Delayed sleep phase disorder: Difference between revisions
→Adaptation to late sleeping times: invisible disability |
invisible disability |
||
| Line 13: | Line 13: | ||
The syndrome usually develops in early childhood or adolescence.<ref name=Dagan_1999>{{cite journal |author=Dagan Y, Eisenstein M |title=Circadian rhythm sleep disorders: toward a more precise definition and diagnosis |journal=Chronobiol. Int. |volume=16 |issue=2 |pages=213–22 |year=1999 |pmid=10219492 |doi=10.3109/07420529909019087}}</ref> An adolescent version disappears in adolescence or early adulthood; otherwise DSPS is a lifelong condition. Depending on the severity, it can be to a greater or lesser degree treatable. Prevalence among adults, equally distributed among women and men, is approximately 0.15%, or 3 in 2,000. |
The syndrome usually develops in early childhood or adolescence.<ref name=Dagan_1999>{{cite journal |author=Dagan Y, Eisenstein M |title=Circadian rhythm sleep disorders: toward a more precise definition and diagnosis |journal=Chronobiol. Int. |volume=16 |issue=2 |pages=213–22 |year=1999 |pmid=10219492 |doi=10.3109/07420529909019087}}</ref> An adolescent version disappears in adolescence or early adulthood; otherwise DSPS is a lifelong condition. Depending on the severity, it can be to a greater or lesser degree treatable. Prevalence among adults, equally distributed among women and men, is approximately 0.15%, or 3 in 2,000. |
||
DSPS was first formally described in 1981 by Dr. Elliot D. Weitzman and others at [[Montefiore Medical Center]].<ref name=weitzman_1981>{{cite journal |author=Weitzman ED, Czeisler CA, Coleman RM, et al. |title=Delayed sleep phase syndrome. A chronobiological disorder with sleep-onset insomnia |journal=Arch. Gen. Psychiatry |volume=38 |issue=7 |pages=737–46 |year=1981 |pmid=7247637}}</ref> It is responsible for 7–10% of patient complaints of chronic [[insomnia]].<ref>{{cite web |title=Sleeplessness and Circadian Rhythm Disorder |publisher=eMedicine World Medical Library from WebMD |url=http://www.emedicine.com/neuro/topic655.htm |accessdate=2006-06-04 |quote=Implicit in the diagnosis of circadian rhythm disorder is a desire to conform to traditionally accepted sleep-wake patterns.}}</ref> However, as few doctors are aware of it, it often goes untreated or is treated inappropriately; DSPS is often misdiagnosed as primary [[insomnia]] or as a [[psychiatric]] condition.<ref>{{cite journal |author=Dagan Y |title=Circadian rhythm sleep disorders (CRSD) |journal=Sleep Med Rev |volume=6 |issue=1 |pages=45–54 |year=2002 |pmid=12531141 |doi=10.1053/smrv.2001.0190 |url=http://www.neurosono.com.br/arquivos/1155473343.pdf |format= PDF: full text |accessdate=2007-11-08 |quote=Early onset of CRSD, the ease of diagnosis, the high frequency of misdiagnosis and erroneous treatment, the potentially harmful psychological and adjustment consequences, and the availability of promising treatments, all indicate the importance of greater awareness of these disorders.}}</ref> |
DSPS was first formally described in 1981 by Dr. Elliot D. Weitzman and others at [[Montefiore Medical Center]].<ref name=weitzman_1981>{{cite journal |author=Weitzman ED, Czeisler CA, Coleman RM, et al. |title=Delayed sleep phase syndrome. A chronobiological disorder with sleep-onset insomnia |journal=Arch. Gen. Psychiatry |volume=38 |issue=7 |pages=737–46 |year=1981 |pmid=7247637}}</ref> It is responsible for 7–10% of patient complaints of chronic [[insomnia]].<ref>{{cite web |title=Sleeplessness and Circadian Rhythm Disorder |publisher=eMedicine World Medical Library from WebMD |url=http://www.emedicine.com/neuro/topic655.htm |accessdate=2006-06-04 |quote=Implicit in the diagnosis of circadian rhythm disorder is a desire to conform to traditionally accepted sleep-wake patterns.}}</ref> However, as few doctors are aware of it, it often goes untreated or is treated inappropriately; DSPS is often misdiagnosed as primary [[insomnia]] or as a [[psychiatric]] condition.<ref>{{cite journal |author=Dagan Y |title=Circadian rhythm sleep disorders (CRSD) |journal=Sleep Med Rev |volume=6 |issue=1 |pages=45–54 |year=2002 |pmid=12531141 |doi=10.1053/smrv.2001.0190 |url=http://www.neurosono.com.br/arquivos/1155473343.pdf |format= PDF: full text |accessdate=2007-11-08 |quote=Early onset of CRSD, the ease of diagnosis, the high frequency of misdiagnosis and erroneous treatment, the potentially harmful psychological and adjustment consequences, and the availability of promising treatments, all indicate the importance of greater awareness of these disorders.}}</ref> At its most severe and inflexible, it is an [[invisible disability]]. |
||
==Definition== |
==Definition== |
||
Revision as of 13:52, 9 January 2011
| Delayed sleep phase disorder | |
|---|---|
| Specialty | Neurology |
Delayed sleep-phase syndrome (DSPS), also known as delayed sleep-phase disorder (DSPD) or delayed sleep-phase type (DSPT), is a circadian rhythm sleep disorder, a chronic disorder of the timing of sleep, peak period of alertness, the core body temperature rhythm, hormonal and other daily rhythms, compared to the normal population and relative to societal requirements. People with DSPS generally fall asleep some hours after midnight and have difficulty waking up in the morning.[1]
Often, people with the disorder report that they cannot sleep until early morning, but fall asleep at about the same time every "night". Unless they have another sleep disorder such as sleep apnea in addition to DSPS, patients can sleep well and have a normal need for sleep. Therefore, they find it very difficult to wake up in time for a typical school or work day. If, however, they are allowed to follow their own schedules, e.g. sleeping from 4 a.m. to noon, they sleep soundly, awaken spontaneously, and do not experience excessive daytime sleepiness.
