Artificial cardiac pacemaker

- For other uses see Pacemaker (disambiguation)
A pacemaker (or artificial pacemaker, so as not to be confused with the heart's natural pacemaker) is a medical device which uses electrical impulses, delivered by electrodes contacting the heart muscles, to regulate the beating of the heart. The primary purpose of a pacemaker is to maintain an adequate heart rate, either because the heart's native pacemaker is not fast enough, or there is a block in the heart's electrical conduction system. Modern pacemakers are externally programmable and allow the cardiologist to select the optimum pacing modes for individual patients. Some combine a pacemaker and implantable defibrillator in a single implantable device. Others have multiple electrodes stimulating differing positions within the heart to improve synchronisation of the lower chambers of the heart.
History of the artificial pacemaker
In 1889, J A McWilliam reported in the British Medical Journal of his experiments in which application of an electrical impulse to the human heart in asystole caused a ventricular contraction and that a heart rhythm of 60-70 beats per minute could be evoked by impulses applied at spacings equal to 60-70/minute.[1]
In 1928, Dr Mark C Lidwell of the Royal Prince Alfred Hospital of Sydney, supported by physicist Edgar H Booth of the University of Sydney, devised a portable apparatus which "plugged into a lighting point" and in which "One pole was applied to a skin pad soaked in strong salt solution" while the other pole "consisted of a needle insulated except at its point, and was plunged into the appropriate cardiac chamber". "The pacemaker rate was variable from about 80 to 120 pulses per minute, and likewise the voltage variable from 1.5 to 120 volts" The apparatus was used to revive a stillborn infant at Crown Street Women's Hospital, Sydney whose heart continued "to beat on its own accord", "at the end of 10 minutes" of stimulation.[2][3]
In 1932, American physiologist Albert Hyman, working independently, described an electro-mechanical instrument of his own, powered by a spring-wound hand-cranked motor. Hyman himself referred to his invention as an "artificial pacemaker", the term continuing in use to this day.[4][5]
An apparent hiatus in publication of research conducted between the early 1930s and World War II may be attributed to the public perception of interfering with nature by 'reviving the dead'. For example, "Hyman did not publish data on the use of his pacemaker in humans because of adverse publicity, both among his fellow physicians, and due to newspaper reporting at the time. Lidwell may have been aware of this and did not proceed with his experiments in humans".[3]
An external pacemaker was designed and built by the Canadian electrical engineer John Hopps in 1950 based upon observations by cardio-thoracic surgeon Wilfred Gordon Bigelow at Toronto General Hospital . A substantial external device using vacuum tube technology to provide transcutaneous pacing, it was somewhat crude and painful to the patient in use and, being powered from an AC wall socket, carried a potential hazard of electrocution of the patient by inducing ventricular fibrillation.
A number of innovators, including Paul Zoll, made smaller but still bulky transcutaneous pacing devices in the following years using a large rechargeable battery as the power supply.[6]
In 1957, Dr. William L. Weirich published the results of research performed at the University of Minnesota. These studies demonstrated the restoration of heart rate, cardiac output and mean aortic pressures in animal subjects with complete heart block through the use of a myocardial electrode. This effective control of postsurgical heart block proved to be a significant contribution to decreasing mortality of open heart surgery in this time period.[7]
The development of the silicon transistor and its first commercial availability in 1956 was the pivotal event which led to rapid development of practical cardiac pacemaking.
In 1957, engineer Earl Bakken of Minneapolis, Minnesota, produced the first wearable external pacemaker for a patient of Dr. C. Walton Lillehei. This transistorised pacemaker, housed in a small plastic box, had controls to permit adjustment of pacing heart rate and output voltage and was connected to electrode leads which passed through the skin of the patient to terminate in electrodes attached to the surface of the myocardium of the heart.
The first clinical implantation into a human of a fully implantable pacemaker was in 1958 at the Karolinska University Hospital in Solna, Sweden, using a pacemaker designed by Rune Elmqvist and surgeon Åke Senning, connected to electrodes attached to the myocardium of the heart by thoracotomy. The device failed after three hours. A second device was then implanted which lasted for two days. The world's first implantable pacemaker patient, Arne Larsson, went on to receive 26 different pacemakers during his lifetime. He died in 2001, at the age of 86[8].
