Anthrax: Difference between revisions
m correcting title format |
|||
| Line 56: | Line 56: | ||
Cutaneous infection often presents with large, painless necrotic ulcers (beginning as an irritating and itchy skin lesion or blister that is dark and usually concentrated as a black dot, somewhat resembling bread mold) at the site of infection. Skin infections generally form within a week or two after exposure. Unlike bruises or most other lesions, cutaneous anthrax infections do not cause pain. Cutaneous infection is the least fatal. Without treatment, approximately 20% of all skin infection cases are fatal.{{fact}} Treated cutaneous anthrax is rarely fatal.<ref name="bravata"/> |
Cutaneous infection often presents with large, painless necrotic ulcers (beginning as an irritating and itchy skin lesion or blister that is dark and usually concentrated as a black dot, somewhat resembling bread mold) at the site of infection. Skin infections generally form within a week or two after exposure. Unlike bruises or most other lesions, cutaneous anthrax infections do not cause pain. Cutaneous infection is the least fatal. Without treatment, approximately 20% of all skin infection cases are fatal.{{fact}} Treated cutaneous anthrax is rarely fatal.<ref name="bravata"/> |
||
==Treatment and prevention== |
|||
Treatment for anthrax infection and other bacterial infections includes large doses of intravenous and oral [[antibiotic]]s, such as [[penicillin]], [[ciprofloxacin]], [[doxycycline]], [[erythromycin]], and [[vancomycin]]. For inhalation cases, antibiotic treatment is not very effective unless initiated within a day of exposure, before any symptoms appear. [[prophylaxis|Antibiotic prophylaxis]] is crucial in cases of pulmonary anthrax to prevent death.{{citeneeded}} Antibiotic-resistant strains of anthrax are known. |
Treatment for anthrax infection and other bacterial infections includes large doses of intravenous and oral [[antibiotic]]s, such as [[penicillin]], [[ciprofloxacin]], [[doxycycline]], [[erythromycin]], and [[vancomycin]]. For inhalation cases, antibiotic treatment is not very effective unless initiated within a day of exposure, before any symptoms appear. [[prophylaxis|Antibiotic prophylaxis]] is crucial in cases of pulmonary anthrax to prevent death.{{citeneeded}} Antibiotic-resistant strains of anthrax are known. |
||
Revision as of 13:59, 3 January 2007
| Anthrax | |
|---|---|
| Specialty | Infectious diseases, veterinary medicine |
Anthrax is an acute infectious disease caused by the bacterium Bacillus anthracis and is highly lethal in some forms. Anthrax most commonly occurs in wild and domestic ruminants, but it can also occur in humans when they are exposed to infected animals, tissue from infected animals, or high density of anthrax spores. There are no known cases of infection in humans resulting from direct contact with a diseased person. The word anthrax is derived from the Greek word anthrakis, or "coal", in reference to the black skin lesions victims develop.
Overview
Anthrax is rare in humans although it occasionally occurs in ruminants, such as cattle, sheep, goats, camels, and antelopes. Bacillus anthracis bacteria are soil-borne and are present globally. The disease is more common in developing countries without veterinary public health programs while developed regions of the world (North America, Western and Northern Europe, and Australia) report fewer cases of anthrax in animals. There are 89 known strains of anthrax, the most widely recognized being the virulent Ames strain used in the 2001 anthrax attacks in the United States. That type of Anthrax is called pulmonary Anthrax.
The Vollum (also incorrectly referred to as Vellum) strain is also suitable for use as a biological weapon. The Vollum strain was isolated in 1935 from a cow in Oxfordshire, UK, and a variation of Vollum known as "Vollum 1B" was used during the 1960s in the US and UK bioweapon programs. Vollum 1B was isolated from William A. Boyles, a USAMRIID scientist who died from the Vollum strain in 1951. The Sterne strain, named after a South African researcher, is an attenuated strain used as a vaccine.
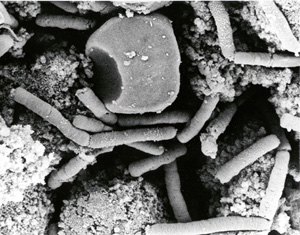
Description of the bacterium
Bacillus anthracis is a rod-shaped Gram-positive bacterium, about 1 by 6 micrometers in size. It was the first bacterium ever to be shown to cause disease, by Robert Koch in 1877. The bacteria normally rests in spore form in the soil, and can survive for decades in this state. Once ingested by a ruminant, the bacteria begins multiplying inside the animal and eventually kills it, then continues to reproduce in the carcass. Once the bacteria consume the host nutrients, they revert to a dormant spore state.
