Protein allergy
This article or section is in a state of significant expansion or restructuring. You are welcome to assist in its construction by editing it as well. If this article or section has not been edited in several days, please remove this template. If you are the editor who added this template and you are actively editing, please be sure to replace this template with {{in use}} during the active editing session. Click on the link for template parameters to use.
This redirect was last edited by 165.190.89.146 (talk | contribs) 14 years ago. (Update timer) |
Protein allergies are among the most common allergies, especially seen in young children. A protein is vital to correct cellular function. Its structure is a polypeptide backbone, and it is made from an amino acid sequence. The folding of the protein gives a cell its function. Four types of weak interactions create protein folding. A protein can have a variety of functions, determined by the folding of the protein.
There are many ways that proteins are regulated in the cell, three of which are feedback inhibition, phosphorylation, and GTP-binding proteins. There are a variety of ways of protein consumption, mainly through food intake. When a person with a protein allergy absorbs specific foods, many symptoms can arise. Some symptoms are not severe, merely an annoyance; others can be life threatening. When an allergic reaction occurs, there are treatments that can terminate the reaction. There are also ways to avoid the foods that cause the reaction, while still being able to maintain a healthy lifestyle.
Protein structure
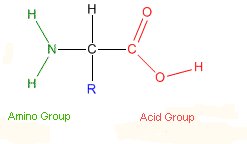
A protein is made from a long chain of amino acids (also known as a polypeptide chain linked via peptide bonds[1]. The higher order structure of a protein depends entirely on the sequence of amino acids which form its primary sequence, as various noncovalent interactions between these amino acids ensure proper protein folding. Proteins have specific amino acid sequences, which all identical proteins share. [2] The twenty different amino acids differ in their side chains, which are relatively large and somewhat polar. These individual amino acids are known as monomers, in the polymer chain known as the protein, which assembles through polymerization. [3]
Levels of protein organization
A protein's secondary structure is created by hydrogen-bond interactions between the amide and carboxyl groups of the amino acid backbone. Secondary structure includes the formation of alpha helices and beta sheets. [4] The tertiary structure is the overall shape of the protein, and is usually driven by the protein's tendency to orient hydrophobic amino acid sidechains internally, although hydrogen bonding, ionic interactions and disulfide bonds also help to stabilize proteins in the tertiary state. [5] Quaternary structure is the overall combination of polypeptide subunits to form the functional unit. [6]All levels of protein structure are based on the previous level. If there is an error in the primary structure of the protein this will carry to the higher levels.
Protein folding
Protein folding is essential to the overall function of the individual protein. The polypeptide chain is often very long and flexible, this leads to a wide variety of ways for a protein to fold. Noncovalent bonds are the only force controlling protein folding. They provide the protein with the power to control their shape and provide structure. While a single noncovalent bond is very weak, a combination of many weak bonds provide the needed strength and structure for a given protein.There are three types of noncovalent bonds that aid in protein folding. They are as follows: electrostatic attractions, hydrogen bonds, and van deer Waals attractions. Hydrophobic interactions are often considered a fourth type of weak interaction that hold proteins together. [7].
Another factor that needs to be considered during protein folding is the type of side chains present in the specific amino acid of a protein. Polar and nonpolar side chains can greatly affect the folding of a protein and in turn its function. A polar side chain is known as a hydrophilic side chain. Hydrophilic means "water loving", therefore these specific side chains arrange towards the outside of the structure. This is because they form hydrogen bonds with water and other polar groups. Common polar side chains are:arginine, glutamine, and histidine. [8]. In contrast to hydrophilic side chains are those of the nonpolar category which are considered to be hydrophobic side chains or "water hating". Hydrophobic side chains include: phenylalanine, leucine, valine, and trytophan. [9]. Hydrophobic side chains attempt to avoid contact with water and other polar molecules, and in turn are often found on the inside of a protein.