In 1959, temporary transvenous pacing was first demonstrated by Furman et al in which the catheter electrode was inserted via the patient's basilic vein.[9]
In February 1960, an improved version of the Swedish Elmqvist design was implanted in Montevideo, Uruguay in the Casmu Hospital by Doctors Fiandra and Rubio. That device lasted until the patient died of other ailments, 9 months later. The early Swedish-designed devices used rechargeable batteries, which were charged by an induction coil from the outside.
Implantable pacemakers constructed by engineer Wilson Greatbatch entered use in humans from April 1960 following extensive animal testing. The Greatbatch innovation varied from the earlier Swedish devices in using primary cells (mercury battery) as the energy source. The first patient lived for a further 18 months.
The first use of transvenous pacing in conjunction with an implanted pacemaker was by Parsonnet in the USA [10][11], Lageren in Sweden[12][13] and Jean-Jaques Welti in France[14] in 1962-63. The transvenous, or pervenous, procedure involved incision of a vein into which was inserted the catheter electrode lead under fluoroscopic guidance, until it was lodged within the trabeculae of the right ventricle. This method was to become the method of choice by the mid-1960s.

The preceding implantable devices all suffered from the unreliability and short lifetime of the available primary cell technology which was mainly that of the mercury battery.
In the late 1960s, several companies, including ARCO in the USA, developed isotope powered pacemakers, but this development was overtaken by the development in 1970 of the lithium-iodide cell by Wilson Greatbatch. Lithium-iodide or lithium anode cells became the standard for future pacemaker designs.
A further impediment to reliability of the early devices was the diffusion of water vapour from the body fluids through the epoxy resin encapsulation affecting the electronic circuitry. This phenomenon was overcome by encasing the pacemaker generator in an hermetically sealed metal case, initially by Telectronics of Australia in 1969 followed by Cardiac Pacemakers Inc of Minneapolis in 1972. This technology, using titanium as the encasing metal, became the standard by the mid-1970s.
Others who contributed significantly to the technological development of the pacemaker in the pioneering years were Bob Anderson of Medtronic Minneapolis, J.G (Geoffrey) Davies of St George's Hospital London, Barouh Berkovits and Sheldon Thaler of American Optical, Geoffrey Wickham of Telectronics Australia, Walter Keller of Cordis Corp. of Miami, Hans Thornander who joined previously mentioned Rune Elmquist of Elema-Schonander in Sweden, Janwillem van den Berg of Holland and Anthony Adducci of Cardiac Pacemakers Inc.(Guidant)
Applications
Artificial pacemakers can be used in order to help with and/or treat these conditions:
- Sinus node dysfunction - when the sinoatrial node does not fire properly to contract the heart
- Bifascicular block, trifascicular block, or third degree AV block.
- Stokes-Adams attack involving disruption of conduction between the sinoatrial node and the atrioventricular node.
Methods of pacing
Percussive Pacing
Percussive Pacing, also known as Transthoracic Mechanical Pacing, is the use of the closed fist, usually on the left lower edge of the sternum over the right ventricle, striking from a distance of 20 - 30 cm to induce a ventricular beat (the British Journal of Anesthesia suggests this must be done to raise the ventricular pressure to 10 - 15mmhg to induce electrical activity). This is an old procedure used only as a life saving means until an electrical pacemaker is brought to the patient.[15]
Transcutaneous pacing
Transcutaneous pacing (TCP), also called external pacing, is recommended for the initial stabilization of hemodynamically significant bradycardias of all types. The procedure is performed by placing two pacing pads on the patient's chest, either in the anterior/lateral position or the anterior/posterior position. The rescuer selects the pacing rate, and gradually increases the pacing current (measured in mA) until electrical capture (characterized by a wide QRS complex with a tall, broad T wave on the ECG) is achieved, with a corresponding pulse. Pacing artifact on the ECG and severe muscle twitching may make this determination difficult. External pacing should not be relied upon for an extended period of time. It is an emergency procedure that acts as a bridge until transvenous pacing or other therapies can be applied.
