Huntington's disease: Difference between revisions
→Physical: grammar |
Fixed missing space |
||
| Line 16: | Line 16: | ||
The name is derived from the physician [[George Huntington]] who described the disorder in 1872. In 1993 the gene causing HD was found, making it one of the first inherited [[genetic disorder]]s for which an accurate test could be performed. Because of this, and the disorder having aspects applicable to other neurological disorders such as [[Alzheimer's disease]], it has been extensively researched since then. |
The name is derived from the physician [[George Huntington]] who described the disorder in 1872. In 1993 the gene causing HD was found, making it one of the first inherited [[genetic disorder]]s for which an accurate test could be performed. Because of this, and the disorder having aspects applicable to other neurological disorders such as [[Alzheimer's disease]], it has been extensively researched since then. |
||
The gene causing the disorder is [[dominance relationship|dominant]] and may, therefore, be inherited from a single parent. Global incidence varies, from 3 to 7 per 100,000 people of Western European descent, down to 1 per 1,000,000 of Asian and African descent. The onset of physical symptoms in Huntington's disease occur in a large range around a [[arithmetic mean|mean]] of a person's late forties to early fifties. If symptoms become noticeable before a person is twenty, then their condition is known as'''Juvenile HD'''. |
The gene causing the disorder is [[dominance relationship|dominant]] and may, therefore, be inherited from a single parent. Global incidence varies, from 3 to 7 per 100,000 people of Western European descent, down to 1 per 1,000,000 of Asian and African descent. The onset of physical symptoms in Huntington's disease occur in a large range around a [[arithmetic mean|mean]] of a person's late forties to early fifties. If symptoms become noticeable before a person is twenty, then their condition is known as '''Juvenile HD'''. |
||
<!-- Note: Huntingtin protein and gene are correctly spelled with an 'i' in place of the 'o'. --> |
<!-- Note: Huntingtin protein and gene are correctly spelled with an 'i' in place of the 'o'. --> |
||
Revision as of 14:08, 27 June 2008
| Huntington's disease | |
|---|---|
| Specialty | Neurology |
| Frequency | 0.0123% (United Kingdom) |
Huntington's disease, also called Huntington's chorea, chorea major, or HD, is a genetic neurological disorder characterized by abnormal body movements called chorea and a lack of coordination; it also affects a number of mental abilities and some aspects of behavior. The name is derived from the physician George Huntington who described the disorder in 1872. In 1993 the gene causing HD was found, making it one of the first inherited genetic disorders for which an accurate test could be performed. Because of this, and the disorder having aspects applicable to other neurological disorders such as Alzheimer's disease, it has been extensively researched since then.
The gene causing the disorder is dominant and may, therefore, be inherited from a single parent. Global incidence varies, from 3 to 7 per 100,000 people of Western European descent, down to 1 per 1,000,000 of Asian and African descent. The onset of physical symptoms in Huntington's disease occur in a large range around a mean of a person's late forties to early fifties. If symptoms become noticeable before a person is twenty, then their condition is known as Juvenile HD.
Huntington's disease is one of several polyglutamine diseases caused by a trinucleotide repeat expansion. This expansion is in the Huntingtin gene, which normally codes for Huntingtin protein (Htt), producing mutant Huntingtin (mHtt). The presence of this protein increases the rate of neuron cell death in select areas of the brain, affecting certain neurological functions. The loss of neurons isn't fatal, but complications caused by symptoms reduce life expectancy. There is currently no proven cure, so symptoms are managed with a range of medications and supportive services.
Symptoms
Symptoms increase in severity progressively, but aren't often recognised until they reach certain stages. Physical symptoms are usually the first to cause problems and be noticed, but these are accompanied by cognitive and psychiatric ones which aren't often recognized. Almost everyone with Huntington's Disease eventually exhibits all physical symptoms, but cognitive symptoms vary, and so any psychopathological problems caused by these, also vary per individual. The symptoms of juvenile HD differ in that they generally progress faster and are more likely to exhibit rigidity and bradykinesia instead of chorea and often include seizures.[1]
Physical
The most characteristic symptoms are jerky, random, and uncontrollable movements called chorea, although sometimes very slow movement and stiffness (bradykinesia, dystonia) can occur instead or in later stages. These abnormal movements are initially exhibited as general lack of coordination, an unsteady gait and slurring of speech. As the disease progresses, any function that requires muscle control is affected, this causes reduced physical stability, abnormal facial expression, impaired speech comprehensibility, and difficulties chewing and swallowing. Eating difficulties commonly cause weight loss.[2][3] HD has been associated with sleep cycle disturbances, including insomnia and rapid eye movement sleep alterations.[4]
Counter intuitively, there may be some health benefits as carriers of the gene are hypothesized to have higher levels of the tumor suppressor protein p53 and a better than average immune system than non-carriers. As of April 2008, neither of these hypotheses have been supported by rigorous study.[5]
Cognitive
Selective cognitive abilities are progressively impaired, including executive function (planning, cognitive flexibility, abstract thinking, rule acquisition, initiating appropriate actions and inhibiting inappropriate actions), psychomotor function (slowing of thought processes to control muscles), perceptual and spatial skills of self and surrounding environment, selection of correct methods of remembering information (but not actual memory itself), short-term memory, and ability to learn new skills, depending on the pathology of the individual.
