Emphysema: Difference between revisions
←Replaced content with '{{For|the condition describing air trapped under the skin|subcutaneous emphysema}} {{Infobox disease I bet your wondering what the world happened to this....' Tag: possible vandalism |
ClueBot NG (talk | contribs) m Reverting possible vandalism by 96.228.16.10 to version by DragonLord. False positive? Report it. Thanks, ClueBot NG. (1579626) (Bot) |
||
| Line 1: | Line 1: | ||
{{For|the condition describing air trapped under the skin|subcutaneous emphysema}} |
{{For|the condition describing air trapped under the skin|subcutaneous emphysema}} |
||
{{Infobox disease |
{{Infobox disease |
||
| Image = Barrowchest.JPG |
|||
| Caption = A lateral chest x-ray of a person with emphysema. Note the barrel chest and flat diaphragm. |
|||
I bet your wondering what the world happened to this....... I DROP BUCKETS!!!!!!!!!!!!!!!!!!!!! |
|||
| DiseasesDB = 4190 |
|||
| ICD10 = {{ICD10|J|43||j|40}} |
|||
| ICD9 = {{ICD9|492}} |
|||
| ICDO = |
|||
| OMIM = |
|||
| MedlinePlus = 000136 |
|||
| eMedicineSubj = med |
|||
| eMedicineTopic = 654 |
|||
| MeshID = D011656 |
|||
}} |
|||
'''Emphysema''' is a long-term lung disease. ''[[Subcutaneous emphysema]]'' is a condition where air is present beneath the skin. |
|||
In people with emphysema, the [[Tissue (biology)|tissue]]s necessary to support the physical shape and function of the lungs are destroyed. It is included in a group of diseases called [[chronic obstructive pulmonary disease]] or COPD. Emphysema is called an obstructive lung disease because the destruction of lung tissue around smaller sacs, called [[alveoli]], makes these air sacs unable to hold their functional shape upon [[exhalation]]. Emphysema is most often caused by [[tobacco]] [[smoking]] and long-term exposure to [[air pollution]]. |
|||
The term "emphysema" is derived from the [[Greek language|Greek]] {{lang|el|ἐμφυσᾶν}} ''emphysan'' meaning "''inflate''" - itself composed of ἐν ''en'', meaning "''in''", and φυσᾶν ''physan'', meaning "''breath, blast''".<ref>[http://dictionary.reference.com/browse/emphysema emphysema] at [[dictionary.com]]</ref> |
|||
== Signs and symptoms == |
|||
Emphysema is a disease of the [[lung]] tissue caused by destruction of structures feeding the [[alveoli]], in some cases owing to the consequences of [[alpha 1-antitrypsin deficiency]]. Smoking is one major cause of this destruction, which results in the collapse of small airways in the [[lungs]] during forced [[exhalation]]. As a result, airflow is impeded and air becomes trapped, just as in other obstructive lung diseases. Symptoms include shortness of breath ("[[dyspnea]]") on [[exercise|exertion]] and an [[expanded chest]]. |
|||
People with this disease do not get enough [[oxygen]] and suffer a buildup of [[carbon dioxide]] in their [[blood]], which generates dyspnea. At first, when emphysema is mild, dyspnea occurs only during physical activity. Eventually, as the disease progresses, dyspnea will occur after even small amounts of physical exertion. On the other hand, if the lungs are compromised badly enough, the victim may feel short of breath all the time - even when at rest, relaxing. Because breathing is more difficult, the person must use accessory muscles to help them breathe; the increased work of breathing, use of additional muscles, and blood gas abnormalities then combine to cause "[[tachypnea]]" (rapid breathing), which may continue in a "vicious circle". Individuals with severe emphysema eventually may have trouble coughing and decreased amounts of [[sputum]]. They may also lose weight. |
|||
The [[Anteroposterior#Anterior_and_posterior|anteroposterior]] diameter of their chest may increase; this sign is sometimes referred as "barrel chest." They may lean forward with arms extended and/or resting on something to help them breathe ("orthopneic breathing"). |
|||
When lung [[auscultation]] and [[chest]] [[Percussion (medicine)|percussion]] is performed a hyperresonant sound is heard. |
|||
The person may also exhibit symptoms of [[hypoxia (medical)|hypoxia]]-induced [[cyanosis]], or the appearance of a blue-to-purplish discoloration of the skin, because of increased levels of [[Hemoglobin#Deoxyhemoglobin|deoxyhemoglobin]] in the blood. |
|||
==Causes== |
|||
The majority of all emphysema cases are caused by many years of [[Health effects of tobacco|smoking tobacco]]. Emphysema does not develop suddenly. It comes on very gradually. Years of exposure to the irritation of cigarette smoke usually precede the development of emphysema. Of the estimated 3.7 million Americans ever diagnosed with emphysema, 94 percent are 45 or older. <ref> Centers for Disease Control and Prevention. National Center for Health Statistics: National Health Interview Survey Raw Data, 2008. Analysis performed by American Lung Association Research and Program [http://www.lung.org/lung-disease/copd/resources/facts-figures/COPD-Fact-Sheet.html#note_18 www.lung.org COPD-Fact-Sheet note 18]</ref> Emphysema cases that are caused by other [[etiology|etiologies]] are referred to as ''secondary'' emphysema. {{Citation needed|date=October 2011}} Anything that causes the body to be unable to inhibit [[proteolytic enzymes]] occurring naturally in the lung can cause, or contribute to, the development of emphysema. This could include exposure to air pollution, second-hand smoke, and/or other chemicals and toxins.<ref>{{cite journal |author=Takeshi Terashima, Maria E. Klut, Dean English, Jennifer Hards, James C. Hogg, and Stephan F. van Eeden |title=Cigarette Smoking Causes Sequestration of Polymorphonuclear Leukocytes |
