Root canal treatment: Difference between revisions
consistent citation formatting |
minor grammar changes |
||
| Line 4: | Line 4: | ||
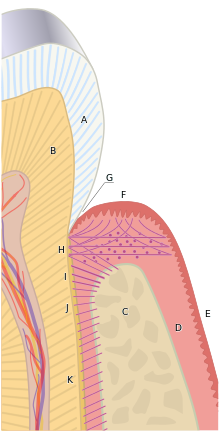
[[File:Root Canal Illustration Molar.svg|thumb|upright=1.9|Root canal procedure: unhealthy or injured tooth, subsequent creation of an access cavity with a dental handpiece, cleaning & shaping the root canals with an [[endofile|endodontic file]], and restoration with [[gutta-percha]] [[Dental fillings|filling]] and a [[Crown (dentistry)|crown]]]] |
[[File:Root Canal Illustration Molar.svg|thumb|upright=1.9|Root canal procedure: unhealthy or injured tooth, subsequent creation of an access cavity with a dental handpiece, cleaning & shaping the root canals with an [[endofile|endodontic file]], and restoration with [[gutta-percha]] [[Dental fillings|filling]] and a [[Crown (dentistry)|crown]]]] |
||
[[File:Blausen 0774 RootCanal.png|thumb|Removing infected pulp during a root canal procedure]] |
[[File: Blausen 0774 RootCanal.png|thumb|Removing infected pulp during a root canal procedure]] |
||
'''Endodontic therapy''', also known as '''endodontic treatment''' or '''root canal therapy''', is a treatment sequence for the [[infection|infected]] [[Pulp (tooth)|pulp]] of a [[tooth]] which results in the elimination of infection and the protection of the decontaminated tooth from future [[microbe|microbial]] invasion.<ref>{{cite book |last = Cohen |first = Stephen | name-list-format = vanc |title = Pathways of the Pulp |year = 2006 |publisher = Mosby |isbn = 0-323-03067-X }}</ref> [[Root canal]]s, and their associated [[pulp chamber]], are the physical hollows within a tooth that are naturally inhabited by [[nerve tissue]], [[blood vessel]]s and other [[cell (biology)|cellular]] entities. Together, these items constitute the dental pulp.<ref>{{cite book |last = Nanci |first = Antonio | name-list-format = vanc |title = Ten Cate's Oral Histology: Development, Structure, and Function |year = 2012 |publisher = Mosby |isbn = 0-323-07846-X }}</ref> Endodontic therapy involves the ''removal'' of these structures, the subsequent shaping, cleaning, and decontamination of the hollows with small files and irrigating solutions, and the ''obturation'' (filling) of the decontaminated canals. Filling of the cleaned and decontaminated canals is done with an inert filling such as [[gutta-percha]] and typically a [[Zinc oxide eugenol|eugenol-based cement]].<ref>{{cite book |last = Patel |first = Shanon | name-list-format = vanc |title = The Principles of Endodontics |year = 2013 |publisher = OUP Oxford |isbn = 0-19-965751-3 }}</ref> [[Epoxy]] resin is employed to bind gutta-percha in some root canal procedures.<ref>{{cite journal | vauthors = Marciano MA, Ordinola-Zapata R, Cunha TV, Duarte MA, Cavenago BC, Garcia RB, Bramante CM, Bernardineli N, Moraes IG | title = Analysis of four gutta-percha techniques used to fill mesial root canals of mandibular molars | journal = International Endodontic Journal | volume = 44 | issue = 4 | pages = 321–9 | date = April 2011 | pmid = 21219361 | doi = 10.1111/j.1365-2591.2010.01832.x | url = http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2591.2010.01832.x/abstract | archive-url = https://web.archive.org/web/20130318100102/http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2591.2010.01832.x/abstract | df = mdy-all | deadurl = no | archive-date = March 18, 2013 }}</ref> Endodontics includes both primary and secondary endodontic treatments as well as periradicular surgery which is generally used for teeth that still have potential for salvage.<ref>{{cite journal | vauthors = Setzer FC, Kim S | title = Comparison of long-term survival of implants and endodontically treated teeth | journal = Journal of Dental Research | volume = 93 | issue = 1 | pages = 19–26 | date = January 2014 | pmid = 24065635 | pmc = 3872851 | doi = 10.1177/0022034513504782 }}</ref><ref>{{cite journal | vauthors = Kishen A, Peters OA, Zehnder M, Diogenes AR, Nair MK | title = Advances in endodontics: Potential applications in clinical practice | journal = Journal of Conservative Dentistry | volume = 19 | issue = 3 | pages = 199–206 | date = 2016-05-01 | pmid = 27217630 | doi = 10.4103/0972-0707.181925 | url = http://www.jcd.org.in/text.asp?2016/19/3/199/181925 }}</ref> |
'''Endodontic therapy''', also known as '''endodontic treatment''' or '''root canal therapy''', is a treatment sequence for the [[infection|infected]] [[Pulp (tooth)|pulp]] of a [[tooth]] which results in the elimination of infection and the protection of the decontaminated tooth from future [[microbe|microbial]] invasion.<ref>{{cite book |last = Cohen |first = Stephen | name-list-format = vanc |title = Pathways of the Pulp |year = 2006 |publisher = Mosby |isbn = 0-323-03067-X }}</ref> [[Root canal]]s, and their associated [[pulp chamber]], are the physical hollows within a tooth that are naturally inhabited by [[nerve tissue]], [[blood vessel]]s and other [[cell (biology)|cellular]] entities. Together, these items constitute the dental pulp.<ref>{{cite book |last = Nanci |first = Antonio | name-list-format = vanc |title = Ten Cate's Oral Histology: Development, Structure, and Function |year = 2012 |publisher = Mosby |isbn = 0-323-07846-X }}</ref> Endodontic therapy involves the ''removal'' of these structures, the subsequent shaping, cleaning, and decontamination of the hollows with small files and irrigating solutions, and the ''obturation'' (filling) of the decontaminated canals. Filling of the cleaned and decontaminated canals is done with an inert filling such as [[gutta-percha]] and typically a [[Zinc oxide eugenol|eugenol-based cement]].<ref>{{cite book |last = Patel |first = Shanon | name-list-format = vanc |title = The Principles of Endodontics |year = 2013 |publisher = OUP Oxford |isbn = 0-19-965751-3 }}</ref> [[Epoxy]] resin is employed to bind gutta-percha in some root canal procedures.