The syndrome usually develops in early childhood or adolescence.[2] An adolescent version disappears in adolescence or early adulthood; otherwise DSPS is a lifelong condition. Depending on the severity, it can be to a greater or lesser degree treatable. Prevalence among adults, equally distributed among women and men, is approximately 0.15%, or 3 in 2,000.
DSPS was first formally described in 1981 by Dr. Elliot D. Weitzman and others at Montefiore Medical Center.[3] It is responsible for 7–10% of patient complaints of chronic insomnia.[4] However, as few doctors are aware of it, it often goes untreated or is treated inappropriately; DSPS is often misdiagnosed as primary insomnia or as a psychiatric condition.[5] At its most severe and inflexible, it is an invisible disability.
Definition
According to the International Classification of Sleep Disorders (ICSD),[6] the circadian rhythm sleep disorders share a common underlying chronophysiologic basis:
The major feature of these disorders is a misalignment between the patient's sleep pattern and the sleep pattern that is desired or regarded as the societal norm... In most circadian rhythm sleep disorders, the underlying problem is that the patient cannot sleep when sleep is desired, needed or expected.
The ICSD (page 128-133) diagnostic criteria for delayed sleep-phase syndrome are:
- There is an intractable delay in the phase of the major sleep period in relation to the desired clock time, as evidenced by a chronic or recurrent complaint of inability to fall asleep at a desired conventional clock time together with the inability to awaken at a desired and socially acceptable time.
- When not required to maintain a strict schedule, patients will exhibit normal sleep quality and duration for their age and maintain a delayed, but stable, phase of entrainment to local time.
- Patients have little or no reported difficulty in maintaining sleep once sleep has begun.
- Patients have a relatively severe to absolute inability to advance the sleep phase to earlier hours by enforcing conventional sleep and wake times.
- Sleep-wake logs and/or actigraphy monitoring for at least two weeks document a consistent habitual pattern of sleep onsets, usually later than 2 a.m., and lengthy sleeps.
- Occasional noncircadian days may occur (i.e., sleep is "skipped" for an entire day and night plus some portion of the following day), followed by a sleep period lasting 12 to 18 hours.
- The symptoms do not meet the criteria for any other sleep disorder causing inability to initiate sleep or excessive sleepiness.
- If any of the following laboratory methods is used, it must demonstrate a delay in the timing of the habitual sleep period: 1) Twenty-four-hour polysomnographic monitoring (or by means of two consecutive nights of polysomnography and an intervening multiple sleep latency test), 2) Continuous temperature monitoring showing that the time of the absolute temperature nadir is delayed into the second half of the habitual (delayed) sleep episode.[6]
Some people with the abnormality adapt their lives to the delayed sleep phase, avoiding common business hours (e.g., 9 a.m. to 5 p.m.) as much as possible. They have the disorder, but for them it is not a disability. The ICSD's severity criteria, all of them "over at least a one-month period", are:
- Mild: Two hour delay associated with little or mild impairment of social or occupational functioning.
- Moderate: Three hour delay associated with moderate impairment.
- Severe: Four hour delay associated with severe impairment.
Some features of DSPS which distinguish it from other sleep disorders are:
- People with DSPS have at least a normal—and often much greater than normal—ability to sleep during the morning, and sometimes in the afternoon as well. In contrast, those with chronic insomnia do not find it much easier to sleep during the morning than at night.
- People with DSPS fall asleep at more or less the same time every night, and sleep comes quite rapidly if the person goes to bed near the time he or she usually falls asleep. Young children with DSPS resist going to bed before they are sleepy, but the bedtime struggles disappear if they are allowed to stay up until the time they usually fall asleep.
- DSPS patients can sleep well and regularly when they can follow their own sleep schedule, e.g. on weekends and during vacations.
- DSPS is a chronic condition. Symptoms must have been present for at least one month before a diagnosis of DSPS can be made.
