nose or breaks in the skin.<ref name="Lane 2016"/> In developing countries, the disease occurs most commonly in pest control, farmers and low-income people who live in areas with poor sanitation.<ref name="Zoey2020"/> In developed countries, it occurs during heavy downpours and is a risk to pest controllers, [[sewage]] workers<ref>{{cite journal|title=Leptospirosis Risk in Public Cleansing and Sewer Workers|date=16 October 1987|pmid=3446001|last1=Chan|first1=O. Y.|last2=Chia|first2=S. E.|last3=Nadarajah|first3=N.|last4=Sng|first4=E. H.|journal=Annals of the Academy of Medicine, Singapore|volume=16|issue=4|pages=586–90}}</ref> and those involved in outdoor activities in warm and wet areas.<ref name="Zoey2020"/> Diagnosis is typically by testing for [[antibodies]] against the bacteria or finding bacterial [[DNA]] in the blood.<ref name="Zoey2020"/> |
|||
<!-- Prevention and |
<!-- Prevention and treatment --> |
||
Efforts to prevent the disease include protective equipment to |
Efforts to prevent the disease include protective equipment to block contact when working with potentially infected animals, washing after contact, and reducing rodents in areas where people live and work.<ref name="Karpagm2020"/> The antibiotic [[doxycycline]] is effective in preventing leptospirosis infection.<ref name="Karpagm2020">{{cite journal | vauthors = Karpagam KB, Ganesh B | title = Leptospirosis: a neglected tropical zoonotic infection of public health importance-an updated review | journal = European Journal of Clinical Microbiology & Infectious Diseases | date = January 2020 | volume = 39 | issue = 5 | pages = 835–846 | pmid = 31898795 | doi = 10.1007/s10096-019-03797-4 | s2cid = 209669669 }}</ref> Human vaccines are of limited usefulness;<ref name="Teixeira2019"/> vaccines for other animals are more widely available.<ref name="Ellis2015">{{cite book | vauthors = Ellis WA | title = Leptospira and Leptospirosis | chapter = Animal Leptospirosis | series = Current Topics in Microbiology and Immunology | volume = 387 | pages = 99–137 | date = 2015 | pmid = 25388134 | doi = 10.1007/978-3-662-45059-8_6 | isbn = 978-3-662-45058-1<!-- |series=Current Topics in Microbiology and Immunology (including this removes italics from journal title - unnecessary?---> }}</ref> Treatment when infected is with antibiotics such as doxycycline, [[penicillin]], or [[ceftriaxone]].<ref name="Lane 2016"/> The overall risk of death is 5–10%.<ref name="Evangelista2010" /> However, when the lungs are involved, the risk of death increases to the range of 50–70%.<ref name="Lane 2016"/> |
||
<!-- Epidemiology --> |
<!-- Epidemiology --> |
||
It is estimated that |
It is estimated that one million severe cases of leptospirosis in humans occur every year, causing about 58,900 deaths.<ref name=Costa2015>{{cite journal | vauthors = Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, Stein C, Abela-Ridder B, Ko AI | display-authors = 6 | title = Global Morbidity and Mortality of Leptospirosis: A Systematic Review | journal = PLOS Neglected Tropical Diseases | volume = 9 | issue = 9 | pages = e0003898 | year = 2015 | pmid = 26379143 | pmc = 4574773 | doi = 10.1371/journal.pntd.0003898 | doi-access = free }}</ref> The disease is most common in [[tropical]] areas of the world but may occur anywhere.<ref name="Karpagm2020"/> [[epidemic|Outbreaks]] may arise after heavy rainfall.<ref name="Karpagm2020"/> The disease was first described by physician [[Adolf Weil (physician)|Adolf Weil]] in 1886 in Germany.<ref name=AFP2010>{{cite journal | vauthors = Slack A | title = Leptospirosis | journal = Australian Family Physician | volume = 39 | issue = 7 | pages = 495–8 | date = July 2010 | pmid = 20628664 }}</ref><ref name="Weil">{{cite journal| vauthors = Weil A |title=Über eine eigenthümliche, mit Milztumor, Icterus und Nephritis einhergehende, acute Infektionskrankheit|journal=Deutsches Archiv für Klinische Medizin|date=1886|volume=39|pages=209–232|url=https://babel.hathitrust.org/cgi/pt?id=uiug.30112112319931;view=1up;seq=221|trans-title=On a strange, acute infectious disease, accompanied by swelling of the spleen, icterus, and nephritis|language=de |oclc=1040554855 }}</ref> Infected animals may have no, mild or severe symptoms.<ref name=Center2013>{{cite web |
||
|title=Leptospirosis |
|||
|url=http://www.cfsph.iastate.edu/Factsheets/pdfs/leptospirosis.pdf |
|||
|work=The Center for Food Security and Public Health |
|||
|access-date=8 November 2014 |
|||
|date=October 2013 |
|||
|url-status=live |
|||
|archive-url=https://web.archive.org/web/20141124082710/http://www.cfsph.iastate.edu/Factsheets/pdfs/leptospirosis.pdf |
|||
|archive-date=24 November 2014 |
|||
}}</ref> These may vary by the type of animal.<ref name="Ellis2015"/><ref name=Center2013/> In some animals ''Leptospira'' live in the reproductive tract, leading to transmission during mating.<ref name="Ellis2015"/> |
|||
{{TOC limit}} |
|||
==Signs and symptoms== |
==Signs and symptoms== |
||
[[File:Signs and symptoms of leptospirosis.svg|thumb|upright=1.35|alt=A schematic of the human body showing the symptoms and signs of leptospirosis | Schematic depiction of the symptoms and signs of leptospirosis<ref name="Chieng 2022">{{Cite journal |last=Chieng Raymond |first=Siang Ching |date=2022 |title=Leptospirosis |journal=WikiJournal of Medicine |volume=9 |issue=1 |doi=10.15347/WJM/2022.002 |s2cid=250435398 |doi-access=free }}</ref>]] |
|||
Leptospiral infection in humans causes a range of [[symptom]]s, and some infected persons may have no symptoms at all. Leptospirosis is a [[biphasic disease]] that begins with [[flu-like symptoms]] (fever, chills, [[myalgia]]s, intense headache). The first phase (mild leptospirosis) resolves, and the patient is briefly asymptomatic until the second phase (severe leptospirosis) begins. 90 percent of cases of the disease are mild leptospirosis and without any specific treatment and the rest develop to severe leptospirosis. This is characterized by liver damage (causing [[jaundice]]), [[renal failure]] with same signs and symptoms; the heart and brain can be affected, [[meningitis]] of the outer layer of the brain, [[encephalitis]] of brain tissue with same signs and symptoms; and lung affected as the most serious and life-threatening of all leptospirosis complications. The infection is often [[misdiagnosis|incorrectly diagnosed]] due to the nonspecific symptoms. |
|||
[[File:Conjunctival suffusion of the eyes due to leptospirosis.jpg|thumb|upright=1.15|alt=Human eye showing symptomatic red and yellow patches on the white of the eye | [[Conjunctival suffusion]] (red [[conjunctiva]]) together with jaundice is a specific feature of leptospirosis.<ref name="Chieng 2022"/>]] |
|||
The symptoms of leptospirosis usually appear one to two weeks after infection,<ref name="Karpagm2020"/> but the [[incubation period]] can be as long as a month.<ref name="Haake 2015"/> The illness is [[biphasic disease|biphasic]] in a majority of symptomatic cases. Symptoms of the first phase (acute or leptospiremic phase) last five to seven days. In the second phase (immune phase), the symptoms resolve as antibodies against the bacteria are produced.<ref name="Lane 2016"/> Additional symptoms develop in the second phase.<ref>{{cite web |title=Factsheet about leptospirosis |url=https://www.ecdc.europa.eu/en/leptospirosis/factsheet |website=European Centre for Disease Prevention and Control |date=16 July 2010 |access-date=5 September 2020 |language=en}}</ref> The phases of illness may not be distinct, especially in patients with severe illness.<ref name="Waggoner2016">{{cite journal |vauthors=Waggoner JJ, Pinsky BA |title=Molecular diagnostics for human leptospirosis |journal=Current Opinion in Infectious Diseases |volume=29 |issue=5 |pages=440–5 |date=October 2016 |pmid=27537829 |pmc=5127924 |doi=10.1097/QCO.0000000000000295 }}</ref> 90% of those infected experience mild symptoms while 10% experience severe leptospirosis.<ref name="Cagliero 2018">{{cite journal | vauthors = Cagliero J, Villanueva SY, Matsui M | title = Leptospirosis Pathophysiology: Into the Storm of Cytokines | journal = Frontiers in Cellular and Infection Microbiology | volume = 8 | issue = 204 | pages = 204 | date = 20 June 2018 | pmid = 29974037 | doi = 10.3389/fcimb.2018.00204 | pmc = 6019470 | doi-access = free }}</ref> |
|||
Leptospiral infection in humans causes a range of [[symptom]]s, though some infected persons may have none. The disease begins suddenly with fever accompanied by chills, intense headache, severe [[myalgia|muscle aches]] and abdominal pain.<ref name="Zoey2020"/><ref name="Haake 2015"/> A headache brought on by leptospirosis causes throbbing pain and is characteristically located at the head's bilateral [[Temple (anatomy)|temporal]] or [[frontal bone|frontal]] regions. The person could also have pain behind the eyes and a [[photophobia|sensitivity to light]].<!-- <ref name="Haake 2015"/> --> Muscle pain usually involves the [[Calf (leg)|calf muscle]] and the lower back.<!-- <ref name="Haake 2015"/> --> The most characteristic feature of leptospirosis is the [[conjunctival suffusion]] ([[conjunctivitis]] without [[exudate]]) which is rarely found in other [[febrile]] illnesses. Other characteristic findings on the eye include [[subconjunctival bleeding]] and [[jaundice]].<!-- <ref name="Haake 2015"/> --> A rash is rarely found in leptospirosis. When one is found alternative diagnoses such as [[dengue fever]] and [[chikungunya fever]] should be considered.<!-- <ref name="Haake 2015"/> --> Dry cough is observed in 20–57% of people with leptospirosis. Thus, this clinical feature can mislead a doctor to diagnose the disease as a respiratory illness. Additionally, [[gastrointestinal]] symptoms such as [[nausea]], vomiting, abdominal pain, and diarrhoea frequently occur. Vomiting and diarrhea may contribute to [[dehydration]].<!-- <ref name="Haake 2015"/> --> The abdominal pain can be due to [[acalculous cholecystitis]] or [[pancreatitis|inflammation of the pancreas]].<ref name="Haake 2015"/> Rarely, the [[Lymphadenopathy|lymph nodes]], [[Hepatomegaly|liver]], and [[Splenomegaly|spleen]] may be enlarged and palpable.<ref name="Lane 2016"/> |
|||
Signs and symptoms of leptospirosis include high [[fever]], severe [[headache]], chills, muscle aches, and [[vomiting]], and may include jaundice, [[Conjunctival suffusion|red eyes]], [[abdominal pain]], [[diarrhea]], and [[rash]]. Initial presentation may resemble pneumonia. The symptoms in humans appear after a 4–14 day incubation period. More severe manifestations include [[meningitis]], extreme [[fatigue (medical)|fatigue]], [[hearing loss]], respiratory distress, [[azotemia]], and renal interstitial tubular necrosis, which results in [[renal failure]] and occasionally [[liver failure]] (the severe form of this disease is known as Weil's disease, though it is sometimes named Weil Syndrome).<ref>{{cite web|url=http://www.medterms.com/script/main/art.asp?articlekey=23871 |title=Weil syndrome definition – Medical Dictionary definitions of popular medical terms easily defined on MedTerms |publisher=Medterms.com |date=2012-10-09 |accessdate=2013-07-19}}</ref> [[Cardiovascular]] problems are also possible. |
|||
There will be a resolution of symptoms for one to three days.<ref name="Karpagm2020"/> The immune phase starts after this and can last from four to 30 days and can be anything from brain to kidney complications.<ref name="Bennett 2015">{{cite book |last1=Bennett |first1=John E |last2=Raphael |first2=Dolin |last3=Martin |first3=J Blaser |last4=Bart |first4=J Currie | name-list-style = vanc |title=Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases|chapter=223 |date=2015 |publisher=[[Elsevier]] |isbn=978-1-4557-4801-3 |pages=2541–2549 |edition=Eighth}}</ref> The hallmark of the second phase is [[meningitis|inflammation of the membranes covering the brain]].<ref name="Karpagm2020"/> Signs and symptoms of meningitis include severe headache and neck stiffness.<ref name="Karpagm2020"/> Kidney involvement is associated with reduced or absent urine output.<ref name="Karpagm2020"/> |
|||
[[incubation period|Incubation]] (time of exposure to first [[symptom]]s) in animals is anywhere from 2 to 20 days. In dogs, leptospirosis most often damages the liver and kidney. In addition, recent reports describe a pulmonary form of canine leptospirosis associated with severe hemorrhage in the lungs—similar to human pulmonary hemorrhagic syndrome.<ref name=Klopfleisch11>{{cite journal |author=Klopfleisch R, Kohn B, Plog S, Weingart C, Nöckler K, Mayer-Scholl A, Gruber AD. |title=An Emerging Pulmonary Haemorrhagic Syndrome in Dogs: Similar to the Human Leptospiral Pulmonary Haemorrhagic Syndrome? |journal=Vet Med Int. |year=2011 |volume=33 |pmid=21274452 |page=928541 |doi=10.4061/2010/928541 |pmc=3025382}}</ref><ref>{{cite journal|author=Kohn B, Steinicke K, Arndt G, Gruber AD, Guerra B, Jansen A, Kaser-Hotz B, Klopfleisch R, Lotz F, Luge E, Nöckler K.|title=Pulmonary abnormalities in dogs with leptospirosis |journal=J Vet Intern Med. |year=2010 |volume=24 |pmid=20738768 |pages=791–807 |doi=10.1111/j.1939-1676.2010.0585.x|issue=6}}</ref> [[Vasculitis]] may occur, causing [[edema]] and potentially [[disseminated intravascular coagulation]] (DIC). [[Myocarditis]], [[pericarditis]], meningitis, and [[uveitis]] are also possible sequelae.<ref name="Langston 2003"/> |
|||
The classic form of severe leptospirosis, known as Weil's disease, is characterised by liver damage (causing jaundice), [[kidney failure]], and bleeding, which happens in 5–10% of those infected.<ref name="Karpagm2020"/> Lung and brain damage can also occur. For those with signs of [[meningoencephalitis|inflammation of membranes covering the brain and the brain itself]], [[altered level of consciousness]] can happen. A variety of neurological problems such as [[hemiplegia|paralysis of half of the body]], [[transverse myelitis|complete inflammation of a whole horizontal section of spinal cord]], and [[Guillain-Barré syndrome]] are the complications.<!-- <ref name="Haake 2015"/> --> Signs of bleeding such as [[petechiae]], [[ecchymoses]], [[epistaxis|nose bleeding]], [[melena|blackish stools due to bleeding in the stomach]], [[haematemesis|vomiting blood]] and [[pulmonary haemorrhage|bleeding from the lungs]] can also be found. Prolongation of [[prothrombin time]] in [[coagulation testing]] is associated with severe bleeding manifestation. However, [[thrombocytopenia|low platelet count]] is not associated with severe bleeding.<ref name="Haake 2015"/> Pulmonary haemorrhage is alveolar haemorrhage (bleeding into the [[Pulmonary alveolus|alveoli]] of the lungs) leading to massive [[haemoptysis|coughing up of blood]], and causing [[acute respiratory distress syndrome]], where the risk of death is more than 50%.<ref name="Haake 2015"/> Rarely, [[myocarditis|inflammation of the heart muscles]], [[pericarditis|inflammation of membranes covering the heart]], [[heart block|abnormalities in the heart's natural pacemaker]] and [[arrhythmia|abnormal heart rhythms]] may occur.<ref name="Lane 2016"/> |
|||
Eye finding may include [[conjunctival suffusion]] |
|||
==Cause== |
==Cause== |
||
===Bacteria=== |
|||
[[Image:Leptospira scanning micrograph.jpg|thumb|[[Scanning electron micrograph]] of a number of ''Leptospira'' sp. bacteria atop a 0.1 µm [[polycarbonate]] filter]] |
|||
[[File:Leptospira scanning micrograph.jpg|thumb|left|upright=1.15|alt=A scanning electron micrograph of several lepitospira bacteria on a filter | [[Scanning electron micrograph]] of a number of ''Leptospira'' sp. bacteria atop a 0.1 μm [[polycarbonate]] filter<ref name="Chieng 2022"/>]] |
|||
[[File:indian6.jpg|thumb|The Native American lifestyle exposed them to the leptospiral life cycle]] |
|||
Leptospirosis is caused by [[spirochaete]] bacteria that belong to the [[genus]] ''[[Leptospira]]'', which are [[Cellular respiration#Aerobic respiration|aerobic]],<ref name="Lane 2016"/> [[Screw thread#Handedness|right-handed]] [[helix|helical]],<ref name=Picardeau2017/> and 6–20 [[micrometre|micrometer]]s long.<ref name="Karpagm2020"/> Like [[Gram-negative]] bacteria, ''Leptospira'' have an [[Bacterial outer membrane|outer membrane]] studded with [[lipopolysaccharide]] (LPS) on the surface, an [[Cell membrane|inner membrane]] and a layer of [[peptidoglycan]] cell wall. However, unlike Gram-negative bacteria, the peptidoglycan layer in ''Leptospira'' lies closer to the inner than the outer membrane. This results in a fluid outer membrane loosely associated with the cell wall.<ref name=Cameron2015>{{cite book | vauthors = Cameron CE | title = Leptospira and Leptospirosis | chapter = Leptospiral Structure, Physiology, and Metabolism | series = Current Topics in Microbiology and Immunology | volume = 387 | pages = 21–41 | date = 2015 | pmid = 25388131 | doi = 10.1007/978-3-662-45059-8_3 | isbn = 978-3-662-45058-1 }}</ref> In addition, ''Leptospira'' have a [[flagellum]] located in the [[periplasm]], associated with corkscrew style movement.<ref name="Karpagm2020"/> [[Chemoreceptor]]s at the poles of the bacteria sense various substrates and change the direction of its movement.<ref name=Picardeau2017/> The bacteria are traditionally visualised using [[dark-field microscopy]] without staining.<ref name="Karpagm2020"/> |
|||
Leptospirosis is caused by a [[spirochaete]] bacterium called ''[[Leptospira]]'' spp. At least five important [[serotype]]s exist in the [[United States]] and [[Canada]], all of which cause disease in dogs:<ref name="Langston 2003">{{Cite journal|author=Langston CE, Heuter KJ |title=Leptospirosis. A re-emerging zoonotic disease |journal=Veterinary Clinics of North America, Small Animal Practice |volume=33 |issue=4 |pages=791–807 |date=July 2003|pmid=12910744 |doi=10.1016/S0195-5616(03)00026-3}}</ref><ref name=Kohn_1>{{Cite journal|author=Kohn B, Steinicke K, Arndt G, Gruber AD, Guerra B, Jansen A, Kaser-Hotz B, Klopfleisch R, Lotz F, Luge E, Nöckler K.|title=Pulmonary abnormalities in dogs with leptospirosis |journal=J Vet Intern Med. |volume=24 |issue=6 |pages=1277–82 |year=2010|pmid=20738768 |doi= 10.1111/j.1939-1676.2010.0585.x}}</ref><ref name=Klopfleisch11/> |
|||
*Icterohaemorrhagiae |
|||
*Canicola |
|||
*Pomona |
|||
*Grippotyphosa |
|||
*Bratislava |
|||
Other (more common) lethal infectious strains exist. Genetically different leptospira organisms may be identical serologically and vice versa. Hence, some argue about strain identification. The traditional serologic system currently seems more useful from a diagnostic and epidemiologic standpoint—but this may change with further development and spread of technologies like [[polymerase chain reaction]] (PCR). |
|||
A total of 66 species of ''Leptospira'' has been identified. Based on their genomic sequence, they are divided into two [[clade]]s and four subclades: P1, P2, S1, and S2.<ref name=Caimi2020>{{cite journal | vauthors = Caimi K, Ruybal P | title = Leptospira spp., a genus in the stage of diversity and genomic data expansion | journal = Infection, Genetics and Evolution | volume = 81 | pages = 104241 | date = February 2020 | pmid = 32061688 | doi = 10.1016/j.meegid.2020.104241 | bibcode = 2020InfGE..8104241C | s2cid = 211135356 }}</ref> The 19 members of the P1 subclade include the 8 species that can cause severe disease in humans: ''[[Leptospira alexanderi|L. alexanderi]]'', ''[[Leptospira borgpetersenii|L. borgpetersenii]]'', ''[[Leptospira interrogans|L. interrogans]]'', ''[[Leptospira kirschneri|L. kirschneri]]'', ''L. mayottensis'', ''[[Leptospira noguchii|L. noguchii]]'', ''[[Leptospira santarosai|L. santarosai]]'', and ''[[Leptospira weilii|L. weilii]].''<ref name=Picardeau2017/><ref name=Caimi2020/> The P2 clade comprises 21 species that may cause mild disease in humans. The remaining 26 species comprise the S1 and S2 subclades, which include "saprophytes" known to consume decaying matter ([[saprotrophic nutrition]]).<ref name=Caimi2020/> Pathogenic ''Leptospira'' do not multiply in the environment. ''Leptospira'' require high humidity for survival but can remain alive in environments such as stagnant water or contaminated soil. The bacterium can be killed by temperatures of {{cvt|50|°C}} and can be inactivated by 70% [[ethanol]], 1% [[sodium hypochlorite]], [[formaldehyde]], detergents and acids.<ref name="Spickler 2013"/> |