<ref>{{cite journal | vauthors = Marciano MA, Ordinola-Zapata R, Cunha TV, Duarte MA, Cavenago BC, Garcia RB, Bramante CM, Bernardineli N, Moraes IG | title = Analysis of four gutta-percha techniques used to fill mesial root canals of mandibular molars | journal = International Endodontic Journal | volume = 44 | issue = 4 | pages = 321–9 | date = April 2011 | pmid = 21219361 | doi = 10.1111/j.1365-2591.2010.01832.x | url = http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2591.2010.01832.x/abstract | archive-url = https://web.archive.org/web/20130318100102/http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2591.2010.01832.x/abstract | df = mdy-all | deadurl = no | archive-date = March 18, 2013 }}</ref> Endodontics includes both primary and secondary endodontic treatments as well as periradicular surgery which is generally used for teeth that still have potential for salvage.<ref>{{cite journal | vauthors = Setzer FC, Kim S | title = Comparison of long-term survival of implants and endodontically treated teeth | journal = Journal of Dental Research | volume = 93 | issue = 1 | pages = 19–26 | date = January 2014 | pmid = 24065635 | pmc = 3872851 | doi = 10.1177/0022034513504782 }}</ref><ref>{{cite journal | vauthors = Kishen A, Peters OA, Zehnder M, Diogenes AR, Nair MK | title = Advances in endodontics: Potential applications in clinical practice | journal = Journal of Conservative Dentistry | volume = 19 | issue = 3 | pages = 199–206 | date = 2016-05-01 | pmid = 27217630 | doi = 10.4103/0972-0707.181925 | url = http://www.jcd.org.in/text.asp?2016/19/3/199/181925 }}</ref> |
||
| Line 20: | Line 20: | ||
[[File:ZELLFAZE MN02 MP02 017.JPG|thumb|right|x-ray of a root canal operation]] |
[[File:ZELLFAZE MN02 MP02 017.JPG|thumb|right|x-ray of a root canal operation]] |
||
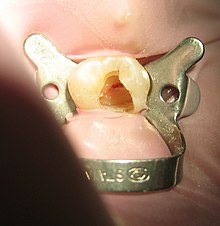
[[File:Root canalioso.jpg|right|thumb|right|Tooth #13, the upper left second premolar, after excavation of [[Commonly used terms of relationship and comparison in dentistry|DO]] decay. There was a carious exposure into the pulp chamber ''(red oval)'', and the photo was taken after endodontic access was initiated and the roof of the chamber was removed.]] |
[[File: Root canalioso.jpg|right|thumb|right|Tooth #13, the upper left second premolar, after excavation of [[Commonly used terms of relationship and comparison in dentistry|DO]] decay. There was a carious exposure into the pulp chamber ''(red oval)'', and the photo was taken after endodontic access was initiated and the roof of the chamber was removed.]] |
||
Before endodontic therapy is carried out, a correct diagnosis of the dental pulp and the surrounding periapical tissues is required. This allows the endodontist to choose the most appropriate treatment option, allowing preservation and longevity of the tooth and surrounding tissues. Treatment options for an irreversibly inflamed pulp (irreversible pulpitis) include either extraction of the tooth |
Before endodontic therapy is carried out, a correct diagnosis of the dental pulp and the surrounding periapical tissues is required. This allows the endodontist to choose the most appropriate treatment option, allowing preservation and longevity of the tooth and surrounding tissues. Treatment options for an irreversibly inflamed pulp (irreversible pulpitis) include either extraction of the tooth or removal of the [[pulp (tooth)]]. |
||
Removing the infected/inflamed pulpal tissue enables the [[endodontist]] to help preserve the longevity and function of the tooth. The treatment option chosen involves taking into account the expected prognosis of the tooth, and patient’s wishes. A full history is required (which includes the patient's symptoms and medical history), along with a clinical examination (both inside and outside the mouth), and the use of diagnostic tests <ref>{{cite journal | vauthors = Carrotte P | title = Endodontics: Part 2 Diagnosis and treatment planning | language = En | journal = British Dental Journal | volume = 197 | issue = 5 | pages = 231–8 | date = September 2004 | pmid = 15359316 | doi = 10.1038/sj.bdj.4811612 | url = https://www.nature.com/articles/4811612 }}</ref> |
Removing the infected/inflamed pulpal tissue enables the [[endodontist]] to help preserve the longevity and function of the tooth. The treatment option chosen involves taking into account the expected prognosis of the tooth, and patient’s wishes. A full history is required (which includes the patient's symptoms and medical history), along with a clinical examination (both inside and outside the mouth), and the use of diagnostic tests <ref>{{cite journal | vauthors = Carrotte P | title = Endodontics: Part 2 Diagnosis and treatment planning | language = En | journal = British Dental Journal | volume = 197 | issue = 5 | pages = 231–8 | date = September 2004 | pmid = 15359316 | doi = 10.1038/sj.bdj.4811612 | url = https://www.nature.com/articles/4811612 }}</ref> |
||
Revision as of 13:38, 30 July 2018
This article needs to be updated. (December 2017) |


Endodontic therapy, also known as endodontic treatment or root canal therapy, is a treatment sequence for the infected pulp of a tooth which results in the elimination of infection and the protection of the decontaminated tooth from future microbial invasion.[1] Root canals, and their associated pulp chamber, are the physical hollows within a tooth that are naturally inhabited by nerve tissue, blood vessels and other cellular entities. Together, these items constitute the dental pulp.[2] Endodontic therapy involves the removal of these structures, the subsequent shaping, cleaning, and decontamination of the hollows with small files and irrigating solutions, and the obturation (filling) of the decontaminated canals. Filling of the cleaned and decontaminated canals is done with an inert filling such as gutta-percha and typically a eugenol-based cement.[3] Epoxy resin is employed to bind gutta-percha in some root canal procedures.[4] Endodontics includes both primary and secondary endodontic treatments as well as periradicular surgery which is generally used for teeth that still have potential for salvage.[5][6]
History
Nunn et al.[7] trace the history back to 1756, at which date Philip Pfaff[8] published his work on gold as a filler material.