|||
Released from the Bone Marrow in Lung Microvessels |journal=AMERICAN JOURNAL OF RESPIRATORY CELL AND MOLECULAR BIOLOGY |volume=20 |pages=171–177 |year=1990 |url=http://ajrcmb.atsjournals.org/content/20/1/171.full.pdf}}</ref> |
|||
In rare cases, emphysema develops as a result of a [[gene]]tic [[mutation]] that leads to [[alpha 1-antitrypsin deficiency]]. Severe cases of A1AD may also develop [[cirrhosis]] of the [[liver]], where the accumulated abnormal A1AT leads to a [[fibrosis|fibrotic]] reaction that produces scarring and dysfunction; longstanding cirrosis may eventually produce liver [[cancer]] ([[hepatocellular carcinoma]]). The hereditary form of emphysema illustrates the detrimental effects that can result from misfolding of proteins in the [[endoplasmic reticulum]] (ER). This disease is caused by a point mutation in alpha1-antitrypsin, which normally is secreted by hepatocytes and macrophages. The wild-type protein binds to and inhibits trypsin and also the blood protease elastase. In the absence of alpha1-antitrypsin, elastase degrades the fine tissue in the lung that participates in the absorption of oxygen, eventually producing the symptoms of emphysema. Although the mutant alpha1-antitrypsin is synthesized in the rough ER, it does not fold properly, forming an almost crystalline aggregate that is not exported from the ER. In hepatocytes, the secretion of other proteins also becomes impaired, as the rough ER is filled with aggregated alpha1-antitrypsin.<ref>Lodish et al - Molecular Cell Biology 5e (page: 675)</ref> |
|||
Some types of emphysema occur as a normal part of aging, and are commonly found in the oldest old (85 years of age and older). At about 20 years of age, [[Homo sapiens|humans]] stop developing new alveolar tissue. In the years following the cessation of development of new alveoli, lung tissue starts to deteriorate (on a "net" basis) at a relatively slow rate. This deterioration of lung capacity and function is a normal and natural part of aging in healthy people. As alveoli die, the number of lung [[capillaries]] decreases, and the [[elastin]] of the lungs begins to break down, causing a loss of pulmonary elasticity. As people age, they also tend to lose strength and mass in their chest muscles, which weaken, [[bone]]s and [[cartilage]] start to deteriorate, and posture changes. Together, all of these age-related changes in [[respiratory system]] structures can cause or contribute to the development of emphysema. Though not all elderly people will develop clinically evident emphysema, they are all at risk of decreasing respiratory function, which limits maximum performance and produces discomfort at higher levels of exertion. |
|||
== Pathophysiology == |
|||
[[File:Centrilobular emphysema 865 lores.jpg|thumb|Pathology of lung showing centrilobular emphysema characteristic of smoking. Closeup of fixed, cut surface shows multiple cavities lined by heavy black carbon deposits. (CDC/Dr. Edwin P. Ewing, Jr., 1973)]] |
|||
In normal breathing, air is drawn in through the [[bronchi]] and into the alveoli, which are tiny sacs surrounded by capillaries. Alveoli absorb [[oxygen]] and then transfer it into the [[blood]]. When toxins, such as cigarette smoke, are breathed into the lungs, the harmful particles become trapped in the alveoli, causing a localized [[inflammation|inflammatory]] response. Chemicals released during the inflammatory response (e.g., [[elastase]]) can eventually cause the [[alveolar septum]] to disintegrate. This condition, known as septal rupture, leads to significant deformations of the lung architecture<ref>S. Nazari : Mechanical Events In Physiopathology Of Idiopathic Pulmonary Emphysema: A Theoretical Analysis. The Internet Journal of Thoracic and Cardiovascular Surgery. 2002 Volume 5 Number 2</ref><ref>Nazari S.The surgical physiopathology of essential pulmonary emphysema and volume-reduction intervention'''. Minerva Chir. 1998 Nov;53(11):899-918. PMID 9973794</ref> [http://www.fondazionecarrel.org/carrel/thorac/files/enphys/new/emphysema1.html (video)] that have important functional consequences. The key mechanical event consequent to septal rupture is that the resulting cavity is larger than the sum of the two alveolar spaces (see figure); in fact because of the lacking mechanical support of the broken septa the lung elastic recoil further enlarges this new space, necessarily at the expenses of the surrounding healthy [[parenchyma]]. In other words, as an immediate and spontaneous consequence of septal rupture, the elastic lung recoil resets healthy parenchyma expansion at a lower level, in proportion to the amount of septal disruption. |