|||
Leptospirosis is transmitted by the urine of an infected animal, and is contagious as long as the urine is still moist. Rats, mice, and moles are important primary hosts—but a wide range of other mammals including dogs, deer, rabbits, hedgehogs, cows, sheep, raccoons, opossums, skunks, and certain marine mammals carry and transmit the disease as secondary hosts. In Africa, the [[banded mongoose]] has been identified as a carrier of the pathogen, likely in addition to other African wildlife hosts.<ref>{{cite journal |author=Jobbins SE, Sanderson CE, Alexander KA |title=''Leptospira interrogans'' at the human-wildlife interface in northern Botswana: a newly identified public health threat |journal=Zoonoses Public Health |volume=61 |issue=2 |pages=113–23 |date=March 2014 |pmid=23672285 |doi=10.1111/zph.12052 |layurl=[http://www.sciencedaily.com/releases/2013/05/130514122756.htm Human disease leptospirosis identified in new species, the banded mongoose, in Africa] |laysource=Sciencedaily |laydate=2013-05-14 }}</ref> Dogs may lick the urine of an infected animal off the grass or [[soil]], or drink from an infected puddle. |
|||
''Leptospira'' are also classified based on their [[serotype|serovar]]. The diverse sugar composition of the lipopolysaccharide on the surface of the bacteria is responsible for the antigenic difference between serovars.<ref name=Picardeau2017/> About 300 pathogenic serovars of ''Leptospira'' are recognised. Antigenically related serovars (belonging to the same serogroup) may belong to different species because of [[horizontal gene transfer]] of [[Lipopolysaccharide biosynthesis|LPS biosynthetic genes]] between different species. Currently, the cross [[Agglutination (biology)|agglutination]] absorption test and DNA-DNA hybridisation are used to classify ''Leptospira'' species, but are time-consuming. Therefore, total genomic sequencing could potentially replace these two methods as the new gold standard of classifying ''Leptospira'' species.<ref name=Picardeau2017/> |
|||
House-bound domestic dogs have contracted leptospirosis, apparently from licking the urine of infected mice in the house. The type of habitats most likely to carry infective bacteria are muddy riverbanks, ditches, gullies, and muddy livestock rearing areas where there is regular passage of wild or farm mammals. The incidence of leptospirosis correlates directly with the amount of rainfall, making it seasonal in temperate climates and year-round in tropical climates. |
|||
Leptospirosis also transmits via the semen of infected animals.<ref name="lept">{{Cite journal| author=Kiktenko VS| title=Leptospirosis infection through insemination of animals| journal=J Hyg Epidemiol Microbiol Immunol.| year=1976| volume=21| issue=2|pages=207–213 | pmid=987112 | last2=Balashov | first2=NG | last3=Rodina | first3=VN}}</ref> |
|||
===Transmission=== |
|||
Humans become infected through contact with water, food, or soil that contains urine from these infected animals. This may happen by swallowing contaminated food or water or through skin contact. The disease is not known to spread between humans, and bacterial dissemination in convalescence is extremely rare in humans. Leptospirosis is common among water-sport enthusiasts in specific areas, as prolonged immersion in water promotes the entry of the bacteria. Surfers and whitewater paddlers<ref name="Kayaking as a risk factor for leptospirosis. Shaw RD.">{{cite journal |author=Shaw RD |title=Kayaking as a risk factor for leptospirosis |journal=Mo Med |volume=89 |issue=6 |pages=354–7 |date=June 1992|pmid=1620089 }}</ref> are at especially high risk in areas that have been shown to contain the bacteria, and can contract the disease by swallowing [[contaminated water]], splashing contaminated water into their eyes or nose, or exposing open wounds to infected water.<ref name="Surfing Sicknesses">[http://surf.transworld.net/2009/01/27/seven-surf-sicknesses/ transworld.net: Seven Surfing Sicknesses].</ref> |
|||
[[File:Working at aaddy rice field without a footwear, is a risk factor for leptospirosis.png|thumb|upright=1.35|alt=Workers in a rice paddy field | Working in a paddy field barefoot is a risk factor for leptospirosis.<ref name="Chieng 2022"/>]] |
|||
The bacteria can be found in ponds, rivers, puddles, sewers, agricultural fields and moist soil.<ref name="Karpagm2020"/> Pathogenic ''Leptospira'' have been found in the form of aquatic [[biofilms]], which may aid survival in the environment.<ref name=Barragan2017>{{cite journal | vauthors = Barragan V, Olivas S, Keim P, Pearson T | title = Critical Knowledge Gaps in Our Understanding of Environmental Cycling and Transmission of Leptospira spp | journal = Applied and Environmental Microbiology | volume = 83 | issue = 19 | date = October 2017 | pmid = 28754706 | pmc = 5601346 | doi = 10.1128/AEM.01190-17 | bibcode = 2017ApEnM..83E1190B }}</ref> |
|||
The number of cases of leptospirosis is directly related to the amount of rainfall, making the disease seasonal in temperate climates and year-round in tropical climates.<ref name="Karpagm2020"/> The risk of contracting leptospirosis depends upon the risk of disease carriage in the community and the frequency of exposure.<ref name="Haake 2015"/> In rural areas, farming and animal husbandry are the major risk factors for contracting leptospirosis.<ref name="Zoey2020"/> Poor housing and inadequate sanitation also increase the risk of infection.<ref name="Haake 2015"/> In tropical and semi-tropical areas, the disease often becomes [[epidemic|widespread]] after heavy rains or after flooding.<ref name="Karpagm2020"/> |
|||
===At risk occupations=== |
|||
''Leptospira'' are found mostly in mammals.<ref name="Zoey2020"/> However, reptiles and [[Poikilotherm|cold-blooded animals]] such as frogs, snakes, turtles, and toads have been shown to have the infection.<ref name="Ellis2015"/> Whether there are reservoirs of human infection is unknown.<ref name="Haake 2015"/><ref name="Ellis2015"/> Rats, mice, and moles are important [[Host (biology)#Definitive and secondary hosts|primary hosts]], but other mammals including dogs, deer, rabbits, hedgehogs, cows, sheep, swine, raccoons, opossums, and skunks can also carry the disease.<ref name="Ellis2015"/> In Africa, a number of wildlife hosts have been identified as carriers, including the [[banded mongoose]], [[fennec fox|Egyptian fox]], [[Rusa deer]], and [[shrews]].<ref>{{cite journal | vauthors = Allan KJ, Biggs HM, Halliday JE, Kazwala RR, Maro VP, Cleaveland S, Crump JA | title = Epidemiology of Leptospirosis in Africa: A Systematic Review of a Neglected Zoonosis and a Paradigm for 'One Health' in Africa | journal = PLOS Neglected Tropical Diseases | volume = 9 | issue = 9 | pages = e0003899 | date = 2015 | pmid = 26368568 | pmc = 4569256 | doi = 10.1371/journal.pntd.0003899 | doi-access = free }}</ref> There are various mechanisms whereby animals can infect each other. Dogs may lick the urine of an infected animal off the grass or [[soil]], or drink from an infected puddle. House-bound domestic dogs have contracted leptospirosis, apparently from licking the urine of infected mice in the house.<ref>{{cite journal | vauthors = Rodriguez-Morales AJ, Castañeda-Hernández DM | title = Spirochetes: Leptospira | journal = Encyclopedia of Food Safety | volume = 2 | issue = | pages = 189–193 | date = 2014 | pmid = | pmc = | doi = 10.1016/B978-0-12-378612-8.00131-1 | isbn = 978-0-12-378613-5 }}</ref> Leptospirosis can also be transmitted via the semen of infected animals.<ref name="Ellis2015"/> The duration of bacteria being consistently present in animal urine may persist for years.<ref name="Ellis2015"/> |
|||
Occupations at risk include [[veterinarian]]s, slaughterhouse workers, farmers, sewer maintenance workers, waste disposal facility workers, and people who work on derelict buildings.<ref>{{cite web | title = Weils Disease at Work | url =http://www.injury-compensation-zone.co.uk/compensation-weils-disease-work/}}</ref> [[Slaughterhouse]] workers can contract the disease through contact with infected blood or body fluids. Rowers, kayakers and canoeists also sometimes contract the disease.<ref name="Langston 2003"/> |
|||
Humans are the [[Host (biology)#Dead-end hosts|accidental host]] of ''Leptospira''.<ref name="Zoey2020"/> Humans become infected through contact with water or moist soil that contains urine & feces from infected animals.<ref name="Karpagm2020"/> The bacteria enter through cuts, abrasions,<ref name="Karpagm2020"/> ingestion of contaminated food, or contact with [[mucous membrane]] of the body (e.g. mouth, nose, and eyes).<ref name="Kin Chin 2019"/> Occupations at risk of contracting leptospirosis include farmers, fishermen, garbage collectors and sewage workers.<ref name="Zoey2020"/> The disease is also related to [[adventure tourism]] and recreational activities.<ref name="Zoey2020"/> It is common among water-sports enthusiasts in specific areas, including [[triathlon]]s, water [[rafting]], [[canoeing]] and swimming, as prolonged immersion in water promotes the entry of the bacteria.<ref name="Zoey2020"/> However, ''Leptospira'' are unlikely to penetrate intact skin.<ref name="Lane 2016"/> The disease is not known to spread between humans, and bacterial dissemination in [[convalescence|recovery period]] is extremely rare in humans.<ref name="Lane 2016">{{cite journal|vauthors=Lane AB, Dore MM|title=Leptospirosis: A clinical review of evidence based diagnosis, treatment and prevention|journal=World Journal of Clinical Infectious Diseases|volume=6|issue=4 |year=2016|pages=61|issn=2220-3176|doi=10.5495/wjcid.v6.i4.61|doi-access=free}}</ref> Once humans are infected, bacterial shedding from the kidneys usually persists for up to 60 days.<ref name="Spickler 2013"/> |
|||
Rarely, leptospirosis can be transmitted through an organ transplant.<ref>{{cite journal |vauthors=Song AT, Abas L, Andrade LC, Andraus W, D'Albuquerque LA, Abdala E |title=A first report of leptospirosis after liver transplantation |journal=Transplant Infectious Disease |volume=18 |issue=1 |pages=137–140 |date=February 2016 |pmid=26671230 |doi=10.1111/tid.12490 |s2cid=3548455}}</ref> Infection through the [[placenta]] during pregnancy is also possible.<ref>{{cite journal |vauthors=Puliyath G, Singh S |title=Leptospirosis in pregnancy |journal=European Journal of Clinical Microbiology & Infectious Diseases |volume=31 |issue=10 |pages=2491–2496 |date=October 2012 |pmid=22549729 |doi=10.1007/s10096-012-1625-7 |s2cid=14033595}}</ref><ref>{{cite journal |vauthors=Carles G, Montoya E, Joly F, Peneau C |title=[Leptospirosis and pregnancy. Eleven cases in French Guyana] |journal=Journal de Gynécologie, Obstétrique et Biologie de la Reproduction |volume=24 |issue=4 |pages=418–421 |date=1995 |pmid=7650320}}</ref><ref>{{cite journal |vauthors=Koe SL, Tan KT, Tan TC |title=Leptospirosis in pregnancy with pathological fetal cardiotocography changes |journal=Singapore Medical Journal |volume=55 |issue=2 |pages=e20-24 |date=February 2014 |pmid=24712035 |pmc=4291937 |doi=10.11622/smedj.2013194}}</ref> It can cause [[miscarriage]] and infection in [[infant]]s.<ref>{{cite journal |vauthors=Shaked Y, Shpilberg O, Samra D, Samra Y |title=Leptospirosis in pregnancy and its effect on the fetus: case report and review |journal=Clinical Infectious Diseases |volume=17 |issue=2 |pages=241–243 |date=August 1993 |pmid=8399874 |doi=10.1093/clinids/17.2.241}}</ref> Leptospirosis transmission through eating raw meat of wildlife animals have also been reported (e.g. psychiatric patients with allotriophagy).<ref>{{Cite journal |vauthors=Fabiani A, Dal Bo E, Di Bella S, Gabrielli M, Bologna A, Albert U, Sanson G |date=2021-07-05 |title=Pica (Allotriophagy): An Underestimated Risk Factor for Severe Leptospirosis (Weil's Diseases)? Report of a Leptospira Septic Shock Successfully Managed with ECMO |journal=Infectious Disease Reports |volume=13 |issue=3 |pages=619–626 |doi=10.3390/idr13030058 |pmid=34287302 |pmc=8293114 |issn=2036-7449 |doi-access=free}}</ref> |
|||
==Pathogenesis== |
|||
[[File:Pathogeneis of leptospirosis.svg|thumb|upright=1.35|alt= Diagram showing the pathogenesis of leptospirosis | Ways of ''Leptospira'' bacteria infecting human cells and blood stream<ref name="Chieng 2022"/>]] |
|||
When animals ingest the bacteria, they circulate in the bloodstream, then lodge themselves into the kidneys through the [[glomerulus|glomerular]] or [[peritubular capillaries]]. The bacteria then pass into the [[Lumen (anatomy)|lumens]] of the [[renal tubules]] and colonise the [[brush border]] and [[proximal convoluted tubule]]. This causes the continuous shedding of bacteria in the urine without the animal experiencing significant ill effects. This relationship between the animal and the bacteria is known as a [[commensal relationship]], and the animal is known as a [[Natural reservoir|reservoir host]].<ref name="Haake 2015">{{cite book |vauthors=Haake DA, Levett PN |title=Leptospira and Leptospirosis |chapter=Leptospirosis in Humans |publisher=Springer |series=Current Topics in Microbiology and Immunology |veditors=Adler B |volume=387 |pages=65–97 |date=25 May 2015 |pmid=25388133 |pmc=4442676 |doi=10.1007/978-3-662-45059-8_5 |isbn=978-3-662-45058-1}}</ref> |
|||
Humans are the [[Host (biology)#Dead-end hosts|accidental host]] of ''Leptospira''.<ref name="Zoey2020"/> The pathogenesis of leptospirosis remains poorly understood despite research efforts.<ref name="Karpagm2020"/><ref name="Kin Chin 2019">{{cite journal | vauthors = Chin VK, Basir R, Nordin SA, Abdullah M, Sekawi Z | title = Pathology and Host Immune Evasion During Human Leptospirosis: a Review | journal = International Microbiology | pages = 127–136 | date = March 2019 | volume = 23 | issue = 2 | pmid = 30875033 | doi = 10.1007/s10123-019-00067-3 | s2cid = 78095369 | url = http://psasir.upm.edu.my/id/eprint/87068/1/Pathology%20and%20host%20immune%20evasion%20during%20human%20leptospirosis.pdf }}</ref> The bacteria enter the human body through either breaches in the skin or the mucous membrane, then into the bloodstream. The bacteria later attach to the [[endothelium|endothelial]] cells of the blood vessels and [[extracellular matrix]] (complex network of proteins and carbohydrates present between cells). The bacteria use their flagella for moving between cell layers. They bind to cells such as [[fibroblast]]s, [[macrophage]]s, endothelial cells, and kidney epithelial cells.<!-- <ref name=Picardeau2017/> --> They also bind to several human proteins such as complement proteins, [[thrombin]], [[fibrinogen]], and [[plasminogen]] using surface leptospiral [[immunoglobulin superfamily|immunoglobulin-like]] (Lig) proteins such as LigB and LipL32, whose genes are found in all pathogenic species.<ref name=Picardeau2017/><ref name="Kin Chin 2019"/> |
|||
Through the [[innate immune system]], endothelial cells of the capillaries in the human body are activated by the presence of these bacteria. The endothelial cells produce [[cytokines]] and [[antimicrobial peptides]] against the bacteria. These products regulate the [[Coagulation#Coagulation cascade|coagulation cascade]] and movements of white blood cells.<ref name=Picardeau2017/> Macrophages presented in humans are able to [[phagocytose|engulf]] ''Leptospira''. However, ''Leptospira'' are able to reside and proliferate in the [[cytosol|cytoplasmic matrix]] after being ingested by macrophages.<ref name=Picardeau2017/> Those with severe leptospirosis can experience a high level of cytokines such as [[interleukin 6]], [[tumor necrosis factor alpha]] (TNF-α), and [[interleukin 10]]. The high level of cytokines causes [[sepsis]]-like symptoms which is life-threatening instead of helping to fight against the infection.<ref name="Cagliero 2018"/> Those who have a high risk of sepsis during a leptospirosis infection are found to have the [[HLA-DQ6]] [[genotype]], possibly due to [[superantigen]] activation, which damages bodily organs.<ref name="Haake 2015"/> |
|||
''Leptospira'' LPS only activates [[toll-like receptor 2]] (TLR2) in [[monocyte]]s in humans. The lipid A molecule of the bacteria is not recognised by human [[TLR4]] receptors. Therefore, the lack of ''Leptospira'' recognition by TLR4 receptors probably contributes to the leptospirosis disease process in humans.<ref name=Picardeau2017/> |
|||
Although there are various mechanisms in the human body to fight against the bacteria, ''Leptospira'' is well adapted to such an inflammatory condition created by it.<!-- <ref name=Picardeau2017/> --> In the bloodstream, it can activate host plasminogen to become [[plasmin]] that breaks down extracellular matrix, degrades [[fibrin]] clots and complemental proteins ([[C3b]] and [[Complement component 5|C5]]) to avoid [[opsonisation]]. It can also recruit complement regulators such as [[Factor H|Factor'' ''H]], [[Complement component 4B|C4b]]-binding protein, factor H-like binding protein, and [[vitronectin]] to prevent the activation of [[Complement membrane attack complex|membrane attack complex]] on its surface. It also secretes [[protease]]s to degrade complement proteins such as [[Complement component 3|C3]]. It can bind to thrombin that decreases the fibrin formation. Reduced fibrin formation increases the risk of bleeding.<ref name=Picardeau2017/> ''Leptospira'' also secretes [[sphingomyelinase]] and [[haemolysin]] that target red blood cells.<ref name="Karpagm2020"/> |
|||
''Leptospira'' spreads rapidly to all organs through the bloodstream.<ref name=Picardeau2017/> They mainly affect the liver. They invade spaces between [[hepatocyte]]s, causing apoptosis. The damaged hepatocytes and hepatocyte intercellular junctions cause leakage of bile into the bloodstream, causing elevated levels of [[bilirubin]], resulting in jaundice. Congested [[liver sinusoid]]s and [[perisinusoidal space]]s have been reported. Meanwhile, in the lungs, petechiae or frank [[haemorrhage|bleeding]] can be found at the [[alveolar septum]] and spaces between alveoli.<ref name="Haake 2015"/> ''Leptospira'' secretes toxins that cause mild to severe kidney failure or [[interstitial nephritis]].<ref name="Kin Chin 2019"/> The kidney failure can recover completely or lead to [[atrophy]] and [[fibrosis]].<ref name="Haake 2015"/> Rarely, inflammation of the heart muscles, coronary arteries, and [[aorta]] are found.<ref name="Bennett 2015"/> |
|||
==Diagnosis== |
==Diagnosis== |
||
[[ |
[[File: Leptospirosis in kidney.jpg|thumb|alt=Kidney tissue showing leptospira bacteria | Kidney tissue, using a [[silver stain]]ing technique, revealing the presence of ''Leptospira'' bacteria<ref name="Chieng 2022"/>]] |
||
[[File: Diffuse pulmonary haemorrhages of the lungs infected by leptospirosis.png|thumb|alt=X-ray showing lungs bleeding due to leptospirosis infection | Diffuse lungs bleeding due to leptospirosis infection<ref name="Chieng 2022"/>]] |
|||
On infection the [[microorganism]] can be found in [[blood]] and [[Cerebrospinal fluid]] (CSF) for the first 7 to 10 days (invoking serologically identifiable reactions) and then moving to the kidneys. After 7 to 10 days the microorganism can be found in fresh urine. Hence, early diagnostic efforts include testing a serum or blood sample serologically with a panel of different strains. |
