Angiotensin-converting enzyme 2
Angiotensin converting enzyme 2 (ACE2) is an enzyme expressed on the membrane of many cell types, including epithelial cells of the pulmonary alveolus and small intestine enterocytes.[5] It is an exopeptidase that catalyses the conversion of angiotensin II to angiotensin 1–7, which acts as a vasodilator.[6][7] It also converts angiotensin I to nanopeptide angiotensin[1–9].[8] ACE2 is a single-pass type I membrane protein.[9] It serves as the entry point into human cells for some coronaviruses.
Coronavirus entry point
ACE2 has been shown to be the entry point into human cells for some coronaviruses, including SARS-CoV, the virus that causes SARS.[10][11] A number of studies have identified that the entry point is the same for SARS-CoV-2,[12] the virus that causes COVID-19.[13][14][15][16]
This might lead some to believe that decreasing the levels of ACE2, in cells, might help in fighting the infection. On the other hand, ACE2 has been shown to have a protective effect against virus-induced lung injury by increasing the production of the vasodilator angiotensin 1–7.[17]Template:Secondary source required
In fact, the interaction of the spike protein of the virus with the ACE2 induces a drop in the levels of ACE2 in cells.[11]
Multiple regulatory bodies have recommended continuing ACE inhibitor therapy.[18][19]
See also
References
- ^ a b c GRCh38: Ensembl release 89: ENSG00000130234 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000015405 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H (June 2004). "Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis". The Journal of Pathology. 203 (2): 631–7. doi:10.1002/path.1570. PMID 15141377.
- ^ Keidar S, Kaplan M, Gamliel-Lazarovich A (February 2007). "ACE2 of the heart: From angiotensin I to angiotensin (1-7)". Cardiovascular Research. 73 (3): 463–9. doi:10.1016/j.cardiores.2006.09.006. PMID 17049503.
- ^ Wang W, McKinnie SM, Farhan M, Paul M, McDonald T, McLean B, et al. (August 2016). "Angiotensin-Converting Enzyme 2 Metabolizes and Partially Inactivates Pyr-Apelin-13 and Apelin-17: Physiological Effects in the Cardiovascular System". Hypertension. 68 (2): 365–77. doi:10.1161/HYPERTENSIONAHA.115.06892. PMID 27217402.
- ^ Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, et al. (September 2000). "A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9". Circulation Research. 87 (5): E1–9. doi:10.1161/01.res.87.5.e1. PMID 10969042.
- ^ Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H (June 2004). "Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis". The Journal of Pathology. 203 (2): 631–7. doi:10.1002/path.1570. PMID 15141377.
- ^ Li F (October 2013). "Receptor recognition and cross-species infections of SARS coronavirus". Antiviral Research. 100 (1): 246–54. doi:10.1016/j.antiviral.2013.08.014. PMC 3840050. PMID 23994189.
- ^ a b Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, et al. (August 2005). "A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury". Nature Medicine. 11 (8): 875–9. doi:10.1038/nm1267. PMID 16007097.
- ^ "What are the official names of the disease and the virus that causes it?". Q&A on coronaviruses. World Health Organization. Retrieved 22 February 2020.
- ^ Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. (March 2020). "A pneumonia outbreak associated with a new coronavirus of probable bat origin". Nature. 579 (7798): 270–273. doi:10.1038/s41586-020-2012-7. PMID 32015507.
- ^ Xu X, Chen P, Wang J, Feng J, Zhou H, Li X, et al. (March 2020). "Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission". Science China. Life Sciences. 63 (3): 457–460. doi:10.1007/s11427-020-1637-5. PMID 32009228.
- ^ Lewis, Ricki (2020-02-20). "COVID-19 Vaccine Will Close in on the Spikes". DNA Science Blog. Public Library of Science.
{{cite web}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D (2020). "Structure, function and antigenicity of the SARS-CoV-2 spike glycoprotein". bioRxiv: 2020.02.19.956581. doi:10.1101/2020.02.19.956581.
- ^ Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, et al. (July 2005). "Angiotensin-converting enzyme 2 protects from severe acute lung failure". Nature. 436 (7047): 112–6. Bibcode:2005Natur.436..112I. doi:10.1038/nature03712. PMID 16001071.
- ^ "ESC Says Continue Hypertension Meds Despite COVID-19 Concern". Medscape. Retrieved 2020-03-20.
- ^ Caldeira D, Alarcão J, Vaz-Carneiro A, Costa J (July 2012). "Risk of pneumonia associated with use of angiotensin converting enzyme inhibitors and angiotensin receptor blockers: systematic review and meta-analysis". Bmj. 345 (jul11 1). BMJ: e4260. doi:10.1136/bmj.e4260. PMC 3394697. PMID 22786934.
Our results suggest an important role of ACE inhibitors, but not ARBs, in reducing the risk of pneumonia. These data may discourage the withdrawal of ACE inhibitors in some patients with tolerable adverse events (namely, cough) who are at particularly high risk of pneumonia. ACE inhibitors also lowered the risk of pneumonia related mortality, mainly in patients with established disease, but the robustness of the evidence was weaker.
External links
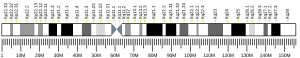
- Human ACE2 genome location and ACE2 gene details page in the UCSC Genome Browser.