|||
The large cavities left by the septal rupture are known as bullae. These deformations result in a large decrease of alveoli surface area used for gas exchange, as well as decreased ventilation of the surrounding healthy parenchyma. This results in a decreased Transfer Factor of the Lung for Carbon Monoxide ([[TLCO]]). To accommodate the decreased surface area, [[thoracic]] cage expansion (barrel chest) and diaphragm contraction (flattening) take place. Expiration, which physiologically depends completely on lung [[elastic recoil]], increasingly depends on the thoracic cage and abdominal muscle action, particularly in the end expiratory phase. Due to decreased ventilation, the ability to exude carbon dioxide is significantly impaired. In the more serious cases, oxygen uptake is also impaired. |
|||
As the alveoli continue to break down, hyperventilation is unable to compensate for the progressively shrinking surface area, and the body is not able to maintain high enough oxygen levels in the blood. The body's last resort is vasoconstricting appropriate vessels. This leads to pulmonary [[hypertension]], which places increased strain on the right side of the heart, the side responsible for pumping deoxygenated blood to the lungs. The heart muscle thickens in order to pump more blood. This condition is often accompanied by the appearance of jugular venous distension. Eventually, as the heart continues to fail, it becomes larger and blood backs up in the liver. |
|||
People with [[alpha 1-antitrypsin deficiency]] (A1AD) are more likely to suffer from emphysema. A1AT inhibits inflammatory enzymes (such as [[elastase]]) from destroying the [[Pulmonary alveolus|alveolar]] [[tissue (biology)|tissue]]. Most people with A1AD do not develop clinically significant emphysema, but smoking and severely decreased A1AT levels (10-15%) can cause emphysema at a young age. The type of emphysema caused by A1AD is known as ''panacinar'' emphysema (involving the entire [[acinus]]) as opposed to ''centrilobular'' emphysema, which is caused by smoking. Panacinar emphysema typically affects the lower lungs, while centrilobular emphysema affects the upper lungs. A1AD causes about 2% of all emphysema. Smokers with A1AD are at the greatest risk for emphysema. Mild emphysema can often develop into a severe case over a short period of time (1–2 weeks). |
|||
While A1AD provides some insight into the pathogenesis of the disease, hereditary A1AT deficiency only accounts for a small proportion of the disease. Studies for the better part of the past century have focused mainly upon the putative role of [[leukocyte]] [[elastase]] (also ''neutrophil elastase''), a serine [[protease]] found in neutrophils, as a primary contributor to the connective tissue damage seen in the disease. This hypothesis, a result of the observation that neutrophil elastase is the primary substrate for A1AT, and A1AT is the primary inhibitor of neutrophil elastase, together have been known as the "''protease-antiprotease''" theory, implicating neutrophils as an important mediator of the disease. However, more recent studies have brought into light the possibility that one of the many other numerous proteases, especially matrix metalloproteases might be equally or more relevant than neutrophil elastase in the development of non-hereditary emphysema. |
|||
The better part of the past few decades of research into the pathogenesis of emphysema involved animal experiments where various proteases were instilled into the trachea of various species of animals. These animals developed connective tissue damage, which was taken as support for the protease-antiprotease theory. However, just because these substances can destroy connective tissue in the lung, as anyone would be able to predict, doesn't establish causality. More recent experiments have focused on more technologically advanced approaches, such as ones involving genetic manipulation. One particular development with respect to our understanding of the disease involves the production of protease "knock-out" animals, which are genetically deficient in one or more proteases, and the assessment of whether they would be less susceptible to the development of the disease. Often individuals who are unfortunate enough to contract this disease have a very short life expectancy, often 0–3 years at most. |
|||
==Diagnosis== |
|||
The diagnosis is usually confirmed by [[pulmonary function test]]ing (e.g. [[spirometry]] or [[body plethysmography]]); however, X-ray [[radiography]] may aid in the diagnosis. Diffusing capacity of the lung for carbon monoxide ([[DLCO]]) may be tested to differentiate emphysema from other types of obstructive disorders such as chronic bronchitis and asthma. D<sub>LCO</sub> is a test that measures the ability of gases to diffuse across the alveolar-capillary membrane. D<sub>LCO</sub> will be decreased in emphysema, whereas it will be normal or increased in asthma and chronic bronchitis. |
