Airborne transmission

Airborne or aerosol transmission is transmission of an infectious disease through small particles suspended in the air.[2] Infectious diseases capable of airborne transmission include many of considerable importance both in human and veterinary medicine. The relevant infectious agent may be viruses, bacteria, or fungi, and they may be spread through breathing, talking, coughing, sneezing, raising of dust, spraying of liquids, flushing toilets, or any activities which generate aerosol particles or droplets.
This is the transmission of diseases via transmission of an infectious agent, and does not include diseases caused by air pollution.
Aerosol transmission has traditionally has been considered distinct from transmission by droplets, but this distinction is no longer used.[3][4] Respiratory droplets were thought to rapidly fall to the ground after emission:[5] but smaller droplets and aerosols also contain live infectious agents and behave differently.[4] Individuals generate aerosols and droplets across a wide range of sizes and concentrations, and the amount produced varies widely by person and activity.[6] Larger droplets greater than 100 μm usually settle within 2 m.[6][5] Smaller particles can carry airborne pathogens for extended periods of time. While the concentration of airborne pathogens is greater within 2m, they can travel farther and concentrate in a room.[4]
The traditional size cutoff of 5 μm between airborne and respiratory droplets has been discarded, as exhaled particles form a continuum of sizes whose fates depend on environmental conditions in addition to their initial sizes. This error has informed hospital based transmission based precautions for decades.[6] Indoor respiratory secretion transfer data suggest that droplets/aerosols in the 20 μm size range initially travel with the air flow from cough jets and air conditioning like aerosols,[7] but fall out gravitationally at a greater distance as "jet riders".[8] As this size range is most efficiently filtered out in the nasal mucosa,[9] the primordial infection site in COVID-19, aerosols/droplets[10] in this size range may contribute to driving the COVID-19 pandemic.
Overview
Airborne diseases can be transmitted from one individual to another through the air. The pathogens transmitted may be any kind of microbe, and they may be spread in aerosols, dust or droplets. The aerosols might be generated from sources of infection such as the bodily secretions of an infected individual, or biological wastes. Infectious aerosols may stay suspended in air currents long enough to travel for considerable distances; sneezes, for example, can easily project infectious droplets for dozens of feet (ten or more meters).[11]
Airborne pathogens or allergens typically enter the body via the nose, throat, sinuses and lungs. Inhalation of these pathogens affects the respiratory system and can then spread to the rest of the body. Sinus congestion, coughing and sore throats are examples of inflammation of the upper respiratory airway. Air pollution plays a significant role in airborne diseases. Pollutants can influence lung function by increasing air way inflammation.[12]
Common infections that spread by airborne transmission include COVID-19;[13] measles morbillivirus,[14] chickenpox virus;[15] Mycobacterium tuberculosis, influenza virus, enterovirus, norovirus and less commonly coronavirus, adenovirus, and possibly respiratory syncytial virus.[16]
Poor ventilation enhances transmission by allowing aerosols to spread undisturbed in an indoor space.[17] Crowded rooms are more likely to contain an infected person. The longer a susceptible person stays in such a space, the greater chance of transmission. Airborne transmission is complex, and hard to demonstrate unequivocally[18] but the Wells-Riley model can be used to make simple estimates of infection probability.[19]
Some airborne diseases can affect non-humans. For example, Newcastle disease is an avian disease that affects many types of domestic poultry worldwide that is airborne.[20]
Airborne transmission can be classified as obligate, preferential, or opportunistic. Obligate airborne infections spread only through aerosols; the most common example of this category is tuberculosis. Preferential airborne infections, such as chicken pox, can be obtained through different routes, but mainly by aerosols. Opportunistic airborne infections such as influenza typically transmit through other routes; however, under favourable conditions, aerosol transmission can occur.[21] Because the drying process can damage the pathogens, the number of airborne diseases is limited.[15]
Transmission
Environmental factors influence the efficacy of airborne disease transmission; the most evident environmental conditions are temperature and relative humidity.[22][23] The transmission of airborne diseases is affected by all the factors that influence temperature and humidity, in both meteorological (outdoor) and human (indoor) environments. Circumstances influencing the spread of droplets containing infectious particles can include pH, salinity, wind, air pollution, and solar radiation as well as human behavior.[24]
Airborne infections usually land in the respiratory system, with the agent present in aerosols (infectious particles < 5 µm in diameter).[25] This includes dry particles, often the remnant of an evaporated wet particle called nuclei, and wet particles.