|||
===Laboratory tests=== |
|||
Kidney function tests ([[blood urea nitrogen]] and [[creatinine]]) as well as blood tests for liver functions are performed. The latter reveal a moderate elevation of transaminases. Brief elevations of [[aspartate aminotransferase]] (AST), [[alanine aminotransferase]] (ALT), and [[gamma-glutamyltransferase]] (GGT) levels are relatively mild. These levels may be normal, even in children with jaundice. |
|||
For those who are infected, a [[complete blood count]] may show a [[leukocytosis|high white cell count]] and a low platelet count. When a [[anaemia|low haemoglobin count]] is present together with a [[leukopenia|low white cell count]] and [[thrombocytopenia]], [[bone marrow suppression]] should be considered.<ref name="Haake 2015"/> [[Erythrocyte sedimentation rate]] and [[C-reactive protein]] may also be elevated.<ref name="Lane 2016"/> |
|||
The kidneys are commonly involved in leptospirosis. Blood [[urea]] and [[creatinine]] levels will be elevated. Leptospirosis increases potassium excretion in urine, which leads to a [[hypokalemia|low potassium level]]<ref name="Haake 2015"/> and a [[hyponatremia|low sodium level]] in the blood.<ref name="Lane 2016"/><ref name="Haake 2015"/> Urinalysis may reveal the [[proteinuria|presence of protein]], [[pyuria|white blood cells]], and microscopic [[haematuria]].<ref name="Lane 2016"/> Because the bacteria settle in the kidneys, urine cultures will be positive for leptospirosis starting after the second week of illness until 30 days of infection.<ref name="Lane 2016"/> |
|||
[[medical diagnosis|Diagnosis]] of leptospirosis is confirmed with tests such as [[ELISA|enzyme-linked immunosorbent assay]] (ELISA) and [[polymerase chain reaction]] (PCR). The MAT (microscopic agglutination test), a serological test, is considered the [[Gold standard (test)|gold standard]] in diagnosing leptospirosis. As a large panel of different leptospira must be subcultured frequently, which is both laborious and expensive, it is underused, especially in developing countries. |
|||
For those with liver involvement, [[transaminase]]s and [[direct bilirubin]] are elevated in [[liver function test]]s. The Icterohaemorrhagiae serogroup is associated with jaundice and elevated bilirubin levels. [[Hemolytic anemia]] contributes to jaundice. A feature of leptospirosis is acute [[haemolytic anaemia]] and [[Conjugation (biochemistry)|conjugated]] hyperbilirubinemia, especially in patients with [[glucose-6-phosphate dehydrogenase deficiency]].<ref name="Haake 2015"/> Abnormal [[serum (blood)|serum]] [[amylase]] and [[lipase]] levels (associated with pancreatitis) are found in those who are admitted to hospital due to leptospirosis. Impaired kidney function with [[creatinine clearance]] less than 50 ml/min is associated with elevated pancreatic enzymes.<ref name="Haake 2015"/> |
|||
[[Differential diagnosis]] list for leptospirosis is very large due to diverse symptomatics. For forms with middle to high severity, the list includes [[dengue fever]] and other hemorrhagic [[fever]]s, [[hepatitis]] of various [[etiology|etiologies]], viral [[meningitis]], [[malaria]], and [[typhoid fever]]. Light forms should be distinguished from [[influenza]] and other related viral diseases. Specific tests are a must for proper diagnosis of leptospirosis. |
|||
For those with severe headache who show signs of meningitis, a [[lumbar puncture]] can be attempted. If infected, [[cerebrospinal fluid]] (CSF) examination shows [[Lymphocyte|lymphocytic]] predominance with a cell count of about 500/mm<sup>3</sup>, protein between 50 and 100 mg/mL and normal glucose levels. These findings are consistent with [[aseptic meningitis]].<ref name="Haake 2015"/> |
|||
Under circumstances of limited access (e.g., developing countries) to specific diagnostic means, close attention must be paid to the [[Anamnesis (medicine)|medical history]] of the patient. Factors such as certain dwelling areas, seasonality, contact with [[stagnant water|stagnant]] contaminated water (bathing, swimming, working on flooded meadows, etc.) or rodents in the medical history support the leptospirosis hypothesis and serve as indications for specific tests (if available). |
|||
====Serological tests==== |
|||
''Leptospira'' can be cultured in [[Ellinghausen-McCullough-Johnson-Harris medium]] (EMJH), which is incubated at 28 to 30 °C.<ref>{{Cite journal |title=Gellan gum as a substitute for agar in leptospiral media |author=Rule PL, Alexander AD |journal=J Clin Microbiol |issue=3 |pages=500–504 |year=1986 |pmid=3754265 |volume=23 |pmc=268682}}</ref> The median time to positivity is three weeks with a maximum of three months. This makes culture techniques useless for diagnostic purposes, but is commonly used in research. |
|||
Rapid detection of ''Leptospira'' can be done by quantifying the IgM antibodies using an [[ELISA|enzyme-linked immunosorbent assay (ELISA)]]. Typically, ''L. biflexa'' antigen is used to detect the IgM antibodies. This test can quickly determine the diagnosis and help in early treatment. However, the test specificity depends upon the type of antigen used and the presence of antibodies from previous infections. The presence of other diseases such as [[Epstein–Barr virus]] infection, viral [[hepatitis]], and [[cytomegalovirus]] infection can cause false-positive results.<ref name="Haake 2015"/> Other rapid screening tests have been developed such as dipsticks, [[Latex fixation test|latex]] and slide agglutination tests.<ref name="Lane 2016"/> |
|||
The microscopic agglutination test (MAT) is the reference test for the diagnosis of leptospirosis.<ref name="Haake 2015"/> MAT is a test where serial dilutions of patient sera are mixed with different serovars of ''Leptospira''. The mixture is then examined under a [[dark field microscopy|dark field microscope]] to look for [[agglutination (biology)|agglutination]]. The highest dilution where 50% agglutination occurs is the result.<ref name="Haake 2015"/> MAT [[titer|titres]] of 1:100 to 1:800 are diagnostic of leptospirosis.<ref name="Lane 2016"/> A fourfold or greater rise in titre of two sera taken at symptoms' onset and three to 10 days of disease onset confirms the diagnosis. During the acute phase of the disease, MAT is not specific in detecting a serotype of ''Leptospira'' because of cross-reactivity between the serovars.<ref name="Haake 2015"/> In the [[convalescent]] phase, MAT is more specific in detecting the serovar types.<ref name="Haake 2015"/> MAT requires a panel of live antigens and requires laborious work.<ref name="Bennett 2015"/> |
|||
====Molecular tests==== |
|||
Leptospiral DNA can be amplified by using [[polymerase chain reaction]] (PCR) from serum, urine, [[aqueous humour]], CSF, and autopsy specimens.<ref name="Haake 2015"/> It detects the presence of bacteria faster than MAT during the first few days of infection without waiting for the appearance of antibodies.<ref name="Bennett 2015"/> As PCR detects the presence of leptospiral DNA in the blood it is useful even when the bacteria is killed by antibiotics.<ref name="Alison 2016">{{cite journal |last1=Alison |first1=B Lane |last2=Michael |first2=M Dore | name-list-style = vanc |title=Leptospirosis: A clinical review of evidence based diagnosis, treatment and prevention |journal=[[World Journal of Clinical Infectious Diseases]] |date=25 November 2016 |volume=6 |issue=4 |pages=61–66 |doi=10.5495/wjcid.v6.i4.61|doi-access=free }}</ref> |
|||
===Imaging=== |
|||
In those who have lung involvement, a chest X-ray may demonstrate diffuse alveolar opacities.<ref name="Haake 2015"/> |
|||
===Diagnostic criteria=== |
|||
In 1982, the [[World Health Organization]] (WHO) proposed the Faine's criteria for the diagnosis of leptospirosis. It consists of three parts: A (clinical findings), B (epidemiological factors), and C (lab findings and bacteriological data). Since the original Faine's criteria only included culture and MAT in part C, which is difficult and complex to perform, the modified Faine's criteria were proposed in 2004 to include ELISA and slide agglutination tests which are easier to perform. In 2012, modified Faine's criteria (with amendment) was proposed to include [[dyspnea|shortness of breath]] and coughing up blood in the diagnosis. In 2013, India recommended modified Faine's criteria in the diagnosis of leptospirosis.<ref name="Kumar India">{{cite book | vauthors = Kumar SS |title=Indian Guidelines for the Diagnosis and Management of Human Leptospirosis |date=2013 |location=India |pages=23–29 |chapter-url=http://www.apiindia.org/medicine_update_2013/chap07.pdf |access-date=16 November 2019 |archive-url=https://web.archive.org/web/20161225181953/http://www.apiindia.org/medicine_update_2013/chap07.pdf |archive-date=25 December 2016 |chapter=7}}</ref> |
|||
==Prevention== |
==Prevention== |
||
[[File:A Leptospirosis warning notice board.jpg|thumb|alt=A sign warning against swimming in a lake with pathogenic Leptospira in Sarawak, Malaysia. | A notice board by a lakeside in [[Sarawak]], Malaysia, that warns against swimming in the lake as it has tested positive for pathogenic ''Leptospira''<ref name="Chieng 2022"/>]] |
|||
[[Doxycycline]] may be used as a [[prophylaxis]] once a week, to prevent infection in high risk areas.<ref name=Pavli2008>{{Cite journal|author=Pavli A, Maltezou HC |title=Travel-acquired leptospirosis |journal=J Travel Med |volume=15 |issue=6 |pages=447–53 |year=2008 |pmid=19090801 |doi=10.1111/j.1708-8305.2008.00257.x |url=}}</ref> Effective rat control and avoidance of urine contaminated water sources are essential preventive measures.Human [[vaccine]]s are available in a few countries, including Cuba and China.<ref name=McB2005/> Currently, no human vaccine is available in the US. Animal vaccines only cover a few strains of the bacteria. Dog vaccines are effective for at least one year.<ref name="pmid20933138">{{cite journal |author=Goldstein RE |title=Canine leptospirosis |journal=The Veterinary Clinics of North America. Small Animal Practice|volume=40 |issue=6 |pages=1091–101 |date=November 2010 |pmid=20933138|doi=10.1016/j.cvsm.2010.07.008 |url=http://linkinghub.elsevier.com/retrieve/pii/S0195-5616(10)00095-1}}</ref> |
|||
[[File:Leptospirosis screening in Indonesia.png|thumb|alt=Blood samples being taken from several men| Blood samples being taken from a group of residents in [[Boyolali Regency]], Indonesia, for leptospirosis screening tests<ref name="Chieng 2022"/>]] |
|||
Rates of leptospirosis can be reduced by improving housing, infrastructure, and sanitation standards. Rodent abatement efforts and flood mitigation projects can also help to prevent it.<ref name="Haake 2015"/> Proper use of [[personal protective equipment]] (PPE) by people who have a high risk of occupational exposure can prevent leptospirosis infections in most cases.<ref name="Haake 2015"/> |
|||
There is no human vaccine suitable for worldwide use.<ref name="Teixeira2019">{{cite journal |
|||
|author=Teixeira AF |
|||
|author2=Fernandes LG |
|||
|author3=Cavenague MF |display-authors=et al |
|||
|title=Adjuvanted leptospiral vaccines: Challenges and future development of new leptospirosis vaccines |
|||
|journal=Vaccine |
|||
|date=2019 |
|||
|volume=37 |
|||
|issue=30 |
|||
|pages=3961–73 |
|||
|doi=10.1016/j.vaccine.2019.05.087 |
|||
|pmid=31186193 |
|||
|s2cid=186204949 |
|||
}}</ref> Only a few countries such as Cuba, Japan, France, and China have approved the use of inactivated vaccines with limited protective effects.<ref name="Teixeira2019"/><ref name="YingHua2018">{{cite journal |
|||
|author=Xu Y |
|||
|author2= Ye Q |
|||
|title=Human leptospirosis vaccines in China |
|||
|journal=Human Vaccines & Immunotherapeutics |
|||
|date=2018 |
|||
|volume=14 |
|||
|issue=4 |
|||
|pages=984–93 |
|||
|doi=10.1080/21645515.2017.1405884 |
|||
|pmid=29148958 |
|||
|pmc=5893195 |
|||
}}</ref> Side effects such as nausea, [[w:erythema|injection site redness]] and swelling have been reported after the vaccine was injected. Since the immunity induced by one ''Leptospira''serovar is only protective against that specific one, [[w:trivalent|trivalent]] vaccines have been developed.<ref name="Haake 2015"/> However, they do not confer long-lasting immunity to humans or animals.<ref name=Picardeau2017/> Vaccines for other animals are more widely available.<ref name="Ellis2015"/> |
|||
[[Doxycycline]] is given once a week as a [[prophylaxis]] and is effective in reducing the rate of leptospirosis infections amongst high-risk individuals in flood-prone areas.<ref>{{cite journal | vauthors = Abd Rahim MA, Zaki AM, Atil A, Azme MH, Him NA, Rahim SS, Jeffree MS, Ahmad N, Hassan MR |title=Effectiveness of Antibiotic Prophylaxis for Leptospirosis among Adults: A Systematic Review |journal=Malaysian Journal of Applied Sciences |volume=3 |issue=2 |pages=46–56 |url= https://journal.unisza.edu.my/myjas/index.php/myjas/article/view/144 |access-date=1 March 2020 }}</ref> In one study, it reduced the number of leptospirosis cases in military personnel undergoing exercises in the jungles. In another study, it reduced the number of symptomatic cases after exposure to leptospirosis under heavy rainfall in [[Endemic (epidemiology)|endemic]] areas.<ref name="Haake 2015"/> |
|||
The prevention of leptospirosis from the environmental sources like contaminated waterways, soil, sewers, and agricultural fields, is disinfection used by [[effective microorganisms]], which is mixed with [[bokashi (horticulture)|bokashi mudballs]] for the infected waterways & sewers. |
|||
==Treatment== |
==Treatment== |
||
Most leptospiral cases resolve spontaneously. Early initiation of antibiotics may prevent the progression to severe disease. Therefore, in resource-limited settings, antibiotics can be started once leptospirosis is suspected after history taking and examination.<ref name="Haake 2015"/> |
|||
Effective [[antibiotics]] include [[penicillin G]], [[ampicillin]], [[amoxicillin]] and Doxycycline. In more severe cases [[cefotaxime]] or [[ceftriaxone]] should be preferred. |
|||
For mild leptospirosis, antibiotic recommendations such as doxycycline, [[azithromycin]], [[ampicillin]] and [[amoxicillin]] were based solely on ''in vitro'' testing.<ref name="Lane 2016"/> In 2001, the WHO recommended oral doxycycline (2 mg/kg up to 100 mg every 12 hours) for five to seven days for those with mild leptospirosis. [[Tetracycline]], ampicillin, and amoxicillin can also be used in such cases.<ref name="WHO"/> However, in areas where both [[rickettsia]] and leptospirosis are endemic, azithromycin and doxycycline are the drugs of choice.<ref name="Lane 2016"/> Doxycycline is not used in cases where the patient suffers from liver damage as it has been linked to hepatotoxicity.<ref>{{Cite book|url=http://www.ncbi.nlm.nih.gov/books/NBK548353/|title=LiverTox: Clinical and Research Information on Drug-Induced Liver Injury|chapter=Doxycycline |date=6 February 2012|publisher=National Institute of Diabetes and Digestive and Kidney Diseases|via=PubMed|pmid=31643675}}</ref> |
|||
Glucose and salt solution infusions may be administered; [[dialysis]] is used in serious cases. Elevations of serum potassium are common and if the potassium level gets too high special measures must be taken. Serum phosphorus levels may likewise increase to unacceptable levels due to renal failure. |
|||
Based on a 1988 study, [[intravenous]] (IV) [[benzylpenicillin]] (also known as penicillin G) is recommended for the treatment of severe leptospirosis.<ref name="Lane 2016"/> Intravenous benzylpenicillin (30 mg/kg up to 1.2 g every six hours) is used for five to seven days. Amoxicillin, ampicillin, and erythromycin may also be used for severe cases.<ref name="WHO">{{cite book |title=WHO recommended strategies for the prevention and control of communicable diseases |date=2001 |publisher=World Health Organization |hdl=10665/67088 |hdl-access=free |page=104 |last1=Organization |first1=World Health }}</ref> [[Ceftriaxone]] (1 g IV every 24 hours for seven days) is also effective for severe leptospirosis.<ref name="Haake 2015"/><ref name="Lane 2016"/><ref>{{cite journal | vauthors = Panaphut T, Domrongkitchaiporn S, Vibhagool A, Thinkamrop B, Susaengrat W | title = Ceftriaxone compared with sodium penicillin g for treatment of severe leptospirosis | journal = Clinical Infectious Diseases | volume = 36 | issue = 12 | pages = 1507–13 | date = June 2003 | pmid = 12802748 | doi = 10.1086/375226 | doi-access = free }}</ref> [[Cefotaxime]] (1 g IV every six hours for seven days) and doxycycline (200 mg initially followed by 100 mg IV every 12 hours for seven days) are equally effective as benzylpenicillin (1.5 million units IV every six hours for seven days).<ref name="Lane 2016"/><ref>{{cite journal | vauthors = Suputtamongkol Y, Niwattayakul K, Suttinont C, Losuwanaluk K, Limpaiboon R, Chierakul W, Wuthiekanun V, Triengrim S, Chenchittikul M, White NJ | display-authors = 6 | title = An open, randomized, controlled trial of penicillin, doxycycline, and cefotaxime for patients with severe leptospirosis | journal = Clinical Infectious Diseases | volume = 39 | issue = 10 | pages = 1417–24 | date = November 2004 | pmid = 15546074 | doi = 10.1086/425001 | doi-access = free }}</ref> Therefore, there is no evidence on differences in death reduction when benzylpenicillin is compared with ceftriaxone or cefotaxime.<ref name="Lane 2016"/> Another study conducted in 2007 also showed no difference in efficacy between doxycycline (200 mg initially followed by 100 mg orally every 12 hours for seven days) or azithromycin (2 g on day one followed by 1 g daily for two more days) for suspected leptospirosis. There was no difference in the resolution of fever and azithromycin is better tolerated than doxycycline.<ref>{{cite journal | vauthors = Phimda K, Hoontrakul S, Suttinont C, Chareonwat S, Losuwanaluk K, Chueasuwanchai S, Chierakul W, Suwancharoen D, Silpasakorn S, Saisongkorh W, Peacock SJ, Day NP, Suputtamongkol Y | display-authors = 6 | title = Doxycycline versus azithromycin for treatment of leptospirosis and scrub typhus | journal = Antimicrobial Agents and Chemotherapy | volume = 51 | issue = 9 | pages = 3259–63 | date = September 2007 | pmid = 17638700 | pmc = 2043199 | doi = 10.1128/AAC.00508-07 }}</ref><ref name=Fret2012/><ref name="Jaykaran 2013"/> |
|||
Treatment for hyperphosphatemia consists of treating the underlying disease, dialysis where appropriate, or oral administration of [[calcium carbonate]], but not without first checking the serum calcium levels (these two levels are related). [[Corticosteroid]]s administration in gradually reduced doses (e.g., [[prednisolone]]) during 7–10 days is recommended by some{{citation needed|date=May 2011}} specialists in cases of severe haemorrhagic effects. Organ specific care and treatment are essential in cases of renal, liver, or heart involvement. |
|||