Psychopathological
Psychopathological symptoms vary more than cognitive and physical ones, and may include anxiety, depression, a reduced display of emotions (blunted affect) and decreased ability to recognize negative expressions like anger, disgust, fear or sadness in others,[6] egocentrism, aggression, and compulsive behavior. The latter can cause, or worsen, hypersexuality and addictions such as alcoholism and gambling.[citation needed]
Genetics
The gene involved in Huntington's disease, called Huntingtin (Htt), or Interesting Transcript 15 (IT15) gene, known historically as the HD gene, is located on the short arm of chromosome 4 (4p16.3). In the first part, called the 5' end of the gene, is a sequence of three DNA bases—cytosine-adenine-guanine (CAG)— repeated multiple times (i.e. ...CAGCAGCAG...) and known as a trinucleotide repeat. CAG is the genetic code for the amino acid glutamine; thus a series of CAG forms a chain of glutamine known as polyglutamine (polyQ).[7]
| Effect | classification | repeat count |
|---|---|---|
| unaffected | normal | < 27 |
| intermediate | 27 - 35 | |
| affected | Reduced Penetrance | 36 - 39 |
| Full Penetrance | > 39 |
A polyQ length of less than 36 glutamines produces a cytoplasmic protein called huntingtin protein (Htt), whereas a sequence of 36 or more produces an erroneous form of Htt, mHtt (standing for mutant Htt), this causes certain neurons, in select areas of the brain, to have an increased mortality. As the number of neurons reduces in these areas their functionality is impaired. Generally, the number of CAG repeats is related to the rate that these neurons die, affecting the age at onset and progression of symptoms.[8] Counts of 36-39 repeats result in later onset and slower progression of symptoms termed "reduced penetrance". No case of HD has been diagnosed with a count of less than 36.[9]
Inheritance
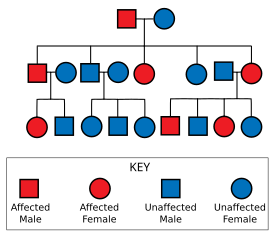
Huntington's disease is autosomal dominant, needing only one affected allele from either parent to inherit the disease. Although this generally means there is a one in two chance of inheriting the disorder from an affected parent, the inheritance of HD is more complex due to potential dynamic mutations, where DNA replication doesn't produce an exact copy of itself. This can cause the number of repeats to change in successive generations. This can mean that a parent with a count close to the threshold, may pass on a gene with a count either side of the threshold. Repeat counts maternally inherited are usually similar, whereas paternally inherited ones tend to increase.[10] This potential increase in repeats in successive generations is known as anticipation.
In families where neither parent has HD, new mutations account for truly sporadic cases of the disease. The frequency of these de novo mutations is extremely low.[11],[12]
Homozygous individuals, who carry two mutated genes because both parents passed on one, are rare. While HD seemed to be the first disease for which homozygotes did not differ in clinical expression or course from typical heterozygotes[13], more recent analysis suggest that homozygosity affects the phenotype and the rate of disease progression though it does not alter the age of onset[14] suggesting that the mechanisms underlying the onset and the progression are different.
Mechanism
Like all proteins, Htt and mHtt are translated, perform or affect biological functioning, and are finally dissolved in a process called biodegradation. The exact role mHtt has in DNA replication and its influence in programmed cell death is unknown. Research focuses on identifying the functioning of Htt, how mHtt differs or interferes with it, and the detrimental effects of remnants of mHtt left after biodegradation (Proteopathy).
Function
The Htt protein is involved in vesicle trafficking as it interacts with HIT1, a clathrin binding protein, to mediate endocytosis, the absorption of materials into a cell.[15][16]
The mHtt protein reduces the production of brain-derived neurotrophic factor (BDNF). BDNF protects neurons and regulates the neurogenesis of new ones. The precise way it does this is unknown but a reduction in its level increases neuron cell death and creation, leading to atrophy of areas of the brain.[17][18][19]
Degradation
Both Htt and mHtt are cleaved (the first step in degradation) by caspase-3, which removes the protein's amino end (the N-terminal).[20] Caspase-2 then further breaks down the amino terminal fragment (the part with the CAG repeat) of Htt, but cannot process all of the mHtt protein.[21] The unprocessed pieces left in the cell are called aggregates, or N-fragments, and are able to affect genetic transcription.[22] Specifically, mHtt binds with TAFII130, a coactivator to CREB dependent transcription.[23] The aggregates also interact with the transcription factor protein SP1, preventing it from binding to DNA.[24]
In transgenic mice neurodegeneration caused by mHtt is related to the caspase-6 enzyme cleaving the Htt protein, as they did not show effects of HD in experiments.[25]
In genetically altered "knockin" mice, the extended CAG repeat portion of the gene is all that is needed to cause disease.[26] Aggregates of mHtt are present in the brains of people and mice with HD,[27][28] and are most prevalent in cortical pyramidal neurons, less so in striatal medium-sized spiny neurons and almost absent in most other brain regions including the hippocampus and cerebellum.[27][29][30] These aggregates consist mainly of the amino terminal end of mHtt (CAG repeat), and are found in both the cytoplasm and nucleus of neurons.[31] The presence of these aggregates however does not correlate with cell death.[32] Thus mHtt acts in the nucleus but does not cause apoptosis through aggregation.[33]
Pathophysiology
Brain
Studies on physiopathology are mainly focused on the brain because most notable symptoms are related to it.
Profound neuronal degeneration in the striatum with some additional atrophy of the frontal and temporal cortices.[34] There is also astrogliosis[citation needed] and loss of medium spiny neurons.[35]
The brain initiates motion by sending a signal down the spinal cord from the external globus pallidus. At the same time that the stimulus is being sent down the spinal cord, the subthalamic nuclei of the striatum excite the internal globus pallidus, which inhibits the thalamus and modulates motion.[citation needed]
In Huntington's disease the external globus pallidus over-inhibits the flow of excitation from the subthalamic nuclei, which interferes with the initiation of motion. The subthalamic nuclei also generate reduced excitation to the internal globus pallidus, resulting in a weak inhibitory signal to the thalamus. The thalamus in turn then sends a strong excitatory signal to the putamen resulting in unmodulated motion.[citation needed]
Other systems
Huntington's disease appears to affect non nervous physiological functions. One study in humans highlighted a systemic, early hypermetabolic state and a lower level of branched chain amino acids in the plasma as the disease progresses;[36] this seems to originate from the brain's own need for energetic substrates.
In a murine model, heart restricted expression of amyloid-forming polyglutamine fragments resulted in heart failure.[37]
Diagnosis
To determine whether initial symptoms are evident, a physical and/or psychological examination is required. The uncontrollable movements are often the symptoms which cause initial alarm and lead to diagnosis; however, the disease may begin with cognitive or emotional symptoms, which are not always recognized. Pre-symptomatic testing is possible by means of a blood test which counts the number of repetitions in the gene. [citation needed]
A negative blood test means that the individual does not carry the expanded copy of the gene, will never develop symptoms, and cannot pass it on to children. A positive blood test means that the individual does carry the expanded copy of the gene, will develop the disease, and has a 50% chance of passing it on to children. A pre-symptomatic positive blood test is not considered a diagnosis, because it may be decades before onset.
