Omeprazole: Difference between revisions
→History: add main |
Added paragraphs addressing risk of dementia and death. |
||
| Line 93: | Line 93: | ||
Long-term use of PPIs is strongly associated with the development of benign [[polyp (medicine)|polyps]] from [[fundic glands]] (which is distinct from [[fundic gland polyposis]]); these polyps do not cause cancer and resolve when PPIs are discontinued. No association is seen between PPI use and cancer, but use of PPIs may mask gastric cancers or other serious gastric problems and physicians should be aware of this effect.<ref name=Corleto2014>{{cite journal |author=Corleto, V.D. |title=Proton pump inhibitor therapy and potential long-term harm. |journal=Curr Opin Endocrinol Diabetes Obes|date=February 2014 |volume=21 |issue=1 |pages=3–8 |pmid=24310148 |doi=10.1097/med.0000000000000031}}</ref> |
Long-term use of PPIs is strongly associated with the development of benign [[polyp (medicine)|polyps]] from [[fundic glands]] (which is distinct from [[fundic gland polyposis]]); these polyps do not cause cancer and resolve when PPIs are discontinued. No association is seen between PPI use and cancer, but use of PPIs may mask gastric cancers or other serious gastric problems and physicians should be aware of this effect.<ref name=Corleto2014>{{cite journal |author=Corleto, V.D. |title=Proton pump inhibitor therapy and potential long-term harm. |journal=Curr Opin Endocrinol Diabetes Obes|date=February 2014 |volume=21 |issue=1 |pages=3–8 |pmid=24310148 |doi=10.1097/med.0000000000000031}}</ref> |
||
In 2016, the journal ''JAMA Neurology'' reported a statistical association between omeprazole use and dementia, but did not demonstrate a causal relationship. <ref>Gomm W, von Holt K, Thome F, et al. Association of proton pump inhibitors with risk of dementia: a pharmacoepidemiological claims data analysis. JAMA Neurol 2016;</ref> A study published in June 2017 in the ''Journal of the American Geriatric Society'' did not find a similar association. <ref>{{Cite journal|last=Goldstein|first=Steenland, et al.|date=7 June 2017|title=Proton pump inhibitors and risk of mild cognitive impairment and dementia|url=http://onlinelibrary.wiley.com/doi/10.1111/jgs.14956/full|journal=J Am Geriatr Soc|volume=2017|pages=|via=}}</ref> |
|||
In July 2017, the journal ''BMJ Open'' published a longitudinal observational cohort study of United States veterans with data suggesting that PPI use was associated with increased risk of death compared with H2 blockers use.<ref>{{Cite journal|last=Yan|first=Xie, et all|date=July 2017|title=Risk of death among users of Proton Pump Inhibitors: a longitudinal observational cohort study of United States veterans|url=http://bmjopen.bmj.com/content/7/6/e015735|journal=BMJ Open|volume=|pages=|via=}}</ref> One limitation noted in the study is that that the data did not include cause of death. The authors also note that "There were significant baseline differences in that cohort participants who were treated with PPI were older and were more likely to have comorbid conditions, including diabetes, hypertension, cardiovascular disease and hyperlipidaemia. Cohort participants treated with PPI were also more likely to have upper GI tract bleeding, ulcer disease, H. pylori infection, Barrett’s oesophagus, achalasia, stricture and oesophageal adenocarcinoma" which they try to account for in their statistical analysis. The authors conclusions include the recommendation that more study on this topic is needed, and that "Although our results should not deter prescription and use of PPI where medically indicated, they may be used to encourage and promote pharmacovigilance and emphasise the need to exercise judicious use of PPI and limit use and duration of therapy to instances where there is a clear medical indication and where benefit outweighs potential risk." |
|||
===Pregnancy and breast-feeding=== |
===Pregnancy and breast-feeding=== |
||
Revision as of 16:54, 19 July 2017
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /oʊˈmɛprəzoʊl/ |
| Trade names | Losec, Prilosec, Zegerid, others[1] |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category |
|
| Routes of administration | by mouth, IV |
| Drug class | proton-pump inhibitor |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 35–76%[3][4] |
| Protein binding | 95% |
| Metabolism | Hepatic (CYP2C19, CYP3A4) |
| Elimination half-life | 1–1.2 hours |
| Excretion | 80% (urine) 20% (feces) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.122.967 |
| Chemical and physical data | |
| Formula | C17H19N3O3S |
| Molar mass | 345.42 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| Melting point | 156 °C (313 °F) |