Outpatients are given doxycycline or azithromycin. Doxycycline can shorten the duration of leptospirosis by two days, improve symptoms, and prevent the shedding of organisms in their urine. Azithromycin and amoxicillin are given to pregnant women and children.<ref name="Haake 2015"/> Rarely, a [[Jarisch–Herxheimer reaction]] can develop in the first few hours after antibiotic administration.<ref name="Lane 2016"/> However, according to a [[meta-analysis]] done in 2012, the benefit of antibiotics in the treatment of leptospirosis was unclear although the use of antibiotics may reduce the duration of illness by two to four days.<ref name="Lane 2016"/><ref name=Fret2012>{{cite journal | vauthors = Brett-Major DM, Coldren R | title = Antibiotics for leptospirosis | journal = The Cochrane Database of Systematic Reviews | issue = 2 | pages = CD008264 | date = February 2012 | pmid = 22336839 | doi = 10.1002/14651858.CD008264.pub2 | s2cid = 44941071 | pmc = 11299142 }}</ref> Another meta-analysis done in 2013 reached a similar conclusion.<ref name="Lane 2016"/><ref name="Jaykaran 2013">{{cite journal | vauthors = Charan J, Saxena D, Mulla S, Yadav P | title = Antibiotics for the treatment of leptospirosis: systematic review and meta-analysis of controlled trials | journal = International Journal of Preventive Medicine | volume = 4 | issue = 5 | pages = 501–10 | date = May 2013 | pmid = 23930159 | pmc = 3733179 }}</ref> |
|||
==Epidemiology== |
|||
It is estimated that seven to ten million peoples are infected by leptospirosis annually.<ref name=NHS2012/> Annual rates of infection vary from 0.02 per 100,000 in temperate climates to 10 to 100 per 100,000 in tropical climates.<ref name=Pavli2008/> This leads to a lower number of registered cases than likely exists. |
|||
For those with severe leptospirosis, including potassium wasting with high kidney output dysfunction, intravenous hydration and potassium supplements can prevent dehydration and [[hypokalemia]]. When [[acute kidney failure]] occurs, early initiation of [[haemodialysis]] or [[peritoneal dialysis]] can help to improve survival. For those with respiratory failure, [[tracheal intubation]] with low [[tidal volume]] improves survival rates.<ref name="Haake 2015"/> |
|||
==History== |
|||
The disease was first described by [[Adolf Weil (physician)|Adolf Weil]] in 1886 when he reported an "acute infectious disease with [[splenomegaly|enlargement of spleen]], [[jaundice]], and [[nephritis]]." ''Leptospira'' was first observed in 1907 from a [[post mortem]] [[kidney|renal tissue]] slice.<ref>{{Cite journal | last1 = Stimson | first1 = AM | year = 1907 | title = Note on an organism found in yellow-fever tissue | journal = Public Health Reports | volume = 22 | page = 541 | doi = 10.2307/4559008 | issue = 18 }}</ref> In 1908, Inada and Ito first identified it as the causative organism<ref>{{cite journal |author=Inada R, Ito Y |title=A report of the discovery of the causal organism (a new species of spirocheta) of Weil's disease |journal=Tokyo Ijishinshi |volume=1915 |pages=351–60 |year=1908 }}</ref> and in 1916 noted its presence in rats.<ref>{{cite journal |author=Inanda R, Ido Y, Hoke R, Kaneko R, Ito H |title=The Etiology, Mode of Infection and Specific Therapy of Weil's Disease |journal=J Exper Med |volume=23 |page=377 |year=1916 |doi=10.1084/jem.23.3.377 |issue=3 }}</ref> |
|||
[[Corticosteroids]] have been proposed to suppress inflammation in leptospirosis because ''Leptospira'' infection can induce the release of [[cytokine|chemical signals]] which promote [[inflammation]] of blood vessels in the lungs. However, there is insufficient evidence to determine whether the use of corticosteroids is beneficial.<ref name="Lane 2016"/><ref>{{cite journal | vauthors = Rodrigo C, Lakshitha de Silva N, Goonaratne R, Samarasekara K, Wijesinghe I, Parththipan B, Rajapakse S | title = High dose corticosteroids in severe leptospirosis: a systematic review | journal = Transactions of the Royal Society of Tropical Medicine and Hygiene | volume = 108 | issue = 12 | pages = 743–50 | date = December 2014 | pmid = 25266477 | doi = 10.1093/trstmh/tru148 }}</ref> |
|||
Leptospirosis was postulated as the cause of an [[List of epidemics|epidemic]] among [[Native Americans in the United States|Native Americans]] along the coast of present-day [[Massachusetts]] that occurred immediately before the arrival of the [[Pilgrim (Plymouth Colony)|Pilgrims]] in 1620 and killed most of the native population.<ref>{{cite journal |author=Marr JS, Cathey JT |title=New hypothesis for cause of an epidemic among Native Americans, New England, 1616–1619 |journal=Emerg Infect Dis |volume=16 |issue=2 |date=February 2010 |doi=10.3201/eid1602.090276 |url=http://www.cdc.gov/EID/content/16/2/281.htm |pages=281–6 |pmid=20113559 |pmc=2957993}}</ref> Earlier proposals included [[plague (disease)|plague]], [[yellow fever]], [[smallpox]], [[influenza]], [[chickenpox]], [[typhus]], [[typhoid fever]], [[trichinellosis]], [[meningitis]], and [[syndemic]] infection of [[hepatitis B virus]] with the [[delta agent]].<ref>{{cite book |author=Webster N |title=A brief history of epidemic and pestilential diseases |publisher=Hudson and Goodwin |location=Hartford CT |year=1799 |url=http://books.google.com/books?id=uen8dansteEC}}</ref><ref>{{cite journal |author=Williams H |title=The epidemic of the Indians of New England, 1616–1620, with remarks on Native American infections |journal=Johns Hopkins Hospital Bulletin |volume=20 |pages=340–9 |year=1909 }}</ref><ref>{{cite journal |author=Bratton TL |title=The identity of the New England Indian epidemic of 1616–19 |journal=Bull Hist Med |volume=62 |issue=3 |pages=351–83 |year=1988 |pmid=3067787 }}</ref><ref>{{cite journal |author=Speiss A, Speiss BD |title=New England pandemic of 1616–1622. cause and archeological implication |journal=Man in the Northeast |volume=34 |pages=71–83 |year=1987 }}</ref> The disease may have been brought to the [[New World]] by Europeans and spread by the high-risk daily activities of the Native Americans{{citation needed|date=June 2014}}. |
|||
==Prognosis== |
|||
Before Weil's characterization in 1886, the disease known as infectious jaundice was very likely the same as Weil's disease, or severe icteric leptospirosis. During the Egyptian campaign, Napoleon's army suffered from what was probably infectious jaundice.<ref>{{cite book |author1=Edward Rhodes Stitt |author2=Richard Pearson Strong |title=Stitt's Diagnosis, prevention and treatment of tropical diseases |url=http://books.google.com/books?id=uqU0AAAAIAAJ |year=1944 |publisher=Blakiston |location=York, PA |edition=7th}}</ref> Infectious jaundice occurred among troops during the [[American Civil War]].<ref>{{cite journal |author=Neill M |title=The problem of acute infectious jaundice in the United States |journal=Public Health Rep |volume=33 |pages=717–26 |year=1918 |doi=10.2307/4574792 |issue=19 }}</ref> |
|||
The overall risk of death for leptospirosis is 5–10%.<ref name="Evangelista2010"/> For those with jaundice, the case fatality can increase up to 15%.<ref name="Spickler 2013"/> For those infected who present with confusion and neurological signs, there is a high risk of death.<ref name="Haake 2015"/> Other factors that increase the risk of death include reduced urine output, age more than 36 years, and respiratory failure.<ref name="Haake 2015"/> With proper care, most of those infected will recover completely. Those with acute kidney failure may develop persistent mild kidney impairment after they recover.<ref name="Haake 2015"/> In those with severe lung involvement, the risk of death is 50–70%.<ref name="Lane 2016"/> Thirty percent of people with acute leptospirosis complained of long-lasting symptoms characterised by weakness, muscle pain, and headaches.<ref name="Haake 2015" /> |
|||
===Eye complications=== |
|||
It was also reported among troops at [[Gallipoli Campaign|Gallipoli]] and other battles of [[World War I]], where the sodden conditions of [[trench warfare]] favored infection. Terms used in early 20th century descriptions of leptospirosis include the pseudo-dengue of Java, seven-day fever, autumn fever, Akiyama disease, and marsh or swamp fever. ''L icterohaemorrhagiae'' was identified as the causative agent in pre-[[World War II]] outbreaks in Japan, which were characterized by jaundice and a high mortality rate. |
|||
Eye problems can occur in 10% of those who recovered from leptospirosis<ref name="Spickler 2013"/> in the range from two weeks to a few years post-infection. Most commonly, eye complications can occur at six months after the infection. This is due to the [[Immune privilege#Eye|immune privilege]] of the eye which protects it from immunological damage during the initial phase of leptospiral infection.<ref name="Verma 2012">{{cite journal |
|||
|author=Verma A |
|||
|author2=Stevenson B |
|||
|title=Leptospiral Uveitis – There Is More to It Than Meets the Eye! |
|||
|journal=Zoonoses and Public Health |
|||
|date=7 September 2012 |
|||
|volume=59 |
|||
| issue=s2 |
|||
| pages=132–41 |
|||
|doi=10.1111/j.1863-2378.2011.01445.x |
|||
|pmid=22958257 |
|||
|s2cid=37444586 |
|||
|doi-access=free |
|||
}}</ref> These complications can range from mild [[anterior uveitis]] to severe panuveitis (which involves all three vascular layers of the eye).<ref name="Spickler 2013"/> The uveitis is more commonly happen in young to middle-aged males and those working in agricultural farming.<ref name="Verma 2012"/> In up to 80% of those infected, ''Leptospira'' DNA can be found in the aqueous humour of the eye.<ref name="Haake 2015"/> Eye problems usually have a good prognosis following treatment or they are self-limiting.<ref name="Spickler 2013"/> In anterior uveitis, only topical steroids and [[mydriasis|mydriatics]] (an agent that causes dilation of the pupil) are needed while in panuveitis, it requires periocular corticosteroids.<ref name="Verma 2012"/> Leptospiral [[uveitis]] is characterised by [[hypopyon]], rapidly maturing [[cataract]], free floating vitreous membranes, disc [[hyperemia]] and retinal [[vasculitis]].<ref name="Verma 2012" /><ref name="Sivakumar 2018">{{cite journal |
|||
|author=Sivakumar R |
|||
|author2=Balakrishnan V |
|||
|author3=Gowri P |
|||
|date=2018 |
|||
|title=Leptospiral Uveitis: Usefulness of Clinical Signs as Diagnostic Predictors |
|||
|journal=Ocular Immunology and Inflammation |
|||
|volume=26 |
|||
|issue=4 |
|||
|pages=569–76 |
|||
|doi=10.1080/09273948.2016.1217341 |
|||
|pmid=27598430 |
|||
|s2cid=21683688 |
|||
}}</ref><ref name="Rathinam 2020">{{cite journal |
|||
|author=Rathinam SR |
|||
|author2=Rathakrishnan S |
|||
|date=September 2020 |
|||
|title=Rapid maturation of unilateral cataract in leptospirosis|journal=Indian Journal of Ophthalmology |
|||
|volume=68 |
|||
|issue=9 |
|||
|pages=1977–79 |
|||
|doi=10.4103/ijo.IJO_535_20 |
|||
|pmid=32823447 |
|||
|pmc=7690476 |
|||
|doi-access=free |
|||
}}</ref> |
|||
==Epidemiology== |
|||
In October 2010 British rower [[Andy Holmes]] died after contracting Weil's Disease.<ref name="NZ_Herald_10683245">{{cite news |url=http://www.nzherald.co.nz/sport/news/article.cfm?c_id=4&objectid=10683245 |title=Rowing: Rare disease kills rowing great |author=Leggat, David |date=27 October 2010 |work=[[The New Zealand Herald]] |accessdate=14 October 2011}}</ref> His death has raised awareness of the disease among the public and medical professionals.<ref name=Forbes2012>{{cite journal |author=Forbes AE, Zochowski WJ, Dubrey SW, Sivaprakasam V |title=Leptospirosis and Weil's disease in the UK |journal=QJM : Monthly Journal of the Association of Physicians |volume= 105|issue= 12|pages= 1151–62|date=July 2012 |pmid=22843698 |doi=10.1093/qjmed/hcs145 |url=}}</ref> |
|||
[[File:Global burden of leptospirosis in DALY per 100,000 per year.png|thumb|upright=1.35|alt=Disability-adjusted life year world map | Global burden of leptospirosis calculated as [[disability-adjusted life year]] (DALY) lost per 100,000 people per year<ref name="Chieng 2022"/>]] |
|||
It is estimated that one million severe cases of leptospirosis occur annually, with 58,900 deaths. Severe cases account for 5–15% of all leptospirosis cases.<ref name=Costa2015/> Leptospirosis is found in both urban and rural areas in [[tropical]], [[subtropical]], and [[temperate]] regions.<ref name="Evangelista2010">{{cite journal | vauthors = Evangelista KV, Coburn J | title = Leptospira as an emerging pathogen: a review of its biology, pathogenesis and host immune responses | journal = Future Microbiology | volume = 5 | issue = 9 | pages = 1413–25 | date = September 2010 | pmid = 20860485 | pmc = 3037011 | doi = 10.2217/fmb.10.102 }}</ref> The global health burden for leptospirosis can be measured by [[disability-adjusted life year]] (DALY). The score is 42 per 100,000 people per year, which is more than other diseases such as [[rabies]] and [[filariasis]].<ref name="Karpagm2020"/> |
|||
The disease is observed persistently in parts of Asia, Oceania, the Caribbean, Latin America and Africa.<ref name="Spickler 2013"/> [[Antarctica]] is the only place not affected by leptospirosis.<ref name="Spickler 2013">{{cite web | vauthors = Spickler AR, Leedom Larson KR |title=Leptospirosis (Fact sheet) |date=October 2013 |access-date=15 March 2019 |publisher=The Center for Food Security and Public Health |url=http://www.cfsph.iastate.edu/Factsheets/pdfs/leptospirosis.pdf |archive-url=https://web.archive.org/web/20141124082710/http://www.cfsph.iastate.edu/Factsheets/pdfs/leptospirosis.pdf |archive-date=24 November 2014 |url-status=live }}</ref> In the United States, there were 100 to 150 leptospirosis cases annually.<ref name="CDC 2017">{{cite web |title=Healthcare Workers – Technical Information for Leptospirosis |url=https://www.cdc.gov/leptospirosis/health_care_workers/index.html |publisher=[[Centers for Disease Control and Prevention]] (CDC) |access-date=28 April 2019 |archive-url=https://web.archive.org/web/20190111230629/https://www.cdc.gov/leptospirosis/health_care_workers/index.html |archive-date=11 January 2019 |date=9 November 2017}}</ref> In 1994, leptospirosis ceased to be a notifiable disease in the United States except in 36 states/territories where it is prevalent such as Hawaii, Texas, California, and Puerto Rico.<ref>{{cite journal | vauthors = Guerra MA | title = Leptospirosis: public health perspectives | journal = Biologicals | volume = 41 | issue = 5 | pages = 295–7 | date = September 2013 | pmid = 23850378 | pmc = 4629849 | doi = 10.1016/j.biologicals.2013.06.010 }}</ref> About 50% of the reported cases occurred in Puerto Rico. In January 2013, leptospirosis was reinstated as a nationally notifiable disease in the United States.<ref name="CDC 2017"/> Research on epidemiology of leptospirosis in high-risk groups and risk factors is limited in India.<ref>{{Cite journal|last1=Moola|first1=Sandeep|last2=Beri|first2=Deepti|last3=Salam|first3=Abdul|last4=Jagnoor|first4=Jagnoor|last5=Teja|first5=Arun|last6=Bhaumik|first6=Soumyadeep|date=July 2021|title=Leptospirosis prevalence and risk factors in India: Evidence gap maps|journal=Tropical Doctor|volume=51|issue=3|pages=415–421|doi=10.1177/00494755211005203|issn=1758-1133|pmid=33832378|s2cid=233191847}}</ref> |
|||
===Names=== |
|||
Leptospirosis has many different names including: "7-day fever",<ref name=Mos2013/> "harvest fever",<ref name=Mos2013/> "field fever",<ref name=Mos2013/> "canefield fever",<ref name=Mos2013/> "mild fever",<ref name=Mos2013/> "rat catcher's yellows",<ref name=Mckay2001/> "Fort Bragg fever",<ref name="Andrews"/> and "pretibial fever".<ref name="Andrews"/> |
|||
The global rates of leptospirosis have been underestimated because most affected countries lack notification or notification is not mandatory.<ref name="Haake 2015"/> Distinguishing clinical signs of leptospirosis from other diseases and lack of laboratory diagnostic services are other problems.<ref name=":0">{{Cite web|url=https://www.who.int/zoonoses/diseases/lerg/en/index2.html|title=WHO {{!}} Leptospirosis Burden Epidemiology Reference Group (LERG)|website=www.who.int|access-date=30 November 2017|archive-url=https://web.archive.org/web/20171117150425/http://www.who.int/zoonoses/diseases/lerg/en/index2.html|archive-date=17 November 2017}}</ref> The socioeconomic status of many of the world's population is closely tied to malnutrition; subsequent lack of [[micronutrients]] may lead to increased risk of infection and death due to leptospirosis infection.<ref name=":1" /> Micronutrients such as [[iron]], [[calcium]], and [[magnesium]] represent important areas for future research.<ref name=":1">{{cite journal | vauthors = Herman HS, Mehta S, Cárdenas WB, Stewart-Ibarra AM, Finkelstein JL | title = Micronutrients and Leptospirosis: A Review of the Current Evidence | journal = PLOS Neglected Tropical Diseases | volume = 10 | issue = 7 | pages = e0004652 | date = July 2016 | pmid = 27387046 | pmc = 4936698 | doi = 10.1371/journal.pntd.0004652 | doi-access = free }}</ref> |
|||
It has historically been known as "black jaundice"<ref>{{cite book|title=Small Water Supplies: A Practical Guide|year=2004|publisher=Routledge|isbn=9781134457496|page=125|url=http://books.google.ca/books?id=N1uBAgAAQBAJ&pg=PA125|author=David Clapham}}</ref> and in Japan it is called "nanukayami fever".<ref name="Elsevier/Saunders">{{cite book|title=Dorland's illustrated medical dictionary|year=2012|publisher=Elsevier/Saunders|location=Philadelphia|isbn=9781455709854|page=1231|url=http://books.google.ca/books?id=mNACisYwbZoC&pg=PA1231|edition=32nd ed.}}</ref> |
|||
==History== |
|||
The disease was first described by [[Adolf Weil (physician)|Adolf Weil]] in 1886 when he reported an "acute infectious disease with enlargement of spleen, jaundice, and [[nephritis]]."<ref name="Weil" /> Before Weil's description, the disease was known as "rice field [[jaundice]]" in ancient Chinese text, "autumn fever", "seven-day fever",<ref name="Ben Adler 2015"/> and "''nanukayami'' fever"<ref name="Elsevier/Saunders">{{cite book|title=Dorland's illustrated medical dictionary|year=2012|publisher=[[Elsevier/Saunders]]|location=Philadelphia|isbn=978-1-4557-0985-4|page=1231|url=https://books.google.com/books?id=mNACisYwbZoC&pg=PA1231|access-date=21 February 2016|archive-url=https://web.archive.org/web/20170908221631/https://books.google.com/books?id=mNACisYwbZoC&pg=PA1231|archive-date=8 September 2017|url-status=live}}</ref> in Japan; in Europe and Australia, the disease was associated with certain occupations and given names such as "cane-cutter's disease", "swine-herd's disease", and "''Schlammfieber''" (mud fever).<ref name="Ben Adler 2015">{{cite book | vauthors = Adler B | title = Leptospira and Leptospirosis | chapter = History of Leptospirosis and Leptospira | series = Current Topics in Microbiology and Immunology | volume = 387 | pages = 1–9 | date = 2015 | pmid = 25388129 | doi = 10.1007/978-3-662-45059-8_1 | isbn = 978-3-662-45058-1 }}</ref> It has been known historically as "black jaundice",<ref>{{cite book|title=Small Water Supplies: A Practical Guide|year=2004|publisher=[[Routledge]]|isbn=978-1-134-45749-6|page=125|url=https://books.google.com/books?id=N1uBAgAAQBAJ&pg=PA125| first = David | last = Clapham | name-list-style = vanc |access-date=21 February 2016|archive-url=https://web.archive.org/web/20170908221631/https://books.google.com/books?id=N1uBAgAAQBAJ&pg=PA125|archive-date=8 September 2017|url-status=live}}</ref> or "dairy farm fever" in New Zealand.<ref>{{cite journal | vauthors = Christmas BW, Tennent RB, Lindsay PG | title = Dairy farm fever in New Zealand: a local outbreak of human leptospirosis | journal = The New Zealand Medical Journal | volume = 79 | issue = 514 | pages = 901–4 | date = May 1974 | pmid = 4527727 }}</ref> Leptospirosis was postulated as the cause of an epidemic among [[Native Americans in the United States|Native Americans]] along the coast of what is now [[New England]] during 1616–1619. The disease was most likely brought to the [[New World]] by Europeans.<ref>{{cite journal | vauthors = Marr JS, Cathey JT | title = New hypothesis for cause of epidemic among native Americans, New England, 1616-1619 | journal = [[Emerging Infectious Diseases (journal)|Emerging Infectious Diseases]] | volume = 16 | issue = 2 | pages = 281–6 | date = February 2010 | pmid = 20113559 | pmc = 2957993 | doi = 10.3201/eid1602.090276 }}</ref> |
|||