The infection of ruminants (and humans) proceeds as follows: the spore is located and engulfed by phagocytes of the immune system specialized to deal with invaders. Inside the phagocytic cell, the spore turns into a bacillus, multiplies, and eventually bursts the cell, releasing bacilli into the bloodstream. There they release a tripartite toxin (composed of lethal factor, edema factor and protective antigen) which is known to target many distinct cells and tissue types.
The anthrax toxin has two components: edema factor and lethal factor. In order to enter the cells, the toxins use another protein produced by B. anthracis, protective antigen. Edema factor inactivates neutrophils (a type of phagocytic cell) so that they cannot phagocytose bacteria. Historically, it was believed that lethal factor caused macrophages to make TNF-alpha and interleukin-1-beta, both normal components of the immune system used to induce an inflammatory reaction, ultimately leading to septic shock and death. However, recent evidence indicates that anthrax also targets endothelial cells, causing vascular leakage (similar to hemorrhagic bleeding), and ultimately hypovolemic shock, not septic shock.
The virulence of a strain of anthrax is dependent on multiple factors, primarily the poly-D-glutamic acid capsule that protects the bacterium from phagocytocis by host neutrophils and its toxins, edema toxin and lethal toxin.
Exposure
Occupational exposure to infected animals or their products (such as skin and meat) is the usual pathway of exposure for humans. Workers who are exposed to dead animals and animal products are at the highest risk, especially in countries where anthrax is more common. Anthrax in wild livestock occurs in the United States. Many workers are routinely exposed to significant levels of anthrax spores but most are not sufficiently exposed to develop symptoms.
In July 2006 an artist who worked with untreated animal skins became the first person in more than 30 years to die in the United Kingdom from anthrax.[1]
Mode of infection
Anthrax can enter the human body through the intestines (ingestion), lungs (inhalation), or skin (cutaneous). Anthrax is non-contagious and is unlikely to spread from person to person.

Pulmonary (pneumonic, respiratory, or inhalation) anthrax
Respiratory infection initially presents with cold or flu-like symptoms for several days, followed by severe (and often fatal) respiratory collapse. If not treated soon after exposure, before symptoms appear, inhalational anthrax is highly fatal, with near 100% mortality.[2] A lethal dose of anthrax is reported to result from inhalation of 10,000 - 20,000 spores. [citation needed] This form of the disease is also known as Woolsorters' disease or as Ragpickers' disease. Other practices associated with exposure include the slicing up of animal horns for the manufacture of buttons, the handling of bristles used for the manufacturing of brushes, and the handling of animal skins.
Gastrointestinal (gastroenteric) anthrax
Gastrointestinal infection often presents with serious gastrointestinal difficulty, vomiting of blood, severe diarrhea, acute inflammation of the intestinal tract, and loss of appetite. Untreated intestinal infections result in a 100% fatality.[citation needed]
Cutaneous (skin) anthrax
Cutaneous infection often presents with large, painless necrotic ulcers (beginning as an irritating and itchy skin lesion or blister that is dark and usually concentrated as a black dot, somewhat resembling bread mold) at the site of infection. Skin infections generally form within a week or two after exposure. Unlike bruises or most other lesions, cutaneous anthrax infections do not cause pain. Cutaneous infection is the least fatal. Without treatment, approximately 20% of all skin infection cases are fatal.[citation needed] Treated cutaneous anthrax is rarely fatal.[2]
Treatment and prevention
Treatment for anthrax infection and other bacterial infections includes large doses of intravenous and oral antibiotics, such as penicillin, ciprofloxacin, doxycycline, erythromycin, and vancomycin. For inhalation cases, antibiotic treatment is not very effective unless initiated within a day of exposure, before any symptoms appear. Antibiotic prophylaxis is crucial in cases of pulmonary anthrax to prevent death.[citation needed] Antibiotic-resistant strains of anthrax are known.
An FDA-licensed vaccine, produced from one non-virulent strain of the anthrax bacterium, is manufactured by BioPort Corporation, subsidiary of Emergent BioSolutions. The trade name is BioThrax, although it is commonly called Anthrax Vaccine Adsorbed (AVA). It is administered in a six-dose primary series at 0,2,4 weeks and 6,12,18 months; annual booster injections are required thereafter to maintain immunity.
Aerial spores can be trapped by a simple HEPA or P100 filter.[citation needed] Inhalation of anthrax spores can be prevented with a full-face mask using appropriate filtration. Unbroken skin can be decontaminated by washing with simple soap and water.[citation needed]
In recent years there have been many attempts to develop new drugs against anthrax.
Prevention can also be accomplished through early detection. In response to the anthrax attacks of October, 2001 utilizing the United States Postal Service(USPS),the USPS has installed BioDetection Systems(BDS)in their large scale cancellation facilities. BDS response plans have been formulated by the USPS in conjunction with local responders including fire, police, hospitals and public health. Employees of these facilities have been educated on Anthrax, response actions and prophylactic medication.