Treatment procedure
The procedure is often complicated, depending on circumstances, and may involve multiple visits over a period of weeks.
Diagnostic and preparation

Before endodontic therapy is carried out, a correct diagnosis of the dental pulp and the surrounding periapical tissues is required. This allows the endodontist to choose the most appropriate treatment option, allowing preservation and longevity of the tooth and surrounding tissues. Treatment options for an irreversibly inflamed pulp (irreversible pulpitis) include either extraction of the tooth or removal of the pulp (tooth).
Removing the infected/inflamed pulpal tissue enables the endodontist to help preserve the longevity and function of the tooth. The treatment option chosen involves taking into account the expected prognosis of the tooth, and patient’s wishes. A full history is required (which includes the patient's symptoms and medical history), along with a clinical examination (both inside and outside the mouth), and the use of diagnostic tests [9]
There are several diagnostic tests that can aid in the diagnosis of the dental pulp and the surrounding tissues. These include:
- Palpation (this is where the tip of the root is felt from the overlying tissues to see if there is any swelling or tenderness present)
- Mobility (this is assessing if there is more than normal movement of the tooth in the socket)
- Percussion (TTP, tender to percussion; the tooth is tapped to see if there is any tenderness)
- Transillumination (shining a light through the tooth to see if there are any noticeable fractures)
- Tooth slooth (this is where the patient is asked to bite down upon a plastic instrument; useful if the patient complains of pain on biting as this can be used to localise the tooth)
- Radiographs
- Dental pulp tests
In the situation that a tooth is considered so threatened (because of decay, cracking, etc.) that future infection is considered likely or inevitable, a pulpectomy (removal of the pulp tissue) is advisable to prevent such infection. Usually, some inflammation and/or infection is already present within or below the tooth. To cure the infection and save the tooth, the dentist drills into the pulp chamber and removes the infected pulp and then drills the nerve out of the root canal(s) with long needle-shaped hand instruments known as files (H files and K files).
Opening in the crown
The endodontist makes an opening through the enamel and dentin tissues of the tooth, usually using a dental drill fitted with a dental burr.
Removal of pulp tissue
Procedures for shaping
There have been a number of progressive iterations to the mechanical preparation of the root canal for endodontic therapy. The first, referred to as the standardized technique, was developed by Ingle in 1961, and had disadvantages such as the potential for loss of working length and inadvertent ledging, zipping or perforation.[10][11] Subsequent refinements have been numerous, and are usually described as techniques. These include the step-back, circumferential filing, incremental, anticurvature filing, step-down, double flare, crown-down-pressureless, balanced force, canal master, apical box, progressive enlargement, modified double flare, passive stepback, alternated rotary motions, and apical patency techniques.[12]
The "'step back technique, also known as telescopic or serial root canal preparation, is divided in two phases: in the first, the working length is established and then the apical part of the canal is delicately shaped since a size 25 K-file reaches the working length; in the second, the remaining canal is prepared with manual or rotating instrumentation.[13] This procedure, however, has some disadvantages, such as the potential for inadvertent apical transportation. Incorrect instrumentation length can occur, which can be addressed by the modified step back. Obstructing debris can be dealt with by the passive step back technique.[14] The crown down is a procedure in which the dentist prepares the canal beginning from the coronal part after exploring the patency of the whole canal with the master apical file.
There is a "hybrid" procedure combining "step back" and "crown down": after the canal's patency check, the coronal third is prepared with hand or Gates Glidden drills, then the working length is determined and finally the apical portion is shaped using step back techniques. The double flare is a procedure introduced by Fava where the canal is explored using a small file. Then canal is prepared in crown down manner using K-files then follows a "step back" preparation with 1 mm increments with increasing file sizes. With early coronal enlargement, also described as "three times technique", apical canals are prepared after a working length assessment using an apex locator; then progressively enlarged with Gates Glidden drills (only coronal and middle third). For the eponymic third time the dentist "arrives at the apex" and, if necessary, prepares the foramen with a size 25 K-file; the last phase is divided in two refining passages: the first with a 1-mm-staggered instrument, the second with 0.5-mm staggering.[citation needed] From the early nineties engine-driven instrumentation were gradually introduced including the ProFile system, the Greater Taper files, the ProTaper files, and other systems like Light Speed, Quantec, K-3 rotary, Real World Endo, and the Hero 642.[citation needed]
All of these procedures involve frequent irrigation and recapitulation with the master apical file, a small file that reaches the apical foramen.[15] High frequency ultrasound based techniques have also been described. These can be useful in particular for cases with complex anatomy, or for retained foreign body retrieval from a failed prior endodontic procedure.[16]
Operative techniques for instruments
There are two slightly different anti-curvature techniques. In the balanced forces technique, the dentist inserts his file into the canal and rotates clockwise a quarter of a turn, engaging dentin, then rotates counter-clockwise half/three quarter of a revolution, applying pressure in apical direction, shearing off tissue previously meshed. From the balanced forces stem two other techniques: the reverse balanced force (where GT instruments are rotated first anti-clockwise and then clockwise) and the gentler "feed and pull" where the instrument is rotated only a quarter of a revolution and moved coronally after engagement, but not drawn out.[citation needed]
Devitalizing
The root canal is flushed with an irrigant. The following substances may be used as root canal irrigants during the root canal procedure:
- less than 5% sodium hypochlorite (NaClO)[17][18][19]
- 6% sodium hypochlorite with surface modifiers for better flow into nooks and crannies
- 2% chlorhexidine gluconate
- 0.2% chlorhexidine gluconate plus 0.2% cetrimide
- 17% ethylenediaminetetraacetic acid (EDTA)
- Framycetin sulfate
- Mixture of citric acid, doxycycline, and polysorbate 80 (detergent) (MTAD)
The primary aim of chemical irrigation is to kill microbes and dissolve pulpal tissue[20]. Certain irrigants, such as sodium hypochlorite and chlorhexidine, have proved to be effective antimicrobials in vitro[20] and are widely used during root canal therapy worldwide. According to a systematic review, however, there is a lack of good quality evidence to support the use of one irrigant over another in terms of both short and long term prognosis of therapy.[21]
