Estetrol
| |
| |
| Names | |
|---|---|
| Preferred IUPAC name
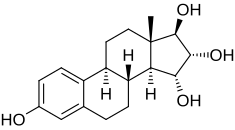
(1R,2R,3R,3aS,3bR,9bS,11aS)-11a-Methyl-2,3,3a,3b,4,5,9b,10,11,11a-decahydro-1H-cyclopenta[a]phenanthrene-1,2,3,7-tetrol | |
| Other names
Oestetrol; E4; 15α-Hydroxyestriol; Estra-1,3,5(10)-triene-3,15α,16α,17β-tetrol
| |
| Identifiers | |
3D model (JSmol)
|
|
| ChEBI | |
| ECHA InfoCard | 100.276.707 |
| KEGG | |
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| Properties | |
| C18H24O4 | |
| Molar mass | 304.386 g/mol |
| 1.38 mg/mL | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Estetrol (E4), or oestetrol, is one of the four natural estrogenic steroid hormones found in humans, along with estrone (E1), estradiol (E2), and estriol (E3), estetrol is a major estrogen in the body.[1][2] In contrast to estrone and estradiol, estetrol is a native estrogen of fetal life. Estetrol is produced exclusively by the fetal liver[1] and is found in dectable levels only during pregnancy, with relatively high levels in the fetus and lower levels in the maternal circulation.[1][2]
In addition to its physiological role as a native hormone, estetrol can be used as a medication, see estetrol (medication). E4, in combination with drospirenone, has recently been approved as a new estrogenic component of a combined oral contraceptive (COC) and E4 alone is in clinical development for the treatment of menopausal symptoms as well as breast and prostate cancer.
Biological function
So far, the physiological function of estetrol remains unknown. The potential role of estetrol as a marker for fetal well-being has been studied quite extensively, but no correlation was found[3] due to the large intra- and inter-individual variation in maternal estetrol plasma levels during pregnancy.[4][5][6][7][8]
Biological activity
[9][10] Estetrol has a moderate affinity for estrogen receptors alpha (ERα) and beta (ERβ), with Ki values of 4.9 nM and 19 nM, respectively.[9][11] As such, estetrol has 4- to 5-fold preference for ERα over ERβ.[9][11] In different animal models, the potency of estetrol regarding its estrogenic effect observed in vivo is generally 10 to 20 times lower than the potency of ethinyl estradiol (EE) and is also lower than the potency of estradiol.[1][9] Estetrol displays a highly selective binding to its primary targets ERα and ERβ[9][11], which ensures that E4 has a low risk of non-specific side effects.
| Estrogen | ER RBA (%) | Uterine weight (%) | Uterotrophy | LH levels (%) | SHBG RBA (%) |
|---|---|---|---|---|---|
| Control | – | 100 | – | 100 | – |
| Estradiol (E2) | 100 | 506 ± 20 | +++ | 12–19 | 100 |
| Estrone (E1) | 11 ± 8 | 490 ± 22 | +++ | ? | 20 |
| Estriol (E3) | 10 ± 4 | 468 ± 30 | +++ | 8–18 | 3 |
| Estetrol (E4) | 0.5 ± 0.2 | ? | Inactive | ? | 1 |
| 17α-Estradiol | 4.2 ± 0.8 | ? | ? | ? | ? |
| 2-Hydroxyestradiol | 24 ± 7 | 285 ± 8 | +b | 31–61 | 28 |
| 2-Methoxyestradiol | 0.05 ± 0.04 | 101 | Inactive | ? | 130 |
| 4-Hydroxyestradiol | 45 ± 12 | ? | ? | ? | ? |
| 4-Methoxyestradiol | 1.3 ± 0.2 | 260 | ++ | ? | 9 |
| 4-Fluoroestradiola | 180 ± 43 | ? | +++ | ? | ? |
| 2-Hydroxyestrone | 1.9 ± 0.8 | 130 ± 9 | Inactive | 110–142 | 8 |
| 2-Methoxyestrone | 0.01 ± 0.00 | 103 ± 7 | Inactive | 95–100 | 120 |
| 4-Hydroxyestrone | 11 ± 4 | 351 | ++ | 21–50 | 35 |
| 4-Methoxyestrone | 0.13 ± 0.04 | 338 | ++ | 65–92 | 12 |
| 16α-Hydroxyestrone | 2.8 ± 1.0 | 552 ± 42 | +++ | 7–24 | <0.5 |
| 2-Hydroxyestriol | 0.9 ± 0.3 | 302 | +b | ? | ? |
| 2-Methoxyestriol | 0.01 ± 0.00 | ? | Inactive | ? | 4 |
| Notes: Values are mean ± SD or range. ER RBA = Relative binding affinity to estrogen receptors of rat uterine cytosol. Uterine weight = Percentage change in uterine wet weight of ovariectomized rats after 72 hours with continuous administration of 1 μg/hour via subcutaneously implanted osmotic pumps. LH levels = Luteinizing hormone levels relative to baseline of ovariectomized rats after 24 to 72 hours of continuous administration via subcutaneous implant. Footnotes: a = Synthetic (i.e., not endogenous). b = Atypical uterotrophic effect which plateaus within 48 hours (estradiol's uterotrophy continues linearly up to 72 hours). Sources: See template. | |||||
Mode of Action
Tissue-selective effects of Estetrol
Estetrol shows selective estrogenic, neutral or anti-estrogenic activities in certain cell types and tissues.[11][12][13] In rodent models, estetrol has shown to elicit potent estrogenic activity on ovulation[14], brain[15], bone tissue[16], cardiovascular system[17], and uterus, associated with ovulation inhibition, prevention of bone demineralization, cardioprotective effects and maintenance of uterovaginal tissues, respectively.[17][18]