Attempting to force oneself onto daytime society's schedule with DSPS has been compared to constantly living with 6 hours of jet lag; the disorder has, in fact, been referred to as "social jet lag".[7] Often, sufferers manage only a few hours sleep a night during the working week, then compensate by sleeping until the afternoon on weekends. Sleeping in on weekends, and/or taking long naps during the day, may give people with the disorder relief from daytime sleepiness but may also perpetuate the late sleep phase.
People with DSPS can be called extreme night owls. They feel most alert and say they function best and are most creative in the evening and at night. DSPS patients cannot simply force themselves to sleep early. They may toss and turn for hours in bed, and sometimes not sleep at all, before reporting to work or school. Less extreme and more flexible night owls, and indeed morning larks, are within the normal chronotype spectrum.
By the time DSPS patients seek medical help, they usually have tried many times to change their sleeping schedule. Failed tactics to sleep at earlier times may include maintaining proper sleep hygiene, relaxation techniques, early bedtimes, hypnosis, alcohol, sleeping pills, dull reading, and home remedies. DSPS patients who have tried using sedatives at night often report that the medication makes them feel tired or relaxed, but that it fails to induce sleep. They often have asked family members to help wake them in the morning, or they have used several alarm clocks. As the syndrome occurs in childhood and is most common in adolescence, it is often the patient's parents who initiate seeking help, after great difficulty waking their child in time for school.
The current formal name established in the second edition of the International Classification of Sleep Disorders is circadian rhythm sleep disorder, delayed sleep phase type; the preferred common name is delayed sleep-phase disorder.[8]
Prevalence
About 0.15% of adults, three in 2,000, have DSPS. Using the strict ICSD diagnostic criteria, a random study in 1993 of 7700 adults (aged 18–67) in Norway estimated the prevalence of DSPS at 0.17%.[9] A similar study of 1525 adults (aged 15–59) in Japan estimated its prevalence at 0.13%.[10]

DSPS is not uncommon among teenagers;[11]at least one study has indicated that the prevalence of DSPS among adolescents is as high as 7%. Among adolescents, boys predominate, while the gender distribution shows equal numbers of women and men in adults.[6]
A marked delay of sleep patterns is a normal feature of the development of adolescent humans. According to Mary Carskadon, both circadian phase and homeostasis (the accumulation of sleep pressure during the wake period) contribute to a DSPS-like condition in post-pubertal as compared to pre-pubertal adolescents.[12]
Physiology
DSPS is a disorder of the body's timing system—the biological clock. Individuals with DSPS might have an unusually long circadian cycle, might have a reduced response to the re-setting effect of daylight on the body clock and/or may respond overly to the delaying effects of evening light and too little to the advancing effect of light earlier in the day. In support of the increased sensitivity to evening light hypothesis, "the percentage of melatonin suppression by a bright light stimulus of 1,000 lux administered 2 hours prior to the melatonin peak has been reported to be greater in 15 DSPS patients than in 15 controls."[13]
People with normal circadian systems can generally fall asleep quickly at night if they slept too little the night before. Falling asleep earlier will in turn automatically help to advance their circadian clocks due to decreased light exposure in the evening. In contrast, people with DSPS are unable to fall asleep before their usual sleep time, even if they are sleep-deprived. Sleep deprivation does not reset the circadian clock of DSPS patients, as it does with normal people.[14]
People with the disorder who try to live on a normal schedule have difficulty falling asleep and difficulty waking because their biological clocks are not in phase with that schedule. Normal people who do not adjust well to working a night shift have similar symptoms (diagnosed as shift-work sleep disorder, SWSD).
In most cases, it is not known what causes the abnormality in the biological clocks of DSPS patients. DSPS tends to run in families,[15] and a growing body of evidence suggests that the problem is associated with the hPer3 (human period 3) gene.[16][17] There have been several documented cases of DSPS and non-24-hour sleep-wake syndrome developing after traumatic head injury.[18][19]
There have been a few cases of DSPS developing into non-24-hour sleep-wake syndrome, a more severe and debilitating disorder in which the individual sleeps later each day.[20] It has been suggested that, instead of (or perhaps in addition to) a reduced reaction to light in the morning, an abnormal over-sensitivity to light in the late evening might contribute to the odd non-circadian pattern.[21]
Diagnosis
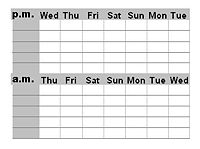
DSPS is diagnosed by a clinical interview, actigraphic monitoring and/or a sleep diary kept by the patient for at least three weeks. When polysomnography is also used, it is primarily for the purpose of ruling out other disorders such as narcolepsy or sleep apnea. If a person can, on her/his own with just the help of alarm clocks and will-power, adjust to a daytime schedule, the diagnosis is not given.