Transvenous pacing (temporary)
Transvenous pacing, when used for temporary pacing, is an alternative to transcutaneous pacing. A pacemaker wire is placed into a vein, under sterile conditions, and then passed into either the right atrium or right ventricle. The pacing wire is then connected to an external pacemaker outside the body. Transvenous pacing is often used as a bridge to permanent pacemaker placement. It can be kept in place until a permanent pacemaker is implanted or until there is no longer a need for a pacemaker and then it is removed.
Permanent pacing

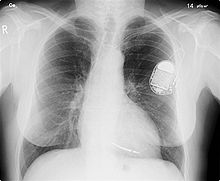
Permanent pacing with an implantable pacemaker involves transvenous placement of one or more pacing electrodes within a chamber, or chambers, of the heart. The procedure is performed by incision of a suitable vein into which the electrode lead is inserted and passed along the vein, through the valve of the heart, until positioned in the chamber. The procedure is facilitated by fluoroscopy which enables the physician or cardiologist to view the passage of the electrode lead. After satisfactory lodgement of the electrode is confirmed the opposite end of the electrode lead is connected to the pacemaker generator.
The pacemaker generator is an hermetically sealed device containing a power source, usually a lithium battery, a sensing amplifier which processes the electrical manifestation of naturally occurring heart beats as sensed by the heart electrodes, the computer logic for the pacemaker and the output circuitry which delivers the pacing impulse to the electrodes.
Most commonly, the generator is placed below the subcutaneous fat of the chest wall, above the muscles and bones of the chest. However, the placement may vary on a case by case basis.
The outer casing of pacemakers is so designed that it will rarely be rejected by the body's immune system. It is usually made of titanium, which is inert in the body.
Basic pacemaker function
Modern pacemakers usually have multiple functions. The most basic form monitors the heart's native electrical rhythm. When the pacemaker doesn't sense a heartbeat within a normal beat-to-beat time period, it will stimulate the ventricle of the heart with a short low voltage pulse. This sensing and stimulating activity continues on a beat by beat basis.
The more complex forms include the ability to sense and/or stimulate both the atrial and ventricular chambers.
| I | II | III | IV | V |
|---|---|---|---|---|
| Chamber(s) paced | Chamber(s) sensed | Response to sensing | Rate modulation | Multisite pacing |
| O = None | O = None | O = None | O = None | O = None |
| A = Atrium | A = Atrium | T = Triggered | R = Rate modulation | A = Atrium |
| V = Ventricle | V = Ventricle | I = Inhibited | V = Ventricle | |
| D = Dual (A+V) | D = Dual (A+V) | D = Dual (T+I) | D = Dual (A+V) |
Biventricular Pacing (BVP)
A biventricular pacemaker, also known as CRT (cardiac resynchronization therapy) is a type of pacemaker that can pace both ventricles (right and left) of the heart. By pacing both sides of the heart, the pacemaker can resynchronize a heart that does not beat in synchrony, which is common in heart failure patients. CRT devices have three leads, one in the atrium, one in the right ventricle, and a final one is inserted through the coronary sinus to pace the left ventricle. CRT devices are shown to reduce mortality and improve quality of life in groups of heart failure patients.[17][18][19]. CRT can be combined with an implantable cardioverter-defibrillator (ICD) [20].
Advancements in pacemaker function
One unrealized advancement in pacemaker function could mimic nature by utilizing various bodily input parameters such as CO2 - O2 at in arterial-vein system, body temperature, ATP levels, Adrenaline, etc. Instead of producing a static, predetermined heart rate, or intermittent control, a Dynamic Pacemaker could compensate for both actual respiratory loading and potentially anticipated respiratory loading. A Dynamic Pacemaker would require sensory technology for which heart-rate regulation parameters must first be acutely identified. Dynamic Pacemaking technology could also be applied to future artificial hearts. Advances in transitional tissue welding would support this and other artificial organ/joint/tissue replacement efforts. Stem cells may or may not be of interest to transitional tissue welding.
When first invented, pacemakers controlled only the rate at which the heart's two largest chambers, the ventricles, beat.