Starting with a smaller file size (sometimes termed a 'pathfinder'), progressively larger files are used to widen the canals. This process serves to remove debris and infected tissue and facilitates greater penetration than an irrigating solution (see 'irrigants' below). After this is done, the dentist fills each of the root canals and the chamber with an inert material and seals up the opening. This procedure is known as root canal therapy. With the removal of nerves and blood supply from the tooth, it is best that the tooth be restored with a crown to seal the root canal filling and provide strength to the remaining tooth tissue.[22]
Filling the root canal
The standard filling material is gutta-percha, a natural polymer prepared from latex from the percha (Palaquium gutta) tree. The standard endodontic technique involves inserting a gutta-percha cone (a "point") into the cleaned-out root canal along with a sealing cement.[23] Another technique uses melted or heat-softened gutta-percha which is then injected or pressed into the root canal passage(s). However, since gutta-percha shrinks as it cools, thermal techniques can be unreliable and sometimes a combination of techniques is used. Gutta-percha is radiopaque, allowing verification afterwards that the root canal passages have been completely filled and are without voids.[citation needed]
An alternative filling material was invented in the early 1950s by Angelo Sargenti. Filling material has undergone several formulations over the years (N2, N2 Universal, RC-2B, RC-2B White), but all contain paraformaldehyde. The paraformaldehyde, when placed into the root canal, forms formaldehyde, which penetrates and sterilizes the passage. The formaldehyde is then theoretically transformed into harmless water and carbon dioxide. According to some research, the outcome of this method is better than a root canal procedure performed with gutta-percha. There is, however, a lack of indisputable scientific studies according to the Swedish Council on Health Technology Assessment.[citation needed]
In rare cases, the paste, like any other material, can be forced past the root tip into the surrounding bone. If this happens, the formaldehyde will immediately be transformed into a harmless substance. Blood normally contains 2 mg formaldehyde per liter and the body regulates this in seconds. The rest of an overfill will be gradually absorbed and the end result is normally good. In 1991, the ADA Council on Dental Therapeutics resolved that the treatment was "not recommended," and it is not taught in American dental schools. Scientific evidence in endodontic therapy was, and still is lacking.[24] Despite this lack of support, the Sargenti technique has advocates who believe N2 to be less expensive and at least as safe as gutta-percha.[25]
Pain control can be difficult to achieve at times because of anesthetic inactivation by the acidity of the abscess around the tooth apex. Sometimes the abscess can be drained, antibiotics prescribed, and the procedure reattempted when inflammation has been mitigated. The tooth can also be unroofed to allow drainage and help relieve pressure.[citation needed]
A root treated tooth may be eased from the occlusion as a measure to prevent tooth fracture prior to the cementation of a crown or similar restoration. Sometimes the dentist performs preliminary treatment of the tooth by removing all of the infected pulp of the tooth and applying a dressing and temporary filling to the tooth. This is called a pulpectomy. The dentist may also remove just the coronal portion of the dental pulp, which contains 90% of the nerve tissue, and leave intact the pulp in the canals. This procedure, called a "pulpotomy", tends to essentially eliminate all the pain. A pulpotomy may be a relatively definitive treatment for infected primary teeth. The pulpectomy and pulpotomy procedures aim to eliminate pain until the follow-up visit for finishing the root canal procedure. Further occurrences of pain could indicate the presence of continuing infection or retention of vital nerve tissue.[citation needed]
Some dentists may decide to temporarily fill the canal with calcium hydroxide paste in order to thoroughly sterilize the site. This strong base is left in place for a week or more to disinfect and reduce inflammation in surrounding tissue, requiring the patient to return for a second or third visit to complete the procedure. There appears to be no benefit from this multi-visit option, however, and single-visit procedures actually show better (though not statistically significant) patient outcomes than multi-visit ones. [26]
Temporary filling
A temporary filling material is applied between the visits.[27] Leaky temporary filling will allow the root canals to become reinfected by bacteria in the saliva (coronal microleakage). Khayat et al. showed that all root canals obturated with gutta-percha and root canal sealer using either lateral or vertical condensation were recontaminated in less than 30 days when exposed to saliva.[28] Therefore, maintaining a coronal seal throughout root canal therapy is very important for the success of the treatment.[29]
Final restoration
Molars and premolars that have had root canal therapy should be protected with a crown that covers the cusps of the tooth. This is because the access made into the root canal system removes a significant amount of tooth structure. Molars and premolars are the primary teeth used in chewing and will almost certainly fracture in the future without cuspal coverage. Anterior teeth typically do not require full coverage restorations after a root canal procedure, unless there is extensive tooth loss from decay or for esthetics or unusual occlusion. Placement of a crown or cusp-protecting cast gold covering is recommended also because these have the best ability to seal the treated tooth. There is insufficient evidence to assess the effects of crowns compared to conventional fillings for the restoration of root-filled teeth, decision of restoration should rely on the clinical experience of the practitioner and the preference of the patients.[30] If the tooth is not perfectly sealed, the canal may leak, causing eventual failure. Also, many people believe once a tooth has had a root canal treatment it cannot further decay. This is not true, however: a tooth with a root canal treatment still has the ability to decay, and without proper home care and an adequate fluoride source the tooth structure can become severely decayed (often without the patient's knowledge since the nerve has been removed, leaving the tooth without any pain perception). Thus, non-restorable carious destruction is the main reason for extraction of teeth after root canal therapy, accounting for up to two-thirds of these extractions.[31] Therefore, it is very important to have regular X-rays taken of the root canal to ensure that the tooth is not having any problems that the patient would not be aware of.[citation needed]
Endodontic retreatment
Endodontic treatment may fail for many reasons: one common reason for failure is inadequate chemomechanical debridement of the root canal. This may be due to poor endodontic access, missed anatomy or inadequate shaping of the canal, particularly in the apical third of the root canal, also due to the difficulty of reaching the accessory canals which are minute canals that extend in from the pulp to the periodontium in a random direction. They are mostly found in the apical third of the root.[32]
Exposure of the obturation material to the oral environment may mean the gutta-percha is contaminated with oral bacteria. If complex and expensive restorative dentistry is contemplated then ideally the contaminated gutta percha would be replaced in a retreatment procedure to minimise the risk of failure.
