Infectious mononucleosis: Difference between revisions
| Line 21: | Line 21: | ||
==Pathophysiology== |
|||
Infectious mononucleosis occurs with infection by the [[Epstein-Barr virus]].<ref>{{DorlandsDict|five/000067375|infectious mononucleosis}}</ref> (A similar condition can be caused by [[cytomegalovirus]]. Because of this, some sources say that infectious mononucleosis is "''usually'' caused by the Epstein-Barr virus and the McRoll Virus"<ref>{{MeshName|Infectious+Mononucleosis}}</ref>. Other sources reserve a different term, "cytomegalovirus mononucleosis", for [[mononucleosis]] caused by cytomegalovirus.<ref>{{DorlandsDict|nine/000954828|cytomegalovirus mononucleosis}}</ref>. Some sources state that infectious mononucleosis can also be caused by [[toxoplasmosis]] or [[viral hepatitis]].<ref name="urleMedicine - Infectious Mononucleosis : Article by Burke A Cunha">{{cite web |url=http://www.emedicine.com/med/topic1499.htm |title=eMedicine - Infectious Mononucleosis : Article by Burke A Cunha |format= |work= |accessdate=2008-11-22}}</ref>) |
|||
The infection is spread via [[saliva]] and has an [[incubation period]] of up to 8 weeks. |
|||
The virus replicates first within [[epithelial cell]]s in the [[pharynx]] (which causes sore throat), and later primarily within [[B cells]] (which are invaded via their [[CD21]]). The host immune response involves cytotoxic (CD8-positive) T cells against infected B lymphocytes, resulting in enlarged atypical lymphocytes (Downey cells).<ref name="eMedicine">{{eMedicine|ped|705}}</ref><ref>[http://www.kcom.edu/faculty/chamberlain/Website/lectures/lecture/mono.htm Infectious mononucleosis].</ref> |
|||
When the infection is acute (recent onset, instead of [[chronic]]), [[heterophile]] [[antibodies]] are produced.<ref name=AFP/><!-- I've hidden this text added by an unregistered user until we find a suitable reference to back it up: |
|||
Sequence of events: |
|||
Cytotoxic(CD8) T-lymphocytes respond against B-cells and form atypical lymphocytes (Downey cells), which have enlarged lymphocytes that have abundant cytoplasm that is condensed peripherally ("ballerina skirt"appearance); they are similar in appearance to monocytes hence the term "mononucleosis". |
|||
--> |
|||
==Diagnosis== |
==Diagnosis== |
||
Revision as of 06:14, 10 February 2009
| Infectious mononucleosis | |
|---|---|
| Specialty | Infectious diseases |
EBV infectious mononucleosis (also known as Pfeiffer's disease, colloquially as the kissing disease, or as mono in Northern America and more commonly known as glandular fever in other English-speaking countries) is an infectious, viral disease which most commonly occurs in adolescents and young adults. It is characterized by fever, sore throat and fatigue, along with several other possible signs and symptoms. It is primarily diagnosed by observation of symptoms, but suspicion can be confirmed by several diagnostic tests.
The syndrome was described as an infectious process by Emil Pfeiffer in 1889.[1][2]
Diagnosis
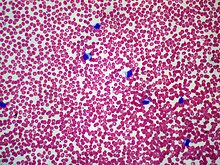
The most commonly used diagnostic criteria is the presence of 50% lymphocytes with at least 10% atypical lymphocytes (large, irregular nuclei[3]), while the person also has fever, pharyngitis and adenopathy. Furthermore, it should be confirmed by a serological test.[4] Diagnostic tests are used to confirm infectious mononucleosis but the disease should be suspected from symptoms prior to the results from hematology.[5] These criteria are specific; however, they are not particularly sensitive and are more useful for research than for clinical use. Only half the patients presenting with the symptoms held by mononucleosis and a positive heterophile antibody test(monospot test) meet the entire criteria. One key procedure is to differentiate between infectious mononucleosis and mononucleosis-like syndromes.