Because of the ramifications on the life of an at-risk individual, with no cure for the disease and no proven way of slowing it, several counseling sessions are usually required before the blood test. Unless a child shows significant symptoms or is sexually active or considered to be Gillick competent, children under eighteen will not be tested. The members of the Huntington's Disease Society of America strongly encourage these restrictions in their testing protocol. A pre-symptomatic test is a life-changing event and a very personal decision. Embryonic screening is also possible, giving HD carriers or at-risk individuals the option of ensuring their children will not inherit the disease if abortion is acceptable to them. It is possible to test an embryo either in the womb (prenatal diagnosis) or to ensure a child will not have HD by utilising in vitro fertilisation and testing before implantation. [citation needed]
A full pathological diagnosis can only be established by a neurological examination's findings and/or demonstration of cell loss in the areas affected by HD, supported by a cranial CT or MRI scan findings.[citation needed]
Management
There is no treatment to fully arrest the progression of the disease, but symptoms can be reduced or alleviated through the use of medication and care methods. Huntington mice models exposed to better husbandry techniques, especially better access to food and water, lived much longer than mice that were not well cared for.[citation needed]
Medication
Other standard treatments to alleviate emotional symptoms include the use of antidepressants and sedatives, with antipsychotics (in low doses) for psychotic symptoms.[citation needed]
Therapies
Speech therapy helps by improving speech and swallowing methods; this therapy is more effective if started early on, as the ability to learn is reduced as the disease progresses. A two-year pilot study, of intensive speech, pyschiatric and physical therapy, applied to inpatient rehabilitation, showed motor decline was greatly reduced.[38]
Nutrition
Nutrition is an important part of treatment; most third and fourth stage HD sufferers need two to three times the calories of the average person to maintain body weight.[39] Healthier foods in pre-symptomatic and earlier stages may slow down the onset and progression of the disease. High calorie intake in pre-symptomatic and earlier stages has been shown to speed up the onset and reduce IQ level.[citation needed]
Thickening agent can be added to drinks as swallowing becomes more difficult, as thicker fluids are easier and safer to swallow. The option of using a stomach PEG is available when eating becomes too hazardous or uncomfortable; this greatly reduces the chances of aspiration of food, and the subsequent increased risk of pneumonia, and increases the amount of nutrients and calories that can be ingested.[citation needed]
EPA, an Omega-3 fatty acid, may slow and possibly reverse the progression of the disease.[40] As of April 2008, it is in FDA clinical trial as ethyl-EPA, (brand name Miraxion), for prescription use. Clinical trials utilise 2 grams per day of EPA. In the United States, it is available over the counter in lower concentrations in Omega-3 and fish oil supplements. Results of the first Phase III trial showed an improvement in motor function scores over the control group, but the small sample size render the result inconclusive. A larger trial is near completion and will be more statistically robust when results are posted.[citation needed]
Prognosis
Development of Huntington’s disease is highly dependent on how many times CAG is repeated. Usually, CAG is repeated between 7 and 35 times; more than this, however, will cause the disease.[41] The age of onset (and to a degree the severity of the disease) and hence the age at death, are inversely correlated with the length of the expanded CAG repeat, such that those with longer repeats develop the disease earlier. Individuals with greater than approximately 60 CAG repeats often develop juvenile Huntington's disease.[42] There is a large variation in age of onset for any given CAG repeat length within the intermediate range (40-50 CAGs). For example, a repeat length of 40 CAGs leads to an onset ranging from 40 to 70 years of age in the North American and Canadian population. This variation means that, although logarithmic algorithms have been proposed for predicting the age of onset,[43][44] in reality predicting the precise age of onset can be generalised, but not precisely predicted with confidence.
Following the onset of obvious physical diagnosis of the disorder, life expectancy is generally a further 15 to 20 years.[45] Mortality is not caused by Huntington’s disease directly, but by associated complications, these include pneumonia (which causes one third of fatalities), heart failure (although heart disease, cerebrovascular disease and atherosclerosis show no increase), choking and nutritional deficiencies.[46] Suicide is an associated risk, with suicide rates of up to 7.3 percent; four times that of the general population.[47][48] Suicide, in general, is likely to be underestimated; reports, which have accounted for this, estimate up to 27 percent of possibly affected individuals attempt suicide. [1]
Social impact
Whether or not to have the test for HD Genetic counseling may provide perspective for those at risk of the disease. Some choose not to undergo HD testing due to numerous concerns (for example, insurability). Testing of a descendant of a person, who is 'at-risk', has serious ethical implications as a positive result automatically diagnoses one of the parents.
Parents and grandparents have to decide when and how to tell their children and grandchildren. The issue of disclosure also comes up when siblings are diagnosed with the disease, and especially in the case of identical twins.