Data from preclinical studies also suggest that estetrol has anti-estrogenic like effects on the breast and a limited impact on normal or malignant breast tissue when used at therapeutic concentration.[13][19] This property of estetrol is associated with antagonistic effects on breast cell proliferation, migration and invasion in the presence of estradiol.[13][20]
The molecular mechanisms of action driving its tissue-selective actions rely on a specific profile of ERα activation, uncoupling nuclear and membrane activation.
In the liver, Estetrol has a neutral activity, which is reflected by a minimal impact on synthesis of hepatic coagulation factors, minimal impact on sex hormone-binding globulin (SHBG) synthesis and limited impact on lipid parameters, including triglycerides.[21]
Estetrol can therefore be described as the first Native Estrogen with Selective Tissue activity (NEST).[22][23]
Estetrol is different from selective estrogen receptor modulators (SERMs)
The selective tissue activity of estetrol is different from the effects of selective estrogen receptor modulators (SERMs), like tamoxifen and raloxifene.[24] Estetrol, like SERMs, has selective tissue activity. However, SERMs interact with the ligand binding domain of ERα in a manner that is distinct from that of estrogens, including estetrol.[24] Estetrol recruits the same co-regulators as other estrogens, while SERMs recruit other co-regulators.[23]
Estetrol activates ERα differently than other estrogens
Estrogens can elicit their effects via nuclear ERα and/or membrane ERα signaling pathways. Estetrol presents a distinctive mode of action in terms of ERα activation. Like other estrogens, estetrol binds to, and activates the nuclear ERα to induce gene transcription. However, estetrol induces very limited activity via membrane ERα in several tissues (e.g. in the breast) and antagonizes this pathway in the presence of estradiol, thereby uniquely uncoupling nuclear and membrane activation.[17]
Biochemistry
Biosynthesis
In the fetal liver, estetrol is synthesized from estradiol (E2) and estriol (E3) by two fetal liver enzymes, 15α- and 16α-hydroxylase, through hydroxylation.[25][26][27] Alternatively, estetrol is synthesized with 15α-hydroxylation of 16α-hydroxy-DHEA sulfate as an intermediate step.[28] Estetrol can be detected in maternal urine from the 9th week of gestation.[2][29][30] After birth, the neonatal liver rapidly loses its capacity to synthesize estetrol. During the second trimester of pregnancy, high levels of estetrol can be found in maternal plasma, with steadily rising concentrations of unconjugated estetrol to about 1 ng/mL (>3 nM) towards the end of pregnancy. Fetal plasma levels have been reported to be over 10 times higher than maternal plasma levels at parturition. [1]
Distribution
In terms of plasma protein binding, estetrol displays moderate binding to albumin, and shows no binding to SHBG.[31][32] The overall low plasma protein binding results in a ~50% free active fraction.[31] This compares to a 1% active form for EE and ~2% for estradiol.[33] E4 is equally distributed between red blood cells and plasma.[3]
Metabolism
Cytochrome P450 (CYP) enzymes do not play a major role in the metabolism of E4.[9] Instead, E4 undergoes extensive phase 2 metabolism in the liver to form glucuronide and sulphate conjugates.[9][12] The two main metabolites, estetrol-3-glucuronide and estetrol-16-glucuronide, have negligible estrogenic activity. (see Drospirenone/estetrol)
Excretion
Estetrol is mainly excreted in urine.[9][12] E4 is an end-stage product of metabolism, which is not converted back into active metabolites like estriol, estradiol or estrone.[11][31]
Chemistry
Estetrol, also known as 15α-hydroxyestriol or as estra-1,3,5(10)-triene-3,15α,16α,17β-tetrol, is an estrane steroid and derivative of estrin (estratriene).[9][10] It is structurally different from the other estrogens because of the presence of four hydroxyl groups, which explains the abbreviation E4.[9][10]
Synthesis
Estetrol itself is a naturally-produced estrogen by the human fetal liver. However, for human use, estetrol is synthesized from estrone, which is obtained from phytosterols extracted from soybeans. The synthesis of estetrol results in very pure estetrol (>99.9%)[34] without contaminants.
