Hydroxycarboxylic acid receptor 2
| HCAR2 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | HCAR2, GPR109A, HCA2, HM74a, HM74b, NIACR1, PUMAG, Puma-g, Niacin receptor 1, hydroxycarboxylic acid receptor 2 | ||||||||||||||||||||||||||||||||||||||||||||||||||
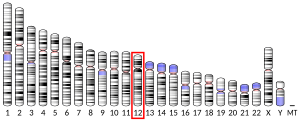
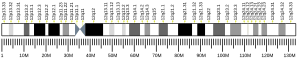
| External IDs | OMIM: 609163; MGI: 1933383; HomoloGene: 4391; GeneCards: HCAR2; OMA:HCAR2 - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Hydroxycarboxylic acid receptor 2 (HCA2), also known as niacin receptor 1 (NIACR1) and GPR109A,[5] is a protein which in humans is encoded by the HCAR2 gene.[6][7][8][9] HCA2, like the other hydroxycarboxylic acid receptors HCA1 and HCA3, is a Gi/o-coupled G protein-coupled receptor (GPCR).[10][11] The primary endogenous agonists of HCA2 are β-D-hydroxybutyric acid and butyric acid (and their conjugate bases, β-hydroxybutyrate and butyrate).[10][11] HCA2 is also a high-affinity biomolecular target for niacin (aka nicotinic acid).[8][9]
HCA2 activation inhibits lipolytic and atherogenic activity (i.e., it inhibits the breakdown of fats and the development of atherosclerosis), induces vasodilation (i.e., the dilation of blood vessels), and is responsible for mediating niacin-induced flushing.[12]
Function
HCA2 is a high-affinity Gi/Go-coupled G protein-coupled receptor (GPCR) for nicotinic acid (niacin),[8][9] and is a member of the nicotinic acid receptor family of GPCRs. HCA2 activation inhibits lipolytic and atherogenic activity (i.e., it inhibits the breakdown of fats and the development of atherosclerosis), induces vasodilation (i.e., the dilation of blood vessels), and is responsible for niacin-induced flushing.[13]
5-oxo-ETE
The mouse ortholog of HCA2, Niacr1, has been proposed to mediate the ability of 5-oxo-ETE, a member of the 5-HETE family of eicosanoids, to stimulate the production of steroidogenic acute regulatory protein mRNA, Steroidogenic acute regulatory protein, and thereby progesterone in mouse cultured MA-10 Leydig cells.[14] Human tissues respond to 5-oxo-ETE and other 5-HETE family members though the OXER1 G protein-coupled receptor. The roles, if any, of Niacr1 in the response of leydig cells to other 5-HETE family members, of Niacr1 in the response of other mouse cells to 5-HETE family members, and the role of HCA2 in the response of human tissues to 5-HETE family members has not been determined.
Clinical significance
HCA2 is an important biomolecular target of niacin which is a widely prescribed drug for the treatment of dyslipidemia and to increase HDL cholesterol but whose therapeutic use is limited by flushing.[15] In HCA2 knockout mice, the effects of niacin on both lipids[16] and flushing[17] is eliminated. Furthermore, in arrestin beta 1 knockout mice, niacin's effect on flushing is greatly reduced while the lipid modifying effects are maintained.[18] At high doses, niacin produces marked anti-inflammatory effects in a variety of tissues – including the brain, gastrointestinal tract, skin, and vascular tissue – through activation of HCA2.[19][20][21][22] Niacin has also been shown to attenuate neuroinflammation in part through NIACR1 binding;[19] consequently, HCA2 has been identified as a potential therapeutic target for treating neuroimmune disorders such as multiple sclerosis and Parkinson's disease.[19][22]
The precise mechanism of action of niacin therapeutic effects has not been fully elucidated, but appears to work in part through activation of HCA2 which reduces the levels of intracellular cAMP thereby inhibiting lipolysis in adipocytes.[23] In contrast, the flushing effect is due to HCA2 activation of ERK 1/2 MAP kinase[24] mediated by arrestin beta 1.[18] Activation of MAP kinase in turn causes release of prostaglandin D2 from Langerhans cells in the skin.[25]
Ligands
Full agonists of HCA2 include:
- β-D-hydroxybutyric acid and β-hydroxybutyrate[10][11]
- Butyric acid and butyrate[26][27]
- Niacin (also known as vitamin B3 and nicotinic acid)[10][11]
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000182782 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000045502 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Offermanns S, Colletti SL, Lovenberg TW, Semple G, Wise A, IJzerman AP (June 2011). "International Union of Basic and Clinical Pharmacology. LXXXII: Nomenclature and Classification of Hydroxy-carboxylic Acid Receptors (GPR81, GPR109A, and GPR109B)". Pharmacological Reviews. 63 (2): 269–90. doi:10.1124/pr.110.003301. PMID 21454438.
- ^ Takeda S, Kadowaki S, Haga T, Takaesu H, Mitaku S (June 2002). "Identification of G protein-coupled receptor genes from the human genome sequence". FEBS Letters. 520 (1–3): 97–101. doi:10.1016/S0014-5793(02)02775-8. PMID 12044878.