The final folded structure of a protein its considered to be the protein's conformation.[10]. The needed information for the correct protein folding is found in a proteins amino acid sequence. This sequence allows the protein to fold into is desired three-dimensional shape. This is often considered to be the proteins overall conformation. Proper protein folding is done with the aid of molecular chaperones. These proteins bind to a partially folded chain and help them to fold along the most energetically favored pathway [11]. Two common folding patterns seen in proteins are the alpha helix and beta sheets.
Functionality
The function of a protein is directly determined by its structure, specifically the aforementioned noncovalent bonds. Proteins interact with other molecules at unique protein binding sites on the ligand.[12]
Proteins can have a myriad of functions, including as the enzymatic catalysts which facilitate essential reactions in cells.[13] Proteins can also act as a cell signal receptor, essential to initiating cellular responses to chemical signals,[14] or as motor proteins, which are involved with movement of or within individual cells.[15] Another example of protein function is that of structural proteins, which enable cell flexibility and support stability.
Allergic response
Allergic reactions are reactions that are hypersensitive to substances that are usually harmless. Hypersensitivities are categorized according to the parts of the immune system that are attacked and the amount of time it takes for the response to occur. There are four types of hypersensitivity reactions: Type 1, Immediate IgE-mediated, Type 2, Cytotoxic, Type 3, Immune complex-mediated, and Type 4, Delayed cell-mediated.[16] The pathophysiology of allergic responses can be divided into two phases. The first is an acute response that occurs immediately after exposure to an allergen. This phase can either subside or progress into a "late phase reaction" which can substantially prolong the symptoms of a response, and result in tissue damage.
Acute response

In the early stages of allergy, a type I hypersensitivity reaction against an allergen, encountered for the first time, causes a response in a type of immune cell called a TH2 lymphocyte, which belongs to a subset of T cells that produce a cytokine called interleukin-4 (IL-4). These TH2 cells interact with other lymphocytes called B cells, whose role is production of antibodies. Coupled with signals provided by IL-4, this interaction stimulates the B cell to begin production of a large amount of a particular type of antibody known as IgE. Secreted IgE circulates in the blood and binds to an IgE-specific receptor (a kind ofFc receptor called FcεRI) on the surface of other kinds of immune cells called mast cells and basophils, which are both involved in the acute inflammatory response. The IgE-coated cells, at this stage are sensitized to the allergen.[17]
If later exposure to the same allergen occurs, the allergen can bind to the IgE molecules held on the surface of the mast cells or basophils. Cross-linking of the IgE and Fc receptors occurs when more than one IgE-receptor complex interacts with the same allergenic molecule, and activates the sensitized cell. Activated mast cells and basophils undergo a process called degranulation, during which they release histamine and other inflammatory chemical mediators (cytokines, interleukins,leukotrienes, and prostaglandins) from their granules into the surrounding tissue causing several systemic effects, such as vasodilation, mucous secretion,nerve stimulation and smooth muscle contraction. This results in rhinorrhea, itchiness, dyspnea, and anaphylaxis. Depending on the individual, allergen, and mode of introduction, the symptoms can be system-wide (classical anaphylaxis), or localized to particular body systems; asthma is localized to the respiratory system and eczema is localized to the dermis.[17]
Late-phase response
After the chemical mediators of the acute response subside, late phase responses can often occur. This is due to the migration of other leukocytes such as neutrophils,lymphocytes, eosinophils and macrophages to the initial site. The reaction is usually seen 2–24 hours after the original reaction.[18] Cytokines from mast cells may also play a role in the persistence of long-term effects. Late phase responses seen in asthma are slightly different from those seen in other allergic responses, although they are still caused by release of mediators from eosinophils, and are still dependent on activity of TH2 cells.[19]