History
Estetrol was first described in 1965 by Egon Diczfalusy and coworkers at the Karolinska Institute in Stockholm, Sweden,[35][25][26][36] who identified and isolated this novel, native estrogen from late pregnancy urine and from the urine of newborn infants.
References
- ^ a b c d e Holinka CF, Diczfalusy E, Coelingh Bennink HJ (May 2008). "Estetrol: a unique steroid in human pregnancy". J. Steroid Biochem. Mol. Biol. 110 (1–2): 138–43. doi:10.1016/j.jsbmb.2008.03.027. PMID 18462934. S2CID 28007341.
- ^ a b c Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management, 3rd ed., SSC Yen and RB Jaffe (eds.), pp. 936–981, Copyright Elsevier/Saunders 1991
- ^ a b Fruzzetti, Franca; Fidecicchi, Tiziana; Montt Guevara, Maria Magdalena; Simoncini, Tommaso (2021). "Estetrol: A New Choice for Contraception". Journal of Clinical Medicine. 10 (23): 5625. doi:10.3390/jcm10235625. ISSN 2077-0383. PMC 8658652. PMID 34884326.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ J. Heikkilä, T. Luukkainen, Urinary excretion of estriol and 15a-hydroxyestriol in complicated pregnancies, Am. J. Obstet. Gynecol. 110 (1971) 509-521.
- ^ D. Tulchinsky, F.D. Frigoletto, K.J. Ryan, J. Fishman, Plasma estetrol as an index of fetal well-being, J. Clin. Endocrinol. Metab. 40 (1975) 560-567
- ^ A.D. Notation, G.E. Tagatz, Unconjugated estriol and 15a-hydroxyestriol in complicated pregnancies, Am. J. Obstet. Gynecol. 128 (1977) 747-756.
- ^ N. Kundu, M. Grant, Radioimmunoassay of 15a-hydroxyestriol (estetrol) in pregnancy serum, Steroids 27 (1976) 785-796.
- ^ N. Kundu, M. Wachs, G.B. Iverson, L.P. Petersen, Comparison of serum unconjugated estriol and estetrol in normal and complicated pregnancies, Obstet. Gynecol. 58 (1981) 276-281.
- ^ a b c d e f g h i j Coelingh Bennink HJ, Holinka CF, Diczfalusy E (2008). "Estetrol review: profile and potential clinical applications". Climacteric. 11 Suppl 1: 47–58. doi:10.1080/13697130802073425. PMID 18464023. S2CID 24003341.
- ^ a b c Visser M, Coelingh Bennink HJ (March 2009). "Clinical applications for estetrol" (PDF). J. Steroid Biochem. Mol. Biol. 114 (1–2): 85–9. doi:10.1016/j.jsbmb.2008.12.013. PMID 19167495. S2CID 32081001.
- ^ a b c d e Visser M, Foidart JM, Coelingh Bennink HJ (2008). "In vitro effects of estetrol on receptor binding, drug targets and human liver cell metabolism". Climacteric. 11 Suppl 1: 64–8. doi:10.1080/13697130802050340. PMID 18464025. S2CID 11027782.
- ^ a b c Mawet M, Maillard C, Klipping C, Zimmerman Y, Foidart JM, Coelingh Bennink HJ (2015). "Unique effects on hepatic function, lipid metabolism, bone and growth endocrine parameters of estetrol in combined oral contraceptives". Eur J Contracept Reprod Health Care. 20 (6): 463–75. doi:10.3109/13625187.2015.1068934 (inactive 28 February 2022). PMC 4699469. PMID 26212489.