- Relative humidity (RH) plays an important role in the evaporation of droplets and the distance they travel. 30 μm droplets evaporate in seconds.[26] The CDC recommends a minimum of 40% RH indoors[27] to significantly reduce the infectivity of aerosolized virus. An ideal humidity for preventing aerosol respiratory viral transmission at room temperature appears to be between 40% and 60% RH. If the relative humidity goes below 35% RH, infectious virus stays longer in the air.
- The number of rainy days[28] (more important than total precipitation);[29][30] mean daily sunshine hours;[31] latitude and altitude[29] are relevant when assessing the possibility of spread of airborne disease. Some infrequent or exceptional events influence the dissemination of airborne diseases, including tropical storms, hurricanes, typhoons, or monsoons.[32]
- Climate affects temperature, winds and relative humidity, the main factors affecting the spread, duration and infectiousness of droplets containing infectious particles.[22] The influenza virus spreads easily in the Northern Hemisphere winter due to climate conditions that favour the infectiousness of the virus.[24]
- Isolated weather events decrease the concentration of airborne fungal spores; a few days later, number of spores increases exponentially.[33]
- Socioeconomics has a minor role in airborne disease transmission. In cities, airborne disease spreads more rapidly than in rural areas and urban outskirts. Rural areas generally favor higher airborne fungal dissemination.[34]
- Proximity to large bodies of water such as rivers and lakes can enhance airborne disease.[32]
- Poor maintenance of air conditioning systems has led to outbreaks of Legionella pneumophila.[35]
- Hospital-acquired airborne diseases are associated with poorly-resourced medical systems, which make isolation challenging.[citation needed]
- Air conditioning may reduce transmission by removing contaminated air, but may also contribute to the spread of respiratory secretions inside a room.[7]
Prevention
A layered risk-management approach to slowing the spread of a transmissable disease attempts to minimize risk through multiple layers of interventions. Each intervention has the potential to reduce risk. A layered approach can include interventions by individuals (e.g. mask wearing, hand hygiene), institutions (e.g. surface disinfection, ventilation, and air filtration measures to control the indoor environment), the medical system (e.g. vaccination) and public health at the population level (e.g. testing, quarantine, and contact tracing).[4]
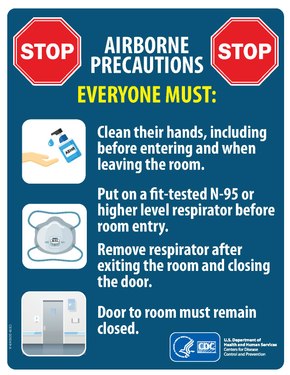
Preventive techniques can include disease-specific immunization as well as nonpharmaceutical interventions such as wearing a respirator and limiting time spent in the presence of infected individuals.[36] Wearing a face mask can lower the risk of airborne transmission to the extent that it limits the transfer of airborne particles between individuals.[37] The type of mask that is effective against airborne transmission is dependent on the size of the particles. While fluid-resistant surgical masks prevent large droplet inhalation, smaller particles which form aerosols require a higher level of protection with filtration masks rated at N95 (US) or FFP3 (EU) required.[38] Use of FFP3 masks by staff managing patients with COVID-19 reduced acquisition of COVID-19 by staff members.[39]
Engineering solutions which aim to control or eliminate exposure to a hazard are higher on the hierarchy of control than personal protective equipment (PPE). At the level of physically based engineering interventions, effective ventilation and high frequency air changes, or air filtration through high efficiency particulate filters, reduce detectable levels of virus and other bioaerosols, improving conditions for everyone in an area.[4][40] Portable air filters, such as those tested in Conway Morris A et al. present a readily deployable solution when existing ventilation is inadequate, for instance in repurposed COVID-19 hospital facilities.[40]
The United States Centers for Disease Control and Prevention (CDC) advises the public about vaccination and following careful hygiene and sanitation protocols for airborne disease prevention.[41] Many public health specialists recommend physical distancing (also known as social distancing) to reduce transmission.[42]
A 2011 study concluded that vuvuzelas (a type of air horn popular e.g. with fans at football games) presented a particularly high risk of airborne transmission, as they were spreading a much higher number of aerosol particles than e.g., the act of shouting.[43]
Exposure does not guarantee infection, as infection is dependent on host immune system competency plus the quantity of infectious particles ingested.[36] Antibiotics may be used in dealing with airborne bacterial primary infections, such as pneumonic plague.[44]
See also
- Aeroplankton
- Basic reproduction number
- Miasma theory
- Vector (epidemiology)
- Waterborne diseases
- Zoonosis
References
- ^ "Transmission-Based Precautions". U.S. Centers for Disease Control and Prevention. 7 January 2016. Retrieved 31 March 2020.