DSPS is frequently misdiagnosed or dismissed. It has been named as one of the sleep disorders most commonly misdiagnosed as a primary psychiatric disorder.[22] DSPS is often confused with: psychophysiological insomnia; depression; psychiatric disorders such as schizophrenia, ADHD or ADD; other sleep disorders; or school refusal. Practitioners of sleep medicine point out the dismally low rate of accurate diagnosis of the disorder, and have often asked for better physician education on sleep disorders.[23]
Management
Treatment, a set of management techniques, is specific to DSPS. It is different from treatment of insomnia, and recognizes the patients' ability to sleep well on their own schedules, while addressing the timing problem. Success, if any, may be partial; for example, a patient who normally awakens at noon may only attain a wake time of 10 or 10:30 with treatment and follow-up. Being consistent with the treatment is paramount.
Before starting DSPS treatment, patients are often asked to spend at least a week sleeping regularly, without napping, at the times when the patient is most comfortable. It is important for patients to start treatment well-rested.
Treatments that have been reported in the medical literature include:
Light therapy (phototherapy) with a full spectrum lamp or portable visor, usually 10,000 lux for 30–90 minutes at the patient's usual time of spontaneous awakening, or shortly before (but not long before), which is in accordance with the phase response curve (PRC) for light. The use of an LED light therapy device can reduce this to 15-30 minutes.[24] Sunlight can also be used. Only experimentation, preferably with specialist help, will show how great an advance is possible and comfortable. For maintenance, some patients must continue the treatment indefinitely, some may reduce the daily treatment to 15 minutes, others may use the lamp, for example, just a few days a week or just every third week. Whether the treatment is successful is highly individual. Light therapy generally requires adding some extra time to the patient's morning routine. Patients with a family history of macular degeneration are advised to consult with an eye doctor. The use of exogenous melatonin administration (see below) in conjunction with light therapy is common.
Dim lights in the evening, sometimes called darkness therapy. Just as bright light upon awakening should advance one's sleep-phase, bright light in the evening and night delays it (see the PRC). One might be advised to keep lights dim the last hours before bedtime and even wear sunglasses or amber-colored goggles. Attaining an earlier sleep onset, in a dark room with eyes closed, effectively blocks a period of phase-delaying light. An understanding of this is a motivating factor in treatment.
Chronotherapy, which is intended to reset the circadian clock by manipulating bedtimes. Often, chronotherapy must be repeated every few months to maintain results, and its safety is uncertain.[25] It can be one of two types. The most common consists of going to bed two or more hours later each day for several days until the desired bedtime is reached. A modified chronotherapy (Thorpy, 1988) is called controlled sleep deprivation with phase advance, SDPA. One stays awake one whole night and day, then goes to bed 90 minutes earlier than usual and maintains the new bedtime for a week. This process is repeated weekly until the desired bedtime is reached.
Melatonin taken an hour or so before usual bedtime may induce sleepiness.

Taken this late, it does not, of itself, affect circadian rhythms,[26] but a decrease in exposure to light in the evening is helpful in establishing an earlier pattern. In accordance with its phase response curve (PRC), a very small dose of melatonin can also, or instead, be taken some hours earlier as an aid to resetting the body clock;[27] it must then be so small as to not induce excessive sleepiness.
Side effects of melatonin may include disturbance of sleep, nightmares, daytime sleepiness and depression, though the current tendency to use lower doses has decreased such complaints. Large doses of melatonin can even be counterproductive: Lewy et al.[28] provide support to the "idea that too much melatonin may spill over onto the wrong zone of the melatonin phase-response curve." The long-term effects of melatonin administration have not been examined. In some countries the hormone is available only by prescription or not at all. In the United States and Canada, melatonin is freely available as a dietary supplement. The prescription drug Rozerem (ramelteon) is a melatonin analogue that selectively binds to the melatonin MT1 and MT2 receptors and, hence, has the possibility of being effective in the treatment of DSPS.
A review by a US government agency found little difference between melatonin and placebo for most primary and secondary sleep disorders. The one exception, where melatonin is effective, is the "circadian abnormality" DSPS.[29]
Cannabis has been suggested as an aid to combat DSPS. However, no research has yet been done that shows cannabis works in DSPS. Sleep onset is affected by the two primary cannabinoids. THC, Δ9-Tetrahydrocannabinol, dramatically increased melatonin production in some subjects in a small study in 1986 where the authors state that "[t]hese preliminary results are difficult to interpret".[30] An older study showed that CBD, cannabidiol, was effective in helping insomniacs sleep.[31] Several studies have shown that acute administration of THC decreases sleep latency,[32] and is associated with reports of greater ease in getting to sleep[33][34]. Heavy cannabis use can lead to decreased levels of REM sleep and increased levels of slow-wave sleep along with reduced mental function the next morning. However, 5 mg doses of THC and CBD have been shown not to have these effects.[35]
Modafinil (Provigil) is approved in the US for treatment of shift-work sleep disorder, which shares some characteristics with DSPS, and a number of clinicians are prescribing it for DSPS patients. Modafinil does not deal with underlying causes of DSPS, but it may improve a sleep-deprived patient's quality of life. Taking modafinil less than 12 hours before the desired sleep onset time will likely exacerbate the symptoms by delaying the sleep/wake cycle.