{{cite journal}}: CS1 maint: DOI inactive as of February 2022 (link) - ^ a b c Gérard, C.; Blacher, S.; Communal, L.; Courtin, A.; Tskitishvili, E.; Mestdagt, M.; Munaut, C.; Noel, A.; Gompel, A.; Péqueux, C.; Foidart, J. M. (2015). "Estetrol is a weak estrogen antagonizing estradiol-dependent mammary gland proliferation". The Journal of Endocrinology. 224 (1): 85–95. doi:10.1530/JOE-14-0549. ISSN 1479-6805. PMID 25359896.
- ^ Bennink, Herjan J. T. Coelingh; Skouby, Sven; Bouchard, Philippe; Holinka, Christian F. (2008-03-01). "Ovulation inhibition by estetrol in an in vivo model". Contraception. 77 (3): 186–190. doi:10.1016/j.contraception.2007.11.014. ISSN 0010-7824.
- ^ Pluchino, N.; Santoro, A. N.; Casarosa, E.; Giannini, A.; Genazzani, A.; Russo, M.; Russo, N.; Petignat, P.; Genazzani, A. R. (2014-09-01). "Effect of estetrol administration on brain and serum allopregnanolone in intact and ovariectomized rats". The Journal of Steroid Biochemistry and Molecular Biology. 143: 285–290. doi:10.1016/j.jsbmb.2014.04.011. ISSN 0960-0760.
- ^ Coelingh Bennink, H. J. T.; Heegaard, A.-M.; Visser, M.; Holinka, C. F.; Christiansen, C. (2008-01-01). "Oral bioavailability and bone-sparing effects of estetrol in an osteoporosis model". Climacteric. 11 (sup1): 2–14. doi:10.1080/13697130701798692. ISSN 1369-7137. PMID 18464016.
- ^ a b c Abot, Anne; Fontaine, Coralie; Buscato, Mélissa; Solinhac, Romain; Flouriot, Gilles; Fabre, Aurélie; Drougard, Anne; Rajan, Shyamala; Laine, Muriel; Milon, Alain; Muller, Isabelle (2014). "The uterine and vascular actions of estetrol delineate a distinctive profile of estrogen receptor α modulation, uncoupling nuclear and membrane activation". EMBO Molecular Medicine. 6 (10): 1328–1346. doi:10.15252/emmm.201404112. ISSN 1757-4676. PMC 4287935. PMID 25214462.
- ^ Benoit, Thibaut; Valera, Marie-Cecile; Fontaine, Coralie; Buscato, Melissa; Lenfant, Francoise; Raymond-Letron, Isabelle; Tremollieres, Florence; Soulie, Michel; Foidart, Jean-Michel; Game, Xavier; Arnal, Jean-Francois (2017-11-01). "Estetrol, a Fetal Selective Estrogen Receptor Modulator, Acts on the Vagina of Mice through Nuclear Estrogen Receptor α Activation". The American Journal of Pathology. 187 (11): 2499–2507. doi:10.1016/j.ajpath.2017.07.013. ISSN 0002-9440. PMID 28827141.
- ^ Gallez, Anne; Blacher, Silvia; Maquoi, Erik; Konradowski, Erika; Joiret, Marc; Primac, Irina; Gérard, Céline; Taziaux, Mélanie; Houtman, René; Geris, Liesbet; Lenfant, Françoise (2021). "Estetrol Combined to Progestogen for Menopause or Contraception Indication Is Neutral on Breast Cancer". Cancers. 13 (10): 2486. doi:10.3390/cancers13102486. ISSN 2072-6694. PMC 8160902. PMID 34065180.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Giretti, Maria Silvia; Montt Guevara, Maria Magdalena; Cecchi, Elena; Mannella, Paolo; Palla, Giulia; Spina, Stefania; Bernacchi, Guja; Di Bello, Silvia; Genazzani, Andrea Riccardo; Genazzani, Alessandro D.; Simoncini, Tommaso (2014-05-26). "Effects of Estetrol on Migration and Invasion in T47-D Breast Cancer Cells through the Actin Cytoskeleton". Frontiers in Endocrinology. 5. doi:10.3389/fendo.2014.00080. ISSN 1664-2392. PMC 4033260. PMID 24904530.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ Klipping, Christine; Duijkers, Ingrid; Mawet, Marie; Maillard, Catherine; Bastidas, Adriana; Jost, Maud; Foidart, Jean-Michel (2021). "Endocrine and metabolic effects of an oral contraceptive containing estetrol and drospirenone". Contraception. 103 (4): 213–221. doi:10.1016/j.contraception.2021.01.001.