- ^ Siegel JD, Rhinehart E, Jackson M, Chiarello L, Healthcare Infection Control Practices Advisory Committee. "2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings" (PDF). CDC. p. 19. Retrieved 7 February 2019.
Airborne transmission occurs by dissemination of either airborne droplet nuclei or small particles in the respirable size range containing infectious agents that remain infective over time and distance
- ^ Tang, Julian W.; Marr, Linsey C.; Li, Yuguo; Dancer, Stephanie J. (14 April 2021). "Covid-19 has redefined airborne transmission". BMJ. 373: n913. doi:10.1136/bmj.n913. ISSN 1756-1833. PMID 33853842. S2CID 233235666.
- ^ a b c d e McNeill, VF (10 June 2022). "Airborne Transmission of SARS-CoV-2: Evidence and Implications for Engineering Controls". Annual Review of Chemical and Biomolecular Engineering. 13 (1): 123–140. doi:10.1146/annurev-chembioeng-092220-111631. ISSN 1947-5438. Retrieved 13 June 2022.
- ^ a b Zhang N, Chen W, Chan PT, Yen HL, Tang JW, Li Y (July 2020). "Close contact behavior in indoor environment and transmission of respiratory infection". Indoor Air. 30 (4): 645–661. doi:10.1111/ina.12673. PMID 32259319.
- ^ a b c Staudt A, Saunders J, Pavlin J, Shelton-Davenport M, et al. (Environmental Health Matters Initiative, National Academies of Sciences, Engineering, and Medicine) (22 October 2020). Shelton-Davenport M, Pavlin J, Saunders J, Staudt A (eds.). Airborne Transmission of SARS-CoV-2: Proceedings of a Workshop in Brief. Washington, D.C.: National Academies Press. doi:10.17226/25958. ISBN 978-0-309-68408-8. PMID 33119244.
- ^ a b Hunziker, Patrick (1 October 2021). "Minimising exposure to respiratory droplets, 'jet riders' and aerosols in air-conditioned hospital rooms by a 'Shield-and-Sink' strategy". BMJ Open. 11 (10): e047772. doi:10.1136/bmjopen-2020-047772. ISSN 2044-6055. PMID 34642190.
- ^ Hunziker P (16 December 2020). "Minimizing exposure to respiratory droplets, 'jet riders' and aerosols in air-conditioned hospital rooms by a 'Shield-and-Sink' strategy". doi:10.1101/2020.12.08.20233056. S2CID 229291099.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Kesavanathan J, Swift DL (January 1998). "Human Nasal Passage Particle Deposition: The Effect of Particle Size, Flow Rate, and Anatomical Factors". Aerosol Science and Technology. 28 (5): 457–463. Bibcode:1998AerST..28..457K. doi:10.1080/02786829808965537. ISSN 0278-6826.
- ^ Adlish, John I.; Neuhold, Piero; Surrente, Riccardo; Tagliapietra, Luca J. (18 June 2021). "RNA Identification and Detection of Nucleic Acids as Aerosols in Air Samples by Means of Photon and Electron Interactions". Instruments. 5 (2): 23. arXiv:2105.00340. doi:10.3390/instruments5020023.
- ^ "Ack! Sneeze germs carry farther than you think".
- ^ "Airborne diseases". Archived from the original on 28 June 2012. Retrieved 21 May 2013.
- ^ "COVID-19: epidemiology, virology and clinical features". GOV.UK. Retrieved 24 October 2020.
- ^ Riley EC, Murphy G, Riley RL (May 1978). "Airborne spread of measles in a suburban elementary school". American Journal of Epidemiology. 107 (5): 421–32. doi:10.1093/oxfordjournals.aje.a112560. PMID 665658.