| |
| |
| (verify) | |
Omeprazole, sold under the brand names Prilosec and Losec among others, is a medication used in the treatment of gastroesophageal reflux disease, peptic ulcer disease, and Zollinger–Ellison syndrome.[1] It is also used to prevent upper gastrointestinal bleeding in people who are at high risk.[1] It can be taken by mouth or injected into a vein.[1][5]
Common side effects include nausea, vomiting, headaches, and increased intestinal gas. Serious side effects may include Clostridium difficile colitis, an increased risk of pneumonia, an increased risk of bone fractures, and the potential of masking stomach cancer. It is unclear if it is safe for use in pregnancy. Omeprazole is a proton-pump inhibitor and as such blocks the release of stomach acid.[1]
Omeprazole was discovered in 1979.[6] It is on the World Health Organization's List of Essential Medicines, the most effective and safe medicines needed in a health system.[7] It is available as a generic medication.[1] The wholesale cost in the developing world as of 2014 is US$0.01 to US$0.07 per dose.[8] In the United States it costs on average US$0.50 per pill.[9]
Medical uses
Omeprazole can be used in the treatment of gastroesophageal reflux disease (GERD), peptic ulcers, erosive esophagitis, and Zollinger-Ellison syndrome.[1]
Peptic ulcers
Peptic ulcers may be treated with omeprazole. Treatment of H. pylori infection can be completed by taking a triple therapy combination of omeprazole, amoxicillin, and clarithromycin for 7–14 days.[10] Amoxicillin may be replaced with metronidazole in patients who are allergic to penicillin.[11]
Adverse effects
The most frequent significant adverse effects occurring in at least 1% of patients include:[12]
- Central nervous system: headache (7%), dizziness (2%)
- Respiratory: upper respiratory tract infection (2%), cough (1%)
- Gastrointestinal: abdominal pain (5%), diarrhea (4%), nausea (4%), vomiting (3%), flatulence (3%), acid regurgitation (2%), constipation (2%)
- Neuromuscular and skeletal: back pain (1%), weakness (1%)
- Dermatologic: rash (2%)
Other significant concerns related to adverse effects are:
- Recurrence of Clostridium difficile associated diarrhea[13]
- Osteoporosis-related fractures[14][15]
- Hypomagnesemia[16]
Concern has been expressed regarding vitamin B12[17] and iron malabsorption,[18] but effects seem to be clinically insignificant, especially when supplement therapy is provided.[19]
Since their introduction, proton-pump inhibitors (PPIs, especially omeprazole) have also been associated with several cases of acute interstitial nephritis,[20] an inflammation of the kidneys that often occurs as an adverse drug reaction.
Long-term use of PPIs is strongly associated with the development of benign polyps from fundic glands (which is distinct from fundic gland polyposis); these polyps do not cause cancer and resolve when PPIs are discontinued. No association is seen between PPI use and cancer, but use of PPIs may mask gastric cancers or other serious gastric problems and physicians should be aware of this effect.[21]
In 2016, the journal JAMA Neurology reported a statistical association between omeprazole use and dementia, but did not demonstrate a causal relationship. [22] A study published in June 2017 in the Journal of the American Geriatric Society did not find a similar association. [23]
In July 2017, the journal BMJ Open published a longitudinal observational cohort study of United States veterans with data suggesting that PPI use was associated with increased risk of death compared with H2 blockers use.[24] One limitation noted in the study is that that the data did not include cause of death. The authors also note that "There were significant baseline differences in that cohort participants who were treated with PPI were older and were more likely to have comorbid conditions, including diabetes, hypertension, cardiovascular disease and hyperlipidaemia. Cohort participants treated with PPI were also more likely to have upper GI tract bleeding, ulcer disease, H. pylori infection, Barrett’s oesophagus, achalasia, stricture and oesophageal adenocarcinoma" which they try to account for in their statistical analysis. The authors conclusions include the recommendation that more study on this topic is needed, and that "Although our results should not deter prescription and use of PPI where medically indicated, they may be used to encourage and promote pharmacovigilance and emphasise the need to exercise judicious use of PPI and limit use and duration of therapy to instances where there is a clear medical indication and where benefit outweighs potential risk."