For those at risk, or known to have the disease, consideration is necessary prior to having children due to the genetically dominant nature of the disease. In vitro and embryonic genetic screening now make it possible (with 99 percent certainty) to have an HD-free child; however, the cost of this process can easily reach tens of thousands of dollars.[citation needed]
Huntington's disease was one of the targets of the eugenics movement, for example the American scientist Charles Davenport proposed in 1910 that compulsory sterilization and immigration control be used for people with certain disease, including HD.[49]
Financial institutions are also faced with the question of whether to use genetic testing results when assessing an individual, e.g. for life insurance. Some countries' organisations have already agreed not to use this information.[citation needed]
Epidemiology
As HD is autosomal dominant, and does not usually affect reproduction, areas of increased prevalence occur according to historical migration of carriers, some of which can be traced back thousands of years using the genes haplotypes.[50] New mutations are less than 10 percent of HD carriers, but account for the less localised occurrences, and origins, of the disorder.[51]
Since the discovery of a genetic test that can also be used pre-symptomatically, estimates of the incidence of the disorder are likely to increase. This is because, without the genetic test, only individuals displaying physical symptoms and a few neurologically examined cases were diagnosed, which excluded anyone who died of other causes before diagnosis. These cases can now be included in statistics as the test becomes more widely available.[citation needed]
The prevalence is, on average, between 3 to 7 per 100,000 people of Western European descent, down to 1 per 1,000,000 of Asian and African descent, but this varies greatly according to geographical location, both by ethnicity and local migration.[52] The highest occurrence is in peoples of Western Europe descent, and relatively lower in the rest of the world. For example the isolated populations of the Lake Maracaibo region of Venezuela ( where the marker for the gene was discovered ), have an extremely high prevalence of up to 700 per 100,000[53], leading to the conclusion that one of their initial founders must have been a carrier of the gene.This is known as the local founder effect.[54]
About 7 percent of HD cases occur in people under the age of 20 years. This is referred to as Juvenile HD, "akinetic-rigid", or "Westphal variant" HD. [55]
History
In the first part of the twentieth century and earlier, many people with HD were misdiagnosed as suffering from alcoholism or manic depression. Previously mortality due to starvation or dehydration was a major risk.
- c. 300: Along with other conditions with abnormal movements, it may have been referred to as St Vitus' dance. St Vitus is the patron saint of epileptics who was martyred in 303.
- Middle Ages: People with the condition were probably persecuted as being witches or as being possessed by spirits, and were shunned, exiled or worse. Some speculate that the "witches" in the Salem Witch Trials in 1692 had HD.[56]
- 1860: One of the early medical descriptions of HD was made in 1860 by a Norwegian district physician, Johan Christian Lund. He noted that in Setesdalen, a remote and rather secluded area, there was a high prevalence of dementia associated with a pattern of jerking movement disorders that tended to run in families. This is the reason for the disease being commonly referred to as Setesdalsrykkja (Setesdalen=the location, rykkja=jerking movements) in Norwegian.
- 1872: George Huntington was the third generation of a family medical practice in Long Island. With their combined experience of several generations of a family with the same symptoms, he realised their conditions were linked and set about describing it. A year after leaving medical school, in 1872, he presented his accurate definition of the disease to a medical society in Middleport, Ohio.
- c. 1923: Smith Ely Jelliffe (1866–1945) and Frederick Tilney (1875–1938) began analyzing the history of HD sufferers in New England.
- 1932: P. R. Vessie expanded Jelliffe and Tilney's work, tracing about a thousand people with HD back to two brothers and their families who left Bures in Essex for Suffolk bound for Boston in 1630.
- 1979: The U.S-Venezuela Huntington's Disease Collaborative Research Project began an extensive study which gave the basis for the gene to be discovered. This was conducted in the small and isolated Venezuelan fishing villages of Barranquitas and Lagunetas. Families there have a high presence of the disease.
- 1983: James Gusella, David Housman, P. Michael Conneally, Nancy Wexler, and their colleagues find the general location of the gene, using DNA marking methods for the first time — an important first step toward the Human Genome Project.
- 1992: Anita Harding, et al., find that trinucleotide repeats affect disease severity[57]
- 1993: The Huntington's Disease Collaborative Research Group isolates the precise gene at 4p16.3.
- 1996: A transgenic mouse (the R6 line) was created that could be made to exhibit HD, greatly advancing how much experimentation can be achieved.
- 1997: DiFiglia M, Sapp E, Chase KO, et al., discover that mHtt aggregates (misfolds) to form nuclear inclusions.[27]
- The full record of research is extensive.[58][59][60]
Society and culture
As public awareness has increased, HD has been depicted increasingly in numerous books, films and TV series. Early works were Arlo Guthrie's 1969 film Alice's Restaurant and Jacqueline Susann's 1966 American novel Valley of the Dolls , with more recent references in ER, Private Practice, Everwood, All Saints, and House. As of 2008, June 6th is designated "National Huntington's Disease Awareness Day" by the USA senate, and the UK HDA holds an awareness week the third week of June.[61]
Organizations
- 1967: Woody Guthrie's wife, Marjorie, helped found the Committee to Combat Huntington's Disease, after his death from HD complications. This eventually became the Huntington's Disease Society of America.[62] Since then, lay organizations have been formed in many countries around the world.
- 1968: After experiencing HD in his wife's family Dr. Milton Wexler was inspired to start the Hereditary Disease Foundation (HDF). Professor Nancy S. Wexler, Dr. Wexler's daughter, was in the research team in Venezuela and is now president of the HDF.
- 1974: The first international meeting took place when the founders of the Canadian HD Society (Ralph Walker) and of the British HD Society (Mauveen Jones) attended the annual meeting of the American HD Society.
- 1977: second meeting organized by the Dutch Huntington Society the "Vereniging van Huntington", representatives of six countries were present.
- 1979: International Huntington Association (IHA) formed during international meeting in Oxford, England organized by HDA of England.
- 1981–2001: Biennial meetings held by IHA which became the World Congress on HD.
- 2003: The first World Congress on Huntington's Disease was held in Toronto.[63] This is a biennial meeting for associations and researchers to share ideas and research, which is held on odd-number years. The Euro-HD Network[64] was started as part of the Huntington Project,[65] funded by the High-Q Foundation.[66]
Research directions
Appropriate animal models are critical for understanding the fundamental mechanisms causing the disease and for supporting the early steps of drug development before moving on to human clinical trials. Neurochemically induced mice or monkeys were first available[67] [68], but they could not mimick the progressive features of the disease. After the HD gene was discovered, transgenic animals exhibiting HD were generated by inserting a CAG repeat expansion into the genome of mice (strain R6/2[69] [70]), Drosophila fruit flies[71], or more recently in monkeys[72]. Expression without insertion of a CAG repeat in nematode worms[73] also produced a valuable model.
As for humans, there are trials of various compounds that are in development, recruiting volunteers[74], in progress or completed. Some of these trials are at the point of testing on larger numbers of people, known as phase III of the clinical trials.