- ^ a b "FAQ: Methods of Disease Transmission". Mount Sinai Hospital (Toronto). Retrieved 31 March 2020.
- ^ La Rosa G, Fratini M, Della Libera S, Iaconelli M, Muscillo M (1 June 2013). "Viral infections acquired indoors through airborne, droplet or contact transmission". Annali dell'Istituto Superiore di Sanità. 49 (2): 124–32. doi:10.4415/ANN_13_02_03. PMID 23771256.
- ^ Noakes CJ, Beggs CB, Sleigh PA, Kerr KG (October 2006). "Modelling the transmission of airborne infections in enclosed spaces". Epidemiology and Infection. 134 (5): 1082–91. doi:10.1017/S0950268806005875. PMC 2870476. PMID 16476170.
- ^ Tang JW, Bahnfleth WP, Bluyssen PM, Buonanno G, Jimenez JL, Kurnitski J, et al. (April 2021). "Dismantling myths on the airborne transmission of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)". The Journal of Hospital Infection. 110: 89–96. doi:10.1016/j.jhin.2020.12.022. PMC 7805396. PMID 33453351.
- ^ Sze To GN, Chao CY (February 2010). "Review and comparison between the Wells-Riley and dose-response approaches to risk assessment of infectious respiratory diseases". Indoor Air. 20 (1): 2–16. doi:10.1111/j.1600-0668.2009.00621.x. PMC 7202094. PMID 19874402.
- ^ Mitchell BW, King DJ (October–December 1994). "Effect of negative air ionization on airborne transmission of Newcastle disease virus". Avian Diseases. 38 (4): 725–32. doi:10.2307/1592107. JSTOR 1592107. PMID 7702504.
- ^ Seto WH (April 2015). "Airborne transmission and precautions: facts and myths". The Journal of Hospital Infection. 89 (4): 225–8. doi:10.1016/j.jhin.2014.11.005. PMC 7132528. PMID 25578684.
- ^ a b Ma, Y; Pei, S; Shaman, J; Dubrow, R; Chen, K (14 June 2021). "Role of meteorological factors in the transmission of SARS-CoV-2 in the United States". Nature Communications. 12 (1): 3602. doi:10.1038/s41467-021-23866-7. ISSN 2041-1723. Retrieved 13 June 2022.
- ^ Božič, A; Kanduč, M (1 March 2021). "Relative humidity in droplet and airborne transmission of disease". Journal of Biological Physics. 47 (1): 1–29. doi:10.1007/s10867-020-09562-5. ISSN 1573-0689. Retrieved 13 June 2022.
- ^ a b Sooryanarain, H; Elankumaran, S (16 February 2015). "Environmental Role in Influenza Virus Outbreaks". Annual Review of Animal Biosciences. 3 (1): 347–373. doi:10.1146/annurev-animal-022114-111017. ISSN 2165-8102. Retrieved 13 June 2022.
- ^ "Prevention of hospital-acquired infections" (PDF). World Health Organization (WHO).
- ^ Bahl P, Doolan C, de Silva C, Chughtai AA, Bourouiba L, MacIntyre CR (April 2020). "Airborne or droplet precautions for health workers treating COVID-19?". The Journal of Infectious Diseases. doi:10.1093/infdis/jiaa189. PMC 7184471. PMID 32301491.
- ^ Noti JD, Blachere FM, McMillen CM, Lindsley WG, Kashon ML, Slaughter DR, Beezhold DH (2013). "High humidity leads to loss of infectious influenza virus from simulated coughs". PLOS ONE. 8 (2): e57485. Bibcode:2013PLoSO...857485N. doi:10.1371/journal.pone.0057485. PMC 3583861. PMID 23460865.
- ^ Pica N, Bouvier NM (February 2012). "Environmental factors affecting the transmission of respiratory viruses". Current Opinion in Virology. 2 (1): 90–5. doi:10.1016/j.coviro.2011.12.003. PMC 3311988. PMID 22440971.
- ^ a b Rodríguez-Rajo FJ, Iglesias I, Jato V (April 2005). "Variation assessment of airborne Alternaria and Cladosporium spores at different bioclimatical conditions". Mycological Research. 109 (Pt 4): 497–507. CiteSeerX 10.1.1.487.177. doi:10.1017/s0953756204001777. PMID 15912938.