Many advancements have been made to enhance the control of the pacemaker once implanted. Many of these enhancements have been made possible by the transition to microprocessor controlled pacemakers. Pacemakers that control not only the ventricles but the atria as well have become common. Pacemakers that control both the atria and ventricles are called dual-chamber pacemakers. Although these dual-chamber models are usually more expensive, timing the contractions of the atria to precede that of the ventricles improves the pumping efficiency of the heart and can be useful in congestive heart failure.
Rate responsive pacing allows the device to sense the physical activity of the patient and respond appropriately by increasing or decreasing the base pacing rate via rate response algorithms.
The DAVID trials[21] have shown that unnecessary pacing of the right ventricle can lead to heart failure and an increased incidence of atrial fibrillation. The newer dual chamber devices can keep the amount of right ventricle pacing to a minimum and thus prevent worsening of the heart disease.
Pacemaker Patient Considerations
Pacemaker Insertion
A pacemaker is typically inserted into the patient through a simple surgery using a local anesthetic. The patient is usually given a drug for relaxation. An incision is made in the left shoulder area below the collar bone where the pacemaker is actually housed in the patient's body. The lead or leads (the number of leads varies depending on the type of pacemaker) are fed into the heart through a large vein using a fluoroscope to monitor the progress of lead insertion. A temporary drain may be installed and removed the following day. The actual surgery may take about an hour.
The patient should exercise reasonable care about the wound as it heals.
Following surgery there is a followup session during which the pacemaker is checked using a portable device that can communicate with the pacemaker and allows a technician to determine the settings such as pacing threshold.
Pacemaker Patient Identification Card
International Pacemaker Patient Identification Cards patient data (between others, sympton primary, ECG, aetiology), pacemaker center (doctor, hospital), IPG (rate, mode, date of implantation, MFG, type) and lead [22] [23].
Living With a Pacemaker
Periodic Pacemaker Checkups
Once the pacemaker is inserted and functional, it is periodically checked to ensure the device is operational and is performing well. Typically, a long distance check is performed via telephone every three months and a more thorough check is made once a year. At the time of the more thorough checkup, a device is used that will communicate with the pacemaker in order to read operational statistics kept by the device as well as to read its current status such as estimated battery life.
Battery life of the pacemaker will vary depending on how often the device is actually pacing the heart. Typically battery life is estimated at eight years though it may vary in a range of five to ten years. One of the purposes of the periodic pacemaker check is to monitor battery reserves and to estimate battery life remaining.
Lifestyle Considerations
A patient's lifestyle is usually not modified to any great degree after insertion of a pacemaker. There are a few activities that are unwise such as full contact sports and activities that involve intense magnetic fields.
The pacemaker patient may find that some types of everyday actions need to be modified. For instance, the shoulder harness of a vehicle seatbelt may be uncomfortable if the harness should fall across the pacemaker insertion site.
Any kind of an activity that involves intense magnetic fields should be avoided. This includes activities such as arc welding or maintaining heavy equipment that may generate intense magnetic fields.
Some medical procedures may require the use of antibiotics to be administered before the procedure. The patient should inform all medical personnel that the patient does have a pacemaker. Some standard medical procedures such as the use of Magnetic resonance imaging or MRI may be ruled out by the patient having a pacemaker.
Other devices with pacemaker function
Sometimes devices resembling pacemakers, called ICDs (implantable cardioverter-defibrillators) are implanted. These devices are often used in the treatment of patients at risk from sudden cardiac death. An ICD has the ability to treat many types of heart rhythm disturbances by means of pacing, cardioversion, or defibrillation.
| I | II | III | IV |
|---|---|---|---|
| Shock chamber | Antitachycardia pacing chamber | Tachycardia detection | Antibradycardia pacing chamber |
| O = None | O = None | E = Electrogram | O = None |
| A = Atrium | A = Atrium | H = Hemodynamic | A = Atrium |
| V = Ventricle | V = Ventricle | V = Ventricle | |
| D = Dual (A+V) | D = Dual (A+V) | D = Dual (A+V) |
| ICD-S | ICD with shock capability only |
| ICD-B | ICD with bradycardia pacing as well as shock |
| ICD-T | ICD with tachycardia (and bradycardia) pacing as well as shock |
See also
External links
References
- ^ McWilliam JA (1889). "Electrical stimulation of the heart in man". Br Med J. 1: 348–50.