Trazodone successfully treated DSPS in one elderly man.[36]
Vitamin B12 was, in the 1990s, suggested as a remedy for DSPS/DSPD, and can still be found to be recommended by many sources. Several case reports were published. However, a review for the American Academy of Sleep Medicine in 2007 concluded that no benefit was seen from this treatment.[37]
A strict schedule and good sleep hygiene are essential in maintaining any good effects of treatment. With treatment, some people with mild DSPS may sleep and function well with an early sleep schedule. Caffeine and other stimulant drugs to keep a person awake during the day may not be necessary, and should be avoided in the afternoon and evening, in accordance with good sleep hygiene. A chief difficulty of treating DSPS is in maintaining an earlier schedule after it has been established. Inevitable events of normal life, such as staying up late for a celebration or having to stay in bed with an illness, tend to reset the sleeping schedule to its intrinsic late times.
Prognosis
Adaptation to late sleeping times
Long-term success rates of treatment have seldom been evaluated. However, experienced clinicians acknowledge that DSPS is extremely difficult to treat. One study of 61 DSPS patients with mean sleep onset at about 3 a.m. and mean waking time of about 11:30 a.m., followed up with questionnaires to the subjects a year later. Good effect was seen during the 6-week treatment with a daily, very large dose (5 mg), of melatonin. Follow-up showed that over 90% had relapsed to pretreatment sleeping patterns within the year, 28.8% reporting that the relapse occurred within one week. The milder cases retained changes significantly longer than the more severe cases.[38]
Working the evening or night shift, or working at home, makes DSPS less of an obstacle for some. Many of these people do not describe their pattern as a "disorder". Some DSPS individuals nap, even taking 4–5 hours of sleep in the morning and 4–5 in the evening. DSPS-friendly careers can include security work, work in theater, the entertainment industry, hospitality work in restaurants, hotels or bars, call center work, nursing, taxi or truck driving, the media, and freelance writing, translation, IT work, or medical transcription.
Some people with the disorder are unable to adapt to earlier sleeping times, even after many years of treatment. Sleep researchers have proposed that the existence of untreatable cases of DSPS be formally recognized as a "sleep-wake schedule disorder disability", an invisible disability.
Rehabilitation for DSPS patients includes acceptance of the condition, and choosing a career that allows late sleeping times, or running their own home business because it allows flexible hours. In a few schools and universities, students with DSPS have been able to arrange to take exams at times of day when their concentration levels may be good.
Patients suffering from SWSD disability should be encouraged to accept the fact that they suffer from a permanent disability, and that their quality of life can only be improved if they are willing to undergo rehabilitation. It is imperative that physicians recognize the medical condition of SWSD disability in their patients and bring it to the notice of the public institutions responsible for vocational and social rehabilitation.[39]
In the United States, the Americans with Disabilities Act requires that employers accommodate employees with sleeping disorders by providing appropriate accommodations.[citation needed] In the case of DSPS, this requires that the employer accommodate later working hours for jobs normally performed on a "9-to-5" work schedule.
Impact on patients
Lack of public awareness of the disorder contributes to the difficulties experienced by DSPS patients, who are commonly stereotyped as undisciplined or lazy. Parents may be chastised for not giving their children acceptable sleep patterns, and schools and workplaces rarely tolerate chronically late, absent, or sleepy students and workers, failing to see them as having a chronic illness.
By the time DSPS sufferers receive an accurate diagnosis, they often have been misdiagnosed or labelled as lazy and incompetent workers or students for years. Misdiagnosis of circadian rhythm sleep disorders as psychiatric conditions causes considerable distress to patients and their families, and leads to some patients being inappropriately prescribed psychoactive drugs. For many patients, diagnosis of DSPS is itself a life-changing breakthrough.[39]
As DSPS is so little-known and so misunderstood, support groups may be important for information and self-acceptance.[40]
Comorbidity
In the DSPS cases reported in the literature, about half of the patients have suffered from clinical depression or other psychological problems, about the same proportion as among patients with chronic insomnia.[6] According to the ICSD:
Although some degree of psychopathology is present in about half of adult patients with DSPS, there appears to be no particular psychiatric diagnostic category into which these patients fall. Psychopathology is not particularly more common in DSPS patients compared to patients with other forms of "insomnia." ... Whether DSPS results directly in clinical depression, or vice versa, is unknown, but many patients express considerable despair and hopelessness over sleeping normally again.[41]
A direct neurochemical relationship between sleep mechanisms and depression is another possibility.
It is conceivable that DSPS often has a major role in causing depression because it can be such a stressful and misunderstood disorder. A recent study from the University of California, San Diego found no association of bipolar disorder (history of mania) with DSPD, and it states that there may be
behaviorally-mediated mechanisms for comorbidity between DSPD and depression. For example, the lateness of DSPD cases and their unusual hours may lead to social opprobrium and rejection, which might be depressing...[42]
The fact that half of DSPS patients are not depressed indicates that DSPS is not merely a symptom of depression. Sleep researcher M. Terman has suggested that those who follow their internal circadian clocks may be less likely to suffer from depression than those try to live on a different schedule.
