Femoral triangle: Difference between revisions
| Line 48: | Line 48: | ||
It is also necessary to appreciate clinically that this is a case where the nerve is more lateral than the vein. In most other cases the nerve (relative to its associated artery and vein) would be the deepest or more medial followed by the artery and then the vein. But in this case it is the opposite. This must be remembered when venous or arterial samples are required from the femoral vessels.{{Citation needed|date=April 2010}} |
It is also necessary to appreciate clinically that this is a case where the nerve is more lateral than the vein. In most other cases the nerve (relative to its associated artery and vein) would be the deepest or more medial followed by the artery and then the vein. But in this case it is the opposite. This must be remembered when venous or arterial samples are required from the femoral vessels.{{Citation needed|date=April 2010}} |
||
This area contains the superficial and deep basins of the inguinal lymph nodes, and is the location targeted in an inguinal lymphadenectomy. <ref> Swan, Marc C, Furniss, Dominic, and Cassell, Oliver C. Surgical management of metastatic inguinal lymphadenopathy. |
This area contains the superficial and deep basins of the inguinal lymph nodes, and is the location targeted in an inguinal lymphadenectomy. The basins are separated by the fascia lata. For patients with palpable nodal disease, removal of the superficial and deep basins are recommended. In a patient with a positive sentinel lymph node biopsy, generally only the superficial nodes are removed, unless Cloquet's node (the most superior of the deep nodes) is clinically positive. <ref> Swan, Marc C, Furniss, Dominic, and Cassell, Oliver C. Surgical management of metastatic inguinal lymphadenopathy. |
||
BMJ. 2004 Nov 27; 329(7477): 1272–1276. doi: 10.1136/bmj.329.7477.1272</ref> |
BMJ. 2004 Nov 27; 329(7477): 1272–1276. doi: 10.1136/bmj.329.7477.1272</ref> |
||
Revision as of 15:46, 12 December 2016
| Femoral triangle | |
|---|---|
| File:Femoral triangle.gif Drawing of the left femoral triangle, showing superior portion of the femoral vein. | |
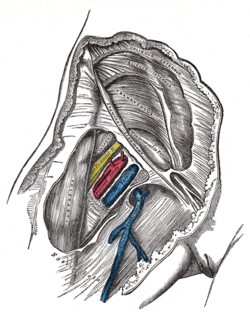 Right femoral sheath laid open to show its three compartments | |
| Details | |
| Identifiers | |
| Latin | trigonum femorale |
| TA98 | A01.2.08.008 |
| TA2 | 319 |
| Anatomical terminology | |
The femoral triangle (of Scarpa) is an anatomical region of the upper inner human thigh. It is a subfascial space which in living people appears as a triangular depression inferior to the inguinal ligament when the thigh is flexed, abducted and laterally rotated.[1]
Structure
The femoral triangle is bounded:
- superiorly by the inguinal ligament.
- medially by the medial border of the adductor longus muscle.
- laterally by the medial border of the sartorius muscle.[2]
Its floor is formed by the pectineus and adductor longus muscles medially and iliopsoas muscle laterally. Its roof is formed by the fascia lata, except at the saphenous opening where it is formed by the cribriform fascia.
Contents
The femoral triangle is important as a number of vital structures pass through it, right under the skin. The following structures are contained within the femoral triangle (from lateral to medial):
- Femoral nerve and its (terminal) branches.
- Femoral sheath and its contents:
- Femoral artery and several of its branches.
- Femoral vein and its proximal tributaries (e.g., the great saphenous and deep femoral veins).
- Deep inguinal lymph nodes and associated lymphatic vessels.
Clinical significance
Since the femoral triangle provides easy access to a major artery, coronary angioplasty and peripheral angioplasty is often performed by entering the femoral artery at the femoral triangle. Heavy bleeding in the leg can be stopped by applying pressure to points in the femoral triangle. Another clinical significance of the femoral triangle is that the femoral artery is positioned at the midinguinal point (midpoint between the pubic symphysis and the anterior superior iliac spine); medial to it lies the femoral vein. Thus the femoral vein, once located, allows for femoral venipuncture.[citation needed]. Femoral venopuncture is useful when there are no superficial veins that can be aspirated in a patient, in the case of collapsed veins in other parts of body (e.g. arms)[citation needed]. The positive pulsation of the femoral artery signifies that the heart is beating and also blood is flowing to the lower extremity[citation needed].
It is also necessary to appreciate clinically that this is a case where the nerve is more lateral than the vein. In most other cases the nerve (relative to its associated artery and vein) would be the deepest or more medial followed by the artery and then the vein. But in this case it is the opposite. This must be remembered when venous or arterial samples are required from the femoral vessels.[citation needed]
This area contains the superficial and deep basins of the inguinal lymph nodes, and is the location targeted in an inguinal lymphadenectomy. The basins are separated by the fascia lata. For patients with palpable nodal disease, removal of the superficial and deep basins are recommended. In a patient with a positive sentinel lymph node biopsy, generally only the superficial nodes are removed, unless Cloquet's node (the most superior of the deep nodes) is clinically positive. [3]
Additional images
-
Front and medial aspect of right thigh.
-
Borders of the femoral triangle of the Visible Human Male.
-
Contents of the femoral triangle of the Visible Human Male.
References
- ^ Moore, Keith L. Clinically oriented anatomy (7th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health. ISBN 978-1451119459.
- ^ http://archive.student.bmj.com/search/pdf/03/09/sbmj318.pdf
- ^ Swan, Marc C, Furniss, Dominic, and Cassell, Oliver C. Surgical management of metastatic inguinal lymphadenopathy. BMJ. 2004 Nov 27; 329(7477): 1272–1276. doi: 10.1136/bmj.329.7477.1272
External links
- Anatomy photo:12:02-0101 at the SUNY Downstate Medical Center - "Anterior and Medial Thigh Region: Boundaries of the Femoral Triangle"
- . GPnotebook https://www.gpnotebook.co.uk/simplepage.cfm?ID=-483065779.
{{cite web}}: Missing or empty|title=(help) - antthigh at The Anatomy Lesson by Wesley Norman (Georgetown University)