|||
<gallery> |
|||
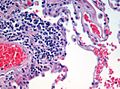
Image:Emphysema H and E.jpg|H&E stained [[lung]] tissue of end-stage emphysema. [[red blood cell|RBCs]] are red, [[cell nucleus|nuclei]] are purple, other material is pink, and air spaces are white. |
|||
Image:Emphysema low mag.jpg|[[Micrograph]] demonstrating emphysema (left of image - large empty spaces) and [[lung]] tissue with relative preservation of the alveoli (right of image). [[H&E stain]]. |
|||
File:Bullus emphasemaCT.png|Axial CT image of the lung of a person with end-stage bullus emphysema. |
|||
Image:Emphysema2008.jpg|A severe case of emphysema. |
|||
Image:BullaCXR.PNG|Lung bulla as seen on CXR in a person with severe COPD</gallery> |
|||
=== Classification === |
|||
Emphysema can be classified into ''primary'' and ''secondary'' types. However, it is more commonly classified by location into '''panacinary''' and '''centroacinary''' (or panacinar and centriacinar,<ref name="urlEmphysema">{{cite web|url=http://www.meddean.luc.edu/Lumen/MedEd/MEDICINE/PULMONAR/pathms/mpath6.htm |title=Emphysema |work=|accessdate=2008-11-20}}</ref> or centrilobular and panlobular).<ref name="pmid4784376">{{cite journal |author=Anderson AE, Foraker AG |title=Centrilobular emphysema and panlobular emphysema: two different diseases |journal=Thorax |volume=28 |issue=5|pages=547–50 |year=1973 |month=September |pmid=4784376 |doi= 10.1136/thx.28.5.547|pmc=470076}}</ref> |
|||
* ''Panacinar'' (or ''panlobular'') emphysema: The entire respiratory lobule, from [[respiratory bronchiole]] to alveoli, has expanded. Occurs more commonly in the lower lobes (especially basal segments) and in the anterior margins of the lungs.<ref name="urlEmphysema"/> |
|||
* ''Centriacinar'' (or ''centrilobular'') emphysema: The respiratory bronchiole (proximal and central part of the acinus) has expanded. The distal acinus or alveoli are unchanged. Occurs more commonly in the upper lobes.<ref name="urlEmphysema">{{cite web |url=http://www.meddean.luc.edu/Lumen/MedEd/MEDICINE/PULMONAR/pathms/mpath6.htm |title=Emphysema|work= |accessdate=2010-01-20}}</ref> |
|||
Other types include distal acinar emphysema and irregular emphysema.<ref name="urlEmphysema"/> A special type is congenital lobar emphysema (or CLE). |
|||
==== Congenital lobar emphysema ==== |
|||
[[File:Medical X-Ray imaging WFH07 nevit.jpg|A severe case of bullous emphysema|thumb]] |
|||
CLE results in overexpansion of a [[pulmonary lobe]], and resultant compression of the remaining lobes of the ipsilateral lung (and possibly also the contralateral [[lung]]). There is [[bronchus|bronchial]] narrowing because of weakened or absent bronchial [[cartilage]].<ref name=Wood>[http://emedicine.medscape.com/article/407635-overview eMedicine Specialties > Radiology > Pediatrics --> Congenital Lobar Emphysema] Author: Beverly P Wood, MD, MS, PhD, University of Southern California. Updated: December 1, 2008</ref> There may be [[congenital]] extrinsic compression, commonly by an abnormally large [[pulmonary artery]]. This causes malformation of bronchial cartilage, making them soft and collapsible.<ref name=Wood/> CLE is a potentially reversible (yet possibly life-threatening) cause of respiratory distress in the [[infant|neonate]].<ref name=Wood/> |
|||
====Paraseptal emphysema==== |
|||
Paraseptal emphysema is a type of emphysema which involves the alveolar ducts and sacs at the lung periphery. The emphysematous areas are subpleural in location and often surrounded by interlobular septa (hence the name). It may be an incidental finding in young adults, and may be associated with spontaneous [[pneumothorax]]. It may also be seen in older people with centrilobular emphysema. Both centrilobular and paraseptal emphysema may progress to bullous emphysema. A bulla is defined as being at least 1 cm in diameter, and with a wall less than 1mm thick. Bullae are thought to arise by [[air trapping]] in emphysematous spaces, causing local expansion.<ref>Webb WR, Higgins CB. ''Thoracic Imaging''. Lippincott, Williams & Wilkins 2005.</ref> |
|||
== Management == |
|||
[[File:Fluticasonejf.JPG|thumb|[[Asthma]] & Emphysema medicines: [[Fluticasone/salmeterol]], [[Salbutamol]] & [[Budesonide/formoterol]].]] |
|||
Emphysema is an irreversible degenerative condition. It is recommended that people who think they may have the disease seek medical attention as soon as possible. The most important measure to slow its progression is for the person to stop smoking and avoid all exposure to cigarette smoke and lung [[irritation|irritant]]s. [[Pulmonary rehabilitation]] can be very helpful to optimize the patient's [[quality of life]] and teach the patient how to actively manage his or her care. |
|||