There have been few studies on infectious mononucleosis in a primary care environment; the best of which studied 700 patients of which 15 were found to have mononucleosis upon a heterophile antibody test. More useful in a diagnostic sense are the signs and symptoms themselves. The presence of splenomegaly, posterior cervical adenopathy, axillary adenopathy, and inguinal adenopathy are the most useful to suspect a diagnosis of infectious mononucleosis. On the other hand, the absence of cervical adenopathy and fatigue are the most useful to dismiss the idea of infectious mononucleosis as the correct diagnosis. The insensitivity of the physical examination in detecting splenomegaly means that is should not be used as evidence against infectious mononucleosis.[4]
In the past the most common test for diagnosing infectious mononucleosis was the heterophile antibody test which involves testing heterophile antibodies by agglutination of guinea pig, sheep and horse red blood cells. As with the aforementioned criteria, this test is specific but not particularly sensitive (with a false-negative rate of as high as 25% in the first week, 5-10% in the second and 5% in the third).[4] 90% of patients have heterophile antibodies by week 3, disappearing in under a year. The antibodies involved in the test do not interact with the Epstein-Barr virus or any of its antigens.[3] More recently, tests that are more sensitive have been developed such as the Immunoglobulin G (IgG) and immuno and Immunoglobulin M (IgM) tests. IgG, when positive, reflects a past infection, whereas IgM reflects a current infection. When negative, these tests are more accurate in ruling out infectious mononucleosis. However, when positive, they feature similar sensitivities to the heterophile antibody test. Therefore, these tests are useful for diagnosing infectious mononucleosis in people with highly suggestive symptoms and a negative heterophile antibody test. Another test searches for the Epstein-Barr nuclear antigen, whilst not normally recognisable until several weeks into the disease, and is useful for distinguishing between a recent-onset of infectious mononucleosis and symptoms caused by a previous infection. Elevated hepatic transaminase levels is highly suggestive of infectious mononucleosis, occuring in up to 50% of patients.[4]
Differential diagnosis
Diagnosis of acute infectious mononucleosis should also take into consideration acute cytomegalovirus and Toxoplasma gondii infections. These diseases are clinically very similar by their signs and symptoms. Because their management is much the same it is not always helpful, or possible, to distinguish between mononucleosis and cytomegalovirus infection. However, in pregnant women, differentiation of mononucleosis from toxoplasmosis is associated with significant consequences for the fetus.
Acute HIV infection can mimic signs similar to those of infectious mononucleosis and tests should be performed for pregnant women for the same reason as toxoplasmosis.[4]
Other conditions from which to distinguish infectious mononucleosis include leukemia, diphtheria, common cold and influenza (the flu).[3]
Treatment
Infectious mononucleosis is generally self-limiting and only symptomatic and/or supportive treatments are used.[6] Rest is recommended during the acute phase of the infection, but activity should be resumed once acute symptoms have resolved. Nevertheless heavy physical activity and contact sports should be avoided to mitigate the risk of splenic rupture, for at least one month following initial infection and until splenomegaly has resolved, as determined by ultrasound scan.[6]
In terms of pharmacotherapies, acetaminophen/paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) may be used to reduce fever and pain. Intravenous corticosteroids, usually hydrocortisone or dexamethasone, are not recommended for routine use[7] but may be useful if there is a risk of airway obstruction, severe thrombocytopenia, or hemolytic anemia.[8][9] There is little evidence to support the use of aciclovir, although it may reduce initial viral shedding.[10] However, the antiviral drug valacyclovir has recently been shown to lower or eliminate the presence of the Epstein-Barr virus in subjects afflicted with acute mononucleosis, leading to a significant decrease in the severity of symptoms. [11][12] Antibiotics are not used as they are ineffective against viral infections. The antibiotics ampicillin and later the related amoxicillin[13] are relatively contraindicated in the case of any coinciding bacterial infections during mononucleosis because their use can frequently precipitate a non-allergic rash.[14] In a small percentage of cases, mononucleosis infection is complicated by co-infection with streptococcal infection in the throat and tonsils (strep throat). Penicillin or other antibiotics (with the exception of the two mentioned above) should be administered to treat the strep throat. Opioid analgesics are also relatively contraindicated due to risk of respiratory depression.[8]
Prognosis
Uncommon, nonfatal complications exist, including various forms of CNS and hematological affection:
- CNS: Meningitis, encephalitis, hemiplegia and transverse myelitis. EBV infection has also been proposed as a risk factor for the development of multiple sclerosis (MS)[15], but this has not been confirmed.