{{cite journal}}:|access-date=requires|url=(help); Cite has empty unknown parameter:|month=(help). Partial quote in "Electrical Stimulation of the Heart in Man - 1889", Heart Rhythm Society, Accessed May 11, 2007. - ^ Lidwell M C, "Cardiac Disease in Relation to Anaesthesia" in Transactions of the Third Session, Australasian Medical Congress, Sydney, Australia, Sept. 2-7 1929, p 160.
- ^ a b Mond H, Sloman J, Edwards R (1982). "The first pacemaker". Pacing and clinical electrophysiology : PACE. 5 (2): 278–82. PMID 6176970.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Aquilina O, "A brief history of cardiac pacing", Images Paediatr Cardiol 27 (2006), pp.17-81.
- ^ Furman S, Szarka G, Layvand D, "Reconstruction of Hyman's second pacemaker", Pacing Clin Electrophysiol.2005 May;28(5):446-453
- ^ Harvard Gazette: Paul Maurice Zoll
- ^ Weirich W, Gott V, Lillehei C: The treatment of complete heart block by the combined use of a myocardial electrode and an artificial pacemaker. Surg. Forum 1957;8;360-363
- ^ Success Stories : Larsson, Arne : St. Jude Medical
- ^ "Furman S, Schwedel JB" An intracardiac pacemaker for Stokes-Adams Seizures N Eng J Med 1959; 261:943-948"
- ^ "Permanent Transvenous Pacing in 1962", Parsonnet V, PACE,1:285, 1978
- ^ "Preliminary Investigation of the Development of a Permanent Implantable Pacemaker Using an Intracardiac Dipolar Electrode", Parsonnet V, Zucker I R, Asa M M, Clin. Res., 10:391, 1962
- ^ "How It Happened: My Recollection of Early Pacing", Lageren H, PACE: Pacing and Clinical Electrophysiology 1.1, Jan. 1978, pp 140-143
- ^ "Intracardiac Stimulation for Complete Heart Block", Lageren H, Acta. Chir. Sca., 125:562, 1963
- ^ Jean Jaques Welti:Biography, Heart Rhythm Foundation
- ^ (Cite_Journal)Percussion pacing in a three year-old girl with complete heart block during cardiac catheterization. C Eich, A Bleckmann and T. Paul, retrieved from http://bja.oxfordjournals.org/cgi/content/full/95/4/465
- ^ Bernstein A, Daubert J, Fletcher R, Hayes D, Lüderitz B, Reynolds D, Schoenfeld M, Sutton R (2002). "The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group". Pacing Clin Electrophysiol. 25 (2): 260–4. PMID 11916002.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cleland JGF, Daubert J-C, Erdmann E, et al; the Cardiac Resynchronization — Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005 March 7 Fulltext. PMID 15753115.
- ^ Bardy GH, Lee KL, Mark DB, et al for the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352:225–237
- ^ Cleland J, Daubert J, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L (2005). "The effect of cardiac resynchronization on morbidity and mortality in heart failure". N Engl J Med. 352 (15): 1539–49. doi:10.1056/NEJMoa050496. PMID 15753115.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bristow M, Saxon L, Boehmer J, Krueger S, Kass D, De Marco T, Carson P, DiCarlo L, DeMets D, White B, DeVries D, Feldman A (2004). "Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure". N Engl J Med. 350 (21): 2140–50. doi:10.1056/NEJMoa032423. PMID 15152059.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wilkoff BL, Cook JR, Epstein AE, et al.: Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the Dual-chamber and VVI Implantable Defibrillator (DAVID) Trial. JAMA 2002, 288: 3115–3123. [1]
- ^ European Pacemaker Patient Identification card
- ^ Eucomed
- ^ a b Bernstein A, Camm A, Fisher J, Fletcher R, Mead R, Nathan A, Parsonnet V, Rickards A, Smyth N, Sutton R (1993). "North American Society of Pacing and Electrophysiology policy statement. The NASPE/BPEG defibrillator code". Pacing Clin Electrophysiol. 16 (9): 1776–80. PMID 7692407.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