''Leptospira'' was first observed in 1907 in a [[post mortem]] kidney tissue slice by Arthur Stimson using [[Silver staining|silver deposition staining]] technique. He called the organism ''Spirocheta interrogans'' because the bacteria resembled a question mark.<ref name="Ben Adler 2015"/><ref>{{Cite journal | vauthors = Stimson AM | year = 1907 | title = Note on an organism found in yellow-fever tissue | journal = [[Public Health Reports]] | volume = 22 | page = 541 | url = https://babel.hathitrust.org/cgi/pt?id=umn.31951002763205f;view=1up;seq=551| doi = 10.2307/4559008 | issue = 18 | jstor = 4559008 }}</ref> In 1908, a Japanese research group led by [[Ryukichi Inada]] and Yutaka Ito first identified this bacterium as the causative agent of leptospirosis<ref>{{cite journal |vauthors=Inada R, Ito Y |title=A report of the discovery of the causal organism (a new species of spirocheta) of Weil's disease |journal=Tokyo Ijishinshi |volume=1915 |pages=351–60 |year=1908 }}</ref> and noted its presence in rats in 1916.<ref>{{cite journal | vauthors = Inada R, Ido Y, Hoki R, Kaneko R, Ito H | title = The Etiology, Mode of Infection, and Specific Therapy of Weil's Disease (Spirochætosis Icterohæmorrhagica) | journal = The Journal of Experimental Medicine | volume = 23 | issue = 3 | pages = 377–402 | date = March 1916 | pmid = 19867994 | pmc = 2125418 | doi = 10.1084/jem.23.3.377 }}</ref> Japanese coal mine workers frequently contracted leptospirosis. In Japan, the organism was named ''Spirocheta icterohaemorrhagiae''. The Japanese group also experimented with the first leptospiral immunisation studies in guinea pigs. They demonstrated that by injecting the infected [[guinea pig]]s with sera from convalescent humans or goats, [[passive immunity]] could be provided to the guinea pigs. In 1917, the Japanese group discovered rats as the carriers of leptospirosis.<ref name="Ben Adler 2015"/> Unaware of the Japanese group's work, two German groups independently and almost simultaneously published their first demonstration of transmitting leptospiral infection in guinea pigs in October 1915. They named the organism ''Spirochaeta nodosa'' and ''Spirochaeta Icterogenes'' respectively.<ref name="Ben Adler 2015"/> |
|||
Leptospirosis was subsequently recognised as a disease of all mammalian species. In 1933, Dutch workers reported the isolation of ''Leptospira canicola'' which specifically infects dogs. In 1940, the strain that specifically infects cattle was first reported in Russia.<ref name="Ben Adler 2015"/> In 1942, soldiers at [[Fort Bragg]], [[North Carolina]], were recorded to have an infectious disease which caused a rash over their [[shinbone]]s. This disease was later known to be caused by leptospirosis.<ref name="Haake 2015"/> By the 1950s, the number of serovars that infected various mammals had expanded significantly. In the 1980s, leptospirosis was recognised as a veterinary disease of major economic importance.<ref name="Ben Adler 2015"/> |
|||
In 1982, there were about 200 serovars of ''Leptospira'' available for classification. The [[International Committee on Systematic Bacteriology]]'s subcommittee on taxonomy of ''Leptospira'' proposed classifying these serovars into two big groups: ''L. interrogans'' containing pathogenic serovars and ''L. biflexa'' containing saprophytic serovars.<ref name="Ben Adler 2015"/> In 1979, the leptospiral family of ''Leptospiraceae'' was proposed. In the same year, ''Leptospira illini'' was reclassified as the new genus ''Leptonema''.<ref name="Ben Adler 2015"/> In 2002, "Lepthangamushi syndrome" was coined to describe a series of overlapping symptoms of leptospirosis with [[Hantavirus hemorrhagic fever with renal syndrome]], and [[scrub typhus]] caused by ''[[Orientia tsutsugamushi]]''.<ref>{{cite journal | vauthors = Paniz-Mondolfi AE, Rodriguez-Morales AJ, Blohm G, Marquez M, Villamil-Gomez WE | title = ChikDenMaZika Syndrome: the challenge of diagnosing arboviral infections in the midst of concurrent epidemics | journal = Annals of Clinical Microbiology and Antimicrobials | volume = 15 | issue = 1 | pages = 42 | date = July 2016 | pmid = 27449770 | pmc = 4957883 | doi = 10.1186/s12941-016-0157-x | doi-access = free }}</ref><ref>{{cite web |title=284184004: Lepthangamushi syndrome (disorder) |url=http://tx.fhir.org/r3/snomed/32506021000036107/?type=snomed&id=284184004 |access-date=18 November 2019 |archive-url=https://web.archive.org/web/20191118153525/http://tx.fhir.org/r3/snomed/32506021000036107/?type=snomed&id=284184004 |archive-date=18 November 2019}}</ref> In 2005, ''Leptospira parva'' was classified as ''Turneriella''.<ref name="Ben Adler 2015"/> With [[DNA-DNA hybridisation]] technology, ''L. interrogans'' was divided into seven species. More ''Leptospira'' species have been discovered since then.<ref name="Ben Adler 2015"/> The WHO established the Leptospirosis Burden Epidemiology Reference Group (LERG) to review the latest disease epidemiological data of leptospirosis, formulate a disease transmission model, and identify gaps in knowledge and research. The first meeting was convened in 2009. In 2011, LERG estimated that the global yearly rate of leptospirosis is five to 14 cases per 100,000 population.<ref name="Haake 2015"/> |
|||
==Other animals== |
==Other animals== |
||
[[File:Liver of an unknown animal infected with leptospirosis.png|thumb|upright=1.35|alt=Unknown animal liver showing blackish necrotic patches from leptospirosis infection | Liver of an unknown animal with multiple blackish [[necrosis|necrotic patches]] secondary to leptospirosis infection<ref name="Chieng 2022"/>]] |
|||
In dogs when leptospirosis is caused by ''L. interrogans'' it may be referred to as "canicola fever".<ref name="Elsevier/Saunders"/> Leptospirosis should be strongly suspected and included as part of a [[differential diagnosis]] if the sclerae of a dog's eyes appear [[jaundice]]d (even slightly yellow). The absence of jaundice does not eliminate the possibility of leptospirosis, and its presence could indicate [[hepatitis]] or other liver pathology rather than leptospirosis. Vomiting, fever, failure to eat, reduced urine output, unusually dark or brown urine, and [[lethargy]] are also indications of the disease. |
|||
[[File:Mediastinum and two lungs of a diseased canine infected with leptospirosis.png|thumb|upright=1.35|alt=Canine lungs with multiple bleeding spots due to leptospirosis | Lungs of a canine with multiple bleeding spots due to leptospirosis<ref name="Chieng 2022"/>]] |
|||
Infected animals can have no, mild, or severe symptoms;<ref name="Center2013"/> the presenting symptoms may vary by the type of animal.<ref name="Ellis2015" /><ref name="Center2013" /> In some animals the bacteria live in the reproductive tract, leading to transmission during mating.<ref name="Ellis2015" /> |
|||
Animals also present with similar clinical features when compared to humans. Clinical signs can appear in 5–15 days in dogs. The incubation period can be prolonged in cats. Leptospirosis can cause abortions after 2–12 weeks in cattle, and 1–4 weeks of infection in pigs. The illness tends to be milder in reservoir hosts. The most commonly affected organs are the kidneys, liver, and reproductive system, but other organs can be affected.<ref name="Spickler 2013"/> In dogs, the acute clinical signs include fever, [[loss of appetite]], shivering, muscle pain, weakness, and urinary symptoms. Vomiting, diarrhea, and abdominal pain may also present. Petechiae and ecchymoses may be seen on mucous membranes. Bleeding from the lungs may also be seen in dogs. In chronic presentations, the affected dog may have no symptoms. In animals that have died of leptospirosis, their kidneys may be swollen with grey and white spots, [[mottle|mottling]], or scarring. Their liver may be enlarged with areas of [[necrosis|cell death]]. Petechiae and ecchymoses may be found in various organs.<ref name="Spickler 2013"/><ref name=Klopfleisch11>{{cite journal | vauthors = Klopfleisch R, Kohn B, Plog S, Weingart C, Nöckler K, Mayer-Scholl A, Gruber AD | title = An emerging pulmonary haemorrhagic syndrome in dogs: similar to the human leptospiral pulmonary haemorrhagic syndrome? | journal = Veterinary Medicine International | volume = 2010 | pages = 928541 | date = December 2010 | pmid = 21274452 | pmc = 3025382 | doi = 10.4061/2010/928541 | doi-access = free }}</ref> [[Vasculitis|Inflammation of the blood vessels]], inflammation of the heart, meningeal layers covering the brain and spinal cord, and [[uveitis]] are also possible.<ref name="Ellis2015"/> [[Equine recurrent uveitis]] (ERU) is the most common disease associated with ''Leptospira'' infection in horses in North America and may lead to blindness.<ref name="Zuerner2015">{{cite book |vauthors=Zuerner RL |title=Leptospira and Leptospirosis |chapter=Host Response to Leptospira Infection |series=Current Topics in Microbiology and Immunology |volume=387 |pages=223–50 |date=2015 |pmid=25388137 |doi=10.1007/978-3-662-45059-8_9 |isbn=978-3-662-45058-1 }}</ref><ref name="Divers2019">{{cite journal |vauthors=Divers TJ, Chang YF, Irby NL, Smith JL, Carter CN |title=Leptospirosis: An important infectious disease in North American horses |journal=Equine Veterinary Journal |volume=51 |issue=3 |pages=287–292 |date=May 2019 |pmid=30629756 |doi=10.1111/evj.13069 |s2cid=58578433 }}</ref> ERU is an autoimmune disease involving antibodies against ''Leptospira'' proteins LruA and LruB cross-reacting with eye proteins.<ref name="Zuerner2015"/> Live ''Leptospira'' can be recovered from the aqueous or vitreous fluid of many horses with ''Leptospira''-associated ERU.<ref name="Divers2019"/> Risk of death or disability in infected animals varies depending upon the species and age of the animals. In adult pigs and cattle, reproductive signs are the most common signs of leptospirosis. Up to 40% of cows may have a spontaneous abortion. Younger animals usually develop more severe disease. About 80% of dogs can survive with treatment, but the survival rate is reduced if the lungs are involved.<ref name="Spickler 2013"/> |
|||
In dogs, penicillin is most commonly used to end the leptospiremic phase (infection of the blood), and doxycycline is used to eliminate the [[asymptomatic carrier|carrier]] state. |
|||
ELISA and microscopic agglutination tests are most commonly used to diagnose leptospirosis in animals. The bacteria can be detected in blood, urine, and milk or liver, kidney, or other tissue samples by using [[immunofluorescence]] or [[Immunohistochemistry|immunohistochemical]] or polymerase chain reaction techniques. Silver staining or immunogold silver staining is used to detect ''Leptospira'' in tissue sections. The organisms stain poorly with [[Gram stain]]. Dark-field microscopy can be used to detect ''Leptospira'' in body fluids, but it is neither sensitive nor specific in detecting the organism.<!-- <ref name="Spickler 2013"/> --> A positive culture for leptospirosis is definitive, but the availability is limited, and culture results can take 13–26 weeks for a result, limiting its utility.<!-- <ref name="Spickler 2013"/> --> Paired acute and convalescent samples are preferred for serological diagnosis of leptospirosis in animals. A positive serological sample from an aborted fetus is also diagnostic of leptospirosis.<ref name="Spickler 2013"/> |
|||
==References== |
|||
{{Reflist|30em}} |
|||
Various antibiotics such as doxycycline, penicillins, [[dihydrostreptomycin]], and [[streptomycin]] have been used to treat leptospirosis in animals. Fluid therapy, blood transfusion, and respiratory support may be required in severe disease.<!-- <ref name="Spickler 2013"/> --> For horses with ERU, the primary treatment is with anti-inflammatory drugs.<ref name="Spickler 2013"/><ref name="Ellis2015"/> |
|||
==Further reading== |
|||
* {{Cite journal | doi = 10.1016/S1473-3099(03)00830-2 | last1 = Bharti | first1 = A. R. | last2 = Nally | year = 2003 | first2 = JE | last3 = Ricaldi | first3 = JN | last4 = Matthias | first4 = MA | last5 = Diaz | first5 = MM | last6 = Lovett | first6 = MA | last7 = Levett | first7 = PN | last8 = Gilman | first8 = RH | last9 = Willig | first9 = MR | title = Leptospirosis: a zoonotic disease of global importance | journal = Lancet Infect. Dis. | volume = 3 | issue = 12| pages = 757–71 | pmid = 14652202 | last10 = Gotuzzo | first10 = Eduardo | last11 = Vinetz | first11 = Joseph M | author12 = Peru-United States Leptospirosis Consortium }} |
|||
{{Gram-negative non-proteobacterial bacterial diseases}} |
|||
Leptospirosis vaccines are available for animals such as pigs, dogs, cattle, sheep, and goats. Vaccines for cattle usually contain ''Leptospira'' serovar Hardjo and Pomona, for dogs, the vaccines usually contain serovar Icterohaemorrhagiae and Canicola.<!-- <ref name="Spickler 2013"/> --> Vaccines containing multiple serovars do not work for cattle as well as vaccines containing a single serovar, yet the multivalent vaccines continue to be sold.<ref name="Ellis2015"/> Isolation of infected animals and prophylactic antibiotics are also effective in preventing leptospirosis transmission between animals. Environmental control and sanitation also reduce transmission rates.<ref name="Spickler 2013"/><ref name="Ellis2015"/> |
|||
==External links== |
|||
{{Clear}} |
|||
* [http://www.cdc.gov/leptospirosis/index.html U.S. Disease Control and Prevention Center page on Leptospirosis] |
|||
*{{cite web |title=''Leptospira'' |work=NCBI Taxonomy Browser |url=http://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi?mode=Info&id=171 |id=171}} |
|||
== References == |
|||
{{Use dmy dates|date=September 2010}} |
|||
{{Academic peer reviewed|Q100400590|doi-access=free}} |
|||
{{Reflist}} |
|||
== External links == |
|||
* {{cite web |url= https://www.cdc.gov/leptospirosis/index.html |publisher= U.S. Disease Control and Prevention Center |title= Leptospirosis |date= 21 November 2018 }} |
|||
* {{cite web |title=''Leptospira'' |publisher=NCBI Taxonomy Browser |url=https://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi?mode=Info&id=171 |id=171}} |
|||
{{Medical resources |
|||
| meshName = Leptospirosis |
|||
| meshNumber = C01.252.400.511 |
|||
| DiseasesDB = 7403 |
|||
| ICD11 = {{ICD11|1B91}} |
|||
| ICD10 = {{ICD10|A|27| |a|20}} |
|||
| ICD9 = {{ICD9|100}} |
|||
| OMIM = 607948 |
|||
| MedlinePlus = 001376 |
|||
| eMedicineSubj = article |
|||
| eMedicineTopic = 220563 |
|||
| eMedicine_mult = {{eMedicine2|article|96569}} {{eMedicine2|article|788751}} |
|||
}} |
|||
{{Gram-negative non-proteobacterial bacterial diseases}} |
|||
{{Bacterial cutaneous infections}} |
|||
{{Vaccines}} |
|||
{{Authority control}} |
|||
[[Category:Bacterium-related cutaneous conditions]] |
[[Category:Bacterium-related cutaneous conditions]] |
||
[[Category:Bovine diseases]] |
[[Category:Bovine diseases]] |
||
[[Category:Dog diseases]] |
[[Category:Dog diseases]] |
||
[[Category:Horse diseases]] |
|||
[[Category:Mammal diseases]] |
|||
[[Category:Rodent-carried diseases]] |
[[Category:Rodent-carried diseases]] |
||
[[Category:Wikipedia medicine articles ready to translate]] |
|||
[[Category:Wikipedia infectious disease articles ready to translate]] |
|||
[[Category:Sheep and goat diseases]] |
|||
[[Category:Spirochaetes]] |
[[Category:Spirochaetes]] |
||
[[Category:Swine diseases]] |
|||
[[Category:Tropical diseases]] |
|||
[[Category:Zoonoses]] |
[[Category:Zoonoses]] |
||
[[Category:Zoonotic bacterial diseases]] |
[[Category:Zoonotic bacterial diseases]] |
||
[[Category:Vaccine-preventable diseases]] |
|||
Latest revision as of 14:38, 28 December 2024
| Leptospirosis | |
|---|---|
| Other names | Rat fever,[1] field fever,[2] rat catcher's yellows,[3] pretibial fever[4] |
 | |
| Leptospira magnified 200-fold with a dark-field microscope | |
| Specialty | Infectious disease |
| Symptoms | None, headaches, muscle pains, fevers[5] |
| Complications | Bleeding from the lungs, meningitis, kidney failure[5][6] |
| Usual onset | One to two weeks[7] |
| Causes | Leptospira typically spread by rodents[8] |
| Risk factors | Exposure to infected animals, especially their urine, or fresh water or damp soil contaminated with infectious urine[8] |
| Diagnostic method | Testing blood for antibodies against the bacterium or its DNA[5] |
| Differential diagnosis | Malaria, enteric fever, rickettsiosis, dengue[9] |
| Prevention | Personal protective equipment, hygiene measures, doxycycline[7] |
| Treatment | Doxycycline, penicillin, ceftriaxone[8] |
| Prognosis | Risk of death ~7.5%[10] |
| Frequency | One million people per year[7][11] |
| Deaths | 58,900 per year[11] |
Leptospirosis is a blood infection caused by the bacterium Leptospira[8] that can infect humans, dogs, rodents and many other wild and domesticated animals.[8] Signs and symptoms can range from none to mild (headaches, muscle pains, and fevers) to severe (bleeding in the lungs or meningitis).[5] Weil's disease (/ˈvaɪlz/ VILES),[12] the acute, severe form of leptospirosis, causes the infected individual to become jaundiced (skin and eyes become yellow), develop kidney failure, and bleed.[6] Bleeding from the lungs associated with leptospirosis is known as severe pulmonary haemorrhage syndrome.[5]
More than ten genetic types of Leptospira cause disease in humans.[13] Both wild and domestic animals can spread the disease, most commonly rodents.[8] The bacteria are spread to humans through animal urine or feces, or water or soil contaminated with animal urine and feces, coming into contact with the eyes, mouth, nose or breaks in the skin.[8] In developing countries, the disease occurs most commonly in pest control, farmers and low-income people who live in areas with poor sanitation.[5] In developed countries, it occurs during heavy downpours and is a risk to pest controllers, sewage workers[14] and those involved in outdoor activities in warm and wet areas.[5] Diagnosis is typically by testing for antibodies against the bacteria or finding bacterial DNA in the blood.[5]
Efforts to prevent the disease include protective equipment to block contact when working with potentially infected animals, washing after contact, and reducing rodents in areas where people live and work.[7] The antibiotic doxycycline is effective in preventing leptospirosis infection.[7] Human vaccines are of limited usefulness;[15] vaccines for other animals are more widely available.[16] Treatment when infected is with antibiotics such as doxycycline, penicillin, or ceftriaxone.[8] The overall risk of death is 5–10%.[10] However, when the lungs are involved, the risk of death increases to the range of 50–70%.[8]
It is estimated that one million severe cases of leptospirosis in humans occur every year, causing about 58,900 deaths.[11] The disease is most common in tropical areas of the world but may occur anywhere.[7] Outbreaks may arise after heavy rainfall.[7] The disease was first described by physician Adolf Weil in 1886 in Germany.[17][18] Infected animals may have no, mild or severe symptoms.[19] These may vary by the type of animal.[16][19] In some animals Leptospira live in the reproductive tract, leading to transmission during mating.[16]
Signs and symptoms
[edit]

The symptoms of leptospirosis usually appear one to two weeks after infection,[7] but the incubation period can be as long as a month.[21] The illness is biphasic in a majority of symptomatic cases. Symptoms of the first phase (acute or leptospiremic phase) last five to seven days. In the second phase (immune phase), the symptoms resolve as antibodies against the bacteria are produced.[8] Additional symptoms develop in the second phase.[22] The phases of illness may not be distinct, especially in patients with severe illness.[23] 90% of those infected experience mild symptoms while 10% experience severe leptospirosis.[24]