Common allergy-causing foods
| High Protein Food | Protein Content (in grams) |
|---|---|
| Bacon | 25 |
| Roast Chicken | 25 |
| Peanut Butter | 7 |
| Broccoli | 2 |
| Almonds (quarter cup) | 8 |
| Cashews (quarter cup) | 5 |
| Salmon | 39.9 |
| White Fish | 67 |
| Low-Fat Yogurt | 8 |
| Tofu | 8 |
| Cheddar Cheese | 25 |
Peanuts are a very popular cause of allergic reactions. Peanut allergies can be outgrown by many infants by the time they become school-aged. Not really a nut, peanuts are a member of the bean family. Many people with a peanut allergy do not show signs of an allergic reaction to other types of beans, although tests may show an allergy is present.[21]
Tree nuts grow on trees. Some of these include: pecans, pistachios, pine nuts, and walnuts. A person can show signs of an allergy to one specific type of nut or to many types.[22]
Seeds, including sesame seeds and poppy seeds, contain oils where protein is present, causing an allergic reaction.[23]
Egg allergies affect about one in fifty children. This allergy, however, is commonly lost by the time a child is five. Although allergies can be caused by the yolk, the white part of the egg is typically the major allergy causing portion.[24]
Milk is another popular allergy causing food. Milk allergies can come from cow's milk, goat's milk, or sheep's milk. Many children who cannot tolerate milk also have a hard time tolerating cheese or other products derived from milk. A very small portion of children with a milk allergy, roughly ten percent, will have a reaction to beef. Beef contains a small amount of protein that is present in cow's milk.[25]
Other foods include: soy, wheat, fish, shellfish, fruits, vegetables, spices, synthetic and natural colors, and chemical additives.
Symptoms
Symptoms of allergies vary from person to person. The amount of food needed to trigger a reaction also varies from person to person. Symptoms vary depending on the severity of the allergy, and they can appear in as little as a few minutes or may take up to an hour. Symptoms affect the skin, gastrointestinal tract, and in severe cases, the respiratory tract and blood circulation.
Skin symptoms
A common skin symptom is hives. Hives are seen as red, itchy bumps. Edema, another common symptom, is the swelling of the skin. Swelling of the eyes and swelling of the lips are also common during an allergic reaction. A less severe symptom is eczema, a dry and bumpy rash, also known as atopic dermatitis. Eczema is a type of skin rash that is inherited and triggered by an irritant, mainly food allergies.
Gastrointestinal symptoms
These symptoms include: itchy mouth with bumps, stomachache, nausea, vomiting, diarrhea, bloody stool in infants and children, and a taste of metal that lingers in the mouth.

Respiratory and blood circulation
Serious danger regarding allergies can begin when the respiratory tract or blood circulation is infected. Less serious symptoms are runny nose, coughing, and constant clearing of the throat. This are signs that more serious symptoms may be seen. These serious symptoms are closing of the windpipe, which leads to trouble swallowing and problems breathing. These can be indicated through wheezing and a blue coloring of the lips and skin. Poor blood circulation leads to a weak pulse, pale skin, and fainting.[26]
A severe case of an allergic reaction, caused by symptoms affecting the respiratory tract and blood circulation, is called anaphylaxis. When symptoms are shown where breathing is impaired and circulation is affected, the person is said to be in anaphylactic shock. Anaphylaxis is where IgE Antibodies are involved, and areas of the body that are not in direct contact with the food get infected and show symptoms.[27] This occurs because no nutrients are circulated throughout the body, causing the widening of blood vessels. The blood vessels widen, and blood pressure decreases, which leads to the loss of consciousness. Those with asthma or an allergy to peanuts, tree nuts, or seafood are at greater risk for anaphylaxis.[28]
Diagnosis
There are three common types of allergy testing: skin prick test, blood test, and food challenges. An allergist can perform these tests, and they can also go in further depth regarding the results.