DSPS patients who also suffer from depression may be best served by seeking treatment for both problems. There is some evidence that effectively treating DSPS can improve the patient's mood and make antidepressants more effective.
Vitamin D deficiency has been linked to depression. As it is a condition which comes from lack of exposure to sunlight, anyone who does not get enough sunlight exposure during the daylight hours could be at risk.
Accommodations
United States
According to the Americans with Disabilities Act of 1990, "disability" is defined as a "physical or mental impairment that substantially limits one or more major life activities". "Sleeping" is defined as a "major life activity" in § 12102(2)(a) of the statute.[43]
See also
- Advanced sleep phase syndrome
- Chronobiology
- Circadian rhythm
- Evolutionary baggage
- Insomnia
- Non-24-hour sleep-wake syndrome
- Irregular sleep-wake rhythm
- Seasonal Affective Disorder
- Sleep inertia
Notes
- ^ Hirshkowitz, Max (2004). "Chapter 10, Neuropsychiatric Aspects of Sleep and Sleep Disorders (pp. 315-340)". In Stuart C. Yudofsky and Robert E. Hales, editors (ed.). Essentials of neuropsychiatry and clinical neurosciences (4 ed.). Arlington, Virginia, USA: American Psychiatric Publishing. pp. 324–325. ISBN 9781585620050.
Individuals with delayed sleep phase are more alert in the evening and early nighttime, stay up later, and are more tired in the morning.
{{cite book}}:|access-date=requires|url=(help);|editor=has generic name (help);|format=requires|url=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ Dagan Y, Eisenstein M (1999). "Circadian rhythm sleep disorders: toward a more precise definition and diagnosis". Chronobiol. Int. 16 (2): 213–22. doi:10.3109/07420529909019087. PMID 10219492.
- ^ Weitzman ED, Czeisler CA, Coleman RM; et al. (1981). "Delayed sleep phase syndrome. A chronobiological disorder with sleep-onset insomnia". Arch. Gen. Psychiatry. 38 (7): 737–46. PMID 7247637.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ "Sleeplessness and Circadian Rhythm Disorder". eMedicine World Medical Library from WebMD. Retrieved 2006-06-04.
Implicit in the diagnosis of circadian rhythm disorder is a desire to conform to traditionally accepted sleep-wake patterns.
- ^ Dagan Y (2002). "Circadian rhythm sleep disorders (CRSD)" (PDF: full text). Sleep Med Rev. 6 (1): 45–54. doi:10.1053/smrv.2001.0190. PMID 12531141. Retrieved 2007-11-08.
Early onset of CRSD, the ease of diagnosis, the high frequency of misdiagnosis and erroneous treatment, the potentially harmful psychological and adjustment consequences, and the availability of promising treatments, all indicate the importance of greater awareness of these disorders.
- ^ a b c d American College of Physicians--American Society of Internal Medicine (2005). International Classification of Sleep Disorders: Diagnostic & Coding Manual (PDF: full text, 2001 version). Amer Academy of Sleep Medicine. ISBN 0-9657220-2-3.
- ^ Okawa M, Uchiyama M (2007). "Circadian rhythm sleep disorders: characteristics and entrainment pathology in delayed sleep phase and non-24-h sleep-wake syndrome" (PDF: full text). Sleep Med Rev. 11 (6): 485–96. doi:10.1016/j.smrv.2007.08.001. PMID 17964201. Retrieved 2008-03-13.
- ^ El-Ad, Baruch. "Delayed sleep phase syndrome". MedLink Neurology. Retrieved 2008-03-24.
(Type 'delayed sleep phase' in search box.)
