Bowel resection: Difference between revisions
m moved pictures |
Expand cancer subsection |
||
| Line 43: | Line 43: | ||
== Medical Indications == |
== Medical Indications == |
||
| ⚫ | |||
=== Cancer === |
=== Cancer === |
||
| ⚫ | |||
[[Small intestine cancer|Small bowel]] or [[Colon Cancer|colon cancer]] may require surgical resection.<ref name=":1">{{Cite journal |last=Chen |first=Emerson Y. |last2=Vaccaro |first2=Gina M. |date=September 4, 2018 |title=Small Bowel Adenocarcinoma |url=https://pubmed.ncbi.nlm.nih.gov/30186048 |journal=Clinics in Colon and Rectal Surgery |volume=31 |issue=5 |pages=267–277 |doi=10.1055/s-0038-1660482 |issn=1531-0043 |pmc=6123009 |pmid=30186048}}</ref> |
[[Small intestine cancer|Small bowel]] or [[Colon Cancer|colon cancer]] may require surgical resection.<ref name=":1">{{Cite journal |last=Chen |first=Emerson Y. |last2=Vaccaro |first2=Gina M. |date=September 4, 2018 |title=Small Bowel Adenocarcinoma |url=https://pubmed.ncbi.nlm.nih.gov/30186048 |journal=Clinics in Colon and Rectal Surgery |volume=31 |issue=5 |pages=267–277 |doi=10.1055/s-0038-1660482 |issn=1531-0043 |pmc=6123009 |pmid=30186048}}</ref> |
||
Small bowel cancer often presents late in the course due to non-specific symptoms and has poor survival rates. Risk factors for small bowel cancer include genetically inherited polyposis syndromes, age over sixty years, and history of Crohn's or Celiac disease. Cases that present before stage IV show survival benefit from surgical resection with clear margins. It is recommended that surgical resection also include lymph node sampling of a minimum of 12 nodes with some groups extolling more extensive resection. When evaluation determines cancer to be stage IV, surgical intervention is no longer curative, and is only used for symptom relief.<ref name=":1" /> |
Small bowel cancer often presents late in the course due to non-specific symptoms and has poor survival rates. Risk factors for small bowel cancer include genetically inherited polyposis syndromes, age over sixty years, and history of Crohn's or Celiac disease. Cases that present before stage IV show survival benefit from surgical resection with clear margins. It is recommended that surgical resection also include lymph node sampling of a minimum of 12 nodes with some groups extolling more extensive resection. When evaluation determines cancer to be stage IV, surgical intervention is no longer curative, and is only used for symptom relief.<ref name=":1" /> |
||
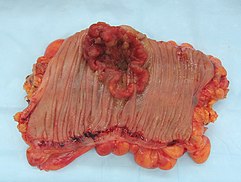
Colon cancer is the third most common cancer and the second most common cause of cancer death in the USA.<ref>{{Cite journal |last=Holt |first=Peter R. |last2=Kozuch |first2=Peter |last3=Mewar |first3=Seetal |date=2009 |title=Colon cancer and the elderly: from screening to treatment in management of GI disease in the elderly |url=https://pubmed.ncbi.nlm.nih.gov/19942166 |journal=Best Practice & Research. Clinical Gastroenterology |volume=23 |issue=6 |pages=889–907 |doi=10.1016/j.bpg.2009.10.010 |issn=1532-1916 |pmc=3742312 |pmid=19942166}}</ref> Due to its prevalence, screening protocols have been created for prevention of disease. Screening colonoscopies with or without polypectomy have been shown to decrease cancer morbidity and mortality.<ref name=":2">{{Cite journal |last=Freeman |first=Hugh James |date=2013-12-14 |title=Early stage colon cancer |url=https://pubmed.ncbi.nlm.nih.gov/24379564 |journal=World Journal of Gastroenterology |volume=19 |issue=46 |pages=8468–8473 |doi=10.3748/wjg.v19.i46.8468 |issn=2219-2840 |pmc=3870492 |pmid=24379564}}</ref> When cancer is more advanced and polypectomy is not possible surgical resection is necessary. Using imaging and pathologic evaluation of resected tissue the tumor may be staged using AJCC stages.<ref name=":2" /> Surgical resection of tumors for staging and for curative purposes requires removal of local blood vessel and lymph nodes. Standard lymph node resection includes three consecutive levels of lymph nodes and is known as a D3 lymphadenectomy.