- For skin prick tests, a tiny board with protruding needles is used. The allergens are placed either on the board or directly on the skin. The board is then placed on the skin, in order to puncture the skin and for the allergens to enter the body. If a hive appears, the person will be positive for the allergy. The down fall to this test is that it only works for for IgE antibodies. Allergic reactions caused by other antibodies cannot be detected. [29]
- Blood testing is another way to test for allergies; however, it poses the same disadvantage and only detects IgE allergens and does not work for every possible allergen. RAST, RadioAllergoSorbent Test, is used to detect IgE antibodies present to a certain allergen. The score taken from the RAST test is compared to predictive values, taken from a specific type of RAST test. If the score is higher than the predictive values, there is a great chance the allergy is present in the person. One advantage of this test is that it can test many allergens at one time. [30]
- Food challenges are tests that work for allergens other than those caused by IgE allergens. The allergen is given to the person in the form of a pill, so the person can ingest the allergen directly. The person is watched for signs and symptoms. The problem with food challenges is that they must be performed in the hospital under careful watch, due to the possibility of anaphylaxis. [31]
Treatment
There are treatments for an allergic reaction. Among the first time the reaction occurs, it is most beneficial to take the person to the emergency room, where proper action may be taken. Other treatments include: epinephrine, antihistamines, and steroids.
Epinephrine

Epinephrine, also known as adrenaline, is a common medication used to treat allergic reactions. Epinephrine reverses the allergic reaction by improving blood circulation. This is done by tightening blood vessels in order to increase the heart beat and circulation to bodily organs. Epinephrine is produces naturally in the body. It is produced during "flight-or-fight" response. When a person is presented with a dangerous situation, the adrenal gland is triggered to release adrenaline; this gives the person an increased heart rate and more energy to try to fight off the danger being imposed on the individual. Epinephrine is also prescribed by a physician in a form that is self-injectable. This is what is called an epi-pen.[32]
Antihistamines

Antihistamines are also used to treat allergic reactions. Antihistamines block the action of histamines, which causes blood vessels to lose their stiffness and cause itchiness. The most common antihistamine given for food allergies is diphenhydramine, also known as Benedryl. Antihistamines relieve symptoms. When it comes to dealing with anaphylaxis, however, they do not completely improve the dangerous symptoms that affect breathing.[33]
Steroids
Steroids are used to calm down the immune system cells that are attacked by the chemicals released during an allergic reaction. This form of treatment in the form of a nasal spray should not be used to treat anaphylaxis, for it only relieves symptoms in the area in which the steroid is in contact. Another reason steroids should not be used to treat anaphylaxis is due to the long amount of time it takes to reduce inflammation and start to work. Steroids can also be taken orally or through injection. By taking a steroid in these manners, every part of the body can be reached and treated, but a long time is usually needed for these to take effect.[34]
Avoidance
In order to avoid an allergic reaction, a strict diet can be followed. It is hard to tell what amount of food can trigger a reaction, so complete avoidance should be followed. In some cases, reactions can be triggered by more than eating foods, and these exposures should try to be avoided. These exposures include: skin contact, inhalation, kissing, participation in sports, blood transfusions, cosmetics, and alcohol.[35]
When avoiding certain foods in order to lessen the risk of reaction, it can be hard to maintain the proper amounts of nutrients. The proper amount of fat and carbohydrates should be maintained. Vitamins and minerals can also be lost and should be maintained in order to live healthily. The chart below shows alternative sources where important nutrients can be obtained when an allergy is present.