- ^ Schrader H, Bovim G, Sand T (1993). "The prevalence of delayed and advanced sleep phase syndromes". J Sleep Res. 2 (1): 51–55. doi:10.1111/j.1365-2869.1993.tb00061.x. PMID 10607071.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Yazaki M, Shirakawa S, Okawa M, Takahashi K (1999). "Demography of sleep disturbances associated with circadian rhythm disorders in Japan". Psychiatry Clin. Neurosci. 53 (2): 267–8. doi:10.1046/j.1440-1819.1999.00533.x. PMID 10459707.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.hopkinschildrens.org/tpl_news.aspx?id=2630
- ^ Carskadon, Mary A. (2008). "Circadian and Homeostatic Regulation of Sleep in Adolescent Humans" (PDF, abstract). conference presentations, p. 44. Society for Research on Biological Rhythms. Retrieved 2008-05-14.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Billiard, Michel (2003). Sleep: Physiology, Investigations and Medicine (Page view, Google books). New York: Springer. pp. 495–97. ISBN 0306474069. Retrieved 2009-08-03.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Uchiyama M, Okawa M, Shibui K; et al. (1999). "Poor recovery sleep after sleep deprivation in delayed sleep phase syndrome". Psychiatry Clin. Neurosci. 53 (2): 195–7. doi:10.1046/j.1440-1819.1999.00481.x. PMID 10459687.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Ancoli-Israel S, Schnierow B, Kelsoe J, Fink R (2001). "A pedigree of one family with delayed sleep phase syndrome". Chronobiol. Int. 18 (5): 831–40. doi:10.1081/CBI-100107518. PMID 11763990.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Archer SN, Robilliard DL, Skene DJ, Smits M, Williams A, Arendt J, von Schantz M. (2003). "A length polymorphism in the circadian clock gene Per3 is linked to delayed sleep phase syndrome and extreme diurnal preference". Sleep. 26 (4): 413–5. PMID 12841365.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Nadkarni NA, Weale ME, von Schantz M, Thomas MG (2005). "Evolution of a length polymorphism in the human PER3 gene, a component of the circadian system". J. Biol. Rhythms. 20 (6): 490–9. doi:10.1177/0748730405281332. PMID 16275768.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Boivin DB, James FO, Santo JB, Caliyurt O, Chalk C (2003). "Non-24-hour sleep-wake syndrome following a car accident". Neurology. 60 (11): 1841–3. PMID 12796546.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Quinto C, Gellido C, Chokroverty S, Masdeu J (2000). "Posttraumatic delayed sleep phase syndrome". Neurology. 54 (1): 250–2. PMID 10636163.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Okawa, Masako (2007). "Clinical Review. Circadian rhythm sleep disorders: Characteristics and entrainment pathology in delayed sleep phase and non-24-h sleep-wake syndrome" (PDF: full text). Sleep Medicine (11). Elsevier Ltd: 485–496. Retrieved 2008-04-16.
Although delaying both bedtime and waking time by 3h, repeated daily until rotation around the clock can achieve the desired sleep-wake schedule, this delaying chronotherapy could lead to non-24 by allowing the system to slip around the clock and cause dangerous situations.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Aoki H, Ozeki Y, Yamada N (2001). "Hypersensitivity of melatonin suppression in response to light in patients with delayed sleep phase syndrome". Chronobiol. Int. 18 (2): 263–71. doi:10.1081/CBI-100103190. PMID 11379666.
Our findings therefore suggest that evening light restriction is important for preventing patients with DSPS from developing a sleep phase delay.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Stores G (2003). "Misdiagnosing sleep disorders as primary psychiatric conditions" (Full text). Advances in Psychiatric Treatment. 9: 69–77. doi:10.1192/apt.9.1.69.
See also subsequent:
* Stores G (2007). "Clinical diagnosis and misdiagnosis of sleep disorders". J. Neurol. Neurosurg. Psychiatr. 78 (12): 1293–7. doi:10.1136/jnnp.2006.111179. PMID 18024690. - ^ Dagan Y, Ayalon L (2005). "Case study: psychiatric misdiagnosis of non-24-hours sleep-wake schedule disorder resolved by melatonin". J Am Acad Child Adolesc Psychiatry. 44 (12): 1271–5. doi:10.1097/01.chi.0000181040.83465.48. PMID 16292119.
- ^ How light therapy can treat DSPS. Retrieved 29/10/2010
- ^ Morgenthaler, TI (2007). "Standards of Practice Committee of the AASM. Practice Parameters for the Clinical Evaluation and Treatment of Circadian Rhythm Sleep Disorders". SLEEP. 30 (11). Associated Professional Sleep Societies, LLC: 1445–59. Retrieved 2010-26-9.
{{cite journal}}: Check date values in:|accessdate=(help); Text "PMCID:PMC2082098" ignored (help) - ^ Burgess HJ, Revell VL, Eastman CI (2008). "A three pulse phase response curve to three milligrams of melatonin in humans". J. Physiol. (Lond.). 586 (2): 639–47. doi:10.1113/jphysiol.2007.143180. PMC 2375577. PMID 18006583.
Using exogenous melatonin as a sleep aid at night has minimal phase shifting effects
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mundey, K (2005). "Phase-dependent treatment of delayed sleep phase syndrome with melatonin". Sleep. 28 (10): 1214–6. PMID 16295212. Retrieved 2009-02-26.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ Lewy AJ, Emens JS, Sack RL, Hasler BP, Bernert RA (2002). "Low, but not high, doses of melatonin entrained a free-running blind person with a long circadian period". Chronobiol Int. 19 (3): 649–58. doi:10.1081/CBI-120004546. PMID 12069043.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Buscemi N., Vandermeer B., Pandya R., et al. Melatonin for Treatment of Sleep Disorders. Summary, Evidence Report/Technology Assessment: Number 108. AHRQ Publication Number 05-E002-1, November 2004. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/clinic/epcsums/melatsum.htm
- ^ Lissoni P, Resentini M, Mauri R; et al. (1986). "Effects of tetrahydrocannabinol on melatonin secretion in man" (Reprint). Horm. Metab. Res. 18 (1): 77–8. doi:10.1055/s-2007-1012235. PMID 3005151.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Carlini EA, Cunha JM (1981). "Hypnotic and antiepileptic effects of cannabidiol". J Clin Pharmacol. 21 (8-9 Suppl): 417S–427S. PMID 7028792.