- ^ Peternel R, Culig J, Hrga I (2004). "Atmospheric concentrations of Cladosporium spp. and Alternaria spp. spores in Zagreb (Croatia) and effects of some meteorological factors". Annals of Agricultural and Environmental Medicine. 11 (2): 303–7. PMID 15627341.
- ^ Sabariego S, Díaz de la Guardia C, Alba F (May 2000). "The effect of meteorological factors on the daily variation of airborne fungal spores in Granada (southern Spain)". International Journal of Biometeorology. 44 (1): 1–5. Bibcode:2000IJBm...44....1S. doi:10.1007/s004840050131. PMID 10879421. S2CID 17834418.
- ^ a b Hedlund C, Blomstedt Y, Schumann B (2014). "Association of climatic factors with infectious diseases in the Arctic and subarctic region--a systematic review". Global Health Action. 7: 24161. doi:10.3402/gha.v7.24161. PMC 4079933. PMID 24990685.
- ^ Khan NN, Wilson BL (2003). "An environmental assessment of mold concentrations and potential mycotoxin exposures in the greater Southeast Texas area". Journal of Environmental Science and Health. Part A, Toxic/Hazardous Substances & Environmental Engineering. 38 (12): 2759–72. doi:10.1081/ESE-120025829. PMID 14672314. S2CID 6906183.
- ^ Tang JW (December 2009). "The effect of environmental parameters on the survival of airborne infectious agents". Journal of the Royal Society, Interface. 6 Suppl 6: S737-46. doi:10.1098/rsif.2009.0227.focus. PMC 2843949. PMID 19773291.
- ^ "Legionnaire disease". Retrieved 12 April 2015.
- ^ a b American Academy of Orthopaedic Surgeons (AAOS) (2011). Bloodborne and Airborne Pathogens. Jones & Barlett Publishers. p. 2. ISBN 9781449668273. Retrieved 21 May 2013.
- ^ Clark RP, de Calcina-Goff ML (December 2009). "Some aspects of the airborne transmission of infection". Journal of the Royal Society, Interface. 6 Suppl 6 (suppl_6): S767-82. doi:10.1098/rsif.2009.0236.focus. PMC 2843950. PMID 19815574.
- ^ "Transmission-Based Precautions | Basics | Infection Control | CDC". www.cdc.gov. 6 February 2020. Retrieved 14 October 2021.
- ^ Ferris, Mark; Ferris, Rebecca; Workman, Chris; O'Connor, Eoin; Enoch, David A; Goldesgeyme, Emma; Quinnell, Natalie; Patel, Parth; Wright, Jo; Martell, Geraldine; Moody, Christine (24 June 2021). "FFP3 respirators protect healthcare workers against infection with SARS-CoV-2". doi:10.22541/au.162454911.17263721/v1.
{{cite journal}}: Cite journal requires|journal=(help) - ^ a b Conway Morris, Andrew; Sharrocks, Katherine; Bousfield, Rachel; Kermack, Leanne; Maes, Mailis; Higginson, Ellen; Forrest, Sally; Pereira-Dias, Joana; Cormie, Claire; Old, Tim; Brooks, Sophie (30 October 2021). "The removal of airborne SARS-CoV-2 and other microbial bioaerosols by air filtration on COVID-19 surge units". Clinical Infectious Diseases: ciab933. doi:10.1093/cid/ciab933. ISSN 1058-4838.
- ^ "Redirect - Vaccines: VPD-VAC/VPD menu page". 7 February 2019.
- ^ Glass RJ, Glass LM, Beyeler WE, Min HJ (November 2006). "Targeted social distancing design for pandemic influenza". Emerging Infectious Diseases. 12 (11): 1671–81. doi:10.3201/eid1211.060255. PMC 3372334. PMID 17283616.
- ^ Lai KM, Bottomley C, McNerney R (23 May 2011). "Propagation of respiratory aerosols by the vuvuzela". PLOS ONE. 6 (5): e20086. Bibcode:2011PLoSO...620086L. doi:10.1371/journal.pone.0020086. PMC 3100331. PMID 21629778.
- ^ Ziady LE, Small N (2006). Prevent and Control Infection: Application Made Easy. Juta and Company Ltd. pp. 119–120. ISBN 9780702167904.