Intrabody therapy
Genetically engineered antibody fragments called intrabodies have shown therapeutic results against mHtt aggregates in drosophila models. This was achieved using an intrabody called C4 sFv, a single chain variable fragment which binds to the end of mHtt within a cell. C4 sFv has been shown to reduce mHtt aggregate formation and accumulation in cultures of tissue taken from the model.[75][76] The intrabody increased larval and pupal survival from 23% to 100% and delayed neurodegeneration in the adult, significantly increasing their lifespan.[77] Intrabody therapy shows promise as a tool for drug discovery, and as a potential therapy for neurodegenerative disorders caused by protein mis-folding or abnormal protein interactions.[78]
Gene silencing
Since HD has been conclusively linked to a single gene, gene silencing could be simpler than with multiple-gene disorders. Researchers have investigated using gene knockdown of mHtt as a potential treatment. Using a mouse model, siRNA therapy achieved a 60 percent reduction in expression of the mHtt and progression of the disease was stalled.[79] However, this study used the human form of the Htt gene in the mouse, and were therefore able to directly target the mHtt gene, leaving endogenous, wild-type Htt gene expression unaffected. Since no single nucleotide polymorphisms have yet been discovered in mHtt it would be impossible, using siRNA, to distinguish between wild-type and mutant forms of the gene. The precise function of Htt is unknown, but the htt knockout mutation is lethal and kills mice during emryogenesis[80]. Thus, using RNA interference to knockout both wild-type and mutant htt could have unforseen, unfavourable consequences. (This is distinct from the other problems associated with using siRNA as a therapy, e.g. delivering the gene; off-target effects of siRNA; toxicity from shRNA over-expression [81].)
In another study, mouse models in late stages of the disease recovered motor function after expression of mHtt was shut down.[82]
Stem cell implants
Treatment using stem cell implants is based on the replacement of damaged neurons by injecting stem cells, which can form themselves into specialized cells, into the damaged area. The stem cell then transforms itself into a replacement neuron. If enough damaged neurons are replaced, symptoms should be alleviated. This treatment would not prevent further neuronal damage, so would be an ongoing treatment. The treatment has yielded some positive results in animal models.[83]
Others
Other agents and measures that have shown promise in initial experiments include dopamine receptor blockers, select dopamine antagonists, such as tetrabenazine, creatine, CoQ10, the antibiotic Minocycline, exercise, antioxidant-containing foods and nutrients, and antidepressants (notably, but not exclusively, selective serotonin reuptake inhibitors SSRIs, such as sertraline, fluoxetine, and paroxetine).[citation needed]
References
- ^ a b Kremer B. Clinical neurology of Huntington's disease. In: Huntington's Disease (Third ed.), edited by Bates GP, Harper PS and Jones L. Oxford: Oxford University Press, 2002, p. 28-61.
- ^ Gaba AM, Zhang K, Marder K, Moskowitz CB, Werner P, Boozer CN (2005). "Energy balance in early-stage Huntington disease". Am. J. Clin. Nutr. 81 (6): 1335–41. PMID 15941884.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Caregiver's Handbook for Advanced-Stage Huntington Disease. Booklet by the Huntington Society of Canada, retrieved 2007-04-11.
- ^ Arnulf I, Nielsen J, Lohmann E, Schieffer J, Wild E, Jennum P, Konofal E, Walker M, Oudiette D, Tabrizi S, Durr A (2008). "Rapid eye movement sleep disturbances in Huntington disease". Arch Neurol. 65 (4): 482–488. PMID 18413470.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Eskenazi BR, Wilson-Rich NS, Starks PT (2007). "A Darwinian approach to Huntington's disease: Subtle health benefits of a neurological disorder". Med. Hypotheses. 69 (6): 1183–9. doi:10.1016/j.mehy.2007.02.046. PMID 17689877.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Johnson SA, Stout JC, Solomon AC; et al. (2007). "Beyond disgust: Impaired recognition of negative emotions prior to diagnosis in Huntington's disease". Brain. 130 (Pt 7): 1732–44. doi:10.1093/brain/awm107. PMID 17584778.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Katsuno M, Banno H, Suzuki K; et al. (2008). "Molecular genetics and biomarkers of polyglutamine diseases". Curr. Mol. Med. 8 (3): 221–34. PMID 18473821.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kieburtz K, MacDonald M, Shih C; et al. (1994). "Trinucleotide repeat length and progression of illness in Huntington's disease". J. Med. Genet. 31 (11): 872–4. PMID 7853373.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Chong, S.S., Almqvist, E., Telenius, et al: (1997). Contribution of DNA sequence and CAG size to mutation frquences of intermediate alleles for Huntington Disease: Evidence from single sperm analyses. Human Molecular Genetics 6:302-309
- ^ RM Ridley, CD Frith, TJ Crow and PM Conneally (1988). "Anticipation in Huntington's disease is inherited through the male line but may originate in the female". Journal of Medical Genetics. 25: 589–595. PMID 2972838.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Myers; et al. (1993). "De novo expansion of a (CAG)n repeat in sporadic Huntington's disease". Nature Genetics. 5: 168–173. doi:doi:10.1038/ng1093-168.