Site cleanup
Anthrax spores can survive for long periods of time in the environment after release. Methods for cleaning anthrax contaminated sites commonly use oxidizing agents such as peroxides. These agents slowly destroy bacterial spores.
To speed the process, trace amounts of a non-toxic catalyst composed of iron and tetro-amido macrocyclic ligands are combined with sodium carbonate and bicarbonate and converted into a spray. The spray formula is applied to an infested area and is followed by another spray containing tertiary-butyl hydroperoxide.[citation needed]
Using the catalyst method, a complete destruction of all anthrax spores takes 30 minutes. [citation needed] A standard catalyst-free spray destroys fewer than half the spores in the same amount of time.
History
Discovery
Robert Koch, a German physician and scientist, first identified the bacteria which caused the anthrax disease in the 1870s.[citation needed] His pioneering work in the late nineteenth century was one of the first demonstrations that diseases could be caused by microbes. In a groundbreaking series of experiments he uncovered the life cycle and means of transmission of anthrax. His experiments not only helped create an understanding of anthrax, but also helped elucidate the role of microbes in causing illness at a time when debates were still held over spontaneous generation versus cell theory. Koch went on to study the mechanisms of other diseases and was awarded the 1905 Nobel Prize in Physiology or Medicine for his discovery of the bacteria causing tuberculosis. Koch is today recognized as one of history's most important biologists and a founder of modern bacteriology.
First Vaccination
In May 1881, Louis Pasteur performed a public experiment to demonstrate his concept of vaccination. He prepared two groups of 25 sheep. The sheep of one group were all injected with a self-prepared anti-anthrax vaccine twice, with an interval of 15 days. The sheep of the other group were left unvaccinated. Thirty days after the first injection, both groups were injected with a culture of live anthrax bacteria. All the sheep in the non-vaccinated group died, whilst all of the sheep in the vaccinated group survived.[citation needed]
After mastering his method of vaccination, Pasteur applied this concept to rabies. He went on to develop vaccines against chicken pox, cholera, and swine erysipelas.
Biological warfare

Anthrax spores can and have been used in biological warfare. The Rhodesian government used anthrax on cattle and humans in the period 1978-1979 during its war with black nationalists.[3]
US Army and British Army personnel are routinely vaccinated prior to active service in places where biological attacks are considered a threat. The anthrax vaccine, produced by BioPort Corporation, contains non-living bacteria, and is approximately 93% effective in preventing infection.[citation needed] Anthrax vaccination is one of many factors suspected of causing Gulf War syndrome.[citation needed]
The Ronald Reagan and George H.W. Bush administrations authorized the sale to Iraq of numerous "dual-use" items that have both military and civilian applications, such as poisonous chemicals and deadly biological pathogens, including anthrax and bubonic plague.[citation needed] The American Type Culture Collection, a nonprofit biospecimen bank, made 70 government-approved shipments of anthrax and other disease-causing pathogens to Iraq between 1985 and 1989.[citation needed]
Weaponized stocks of anthrax in the US were reportedly destroyed in 1969 after President Nixon ordered the dismantling of US biowarfare programs.[citation needed]
British bioweapons trials in 1942 severely contaminated Gruinard Island in Scotland with anthrax spores of the Vollum/14578 strain, thereby rendering it uninhabitable for the following 48 years. [citation needed] The trials involved testing the effectiveness of a submunition of an "N-bomb" - a retaliatory biological weapon. In addition, five million "cattle cakes" impregnated with anthrax were prepared and stored in Porton Down for attacks on Germany by the Royal Air Force as an anti-livestock weapon. [citation needed] However neither the cakes nor the bomb were ever used in combat.
During the Cold War the USAF was displeased with the operational characteristics of the M114 four-pound bomblet charged with porcine brucellosis (agent US), and embarked on a crash program (St. Jo) for the E61 half-pound dumbbell bomblet with N (anthrax). [citation needed] This St. Jo program indicated the median infective dose for anthrax at 8,000 spores per person when inhaled from animal studies in monkeys. [citation needed] Prior to St. Jo, anthrax was considered a low priority biological due to its low potency in comparison with other biologicals. Since there were no human trials to support the estimated median infective dose, and concerns over persistency, the E61 was never standardized. Around the time the St. Jo Program was terminated, tularemia (agent UL) was standardized as a lethal biological in the M143 spherical bomblet, and became the main focus of the biological warfare program since there was a wealth of experimental evidence on its human infectivity. [citation needed] The military symbol was later changed to TR, and was in the United States arsenal when the offensive program was terminated in 1969, and all weapons and agents were destroyed.