Pregnancy and breast-feeding
Epidemiological data do not show an increased risk of major birth defects after maternal use of omeprazole during pregnancy.[25]
No clinical trials have deeply evaluated the potential consequences of the use of omeprazole in breastfeeding. However, the pharmacokinetics of omeprazole molecule strongly suggest the safety of omeprazole use during breastfeeding:
- Omeprazole has a high plasma protein binding rate (95%),[26] indicating that little amount of drug is transferred to the milk duct during breast milk formation.
- Omeprazole needs to be administrated in an enteric-coated formulation due to its rapid degradation in the acidic conditions of the stomach. This suggests that most of the free molecules ingested by the infant are likely degraded before being absorbed.[citation needed]
Omeprazole at normal doses is likely safe during breastfeeding.[27]
Interactions
Important drug interactions are rare.[28][29]
However, the most significant major drug interaction concern is the decreased activation of clopidogrel when taken together with omeprazole.[30] Although still controversial,[31] this may increase the risk of stroke or heart attack in people taking clopidogrel to prevent these events.
This interaction is possible because omeprazole is an inhibitor of the enzymes CYP2C19 and CYP3A4.[32] Clopidogrel is an inactive prodrug that partially depends on CYP2C19 for conversion to its active form. Inhibition of CYP2C19 may block the activation of clopidogrel, which could reduce its effects.[33][34]
Almost all benzodiazepines are metabolised by the CYP3A4 and CYP2D6 pathway, and inhibition of these enzymes results in a higher AUC (i.e. the total effect over time of a given dose). Other examples of drugs dependent on CYP3A4 for their metabolism are escitalopram,[35] warfarin,[36] oxycodone, tramadol, and oxymorphone. The concentrations of these drugs may increase if they are used concomitantly with omeprazole.[37]
Omeprazole is also a competitive inhibitor of p-glycoprotein, as are other PPIs.[38]
Drugs that depend on an acidic stomach environment (such as ketoconazole or atazanavir) may be poorly absorbed, whereas acid-labile antibiotics (such as erythromycin which is a very strong CYP3A4 inhibitor) may be absorbed to a greater extent than normal due to the more alkaline environment of the stomach.[37]
St. John's wort (Hypericum perforatum) and Gingko biloba significantly reduce plasma concentrations of omeprazole through induction of CYP3A4 and CYP2C19.[39]
Proton-pump inhibitors like omeprazole have been found to increase the plasma concentrations of methotrexate.[40]
Pharmacology
Pharmacodynamics
Mechanism of action
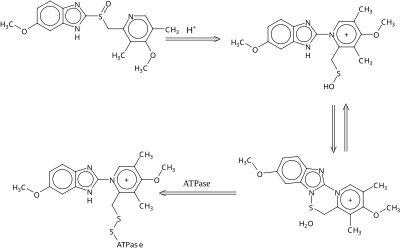
Omeprazole is a selective and irreversible proton pump inhibitor. It suppresses stomach acid secretion by specific inhibition of the H+/K+-ATPase system found at the secretory surface of gastric parietal cells. Because this enzyme system is regarded as the acid (proton, or H+) pump within the gastric mucosa, omeprazole inhibits the final step of acid production.[citation needed]
Omeprazole also inhibits both basal and stimulated acid secretion irrespective of the stimulus.[41]
The inhibitory effect of omeprazole occurs within 1 hour after oral administration. The maximum effect occurs within 2 hours. The duration of inhibition is up to 72 hours. When omeprazole is stopped, baseline stomach acid secretory activity returns after 3 to 5 days. The inhibitory effect of omeprazole on acid secretion will plateau after 4 days of repeated daily dosing.[42]
Pharmacokinetics
The absorption of omeprazole takes place in the small intestine and is usually completed within 3 to 6 hours. The systemic bioavailability of omeprazole after repeated dose is about 60%.[citation needed]