{{cite journal}}: Check|doi=value (help); Explicit use of et al. in:|author=(help) - ^ Sánchez A, Milà M, Castellví-Bel S, Rosich M, Jiménez D, Badenas C, Estivill X. (1997). "Maternal transmission in sporadic Huntington's disease". J Neurol Neurosurg Psychiatry. 62 (5): 535–537. PMID 9153618.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wexler NS, Young AB, Tanzi RE; et al. (1987). "Homozygotes for Huntington's disease". Nature. 326 (6109): 194–197. doi:10.1038/326194a0. PMID 2881213.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Squitieri F, Gellera C, Cannella M, Mariotti C, Cislaghi G, Rubinsztein DC, Almqvist EW, Turner D, Bachoud-Lévi AC, Simpson SA, Delatycki M, Maglione V, Hayden MR, Donato SD (2003). "Homozygosity for CAG mutation in Huntington disease is associated with a more severe clinical course". Brain. 126 (4): 946–955. PMID 12615650.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Velier J, Kim M, Schwarz C; et al. (1998). "Wild-type and mutant huntingtins function in vesicle trafficking in the secretory and endocytic pathways". Exp. Neurol. 152 (1): 34–40. doi:10.1006/exnr.1998.6832. PMID 9682010.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Waelter S, Scherzinger E, Hasenbank R; et al. (2001). "The huntingtin interacting protein HIP1 is a clathrin and alpha-adaptin-binding protein involved in receptor-mediated endocytosis". Hum. Mol. Genet. 10 (17): 1807–17. doi:10.1093/hmg/10.17.1807. PMID 11532990.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Canals JM, Pineda JR, Torres-Peraza JF; et al. (2004). "Brain-derived neurotrophic factor regulates the onset and severity of motor dysfunction associated with enkephalinergic neuronal degeneration in Huntington's disease". J. Neurosci. 24 (35): 7727–39. doi:10.1523/JNEUROSCI.1197-04.2004. PMID 15342740.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Sawa A, Nagata E, Sutcliffe S; et al. (2005). "Huntingtin is cleaved by caspases in the cytoplasm and translocated to the nucleus via perinuclear sites in Huntington's disease patient lymphoblasts". Neurobiol. Dis. 20 (2): 267–74. doi:10.1016/j.nbd.2005.02.013. PMID 15890517.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Strand AD, Baquet ZC, Aragaki AK; et al. (2007). "Expression profiling of Huntington's disease models suggests that brain-derived neurotrophic factor depletion plays a major role in striatal degeneration". J. Neurosci. 27 (43): 11758–68. doi:10.1523/JNEUROSCI.2461-07.2007. PMID 17959817.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kim YJ, Yi Y, Sapp E; et al. (2001). "Caspase 3-cleaved N-terminal fragments of wild-type and mutant huntingtin are present in normal and Huntington's disease brains, associate with membranes, and undergo calpain-dependent proteolysis". Proc. Natl. Acad. Sci. U.S.A. 98 (22): 12784–9. doi:10.1073/pnas.221451398. PMID 11675509.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Hermel E, Gafni J, Propp SS; et al. (2004). "Specific caspase interactions and amplification are involved in selective neuronal vulnerability in Huntington's disease". Cell Death Differ. 11 (4): 424–38. doi:10.1038/sj.cdd.4401358. PMID 14713958.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Freiman RN, Tjian R (2002). "Neurodegeneration. A glutamine-rich trail leads to transcription factors". Science. 296 (5576): 2149–50. doi:10.1126/science.1073845. PMID 12077389.
- ^ Bae BI, Xu H, Igarashi S; et al. (2005). "p53 mediates cellular dysfunction and behavioral abnormalities in Huntington's disease". Neuron. 47 (1): 29–41. doi:10.1016/j.neuron.2005.06.005. PMID 15996546.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Dunah AW, Jeong H, Griffin A; et al. (2002). "Sp1 and TAFII130 transcriptional activity disrupted in early Huntington's disease". Science. 296 (5576): 2238–43. doi:10.1126/science.1072613. PMID 11988536.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Graham RK, Deng Y, Slow EJ; et al. (2006). "Cleavage at the caspase-6 site is required for neuronal dysfunction and degeneration due to mutant huntingtin". Cell. 125 (6): 1179–91. doi:10.1016/j.cell.2006.04.026. PMID 16777606.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Murphy KP, Carter RJ, Lione LA; et al. (2000). "Abnormal synaptic plasticity and impaired spatial cognition in mice transgenic for exon 1 of the human Huntington's disease mutation". J. Neurosci. 20 (13): 5115–23. PMID 10864968.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ a b c DiFiglia M, Sapp E, Chase KO; et al. (1997). "Aggregation of huntingtin in neuronal intranuclear inclusions and dystrophic neurites in brain". Science. 277 (5334): 1990–3. doi:10.1126/science.277.5334.1990. PMID 9302293.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Davies SW, Turmaine M, Cozens BA; et al. (1997). "Formation of neuronal intranuclear inclusions underlies the neurological dysfunction in mice transgenic for the HD mutation". Cell. 90 (3): 537–48. doi:10.1016/S0092-8674(00)80513-9. PMID 9267033.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Gutekunst CA, Li SH, Yi H; et al. (1999). "Nuclear and neuropil aggregates in Huntington's disease: Relationship to neuropathology". J. Neurosci. 19 (7): 2522–34. PMID 10087066.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Sieradzan KA, Mechan AO, Jones L; et al. (1999). "Huntington's disease intranuclear inclusions contain truncated, ubiquitinated huntingtin protein". Exp. Neurol. 156 (1): 92–9. doi:10.1006/exnr.1998.7005. PMID 10192780.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Cooper JK, Schilling G, Peters MF; et al. (1998). "Truncated N-terminal fragments of huntingtin with expanded glutamine repeats form nuclear and cytoplasmic aggregates in cell culture". Hum. Mol. Genet. 7 (5): 783–90. doi:10.1093/hmg/7.5.783. PMID 9536081.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Fusco FR, Chen Q, Lamoreaux WJ; et al. (1999). "Cellular localization of huntingtin in striatal and cortical neurons in rats: Lack of correlation with neuronal vulnerability in Huntington's disease". J. Neurosci. 19 (4): 1189–202. PMID 9952397.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Saudou F, Finkbeiner S, Devys D, Greenberg ME (1998). "Huntingtin acts in the nucleus to induce apoptosis but death does not correlate with the formation of intranuclear inclusions". Cell. 95 (1): 55–66. doi:10.1016/S0092-8674(00)81782-1. PMID 9778247.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Purves, Dale. "Modulation of Movement by the Basal Ganglia - Box A. Huntington's Disease". In Dale Purves (ed.). Neuroscience (2nd edition ed.). Sunderland, MA: Sinauer Associates. ISBN 0-87893-742-0. Retrieved 2008-06-10.
{{cite book}}:|edition=has extra text (help); Cite has empty unknown parameter:|origdate=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Purves, Dale. "Modulation of Movement by the Basal Ganglia - Circuits within the Basal Ganglia System". In Dale Purves (ed.). Neuroscience (2nd edition ed.). Sunderland, MA: Sinauer Associates. ISBN 0-87893-742-0. Retrieved 2008-06-10.