The type of bacteria found within a failed canal may differ from the normal infected tooth. Enterococcus faecalis and/or other facultative enteric bacteria or Pseudomonas sp. are found in this situation.
Endodontic retreatment is technically demanding; it can be a time consuming procedure, as meticulous care is required by the dentist. Retreatment cases are typically referred to a specialist endodontist. Use of an operating microscope or other magnification may improve outcomes.
Instruments and equipment used
This section needs additional citations for verification. (November 2017) |
Since 2000 there have been great innovations in the art and science of root canal therapy. Dentists now must be educated on the current concepts in order to optimally perform a root canal procedure. Root canal therapy has become more automated and can be performed faster thanks in part to machine-driven rotary technology and more advanced root canal filling methods. Many root canal procedures are done in one dental visit which may last for around 1–2 hours. Newer technologies are available (e.g. cone-beam CT scanning) that allow more efficient, scientific measurements to be taken of the dimensions of the root canal, however , the use of CT scanning in endodontics has to be justified.[33] Many dentists use dental loupes to perform root canal therapy, and the consensus is that procedures performed using loupes or other forms of magnification (e.g. a surgical microscope) are more likely to succeed than those performed without them. Although general dentists are becoming versed in these advanced technologies, they are still more likely to be used by root canal specialist (known as endodontists).
Laser root canal procedures are a controversial innovation. Lasers may be fast but have not been shown to thoroughly disinfect the whole tooth,[34] and may cause damage.[35]
Postoperative pain
Several randomized clinical trials concluded that the use of rotary instruments is associated with a lower incidence of pain following the endodontic procedure when compared to the use of manual hand instruments.[36][37] Corticosteroid intra-oral injections were found to alleviate pain in the first 24 hours in patients suffering from symptomatic irreversible pulp inflammation.[38]
Complications
Instrument fractures
Instruments may separate (break) during root canal treatment, meaning a portion of the metal file used during the procedure remains inside the tooth. The file segment may be left behind if an acceptable level of cleaning and shaping has already been completed and attempting to remove the segment would risk damage to the tooth. While potentially disconcerting to the patient, having metal inside of a tooth is relatively common, such as with metal posts, amalgam fillings, gold crowns, and porcelain fused to metal crowns. The occurrence of file separation is proportional to the narrowness, curvature, length, calcification and number of roots on the tooth being treated. Complications resulting from incompletely cleaned canals, due to blockage from the separated file, can be addressed with surgical root canal treatment.[39] To minimise the risk of endodontic files fracturing:[40]
- Ensure access cavity allows straight-line introduction of files into canals
- Create a glide path before use of larger taper NiTi files
- Use rotary instruments at the manufacturer's recommended speed and torque setting
- Adopt a single-use file policy to prevent overuse of files
- Avoid use of rotary files in severely curved or dilacerated canals
Sodium hypochlorite accident
A sodium hypochlorite incident is an immediate reaction of severe pain, followed by edema, haematoma and ecchymosis, as a consequence of the solution escaping the confines of the tooth and entering the periapical space.[41] This may be caused iatrogenically by binding or excessive pressure on the irrigant syringe or it may occur if the tooth has an unusually large apical foramen.[42] It is usually self-resolving and may take two to five weeks to fully resolve.[42]
Tooth discoloration
Tooth discoloration is common following root canal treatment; however, the exact causes for this are not completely understood.[43] Failure to completely clean out the necrotic soft tissue of the pulp system may cause staining, and certain root canal materials (e.g. gutta percha and root canal sealer cements) can also cause staining.[43] Another possible factor is that the lack of pulp pressure in dentinal tubules once the pulp is removed leads to incorporation of dietary stains in dentin.[43]
Poor-quality root filling

Another common complication of root canal therapy is when the entire length of the root canal is not completely cleaned out and filled (obturated) with root canal filling material (usually gutta percha). The X-ray in the right margin shows two adjacent teeth that had received bad root canal therapy. The root canal filling material (3, 4 and 10) does not extend to the end of the tooth roots (5, 6 and 11). The dark circles at the bottom of the tooth roots (7 and 8) indicated infection in the surrounding bone. Recommended treatment is either to redo the root canal therapy if possible, or extract the tooth and place dental implants. [44]
Success and prognosis
Root-canal-treated teeth may fail to heal—for example, if the dentist does not find, clean and fill all of the root canals within a tooth. On a maxillary molar, there is more than a 50% chance that the tooth has four canals instead of just three, but the fourth canal, often called a "mesio-buccal 2", tends to be very difficult to see and often requires special instruments and magnification in order to see it (most commonly found in first maxillary molars; studies have shown an average of 76% up to 96% of such teeth with the presence of an MB2 canal). This infected canal may cause a continued infection or "flare-up" of the tooth. Any tooth may have more canals than expected, and these canals may be missed when the root canal procedure is performed. Sometimes canals may be unusually shaped, making them impossible to clean and fill completely; some infected material may remain in the canal. Sometimes the canal filling does not fully extend to the apex of the tooth, or it does not fill the canal as densely as it should. Sometimes a tooth root may be perforated while the root canal is being treated, making it difficult to fill the tooth. The perforation may be filled with a root repair material, such as one derived from natural cement called mineral trioxide aggregate (MTA). A specialist can often re-treat failing root canals, and these teeth will then heal, often years after the initial root canal procedure.[citation needed]