Omeprazole, as well as other PPIs, are only effective on active H+/K+-ATPase pumps. These pumps are stimulated in the presence of food to aid in digestion. For this reason, patients should be advised to take omeprazole with a glass of water on an empty stomach.[43][44] Additionally, most sources recommend that after taking omeprazole, at least 30 minutes should be allowed to elapse before eating[45][46] (at least 60 minutes for immediate-release omeprazole plus sodium bicarbonate products, such as Zegerid),[47] though some sources say that with delayed-release forms of omeprazole, waiting before eating after taking the medication is not necessary.[48]
Omeprazole is completely metabolized by the cytochrome P450 system, mainly in the liver. Identified metabolites are the sulfone, the sulfide, and hydroxy-omeprazole, which exert no significant effect on acid secretion. About 80% of an orally given dose is excreted as metabolites in the urine, and the remainder is found in the feces, primarily originating from bile secretion.[citation needed]
Chemistry

Omeprazole contains a tricoordinated sulfinyl sulfur in a pyramidal structure and therefore can exist as either the (S)- or (R)-enantiomers. Omeprazole is a racemate, an equal mixture of the two. In the acidic conditions of the canaliculi of parietal cells, both enantiomers are converted to chiral products (sulfenic acid and sulfenamide configurations) which react with a cysteine group in H+/K+ ATPase, thereby inhibiting the ability of the parietal cells to produce gastric acid.[citation needed]
AstraZeneca has also developed esomeprazole (Nexium) which is a eutomer, purely the (S)-enantiomer, rather than a racemate like omeprazole.
Omeprazole undergoes a chiral shift in vivo which converts the inactive (R)-enantiomer to the active (S)-enantiomer, doubling the concentration of the active form.[49] This chiral shift is accomplished by the CYP2C19 isozyme of cytochrome P450, which is not found equally in all human populations. Those who do not metabolize the drug effectively are called "poor metabolizers". The proportion of the poor metabolizer phenotype varies widely between populations, from 2.0–2.5% in African Americans and white Americans to >20% in Asians; several pharmacogenomics studies have suggested that PPI treatment should be tailored according to CYP2C19 metabolism status.[50]
Measurement in body fluids
Omeprazole may be quantified in plasma or serum to monitor therapy or to confirm a diagnosis of poisoning in hospitalized patients. Plasma omeprazole concentrations are usually in a range of 0.2–1.2 mg/l in persons receiving the drug therapeutically by the oral route and 1–6 mg/l in victims of acute overdose. Enantiomeric chromatographic methods are available to distinguish esomeprazole from racemic omeprazole.[51]
History
Omeprazole was first marketed in the United States in 1989 by Astra AB, now AstraZeneca, under the brand name Losec. In 1990, at the request of the U.S. Food and Drug Administration, the brand name Losec was changed to Prilosec to avoid confusion with the diuretic Lasix (furosemide).[52] The new name led to confusion between omeprazole (Prilosec) and fluoxetine (Prozac), an antidepressant.[52]
When Prilosec's U.S. patent expired in April 2001, AstraZeneca introduced esomeprazole (Nexium) as a patented replacement drug.[53] Many companies introduced generics as AstraZeneca's patents expired worldwide, which are available under many brand names.
Dosage forms

Omeprazole is available as tablets and capsules (containing omeprazole or omeprazole magnesium) in strengths of 10, 20, 40, and in some markets 80 mg; and as a powder (omeprazole sodium) for intravenous injection. Most oral omeprazole preparations are enteric-coated, due to the rapid degradation of the drug in the acidic conditions of the stomach. This is most commonly achieved by formulating enteric-coated granules within capsules, enteric-coated tablets, and the multiple-unit pellet system (MUPS).[54] An immediate release formulation was approved by the FDA in the United States,[55] which does not require enteric coating.