<ref>{{Cite journal |last=Okuno |first=Kiyotaka |date=2007 |title=Surgical treatment for digestive cancer. Current issues - colon cancer |url=https://pubmed.ncbi.nlm.nih.gov/17446704 |journal=Digestive Surgery |volume=24 |issue=2 |pages=108–114 |doi=10.1159/000101897 |issn=0253-4886 |pmid=17446704}}</ref> In addition to surgery adjuvant chemotherapy may be used to decrease risk of recurrence. Chemotherapy is standard with stage III cancer, case dependant in stage II and palliative in stage IV.<ref>{{Cite journal |last=Leichsenring |first=Jona |last2=Koppelle |first2=Adrian |last3=Reinacher-Schick |first3=Ank |date=2014-05 |title=Colorectal Cancer: Personalized Therapy |url=https://pubmed.ncbi.nlm.nih.gov/26676107 |journal=Gastrointestinal Tumors |volume=1 |issue=4 |pages=209–220 |doi=10.1159/000380790 |issn=2296-3774 |pmc=4668783 |pmid=26676107}}</ref>[[File:Gross pathology of small intestinal adenocarcinoma, serosal view.jpg|alt=small bowel stricture caused by cancer shown in resected segment of intestine.|thumb|216x216px|Bowel stricture]] |
|||
=== Bowel obstruction. === |
=== Bowel obstruction. === |
||
[[File:Gross pathology of small intestinal adenocarcinoma, serosal view.jpg|alt=small bowel stricture caused by cancer shown in resected segment of intestine.|thumb|216x216px|Bowel stricture]] |
|||
Bowel obstructions are commonly secondary to strictures, adhesions or cancer. |
Bowel obstructions are commonly secondary to strictures, adhesions or cancer. |
||
| Line 58: | Line 57: | ||
=== Perforation === |
=== Perforation === |
||
Perforation is an injury causing damage through the bowel wall and is can be due to trauma or [[peptic ulcer disease]] along with other etiologies. |
Perforation is an injury causing damage through the bowel wall and is can be due to trauma or [[peptic ulcer disease]] along with other etiologies.[[File:Ileus2.png|alt=Ischemic small bowel during open abdominal surgery.|thumb|Ischemic small bowel|179x179px]] |
||
=== Ischemia === |
=== Ischemia === |
||
[[File:Ileus2.png|alt=Ischemic small bowel during open abdominal surgery.|thumb|Ischemic small bowel|179x179px]] |
|||
Bowel ischemia is caused by decreased or absent blood flow through the Celiac, Superior Mesenteric, and Inferior Mesenteric arteries or any combination thereof. Untreated [[acute mesenteric ischemia]] can cause bowel [[necrosis]] in the affected area. This requires emergent surgery as survival without endovascular or operative intervention is around 50%. Ischemic bowel injury often requires multiple surgeries days apart to allow bowel recovery to increase odds of successful [[Anastomosis, surgical|anastomosis]].<ref name=":0">{{cite journal |last1=Bala |first1=Miklosh |last2=Kashuk |first2=Jeffry |last3=Moore |first3=Ernest E. |last4=Kluger |first4=Yoram |last5=Biffl |first5=Walter |last6=Gomes |first6=Carlos Augusto |last7=Ben-Ishay |first7=Offir |last8=Rubinstein |first8=Chen |last9=Balogh |first9=Zsolt J. |last10=Civil |first10=Ian |last11=Coccolini |first11=Federico |last12=Leppaniemi |first12=Ari |last13=Peitzman |first13=Andrew |last14=Ansaloni |first14=Luca |last15=Sugrue |first15=Michael |date=December 2017 |title=Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery |journal=World Journal of Emergency Surgery |volume=12 |issue=1 |pages=38 |doi=10.1186/s13017-017-0150-5 |pmid=28794797 |last16=Sartelli |first16=Massimo |last17=Di Saverio |first17=Salomone |last18=Fraga |first18=Gustavo P. |last19=Catena |first19=Fausto}}</ref> |