Leptospiral infection in humans causes a range of symptoms, though some infected persons may have none. The disease begins suddenly with fever accompanied by chills, intense headache, severe muscle aches and abdominal pain.[5][21] A headache brought on by leptospirosis causes throbbing pain and is characteristically located at the head's bilateral temporal or frontal regions. The person could also have pain behind the eyes and a sensitivity to light. Muscle pain usually involves the calf muscle and the lower back. The most characteristic feature of leptospirosis is the conjunctival suffusion (conjunctivitis without exudate) which is rarely found in other febrile illnesses. Other characteristic findings on the eye include subconjunctival bleeding and jaundice. A rash is rarely found in leptospirosis. When one is found alternative diagnoses such as dengue fever and chikungunya fever should be considered. Dry cough is observed in 20–57% of people with leptospirosis. Thus, this clinical feature can mislead a doctor to diagnose the disease as a respiratory illness. Additionally, gastrointestinal symptoms such as nausea, vomiting, abdominal pain, and diarrhoea frequently occur. Vomiting and diarrhea may contribute to dehydration. The abdominal pain can be due to acalculous cholecystitis or inflammation of the pancreas.[21] Rarely, the lymph nodes, liver, and spleen may be enlarged and palpable.[8]
There will be a resolution of symptoms for one to three days.[7] The immune phase starts after this and can last from four to 30 days and can be anything from brain to kidney complications.[25] The hallmark of the second phase is inflammation of the membranes covering the brain.[7] Signs and symptoms of meningitis include severe headache and neck stiffness.[7] Kidney involvement is associated with reduced or absent urine output.[7]
The classic form of severe leptospirosis, known as Weil's disease, is characterised by liver damage (causing jaundice), kidney failure, and bleeding, which happens in 5–10% of those infected.[7] Lung and brain damage can also occur. For those with signs of inflammation of membranes covering the brain and the brain itself, altered level of consciousness can happen. A variety of neurological problems such as paralysis of half of the body, complete inflammation of a whole horizontal section of spinal cord, and Guillain-Barré syndrome are the complications. Signs of bleeding such as petechiae, ecchymoses, nose bleeding, blackish stools due to bleeding in the stomach, vomiting blood and bleeding from the lungs can also be found. Prolongation of prothrombin time in coagulation testing is associated with severe bleeding manifestation. However, low platelet count is not associated with severe bleeding.[21] Pulmonary haemorrhage is alveolar haemorrhage (bleeding into the alveoli of the lungs) leading to massive coughing up of blood, and causing acute respiratory distress syndrome, where the risk of death is more than 50%.[21] Rarely, inflammation of the heart muscles, inflammation of membranes covering the heart, abnormalities in the heart's natural pacemaker and abnormal heart rhythms may occur.[8]
Cause
[edit]Bacteria
[edit]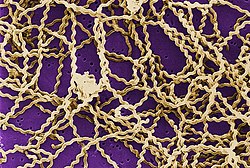
Leptospirosis is caused by spirochaete bacteria that belong to the genus Leptospira, which are aerobic,[8] right-handed helical,[13] and 6–20 micrometers long.[7] Like Gram-negative bacteria, Leptospira have an outer membrane studded with lipopolysaccharide (LPS) on the surface, an inner membrane and a layer of peptidoglycan cell wall. However, unlike Gram-negative bacteria, the peptidoglycan layer in Leptospira lies closer to the inner than the outer membrane. This results in a fluid outer membrane loosely associated with the cell wall.[26] In addition, Leptospira have a flagellum located in the periplasm, associated with corkscrew style movement.[7] Chemoreceptors at the poles of the bacteria sense various substrates and change the direction of its movement.[13] The bacteria are traditionally visualised using dark-field microscopy without staining.[7]
A total of 66 species of Leptospira has been identified. Based on their genomic sequence, they are divided into two clades and four subclades: P1, P2, S1, and S2.[27] The 19 members of the P1 subclade include the 8 species that can cause severe disease in humans: L. alexanderi, L. borgpetersenii, L. interrogans, L. kirschneri, L. mayottensis, L. noguchii, L. santarosai, and L. weilii.[13][27] The P2 clade comprises 21 species that may cause mild disease in humans. The remaining 26 species comprise the S1 and S2 subclades, which include "saprophytes" known to consume decaying matter (saprotrophic nutrition).[27] Pathogenic Leptospira do not multiply in the environment. Leptospira require high humidity for survival but can remain alive in environments such as stagnant water or contaminated soil. The bacterium can be killed by temperatures of 50 °C (122 °F) and can be inactivated by 70% ethanol, 1% sodium hypochlorite, formaldehyde, detergents and acids.[28]
Leptospira are also classified based on their serovar. The diverse sugar composition of the lipopolysaccharide on the surface of the bacteria is responsible for the antigenic difference between serovars.[13] About 300 pathogenic serovars of Leptospira are recognised. Antigenically related serovars (belonging to the same serogroup) may belong to different species because of horizontal gene transfer of LPS biosynthetic genes between different species. Currently, the cross agglutination absorption test and DNA-DNA hybridisation are used to classify Leptospira species, but are time-consuming. Therefore, total genomic sequencing could potentially replace these two methods as the new gold standard of classifying Leptospira species.[13]
Transmission
[edit]
The bacteria can be found in ponds, rivers, puddles, sewers, agricultural fields and moist soil.[7] Pathogenic Leptospira have been found in the form of aquatic biofilms, which may aid survival in the environment.[29]
The number of cases of leptospirosis is directly related to the amount of rainfall, making the disease seasonal in temperate climates and year-round in tropical climates.[7] The risk of contracting leptospirosis depends upon the risk of disease carriage in the community and the frequency of exposure.[21] In rural areas, farming and animal husbandry are the major risk factors for contracting leptospirosis.[5] Poor housing and inadequate sanitation also increase the risk of infection.[21] In tropical and semi-tropical areas, the disease often becomes widespread after heavy rains or after flooding.[7]
Leptospira are found mostly in mammals.[5] However, reptiles and cold-blooded animals such as frogs, snakes, turtles, and toads have been shown to have the infection.[16] Whether there are reservoirs of human infection is unknown.[21][16] Rats, mice, and moles are important primary hosts, but other mammals including dogs, deer, rabbits, hedgehogs, cows, sheep, swine, raccoons, opossums, and skunks can also carry the disease.[16] In Africa, a number of wildlife hosts have been identified as carriers, including the banded mongoose, Egyptian fox, Rusa deer, and shrews.[30] There are various mechanisms whereby animals can infect each other. Dogs may lick the urine of an infected animal off the grass or soil, or drink from an infected puddle. House-bound domestic dogs have contracted leptospirosis, apparently from licking the urine of infected mice in the house.[31] Leptospirosis can also be transmitted via the semen of infected animals.[16] The duration of bacteria being consistently present in animal urine may persist for years.[16]
Humans are the accidental host of Leptospira.[5] Humans become infected through contact with water or moist soil that contains urine & feces from infected animals.[7] The bacteria enter through cuts, abrasions,[7] ingestion of contaminated food, or contact with mucous membrane of the body (e.g. mouth, nose, and eyes).[32] Occupations at risk of contracting leptospirosis include farmers, fishermen, garbage collectors and sewage workers.[5] The disease is also related to adventure tourism and recreational activities.[5] It is common among water-sports enthusiasts in specific areas, including triathlons, water rafting, canoeing and swimming, as prolonged immersion in water promotes the entry of the bacteria.[5] However, Leptospira are unlikely to penetrate intact skin.[8] The disease is not known to spread between humans, and bacterial dissemination in recovery period is extremely rare in humans.[8] Once humans are infected, bacterial shedding from the kidneys usually persists for up to 60 days.[28]
Rarely, leptospirosis can be transmitted through an organ transplant.[33] Infection through the placenta during pregnancy is also possible.[34][35][36] It can cause miscarriage and infection in infants.[37] Leptospirosis transmission through eating raw meat of wildlife animals have also been reported (e.g. psychiatric patients with allotriophagy).[38]
Pathogenesis
[edit]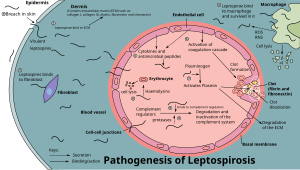
When animals ingest the bacteria, they circulate in the bloodstream, then lodge themselves into the kidneys through the glomerular or peritubular capillaries. The bacteria then pass into the lumens of the renal tubules and colonise the brush border and proximal convoluted tubule. This causes the continuous shedding of bacteria in the urine without the animal experiencing significant ill effects. This relationship between the animal and the bacteria is known as a commensal relationship, and the animal is known as a reservoir host.[21]
Humans are the accidental host of Leptospira.[5] The pathogenesis of leptospirosis remains poorly understood despite research efforts.[7][32] The bacteria enter the human body through either breaches in the skin or the mucous membrane, then into the bloodstream. The bacteria later attach to the endothelial cells of the blood vessels and extracellular matrix (complex network of proteins and carbohydrates present between cells). The bacteria use their flagella for moving between cell layers. They bind to cells such as fibroblasts, macrophages, endothelial cells, and kidney epithelial cells. They also bind to several human proteins such as complement proteins, thrombin, fibrinogen, and plasminogen using surface leptospiral immunoglobulin-like (Lig) proteins such as LigB and LipL32, whose genes are found in all pathogenic species.[13][32]
Through the innate immune system, endothelial cells of the capillaries in the human body are activated by the presence of these bacteria. The endothelial cells produce cytokines and antimicrobial peptides against the bacteria. These products regulate the coagulation cascade and movements of white blood cells.[13] Macrophages presented in humans are able to engulf Leptospira. However, Leptospira are able to reside and proliferate in the cytoplasmic matrix after being ingested by macrophages.[13] Those with severe leptospirosis can experience a high level of cytokines such as interleukin 6, tumor necrosis factor alpha (TNF-α), and interleukin 10. The high level of cytokines causes sepsis-like symptoms which is life-threatening instead of helping to fight against the infection.[24] Those who have a high risk of sepsis during a leptospirosis infection are found to have the HLA-DQ6 genotype, possibly due to superantigen activation, which damages bodily organs.[21]
Leptospira LPS only activates toll-like receptor 2 (TLR2) in monocytes in humans. The lipid A molecule of the bacteria is not recognised by human TLR4 receptors. Therefore, the lack of Leptospira recognition by TLR4 receptors probably contributes to the leptospirosis disease process in humans.[13]
Although there are various mechanisms in the human body to fight against the bacteria, Leptospira is well adapted to such an inflammatory condition created by it. In the bloodstream, it can activate host plasminogen to become plasmin that breaks down extracellular matrix, degrades fibrin clots and complemental proteins (C3b and C5) to avoid opsonisation. It can also recruit complement regulators such as Factor H, C4b-binding protein, factor H-like binding protein, and vitronectin to prevent the activation of membrane attack complex on its surface. It also secretes proteases to degrade complement proteins such as C3. It can bind to thrombin that decreases the fibrin formation. Reduced fibrin formation increases the risk of bleeding.[13] Leptospira also secretes sphingomyelinase and haemolysin that target red blood cells.[7]
Leptospira spreads rapidly to all organs through the bloodstream.[13] They mainly affect the liver. They invade spaces between hepatocytes, causing apoptosis. The damaged hepatocytes and hepatocyte intercellular junctions cause leakage of bile into the bloodstream, causing elevated levels of bilirubin, resulting in jaundice. Congested liver sinusoids and perisinusoidal spaces have been reported. Meanwhile, in the lungs, petechiae or frank bleeding can be found at the alveolar septum and spaces between alveoli.[21] Leptospira secretes toxins that cause mild to severe kidney failure or interstitial nephritis.[32] The kidney failure can recover completely or lead to atrophy and fibrosis.[21] Rarely, inflammation of the heart muscles, coronary arteries, and aorta are found.[25]
Diagnosis
[edit]

Laboratory tests
[edit]For those who are infected, a complete blood count may show a high white cell count and a low platelet count. When a low haemoglobin count is present together with a low white cell count and thrombocytopenia, bone marrow suppression should be considered.[21] Erythrocyte sedimentation rate and C-reactive protein may also be elevated.[8]
The kidneys are commonly involved in leptospirosis. Blood urea and creatinine levels will be elevated. Leptospirosis increases potassium excretion in urine, which leads to a low potassium level[21] and a low sodium level in the blood.[8][21] Urinalysis may reveal the presence of protein, white blood cells, and microscopic haematuria.[8] Because the bacteria settle in the kidneys, urine cultures will be positive for leptospirosis starting after the second week of illness until 30 days of infection.[8]
For those with liver involvement, transaminases and direct bilirubin are elevated in liver function tests. The Icterohaemorrhagiae serogroup is associated with jaundice and elevated bilirubin levels. Hemolytic anemia contributes to jaundice. A feature of leptospirosis is acute haemolytic anaemia and conjugated hyperbilirubinemia, especially in patients with glucose-6-phosphate dehydrogenase deficiency.[21] Abnormal serum amylase and lipase levels (associated with pancreatitis) are found in those who are admitted to hospital due to leptospirosis. Impaired kidney function with creatinine clearance less than 50 ml/min is associated with elevated pancreatic enzymes.[21]
For those with severe headache who show signs of meningitis, a lumbar puncture can be attempted. If infected, cerebrospinal fluid (CSF) examination shows lymphocytic predominance with a cell count of about 500/mm3, protein between 50 and 100 mg/mL and normal glucose levels. These findings are consistent with aseptic meningitis.[21]
Serological tests
[edit]Rapid detection of Leptospira can be done by quantifying the IgM antibodies using an enzyme-linked immunosorbent assay (ELISA). Typically, L. biflexa antigen is used to detect the IgM antibodies. This test can quickly determine the diagnosis and help in early treatment. However, the test specificity depends upon the type of antigen used and the presence of antibodies from previous infections. The presence of other diseases such as Epstein–Barr virus infection, viral hepatitis, and cytomegalovirus infection can cause false-positive results.[21] Other rapid screening tests have been developed such as dipsticks, latex and slide agglutination tests.[8]
The microscopic agglutination test (MAT) is the reference test for the diagnosis of leptospirosis.[21] MAT is a test where serial dilutions of patient sera are mixed with different serovars of Leptospira. The mixture is then examined under a dark field microscope to look for agglutination. The highest dilution where 50% agglutination occurs is the result.[21] MAT titres of 1:100 to 1:800 are diagnostic of leptospirosis.[8] A fourfold or greater rise in titre of two sera taken at symptoms' onset and three to 10 days of disease onset confirms the diagnosis. During the acute phase of the disease, MAT is not specific in detecting a serotype of Leptospira because of cross-reactivity between the serovars.[21] In the convalescent phase, MAT is more specific in detecting the serovar types.[21] MAT requires a panel of live antigens and requires laborious work.[25]
Molecular tests
[edit]Leptospiral DNA can be amplified by using polymerase chain reaction (PCR) from serum, urine, aqueous humour, CSF, and autopsy specimens.[21] It detects the presence of bacteria faster than MAT during the first few days of infection without waiting for the appearance of antibodies.[25] As PCR detects the presence of leptospiral DNA in the blood it is useful even when the bacteria is killed by antibiotics.[39]
Imaging
[edit]In those who have lung involvement, a chest X-ray may demonstrate diffuse alveolar opacities.[21]
Diagnostic criteria
[edit]In 1982, the World Health Organization (WHO) proposed the Faine's criteria for the diagnosis of leptospirosis. It consists of three parts: A (clinical findings), B (epidemiological factors), and C (lab findings and bacteriological data). Since the original Faine's criteria only included culture and MAT in part C, which is difficult and complex to perform, the modified Faine's criteria were proposed in 2004 to include ELISA and slide agglutination tests which are easier to perform. In 2012, modified Faine's criteria (with amendment) was proposed to include shortness of breath and coughing up blood in the diagnosis. In 2013, India recommended modified Faine's criteria in the diagnosis of leptospirosis.[40]
Prevention
[edit]

Rates of leptospirosis can be reduced by improving housing, infrastructure, and sanitation standards. Rodent abatement efforts and flood mitigation projects can also help to prevent it.[21] Proper use of personal protective equipment (PPE) by people who have a high risk of occupational exposure can prevent leptospirosis infections in most cases.[21]
There is no human vaccine suitable for worldwide use.[15] Only a few countries such as Cuba, Japan, France, and China have approved the use of inactivated vaccines with limited protective effects.[15][41] Side effects such as nausea, injection site redness and swelling have been reported after the vaccine was injected. Since the immunity induced by one Leptospiraserovar is only protective against that specific one, trivalent vaccines have been developed.[21] However, they do not confer long-lasting immunity to humans or animals.[13] Vaccines for other animals are more widely available.[16]
Doxycycline is given once a week as a prophylaxis and is effective in reducing the rate of leptospirosis infections amongst high-risk individuals in flood-prone areas.[42] In one study, it reduced the number of leptospirosis cases in military personnel undergoing exercises in the jungles. In another study, it reduced the number of symptomatic cases after exposure to leptospirosis under heavy rainfall in endemic areas.[21]
The prevention of leptospirosis from the environmental sources like contaminated waterways, soil, sewers, and agricultural fields, is disinfection used by effective microorganisms, which is mixed with bokashi mudballs for the infected waterways & sewers.