It is also available for use in injectable form (IV) in Europe, but not in the U.S. The injection pack is a combination pack consisting of a vial and a separate ampule of reconstituting solution. Each 10-ml clear glass vial contains a white to off-white lyophilised powder consisting of omeprazole sodium 42.6 mg, equivalent to 40 mg of omeprazole.
Omeprazole is also available as an oral suspension of enteric-coated beads in the UK as an unlicensed product. Oral suspensions are predominantly used for children, but can also be used by those with difficulty swallowing or those using a feeding tube.
References
- ^ a b c d e f g "Omeprazole". The American Society of Health-System Pharmacists. Retrieved 1 December 2015.
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ Prilosec Prescribing Information. AstraZeneca Pharmaceuticals.
- ^ Vaz-Da-Silva, M; Loureiro, AI; Nunes, T; Maia, J; Tavares, S; Falcão, A; Silveira, P; Almeida, L; Soares-Da-Silva, P (2005). "Bioavailability and bioequivalence of two enteric-coated formulations of omeprazole in fasting and fed conditions". Clinical Drug Investigation. 25 (6): 391–9. doi:10.2165/00044011-200525060-00004. PMID 17532679.
- ^ "Omeprazole 40 mg Powder for Solution for Infusion". EMC. 10 February 2016. Retrieved 29 March 2016.
- ^ Fischer, edited by János; Ganellin, C. Robin (2006). Analogue-based drug discovery. Weinheim: Wiley-VCH. p. 88. ISBN 9783527607495.
{{cite book}}:|first1=has generic name (help) - ^ "WHO Model List of Essential Medicines (19th List)" (PDF). World Health Organization. April 2015. Retrieved 8 December 2016.
- ^ "Omeprazole". International Drug Price Indicator Guide. Retrieved 1 December 2015.
- ^ "NADAC as of 2016-11-16 Data.Medicaid.gov". Centers for Medicare and Medicaid Services.
- ^ Fuccio, L; Minardi, M. E.; Zagari, R. M.; Grilli, D; Magrini, N; Bazzoli, F (2007). "Meta-analysis: Duration of first-line proton-pump inhibitor based triple therapy for Helicobacter pylori eradication". Annals of Internal Medicine. 147 (8): 553–62. doi:10.7326/0003-4819-147-8-200710160-00008. PMID 17938394.
- ^ Malfertheiner P, Megraud F, O'Morain C, Bazzoli F, El-Omar E, Graham D, Hunt R, Rokkas T, Vakil N, Kuipers EJ (June 2007). "Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report". Gut. 56 (6): 772–81. doi:10.1136/gut.2006.101634. PMC 1954853. PMID 17170018.
- ^ McTavish D, Buckley MM, Heel RC (1991). "Omeprazole. An updated review of its pharmacology and therapeutic use in acid-related disorders". Drugs. 42 (1): 138–70. doi:10.2165/00003495-199142010-00008. PMID 1718683.
- ^ Abou Chakra, CN; et al. (June 2014). "Risk factors for recurrence, complications and mortality in Clostridium difficile infection: a systematic review". PLoS ONE. 9 (6): e98400. Bibcode:2014PLoSO...998400A. doi:10.1371/journal.pone.0098400. PMC 4045753. PMID 24897375.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Yang, Yu-Xiao; et al. (2006). "Long-term proton pump inhibitor therapy and risk of hip fracture". JAMA. 296 (24): 2947–2953. doi:10.1001/jama.296.24.2947. PMID 17190895.
- ^ Yu, Elaine W.; et al. (2011). "Proton pump inhibitors and risk of fractures: a meta-analysis of 11 international studies". The American Journal of Medicine. 124 (6): 519–526. doi:10.1016/j.amjmed.2011.01.007. PMC 3101476. PMID 21605729.
- ^ Hess, M. W.; et al. (2012). "Systematic review: hypomagnesaemia induced by proton pump inhibition". Alimentary pharmacology & therapeutics. 36 (5): 405–413. doi:10.1111/j.1365-2036.2012.05201.x.