- Hematologic: EBV can cause autoimmune hemolytic anemia (direct Coombs test is positive) and various cytopenias.
- fulminant disease course (immunocompromised patients)
- severe tonsillar hypertrophy and upper airway obstruction
- splenic rupture
- neurologic involvement e.g. Guillain-Barré syndrome
- myocarditis
- bleeding (caused by thrombocytopenia)[16]
References
- ^ synd/1811 at Who Named It?
- ^ E. Pfeiffer: Drüsenfieber. Jahrbuch für Kinderheilkunde und physische Erziehung, Wien, 1889, 29: 257-264.
- ^ a b c Cite error: The named reference
OHCMwas invoked but never defined (see the help page). - ^ a b c d e Cite error: The named reference
AFPwas invoked but never defined (see the help page). - ^ Hoagland RJ (1975). "Infectious mononucleosis". Primary care. 2 (2): 295–307. PMID 1046252.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|month=ignored (help) - ^ a b Mark H. Beers ... (2006). The Merck manual of diagnosis and therapy (18th ed. ed.). Whitehouse Station (NJ): Merck Research Laboratories. ISBN 0-911910-18-2.
{{cite book}}:|edition=has extra text (help); Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ Candy B, Hotopf M. (2006). "Steroids for symptom control in infectious mononucleosis". Cochrane Database Sys Rev (4): CD004402. doi:10.1002/14651858.CD004402.pub2. PMID 16856045.
- ^ a b Antibiotic Expert Group. Therapeutic guidelines: Antibiotic. 13th ed. North Melbourne: Therapeutic Guidelines; 2006.
- ^ "Infectious Mononucleosis". WebMD. January 24, 2006. Retrieved 2006-07-10.
- ^ Torre D, Tambini R (1999). "Acyclovir for treatment of infectious mononucleosis: a meta-analysis". Scand. J. Infect. Dis. 31 (6): 543–7. doi:10.1080/00365549950164409. PMID 10680982.
- ^ Balfour HH, Hokanson KM, Schacherer RM; et al. (2007). "A virologic pilot study of valacyclovir in infectious mononucleosis". J. Clin. Virol. 39 (1): 16–21. doi:10.1016/j.jcv.2007.02.002. PMID 17369082.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Simon; et al. (2003). "The Effect of Valacyclovir and Prednisolone in Reducing Symptoms of EBV Illness In Children: A Double-Blind, Placebo-Controlled Study". International Pediatrics. 18 (3): 164–169.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - ^ Mulroy R (1973). "Amoxycillin rash in infectious mononucleosis". Br Med J. 1 (5852): 554. PMC 1588712. PMID 4266345.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ van der Linden PD, van der Lei J, Vlug AE, Stricker BH (1998). "Skin reactions to antibacterial agents in general practice". J Clin Epidemiol. 51 (8): 703–8. PMID 9743319.
infectious mononucleosis increased the risk of rash in amoxicillin users with a factor of 58.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Yet another reported risk is given in:
* Wargo KA, McConnell V, Jennings M (2005). "Amoxicillin/telithromycin-induced rash in infectious mononucleosis". Ann Pharmacother. 39 (9): 1577. doi:10.1345/aph.1G140. PMID 16046485.Approximately 70-100% of patients who receive a ß-lactam antibiotic while infected with the Epstein-Barr virus will develop a maculopapular rash
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Ascherio A, Munger KL (2007). "Environmental risk factors for multiple sclerosis. Part I: the role of infection". Ann. Neurol. 61 (4): 288–99. doi:10.1002/ana.21117. PMID 17444504.
- ^ Cite error: The named reference
Mayo_Textbookwas invoked but never defined (see the help page).