| Nutrient | Allergen | Alternative Source |
|---|---|---|
| Vitamin A | Milk | Spinach, potato, squash, carrot |
| Vitamin D | Milk | Fortified alternative "milks" and juices, margarine |
| Vitamin E | Peanut | Green leafy vegetables, vegetable oils, grains |
| Thiamin | Soy, wheat | Pork, beef, beans, grains |
| Riboflavin | Milk, egg, soy, wheat | Meats, leafy green vegetables, grains |
| Niacin | Wheat, peanut | Meats, beans, enriched grains |
| Vitamin B12 | Milk, egg | Meats |
| Folate | Soy | Leafy green vegetables, beans |
| Pantothenic acid | Milk, Egg | Meats, fruits, vegetables, grains |
| Calcium | Milk | leafy green vegetables, beans, calcium-fortified drinks |
| Chromium | Peanut | Whole grains |
| Iron | Wheat, soy | Meat, beans, dried fruits, iron-fortified grains |
| Magnesium | Soy, peanut | Fruits, vegetables, grains |
| Manganese | Peanut | Leafy green vegetables, whole grains |
| Phosphorus | Milk, soy | Poultry meats, carbonated beverages |
| Selenium | Egg | Meat, grains |
| Zinc | Soy | Meat, beans |
Bibliography
Footnotes
- ^ Freeman 53
- ^ Alberts 121
- ^ Freeman 48
- ^ Freeman 53
- ^ Freeman 54
- ^ Freeman 56
- ^ Alberts 123
- ^ Alberts 126
- ^ Alberts 126
- ^ Alberts 124
- ^ Alberts 125
- ^ Alberts 141
- ^ Freeman 44
- ^ Freeman 44
- ^ Freeman 44
- ^ Nester 414
- ^ a b Janeway, Charles (2001). Immunobiology; Fifth Edition. New York and London: Garland Science. pp. e–book. ISBN 0-8153-4101-6.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help). - ^ Grimbaldeston MA, Metz M, Yu M, Tsai M, Galli SJ (2006). "Effector and potential immunoregulatory roles of mast cells in IgE-associated acquired immune responses". Curr. Opin. Immunol. 18 (6): 751–60. doi:10.1016/j.coi.2006.09.011. PMID 17011762.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Holt PG, Sly PD (2007). "Th2 cytokines in the asthma late-phase response". Lancet. 370 (9596): 1396–8. doi:10.1016/S0140-6736(07)61587-6. PMID 17950849.
- ^ highproteinfoods.net
- ^ Sicherer 62
- ^ Sicherer 63
- ^ Sicherer 63
- ^ Sicherer 63
- ^ Sicherer 64
- ^ van Ree 1
- ^ Sicherer 12
- ^ www.foodallergy.org
- ^ Sicherer 185
- ^ Sicherer 187-88
- ^ Sicherer 189
- ^ Sicherer 133
- ^ Sicherer 131
- ^ Sicherer 134
- ^ Sicherer 151-158
- ^ Sicherer 162
Sources
- Alberts, Bruce, Dennis Bray, Karen Hopkin, Alexander Johnson, Julian Lewis, Martin Raff, Keith Roberts, and Peter Walter. "Protein Structure and Function." Essential Cell Biology. Edition 3. New York: Garland Science, Taylor and Francis Group, LLC, 2010. Pg 120-170.
- Freeman, Scott. "Protein Structure and Function." ' 'Biological Science.' ' Edition 3. San Francisco, California: Pearson Education Inc. 2008. Pg 43-65.
- http://foodallergy.org/srction/a. 2008. Accessed 25 Mar 2010.
- http://medicalert.org. 2010. Accessed 25 Mar 2010.
- http://www.aaaai.org. 2010. Accessed 25 Mar 2010.
- http://www.cfsan.fda.gov. 2010. Accessed 27 Mar 2010.
- http://www.foodallergyinitiative.org. 2009. Accessed 27 Mar 2010.
- http://www.highproteinfoods.net. 2004. Accessed 21 Mar 2010.
- http://www.mssm.edu/jaffe_food_allergy. 2010. Accessed 25 Mar 2010.
- Nester, Eugene W., Denise G. Anderson, C. Evans Roberts, Jr, Martha T. Nester. "Immunologic Disorders." Microbiology: A Human Perspective. Edition 6. New York: McGraw-Hill Companies, Inc. 2009. Pg 414-428.
- Sicherer, Scott H. M.D., Understanding and Managing Your Child's Food Allergy. Baltimore: The Johns Hopkins University Press, 2006.
- Wikimedia.org
- van Ree, Ronald, and Laurian Zuidmeer. "Lipid transfer Protein Allergy: Primary Food Allergy or Pollen/Food Syndrome in Some Cases." Current Opinion in Allergy and Clinical Immunology. Vol 7: pg 269-273. June 2007. Web: 4 Feb 2010.