Emphysema is also treated by supporting the breathing with [[anticholinergics]], bronchodilators, steroid medication (inhaled or oral), effective body positioning ([[Fowler's position|high Fowler's]]), and supplemental oxygen as required. Treating the patient's other conditions including [[gastric reflux]] and [[allergy|allergies]] may improve lung function. Supplemental oxygen used as prescribed (usually more than 20 hours per day) is the only non-surgical treatment which has been shown to prolong life in emphysema patients. There are lightweight portable oxygen systems which allow patients increased mobility. Patients can fly, cruise, and work while using supplemental oxygen. Other medications are being researched. |
|||
[[Lung volume reduction surgery]] (LVRS) can improve the quality of life for certain carefully selected patients. It can be done by different methods, some of which are minimally invasive. In July 2006 a new treatment, placing tiny [[valve]]s in passages leading to diseased lung areas, was announced to have good results, but 7% of patients suffered partial lung collapse. |
|||
The only known "cure" for emphysema is [[lung transplant]], but few patients are strong enough physically to survive the [[surgery]]. The combination of a patient's age, oxygen deprivation and the side-effects of the medications used to treat emphysema cause damage to the [[kidney]]s and other [[organ (anatomy)|organs]]. [[organ transplant|Surgical transplantation]] also requires the patient to take an [[Transplant rejection#Prevention of rejection|anti-rejection drug regimen]] which suppresses the immune system, and can lead to microbial [[infection]] of the patient. |
|||
== Research == |
|||
With the discovery of [[multipotent]] lung stem cells in 2011, a new treatment option may soon become available. Scientists injected human lung stem cells into mice with damaged lungs. The stem cells formed human bronchioles, alveoli, and pulmonary vessels integrated structurally and functionally with the damaged mouse organ. The May 2011 report in the New England Journal of Medicine <ref>{{cite web|title=Evidence for Human Lung Stem Cells|url=http://www.nejm.org/doi/full/10.1056/NEJMoa1101324|work=New England Journal of Medicine|accessdate=07-12-2011}}</ref> concluded that human lung stem cells "have the undemonstrated potential to promote tissue restoration in patients with lung disease". |
|||
== Footnotes == |
|||
{{Reflist|2}} |
|||
== External links == |
|||
* Images of Emphysema http://www.radrounds.com/photo/paraseptal-and-centrilobular-1 |
|||
* [http://library.med.utah.edu/WebPath/webpath.html#MENU The Internet Pathology Laboratory for Medical Education of Mercer University School of Medicine] |
|||
{{Respiratory pathology}} |
|||
[[Category:Chronic lower respiratory diseases]] |
|||
[[Category:Smoking]] |
|||
[[es:Enfisema]] |
|||
[[sl:Kronična obstruktivna pljučna bolezen]] |
|||
Revision as of 15:33, 4 April 2013
| Emphysema | |
|---|---|
| Specialty | Pulmonology |
Emphysema is a long-term lung disease. Subcutaneous emphysema is a condition where air is present beneath the skin.
In people with emphysema, the tissues necessary to support the physical shape and function of the lungs are destroyed. It is included in a group of diseases called chronic obstructive pulmonary disease or COPD. Emphysema is called an obstructive lung disease because the destruction of lung tissue around smaller sacs, called alveoli, makes these air sacs unable to hold their functional shape upon exhalation. Emphysema is most often caused by tobacco smoking and long-term exposure to air pollution.
The term "emphysema" is derived from the Greek ἐμφυσᾶν emphysan meaning "inflate" - itself composed of ἐν en, meaning "in", and φυσᾶν physan, meaning "breath, blast".[1]
Signs and symptoms
Emphysema is a disease of the lung tissue caused by destruction of structures feeding the alveoli, in some cases owing to the consequences of alpha 1-antitrypsin deficiency. Smoking is one major cause of this destruction, which results in the collapse of small airways in the lungs during forced exhalation. As a result, airflow is impeded and air becomes trapped, just as in other obstructive lung diseases. Symptoms include shortness of breath ("dyspnea") on exertion and an expanded chest.
People with this disease do not get enough oxygen and suffer a buildup of carbon dioxide in their blood, which generates dyspnea. At first, when emphysema is mild, dyspnea occurs only during physical activity. Eventually, as the disease progresses, dyspnea will occur after even small amounts of physical exertion. On the other hand, if the lungs are compromised badly enough, the victim may feel short of breath all the time - even when at rest, relaxing. Because breathing is more difficult, the person must use accessory muscles to help them breathe; the increased work of breathing, use of additional muscles, and blood gas abnormalities then combine to cause "tachypnea" (rapid breathing), which may continue in a "vicious circle". Individuals with severe emphysema eventually may have trouble coughing and decreased amounts of sputum. They may also lose weight.