Bowel ischemia is caused by decreased or absent blood flow through the Celiac, Superior Mesenteric, and Inferior Mesenteric arteries or any combination thereof. Untreated [[acute mesenteric ischemia]] can cause bowel [[necrosis]] in the affected area. This requires emergent surgery as survival without endovascular or operative intervention is around 50%. Ischemic bowel injury often requires multiple surgeries days apart to allow bowel recovery to increase odds of successful [[Anastomosis, surgical|anastomosis]].<ref name=":0">{{cite journal |last1=Bala |first1=Miklosh |last2=Kashuk |first2=Jeffry |last3=Moore |first3=Ernest E. |last4=Kluger |first4=Yoram |last5=Biffl |first5=Walter |last6=Gomes |first6=Carlos Augusto |last7=Ben-Ishay |first7=Offir |last8=Rubinstein |first8=Chen |last9=Balogh |first9=Zsolt J. |last10=Civil |first10=Ian |last11=Coccolini |first11=Federico |last12=Leppaniemi |first12=Ari |last13=Peitzman |first13=Andrew |last14=Ansaloni |first14=Luca |last15=Sugrue |first15=Michael |date=December 2017 |title=Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery |journal=World Journal of Emergency Surgery |volume=12 |issue=1 |pages=38 |doi=10.1186/s13017-017-0150-5 |pmid=28794797 |last16=Sartelli |first16=Massimo |last17=Di Saverio |first17=Salomone |last18=Fraga |first18=Gustavo P. |last19=Catena |first19=Fausto}}</ref> |
||
Revision as of 17:26, 8 March 2023
| Bowel resection | |
|---|---|
 Drawing showing bowel resection for colon cancer | |
| Specialty | Gastroenterology |
A bowel resection or enterectomy (enter- + -ectomy) is a surgical procedure in which a part of an intestine (bowel) is removed, from either the small intestine or large intestine. Often the word enterectomy is reserved for the sense of small bowel resection, in distinction from colectomy, which covers the sense of large bowel resection. Bowel resection may be performed to treat gastrointestinal cancer, bowel necrosis, severe enteritis, diverticular disease, Crohn's disease, endometriosis, ulcerative colitis, or bowel obstruction due to scar tissue. Other reasons to perform bowel resection include traumatic injuries and to remove polyps when polypectomy is insufficient, either to prevent polyps from ever becoming cancerous or because they are causing or threatening bowel obstruction, such as in familial adenomatous polyposis, Peutz–Jeghers syndrome, or other polyposis syndromes.[1] Some patients require ileostomy or colostomy after this procedure as alternative means of excretion.[1] Depending on which part and how much of the intestines are removed, there may be digestive and metabolic challenges afterward, such as short bowel syndrome.
Types
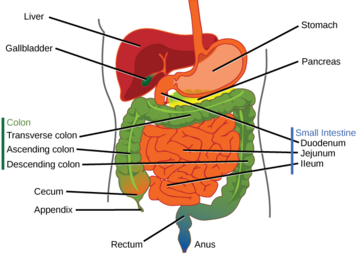
Types of enterectomy are named according to the relevant bowel segment:
| Procedure | Bowel segment | Notes |
|---|---|---|
| duodenectomy | duodenum | |
| Whipple | duodenum and Pancreas | |
| jejunectomy | jejunum | |
| ileectomy | ileum | |
| colectomy | colon |
Medical Indications
Cancer
Small bowel or colon cancer may require surgical resection.[2]
Small bowel cancer often presents late in the course due to non-specific symptoms and has poor survival rates. Risk factors for small bowel cancer include genetically inherited polyposis syndromes, age over sixty years, and history of Crohn's or Celiac disease. Cases that present before stage IV show survival benefit from surgical resection with clear margins. It is recommended that surgical resection also include lymph node sampling of a minimum of 12 nodes with some groups extolling more extensive resection. When evaluation determines cancer to be stage IV, surgical intervention is no longer curative, and is only used for symptom relief.[2]
Colon cancer is the third most common cancer and the second most common cause of cancer death in the USA.[3] Due to its prevalence, screening protocols have been created for prevention of disease. Screening colonoscopies with or without polypectomy have been shown to decrease cancer morbidity and mortality.[4] When cancer is more advanced and polypectomy is not possible surgical resection is necessary. Using imaging and pathologic evaluation of resected tissue the tumor may be staged using AJCC stages.[4] Surgical resection of tumors for staging and for curative purposes requires removal of local blood vessel and lymph nodes. Standard lymph node resection includes three consecutive levels of lymph nodes and is known as a D3 lymphadenectomy.[5] In addition to surgery adjuvant chemotherapy may be used to decrease risk of recurrence. Chemotherapy is standard with stage III cancer, case dependant in stage II and palliative in stage IV.[6]

Bowel obstruction.