- ^ "Entrez Gene: GPR109A G protein-coupled receptor 109A".
- ^ a b c Wise A, Foord SM, Fraser NJ, Barnes AA, Elshourbagy N, Eilert M, Ignar DM, Murdock PR, Steplewski K, Green A, Brown AJ, Dowell SJ, Szekeres PG, Hassall DG, Marshall FH, Wilson S, Pike NB (March 2003). "Molecular identification of high and low affinity receptors for nicotinic acid". The Journal of Biological Chemistry. 278 (11): 9869–74. doi:10.1074/jbc.M210695200. PMID 12522134.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c Soga T, Kamohara M, Takasaki J, Matsumoto S, Saito T, Ohishi T, Hiyama H, Matsuo A, Matsushime H, Furuichi K (March 2003). "Molecular identification of nicotinic acid receptor". Biochemical and Biophysical Research Communications. 303 (1): 364–9. doi:10.1016/S0006-291X(03)00342-5. PMID 12646212.
- ^ a b c d Offermanns S, Colletti SL, Lovenberg TW, Semple G, Wise A, IJzerman AP (June 2011). "International Union of Basic and Clinical Pharmacology. LXXXII: Nomenclature and Classification of Hydroxy-carboxylic Acid Receptors (GPR81, GPR109A, and GPR109B)". Pharmacological Reviews. 63 (2): 269–90. doi:10.1124/pr.110.003301. PMID 21454438.
- ^ a b c d S Offermanns, SL Colletti, AP IJzerman, TW Lovenberg, G Semple, A Wise, MG Waters. "Hydroxycarboxylic acid receptors". IUPHAR/BPS Guide to Pharmacology. International Union of Basic and Clinical Pharmacology. Retrieved 13 July 2018.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ "HCA2 receptor". International Union of Basic and Clinical Pharmacology. Retrieved 24 March 2016.
- ^ "HCA2 receptor". International Union of Basic and Clinical Pharmacology. Retrieved 24 March 2016.
- ^ Cooke M, Di Cónsoli H, Maloberti P, Cornejo Maciel F (May 2013). "Expression and function of OXE receptor, an eicosanoid receptor, in steroidogenic cells". Molecular and Cellular Endocrinology. 371 (1–2): 71–8. doi:10.1016/j.mce.2012.11.003. PMID 23159987.
- ^ Pike NB (December 2005). "Flushing out the role of GPR109A (HM74A) in the clinical efficacy of nicotinic acid". The Journal of Clinical Investigation. 115 (12): 3400–3. doi:10.1172/JCI27160. PMC 1297267. PMID 16322787.
- ^ Tunaru S, Kero J, Schaub A, Wufka C, Blaukat A, Pfeffer K, Offermanns S (March 2003). "PUMA-G and HM74 are receptors for nicotinic acid and mediate its anti-lipolytic effect". Nature Medicine. 9 (3): 352–5. doi:10.1038/nm824. PMID 12563315.
- ^ Benyó Z, Gille A, Kero J, Csiky M, Suchánková MC, Nüsing RM, Moers A, Pfeffer K, Offermanns S (December 2005). "GPR109A (PUMA-G/HM74A) mediates nicotinic acid-induced flushing". The Journal of Clinical Investigation. 115 (12): 3634–40. doi:10.1172/JCI23626. PMC 1297235. PMID 16322797.
- ^ a b Walters RW, Shukla AK, Kovacs JJ, Violin JD, DeWire SM, Lam CM, Chen JR, Muehlbauer MJ, Whalen EJ, Lefkowitz RJ (May 2009). "beta-Arrestin1 mediates nicotinic acid-induced flushing, but not its antilipolytic effect, in mice". The Journal of Clinical Investigation. 119 (5): 1312–21. doi:10.1172/JCI36806. PMC 2673863. PMID 19349687.
- ^ a b c Offermanns S, Schwaninger M (April 2015). "Nutritional or pharmacological activation of HCA(2) ameliorates neuroinflammation". Trends in Molecular Medicine. 21 (4): 245–55. doi:10.1016/j.molmed.2015.02.002. PMID 25766751.
Neuroinflammatory cells express HCA2, a receptor for the endogenous neuroprotective ketone body β-hydroxybutyrate (BHB) as well as for the drugs dimethyl fumarate (DMF) and nicotinic acid, which have established efficacy in the treatment of MS and experimental stroke, respectively. This review summarizes the evidence that HCA2 is involved in the therapeutic effects of DMF, nicotinic acid, and ketone bodies in reducing neuroinflammation.
- ^ Chai JT, Digby JE, Choudhury RP (May 2013). "GPR109A and vascular inflammation". Current Atherosclerosis Reports. 15 (5): 325. doi:10.1007/s11883-013-0325-9. PMC 3631117. PMID 23526298.
This interest is generated especially because of the continuing exploration of niacin's "pleiotropic" mechanisms of action and its potential in the "cross-talk" between metabolic and inflammatory pathways. As GPR109A's primary pharmacological ligand in clinical use, niacin has been used for over 50 years in the treatment of cardiovascular disease, mainly due to its favourable effects on plasma lipoproteins. However, it has become apparent that niacin also possesses lipoprotein-independent effects that influence inflammatory pathways mediated through GPR109A. In addition to its G-protein-mediated effects, recent evidence has emerged to support alternative GPR109A signalling via adaptive protein β-arrestins.