The anteroposterior diameter of their chest may increase; this sign is sometimes referred as "barrel chest." They may lean forward with arms extended and/or resting on something to help them breathe ("orthopneic breathing").
When lung auscultation and chest percussion is performed a hyperresonant sound is heard.
The person may also exhibit symptoms of hypoxia-induced cyanosis, or the appearance of a blue-to-purplish discoloration of the skin, because of increased levels of deoxyhemoglobin in the blood.
Causes
The majority of all emphysema cases are caused by many years of smoking tobacco. Emphysema does not develop suddenly. It comes on very gradually. Years of exposure to the irritation of cigarette smoke usually precede the development of emphysema. Of the estimated 3.7 million Americans ever diagnosed with emphysema, 94 percent are 45 or older. [2] Emphysema cases that are caused by other etiologies are referred to as secondary emphysema. [citation needed] Anything that causes the body to be unable to inhibit proteolytic enzymes occurring naturally in the lung can cause, or contribute to, the development of emphysema. This could include exposure to air pollution, second-hand smoke, and/or other chemicals and toxins.[3]
In rare cases, emphysema develops as a result of a genetic mutation that leads to alpha 1-antitrypsin deficiency. Severe cases of A1AD may also develop cirrhosis of the liver, where the accumulated abnormal A1AT leads to a fibrotic reaction that produces scarring and dysfunction; longstanding cirrosis may eventually produce liver cancer (hepatocellular carcinoma). The hereditary form of emphysema illustrates the detrimental effects that can result from misfolding of proteins in the endoplasmic reticulum (ER). This disease is caused by a point mutation in alpha1-antitrypsin, which normally is secreted by hepatocytes and macrophages. The wild-type protein binds to and inhibits trypsin and also the blood protease elastase. In the absence of alpha1-antitrypsin, elastase degrades the fine tissue in the lung that participates in the absorption of oxygen, eventually producing the symptoms of emphysema. Although the mutant alpha1-antitrypsin is synthesized in the rough ER, it does not fold properly, forming an almost crystalline aggregate that is not exported from the ER. In hepatocytes, the secretion of other proteins also becomes impaired, as the rough ER is filled with aggregated alpha1-antitrypsin.[4]
Some types of emphysema occur as a normal part of aging, and are commonly found in the oldest old (85 years of age and older). At about 20 years of age, humans stop developing new alveolar tissue. In the years following the cessation of development of new alveoli, lung tissue starts to deteriorate (on a "net" basis) at a relatively slow rate. This deterioration of lung capacity and function is a normal and natural part of aging in healthy people. As alveoli die, the number of lung capillaries decreases, and the elastin of the lungs begins to break down, causing a loss of pulmonary elasticity. As people age, they also tend to lose strength and mass in their chest muscles, which weaken, bones and cartilage start to deteriorate, and posture changes. Together, all of these age-related changes in respiratory system structures can cause or contribute to the development of emphysema. Though not all elderly people will develop clinically evident emphysema, they are all at risk of decreasing respiratory function, which limits maximum performance and produces discomfort at higher levels of exertion.
Pathophysiology

In normal breathing, air is drawn in through the bronchi and into the alveoli, which are tiny sacs surrounded by capillaries. Alveoli absorb oxygen and then transfer it into the blood. When toxins, such as cigarette smoke, are breathed into the lungs, the harmful particles become trapped in the alveoli, causing a localized inflammatory response. Chemicals released during the inflammatory response (e.g., elastase) can eventually cause the alveolar septum to disintegrate. This condition, known as septal rupture, leads to significant deformations of the lung architecture[5][6] (video) that have important functional consequences. The key mechanical event consequent to septal rupture is that the resulting cavity is larger than the sum of the two alveolar spaces (see figure); in fact because of the lacking mechanical support of the broken septa the lung elastic recoil further enlarges this new space, necessarily at the expenses of the surrounding healthy parenchyma. In other words, as an immediate and spontaneous consequence of septal rupture, the elastic lung recoil resets healthy parenchyma expansion at a lower level, in proportion to the amount of septal disruption. The large cavities left by the septal rupture are known as bullae. These deformations result in a large decrease of alveoli surface area used for gas exchange, as well as decreased ventilation of the surrounding healthy parenchyma. This results in a decreased Transfer Factor of the Lung for Carbon Monoxide (TLCO). To accommodate the decreased surface area, thoracic cage expansion (barrel chest) and diaphragm contraction (flattening) take place. Expiration, which physiologically depends completely on lung elastic recoil, increasingly depends on the thoracic cage and abdominal muscle action, particularly in the end expiratory phase. Due to decreased ventilation, the ability to exude carbon dioxide is significantly impaired. In the more serious cases, oxygen uptake is also impaired. As the alveoli continue to break down, hyperventilation is unable to compensate for the progressively shrinking surface area, and the body is not able to maintain high enough oxygen levels in the blood. The body's last resort is vasoconstricting appropriate vessels. This leads to pulmonary hypertension, which places increased strain on the right side of the heart, the side responsible for pumping deoxygenated blood to the lungs. The heart muscle thickens in order to pump more blood. This condition is often accompanied by the appearance of jugular venous distension. Eventually, as the heart continues to fail, it becomes larger and blood backs up in the liver.