- ^ Gérard, C.; Jost, M.; Oligschläger, Y.; Foidart, JM. (2021). "Estetrol, a natural estrogen with selective tissue activity (NEST). Poster Abstract". International Journal of Gynecology & Obstetrics. 155: 127–532.
- ^ a b Gérard, Céline; Arnal, Jean-François; Jost, Maud; Douxfils, Jonathan; Lenfant, Françoise; Fontaine, Coralie; Houtman, René; Archer, David F.; Reid, Robert L.; Lobo, Rogerio A.; Gaspard, Ulysse (2022-02-01). "Profile of estetrol, a promising native estrogen for oral contraception and the relief of climacteric symptoms of menopause". Expert Review of Clinical Pharmacology. 15 (2): 121–137. doi:10.1080/17512433.2022.2054413. ISSN 1751-2433.
- ^ a b Garefalakis, Maria; Hickey, Martha (2008-03-07). "Role of androgens, progestins and tibolone in the treatment of menopausal symptoms: a review of the clinical evidence". Clinical Interventions in Aging. 3 (1): 1–8. doi:10.2147/CIA.S1043. PMC 2544356. PMID 18488873.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ a b J. Schwers, G. Eriksson, N. Wiqvist, E. Diczfalusy, 15a-hydroxylation: A new pathway of estrogen metabolism in the human fetus and newborn, Biochim. Biophys. Acta. 100 (1965) 313-316
- ^ a b J. Schwers, M. Govaerts-Videtsky, N. Wiqvist, E. Diczfalusy, Metabolism of oestrone sulphate by the previable human foetus, Acta Endocrinol. 50 (1965) 597-610.
- ^ S. Mancuso, G. Benagiano, S. Dell’Acqua, M. Shapiro, N. Wiqvist, E. Diczfalusy, Studies on the metabolism of C-19 steroids in the human foeto-placental unit, Acta Endocrinol. 57 (1968) 208-227.
- ^ Jerome Frank Strauss; Robert L. Barbieri (2009). Yen and Jaffe's Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management. Elsevier Health Sciences. pp. 262–. ISBN 978-1-4160-4907-4.
- ^ J. Heikkilä, H. Adlercreutz, A method for the determination of urinary 15α-hydroxyestriol and estriol, J. Steroid Biochem. 1 (1970) 243-253
- ^ J. Heikkilä, Excretion of 15α-hydroxyestriol and estriol in maternal urine during normal pregnancy, J. Steroid Biochem. 2 (1971) 83-93.
- ^ a b c Visser M, Holinka CF, Coelingh Bennink HJ (2008). "First human exposure to exogenous single-dose oral estetrol in early postmenopausal women". Climacteric. 11 Suppl 1: 31–40. doi:10.1080/13697130802056511. PMID 18464021. S2CID 23568599.
- ^ Hammond GL, Hogeveen KN, Visser M, Coelingh Bennink HJ (2008). "Estetrol does not bind sex hormone binding globulin or increase its production by human HepG2 cells". Climacteric. 11 Suppl 1: 41–6. doi:10.1080/13697130701851814. PMID 18464022. S2CID 22715507.
- ^ Stanczyk, Frank Z.; Archer, David F.; Bhavnani, Bhagu R. (2013-06-01). "Ethinyl estradiol and 17beta-estradiol in combined oral contraceptives: pharmacokinetics, pharmacodynamics and risk assessment". Contraception. 87 (6): 706–727. doi:10.1016/j.contraception.2012.12.011. ISSN 0010-7824.
- ^ Warmerdam EG, Visser M, Coelingh Bennink HJ, Groen M (2008). "A new route of synthesis of estetrol". Climacteric. 11 Suppl 1: 59–63. doi:10.1080/13697130802054078. PMID 18464024. S2CID 42017011.
- ^ Hagen AA, Barr M, Diczfalusy E (June 1965). "Metabolism of 17-beta-oestradiol-4-14-C in early infancy". Acta Endocrinol. 49 (2): 207–20. doi:10.1530/acta.0.0490207. PMID 14303250.
- ^ Zucconi, G.; Lisboa, B. P.; Simonitsch, E.; Roth, L.; Hagen, A. A.; Diczfalusy, E. (1967). "ISOLATION OF 15α-HYDROXY-OESTRIOL FROM PREGNANCY URINE AND FROM THE URINE OF NEWBORN INFANTS". Acta Endocrinologica. 56 (3): 413–423. doi:10.1530/acta.0.0560413. ISSN 0804-4643.

