Locked-in syndrome
| Locked-in syndrome | |
|---|---|
| Other names | Cerebromedullospinal disconnection,[1] de-efferented state, pseudocoma,[2] ventral pontine syndrome |
 | |
| Locked-in syndrome can be caused by a stroke at the level of the basilar artery denying blood to the pons, among other causes. | |
| Specialty | Neurology, Psychiatry |
Locked-in syndrome (LIS), also known as pseudocoma, is a condition in which a patient is aware but cannot move or communicate verbally due to complete paralysis of nearly all voluntary muscles in the body except for vertical eye movements and blinking. The individual is conscious and sufficiently intact cognitively to be able to communicate with eye movements.[3] Electroencephalography results are normal in locked-in syndrome. Total locked-in syndrome, or completely locked-in state (CLIS), is a version of locked-in syndrome wherein the eyes are paralyzed as well.[4] Fred Plum and Jerome Posner coined the term for this disorder in 1966.[5][6]
Signs and symptoms
Locked-in syndrome is usually characterized by quadriplegia (loss of limb function) and the inability to speak in otherwise cognitively intact individuals. Those with locked-in syndrome may be able to communicate with others through coded messages by blinking or moving their eyes, which are often not affected by the paralysis. The symptoms are similar to those of sleep paralysis. Patients who have locked-in syndrome are conscious and aware, with no loss of cognitive function. They can sometimes retain proprioception and sensation throughout their bodies. Some patients may have the ability to move certain facial muscles, and most often some or all of the extraocular muscles. Individuals with the syndrome lack coordination between breathing and voice.[7] This prevents them from producing voluntary sounds, though the vocal cords themselves may not be paralysed.[7]
Causes
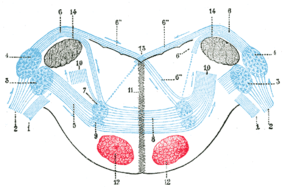
Unlike persistent vegetative state, in which the upper portions of the brain are damaged and the lower portions are spared, locked-in syndrome is essentially the opposite, caused by damage to specific portions of the lower brain and brainstem, with no damage to the upper brain.[citation needed]
Possible causes of locked-in syndrome include:
- Poisoning cases – More frequently from a krait bite and other neurotoxic venoms, as they cannot usually cross the blood–brain barrier[citation needed]
- Brainstem stroke[citation needed]
- Diseases of the circulatory system
- Medication overdose[examples needed]
- Damage to nerve cells, particularly destruction of the myelin sheath, caused by disease or osmotic demyelination syndrome (formerly designated central pontine myelinolysis) secondary to excessively rapid correction of hyponatremia [>1 mEq/L/h])[9]
- A stroke or brain hemorrhage, usually of the basilar artery[citation needed]
- Traumatic brain injury[citation needed]
- Result from lesion of the brain-stem
Curare poisoning mimics a total locked-in syndrome by causing paralysis of all voluntarily controlled skeletal muscles.[10] The respiratory muscles are also paralyzed, but the victim can be kept alive by artificial respiration.
Diagnosis
Locked-in syndrome can be difficult to diagnose. In a 2002 survey of 44 people with LIS, it took almost three months to recognize and diagnose the condition after it had begun.[11] Locked-in syndrome may mimic loss of consciousness in patients, or, in the case that respiratory control is lost, may even resemble death. People are also unable to actuate standard motor responses such as withdrawal from pain; as a result, testing often requires making requests of the patient such as blinking or vertical eye movement.[citation needed]
Brain imaging may provide additional indicators of locked-in syndrome, as brain imaging provides clues as to whether or not brain function has been lost. Additionally, an EEG can allow the observation of sleep-wake patterns indicating that the patient is not unconscious but simply unable to move.[12]
Similar conditions
- Amyotrophic lateral sclerosis (ALS)
- Bilateral brainstem tumors
- Brain death (of the whole brain or the brain stem or other part)
- Coma (deep or irreversible)
- Guillain–Barré syndrome
- Myasthenia gravis
- Poliomyelitis
- Polyneuritis
- Vegetative state (chronic or otherwise)
Treatment
Neither a standard treatment nor a cure is available. Stimulation of muscle reflexes with electrodes (NMES) has been known to help patients regain some muscle function. Other courses of treatment are often symptomatic.[13] Assistive computer interface technologies such as Dasher, combined with eye tracking, may be used to help people with LIS communicate with their environment.[citation needed]
Prognosis
It is extremely rare for any significant motor function to return. The majority of locked-in syndrome patients do not regain motor control. However, some people with the condition continue to live much longer,[14][15] while in exceptional cases, like that of Kerry Pink,[16] Gareth Shepherd,[17] Jacob Haendel[18] and Kate Allatt[19] a full spontaneous recovery may be achieved.