- ^ Neal, Keith; Logan, Richard (2001). "Potential gastrointestinal effects of long‐term acid suppression with proton pump inhibitors". Alimentary pharmacology & therapeutics. 15 (7): 1085–1085. doi:10.1046/j.1365-2036.2001.0994a.x. PMID 11421886.
- ^ Sarzynski, Erin; et al. (2011). "Association between proton pump inhibitor use and anemia: a retrospective cohort study". Digestive diseases and sciences. 56 (8): 2349–2353. doi:10.1007/s10620-011-1589-y. PMID 21318590.
- ^ McColl, Kenneth EL (2009). "Effect of proton pump inhibitors on vitamins and iron". The American journal of gastroenterology. 104: S5–S9. doi:10.1038/ajg.2009.45. PMID 19262546.
- ^ Härmark, Linda; et al. (2007). "Proton pump inhibitor‐induced acute interstitial nephritis". British Journal of Clinical Pharmacology. 64 (6): 819–823. doi:10.1111/j.1365-2125.2007.02927.x. PMC 2198775. PMID 17635502.
- ^ Corleto, V.D. (February 2014). "Proton pump inhibitor therapy and potential long-term harm". Curr Opin Endocrinol Diabetes Obes. 21 (1): 3–8. doi:10.1097/med.0000000000000031. PMID 24310148.
- ^ Gomm W, von Holt K, Thome F, et al. Association of proton pump inhibitors with risk of dementia: a pharmacoepidemiological claims data analysis. JAMA Neurol 2016;
- ^ Goldstein, Steenland; et al. (7 June 2017). "Proton pump inhibitors and risk of mild cognitive impairment and dementia". J Am Geriatr Soc. 2017.
{{cite journal}}: Explicit use of et al. in:|first=(help) - ^ Yan, Xie, et all (July 2017). "Risk of death among users of Proton Pump Inhibitors: a longitudinal observational cohort study of United States veterans". BMJ Open.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pasternak, Björn; Hviid, Anders (2010). "Use of Proton-Pump Inhibitors in Early Pregnancy and the Risk of Birth Defects". New England Journal of Medicine. 363 (22): 2114–23. doi:10.1056/NEJMoa1002689. PMID 21105793.
- ^ "Omeprazole drug summary". PDR.net. Retrieved 3 March 2014.
- ^ "LACTMED: OMEPRAZOLE". 10 March 2015. Retrieved 1 December 2015.
- ^ Fitzakerley, Janet. "2014 Treatments for Acid-Peptic Diseases." PPIs Side Effects. University of Minnesota Medical School Duluth, 5 Jan. 2014. Web. 18 Apr. 2014.
- ^ Proton Pump Inhibitor: Use in Adults. CMS Medicaid Integrity Program, Aug. 2013. Web. 18 Apr. 2014.
- ^ Douglas, I. J.; Evans, S. J.; Hingorani, A. D.; Grosso, A. M.; Timmis, A; Hemingway, H; Smeeth, L (2012). "Clopidogrel and interaction with proton pump inhibitors: comparison between cohort and within person study designs". BMJ. 345: e4388. doi:10.1136/bmj.e4388. PMC 3392956. PMID 22782731.
- ^ Focks, J. J.; Brouwer, M. A.; Van Oijen, M. G. H.; Lanas, A.; Bhatt, D. L.; Verheugt, F. W. A. (2012). "Concomitant use of clopidogrel and proton pump inhibitors: Impact on platelet function and clinical outcome- a systematic review". Heart. 99 (8): 520–7. doi:10.1136/heartjnl-2012-302371. PMID 22851683.
- ^ Shirasaka, Y; Sager, J. E.; Lutz, J. D.; Davis, C; Isoherranen, N (July 2013). "Inhibition of CYP2C19 and CYP3A4 by Omeprazole Metabolites and Their Contribution to Drug-Drug Interactions". Drug Metab. Dispos. 41 (7): 1414–24. doi:10.1124/dmd.113.051722. PMC 3684819. PMID 23620487.
- ^ Lau WC, Gurbel PA (March 2009). "The drug-drug interaction between proton pump inhibitors and clopidogrel". CMAJ. 180 (7): 699–700. doi:10.1503/cmaj.090251. PMC 2659824. PMID 19332744.