Treatment
[edit]Most leptospiral cases resolve spontaneously. Early initiation of antibiotics may prevent the progression to severe disease. Therefore, in resource-limited settings, antibiotics can be started once leptospirosis is suspected after history taking and examination.[21]
For mild leptospirosis, antibiotic recommendations such as doxycycline, azithromycin, ampicillin and amoxicillin were based solely on in vitro testing.[8] In 2001, the WHO recommended oral doxycycline (2 mg/kg up to 100 mg every 12 hours) for five to seven days for those with mild leptospirosis. Tetracycline, ampicillin, and amoxicillin can also be used in such cases.[43] However, in areas where both rickettsia and leptospirosis are endemic, azithromycin and doxycycline are the drugs of choice.[8] Doxycycline is not used in cases where the patient suffers from liver damage as it has been linked to hepatotoxicity.[44]
Based on a 1988 study, intravenous (IV) benzylpenicillin (also known as penicillin G) is recommended for the treatment of severe leptospirosis.[8] Intravenous benzylpenicillin (30 mg/kg up to 1.2 g every six hours) is used for five to seven days. Amoxicillin, ampicillin, and erythromycin may also be used for severe cases.[43] Ceftriaxone (1 g IV every 24 hours for seven days) is also effective for severe leptospirosis.[21][8][45] Cefotaxime (1 g IV every six hours for seven days) and doxycycline (200 mg initially followed by 100 mg IV every 12 hours for seven days) are equally effective as benzylpenicillin (1.5 million units IV every six hours for seven days).[8][46] Therefore, there is no evidence on differences in death reduction when benzylpenicillin is compared with ceftriaxone or cefotaxime.[8] Another study conducted in 2007 also showed no difference in efficacy between doxycycline (200 mg initially followed by 100 mg orally every 12 hours for seven days) or azithromycin (2 g on day one followed by 1 g daily for two more days) for suspected leptospirosis. There was no difference in the resolution of fever and azithromycin is better tolerated than doxycycline.[47][48][49]
Outpatients are given doxycycline or azithromycin. Doxycycline can shorten the duration of leptospirosis by two days, improve symptoms, and prevent the shedding of organisms in their urine. Azithromycin and amoxicillin are given to pregnant women and children.[21] Rarely, a Jarisch–Herxheimer reaction can develop in the first few hours after antibiotic administration.[8] However, according to a meta-analysis done in 2012, the benefit of antibiotics in the treatment of leptospirosis was unclear although the use of antibiotics may reduce the duration of illness by two to four days.[8][48] Another meta-analysis done in 2013 reached a similar conclusion.[8][49]
For those with severe leptospirosis, including potassium wasting with high kidney output dysfunction, intravenous hydration and potassium supplements can prevent dehydration and hypokalemia. When acute kidney failure occurs, early initiation of haemodialysis or peritoneal dialysis can help to improve survival. For those with respiratory failure, tracheal intubation with low tidal volume improves survival rates.[21]
Corticosteroids have been proposed to suppress inflammation in leptospirosis because Leptospira infection can induce the release of chemical signals which promote inflammation of blood vessels in the lungs. However, there is insufficient evidence to determine whether the use of corticosteroids is beneficial.[8][50]
Prognosis
[edit]The overall risk of death for leptospirosis is 5–10%.[10] For those with jaundice, the case fatality can increase up to 15%.[28] For those infected who present with confusion and neurological signs, there is a high risk of death.[21] Other factors that increase the risk of death include reduced urine output, age more than 36 years, and respiratory failure.[21] With proper care, most of those infected will recover completely. Those with acute kidney failure may develop persistent mild kidney impairment after they recover.[21] In those with severe lung involvement, the risk of death is 50–70%.[8] Thirty percent of people with acute leptospirosis complained of long-lasting symptoms characterised by weakness, muscle pain, and headaches.[21]
Eye complications
[edit]Eye problems can occur in 10% of those who recovered from leptospirosis[28] in the range from two weeks to a few years post-infection. Most commonly, eye complications can occur at six months after the infection. This is due to the immune privilege of the eye which protects it from immunological damage during the initial phase of leptospiral infection.[51] These complications can range from mild anterior uveitis to severe panuveitis (which involves all three vascular layers of the eye).[28] The uveitis is more commonly happen in young to middle-aged males and those working in agricultural farming.[51] In up to 80% of those infected, Leptospira DNA can be found in the aqueous humour of the eye.[21] Eye problems usually have a good prognosis following treatment or they are self-limiting.[28] In anterior uveitis, only topical steroids and mydriatics (an agent that causes dilation of the pupil) are needed while in panuveitis, it requires periocular corticosteroids.[51] Leptospiral uveitis is characterised by hypopyon, rapidly maturing cataract, free floating vitreous membranes, disc hyperemia and retinal vasculitis.[51][52][53]
Epidemiology
[edit]
It is estimated that one million severe cases of leptospirosis occur annually, with 58,900 deaths. Severe cases account for 5–15% of all leptospirosis cases.[11] Leptospirosis is found in both urban and rural areas in tropical, subtropical, and temperate regions.[10] The global health burden for leptospirosis can be measured by disability-adjusted life year (DALY). The score is 42 per 100,000 people per year, which is more than other diseases such as rabies and filariasis.[7]
The disease is observed persistently in parts of Asia, Oceania, the Caribbean, Latin America and Africa.[28] Antarctica is the only place not affected by leptospirosis.[28] In the United States, there were 100 to 150 leptospirosis cases annually.[54] In 1994, leptospirosis ceased to be a notifiable disease in the United States except in 36 states/territories where it is prevalent such as Hawaii, Texas, California, and Puerto Rico.[55] About 50% of the reported cases occurred in Puerto Rico. In January 2013, leptospirosis was reinstated as a nationally notifiable disease in the United States.[54] Research on epidemiology of leptospirosis in high-risk groups and risk factors is limited in India.[56]
The global rates of leptospirosis have been underestimated because most affected countries lack notification or notification is not mandatory.[21] Distinguishing clinical signs of leptospirosis from other diseases and lack of laboratory diagnostic services are other problems.[57] The socioeconomic status of many of the world's population is closely tied to malnutrition; subsequent lack of micronutrients may lead to increased risk of infection and death due to leptospirosis infection.[58] Micronutrients such as iron, calcium, and magnesium represent important areas for future research.[58]
History
[edit]The disease was first described by Adolf Weil in 1886 when he reported an "acute infectious disease with enlargement of spleen, jaundice, and nephritis."[18] Before Weil's description, the disease was known as "rice field jaundice" in ancient Chinese text, "autumn fever", "seven-day fever",[59] and "nanukayami fever"[60] in Japan; in Europe and Australia, the disease was associated with certain occupations and given names such as "cane-cutter's disease", "swine-herd's disease", and "Schlammfieber" (mud fever).[59] It has been known historically as "black jaundice",[61] or "dairy farm fever" in New Zealand.[62] Leptospirosis was postulated as the cause of an epidemic among Native Americans along the coast of what is now New England during 1616–1619. The disease was most likely brought to the New World by Europeans.[63]
Leptospira was first observed in 1907 in a post mortem kidney tissue slice by Arthur Stimson using silver deposition staining technique. He called the organism Spirocheta interrogans because the bacteria resembled a question mark.[59][64] In 1908, a Japanese research group led by Ryukichi Inada and Yutaka Ito first identified this bacterium as the causative agent of leptospirosis[65] and noted its presence in rats in 1916.[66] Japanese coal mine workers frequently contracted leptospirosis. In Japan, the organism was named Spirocheta icterohaemorrhagiae. The Japanese group also experimented with the first leptospiral immunisation studies in guinea pigs. They demonstrated that by injecting the infected guinea pigs with sera from convalescent humans or goats, passive immunity could be provided to the guinea pigs. In 1917, the Japanese group discovered rats as the carriers of leptospirosis.[59] Unaware of the Japanese group's work, two German groups independently and almost simultaneously published their first demonstration of transmitting leptospiral infection in guinea pigs in October 1915. They named the organism Spirochaeta nodosa and Spirochaeta Icterogenes respectively.[59]
Leptospirosis was subsequently recognised as a disease of all mammalian species. In 1933, Dutch workers reported the isolation of Leptospira canicola which specifically infects dogs. In 1940, the strain that specifically infects cattle was first reported in Russia.[59] In 1942, soldiers at Fort Bragg, North Carolina, were recorded to have an infectious disease which caused a rash over their shinbones. This disease was later known to be caused by leptospirosis.[21] By the 1950s, the number of serovars that infected various mammals had expanded significantly. In the 1980s, leptospirosis was recognised as a veterinary disease of major economic importance.[59]
In 1982, there were about 200 serovars of Leptospira available for classification. The International Committee on Systematic Bacteriology's subcommittee on taxonomy of Leptospira proposed classifying these serovars into two big groups: L. interrogans containing pathogenic serovars and L. biflexa containing saprophytic serovars.[59] In 1979, the leptospiral family of Leptospiraceae was proposed. In the same year, Leptospira illini was reclassified as the new genus Leptonema.[59] In 2002, "Lepthangamushi syndrome" was coined to describe a series of overlapping symptoms of leptospirosis with Hantavirus hemorrhagic fever with renal syndrome, and scrub typhus caused by Orientia tsutsugamushi.[67][68] In 2005, Leptospira parva was classified as Turneriella.[59] With DNA-DNA hybridisation technology, L. interrogans was divided into seven species. More Leptospira species have been discovered since then.[59] The WHO established the Leptospirosis Burden Epidemiology Reference Group (LERG) to review the latest disease epidemiological data of leptospirosis, formulate a disease transmission model, and identify gaps in knowledge and research. The first meeting was convened in 2009. In 2011, LERG estimated that the global yearly rate of leptospirosis is five to 14 cases per 100,000 population.[21]
Other animals
[edit]

Infected animals can have no, mild, or severe symptoms;[19] the presenting symptoms may vary by the type of animal.[16][19] In some animals the bacteria live in the reproductive tract, leading to transmission during mating.[16]
Animals also present with similar clinical features when compared to humans. Clinical signs can appear in 5–15 days in dogs. The incubation period can be prolonged in cats. Leptospirosis can cause abortions after 2–12 weeks in cattle, and 1–4 weeks of infection in pigs. The illness tends to be milder in reservoir hosts. The most commonly affected organs are the kidneys, liver, and reproductive system, but other organs can be affected.[28] In dogs, the acute clinical signs include fever, loss of appetite, shivering, muscle pain, weakness, and urinary symptoms. Vomiting, diarrhea, and abdominal pain may also present. Petechiae and ecchymoses may be seen on mucous membranes. Bleeding from the lungs may also be seen in dogs. In chronic presentations, the affected dog may have no symptoms. In animals that have died of leptospirosis, their kidneys may be swollen with grey and white spots, mottling, or scarring. Their liver may be enlarged with areas of cell death. Petechiae and ecchymoses may be found in various organs.[28][69] Inflammation of the blood vessels, inflammation of the heart, meningeal layers covering the brain and spinal cord, and uveitis are also possible.[16] Equine recurrent uveitis (ERU) is the most common disease associated with Leptospira infection in horses in North America and may lead to blindness.[70][71] ERU is an autoimmune disease involving antibodies against Leptospira proteins LruA and LruB cross-reacting with eye proteins.[70] Live Leptospira can be recovered from the aqueous or vitreous fluid of many horses with Leptospira-associated ERU.[71] Risk of death or disability in infected animals varies depending upon the species and age of the animals. In adult pigs and cattle, reproductive signs are the most common signs of leptospirosis. Up to 40% of cows may have a spontaneous abortion. Younger animals usually develop more severe disease. About 80% of dogs can survive with treatment, but the survival rate is reduced if the lungs are involved.[28]
ELISA and microscopic agglutination tests are most commonly used to diagnose leptospirosis in animals. The bacteria can be detected in blood, urine, and milk or liver, kidney, or other tissue samples by using immunofluorescence or immunohistochemical or polymerase chain reaction techniques. Silver staining or immunogold silver staining is used to detect Leptospira in tissue sections. The organisms stain poorly with Gram stain. Dark-field microscopy can be used to detect Leptospira in body fluids, but it is neither sensitive nor specific in detecting the organism. A positive culture for leptospirosis is definitive, but the availability is limited, and culture results can take 13–26 weeks for a result, limiting its utility. Paired acute and convalescent samples are preferred for serological diagnosis of leptospirosis in animals. A positive serological sample from an aborted fetus is also diagnostic of leptospirosis.[28]
Various antibiotics such as doxycycline, penicillins, dihydrostreptomycin, and streptomycin have been used to treat leptospirosis in animals. Fluid therapy, blood transfusion, and respiratory support may be required in severe disease. For horses with ERU, the primary treatment is with anti-inflammatory drugs.[28][16]
Leptospirosis vaccines are available for animals such as pigs, dogs, cattle, sheep, and goats. Vaccines for cattle usually contain Leptospira serovar Hardjo and Pomona, for dogs, the vaccines usually contain serovar Icterohaemorrhagiae and Canicola. Vaccines containing multiple serovars do not work for cattle as well as vaccines containing a single serovar, yet the multivalent vaccines continue to be sold.[16] Isolation of infected animals and prophylactic antibiotics are also effective in preventing leptospirosis transmission between animals. Environmental control and sanitation also reduce transmission rates.[28][16]
References
[edit]![]() This article was submitted to WikiJournal of Medicine for external academic peer review in 2019 (reviewer reports). The updated content was reintegrated into the Wikipedia page under a CC-BY-SA-3.0 license (2022). The version of record as reviewed is:
Siang Ching Raymond Chieng; et al. (21 June 2022). "Leptospirosis". WikiJournal of Medicine. 9 (1): 2. doi:10.15347/WJM/2022.002. ISSN 2002-4436. Wikidata Q100400590.
This article was submitted to WikiJournal of Medicine for external academic peer review in 2019 (reviewer reports). The updated content was reintegrated into the Wikipedia page under a CC-BY-SA-3.0 license (2022). The version of record as reviewed is:
Siang Ching Raymond Chieng; et al. (21 June 2022). "Leptospirosis". WikiJournal of Medicine. 9 (1): 2. doi:10.15347/WJM/2022.002. ISSN 2002-4436. Wikidata Q100400590.
- ^ Berger S (2018). Leptospirosis: Global Status. GIDEON Informatics Inc. p. 7. ISBN 978-1-4988-2031-8.
- ^ Mosby's Medical Dictionary (9 ed.). Elsevier Health Sciences. 2013. p. 697. ISBN 978-0-323-11258-1. Archived from the original on 8 September 2017. Retrieved 21 February 2016.
- ^ McKay JE (2001). Comprehensive Health Care for Dogs. Minnetonka, MN.: Creative Pub. International. p. 97. ISBN 978-1-55971-783-0.
- ^ James WD, Elston DM, Berger TG, Andrews GC (2006). Andrews' Diseases of the Skin: Clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.: 290
- ^ a b c d e f g h i j k l m n o p Soo ZM, Khan NA, Siddiqui R (January 2020). "Leptospirosis: Increasing importance in developing countries". Acta Tropica. 201: 105183. doi:10.1016/j.actatropica.2019.105183. PMID 31542372.