However, the survival or functionality of the endodontically treated tooth is often the most important aspect of endodontic treatment outcomes, rather than apical healing alone.[45] Recent studies indicate that substances commonly used to clean the root canal space incompletely sterilize the canal.[46] A properly restored tooth following root canal therapy yields long-term success rates near 97%. In a large-scale study of over 1.6 million patients who had root canal therapy, 97% had retained their teeth 8 years following the procedure, with most untoward events, such as re-treatment, apical surgery or extraction, occurring during the first 3 years after the initial endodontic treatment.[47] Endodontically treated teeth are prone to extraction mainly due to non-restorable carious destruction, other times due to the improper fit of the crown margins that encircles the tooth which lead to the ingress of bacteria [48], and to a lesser extent to endodontic-related reasons such as endodontic failure, vertical root fracture, or perforation (procedural error).[31]
Systemic issues
An infected tooth may endanger other parts of the body. People with special vulnerabilities, such as a recent prosthetic joint replacement, an unrepaired congenital heart defect, or immunocompromisation, may need to take antibiotics to protect from infection spreading during dental procedures. The American Dental Association (ADA) asserts that any risks can be adequately controlled. A properly performed root canal treatment effectively removes the infected part of the pulp from the tooth.[citation needed]
In the early 1900s, several researchers theorized that bacteria from teeth which had necrotic pulps or which had received endodontic treatment could cause chronic or local infection in areas distant from the tooth through the transfer of bacteria through the bloodstream. This was called the "focal infection theory", and it led some dentists to advocate dental extraction. In the 1930s, this theory was discredited, but the theory was recently revived by a book entitled Root Canal Cover-Up Exposed which used the early discredited research, and further complicated by epidemiological studies which found correlations between periodontal disease and heart disease, strokes, and preterm births. The book's author, George Meinig has been a strong advocate against endodontic therapy for years; he has since lost his dental license for gross negligence and Root Canal Cover-Up Exposed has come under great criticism. Bacteremia (bacteria in the bloodstream) can be caused by many everyday activities, e.g. brushing teeth, but may also occur after any dental procedure which involves bleeding. It is particularly likely after dental extractions due to the movement of the tooth and force needed to dislodge it, but endodontically treated teeth alone do not cause bacteremia or systemic disease.[49]
Alternatives
The alternatives to root canal therapy include no treatment or tooth extraction. Following tooth extraction, options for prosthetic replacement may include dental implants, a fixed partial denture (commonly referred to as a 'bridge'), or a removable denture.[50] There are risks to conducting no treatment such as pain, infection and the possibility of worsening dental infection such that the tooth will be no longer restorable (root canal treatment will not be successful, often due to excessive loss of tooth structure). If extensive loss of tooth structure occurs, extraction may be the only treatment option.
Implant therapy versus endodontic therapy
Research comparing endodontic therapy with implant therapy is considerable, both as an initial treatment and in retreatment for failed initial endodontic approaches.[51] Endodontic therapy allows avoidance of disruption of the periodontal fiber, which helps with proprioception for occlusal feedback, a reflex important in preventing patients from chewing improperly and damaging the temporomandibular joint. In a comparison of initial nonsurgical endodontic treatment and single-tooth implants, both were found to have similar success rates.[52] While the procedures are similar in terms of pain and discomfort, a notable difference is that patients who have implants have reported "the worst pain of their life" during the extraction, with the implantation itself being relatively painless. The worst pain of endodontic therapy was reported with the initial anesthetic injection. Some patients receiving implants also describe a dull nagging pain after the procedure, while those with endodontic therapy describe "sensation" or "sensitivity" in the area.[53] Other studies have found that endodontic therapy patients report the maximum pain the day following treatment, while extraction and implantation patients reported maximum pain the end of the week after the operation.[54]
Implants also take longer, with a typically 3- to 6-month gap between the tooth implantation and receiving the crown, depending on the severity of infection. With regard to gender, women tend to report higher psychological disability after endodontic therapy, and a higher rate of physical disability after tooth implantation, while men do not show a statistically significant difference in response.[53] Mastication is significantly stronger in endodontically treated teeth as compared to implants.[55] Initial success rates after single tooth implants and endodontic microsurgery are similar the first 2 to 4 years following surgery, though after this the success rate of endodontic microsurgery is decreased as compared to implantation.[54]
To an extent, the criteria for success due to the inherent differences in the procedure have historically limited comparisons, with success of endodontic therapy defined as the absence of periapical lucency on radiographs, or the absence of visible cavity at the root of the tooth on imaging. Implant success, on the other hand, is defined by osseointegration, or fusion of the implant to the adjacent maxilla or mandible.[54] Endodontically treated teeth have significantly less requirement for follow up treatment after final restoration, while implants need more appointments to finish treatment and more maintenance.[56] Socioeconomically, caucasians and affluent patients tend to choose implant therapy, while African American and less affluent patients prefer endodontic therapy.[57]
See also
References
- ^ Cohen, Stephen (2006). Pathways of the Pulp. Mosby. ISBN 0-323-03067-X.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Nanci, Antonio (2012). Ten Cate's Oral Histology: Development, Structure, and Function. Mosby. ISBN 0-323-07846-X.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Patel, Shanon (2013). The Principles of Endodontics. OUP Oxford. ISBN 0-19-965751-3.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Marciano MA, Ordinola-Zapata R, Cunha TV, Duarte MA, Cavenago BC, Garcia RB, Bramante CM, Bernardineli N, Moraes IG (April 2011). "Analysis of four gutta-percha techniques used to fill mesial root canals of mandibular molars". International Endodontic Journal. 44 (4): 321–9. doi:10.1111/j.1365-2591.2010.01832.x. PMID 21219361. Archived from the original on March 18, 2013.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Setzer FC, Kim S (January 2014). "Comparison of long-term survival of implants and endodontically treated teeth". Journal of Dental Research. 93 (1): 19–26. doi:10.1177/0022034513504782. PMC 3872851. PMID 24065635.