Research
New brain-computer interfaces (BCIs) may provide future remedies. One effort in 2002 allowed a fully locked-in patient to answer yes-or-no questions.[20][21] In 2006, researchers created and successfully tested a neural interface which allowed someone with locked-in syndrome to operate a web browser.[22] Some scientists have reported that they have developed a technique that allows locked-in patients to communicate via sniffing.[23]
See also
- Akinetic mutism
- List of people with locked-in syndrome
- The Diving Bell and the Butterfly: memoirs of journalist Jean-Dominique Bauby about his life with the condition
References
- ^ Nordgren RE, Markesbery WR, Fukuda K, Reeves AG (1971). "Seven cases of cerebromedullospinal disconnection: the "locked-in" syndrome". Neurology. 21 (11): 1140–8. doi:10.1212/wnl.21.11.1140. PMID 5166219.
- ^ Flügel KA, Fuchs HH, Druschky KF (1977). "The "locked-in" syndrome: pseudocoma in thrombosis of the basilar artery (author's trans.)". Dtsch. Med. Wochenschr. (in German). 102 (13): 465–70. doi:10.1055/s-0028-1104912. PMID 844425.
- ^ Duffy, Joseph. motor speech disorders substrates, differential diagnosis, and management. Elsevier. p. 295.
- ^ Bauer, G.; Gerstenbrand, F. & Rumpl, E. (1979). "Varieties of the locked-in syndrome". Journal of Neurology. 221 (2): 77–91. doi:10.1007/BF00313105. PMID 92545.
- ^ Agranoff, Adam B. "Stroke Motor Impairment". eMedicine. Retrieved 2007-11-29.
- ^ Plum, F; Posner, JB (1966), The diagnosis of stupor and coma, Philadelphia, PA, USA: FA Davis, 197 pp.
- ^ a b Fager, Susan; Beukelman, Dave; Karantounis, Renee; Jakobs, Tom (2006). "Use of safe-laser access technology to increase head movements in persons with severe motor impairments: a series of case reports". Augmentative and Alternative Communication. 22 (3): 222–29. doi:10.1080/07434610600650318. PMID 17114165.
- ^ Bruno MA, Schnakers C, Damas F, et al. (October 2009). "Locked-in syndrome in children: report of five cases and review of the literature". Pediatr. Neurol. 41 (4): 237–46. doi:10.1016/j.pediatrneurol.2009.05.001. PMID 19748042.
- ^ Aminoff, Michael (2015). Clinical Neurology (9nth ed.). Lange. p. 76. ISBN 978-0-07-184142-9.
- ^ Page 357 in: Damasio, Antonio R. (1999). The feeling of what happens: body and emotion in the making of consciousness. San Diego: Harcourt Brace. ISBN 978-0-15-601075-7.
- ^ León-Carrión, J.; van Eeckhout, P.; Domínguez-Morales Mdel, R.; Pérez-Santamaría, F. J. (2002). "The locked-in syndrome: a syndrome looking for a therapy". Brain Inj. 16 (7): 571–82. doi:10.1080/02699050110119781. PMID 12119076.
- ^ Maiese, Kenneth (March 2014). "Locked-in Syndrome".
- ^ Locked-in syndrome at NINDS
- ^ Joshua Foer (October 2, 2008). "The Unspeakable Odyssey of the Motionless Boy". Esquire.
- ^ Piotr Kniecicki "An art of graceful dying". Clitheroe: Łukasz Świderski, 2014, s. 73. ISBN 978-0-9928486-0-6
- ^ Stephen Nolan (August 16, 2010). "I recovered from locked-in syndrome". BBC Radio 5 Live.
- ^ "He crashed his motorbike and had a stroke - but Hampshire man Gareth Shepherd is back on his feet". Daily Echo. November 8, 2016.
- ^ "Jacob Haendel Recovery Channel". Jacob Handel Recovery. June 29, 2020.
- ^ "Woman's recovery from 'locked-in' syndrome". BBC News. March 14, 2012.
- ^ Parker, I., "Reading Minds," The New Yorker, January 20, 2003, 52–63
- ^ Keiper, Adam (Winter 2006). "The Age of Neuroelectronics". The New Atlantis. pp. 4–41. Archived from the original on 2016-02-12.
- ^ Karim AA, Hinterberger T, Richter J, Mellinger J, Neumann N, Flor H, Kübler A, Birbaumer N. "Neural internet: Web surfing with brain potentials for the completely paralyzed". Neurorehabilitation & Neural Repair. 40 (4): 508–515.
- ^ "'Locked-In' Patients Can Follow Their Noses". Science Mag. 26 Jul 2010. Retrieved 27 Dec 2016.
Further reading
- Piotr Kniecicki (2014). An Art of Graceful Dying. Lukasz Swiderski ISBN 978-0-9928486-0-6 (Autobiography, written with residual wrist movements and specially adapted computer)