People with alpha 1-antitrypsin deficiency (A1AD) are more likely to suffer from emphysema. A1AT inhibits inflammatory enzymes (such as elastase) from destroying the alveolar tissue. Most people with A1AD do not develop clinically significant emphysema, but smoking and severely decreased A1AT levels (10-15%) can cause emphysema at a young age. The type of emphysema caused by A1AD is known as panacinar emphysema (involving the entire acinus) as opposed to centrilobular emphysema, which is caused by smoking. Panacinar emphysema typically affects the lower lungs, while centrilobular emphysema affects the upper lungs. A1AD causes about 2% of all emphysema. Smokers with A1AD are at the greatest risk for emphysema. Mild emphysema can often develop into a severe case over a short period of time (1–2 weeks).
While A1AD provides some insight into the pathogenesis of the disease, hereditary A1AT deficiency only accounts for a small proportion of the disease. Studies for the better part of the past century have focused mainly upon the putative role of leukocyte elastase (also neutrophil elastase), a serine protease found in neutrophils, as a primary contributor to the connective tissue damage seen in the disease. This hypothesis, a result of the observation that neutrophil elastase is the primary substrate for A1AT, and A1AT is the primary inhibitor of neutrophil elastase, together have been known as the "protease-antiprotease" theory, implicating neutrophils as an important mediator of the disease. However, more recent studies have brought into light the possibility that one of the many other numerous proteases, especially matrix metalloproteases might be equally or more relevant than neutrophil elastase in the development of non-hereditary emphysema.
The better part of the past few decades of research into the pathogenesis of emphysema involved animal experiments where various proteases were instilled into the trachea of various species of animals. These animals developed connective tissue damage, which was taken as support for the protease-antiprotease theory. However, just because these substances can destroy connective tissue in the lung, as anyone would be able to predict, doesn't establish causality. More recent experiments have focused on more technologically advanced approaches, such as ones involving genetic manipulation. One particular development with respect to our understanding of the disease involves the production of protease "knock-out" animals, which are genetically deficient in one or more proteases, and the assessment of whether they would be less susceptible to the development of the disease. Often individuals who are unfortunate enough to contract this disease have a very short life expectancy, often 0–3 years at most.
Diagnosis
The diagnosis is usually confirmed by pulmonary function testing (e.g. spirometry or body plethysmography); however, X-ray radiography may aid in the diagnosis. Diffusing capacity of the lung for carbon monoxide (DLCO) may be tested to differentiate emphysema from other types of obstructive disorders such as chronic bronchitis and asthma. DLCO is a test that measures the ability of gases to diffuse across the alveolar-capillary membrane. DLCO will be decreased in emphysema, whereas it will be normal or increased in asthma and chronic bronchitis.
-
Micrograph demonstrating emphysema (left of image - large empty spaces) and lung tissue with relative preservation of the alveoli (right of image). H&E stain.
-
Axial CT image of the lung of a person with end-stage bullus emphysema.
-
A severe case of emphysema.
-
Lung bulla as seen on CXR in a person with severe COPD
Classification
Emphysema can be classified into primary and secondary types. However, it is more commonly classified by location into panacinary and centroacinary (or panacinar and centriacinar,[7] or centrilobular and panlobular).[8]
- Panacinar (or panlobular) emphysema: The entire respiratory lobule, from respiratory bronchiole to alveoli, has expanded. Occurs more commonly in the lower lobes (especially basal segments) and in the anterior margins of the lungs.[7]
- Centriacinar (or centrilobular) emphysema: The respiratory bronchiole (proximal and central part of the acinus) has expanded. The distal acinus or alveoli are unchanged. Occurs more commonly in the upper lobes.[7]
Other types include distal acinar emphysema and irregular emphysema.[7] A special type is congenital lobar emphysema (or CLE).