- ^ K. Cousens and A. DiMascio (1973). "Delta 9 THC as an hypnotic". Psychopharmacologia. 33 (4): 355–364. PMID 4776660.
- ^ L.D. Chait (1990). "Subjective and behavioral effects of marijuana the morning after smoking". Psychopharmacology. 100 (3): 328–333. PMID 2315429.
- ^ M. Haney, C.L. Hart and S.K. Vosburg; et al. (2004). "Marijuana withdrawal in humans: effects of oral THC or divalproex". Neuropsychopharmacology. 29 (1): 158–170. PMID 14560320.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Nicholson AN, Turner C, Stone BM, Robson PJ (2004). "Effect of Delta-9-tetrahydrocannabinol and cannabidiol on nocturnal sleep and early-morning behavior in young adults" (PDF: full text). J Clin Psychopharmacol. 24 (3): 305–13. doi:10.1097/01.jcp.0000125688.05091.8f. PMID 15118485.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Nakasei S; et al. (2005). "Trazodone advanced a delayed sleep phase of an elderly male: A case report". Sleep and Biological Rhythms. 3: 169. doi:10.1111/j.1479-8425.2005.00177.x.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - ^ Sack RL, Auckley D, Auger RR; et al. (2007). "Circadian rhythm sleep disorders: part II, advanced sleep phase disorder, delayed sleep phase disorder, free-running disorder, and irregular sleep-wake rhythm. An American Academy of Sleep Medicine review" (PDF: full text). Sleep. 30 (11): 1484–501. PMC 2082099. PMID 18041481.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Dagan Y, Yovel I, Hallis D, Eisenstein M, Raichik I (1998). "Evaluating the role of melatonin in the long-term treatment of delayed sleep phase syndrome (DSPS)". Chronobiol. Int. 15 (2): 181–90. doi:10.3109/07420529808998682. PMID 9562922.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Dagan Y, Abadi J (2001). "Sleep-wake schedule disorder disability: a lifelong untreatable pathology of the circadian time structure". Chronobiol. Int. 18 (6): 1019–27. doi:10.1081/CBI-100107975. PMID 11777076.
- ^ Potts, Henry W.W. ([2005]). "Online support groups: An overlooked resource for patients" (PDF: full text). University College London. Retrieved 2008-04-14.
{{cite web}}: Check date values in:|year=(help)CS1 maint: year (link) - ^ Thorpy M (2001). The International Classification of Sleep Disorders, Revised: Diagnostic and Coding Manual (PDF: full text). Chicago, Illinois, USA: The American Academy of Sleep Medicine in association with the European Sleep Research Society, the Japanese Society of Sleep Research and the Latin American Sleep Society. pp. 72–73. ISBN 0-9657220-1-5. Retrieved 2008-03-23.
- ^ Kripke, Daniel F. (2008). "Delayed sleep phase cases and controls" (PDF: full text). Journal of Circadian Rhythms. 6 (6): 6. doi:10.1186/1740-3391-6-6. PMC 2391143. PMID 18445295. Retrieved 2008-05-01.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - ^ "Americans with Disabilities Act of 1990". Retrieved 2010-01-20.
References
- Thorpy MJ, Korman E, Spielman AJ, Glovinsky PB (1988). "Delayed sleep phase syndrome in adolescents". J Adolesc Health Care. 9 (1): 22–7. doi:10.1016/0197-0070(88)90014-9. PMID 3335467.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "When the body clock goes wrong: delayed sleep phase syndrome". Lancet. 340 (8824): 884–5. 1992. doi:10.1016/0140-6736(92)93292-U. PMID 1357304.
- Regestein QR, Pavlova M (1995). "Treatment of delayed sleep phase syndrome". Gen Hosp Psychiatry. 17 (5): 335–45. doi:10.1016/0163-8343(95)00062-V. PMID 8522148.
- Regestein QR, Monk TH (1995). "Delayed sleep phase syndrome: a review of its clinical aspects". Am J Psychiatry. 152 (4): 602–8. PMID 7694911.
- Terman, Michael (2010-04-19). "Sleeping (or Not) by the Wrong Clock". New York Times.
{{cite journal}}: Italic or bold markup not allowed in:|journal=(help)
External links
- Australian DSPS fact sheet, PDF
- DSPS blog
- Dement W.C. (1999-02-26). "Delayed sleep phase syndrome". Stanford University.
- "DSPS - Delayed Sleep-Phase Syndrome". DSPSinfo.org. - Written by and for people with DSPS
- Parker-Pope, Tara (2006-03-21). "Health Journal: Doctors probe why it's hard for many kids to get up". The Wall Street Journal. Retrieved 2008-12-02.