Further reading
- Turner AJ, Hiscox JA, Hooper NM (June 2004). "ACE2: from vasopeptidase to SARS virus receptor". Trends in Pharmacological Sciences. 25 (6): 291–4. doi:10.1016/j.tips.2004.04.001. PMID 15165741.
- Katovich MJ, Grobe JL, Huentelman M, Raizada MK (May 2005). "Angiotensin-converting enzyme 2 as a novel target for gene therapy for hypertension". Experimental Physiology. 90 (3): 299–305. doi:10.1113/expphysiol.2004.028522. PMID 15640278.
- Ferrario CM, Trask AJ, Jessup JA (December 2005). "Advances in biochemical and functional roles of angiotensin-converting enzyme 2 and angiotensin-(1-7) in regulation of cardiovascular function". American Journal of Physiology. Heart and Circulatory Physiology. 289 (6): H2281–90. doi:10.1152/ajpheart.00618.2005. PMID 16055515.
- Jia HP, Look DC, Hickey M, Shi L, Pewe L, Netland J, et al. (2006). "Infection of human airway epithelia by SARS coronavirus is associated with ACE2 expression and localization". Advances in Experimental Medicine and Biology. 581: 479–84. doi:10.1007/978-0-387-33012-9_85. ISBN 978-0-387-26202-4. PMID 17037581.
- Lazartigues E, Feng Y, Lavoie JL (2007). "The two fACEs of the tissue renin-angiotensin systems: implication in cardiovascular diseases". Current Pharmaceutical Design. 13 (12): 1231–45. doi:10.2174/138161207780618911. PMID 17504232.
- Raizada MK, Ferreira AJ (August 2007). "ACE2: a new target for cardiovascular disease therapeutics". Journal of Cardiovascular Pharmacology. 50 (2): 112–9. doi:10.1097/FJC.0b013e3180986219. PMID 17703127.
- Dean RG, Burrell LM (2007). "ACE2 and diabetic complications". Current Pharmaceutical Design. 13 (26): 2730–5. doi:10.2174/138161207781662876. PMID 17897017.
- Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ (October 2000). "A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase". The Journal of Biological Chemistry. 275 (43): 33238–43. doi:10.1074/jbc.M002615200. PMID 10924499.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, et al. (September 2000). "A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9". Circulation Research. 87 (5): E1–9. doi:10.1161/01.res.87.5.e1. PMID 10969042.
- Vickers C, Hales P, Kaushik V, Dick L, Gavin J, Tang J, et al. (April 2002). "Hydrolysis of biological peptides by human angiotensin-converting enzyme-related carboxypeptidase". The Journal of Biological Chemistry. 277 (17): 14838–43. doi:10.1074/jbc.M200581200. PMID 11815627.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Crackower MA, Sarao R, Oudit GY, Yagil C, Kozieradzki I, Scanga SE, et al. (June 2002). "Angiotensin-converting enzyme 2 is an essential regulator of heart function". Nature. 417 (6891): 822–8. Bibcode:2002Natur.417..822C. doi:10.1038/nature00786. PMID 12075344.
- Harmer D, Gilbert M, Borman R, Clark KL (December 2002). "Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme". FEBS Letters. 532 (1–2): 107–10. doi:10.1016/S0014-5793(02)03640-2. PMID 12459472.
- Donoghue M, Wakimoto H, Maguire CT, Acton S, Hales P, Stagliano N, et al. (September 2003). "Heart block, ventricular tachycardia, and sudden death in ACE2 transgenic mice with downregulated connexins". Journal of Molecular and Cellular Cardiology. 35 (9): 1043–53. doi:10.1016/S0022-2828(03)00177-9. PMID 12967627.
- Clark HF, Gurney AL, Abaya E, Baker K, Baldwin D, Brush J, et al. (October 2003). "The secreted protein discovery initiative (SPDI), a large-scale effort to identify novel human secreted and transmembrane proteins: a bioinformatics assessment". Genome Research. 13 (10): 2265–70. doi:10.1101/gr.1293003. PMC 403697. PMID 12975309.
- Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, et al. (November 2003). "Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus". Nature. 426 (6965): 450–4. Bibcode:2003Natur.426..450L. doi:10.1038/nature02145. PMID 14647384.
- Wong SK, Li W, Moore MJ, Choe H, Farzan M (January 2004). "A 193-amino acid fragment of the SARS coronavirus S protein efficiently binds angiotensin-converting enzyme 2". The Journal of Biological Chemistry. 279 (5): 3197–201. doi:10.1074/jbc.C300520200. PMID 14670965.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Towler P, Staker B, Prasad SG, Menon S, Tang J, Parsons T, et al. (April 2004). "ACE2 X-ray structures reveal a large hinge-bending motion important for inhibitor binding and catalysis". The Journal of Biological Chemistry. 279 (17): 17996–8007. doi:10.1074/jbc.M311191200. PMID 14754895.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Pelini P (January 2019). Therapeutic strategies for the treatment of the new coronavirus COVID-19. Researchgate (Thesis). Rome, Italy: Sapienza University. doi:10.13140/RG.2.2.32240.40966.