Congenital lobar emphysema

CLE results in overexpansion of a pulmonary lobe, and resultant compression of the remaining lobes of the ipsilateral lung (and possibly also the contralateral lung). There is bronchial narrowing because of weakened or absent bronchial cartilage.[9] There may be congenital extrinsic compression, commonly by an abnormally large pulmonary artery. This causes malformation of bronchial cartilage, making them soft and collapsible.[9] CLE is a potentially reversible (yet possibly life-threatening) cause of respiratory distress in the neonate.[9]
Paraseptal emphysema
Paraseptal emphysema is a type of emphysema which involves the alveolar ducts and sacs at the lung periphery. The emphysematous areas are subpleural in location and often surrounded by interlobular septa (hence the name). It may be an incidental finding in young adults, and may be associated with spontaneous pneumothorax. It may also be seen in older people with centrilobular emphysema. Both centrilobular and paraseptal emphysema may progress to bullous emphysema. A bulla is defined as being at least 1 cm in diameter, and with a wall less than 1mm thick. Bullae are thought to arise by air trapping in emphysematous spaces, causing local expansion.[10]
Management

Emphysema is an irreversible degenerative condition. It is recommended that people who think they may have the disease seek medical attention as soon as possible. The most important measure to slow its progression is for the person to stop smoking and avoid all exposure to cigarette smoke and lung irritants. Pulmonary rehabilitation can be very helpful to optimize the patient's quality of life and teach the patient how to actively manage his or her care.
Emphysema is also treated by supporting the breathing with anticholinergics, bronchodilators, steroid medication (inhaled or oral), effective body positioning (high Fowler's), and supplemental oxygen as required. Treating the patient's other conditions including gastric reflux and allergies may improve lung function. Supplemental oxygen used as prescribed (usually more than 20 hours per day) is the only non-surgical treatment which has been shown to prolong life in emphysema patients. There are lightweight portable oxygen systems which allow patients increased mobility. Patients can fly, cruise, and work while using supplemental oxygen. Other medications are being researched.
Lung volume reduction surgery (LVRS) can improve the quality of life for certain carefully selected patients. It can be done by different methods, some of which are minimally invasive. In July 2006 a new treatment, placing tiny valves in passages leading to diseased lung areas, was announced to have good results, but 7% of patients suffered partial lung collapse.
The only known "cure" for emphysema is lung transplant, but few patients are strong enough physically to survive the surgery. The combination of a patient's age, oxygen deprivation and the side-effects of the medications used to treat emphysema cause damage to the kidneys and other organs. Surgical transplantation also requires the patient to take an anti-rejection drug regimen which suppresses the immune system, and can lead to microbial infection of the patient.
Research
With the discovery of multipotent lung stem cells in 2011, a new treatment option may soon become available. Scientists injected human lung stem cells into mice with damaged lungs. The stem cells formed human bronchioles, alveoli, and pulmonary vessels integrated structurally and functionally with the damaged mouse organ. The May 2011 report in the New England Journal of Medicine [11] concluded that human lung stem cells "have the undemonstrated potential to promote tissue restoration in patients with lung disease".
Footnotes
- ^ emphysema at dictionary.com
- ^ Centers for Disease Control and Prevention. National Center for Health Statistics: National Health Interview Survey Raw Data, 2008. Analysis performed by American Lung Association Research and Program www.lung.org COPD-Fact-Sheet note 18
- ^ Takeshi Terashima, Maria E. Klut, Dean English, Jennifer Hards, James C. Hogg, and Stephan F. van Eeden (1990). "Cigarette Smoking Causes Sequestration of Polymorphonuclear Leukocytes Released from the Bone Marrow in Lung Microvessels" (PDF). AMERICAN JOURNAL OF RESPIRATORY CELL AND MOLECULAR BIOLOGY. 20: 171–177.
{{cite journal}}: line feed character in|title=at position 71 (help)CS1 maint: multiple names: authors list (link) - ^ Lodish et al - Molecular Cell Biology 5e (page: 675)
- ^ S. Nazari : Mechanical Events In Physiopathology Of Idiopathic Pulmonary Emphysema: A Theoretical Analysis. The Internet Journal of Thoracic and Cardiovascular Surgery. 2002 Volume 5 Number 2
- ^ Nazari S.The surgical physiopathology of essential pulmonary emphysema and volume-reduction intervention. Minerva Chir. 1998 Nov;53(11):899-918. PMID 9973794
- ^ a b c d "Emphysema". Retrieved 2008-11-20. Cite error: The named reference "urlEmphysema" was defined multiple times with different content (see the help page).
- ^ Anderson AE, Foraker AG (1973). "Centrilobular emphysema and panlobular emphysema: two different diseases". Thorax. 28 (5): 547–50. doi:10.1136/thx.28.5.547. PMC 470076. PMID 4784376.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c eMedicine Specialties > Radiology > Pediatrics --> Congenital Lobar Emphysema Author: Beverly P Wood, MD, MS, PhD, University of Southern California. Updated: December 1, 2008
- ^ Webb WR, Higgins CB. Thoracic Imaging. Lippincott, Williams & Wilkins 2005.
- ^ "Evidence for Human Lung Stem Cells". New England Journal of Medicine. Retrieved 07-12-2011.
{{cite web}}: Check date values in:|accessdate=(help)