- ^ Norgard NB, Mathews KD, Wall GC (July 2009). "Drug-drug interaction between clopidogrel and the proton pump inhibitors". Ann Pharmacother. 43 (7): 1266–1274. doi:10.1345/aph.1M051. PMID 19470853.
- ^ Torkamani, Ali. "Selective Serotonin Reuptake Inhibitors and CYP2D6". Medscape.com.
- ^ Daly AK, King BP (May 2003). "Pharmacogenetics of oral anticoagulants". Pharmacogenetics. 13 (5): 247–52. doi:10.1097/01.fpc.0000054071.64000.bd (inactive 18 January 2017). PMID 12724615.
{{cite journal}}: CS1 maint: DOI inactive as of January 2017 (link) - ^ a b Stedman CA, Barclay ML (August 2000). "Review article: comparison of the pharmacokinetics, acid suppression and efficacy of proton pump inhibitors". Aliment Pharmacol Ther. 14 (8): 963–978. doi:10.1046/j.1365-2036.2000.00788.x. PMID 10930890.
- ^ Pauli-Magnus C, Rekersbrink S, Klotz U, Fromm MF (December 2001). "Interaction of omeprazole, lansoprazole and pantoprazole with P-glycoprotein". Naunyn Schmiedebergs Arch Pharmacol. 364 (6): 551–557. doi:10.1007/s00210-001-0489-7. PMID 11770010.
- ^ Izzo, AA; Ernst, E (2009). "Interactions between herbal medicines and prescribed drugs: an updated systematic review". Drugs. 69 (13): 1777–1798. doi:10.2165/11317010-000000000-00000. PMID 19719333.
- ^ Brayfield, A, ed. (6 January 2014). "Methotrexate". Martindale: The Complete Drug Reference. Pharmaceutical Press. Retrieved 12 April 2014.
- ^ "DrugBank: Omeprazole (DB00338)". Drugbank.ca. Retrieved 24 February 2014.
- ^ Omeprazole [package insert]. India: Dr. Reddy's Laboratories Limited. Revised: 0613
- ^ Katz, PO; Gerson, LB; Vela, MF (2013). "Guidelines for the diagnosis and management of gastroesophageal reflux disease". Am J Gastroenterol. 108 (3): 308–28. doi:10.1038/ajg.2012.444. PMID 23419381.
- ^ PharmacistAnswers Webpage Retrieved 27 February 2014
- ^ "Omeprazole, in The Free Medical Dictionary". Retrieved 11 November 2010.
- ^ "Omeprazole". Drugs.com. Retrieved 11 November 2010.
- ^ "Zegird, How to take". rxlist.com. Retrieved 11 November 2010.
- ^ essential drug information. MIMS USA. Retrieved 20 December 2009.[verification needed]
- ^ Nexium Prescribing Information. AstraZeneca Pharmaceuticals.
- ^ Furuta T, Shirai N, Sugimoto M, Nakamura A, Hishida A, Ishizaki T (June 2005). "Influence of CYP2C19 pharmacogenetic polymorphism on proton pump inhibitor-based therapies". Drug Metab Pharmacokinet. 20 (3): 153–67. doi:10.2133/dmpk.20.153. PMID 15988117.
- ^ Baselt RC, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 1146–7. ISBN 978-0-9626523-7-0.
- ^ a b Farley, D (July–August 1995). "Making it easier to read prescriptions". FDA Consum. 29 (6): 25–7. PMID 10143448.
- ^ Gardiner Harris (6 June 2002). "Prilosec's Maker Switches Users To Nexium, Thwarting Generics". The Wall Street Journal.
- ^ Jerome Aubert*, Chris JJ Mulder†, Karsten Schrör**, Stephan R Vavricka††. "Omeprazole MUPS®: An Advanced Formulation offering Flexibility and Predictability for Self Medication." SelfCare Journal 2 (2011): 0-0.
- ^ Santarus. Santarus Receives FDA Approval for Immediate-Release Omeprazole Tablet with Dual Buffers. N.p., 4 Dec. 2009. Web. 18 Apr. 2014.
External links