{{cite book}}:|edition=has extra text (help); Cite has empty unknown parameter:|origdate=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Mochel F, Charles P, Seguin F, Barritault J, Coussieu C, Perin L, Le Bouc Y, Gervais C, Carcelain G, Vassault A, Feingold J, Rabier D, Durr A (2007). "Early energy deficit in Huntington disease: identification of a plasma biomarker traceable during disease progression". PLoS ONE. 2 (7). PMID 17653274.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pattison JS, Sanbe A, Maloyan A, Osinska H, Klevitsky R, Robbins J (2008). "Cardiomyocyte Expression of a Polyglutamine Preamyloid Oligomer Causes Heart Failure". Circulation. PMID 18490523.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Zinzi P, Salmaso D, De Grandis R; et al. (2007-Jul-21). "Effects of an intensive rehabilitation programme on patients with Huntington's disease: A pilot study". Clin Rehabil. 2007 Jul;21(7):603-13.
{{cite web}}: Check date values in:|date=(help); Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Gaba, Anna. "Family Guide Series - Nutrition and Huntington's Disease". Huntington's Disease Society of America Publications. Retrieved 2008-04-02.
- ^ Huntington's Disease Reversed
- ^ Andrew SE, Goldberg YP, Kremer B; et al. (1993). "The relationship between trinucleotide (CAG) repeat length and clinical features of Huntington's disease". Nat. Genet. 4 (4): 398–403. doi:10.1038/ng0893-398. PMID 8401589.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Harper PS (1999). "Huntington's disease: A clinical, genetic and molecular model for polyglutamine repeat disorders". Philos. Trans. R. Soc. Lond., B, Biol. Sci. 354 (1386): 957–61. doi:10.1098/rstb.1999.0446. PMID 10434293.
- ^ Rubinsztein DC, Leggo J, Chiano M; et al. (1997). "Genotypes at the GluR6 kainate receptor locus are associated with variation in the age of onset of Huntington disease". Proc. Natl. Acad. Sci. U.S.A. 94 (8): 3872–6. doi:10.1073/pnas.94.8.3872. PMID 9108071.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Adams P, Falek A, Arnold J (1988). "Huntington disease in Georgia: Age at onset". Am. J. Hum. Genet. 43 (5): 695–704. PMID 2973230.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Roos RA, Hermans J, Vegter-van der Vlis M; et al. (1993). "Duration of illness in Huntington's disease is not related to age at onset". J. Neurol. Neurosurg. Psychiatr. 56 (1): 98–100. PMID 8429330.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Lanska DJ, Lanska MJ, Lavine L, Schoenberg BS (1988). "Conditions associated with Huntington's disease at death. A case-control study". Arch. Neurol. 45 (8): 878–80. PMID 2969233.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Di Maio L, Squitieri F, Napolitano G; et al. (1993). "Suicide risk in Huntington's disease". J. Med. Genet. 30 (4): 293–5. PMID 8487273.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Schoenfeld M, Myers RH, Cupples LA; et al. (1984). "Increased rate of suicide among patients with Huntington's disease". J. Neurol. Neurosurg. Psychiatr. 47 (12): 1283–7. PMID 6239910.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ [1]
- ^ Squitieri F, Andrew SE, Goldberg YP; et al. (1994). "DNA haplotype analysis of Huntington disease reveals clues to the origins and mechanisms of CAG expansion and reasons for geographic variations of prevalence". Hum. Mol. Genet. 3 (12): 2103–14. doi:10.1093/hmg/3.12.2103. PMID 7881406.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ García-Planells J, Burguera JA, Solís P; et al. (2005). "Ancient origin of the CAG expansion causing Huntington disease in a Spanish population". Hum. Mutat. 25 (5): 453–9. doi:10.1002/humu.20167. PMID 15832309.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ NCBI OMIM. "Huntington's Disease". Retrieved 2008-05-22.
- ^ R. Avila-Giron Medical and Social Aspects of Huntington's Chorea in the State of Zulia, Venezuela in: Advances in Neurology, Vol 1 (eds A. Barbeau, T.N. Chase and G.W. Paulson) New York: Raven Press, 1973, pp. 261-266
- ^ Gusella JF, Wexler NS, Conneally PM; et al. (1983). "A polymorphic DNA marker genetically linked to Huntington's disease". Nature. 306 (5940): 234–8. doi:10.1038/306234a0. PMID 6316146.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Nance MA, Myers RH (2001). "Juvenile onset Huntington's disease--clinical and research perspectives". Ment Retard Dev Disabil Res Rev. 7 (3): 153–7. doi:10.1002/mrdd.1022. PMID 11553930.
- ^ The brief history of HD on stanford.edu
- ^ La Spada AR, Roling DB, Harding AE; et al. (1992). "Meiotic stability and genotype-phenotype correlation of the trinucleotide repeat in X-linked spinal and bulbar muscular atrophy". Nat. Genet. 2 (4): 301–4. doi:10.1038/ng1292-301. PMID 1303283.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Achievements of Hereditary Disease Foundation
- ^ HDA research news—medical research into treatment & prevention on hda.org.uk
- ^ Bates G, Harper PS, Jones L (2002) Huntington's disease, 3rd Edition. Oxford: Oxford University Press.
- ^ [2]
- ^ Huntington's Disease Society of America
- ^ World Congress on Huntington's Disease
- ^ Euro-HD Network
- ^ Huntington Project
- ^ High-Q Foundation
- ^ Beal MF, Kowall NW, Ellison DW, Mazurek MF, Swartz KJ, Martin JB (1986). "Replication of the neurochemical characteristics of Huntington's disease by quinolinic acid". Nature. 321 (321): 168–171. doi:10.1038/321168a0.
{{cite journal}}: Cite has empty unknown parameter:|month=(help)CS1 maint: multiple names: authors list (link) - ^ Brouillet E, Hantraye P, Ferrante RJ, Dolan R, Leroy-Willig A, Kowall NW, Beal MF (1995). "Chronic mitochondrial energy impairment produces selective striatal degeneration and abnormal choreiform movements in primates". Proc Natl Acad Sci USA. 92: 7105–7109. doi:10.1073/pnas.92.15.7105. PMID 7624378.