- ^ Graff EC, Fang H, Wanders D, Judd RL (February 2016). "Anti-inflammatory effects of the hydroxycarboxylic acid receptor 2". Metabolism. 65 (2): 102–13. doi:10.1016/j.metabol.2015.10.001. PMID 26773933.
HCA2 is highly expressed on immune cells, including macrophages, monocytes, neutrophils and dermal dendritic cells, among other cell types. ... Recent studies demonstrate that HCA2 mediates profound anti-inflammatory effects in a variety of tissues, indicating that HCA2 may be an important therapeutic target for treating inflammatory disease processes.
- ^ a b Wakade C, Chong R (December 2014). "A novel treatment target for Parkinson's disease". Journal of the Neurological Sciences. 347 (1–2): 34–8. doi:10.1016/j.jns.2014.10.024. PMID 25455298.
GPR109A and its agonists are known to exert anti-inflammatory actions in the skin, gut and retina.
- ^ Zhang Y, Schmidt RJ, Foxworthy P, Emkey R, Oler JK, Large TH, Wang H, Su EW, Mosior MK, Eacho PI, Cao G (August 2005). "Niacin mediates lipolysis in adipose tissue through its G-protein coupled receptor HM74A". Biochemical and Biophysical Research Communications. 334 (2): 729–32. doi:10.1016/j.bbrc.2005.06.141. PMID 16018973.
- ^ Richman JG, Kanemitsu-Parks M, Gaidarov I, Cameron JS, Griffin P, Zheng H, Guerra NC, Cham L, Maciejewski-Lenoir D, Behan DP, Boatman D, Chen R, Skinner P, Ornelas P, Waters MG, Wright SD, Semple G, Connolly DT (June 2007). "Nicotinic acid receptor agonists differentially activate downstream effectors". The Journal of Biological Chemistry. 282 (25): 18028–36. doi:10.1074/jbc.M701866200. PMID 17452318.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Tang Y, Zhou L, Gunnet JW, Wines PG, Cryan EV, Demarest KT (June 2006). "Enhancement of arachidonic acid signaling pathway by nicotinic acid receptor HM74A". Biochemical and Biophysical Research Communications. 345 (1): 29–37. doi:10.1016/j.bbrc.2006.04.051. PMID 16674924.
- ^ Kasubuchi M, Hasegawa S, Hiramatsu T, Ichimura A, Kimura I (April 2015). "Dietary gut microbial metabolites, short-chain fatty acids, and host metabolic regulation". Nutrients. 7 (4): 2839–49. doi:10.3390/nu7042839. PMC 4425176. PMID 25875123.
Short-chain fatty acids (SCFAs) such as acetate, butyrate, and propionate, which are produced by gut microbial fermentation of dietary fiber, are recognized as essential host energy sources and act as signal transduction molecules via G-protein coupled receptors (FFAR2, FFAR3, OLFR78, GPR109A) and as epigenetic regulators of gene expression by the inhibition of histone deacetylase (HDAC). Recent evidence suggests that dietary fiber and the gut microbial-derived SCFAs exert multiple beneficial effects on the host energy metabolism not only by improving the intestinal environment, but also by directly affecting various host peripheral tissues.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Hoeppli RE, Wu D, Cook L, Levings MK (February 2015). "The environment of regulatory T cell biology: cytokines, metabolites, and the microbiome". Frontiers in Immunology. 6: 61. doi:10.3389/fimmu.2015.00061. PMC 4332351. PMID 25741338.
Specific species that have been recognized by their high levels of butyrate production include Faecalibacterium prausnitzii and the cluster IV and XIVa of genus Clostridium ... Administration of acetate, propionate, and butyrate in drinking water mimics the effect of Clostridium colonization in germ-free mice, resulting in an elevated Treg frequency in the colonic lamina propria and increased IL-10 production by these Tregs (180, 182). Of the three main SCFAs, butyrate has been found to be the most potent inducer of colonic Tregs. Mice fed a diet enriched in butyrylated starches have more colonic Tregs than those fed a diet containing propinylated or acetylated starches (181). Arpaia et al. tested an array of SCFAs purified from commensal bacteria and confirmed butyrate was the strongest SCFA-inducer of Tregs in vitro (180). Mechanistically, it has been proposed that butyrate, and possibly propionate, promote Tregs through inhibiting histone deacetylase (HDAC), causing increased acetylation of histone H3 in the Foxp3 CNS1 region, and thereby enhancing FOXP3 expression (180, 181). Short-chain fatty acids partially mediate their effects through G-protein coupled receptors (GPR), including GPR41, GPR43, and GPR109A. GPR41 and GPR43 are stimulated by all three major SCFAs (191), whereas GPR109A only interacts with butyrate (192).
{{cite journal}}: CS1 maint: unflagged free DOI (link)
Figure 1: Microbial-derived molecules promote colonic Treg differentiation.