An accidental release of anthrax in a research lab at Fort Detrick in Frederick, Maryland in the United States led to the permanent sealing of a building with plastics and glues.[citation needed]
The government of the Soviet Union had an active bioweapons program that included the production of hundreds of tons of weapons-grade anthrax. An overnight accident at a weapons facility in Sverdlovsk in 1979 released weaponized anthrax into the air and resulted in the deaths of at least 60 people, according to the Soviet government but facility employees think that death toll is closer to 100 (Alibek, 1999). It was the largest documented human outbreak of inhalation anthrax in history (Sternbach, 2002). There was a plant directly across the street and all of the night shift workers got sick and most died. Since most of these people were men, there were suspicions by Western governments that the Soviet Union had developed a gender-specific weapon (Alibek, 1999). The government blamed the outbreak on the consumpton of tainted meat and ordered the confiscation of all uninspected meat that entered the city. They also ordered that all stray dogs be shot and that people not have contact with sick animals. There was also a voluntary evacuation program established for people from 18-55 (Meselson et al., 1994).
To support the story, Soviet medical and legal journals published articles about an outbreak in livestock that caused GI anthrax in people who consumed the meat and cutaneous anthrax in people who came into contact with the animals. All medical and public health records were confiscated by the KGB (Meselson et al., 1994). In addition to the medical problems that the outbreak caused, it also caused Western countries to be more suspicious of a covert Soviet Bioweapons program and to increase their surveillance of suspected sites. In 1986, the American government was allowed to investigate the matter and concluded that the exposure was from aerosol anthrax from a military weapons facility (Sternbach, 2002). In 1992, President Yeltsin admitted that he was "absolutely certain" that rumors about the Soviet Union violating the 1972 Bioweapons Treaty were true. The Russians, like the US and UK, agreeed to submit information to the UN about their bioweapons programs but the Russian report omitted known facilities and never acknowledged their weapons program (Alibek, 1999).
Cultivating anthrax spores can take minimal equipment and a first-year collegiate microbiological education. However, to make an aerosol form of anthrax suitable for biological warfare (the process of "weaponizing" the spores), requires extensive training and highly advanced equipment. Bentonite is one of the few substances identified publicly that helps reduce the static charge of anthrax spores (causing them to disperse more easily).
High quality weaponized anthrax spores were used for bioterrorism in the 2001 anthrax attacks, delivered by mailing postal letters containing the spores. These events also spawned innumerable anthrax hoaxes. A scientific experiment performed by a high school student (later published in The Journal of Medical Toxicology) suggested that a common electric iron adjusted to the hottest setting (at least 400 degrees Fahrenheit) and used for at least 5 minutes should destroy all anthrax spores in a common envelope contaminated with anthrax.[4]
See also
- 2001 anthrax attacks
- Anthrax hoaxes
- Ames strain
- Sverdlovsk Anthrax leak
- Anthrax toxin
- Anthrax Detection Device
References
- ^ Artist dies from anthrax caught from animal skins Independent News and Media Limited, 17 August 2006. Retrieved 6 October 2006.
- ^ a b Bravata DM, Holty JE, Liu H, McDonald KM, Olshen RA, Owens DK (2006), Systematic review: a century of inhalation anthrax cases from 1900 to 2005, Annals of Internal Medicine; 144(4): 270-80.
- ^ Southern African News Feature :the plague wars
- ^ Pittsburgh Tribune-Review, February 2006 HAHA:high school research findings
- Alibek, K. Biohazard. New York, New York: Dell Publishing, 1999.
- "Bacillus anthracis and anthrax". Todar's Online Textbook of Bacteriology (University of Wisconsin-Madison Department of Bacteriology). Retrieved June 17.
{{cite web}}: Check date values in:|accessdate=(help); Unknown parameter|accessyear=ignored (|access-date=suggested) (help) - "Anthrax". CDC Division of Bacterial and Mycotic Diseases. Retrieved June 17.
{{cite web}}: Check date values in:|accessdate=(help); Unknown parameter|accessyear=ignored (|access-date=suggested) (help) - "Focus on anthrax". Nature.com. Retrieved June 17.
{{cite web}}: Check date values in:|accessdate=(help); Unknown parameter|accessyear=ignored (|access-date=suggested) (help) - Chanda, A., S. Ketan, and C.P. Horwitz. 2004. Fe-TAML catalysts: A safe way to decontaminate an anthrax simulant. Society of Environmental Journalists annual meeting. October 20-24. Pittsburgh.
- Meselson, M. et al. (1994). "The Sverdlovsk Outbreak of 1979". Science 266(5188) 1202-1208
- Sternbach, G. (2002). "The History of Anthrax". The Journal of Emergency Medicine 24(4) 463-467.
External links
- Anthrax - Comprehensive information from the Centers for Disease Control and Prevention (CDC)
- Bioterrorism Category A Agents - Information Resources
- Cutaneous Anthrax Images and Diagnosis Synopsis
- Anthrax Detection Device