- ^ a b McBride AJ, Athanazio DA, Reis MG, Ko AI (October 2005). "Leptospirosis". Current Opinion in Infectious Diseases. 18 (5): 376–86. doi:10.1097/01.qco.0000178824.05715.2c. PMID 16148523. S2CID 220576544.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x Karpagam KB, Ganesh B (January 2020). "Leptospirosis: a neglected tropical zoonotic infection of public health importance-an updated review". European Journal of Clinical Microbiology & Infectious Diseases. 39 (5): 835–846. doi:10.1007/s10096-019-03797-4. PMID 31898795. S2CID 209669669.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af Lane AB, Dore MM (2016). "Leptospirosis: A clinical review of evidence based diagnosis, treatment and prevention". World Journal of Clinical Infectious Diseases. 6 (4): 61. doi:10.5495/wjcid.v6.i4.61. ISSN 2220-3176.
- ^ Farrar J, Hotez P, Junghanss T, Kang G, Lalloo D, White NJ (2013). Manson's Tropical Diseases E-Book. Elsevier Health Sciences. p. 438. ISBN 978-0-7020-5306-1. Archived from the original on 8 September 2017. Retrieved 2 September 2017.
- ^ a b c d Evangelista KV, Coburn J (September 2010). "Leptospira as an emerging pathogen: a review of its biology, pathogenesis and host immune responses". Future Microbiology. 5 (9): 1413–25. doi:10.2217/fmb.10.102. PMC 3037011. PMID 20860485.
- ^ a b c d Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, et al. (2015). "Global Morbidity and Mortality of Leptospirosis: A Systematic Review". PLOS Neglected Tropical Diseases. 9 (9): e0003898. doi:10.1371/journal.pntd.0003898. PMC 4574773. PMID 26379143.
- ^ "Rats / RHS Gardening". www.rhs.org.uk.
- ^ a b c d e f g h i j k l m Picardeau M (May 2017). "Virulence of the zoonotic agent of leptospirosis: still terra incognita?". Nature Reviews. Microbiology. 15 (5): 297–307. doi:10.1038/nrmicro.2017.5. PMID 28260786. S2CID 11626842.
- ^ Chan, O. Y.; Chia, S. E.; Nadarajah, N.; Sng, E. H. (16 October 1987). "Leptospirosis Risk in Public Cleansing and Sewer Workers". Annals of the Academy of Medicine, Singapore. 16 (4): 586–90. PMID 3446001.
- ^ a b c Teixeira AF; Fernandes LG; Cavenague MF; et al. (2019). "Adjuvanted leptospiral vaccines: Challenges and future development of new leptospirosis vaccines". Vaccine. 37 (30): 3961–73. doi:10.1016/j.vaccine.2019.05.087. PMID 31186193. S2CID 186204949.
- ^ a b c d e f g h i j k l m n o Ellis WA (2015). "Animal Leptospirosis". Leptospira and Leptospirosis. Current Topics in Microbiology and Immunology. Vol. 387. pp. 99–137. doi:10.1007/978-3-662-45059-8_6. ISBN 978-3-662-45058-1. PMID 25388134.
- ^ Slack A (July 2010). "Leptospirosis". Australian Family Physician. 39 (7): 495–8. PMID 20628664.
- ^ a b Weil A (1886). "Über eine eigenthümliche, mit Milztumor, Icterus und Nephritis einhergehende, acute Infektionskrankheit" [On a strange, acute infectious disease, accompanied by swelling of the spleen, icterus, and nephritis]. Deutsches Archiv für Klinische Medizin (in German). 39: 209–232. OCLC 1040554855.
- ^ a b c d "Leptospirosis" (PDF). The Center for Food Security and Public Health. October 2013. Archived (PDF) from the original on 24 November 2014. Retrieved 8 November 2014.
- ^ a b c d e f g h i j k l Chieng Raymond, Siang Ching (2022). "Leptospirosis". WikiJournal of Medicine. 9 (1). doi:10.15347/WJM/2022.002. S2CID 250435398.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao Haake DA, Levett PN (25 May 2015). "Leptospirosis in Humans". In Adler B (ed.). Leptospira and Leptospirosis. Current Topics in Microbiology and Immunology. Vol. 387. Springer. pp. 65–97. doi:10.1007/978-3-662-45059-8_5. ISBN 978-3-662-45058-1. PMC 4442676. PMID 25388133.
- ^ "Factsheet about leptospirosis". European Centre for Disease Prevention and Control. 16 July 2010. Retrieved 5 September 2020.
- ^ Waggoner JJ, Pinsky BA (October 2016). "Molecular diagnostics for human leptospirosis". Current Opinion in Infectious Diseases. 29 (5): 440–5. doi:10.1097/QCO.0000000000000295. PMC 5127924. PMID 27537829.
- ^ a b Cagliero J, Villanueva SY, Matsui M (20 June 2018). "Leptospirosis Pathophysiology: Into the Storm of Cytokines". Frontiers in Cellular and Infection Microbiology. 8 (204): 204. doi:10.3389/fcimb.2018.00204. PMC 6019470. PMID 29974037.
- ^ a b c d Bennett JE, Raphael D, Martin JB, Bart JC (2015). "223". Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases (Eighth ed.). Elsevier. pp. 2541–2549. ISBN 978-1-4557-4801-3.
- ^ Cameron CE (2015). "Leptospiral Structure, Physiology, and Metabolism". Leptospira and Leptospirosis. Current Topics in Microbiology and Immunology. Vol. 387. pp. 21–41. doi:10.1007/978-3-662-45059-8_3. ISBN 978-3-662-45058-1. PMID 25388131.
- ^ a b c Caimi K, Ruybal P (February 2020). "Leptospira spp., a genus in the stage of diversity and genomic data expansion". Infection, Genetics and Evolution. 81: 104241. Bibcode:2020InfGE..8104241C. doi:10.1016/j.meegid.2020.104241. PMID 32061688. S2CID 211135356.
- ^ a b c d e f g h i j k l m n Spickler AR, Leedom Larson KR (October 2013). "Leptospirosis (Fact sheet)" (PDF). The Center for Food Security and Public Health. Archived (PDF) from the original on 24 November 2014. Retrieved 15 March 2019.
- ^ Barragan V, Olivas S, Keim P, Pearson T (October 2017). "Critical Knowledge Gaps in Our Understanding of Environmental Cycling and Transmission of Leptospira spp". Applied and Environmental Microbiology. 83 (19). Bibcode:2017ApEnM..83E1190B. doi:10.1128/AEM.01190-17. PMC 5601346. PMID 28754706.
- ^ Allan KJ, Biggs HM, Halliday JE, Kazwala RR, Maro VP, Cleaveland S, Crump JA (2015). "Epidemiology of Leptospirosis in Africa: A Systematic Review of a Neglected Zoonosis and a Paradigm for 'One Health' in Africa". PLOS Neglected Tropical Diseases. 9 (9): e0003899. doi:10.1371/journal.pntd.0003899. PMC 4569256. PMID 26368568.
- ^ Rodriguez-Morales AJ, Castañeda-Hernández DM (2014). "Spirochetes: Leptospira". Encyclopedia of Food Safety. 2: 189–193. doi:10.1016/B978-0-12-378612-8.00131-1. ISBN 978-0-12-378613-5.
- ^ a b c d Chin VK, Basir R, Nordin SA, Abdullah M, Sekawi Z (March 2019). "Pathology and Host Immune Evasion During Human Leptospirosis: a Review" (PDF). International Microbiology. 23 (2): 127–136. doi:10.1007/s10123-019-00067-3. PMID 30875033. S2CID 78095369.
- ^ Song AT, Abas L, Andrade LC, Andraus W, D'Albuquerque LA, Abdala E (February 2016). "A first report of leptospirosis after liver transplantation". Transplant Infectious Disease. 18 (1): 137–140. doi:10.1111/tid.12490. PMID 26671230. S2CID 3548455.
- ^ Puliyath G, Singh S (October 2012). "Leptospirosis in pregnancy". European Journal of Clinical Microbiology & Infectious Diseases. 31 (10): 2491–2496. doi:10.1007/s10096-012-1625-7. PMID 22549729. S2CID 14033595.
- ^ Carles G, Montoya E, Joly F, Peneau C (1995). "[Leptospirosis and pregnancy. Eleven cases in French Guyana]". Journal de Gynécologie, Obstétrique et Biologie de la Reproduction. 24 (4): 418–421. PMID 7650320.
- ^ Koe SL, Tan KT, Tan TC (February 2014). "Leptospirosis in pregnancy with pathological fetal cardiotocography changes". Singapore Medical Journal. 55 (2): e20-24. doi:10.11622/smedj.2013194. PMC 4291937. PMID 24712035.
- ^ Shaked Y, Shpilberg O, Samra D, Samra Y (August 1993). "Leptospirosis in pregnancy and its effect on the fetus: case report and review". Clinical Infectious Diseases. 17 (2): 241–243. doi:10.1093/clinids/17.2.241. PMID 8399874.
- ^ Fabiani A, Dal Bo E, Di Bella S, Gabrielli M, Bologna A, Albert U, Sanson G (5 July 2021). "Pica (Allotriophagy): An Underestimated Risk Factor for Severe Leptospirosis (Weil's Diseases)? Report of a Leptospira Septic Shock Successfully Managed with ECMO". Infectious Disease Reports. 13 (3): 619–626. doi:10.3390/idr13030058. ISSN 2036-7449. PMC 8293114. PMID 34287302.
- ^ Alison BL, Michael MD (25 November 2016). "Leptospirosis: A clinical review of evidence based diagnosis, treatment and prevention". World Journal of Clinical Infectious Diseases. 6 (4): 61–66. doi:10.5495/wjcid.v6.i4.61.
- ^ Kumar SS (2013). "7" (PDF). Indian Guidelines for the Diagnosis and Management of Human Leptospirosis. India. pp. 23–29. Archived from the original (PDF) on 25 December 2016. Retrieved 16 November 2019.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Xu Y; Ye Q (2018). "Human leptospirosis vaccines in China". Human Vaccines & Immunotherapeutics. 14 (4): 984–93. doi:10.1080/21645515.2017.1405884. PMC 5893195. PMID 29148958.
- ^ Abd Rahim MA, Zaki AM, Atil A, Azme MH, Him NA, Rahim SS, Jeffree MS, Ahmad N, Hassan MR. "Effectiveness of Antibiotic Prophylaxis for Leptospirosis among Adults: A Systematic Review". Malaysian Journal of Applied Sciences. 3 (2): 46–56. Retrieved 1 March 2020.
- ^ a b Organization, World Health (2001). WHO recommended strategies for the prevention and control of communicable diseases. World Health Organization. p. 104. hdl:10665/67088.
- ^ "Doxycycline". LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. National Institute of Diabetes and Digestive and Kidney Diseases. 6 February 2012. PMID 31643675 – via PubMed.
- ^ Panaphut T, Domrongkitchaiporn S, Vibhagool A, Thinkamrop B, Susaengrat W (June 2003). "Ceftriaxone compared with sodium penicillin g for treatment of severe leptospirosis". Clinical Infectious Diseases. 36 (12): 1507–13. doi:10.1086/375226. PMID 12802748.
- ^ Suputtamongkol Y, Niwattayakul K, Suttinont C, Losuwanaluk K, Limpaiboon R, Chierakul W, et al. (November 2004). "An open, randomized, controlled trial of penicillin, doxycycline, and cefotaxime for patients with severe leptospirosis". Clinical Infectious Diseases. 39 (10): 1417–24. doi:10.1086/425001. PMID 15546074.
- ^ Phimda K, Hoontrakul S, Suttinont C, Chareonwat S, Losuwanaluk K, Chueasuwanchai S, et al. (September 2007). "Doxycycline versus azithromycin for treatment of leptospirosis and scrub typhus". Antimicrobial Agents and Chemotherapy. 51 (9): 3259–63. doi:10.1128/AAC.00508-07. PMC 2043199. PMID 17638700.
- ^ a b Brett-Major DM, Coldren R (February 2012). "Antibiotics for leptospirosis". The Cochrane Database of Systematic Reviews (2): CD008264. doi:10.1002/14651858.CD008264.pub2. PMC 11299142. PMID 22336839. S2CID 44941071.
- ^ a b Charan J, Saxena D, Mulla S, Yadav P (May 2013). "Antibiotics for the treatment of leptospirosis: systematic review and meta-analysis of controlled trials". International Journal of Preventive Medicine. 4 (5): 501–10. PMC 3733179. PMID 23930159.
- ^ Rodrigo C, Lakshitha de Silva N, Goonaratne R, Samarasekara K, Wijesinghe I, Parththipan B, Rajapakse S (December 2014). "High dose corticosteroids in severe leptospirosis: a systematic review". Transactions of the Royal Society of Tropical Medicine and Hygiene. 108 (12): 743–50. doi:10.1093/trstmh/tru148. PMID 25266477.
- ^ a b c d Verma A; Stevenson B (7 September 2012). "Leptospiral Uveitis – There Is More to It Than Meets the Eye!". Zoonoses and Public Health. 59 (s2): 132–41. doi:10.1111/j.1863-2378.2011.01445.x. PMID 22958257. S2CID 37444586.
- ^ Sivakumar R; Balakrishnan V; Gowri P (2018). "Leptospiral Uveitis: Usefulness of Clinical Signs as Diagnostic Predictors". Ocular Immunology and Inflammation. 26 (4): 569–76. doi:10.1080/09273948.2016.1217341. PMID 27598430. S2CID 21683688.
- ^ Rathinam SR; Rathakrishnan S (September 2020). "Rapid maturation of unilateral cataract in leptospirosis". Indian Journal of Ophthalmology. 68 (9): 1977–79. doi:10.4103/ijo.IJO_535_20. PMC 7690476. PMID 32823447.
- ^ a b "Healthcare Workers – Technical Information for Leptospirosis". Centers for Disease Control and Prevention (CDC). 9 November 2017. Archived from the original on 11 January 2019. Retrieved 28 April 2019.
- ^ Guerra MA (September 2013). "Leptospirosis: public health perspectives". Biologicals. 41 (5): 295–7. doi:10.1016/j.biologicals.2013.06.010. PMC 4629849. PMID 23850378.
- ^ Moola, Sandeep; Beri, Deepti; Salam, Abdul; Jagnoor, Jagnoor; Teja, Arun; Bhaumik, Soumyadeep (July 2021). "Leptospirosis prevalence and risk factors in India: Evidence gap maps". Tropical Doctor. 51 (3): 415–421. doi:10.1177/00494755211005203. ISSN 1758-1133. PMID 33832378. S2CID 233191847.
- ^ "WHO | Leptospirosis Burden Epidemiology Reference Group (LERG)". www.who.int. Archived from the original on 17 November 2017. Retrieved 30 November 2017.
- ^ a b Herman HS, Mehta S, Cárdenas WB, Stewart-Ibarra AM, Finkelstein JL (July 2016). "Micronutrients and Leptospirosis: A Review of the Current Evidence". PLOS Neglected Tropical Diseases. 10 (7): e0004652. doi:10.1371/journal.pntd.0004652. PMC 4936698. PMID 27387046.
- ^ a b c d e f g h i j k Adler B (2015). "History of Leptospirosis and Leptospira". Leptospira and Leptospirosis. Current Topics in Microbiology and Immunology. Vol. 387. pp. 1–9. doi:10.1007/978-3-662-45059-8_1. ISBN 978-3-662-45058-1. PMID 25388129.
- ^ Dorland's illustrated medical dictionary. Philadelphia: Elsevier/Saunders. 2012. p. 1231. ISBN 978-1-4557-0985-4. Archived from the original on 8 September 2017. Retrieved 21 February 2016.
- ^ Clapham D (2004). Small Water Supplies: A Practical Guide. Routledge. p. 125. ISBN 978-1-134-45749-6. Archived from the original on 8 September 2017. Retrieved 21 February 2016.
- ^ Christmas BW, Tennent RB, Lindsay PG (May 1974). "Dairy farm fever in New Zealand: a local outbreak of human leptospirosis". The New Zealand Medical Journal. 79 (514): 901–4. PMID 4527727.
- ^ Marr JS, Cathey JT (February 2010). "New hypothesis for cause of epidemic among native Americans, New England, 1616-1619". Emerging Infectious Diseases. 16 (2): 281–6. doi:10.3201/eid1602.090276. PMC 2957993. PMID 20113559.
- ^ Stimson AM (1907). "Note on an organism found in yellow-fever tissue". Public Health Reports. 22 (18): 541. doi:10.2307/4559008. JSTOR 4559008.
- ^ Inada R, Ito Y (1908). "A report of the discovery of the causal organism (a new species of spirocheta) of Weil's disease". Tokyo Ijishinshi. 1915: 351–60.
- ^ Inada R, Ido Y, Hoki R, Kaneko R, Ito H (March 1916). "The Etiology, Mode of Infection, and Specific Therapy of Weil's Disease (Spirochætosis Icterohæmorrhagica)". The Journal of Experimental Medicine. 23 (3): 377–402. doi:10.1084/jem.23.3.377. PMC 2125418. PMID 19867994.
- ^ Paniz-Mondolfi AE, Rodriguez-Morales AJ, Blohm G, Marquez M, Villamil-Gomez WE (July 2016). "ChikDenMaZika Syndrome: the challenge of diagnosing arboviral infections in the midst of concurrent epidemics". Annals of Clinical Microbiology and Antimicrobials. 15 (1): 42. doi:10.1186/s12941-016-0157-x. PMC 4957883. PMID 27449770.
- ^ "284184004: Lepthangamushi syndrome (disorder)". Archived from the original on 18 November 2019. Retrieved 18 November 2019.
- ^ Klopfleisch R, Kohn B, Plog S, Weingart C, Nöckler K, Mayer-Scholl A, Gruber AD (December 2010). "An emerging pulmonary haemorrhagic syndrome in dogs: similar to the human leptospiral pulmonary haemorrhagic syndrome?". Veterinary Medicine International. 2010: 928541. doi:10.4061/2010/928541. PMC 3025382. PMID 21274452.
- ^ a b Zuerner RL (2015). "Host Response to Leptospira Infection". Leptospira and Leptospirosis. Current Topics in Microbiology and Immunology. Vol. 387. pp. 223–50. doi:10.1007/978-3-662-45059-8_9. ISBN 978-3-662-45058-1. PMID 25388137.
- ^ a b Divers TJ, Chang YF, Irby NL, Smith JL, Carter CN (May 2019). "Leptospirosis: An important infectious disease in North American horses". Equine Veterinary Journal. 51 (3): 287–292. doi:10.1111/evj.13069. PMID 30629756. S2CID 58578433.
External links
[edit]- "Leptospirosis". U.S. Disease Control and Prevention Center. 21 November 2018.
- "Leptospira". NCBI Taxonomy Browser. 171.
- Wikipedia articles published in peer-reviewed literature
- Wikipedia articles published in WikiJournal of Medicine
- Externally peer reviewed articles
- Wikipedia articles published in peer-reviewed literature (W2J)
- Bacterium-related cutaneous conditions
- Bovine diseases
- Dog diseases
- Horse diseases
- Mammal diseases
- Rodent-carried diseases
- Sheep and goat diseases
- Spirochaetes
- Swine diseases
- Tropical diseases
- Zoonoses
- Zoonotic bacterial diseases
- Vaccine-preventable diseases