{{cite journal}}: Cite has empty unknown parameter:|month=(help)CS1 maint: multiple names: authors list (link) - ^ Mangiarini L, Sathasivam K, Seller M, Cozens B, Harper A, Hetherington C, Lawton M, Trottier Y, Lehrach H, Davies SW, Bates GP (1996). "Exon 1 of the HD gene with an expanded CAG repeat is sufficient to cause a progressive neurological phenotype in transgenic mice". Cell. 87 (3): 493–506. doi:10.1016/S0092-8674(00)81369-0. PMID 8898202.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Carter RJ, Lione LA, Humby T, Mangiarini L, Mahal A, Bates GP, Dunnett SB, and Morton AJ (1999). "Characterization of Progressive Motor Deficits in Mice Transgenic for the Human Huntington's Disease Mutation". The Journal of Neuroscience. 19 (8): 3248–3257. PMID 10191337.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Marsh JL, Pallos J and Thompson LM (2003). "Fly models of Huntington's disease". Human Molecular Genetics. 12 (2): 187–193. doi:10.1093/hmg/ddg271. PMID 12925571.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ First Transgenic Monkey Model Of Huntington's Disease Developed Science Daily article on HD monkey model, May 19, 2008.
- ^ Voisine C, Varma H, Walker N, Bates EA, Stockwell BR, and Hart AC (2007). "Identification of Potential Therapeutic Drugs for Huntington's Disease using Caenorhabditis elegans". PLoS ONE. 2 (6): e504. doi:10.1371/journal.pone.0000504. PMID 1876812.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Trials for Huntington's disease at clinicaltrials.gov
- ^ Lecerf JM, Shirley TL, Zhu Q; et al. (2001). "Human single-chain Fv intrabodies counteract in situ huntingtin aggregation in cellular models of Huntington's disease". Proc. Natl. Acad. Sci. U.S.A. 98 (8): 4764–9. doi:10.1073/pnas.071058398. PMID 11296304.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Miller TW, Zhou C, Gines S; et al. (2005). "A human single-chain Fv intrabody preferentially targets amino-terminal Huntingtin's fragments in striatal models of Huntington's disease". Neurobiol. Dis. 19 (1–2): 47–56. doi:10.1016/j.nbd.2004.11.003. PMID 15837560.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Wolfgang WJ, Miller TW, Webster JM; et al. (2005). "Suppression of Huntington's disease pathology in Drosophila by human single-chain Fv antibodies". Proc. Natl. Acad. Sci. U.S.A. 102 (32): 11563–8. doi:10.1073/pnas.0505321102. PMID 16061794.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Miller TW, Messer A (2005). "Intrabody applications in neurological disorders: Progress and future prospects". Mol. Ther. 12 (3): 394–401. doi:10.1016/j.ymthe.2005.04.003. PMID 15964243.
- ^ Harper SQ, Staber PD, He X; et al. (2005). "RNA interference improves motor and neuropathological abnormalities in a Huntington's disease mouse model". Proc. Natl. Acad. Sci. U.S.A. 102 (16): 5820–5. doi:10.1073/pnas.0501507102. PMID 15811941.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Jamal Nasira; et al. (1995). "Targeted disruption of the Huntington's disease gene results in embryonic lethality and behavioral and morphological changes in heterozygotes". Cell. 81 (5): 811–23. doi:10.1016/0092-8674(95)90542-1.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Jodi L. McBride; et al. "Artificial miRNAs mitigate shRNA-mediated toxicity in the brain: Implications for the therapeutic development of RNAi". PNAS. 105 (15): 5868–5873. doi:10.1073/pnas.0801775105.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Miguel Díaz-Hernández, Jesús Torres-Peraza, Alejandro Salvatori-Abarca; et al. (October 19, 2005). "Full Motor Recovery Despite Striatal Neuron Loss and Formation of Irreversible Amyloid-Like Inclusions in a Conditional Mouse Model of Huntington's Disease". The Journal of Neuroscience. 25 (42): 9773–9781. doi:10.1523/JNEUROSCI.3183-05.2005. PMID 16237181.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ "Pig cell implants in Huntington's trial". WorldHealth.net. Retrieved 2008-05-15.
Sources
- Conomy, John P., M.D., J.D. "Dr. George Sumner Huntington and the Disease Bearing His Name".
{{cite web}}: CS1 maint: multiple names: authors list (link) - Huntington, G. (1872-04-13). "On Chorea". Medical and Surgical Reporter of Philadelphia. 26 (15): 317–321.
- Online Mendelian Inheritance in Man, Article 143100 - Huntington Disease, Johns Hopkins University
- Online Mendelian Inheritance in Man, Article 606438 - Huntingtons Disease-Like 2, Johns Hopkins University
- Stevenson, Charles S. (1934). "A Biography of George Huntington, M.D." (Microsoft Word). Bulletin of the Institute of the History of Medicine. II (2). Johns Hopkins University. Retrieved 2007-12-05.
{{cite journal}}: Unknown parameter|month=ignored (help) - Vessie, P. R. (1932). "On the transmission of Huntington's chorea for 300 years—the Bures family group". Journal of Nervous and Mental Disease, Baltimore. 76: 553–573.
Bibliography
- Gillian Bates, Peter Harper, and Lesley Jones (2002). Huntington's Disease - Third Edition. Oxford: Oxford University Press. ISBN 0-19-851060-8.
{{cite book}}: CS1 maint: multiple names: authors list (link)
External links
DMOZ HD links directory at the Open Directory Project.
Professional and research
- Huntington Project - worldwide umbrella organization for the clinical research efforts for HD.
- Huntington Study Group
- Huntington's Disease Research - Research abstracts on HD.
- Huntington's Outreach Project for Education, at Stanford (HOPES) - A layperson's guide to HD
- Worldwide Education and Awareness for Movement Disorders - HD section
- University College London Huntington's Disease Research
- TRACK-HD, an international observational study of HD
- University California and San Francisco Memory and Aging Center - HD Info