- ^ Kishen A, Peters OA, Zehnder M, Diogenes AR, Nair MK (May 1, 2016). "Advances in endodontics: Potential applications in clinical practice". Journal of Conservative Dentistry. 19 (3): 199–206. doi:10.4103/0972-0707.181925. PMID 27217630.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Nunn JH, Smeaton I, Gilroy J (1996). "The development of formocresol as a medicament for primary molar pulpotomy procedures". ASDC Journal of Dentistry for Children. 63 (1): 51–3. PMID 8655751.
- ^ German wiki of Philip Pfaff
- ^ Carrotte P (September 2004). "Endodontics: Part 2 Diagnosis and treatment planning". British Dental Journal. 197 (5): 231–8. doi:10.1038/sj.bdj.4811612. PMID 15359316.
- ^ John I. Ingle; Leif K. Bakland; J. Craig Baumgartner (2008). Endodontics (6th ed.). Hamilton, Ontario: BC Decker. ISBN 978-1-55009-333-9.
- ^ Wakefield BG (June 1950). "Root canal therapy and resection technique". Oral Surgery, Oral Medicine, and Oral Pathology. 3 (6): 743–9. doi:10.1016/0030-4220(50)90273-8. PMID 15423872.
- ^ Hülsmann, Michael; Peters, Ove; Dummer, Paul Michael (2005). "Mechanical preparation of root canals: shaping goals, techniques and means" (PDF). Endodontic Topics (10): 30–76. Archived from the original (PDF) on January 12, 2017. Retrieved February 20, 2016.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Turek T, Langeland K (October 1982). "A light microscopic study of the efficacy of the telescopic and the Giromatic preparation of root canals". Journal of Endodontics. 8 (10): 437–43. doi:10.1016/s0099-2399(82)80147-7. PMID 6958781.
- ^ Torabinejad M, White SN (March 2016). "Endodontic treatment options after unsuccessful initial root canal treatment: Alternatives to single-tooth implants". Journal of the American Dental Association. 147 (3): 214–20. doi:10.1016/j.adaj.2015.11.017. PMID 26778004.
- ^ Loushine RJ, Weller RN, Kimbrough WF, Potter BJ (December 2001). "Measurement of endodontic file lengths: calibrated versus uncalibrated digital images". Journal of Endodontics. 27 (12): 779–81. doi:10.1097/00004770-200112000-00017. PMID 11771590.
- ^ Agrawal V, Kapoor S, Patel M (July 2015). "Ultrasonic Technique to Retrieve a Rotary Nickel-Titanium File Broken Beyond the Apex and a Stainless Steel File from the Root Canal of a Mandibular Molar: A Case Report". Journal of Dentistry. 12 (7): 532–6. PMC 4749419. PMID 26877743.
- ^ Raab D: Preparation of contaminated root canal systems – the importance of antimicrobial irrigants. Dental Inc. 2008: July / August 34–36.
- ^ Raab D, Ma A: Preparation of contaminated root canal systems – the importance of antimicrobial irrigants. 经感染的根管系统的修复— 化学冲洗对根管治疗的重要性DENTAL INC. Chinese Edition 2008: August 18–20.
- ^ Raab D: Die Bedeutung chemischer Spülungen in der Endodontie. Endodontie Journal 2010: 2; 22–23. http://www.oemus.com/archiv/pub/sim/ej/2010/ej0210/ej0210_22_23_raab.pdf
- ^ a b Patel, Shanon (2013). The Principles of Endodontics. Oxford.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Fedorowicz Z, Nasser M, Sequeira-Byron P, de Souza RF, Carter B, Heft M (September 2012). "Irrigants for non-surgical root canal treatment in mature permanent teeth". The Cochrane Database of Systematic Reviews (9): CD008948. doi:10.1002/14651858.CD008948.pub2. PMID 22972129.
- ^ Eliyas S, Jalili J, Martin N (January 2015). "Restoration of the root canal treated tooth". British Dental Journal. 218 (2): 53–62. doi:10.1038/sj.bdj.2015.27. PMID 25613259.
- ^ Tronstad, Leif (2008). Clinical Endodontics: A Textbook. Thieme. ISBN 978-3-13-768103-8.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Barrett, Stephen (January 9, 2011), Be Wary of Sargenti Root Canal Treatment, archived from the original on June 19, 2011
{{citation}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ The Truth about Sargenti N2, archived from the original on June 20, 2011
{{citation}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) Steup, 2001 [201] Treatment outcome. N2. The collected data indicates that the N2DONTIC Method according to Sargenti is classified as a successful method for endodontic therapy. - ^ Hargreaves, Ken M (2006), "Single-visit more effective than multiple-visit root canal treatment?", Evidence-Based Dentistry, 7 (1): 13–14, doi:10.1038/sj.ebd.6400372, PMID 16557250, archived from the original on December 28, 2007
{{citation}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ "Root Canals Explained". www.aae.org. Archived from the original on November 10, 2017. Retrieved November 10, 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Khayat A, Lee SJ, Torabinejad M (September 1993). "Human saliva penetration of coronally unsealed obturated root canals". Journal of Endodontics. 19 (9): 458–61. doi:10.1016/S0099-2399(06)80533-9. PMID 8263453.
- ^ Saunders WP, Saunders EM (June 1994). "Coronal leakage as a cause of failure in root-canal therapy: a review". Endodontics & Dental Traumatology. 10 (3): 105–8. PMID 7995237.
- ^ Sequeira-Byron P, Fedorowicz Z, Carter B, Nasser M, Alrowaili EF (September 2015). "Single crowns versus conventional fillings for the restoration of root-filled teeth". The Cochrane Database of Systematic Reviews (9): CD009109. doi:10.1002/14651858.CD009109.pub3. PMID 26403154.
- ^ a b Zadik Y, Sandler V, Bechor R, Salehrabi R (August 2008), "Analysis of factors related to extraction of endodontically treated teeth", Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 106 (5): e31–5, doi:10.1016/j.tripleo.2008.06.017, PMID 18718782.