Bowel obstructions are commonly secondary to strictures, adhesions or cancer.
Trauma
Traumatic injuries may cause bowel damage requiring surgery.
Perforation
Perforation is an injury causing damage through the bowel wall and is can be due to trauma or peptic ulcer disease along with other etiologies.

Ischemia
Bowel ischemia is caused by decreased or absent blood flow through the Celiac, Superior Mesenteric, and Inferior Mesenteric arteries or any combination thereof. Untreated acute mesenteric ischemia can cause bowel necrosis in the affected area. This requires emergent surgery as survival without endovascular or operative intervention is around 50%. Ischemic bowel injury often requires multiple surgeries days apart to allow bowel recovery to increase odds of successful anastomosis.[7]
See also
References
- ^ a b "Small bowel resection". MedlinePlus: U.S. National Library of Medicine. Retrieved 1 June 2013.
- ^ a b Chen, Emerson Y.; Vaccaro, Gina M. (September 4, 2018). "Small Bowel Adenocarcinoma". Clinics in Colon and Rectal Surgery. 31 (5): 267–277. doi:10.1055/s-0038-1660482. ISSN 1531-0043. PMC 6123009. PMID 30186048.
- ^ Holt, Peter R.; Kozuch, Peter; Mewar, Seetal (2009). "Colon cancer and the elderly: from screening to treatment in management of GI disease in the elderly". Best Practice & Research. Clinical Gastroenterology. 23 (6): 889–907. doi:10.1016/j.bpg.2009.10.010. ISSN 1532-1916. PMC 3742312. PMID 19942166.
- ^ a b Freeman, Hugh James (2013-12-14). "Early stage colon cancer". World Journal of Gastroenterology. 19 (46): 8468–8473. doi:10.3748/wjg.v19.i46.8468. ISSN 2219-2840. PMC 3870492. PMID 24379564.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Okuno, Kiyotaka (2007). "Surgical treatment for digestive cancer. Current issues - colon cancer". Digestive Surgery. 24 (2): 108–114. doi:10.1159/000101897. ISSN 0253-4886. PMID 17446704.
- ^ Leichsenring, Jona; Koppelle, Adrian; Reinacher-Schick, Ank (2014-05). "Colorectal Cancer: Personalized Therapy". Gastrointestinal Tumors. 1 (4): 209–220. doi:10.1159/000380790. ISSN 2296-3774. PMC 4668783. PMID 26676107.
{{cite journal}}: Check date values in:|date=(help) - ^ Bala, Miklosh; Kashuk, Jeffry; Moore, Ernest E.; Kluger, Yoram; Biffl, Walter; Gomes, Carlos Augusto; Ben-Ishay, Offir; Rubinstein, Chen; Balogh, Zsolt J.; Civil, Ian; Coccolini, Federico; Leppaniemi, Ari; Peitzman, Andrew; Ansaloni, Luca; Sugrue, Michael; Sartelli, Massimo; Di Saverio, Salomone; Fraga, Gustavo P.; Catena, Fausto (December 2017). "Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery". World Journal of Emergency Surgery. 12 (1): 38. doi:10.1186/s13017-017-0150-5. PMID 28794797.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