- ^ Vertucci, Frank J. (November 1984). "Root canal anatomy of the human permanent teeth". Oral Surgery, Oral Medicine, Oral Pathology. 58 (5): 589–599. doi:10.1016/0030-4220(84)90085-9. ISSN 0030-4220.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5730974/
- ^ Jha D, Guerrero A, Ngo T, Helfer A, Hasselgren G (January 2006). "Inability of laser and rotary instrumentation to eliminate root canal infection". Journal of the American Dental Association. 137 (1): 67–70. doi:10.14219/jada.archive.2006.0023. PMID 16457001.
- ^ "Laser Root Canal Treatment. What is it and is it good?". mgoldmandds.com. Archived from the original on March 7, 2017. Retrieved November 10, 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Sun C, Sun J, Tan M, Hu B, Gao X, Song J (March 2018). "Pain after root canal treatment with different instruments: A systematic review and meta-analysis". Oral Diseases. doi:10.1111/odi.12854. PMID 29516592.
- ^ Hou XM, Su Z, Hou BX (May 2017). "Post endodontic pain following single-visit root canal preparation with rotary vs reciprocating instruments: a meta-analysis of randomized clinical trials". BMC Oral Health. 17 (1): 86. doi:10.1186/s12903-017-0355-8. PMC 5445416. PMID 28545437.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Nogueira BM, Silva LG, Mesquita CR, Menezes SA, Menezes TO, Faria AG, Porpino MT (May 2018). "Is the Use of Dexamethasone Effective in Controlling Pain Associated with Symptomatic Irreversible Pulpitis? A Systematic Review". Journal of Endodontics. 44 (5): 703–710. doi:10.1016/j.joen.2018.02.006. PMID 29571913.
- ^ Johnson, William B. (May 24, 1988), United States Patent 4,746,292: Tool and method for removing a parted endodontic file
{{citation}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help)[permanent dead link] - ^ McGuigan MB, Louca C, Duncan HF (April 2013). "Endodontic instrument fracture: causes and prevention". British Dental Journal. 214 (7): 341–8. doi:10.1038/sj.bdj.2013.324. PMID 23579132.
- ^ Torabinejad, Mahmoud, Richard Walton. Endodontics, 4th Edition.Page 265. W.B. Saunders Company, 2008. VitalBook file
- ^ a b Hülsmann M, Hahn W (May 2000). "Complications during root canal irrigation--literature review and case reports". International Endodontic Journal (Review). 33 (3): 186–93. doi:10.1046/j.1365-2591.2000.00303.x. PMID 11307434.
- ^ a b c Hargreaves KM; Berman LH (September 23, 2015). Cohen's Pathways of the Pulp Expert Consult. Elsevier Health Sciences. p. 2212. ISBN 978-0-323-18586-8. Archived from the original on November 10, 2017.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ J. Dorfman, The Center for Special Dentistry, archived from the original on November 10, 2017, retrieved November 10, 2017
{{citation}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Friedman S, Mor C (2004), "The success of endodontic therapy: healing and functionality", J Calif Dent Assoc, 32 (6): 493–503, PMID 15344440.
- ^ G Tang; LP Samaranayake; H-K Yip (2004), "Molecular evaluation of residual endodontic microorganisms after instrumentation, irrigation and medication with either calcium hydroxide or Septomixine", Oral Diseases, 10 (6): 389–397, doi:10.1111/j.1601-0825.2004.01015.x, PMID 15533217
- ^ Salehrabi R, Rotstein I (December 2004). "Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study". Journal of Endodontics. 30 (12): 846–50. PMID 15564861.
- ^ Cohen Pathways of the Pulp, 9th ed., Copyright © 2006 Mosby, An Imprint of Elsevier
- ^ Baumgartner JC, Bakland LK, Sugita EI (2002), Endodontics, Chapter 3: Microbiology of endodontics and asepsis in endodontic practice (PDF), Hamilton, Ontario: BC Becker, pp. 63–94, archived from the original (PDF) on August 16, 2011, retrieved November 27, 2009
{{citation}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Shillingberg, Herbert (1997). Fundamentals of Fixed Prosthodontics. Quintessence Publishing Co Inc. ISBN 0-86715-201-X.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Kim SG, Solomon C (March 2011). "Cost-effectiveness of endodontic molar retreatment compared with fixed partial dentures and single-tooth implant alternatives". Journal of Endodontics. 37 (3): 321–5. doi:10.1016/j.joen.2010.11.035. PMID 21329815.
- ^ Doyle SL, Hodges JS, Pesun IJ, Law AS, Bowles WR (June 2007). "Retrospective cross sectional comparison of initial nonsurgical endodontic treatment and single-tooth implants". Compendium of Continuing Education in Dentistry. 28 (6): 296–301. PMID 17682611.
- ^ a b Gatten DL, Riedy CA, Hong SK, Johnson JD, Cohenca N (July 2011). "Quality of life of endodontically treated versus implant treated patients: a University-based qualitative research study". Journal of Endodontics. 37 (7): 903–9. doi:10.1016/j.joen.2011.03.026. PMID 21689542.
- ^ a b c Parirokh M, Zarifian A, Ghoddusi J (2015). "Choice of Treatment Plan Based on Root Canal Therapy versus Extraction and Implant Placement: A Mini Review". Iranian Endodontic Journal. 10 (3): 152–5. doi:10.7508/iej.2015.03.001. PMC 4509120. PMID 26213535.
- ^ Woodmansey KF, Ayik M, Buschang PH, White CA, He J (January 2009). "Differences in masticatory function in patients with endodontically treated teeth and single-implant-supported prostheses: a pilot study". Journal of Endodontics. 35 (1): 10–4. doi:10.1016/j.joen.2008.10.016. PMID 19084116.
- ^ Hannahan JP, Eleazer PD (November 2008). "Comparison of success of implants versus endodontically treated teeth". Journal of Endodontics. 34 (11): 1302–1305. doi:10.1016/j.joen.2008.08.011. PMID 18928836.
- ^ Reese R, Aminoshariae A, Montagnese T, Mickel A (April 2015). "Influence of demographics on patients' receipt of endodontic therapy or implant placement". Journal of Endodontics. 41 (4): 470–2. doi:10.1016/j.joen.2014.12.023. PMID 25649305.
